Abstract
Background:
Bone bruise patterns after anterior cruciate ligament (ACL) rupture may predict the presence of intra-articular pathology and help explain the mechanism of injury. Lateral femoral condyle (LFC) and lateral tibial plateau (LTP) bone bruises are pathognomic to ACL rupture. There is a lack of information regarding medial tibial plateau (MTP) and medial femoral condyle (MFC) bone bruises.
Purpose:
To summarize the prevalence and location of MTP bone bruises with acute ACL rupture and to determine the predictors of MTP bone bruises.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Inclusion criteria were patients who underwent ACL reconstruction between February 2015 and November 2017, magnetic resonance imaging (MRI) within 90 days of injury, and participation in the database. Exclusion criteria included previous ipsilateral surgery, multiligamentous injuries, and incomplete imaging. Due to the large number of cases remaining (n = 600), 150 patients were selected randomly from each year included in the study, for a total of 300 patients. Two readers independently reviewed injury MRI scans using the Costa-Paz bone bruise grading system. Logistic regression was used to identify factors associated with MTP bone bruises.
Results:
Included were 208 patients (mean age, 23.8 years; mean body mass index, 25.6). The mechanism of injury was noncontact in 59% of injuries, with over half from soccer, basketball, and football. The median time from injury to MRI scan was 12 days. Of the 208 patients, 98% (203/208) had a bone bruise, 79% (164/208) had an MTP bone bruise, and 83% (172/208) had bruises in both medial and lateral compartments. The most common pattern, representing 46.6% of patients (97/208), was a bruise in all 4 locations (MFC, LFC, MTP, and LTP). Of the 164 MTP bruises, 160 (98%) involved the posterior third of the plateau, and 161 were grade 1. The presence of an MFC bruise was the only independent risk factor for an MTP bruise (odds ratio, 3.71). The resulting nomogram demonstrated MFC bruise, sport, and mechanism of injury were the most important predictors of an MTP bruise.
Conclusion:
MTP bruise after acute ACL rupture was as prevalent as lateral bruises. The presence of a posterior MTP bruise suggested anterior tibial translation at the time of injury and could portend more medial compartment pathology at the time of injury than previously recognized.
Keywords: anterior cruciate ligament rupture, bone bruise, bone marrow pattern
The anterior cruciate ligament (ACL) is the primary passive restraint to anterior tibial translation and it also plays a critical role in the rotational stability of the knee. 9 Roughly 250,000 ACL surgeries are performed each year in the United States with the number steadily increasing. 2 About 70% of ACL ruptures occur due to noncontact mechanisms of injury. Historically, this has been thought of as a hyperextension, pivoting mechanism of injury. 14
Bone bruises are detected in a minimum of 80% of patients with an acute ACL rupture. More recent studies have observed bone bruise in 98% to 100% of ACL tears. 6 Bone bruise, which is visualized on magnetic resonance imaging (MRI), represents post-traumatic findings of the bone including hemorrhage, edema, and microtrabecular fracture. It classically presents as geographic areas of low-signal intensity on T1-weighted images and high-signal intensity on T2-weighted images. 3,5 Whereas some authors differentiate impaction fractures from bone bruises, most studies of ACL injury have considered both injuries together as a spectrum of the same injury. 7 Radiologic studies have shown that bone bruises persist for at least 12 to 14 weeks. 4
During an ACL injury, external forces and the ligament rupture result in an impact between the femoral and tibial articular cartilage, which transfers forces to the bone, resulting in bone bruises. 12 Lateral tibial plateau and lateral femoral condyle bone bruises in the setting of an acute ACL rupture are well-established in the literature as pathognomonic and support a hyperextension, pivoting mechanism of injury. 13 Less attention has been devoted to the posterior medial tibial plateau (MTP) bone bruise. Several small studies have reported the prevalence of MTP bone bruises anywhere between 26% and 60%. 1,10,17 The presence of medial bone bruises is important because this represents not only an increased burden of injury to the knee but also perhaps a different mechanism of injury.
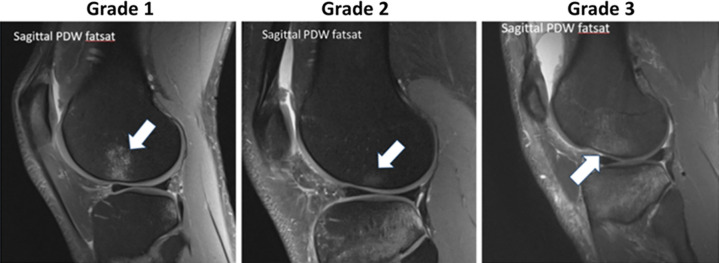
Costa-Paz et al 3 classified bone bruises on MRI into 3 categories: grade 1 is defined as a diffuse signal distant from the subjacent articular surface, grade 2 is a localized signal with contiguity to the subjacent articular surface, and grade 3 involves disruption or depression of the normal contour of the cortical surface (Figure 1).
Figure 1.
Bone bruise classification on magnetic resonance imaging according to Costa-Paz et al 3 : grade 1, diffuse signal distant from the subjacent articular surface; grade 2, localized signal with contiguity to the subjacent articular surface; and grade 3, disruption or depression of the normal contour of the cortical surface. PDW fatsat, proton density–weighted fat saturation. White arrow represents the extent of bone bruise based on its grade.
The presence and location of bone bruise overlap was used in a recent study with a 3-dimensinoal (3-D) model to determine the position of an ACL injury. They showed over 2.5 cm of anterior tibial translation and there was no statistically significant difference between male and female positions of injury. 11 The presence of a posterior MTP bone bruise in the setting of ACL rupture could suggest a different mechanism of injury than commonly thought. It could also represent damage to the structures of the medial compartment, including the posterior horn of the medial meniscus, ramp lesions, and articular cartilage.
Our objectives for this study were 2-fold: first, to summarize the prevalence and location of MTP bone bruises in the setting of acute ACL ruptures; and second, to determine the predictors of MTP bone bruises.
Methods
The protocol for this retrospective study was approved by our institutional review board. We performed a retrospective chart review of patients undergoing ACL reconstruction by 8 surgeons at 1 institution over a 2-year time period. Inclusion criteria were patients undergoing ACL reconstruction between February 2015 and November 2017, MRI scan within 90 days of injury, and participation in the database. Exclusion criteria included previous ipsilateral surgery, multiligamentous injuries, and incomplete imaging. There were 705 patients who underwent ACL reconstruction in this time period. Of these, 15 multiligamentous injuries, 88 revision ACL reconstructions, and 2 simultaneous bilateral reconstructions were excluded. Due to the large number of cases remaining (n = 600), 150 patients were selected randomly from each year included in the study for a total of 300 patients. No criterion was used for randomization since all patients had already met the inclusion criteria and computer randomization was used. This was done to prevent the seasonal variation in ACL injury mechanism from biasing the results of the study. Of the 300 patients, an additional 6 were excluded for previous ipsilateral surgery, 32 had unavailable imaging outside of our institution, and 38 had their MRI scan >90 days from injury, making bruising presence less reliable to be attributed to the acute injury, thus leaving a cohort of 224 patients. There were then 6 more exclusions for incomplete imaging sequences, and 10 exclusions for missing date of injury, resulting in a final cohort of 208 patients (Figure 2).
Figure 2.
STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) diagram of patient inclusion in the study. ACLR, anterior cruciate ligament reconstruction; DOI, date of injury; multilig, multiligamentous; MRI, magnetic resonance imaging; OSH, open-source hardware. ACLR: Anterior cruciate Ligament Reconstruction, Multilig: Multilgamentous knee injury, Revision: Revision ACL reconstruction, OSH: outside hospital, DOI: date of injury
Two independent readers (J.M.B., orthopaedic sports fellow; C.C., radiology fellow) reviewed all 208 MRI scans recording bone bruise location and grade as well as the presence or absence of meniscal and cartilage pathology. Bone bruise grading was based on the Costa-Paz et al 3 classification (Figure 1). 12 There were 71 patients who had discrepancies in the bone bruise read. The two readers then met for a second read and were able to reach a consensus on all patients. MRI scans were obtained from multiple magnets with magnetic strengths ranging from 0.2 to 3 T. Protocols varied depending on the individual magnets, but all included sagittal and coronal 2-dimensional (2-D) fast spin-echo (FSE) fat-suppression proton density (PD) weighted, sagittal 2-D FSE T2/intermediate weighted (Iw), coronal 2D FSE T1, axial 2D FSE PD/Iw, and 3D FSE/gradient-echo sequences. All MRI sequences were used to assess the imaging findings. Readers were blinded to the history of the injury and the demographics of the patients.
Statistical Analysis
The outcomes of our study are the prevalence and location of bone bruises associated with ACL rupture as well as the factors associated with the MTP bone bruise. As a result, data regarding prevalence and location of bone bruises were summarized using counts and percentages. Continuous variables such as age and body mass index (BMI) followed normal distribution, thus were summarized using means and ranges and were compared using 2-sample t tests between those with and without bone bruises. Categorical variables were summarized using counts and percentages and were compared using Pearson chi square test or Fisher exact test when appropriate. Logistic regression was used to identify factors associated with MTP bone bruises. The logistic regression model results were presented visually with a nomogram. Variables (risk factors) were ranked based on their relative contribution to the models, as assessed by Akaike information criteria (AIC) increase upon removal of the variable from the full model. AIC is a statistics methods that measures model quality, and an AIC of 2 or more justifies a statistically better model. Data management and data analysis were performed in R software (Version 4.0).
Results
The average age of our patients was 23.8 years (range, 13-63 years). Half (104/208) were male and the average BMI was 25.6 (range, 16.3-51.8) (Table 1). The median time to MRI scan was 12 days from the time of injury (range, 0-82 days). The mechanism of injury was noncontact in 59% (123/208) of patients, and over half were from soccer, basketball, and football injuries (113/208). Figure 3 shows the incidence of all bone bruise patterns. We detected a bone bruise in 98% (203/208) of patients; 79% (164/208) of patients had a bone bruise of the MTP, and 83% had bone bruises in both the medial and lateral compartments (172/208). The most common bone bruise pattern, representing 46.6% of patients (97/208), was bruising in all 4 locations. There were no bone bruises in 2.4% (5/208) of patients. Of the 164 MTP bone bruises, 98% (160/164) involved the posterior third of the plateau and 98% (161/164) were classified as grade 1. Approximately 55% (115/208) of patients had a medial femoral condyle (MFC) bone bruise. Of these, 86% (99/115) were in the central third of the condyle.
Table 1.
Demographic Data a
| Variable | Value |
|---|---|
| Age, y | 23.8 (13-63) |
| Sex male/female, n | 104/104 |
| BMI, kg/m2 | 25.6 (16.3-51.8) |
a Data are mean (range) unless otherwise indicated. BMI, body mass index.
Figure 3.

Bone bruise patterns and incidence. LFC, lateral femoral condyle; LTP, lateral tibial plateau; MFC, medial femoral condyle; MTP, medial tibial plateau.
In our regression analysis, the presence of an MFC bone bruise was the only independent risk factor associated with a MTP bone bruise with an odds ratio of 3.71. Gender, MRI magnet strength, age, BMI, mechanism of injury, sport, and days from injury to MRI were not independent risk factors for the presence of a MTP bone bruise. The resulting nomogram and AIC demonstrated that the most important predictors of the MTP bone bruise were the MFC bone bruise, sport, and mechanism of injury (Figure 4).
Figure 4.
Nomogram showing logistic regression model results. BMI, body mass index; LFC, lateral femoral condyle; LTP, lateral tibial plateau; MFC, medial femoral condyle; MRI, magnetic resonance imaging; MTP, medial tibial plateau.
Discussion
Bone bruises are seen frequently in the setting of ACL injuries. They occur due to the force of impact between the tibia and femur during an ACL rupture. The location of bone bruises within specific compartments of the knee can provide insight into the potential injury mechanism. The pivot-shift mechanism of injury for ACL rupture is widely accepted in the literature and is presumed to be primarily responsible for the bone bruise pattern seen after ACL injury. 13 Given this, the existence of medial compartment bone bruises has not been commonly recognized with ACL injury and has only recently been recognized in the literature.
A recent systemic review by Patel et al 12 reported a higher prevalence of lateral compartment bone bruises and concluded that a pivot-shift injury mechanism or multiplanar loading mechanism involving valgus and subsequent anterior tibial translation is responsible for the bone bruise pattern seen after ACL rupture. In another study, Kaplan et al 8 proposed that the medial bone bruise pattern can be explained by a counter-coupe type mechanism as the knee rebounds into a compensatory varus alignment with internal femoral rotation while the tibia remains anteriorly displaced. They contend that these patients have higher risk of injury to the meniscocapsular junction and the posterior horn of the medial meniscus. In our study, we found over 80% of patients with medial bone bruise patterns; the high incidence of posterior MTP bone bruises, coupled with the central MFC bone bruise, supports the hypothesis of anterior tibial translation.
In a recent study, Owusu-Akyaw et al 11 investigated the position of the knee at the time of ACL rupture using a 3-D model to maximize bone bruise overlap. These authors concluded that a combination of anterior tibial translation, valgus, internal tibial rotation, and knee flexion occurred during injury and found that there was no statistically significant difference between male and female positions of injury. The high incidence of bone bruises in the posterior MTP in our study further supports this finding of anterior tibial translation as a component of the injury mechanism.
Wittstein et al 16 investigated bone bruise patterns as well as meniscal tears and reported a 61.6% overall incidence of MTP bone bruise and found no difference between male and female patients. The high incidence of MTP bone bruise found in their study is supported by our findings.
Viskontas et al 15 conducted a literature review to investigate the correlation between ACL bone bruises and injury mechanism. Although they found more lateral than medial bruises overall, they did find an increased incidence of MTP bone bruise with noncontact mechanisms of injury. The majority of these bruises were located in the posterior third of the MTP. They suggested that the noncontact mechanism of injury bone bruise patterns are more consistent with anterior tibial translation and internal tibial rotation. This study supports our findings and hypothesis.
We observed the same frequency of bone bruises in both the medial and the lateral compartments in the setting of acute ACL rupture. Furthermore, we showed that an MFC bone bruise is the only factor associated with a posterior MTP bone bruise. These findings suggest anterior tibial subluxation as a component of the mechanism of injury in the majority of ACL tears.
Limitations
The limitations of this study are its retrospective nature, the loss of some patients due to incomplete or unavailable imaging, and imaging obtained past 90 days from injury. The fact that we did not include all patients at the final analysis but included 150 patients for each year may cause concerns regarding external validity. To prevent bias, we performed a power analysis, which showed that 300 patients would provide enough power. Therefore, we decided to limit the number of patients just to provide enough power and added 150 patients/year. Patients were assigned randomly without a criterion. The initial discrepancies may also be a limitation; however, because patients were randomly chosen from a larger cohort, they represent the larger cohort. Finally, the images were obtained using multiple magnet strengths and nonuniform sequences. This could have affected the precision of assessments, which would make it more difficult to identify factors contributing to variations in signal patterns.
Conclusion
Our study shows that posterior MTP bone bruises in the setting of an acute ACL rupture are as prevalent as pathognomonic lateral bruises. An MFC bone bruise was the only independent risk factor for a MTP bone bruise. The presence of a posterior MTP bone bruise suggests that the mechanism of injury of an ACL rupture involves anterior tibial translation and not just hyperextension and rotation. It also suggests that more medial compartment injury is sustained during ACL rupture than previously recognized. These findings are useful to encourage the clinician to be more aware of medial sided injury in the setting of acute ACL rupture.
Further studies should investigate the implications of posterior MTP bone bruises on other medial compartment pathology, including meniscal tears, ramp lesions, and cartilage pathology as well as patient-reported outcomes measures.
Acknowledgment
Thank you to the Cleveland Clinic orthopaedic patients, staff, and research personnel whose efforts related to regulatory, data collection, patient follow-up, data quality control, analysis, and manuscript preparation have made this consortium successful. Thank you to Alan W. Davis, MD, and Thomas E. Anderson, MD, for contributing cases. Also thank you to Cailin Conner, MA, editor assistant, Cleveland Clinic Foundation, for editorial management.
Authors: Jennifer M. Byrd, MD (Atlantic Orthopaedic Specialists, Virginia Beach, Virginia, USA); Ceylan Colak, MD (Atlantic Orthopaedic Specialists, Virginia Beach, Virginia, USA; and Imaging Institute, Cleveland Clinic, Cleveland, Ohio, USA); Sercan Yalcin, MD (Department of Orthopaedics and Rehabilitation, Yale School of Medicine, New Haven, Connecticut, USA); Cleveland Clinic Sports Medicine, and Carl Winalski, MD (Department of Diagnostic Radiology, Imaging Institute; Department of Biomedical Engineering, Lerner Research Institute; and Program of Advanced Musculoskeletal Imaging, Cleveland Clinic, Cleveland, Ohio, USA); Cleveland Clinic Sports Medicine group: Isaac Briskin, MA (Department of Quantitative Health Services, Cleveland Clinic, Cleveland, Ohio, USA); Lutul D. Farrow, MD (Cleveland Clinic Orthopaedic and Rheumatologic Institute, Cleveland Clinic Foundation, Cleveland, Ohio, USA); Morgan H. Jones, MD, MPH (Division of Sports Medicine, Department of Orthopedic Surgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts, USA); Anthony A. Miniaci, MD, Richard D. Parker, MD, James T. Rosneck, MD, Paul M. Saluan, MD, Gregory J. Strnad, MS (all from Cleveland Clinic Orthopaedic and Rheumatologic Institute, Cleveland Clinic Foundation, Cleveland, Ohio, USA); and Kurt P. Spindler, MD (Department of Orthopaedic Surgery, Cleveland Clinic Florida Region, Weston, Florida, USA).
*All authors are listed in the Authors section at the end of this article.
Final revision submitted April 19, 2022; accepted May 24, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.W. has received research support from Janssen Research and Development and consulting fees from Siemens Medical Solutions. L.D.F. has received hospitality payments from DJO. A.A.M. has received education payments from Arthrex; consulting fees from Amniox Medical, Anika Therapeutics, Arthrosurface, Trice Medical, and Zimmer Biomet; speaking fees, royalties, and honoraria from Arthrosurface; and stock options from Anika Therapeutics. J.T.R. has received speaking fees from Smith & Nephew. P.M.S. has received consulting fees and speaking fees from Arthrex and honoraria from NovoPedics. K.P.S. has received research support from DJO and Smith & Nephew and consulting fees from Flexion Therapeutics, the National Football League, and Novopeds. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Cleveland Clinic (ref No. 06-196).
References
- 1. Ali A, Pillai J, Gulati V, Gibbons C, Roberton B. Hyperextension injuries of the knee: do patterns of bone bruising predict soft tissue injury? Skeletal Radiol. 2018;47(2):173–179. [DOI] [PubMed] [Google Scholar]
- 2. Bates NA, McPherson AL, Rao MB, Myer GD, Hewett TE. Characteristics of inpatient anterior cruciate ligament reconstructions and concomitant injuries. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2778–2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Costa-Paz M, Muscolo DL, Ayerza M, Makino A, Aponte-Tinao L. Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy. 2001;17(5):445–449. [DOI] [PubMed] [Google Scholar]
- 4. Davies NH, Niall D, King LJ, Lavelle J, Healy JC. Magnetic resonance imaging of bone bruising in the acutely injured knee–-short-term outcome. Clin Radiol. 2004;59(5):439–445. [DOI] [PubMed] [Google Scholar]
- 5. Faber KJ, Dill JR, Amendola A, et al. Occult osteochondral lesions after anterior cruciate ligament rupture. Am J Sports Med. 1999;27(4):489–494. [DOI] [PubMed] [Google Scholar]
- 6. Frobell RB, Roos HP, Roos EM, et al. The acutely ACL injured knee assessed by MRI: are large volume traumatic bone marrow lesions a sign of severe compression injury? Osteoarthritis Cartilage. 2008;16(7):829–836. [DOI] [PubMed] [Google Scholar]
- 7. Gorbachova T, Amber I, Beckmann NM, et al. Nomenclature of subchondral nonneoplastic bone lesions. AJR Am J Roentgenol. 2019;213(5):963–982. [DOI] [PubMed] [Google Scholar]
- 8. Kaplan PA, Gehl RH, Dussault RG, Anderson MW, Diduch DR. Bone bruises of the posterior lip of the medial tibial plateau (contrecoup injury) and associated internal derangements of the knee at MR imaging. Radiology. 1999;211(3):747–753. [DOI] [PubMed] [Google Scholar]
- 9. Kocabey Y, Yalçın S, Erdil M, Polat G. An alternative femoral fixation in all-inside anterior cruciate ligament reconstruction: a solution for preventing possible graft loosening. Arthrosc Tech. 2019;8(8):e861–e865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lattermann C, Jacobs CA, Reinke EK, et al. Are bone bruise characteristics and articular cartilage pathology associated with inferior outcomes 2 and 6 years after anterior cruciate ligament reconstruction? Cartilage. 2017;8(2):139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Owusu-Akyaw KA, Kim SY, Spritzer CE, et al. Determination of the position of the knee at the time of an anterior cruciate ligament rupture for male versus female patients by an analysis of bone bruises. Am J Sports Med. 2018;46(7):1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med. 2014;44(2):281–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sanders TG, Medynski MA, Feller JF, Lawhorn KW. Bone bruise patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics. 2000;20(suppl 1):S135–S151. [DOI] [PubMed] [Google Scholar]
- 14. Spindler KP, Schils JP, Bergfeld JA, et al. Prospective study of osseous, articular, and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am J Sports Med. 1993;21(4):551–557. [DOI] [PubMed] [Google Scholar]
- 15. Viskontas DG, Giuffre BM, Duggal N, et al. Bone bruises associated with ACL rupture: correlation with injury mechanism. Am J Sports Med. 2008;36(5):927–933. [DOI] [PubMed] [Google Scholar]
- 16. Wittstein J, Vinson E, Garrett W. Comparison between sexes of bone bruises and meniscal tear patterns in noncontact anterior cruciate ligament injuries. Am J Sports Med. 2014;42(6):1401–1407. [DOI] [PubMed] [Google Scholar]
- 17. Yoon KH, Yoo JH, Kim K-I. Bone bruise and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93(16):1510–1518. [DOI] [PubMed] [Google Scholar]