Abstract
Objective:
We assessed the effects of hope, purpose in life, and religiosity on trajectories of depressive symptoms among middle-aged and older Blacks, with a focus on age differences in these associations.
Methods:
Data come from 1906 respondents from the 2006–2016 Health and Retirement Study. Linear mixed models were estimated and included interactions between age and time and between age and each psychosocial resource.
Results:
Depressive symptoms decreased for Blacks ages 51–64, did not change for those 65–74, and increased among Blacks age 75+. Hope and purpose in life were inversely associated with symptom levels but were not associated with change over time in symptomology. Associations were stronger among the youngest age group and weakest among the oldest. Religiosity was unrelated to depressive symptoms.
Discussion:
Psychosocial resources protect against depressive symptoms in age-dependent ways among middle-aged and older Blacks. Differences in these effects may be related to aging, cohort, and selection effects.
Keywords: resilience, mental health, age differences, African Americans, stress process, protective factors
Introduction
Depression and depressive symptoms are significant public health issues. Depressive symptoms are associated with multiple indicators of poor mental and physical health, including major depressive disorder (Moazen-Zadeh & Assari, 2016), cardiovascular diseases (Xiang & An, 2015), declines in cognitive function (Turner et al., 2015), and specific- and all-cause mortality (Assari et al., 2016; Liwo et al., 2020). Middle-aged and older adults may be at an increased risk of experiencing depressive symptoms due to unexpected changes in employment (Abrams et al., 2021), financial strain (Assari et al., 2020), increased frailty (Mezuk et al., 2012), greater feelings of loneliness (Taylor & Nguyen, 2020), and increases in disability, sleep disturbances, and bereavement (Cole & Dendukuri, 2003). Older Black Americans experience relatively similar age-related risk factors for depressive symptoms as whites (Pickett et al., 2013) but are at an even greater risk for poor mental health due to their experiences of racism, discrimination, and socioeconomic disadvantage (Williams & Williams-Morris, 2000). However, research on Black-White differences in depressive symptoms has been mixed with some studies finding greater symptomology among Black older adult (Abrams & Mehta, 2019; Brown et al., 2020) or older White adults (Mouzon, 2017), and others finding no race differences (Byers et al., 2010).
Numerous explanations have been put forth to explain the similar if not better mental health findings for Black Americans. Resilience and the internal psychosocial resources that contribute to resilience have received increasing attention in aging literature. Compared to interpersonal resources (e.g., social support), internal psychosocial resources are intrinsic to an individual, which makes them primarily within a person’s control. Further, they can be mobilized quickly and provide more immediate cognitive and emotional relief from ongoing stressors. Internal psychosocial resources are also modifiable, which makes them feasible targets for the prevention and management of depressive symptoms and their consequences. Additionally, in the absence of adequate social and economic resources to cope with racism and socioeconomic adversity, internal psychosocial resources may be particularly salient and beneficial for maintaining mental health and emotional well-being (Ryff & Singer, 2008). Thus, the primary objective of the current study is to determine whether hope, purpose in life, and religiosity—three internal psychosocial resources that may be particularly relevant for the mental health of Black people—protect against increases in depressive symptoms among middle-aged and older Black adults. We focus on these three resources because prior research has shown an interrelationship among them (Galek et al., 2015; Stoyles et al., 2015). Moreover, they uniquely contribute to resiliency processes among middle-aged and older Black Americans who grew up in the Black Church and, as a result, received messages of hope and learned religious coping mechanisms that emphasized finding meaning and a purpose in the struggles they faced (Chatters, 2000; Ellison & Levin, 1998; Krause, 2003; Taylor et al., 2003).
The Effect of Internal Psychosocial Resources on Depressive Symptoms and Other Mental Health Outcomes
Hope and Mental Health
To be hopeful is not an expression of wishful thinking. Rather, hope or hopefulness is a deliberate cognitive process that not only reflects a general expectation for positive future events but also incorporates goal-directed thinking and a sense of agency or self-efficacy towards accomplishing future goals (Snyder, 2002). It is this latter characteristic of hope that distinguishes it from similar constructs such as optimism (Alarcon et al., 2013; Bryant & Cvengros, 2004; Ciarrocchi et al., 2008) and contributes to its role as a coping resource.
Most research on hope has focused on younger populations (Arnau et al., 2007; Ciarrochi et al., 2015; Stoyles et al., 2015), clinical settings (Billington et al., 2008; Hirsch & Sirois, 2016; Madan & Pakenham, 2014), and physical health outcomes (Hirsch & Sirois, 2016; Mitchell et al., 2020). Although hope and its negative counterpart, hopelessness, have also been shown to be associated with depressive symptoms (Assari & Lankarani, 2016) and general measures of mental health (Barnett, 2014) in adult populations, limited research exists on the nature of this relationship in community-dwelling middle-age and older adults. One exception is a recent study by Long et al., (2020) that used data from the Health and Retirement Study (HRS) to prospectively examine the effects of hope on multiple health indicators. The study showed that higher baseline levels of hope were associated with a reduced risk of depression, fewer depressive symptoms, and lower levels of negative affect 4 years later. Although informative about the effects of hope on mental health during the “second half of life,” this study did not examine between or within-group differences by race or age despite research suggesting sociodemographic variability in the association between hope and health (Mitchell et al., 2020).
To our knowledge, research on the relationship between hope and depressive symptoms—or other mental health outcomes—is nonexistent for middle-aged and older Black adults. That said, we can surmise that hope also protects against poor mental health in the older Black population from research showing an inverse association between hope and suicidal ideation among Black college students (Davidson et al., 2010) and research showing a positive relationship between hope and life satisfaction among older Blacks (Adams & Jackson, 2000). Moreover, one of the most well-known Biblical quotes is Hebrews KJV 11: “Now faith is the substance of things hoped for, the evidence of things not seen,” which discusses the connection between faith and hope. Older Black Americans have the highest levels of religiosity than any other racial group in the U.S. and are predominantly Protestant Christians (Pew Research Center, 2015); therefore, they are more likely to be exposed to messages of hope such as Hebrews KJV 11. Thus, hope—as an extension of one’s faith—may be particularly relevant for the mental health of Black adults, especially those who identify as being religious. This conjecture, however, represents an important gap in the hope-mental health literature that needs to be addressed.
Purpose in Life and Mental Health
Similar to research on hope and mental health, little is known about the effects of a sense of purpose in life on depressive symptoms among middle-aged and older Black Americans. Purpose in life is also often referred to as “meaning in life” and conveys a sense of directedness and intentionality about life decisions that contributes to their meaningfulness (Ryff, 1989). Among middle-aged and older adults, recent evidence suggests that purpose in life is associated with lower mortality risk (Boyle et al., 2009; Shiba et al., 2021), a reduced incidence of stroke (Kim, Sun, Park, & Peterson, 2013), fewer sleep disturbances (Kim et al., 2015), reduced risk for myocardial infarction (Kim, Sun, Park, Kubzansky et al., 2013), and better maintenance of physical functioning over time (Kim et al., 2017). Regarding mental health, a higher sense of purpose or meaning in life also protects against cognitive decline (Kim et al., 2019) and suicidal ideation (Heisel & Flett, 2016) among older adults, and reduces negative affect and symptoms of depression and anxiety in adults of all ages (Crego et al., 2019, 2021).
Research on the relationship between purpose and mental health in the Black community has primarily included adults of all ages. For instance, in a national sample of Black Americans aged 21 and older, (Park et al., 2020) found that meaning in life was associated with lower depressive symptoms and greater positive affect two and a half years later. Studies exclusively focused on Black Americans in midlife and old age are emerging and their findings thus far suggest a salutary effect on mental health. For instance, in a community sample of Black adults ages 65 and older, Nadimpalli et al. (2015) found that purpose in life was associated with lower odds of reporting a high number of depressive symptoms. Similarly, Yoon et al. (2019) found that purpose in life mediates the relationship between discrimination and depressive symptoms in a national sample of Black adults ages 65 and older. Taken together, purpose in life is a psychosocial resource that protects against depressive symptoms in Black Americans. What is unknown, however, is whether it does so similarly for all ages of older adulthood. Damon et al. (2003) argue that the impact of searching for and identifying one’s purpose may depend on when in the life course each process occurs. A study by Cotton Bronk et al. (2009) provided empirical support for this hypothesis by demonstrating age differences in the relationship between purpose and life satisfaction. Moreover, purpose in life declines with age and does so to a greater extent among the oldest-old compared to the young-old and midlife adults (Pinquart, 2002). Accordingly, among older adults in general and Black older adults in particular, the effects of purpose in life on mental health may also vary by age.
Religiosity and Mental Health
Religion has played a critical role in the lives of Black Americans (Lincoln & Mamiya, 1990; Nguyen, 2020; Taylor et al., 2003). It is deeply embedded in the culture, community, and ethnic identity of Black Americans and religious traditions based on liberation and defiance theology (Cone, 2010) serve as unique resources for dealing with discrimination and other chronic stressors this population faces (Frazier & Lincoln, 1974; Mitchell et al., 2020). Unsurprisingly, Black Americans have the highest levels of religiosity of any racial group in the U.S. (Pew Research Center, 2015). Research consistently identifies higher levels of religiosity among older compared to younger adults (Pew Research Center, 2015; Taylor et al., 2014). Thus, older Black Americans are not only more religious than their older white counterparts but also are more religious than younger Black Americans (Chatters et al., 1999). Consequently, older Black Americans have the highest levels of religiosity among all racial and age groups in the United States. Longitudinal research in the general population indicates that religiosity follows a curvilinear pattern throughout the life span, with religiosity decreasing in early adulthood and increasing beginning in late mid-life (Ingersoll-Dayton et al., 2002). Nevertheless, there is no research, to our knowledge, on changes in religiosity over time specifically among Black Americans.
A robust body of research demonstrates the protective qualities of religiosity, linking it to better mental and physical health and psychological well-being (Chatters, 2000; Koenig et al., 2012; Levin & Chatters, 2008). Researchers in this area posit that there are several possible explanatory mechanisms that link religiosity and health (Ellison & Levin, 1998). First, religiosity can lead to higher levels of social support from fellow congregants, which can protect against health problems and buffer the harmful effects of life stressors (Ellison & Levin, 1998). Specifically, people who are more religiously involved at the organizational level (e.g., frequent church attenders) are more socially integrated within the church support network and participate in more frequent exchanges of church-based social support (Nguyen et al., 2019). Second, religion can influence health through doctrines and practices that discourage lifestyles (e.g., gambling) and behaviors (e.g., alcohol, nicotine, caffeine, and illicit drug use) that adversely affect health. Likewise, some religious groups encourage healthy behaviors that can lead to better health outcomes (e.g., Seventh-Day Adventists’ promotion of a plant-based diet). Positive emotions derived from religious participation and devotional practices can also explain the relationship between religiosity and health (Ellison & Levin, 1998) as can religious coping (Pargament, 1997; Pargament & Raiya, 2007). Specifically, religious cognitions (e.g., “God will never give me more than I can handle” and “God is always with me”) and practices, such as prayer and meditation, can act as stress coping resources that intervene in the stress process by altering the appraisal of stressors. The use of religious coping strategies can lead a person to reassess the meaning and magnitude of stressors and to reappraise stressors as less stressful, more manageable, or more positive (e.g., opportunities for spiritual growth or learning).
Religiosity is a multidimensional construct with organizational (e.g., service attendance), nonorganizational (e.g., prayer, reading religious texts), and subjective (i.e., beliefs about God and religion) domains that encompass different forms of expression and associations with health (Levin et al., 1995). Research on the relationship between religion and mental health has shown that most domains of religiosity, especially organizational religiosity, confer salutary effects on health (Nguyen, 2020). Less is known about the relationship between subjective religiosity and health generally and specifically with regard to changes in depressive symptoms. Preliminary evidence suggests that higher levels of subjective religiosity are associated with lower levels of depressive symptoms in the general adult population (Hudson et al., 2015; Stearns et al., 2018). However, this association is yet to be confirmed specifically among Black Americans. Investigations of subjective religiosity among Black Americans across the life span indicate that it varies across sociodemographic groups including age (Chatters, Taylor et al., 2008; Taylor et al., 1999, 2014). Further, studies focusing on other mental health outcomes have demonstrated that those with higher levels of subjective religiosity report lower levels of psychological distress (Jang & Johnson, 2004; Levin & Taylor, 1998) and are at lower risk for suicidal ideation (Taylor et al., 2011).
Among Black older adults specifically, Chatters et al. (2008a) found that subjective religiosity was associated with a lower likelihood of meeting criteria for any lifetime DSM-IV disorder (Chatters, Bullard et al., 2008) only in the absence of other measures of religiosity. Controlling for organizational and nonorganizational religiosity completely accounted for the association between subjective religiosity and lifetime DSM-IV disorders, which suggest that subjective religiosity may indirectly affect mental health through its effects on other forms of religiosity such as service attendance. Studies on subjective measures of well-being also underscore the beneficial effects of subjective religiosity. For instance, in a community sample of older Blacks in New York City, (Frazier et al., 2005) found that subjective religiosity was related to higher levels of environmental mastery, personal growth, purpose in life, and self-acceptance. Together, this body of literature suggests that subjective religiosity may confer either direct or indirect protection against mental health problems and promote well-being among Black Americans. However, the question of whether there is heterogeneity by age in the religiosity-depressive symptoms relationship among middle-aged and older Blacks remains unanswered.
The Current Study
The current study uses three waves of national data from the HRS (2006–2016) to determine the effect of hope, purpose in life, and religiosity on levels of and changes in depressive symptoms over time among middle-aged and older Black Americans. Prior research has documented a U-shaped relationship between age and depressive symptoms (Abrams & Mehta, 2019; Kessler et al., 1992; Mirowsky & Ross, 1992; Montagnier et al., 2014; Sutin et al., 2013; Wu et al., 2012), including studies of race differences in symptom trajectories that use the HRS and include middle-aged and older Black Americans (Abrams & Mehta, 2019; Liang et al., 2011). Therefore, our analysis begins by assessing the age-depressive symptoms relationship to determine if it is U-shaped in this sample as well. We then focus on elucidating the effects of hope, purpose in life, and religiosity on these trajectories. In addition to testing their direct effect on symptom trajectories, we also test their effects on the rate of change in depressive symptoms (i.e., interaction between each resource and time) and age differences in their effect on symptom levels (interaction between each resource and age). The hypotheses guiding our research are as follows: Among middle-aged and older Black adults:
Depressive symptoms will demonstrate a U-shaped relationship with age;
Higher levels of hope, purpose in life, and subjective religiosity will be associated with lower levels of depressive symptoms and slower rates of increase in symptoms over time; and,
The effects of each psychosocial resources on trajectories of depressive symptoms will differ by age, such that the resources will be less protective among the oldest age group relative to the youngest.
Methods
Data Source and Sample
The HRS is a nationally representative sample of adults ages 51 and older. The survey started in 1992 and collects data on the health and aging experiences of older adults every 2 years. As a supplement to the core interview, the HRS introduced an enhanced face-to-face interview and self-administered psychosocial questionnaire in 2006. One half of the HRS core sample completed the questionnaire in 2006, while the other half completed it in 2008. Each half-sample completes a follow-up interview and questionnaire every 4 years. More details about the HRS sample design and data collection procedures are available elsewhere (Sonnega & Weir, 2014). We combined the 2006 and 2008 half-samples to increase our statistical power and sample size, which resulted in a data set with three waves of psychosocial resource and depressive symptoms data (i.e., Wave 1: 2006/2008, Wave 2: 2010/2012, and Wave 3: 2014/2016). We restricted our analytic sample to community-dwelling Black adults ages 51 and older (n = 2507). Respondents missing data on sociodemographic characteristics (n = 186) were excluded as were respondents missing data on the psychosocial resource or depressive symptoms for all waves (n = 415). The final analytic sample was 1906. Excluded respondents were more likely to be male, widowed, lower educated, and retired or unemployed.
Measures
Depressive Symptoms.
Depressive symptoms were assessed using a modified version of the Center for the Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), which has been shown to be valid among older adults (Karim et al., 2015). Eight yes–no items asked about the presence of the following symptoms: felt depressed, everything an effort, restless sleep, was happy (reverse-coded), felt lonely, felt sad, could not get going, and enjoyed life (reverse-coded). A sum score was created with values ranging from 0 to 8.
Psychosocial Resources.
Three internal psychosocial resources are included in our analyses as time-varying covariates: hope, a sense of purpose in life, and religiosity. All three resources were assessed using a 6-point Likert scale, where 0 = “strongly disagree” and 5 = “strongly agree”. Item responses were averaged to construct each scale. Hope was assessed using two items from Everson et al. (1996) (“I feel it is impossible for me to reach the goals that I like to strive for” and “The future seems hopeless to me and I can’t believe that things are changing for the better”) and two items from Beck et al. (1974) (“I don’t expect to get what I really want” and “There is no use in trying to get something I want because I probably won’t get it”). Each item was reverse-coded such that higher values were indicative of greater hope. The scale was constructed for respondents with data on a minimum of two out of the four items. Purpose in Life was assessed with seven items from Ryff’s scale of psychological wellbeing (Ryff, 1989): “I enjoy making plans for the future and working to make them a reality,” “My daily activities often seem trivial and unimportant to me” (reverse-coded), “I am an active person in carrying out the plans I set for myself,” “I don’t have a good sense of what it is I’m trying to accomplish in life” (reverse-coded), “I sometimes feel as if I’ve done all there is to do in life” (reverse-coded), “I live life one day at a time and don’t really think about the future,” and “I have a sense of direction and purpose in my life”. The scale was constructed for respondents with responses on a minimum of four out of the seven items. Religiosity was assessed with four items: “I believe in a God who watches over me,” “The events in my life unfold according to a divine or greater plan,” “I try to carry my religious beliefs over into all my other dealings in life,” and “I find strength and comfort in my religion”. Responses to a minimum of two items were needed to construct the scale and higher scores represented greater levels of religiosity.
Health Factors.
Age related changes in physical functioning and health may explain change in depressive symptoms over time. We therefore control for the number of functional limitations and diagnosed chronic conditions a person has. Both measures are considered time-varying covariates. Functional limitations were assessed as a count of the number of limitations in activities of daily living including walking, dressing, bathing, eating, getting in and out of bed, and toileting (range: 0–6). Chronic disease burden is a count of eight chronic conditions respondents report ever having (range: 0–8). Conditions include high blood pressure, diabetes, cancer (except skin), lung disease, heart problems, stroke, psychiatric problems, and arthritis.
Sociodemographic Factor.
Demographic and socioeconomic characteristics are from Wave 1 (i.e., baseline, 2006/2008) and include age (51–64 years old vs. 65–74 years old and 75+ years old), gender (male vs. female), nativity (foreign-born vs. U.S.-born), marital status (married vs. divorced/separated, widowed, or never married), education (less than high school vs. high school degree, some college, or college or more), poverty status (not living in poverty vs. living in poverty), and employment status (employed vs. partially retired, retired, or unemployed).
Statistical Analyses
We examined sample characteristics by age and used chi-squared tests to assess age differences in baseline demographic and socioeconomic characteristics. Means and standard deviations for time-varying covariates (i.e., depressive symptoms, the psychosocial resources, and the health factors) were examined by age and for each wave of data collection, but bivariate correlations among all continuous variables were only assessed at baseline. Our multivariate analyses modeled change in depressive systems over time using linear mixed models with a random intercept and random slope for time. Linear mixed models are appropriate for modeling repeated observations across waves that are nested within individuals. Time was modeled as years since baseline (i.e., Wave 1 = 0 years, Wave 2 = 4 years, and Wave 3 = 8 years) and models were built sequentially.
Model 1 includes time, age, and the sociodemographic characteristics. Model 2 adds the three psychosocial resources. We then separately tested several interactions between age and time (i.e., Model 3), hope (Model 4), purpose in life (Model 5), and religiosity (Model 6). Preliminary analyses examined the interaction between time and each psychosocial resource. None of these interactions were statistically significant; therefore, we focused the rest of our analyses on interactions between age and time and age and each psychosocial resource. A significant interaction between age and time would suggest that the rate of change in depressive symptoms differs by age; a significant interaction between age and a psychosocial resource would indicate that there are age differences in the effects of the resource on average levels of depressive symptoms. We evaluated significant interactions in more detail by estimating and graphing the simple slopes for depressive symptoms within each age group and examining age-stratified models. The stratified models added the health factors to test whether they accounted for linear change in depressive symptoms and the effects of the psychosocial resources. Stata 15 was used for all analyses and the significance level was set to p < .05.
Handing of Mortality, Attrition, and Missing Data
To account for the effects of attrition, we also include an indicator for the number of waves of missing depressive symptoms data (i.e., not missing any CES-D time point vs. missing 1 CES-D time point, missing 2 CES-D time points). This approach reduces bias that may stem from data that are not missing at random (e.g., attrition) by directly modeling the joint distribution of the observed data and the probability of missingness (Hedeker & Gibbons, 1997).
Results
Sample Characteristics and Bivariate Associations
Table 1 presents demographic and socioeconomic characteristics of the entire sample and by age. Although the proportion female and the proportion living in poverty were similar across age, significant age differences existed in foreign-born status, marital status, education, and employment, with younger age groups (i.e., ages 51–64 and 65–74) more likely to be foreign-born, married, college educated, and employed than the oldest age group. Younger cohorts were also more likely to have data on depressive symptoms for all three waves of data collection compared to the oldest cohort.
Table 1.
Characteristics of the Sample at Baseline: Health and Retirement Study, 2006–2016 (n = 1906).
| Total Sample (n = 1906) |
51–64 Years Old (n = 773) |
65–74 Years Old (n = 747) |
75+ Years Old (n = 386) |
p-Valuea |
|
|---|---|---|---|---|---|
| Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | ||
| Key Variables | |||||
| Depressive symptoms | 1.68 (2.02) | 1.84 (2.15) | 1.53 (1.92) | 1.65 (1.89) | <.01 |
| Hope | 3.58 (1.33) | 3.67 (1.34) | 3.57 (1.32) | 3.42 (1.30) | <.05 |
| Purpose in life | 3.71 (0.93) | 3.78 (0.95) | 3.75 (0.90) | 3.51 (0.93) | <.001 |
| Religiosity | 4.48 (1.07) | 4.39 (1.20) | 4.57 (0.93) | 4.49 (1.08) | <.01 |
| ADL limitations | 0.48 (1.10) | 0.39 (1.00) | 0.46 (1.11) | 0.68 (1.25) | <.001 |
| Chronic disease burden | 2.22 (1.43) | 1.88 (1.45) | 2.38 (1.36) | 2.61 (1.37) | <.001 |
| Covariates | |||||
| Female | 64.7 | 66.3 | 64.1 | 62.4 | .403 |
| Foreign-born | 5.8 | 5.3 | 7.4 | 3.6 | <.05 |
| Married | 49 | 56.3 | 46.3 | 39.4 | <.001 |
| Divorced/separated | 20.5 | 23.9 | 21.2 | 12.4 | |
| Widowed | 25 | 12.3 | 28 | 44.6 | |
| Never married | 5.6 | 7.5 | 4.6 | 3.6 | |
| Less than high school | 32.5 | 20.6 | 37.8 | 46.4 | <.001 |
| High school | 32.7 | 34 | 34.5 | 26.4 | |
| Some college | 21.5 | 27.9 | 17.7 | 15.8 | |
| College or more | 13.3 | 17.6 | 10 | 11.4 | |
| Living in poverty | 21.3 | 21.8 | 20 | 22.8 | .477 |
| Employed | 26.6 | 50.3 | 14.5 | 2.6 | <.001 |
| Partially retired | 9.6 | 6.7 | 12.7 | 9.3 | |
| Retired | 52 | 27.7 | 63.7 | 78 | |
| Unemployed | 11.9 | 15.4 | 9.1 | 10.1 | |
| Not missing any CES-D time point | 65 | 77.4 | 67.5 | 35.2 | <.001 |
| Missing 1 CES-D time point | 18.5 | 12.2 | 18.7 | 30.6 | |
| Missing 2 CES-D time points | 16.6 | 10.5 | 13.8 | 34.2 |
Note. CES-D = Center for the Epidemiologic Studies Depression Scale.
p-value is for the chi-squared test of age differences in each variable.
Table 2 shows that the mean number of functional limitations and chronic conditions tended to increase across wave, as did mean levels of hope, while mean levels of purpose in life and religiosity showed a slight increase in value followed by a decrease and the mean number of depressive symptoms declined across wave. Bivariate correlations at baseline between each psychosocial resource and depressive symptoms were negative and small to moderate in magnitude (i.e., Table 2, r = −0.05—0.29).
Table 2.
Descriptive Statistics and Bivariate Correlations at Baseline for Time-varying Covariates: Health and Retirement Study, 2006–2016 (n = 1906).
| Mean (SD) |
Bivariate Correlation at Wave 1 |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | (1) | (2) | (3) | (4) | (5) | (6) | |
| (1) Functional limitations | 0.48 (1.10) | 0.62 (1.33) | 0.78 (1.50) | — | |||||
| (2) Chronic disease burden | 2.22 (1.43) | 2.59 (1.49) | 2.86 (1.51) | 0.35*** | — | ||||
| (3) Hope | 3.58 (1.33) | 3.60 (1.34) | 3.71 (1.32) | −0.14*** | −0.21*** | — | |||
| (4) Purpose in life | 3.71 (0.93) | 3.77 (0.93) | 3.69 (0.95) | −0.17*** | −0.21*** | 0.44*** | — | ||
| (5) Religiosity | 4.48 (1.07) | 4.50 (1.06) | 4.48 (1.10) | −0.02 | −0.02 | 0.07** | 0.16*** | — | |
| (6) Depressive symptoms | 1.68 (2.02) | 1.62 (1.97) | 1.61 (2.00) | 0.35*** | 0.31*** | −0.29*** | −0.05* | −0.29*** | — |
Note.
p < .05
p < .01
p < .001.
Age Differences in Trajectories of Depressive Symptoms and the Effect of Psychosocial Resources
In Table 3 we present a series of linear mixed models for depressive symptoms trajectories. The coefficient for time in Models 1 and 2 suggests that depressive symptoms among Black middle-aged and older adults did not change over the three waves of data collection (Model 1: b = 0.01, p = .23; Model 2: b = −0.00, p = .66) and that Black adults ages 65 and older had significantly fewer depressive symptoms (Model 1: age 65–74 b = −0.41, p < .001; age 75+ b = −0.42, p < .001) and psychosocial resources (Model 2: age 65–74 b = −0.43, p < .001; age 75+ b = −0.51, p < .001) than Blacks ages 51–64, net of covariates. Higher levels of hope (Model 2: b = −0.15, p < .001) and purpose in life (Model 2: b = −0.30, p < .001) were associated with fewer depressive symptoms, but religiosity was not. None of the interactions between time and the psychosocial resources were statistically significant (Supplementary Table 1).
Table 3.
Linear Mixed Models for the Effects of Psychosocial Resources and Their Interaction With Age on Depressive Symptoms: Health and Retirement Study, 2006–2016 (n = 1906).
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
Model 6 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fixed Effects | b | SE | b | SE | b | SE | b | SE | b | SE | b | SE |
| Time | 0.01 | 0.01 | 0.00 | 0.01 | −0.03* | 0.01 | −0.03* | 0.01 | −0.03* | 0.01 | −0.03* | 0.01 |
| 65–74 years olda | −0.46*** | 0.10 | −0.43*** | 0.09 | −0.55*** | 0.11 | −1.05*** | 0.21 | −1.32*** | 0.29 | −0.71* | 0.29 |
| 75+ years olda | −0.51*** | 0.13 | −0.51*** | 0.12 | −0.70*** | 0.14 | −1.43*** | 0.26 | −2.17*** | 0.37 | −1.12** | 0.37 |
| Hope | −0.15*** | 0.02 | −0.15*** | 0.02 | −0.25*** | 0.04 | −0.15*** | 0.02 | −0.15*** | 0.02 | ||
| Purpose in life | −0.30*** | 0.04 | −0.30*** | 0.04 | −0.29*** | 0.04 | −0.45*** | 0.05 | −0.30*** | 0.04 | ||
| Religiosity | −0.01 | 0.03 | −0.01 | 0.03 | −0.01 | 0.03 | −0.01 | 0.03 | −0.04 | 0.04 | ||
| 65–74 years old × time | 0.04* | 0.02 | 0.04* | 0.02 | 0.04* | 0.02 | 0.04* | 0.02 | ||||
| 75+ years old × time | 0.08*** | 0.02 | 0.08** | 0.02 | 0.09*** | 0.02 | 0.08*** | 0.02 | ||||
| 65–74 years old × hope | 0.14** | 0.05 | ||||||||||
| 75+ years old × hope | 0.21** | 0.07 | ||||||||||
| 65–74 years old × purpose | 0.20** | 0.07 | ||||||||||
| 75+ years old × purpose | 0.40*** | 0.10 | ||||||||||
| 65–74 years old × religiosity | 0.04 | 0.06 | ||||||||||
| 75+ years old × religiosity | 0.09 | 0.08 | ||||||||||
| Constant | 1.67*** | 0.12 | 3.43*** | 0.21 | 3.48*** | 0.21 | 3.83*** | 0.23 | 4.06*** | 0.25 | 3.60*** | 0.24 |
| Random effects | ||||||||||||
| Time variance | −1.81*** | 0.03 | −2.96*** | 0.44 | −3.03*** | 0.5 | −3.06*** | 0.53 | −3.08*** | 0.55 | −3.05*** | 0.52 |
| Constant variance | 0.43*** | 0.02 | 0.21*** | 0.03 | 0.22*** | 0.03 | 0.21*** | 0.03 | 0.21*** | 0.03 | 0.22*** | 0.03 |
| Residual variance | 0.02* | 0.01 | 0.29*** | 0.02 | 0.28*** | 0.02 | 0.28*** | 0.02 | 0.28*** | 0.02 | 0.28*** | 0.02 |
Note. SE = standard error. Models adjust for gender, foreign-born status, marital status, education, poverty status, employment, and indicator for missing depressive symptoms data.
reference = 51–64 years old.
p < .05
p < .01
p < .001.
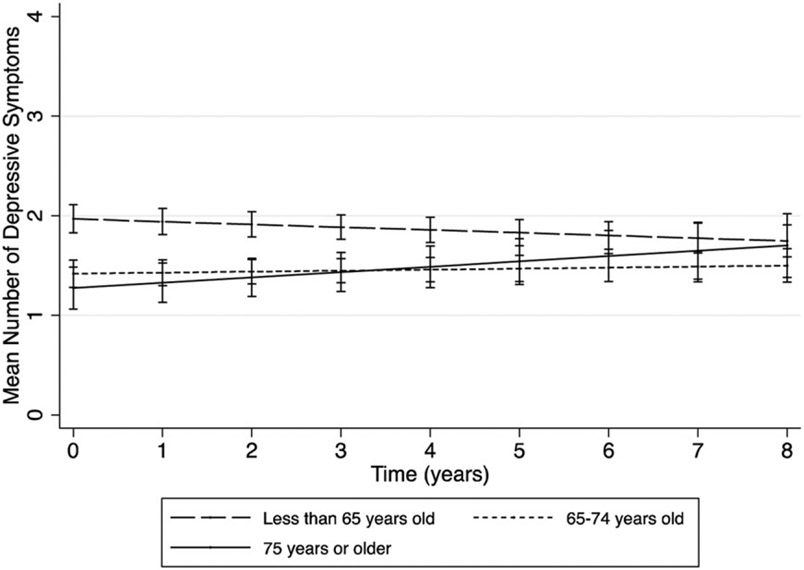
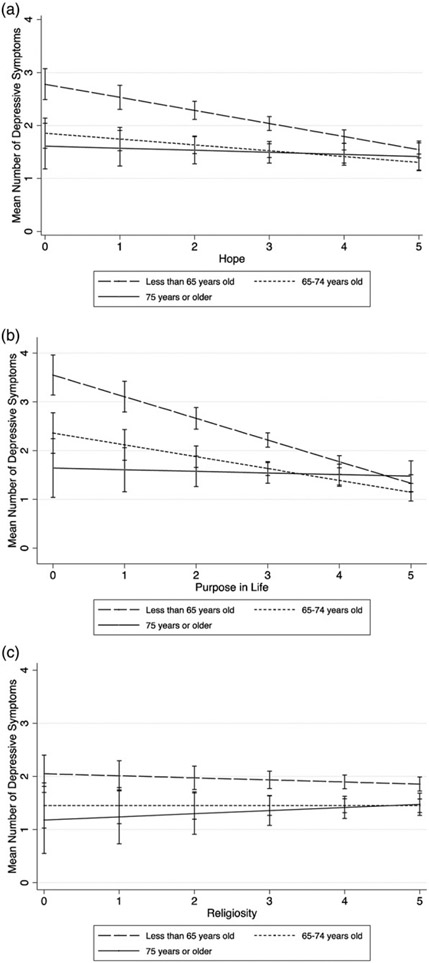
In Models 3–6 of Table 3, we test whether age influences change in depressive symptoms and the effects of each psychosocial resource on depressive symptoms. Model 3 shows that change in depressive symptoms differed significantly by age (age 65–74 b = 0.04, p < .05; age 75+ b = 0.08, p < .001) such that symptoms decreased among Black adults aged 51–64, did not change among the 65–74 age group, and increased for the oldest age group, 75+ (Figure 1). Age differences also existed in the effects of hope (Table 3, Model 4: age 65–74 b = 0.14, p < .01; age 75+ b = 0.21, p < .01) and purpose in life (Table 3, Model 5: age 65–74 b = 0.20, p < .01; age 75+ b = 0.40, p < .001) on levels of depressive symptoms. Figure 2, Panel A depicts the interaction between age and hope and shows that, compared to the two oldest age groups, Black adults ages 51–64 start off with a higher number of depressive symptoms but experience steeper declines in symptomology as feelings of hope increases. It also shows that hope is not associated with depressive symptoms among those aged 75+. A similar pattern of associations exists for purpose in life (Figure 2, Panel B), specifically, steeper declines in depressive symptoms with increasing sense of purpose among the 51–64 age group and no association among the 75+ group. Religiosity, on the other hand, is unrelated to depressive symptoms regardless of age (Figure 2, Panel C).
Figure 1.
Depressive Symptom Trajectories by Age: Health and Retirement Study, 2006–2016 (n = 1906).
Figure 2.
Interaction Between Age and Psychosocial Resources: Health and Retirement Study, 2006–2016 (n = 1906).
Health Factors Account for Change in Depressive Symptoms Among Oldest-Old
Because age differences exist in change in depressive symptoms and in the effects of each psychosocial resource on depressive symptoms, we estimated age-stratified models to better understand the factors—specifically health related factors—that explain these findings. Table 4 presents six models in total for change in depressive symptoms; two nested models are estimated for each age group. The first model controls for the psychosocial resources and covariates, the second adds indicators for ADL limitations and chronic disease burden. For Blacks ages 51–64, depressive symptoms decreased over time (Model 1a: b = −0.03, p < .05) net of demographic and socioeconomic factors and psychosocial resources. Accounting for the health factors resulted in a more negative slope for the time coefficient (Model 1b: b = −0.06, p < .001). Among those ages 65–74, depressive symptoms did not change over time even after accounting for health factors (Model 2a: b = 0.01, p = .215; Model 2b: b = −0.01, p = .237). Lastly, among Blacks age 75+, depressive symptoms increased over time (Model 3a: b = 0.05, p < .05) but that increase was fully accounted for by the health factors (Model 3b: b = 0.02, p = .489). Consistent with the conditional models presented in Table 3, hope and purpose in life were inversely related to depressive symptoms among Blacks ages 51–64 (Model 1b: hope b = −0.20, p < .001; purpose b = −0.34, p < .001) and ages 65–74 (Model 2b: hope b = −0.11, p < .01; purpose b = −0.23, p < .001), although the effect sizes were slightly reduced after accounting for the health factors. For the oldest age group, none of the psychosocial resources were associated with depressive symptoms in Model 3a, but the effects of hope became significant after accounting for the health factors (Model 3b: b = −0.12, p < .05).
Table 4.
Age-Stratified Linear Mixed Models for the Effects of Psychosocial Resources and Health Factors on Depressive Symptoms: Health and Retirement Study, 2006–2016 (n= 1906).
| 51–64 Years Old (n = 773) |
65–74 Years Old (n = 747) |
75+ Years Old (n = 386) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1a |
Model 1b |
Model 2a |
Model 2b |
Model 3a |
Model 3b |
|||||||
| Fixed Effects | b | SE | b | SE | b | SE | b | SE | b | SE | b | SE |
| Time | −0.03* | 0.01 | −0.06*** | 0.01 | 0.01 | 0.01 | −0.01 | 0.01 | 0.05* | 0.02 | 0.02 | 0.02 |
| Hope | −0.22*** | 0.04 | −0.20*** | 0.04 | −0.12** | 0.04 | −0.11** | 0.04 | −0.08 | 0.06 | −0.12* | 0.06 |
| Purpose in life | −0.42*** | 0.06 | −0.34*** | 0.06 | −0.25*** | 0.05 | −0.23*** | 0.05 | −0.09 | 0.09 | 0.02 | 0.08 |
| Religiosity | −0.02 | 0.04 | −0.02 | 0.04 | 0.00 | 0.04 | 0.00 | 0.04 | 0.01 | 0.07 | 0.00 | 0.06 |
| ADL limitations | 0.38*** | 0.05 | 0.24*** | 0.04 | 0.45*** | 0.05 | ||||||
| Chronic disease burden | 0.25*** | 0.04 | 0.23*** | 0.04 | 0.20*** | 0.06 | ||||||
| Constant | 4.17*** | 0.31 | 3.35*** | 0.31 | 2.49*** | 0.34 | 1.99*** | 0.34 | 2.69*** | 0.67 | 1.88** | 0.64 |
| Random effects | ||||||||||||
| Time variance | −12.55*** | 0.81 | −23.75*** | 0.82 | −2.59*** | 0.31 | −2.79*** | 0.43 | −10.00*** | 1.68 | −3.91 | 8.11 |
| Constant variance | 0.22*** | 0.05 | 0.09 | 0.05 | 0.22*** | 0.04 | 0.12* | 0.05 | 0.06 | 0.10 | −0.03 | 0.11 |
| Residual variance | 0.33*** | 0.02 | 0.32*** | 0.02 | 0.19*** | 0.03 | 0.21*** | 0.03 | 0.35*** | 0.05 | 0.28*** | 0.05 |
Note. SE = standard error. Models adjust for gender, foreign-born status, marital status, education, poverty status, employment, and indicator for missing depressive symptoms data
p < .05
p < 01
p < .001.
Discussion
The objectives of this study were three-fold: (1) to examine change in depressive symptoms among middle-aged and older Blacks; (2) to test the association between internal psychosocial resources and change in depressive symptoms in this population, and (3) to determine whether age differences exist in how depressive symptoms change over time and in the effect of psychosocial resources on symptomology. Overall, our findings support our hypotheses and highlight important age-based heterogeneity in the ways in which psychosocial resources influence depressive symptoms.
Similar to previous studies among older populations (Abrams & Mehta, 2019; Liang et al., 2011) and in line with our hypothesis, the interaction between age and time revealed significant age differences in initial levels of depressive symptoms and in the relationship between age and the rate of change in symptomology. At baseline, depressive symptoms were highest among middle-aged Black adults, followed by those ages 65–74 and 75+, respectively. The direction and rate of change over time differed across the three groups such that, symptoms decreased among Black Americans in midlife, did not change among Blacks in early old age, and increased among the oldest Black adults, suggesting a U-shaped relationship. This pattern of change with age is likely due to differences in health and social and economic experiences that are characteristic of each life stage. For instance, bereavement increases with age and contributes to higher reports of depressive symptoms among older adults (Lynch & George, 2002). The loss of loved ones is often accompanied by losses in physical functioning (Schieman & Plickert, 2007), declines in cognitive functioning, and increases in chronic diseases that place older adults at greater risk for experiencing increasing or persistent depression symptoms (Xiang & Cheng, 2019). In our study, age stratified analyses showed that accounting for limitations in activities of daily living and chronic disease burden fully explained the rate of increase in symptoms among Black Americans ages 75+. Thus, the driving force behind depressive symptoms during late life for Black Americans may be the loss of health and functioning.
Health and physical functioning changes also occur during midlife, as do changes in work and family life that contribute to stress (Aldwin & Levenson, 2001; Lachman, 2004). However, middle-aged Black adults likely have more psychosocial resources to begin with than older adults because they have lived fewer years and as a result have presumably experienced fewer resource-depleting stressors. Additionally, the finality of life becomes more apparent as people age, which may limit feelings of hopefulness towards the future and a sense of purpose for the remaining years of life, particularly for older adults who are lonely or socially isolated (Aldwin & Levenson, 2001; Hajek & König, 2021; Lachman, 2004; Neville et al., 2018). The difference in resource levels across midlife, early old age, and old age is evident in our study findings for hope and purpose in life, but not for religiosity. At baseline, middle-aged Black Americans had the highest levels of hope and purpose while the oldest-old Black Americans had the lowest. Both resources were associated with fewer depressive symptoms on average and compared to those in early and late old age, protected against depressive symptoms among middle-aged Black Americans more strongly.
Multiple pathways potentially explain the relationship between psychosocial resources and mental health outcomes, including their influence on different coping responses (Aspinwall & Taylor, 1997), the cognitive appraisal process (Taylor et al., 2008), health behaviors (Thomas et al., 2020), and neural activity (Taylor & Broffman, 2011), all of which impact mental health. The differential effects by age of hope and purpose in life on depressive symptoms are less understood. On the one hand, age differences in these associations may reflect a selection effect. Specifically, the presence of the hope-depressive symptoms relationship among the youngest age group and the lack of an association among the oldest age group may be due to higher depression-related mortality at older ages. On the other hand, age differences in the effects of these resources may be related to the composition of each age group. Although the proportion female was similar across each age group, the oldest age group was less likely to include foreign-born Blacks compared to the younger age groups. Foreign-born Blacks, such as Caribbean Blacks and Africans, grew up in different social environments and presumably had qualitatively different lived experiences from U.S.-born Black Americans. As a result, the nature, distribution, and mental health effects of psychosocial resources and social stressors within each group likely differ. Therefore, examining the intersection of age and Black ethnicity, as well as other within-race heterogeneities, with data sets such as the National Survey of American Life would be beneficial for improving our understanding of the effects of psychosocial resources on depressive symptoms in the broader Black community.
Another explanation for age differences in the effects of psychosocial resources on depressive symptoms pertains to the different political and social environments in which each age group grew up. Middle-aged Blacks—who, in our sample, were born between 1941 and 1955 and for the youngest in this group reached their mid-20s by the late 1970s—may benefit more from hopefulness and a higher sense of purpose in life. This cohort grew up and came of age during a time when changes in the sociopolitical landscape encouraged a more hopeful orientation. Their prime years of adult development (i.e., ages 18–25) occurred shortly after the passing of the Civil Rights Acts of 1964 and 1968 when the socioeconomic status of Black people and the sociopolitical climate regarding race in the U.S. were improving, albeit rather slowly. Although Black Americans belonging to this age cohort spent the early portion of their lives during the period of Jim Crow laws and the Korean and Vietnam wars, they did not experience two world wars and the Great Depression as did persons born before 1941. Respondents who comprised the middle-aged cohort did, however, experience a number of social, political, and economic improvements that may have contributed to the development of a more robust sense of hope and purpose such that “false hopes” for change became real hopes that more effectively protect their mental health.
In contrast to our findings for hope and purpose in life, subjective religiosity was unrelated to depressive symptoms for all age groups. This was an unexpected finding given the statistically significant bivariate correlation we observed between the two factors and prior research demonstrating an inverse relationship between subjective religiosity and mental health more broadly (Nguyen, 2020). However, some studies have also failed to find an association between religiosity and major depressive disorder (Hudson et al., 2015) and depressive symptoms (Davenport & McClintock, 2021; Taylor et al., 2012). A possible reason for our null findings is that other aspects of religion among Black Americans (i.e., religious coping, religious social support, service attendance) may be more salient for mitigating depressive symptoms. In fact, studies that examine the effect of subjective religiosity in tandem with that of service attendance find that subjective religiosity is not a significant predictor of mental health in the presence of service attendance (Chatters et al., 2008b; Taylor et al., 2012). These studies suggest that service attendance is a stronger determinant of mental health than subjective religiosity. Moreover, church-based social support, which is positively correlated with service attendance, may also be more protective against poor mental health than subjective beliefs and attitudes about God (Chatters et al., 2015).
Strengths and Limitations
There are strengths and limitations to our study. Notably, this is one of the first population-based studies to examine the effects of hope and purpose in life on the mental health of middle-aged and older Black adults. An extensive body of research has assessed the relationship between religiosity and mental health in this population. Thus, investigating the protective effects of hope and purpose in life is novel and provides a steppingstone towards a more comprehensive understanding of the factors that contribute to the resilience of Black Americans. Additionally, our study was a longitudinal analysis, which allowed us to examine the effects of these resources on both levels of and change in depressive symptoms over time. That said, the psychosocial resources and depressive symptoms were measured concurrently, which does not allow us to clearly disentangle the temporal ordering of this relationship. Moreover, the CES-D includes an item that asks about feelings of hopelessness, which might inflate or explain the significant relationship between hope and depressive symptoms we found in our study. That said, the bivariate correlation between these two measures in our sample is relatively low (ranges from −0.22 to −0.30 across the three waves of data collection) and seminal research on hopelessness (the opposite of hope) has shown that it is conceptually and empirically distinct from depressive symptoms (Abramson et al., 1989; Minkoff et al., 1973) and has independent effects on health (Greene, 1989). Lastly, our analysis is based on self-reported data which is subject to recall and social desirability biases. Future research should build upon the stated strengths and address these limitations.
Implications and Conclusion
Our study demonstrated that, among middle-aged and older Black adults, trajectories of depressive symptoms and the effects of psychosocial resources are influenced by age. These findings have important clinical, public health, and research implications. First, awareness of how depressive symptoms change over time among Black Americans of different ages may be beneficial for risk assessment and symptom management. Additionally, to the extent that hope and purpose in life are modifiable resources (Hernandez & Overholser, 2021; Irving et al., 2017), they can be leveraged for prevention efforts aimed at mitigating depressive symptoms and its consequences. For instance, research has shown that counseling-based interventions designed to improve feelings of hope are successful at improving psychological health (Howell et al., 2015). Similarly, volunteering has been shown to be associated with positive psychological outcomes among older adults through its effects on purpose in life (Greenfield & Marks, 2004). Thus, our study has identified novel targets for public health intervention for middle-aged and older Blacks adults at risk for experiencing symptoms of depression. Lastly, our study highlights the diversity inherent in the Black community with regard to age and among Black adults in the second half of life. Continued examination of within-group heterogeneity by age and other sociodemographic characteristics is needed to more fully understand the lived experiences of Black people in older adulthood.
Supplementary Material
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The preparation of this article was supported by a grant from the National Institute on Aging to UAM (1R21AG065654-01A1) and by the National Heart, Lung, and Blood Institute to AWN (5R25HL105444-11).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- Abrams LR, Clarke PJ, & Mehta NK (2021). Unmet expectations about work at age 62 and depressive symptoms. The Journals of Gerontology: Series B. Advance online publication. 10.1093/geronb/gbab113 [DOI] [PubMed] [Google Scholar]
- Abrams LR, & Mehta NK (2019). Changes in depressive symptoms over age among older Americans: Differences by gender, race/ethnicity, education, and birth cohort. SSM-population Health, 7(April), 100399. 10.1016/j.ssmph.2019.100399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abramson LY, Metalsky GI, & Alloy LB (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96(2), 358–372. 10.1037/0033-295x.96.2.358 [DOI] [Google Scholar]
- Adams VH III, & Jackson JS (2000). The contribution of hope to the quality of life among aging African Americans: 1980–1992. The International Journal of Aging and Human Development, 50(4), 279–295. 10.2190/AWB4-7CLU-A2EP-BQLF [DOI] [PubMed] [Google Scholar]
- Alarcon GM, Bowling NA, & Khazon S (2013). Great expectations: A meta-analytic examination of optimism and hope. Personality and Individual Differences, 54(7), 821–827. 10.1016/j.paid.2012.12.004 [DOI] [Google Scholar]
- Aldwin CM, & Levenson MR (2001). Stress, coping, and health at mid-life (pp. 188–214). The Handbook of Midlife Development [Google Scholar]
- Arnau RC, Rosen DH, Finch JF, Rhudy JL, & Fortunato VJ (2007). Longitudinal effects of hope on depression and anxiety: A latent variable analysis. Journal of Personality, 75(1), 43–64. 10.1111/j.1467-6494.2006.00432.x [DOI] [PubMed] [Google Scholar]
- Aspinwall LG, & Taylor SE (1997). A stitch in time: self-regulation and proactive coping. Psychological Bulletin, 121(3), 417–436. 10.1037/0033-2909.121.3.417 [DOI] [PubMed] [Google Scholar]
- Assari S, Cobb S, Saqib M, & Bazargan M (2020). Economic strain deteriorates while education fails to protect black older adults against depressive symptoms, pain, self-rated health, chronic disease, and sick days. Journal of Mental Health & Clinical Psychology, 4(2), 49–62. 10.29245/2578-2959/2020/2.1203 [DOI] [PubMed] [Google Scholar]
- Assari S, & Lankarani MM (2016). Depressive symptoms are associated with more hopelessness among white than black older adults. Frontiers in Public Health, 4(10), 82. 10.3389/fpubh.2016.00082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S, Moazen-Zadeh E, Lankarani MM, & Micol-Foster V (2016). Race, depressive symptoms, and all-cause mortality in the United States. Frontiers in Public Health, 4(1), 40. 10.3389/fpubh.2016.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett MD (2014). Future orientation and health among older adults: The importance of hope. Educational Gerontology, 40(10), 745–755. 10.1080/03601277.2014.898496 [DOI] [Google Scholar]
- Beck AT, Weissman A, Lester D, & Trexler L (1974). The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology, 42(6), 861–865. 10.1037/h0037562 [DOI] [PubMed] [Google Scholar]
- Billington E, Simpson J, Unwin J, Bray D, & Giles D (2008). Does hope predict adjustment to end stage renal failure and consequent dialysis? British Journal of Health Psychology, 13(Pt 4), 683–699. 10.1348/135910707X248959 [DOI] [PubMed] [Google Scholar]
- Boyle PA, Barnes LL, Buchman AS, & Bennett DA (2009). Purpose in life is associated with mortality among community-dwelling older persons. Psychosomatic Medicine, 71(5), 574–579. 10.1097/PSY.0b013e3181a5a7c0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LL, Mitchell UA, & Ailshire JA (2020). Disentangling the stress process: Race/ethnic differences in the exposure and appraisal of chronic stressors among older adults. The Journals of Gerontology: Series B, 75(3), 650–660. 10.1093/geronb/gby072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant FB, & Cvengros JA (2004). Distinguishing hope and optimism: Two sides of a coin, or two separate coins? Journal of Social and Clinical Psychology, 23(2), 273–302. 10.1521/jscp.23.2.273.31018 [DOI] [Google Scholar]
- Byers AL, Yaffe K, Covinsky KE, Friedman MB, & Bruce ML (2010). High occurrence of mood and anxiety disorders among older adults: The national comorbidity survey replication. Archives of General Psychiatry, 67(5), 489–496. 10.1001/archgenpsychiatry.2010.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatters LM (2000). Religion and health: Public health research and practice. Annual Review of Public Health, 21(1), 335–367. 10.1146/annurev.publhealth.21.1.335 [DOI] [PubMed] [Google Scholar]
- Chatters LM, Bullard KM, Taylor RJ, Woodward AT, Neighbors HW, & Jackson JS (2008a). Religious participation and DSM-IV disorders among older African Americans: Findings from the national survey of American life. The American Journal of Geriatric Psychiatry, 16(12), 957–965. 10.1097/JGP.0b013e3181898081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatters LM, Taylor RJ, Bullard KM, & Jackson JS (2008b). Spirituality and subjective religiosity among African Americans, Caribbean Blacks, and Non Hispanic Whites. Journal for the Scientific Study of Religion, 47(4), 725–737. 10.1111/j.1468-5906.2008.00437.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatters LM, Taylor RJ, & Lincoln KD (1999). African American religious participation: A multi-sample comparison. Journal for the Scientific Study of Religion, 38(1), 132–145. [Google Scholar]
- Chatters LM, Taylor RJ, Woodward AT, & Nicklett EJ (2015). Social support from church and family members and depressive symptoms among older African Americans. The American Journal of Geriatric Psychiatry, 23(6), 559–567. 10.1016/j.jagp.2014.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciarrocchi JW, Dy-Liacco GS, & Deneke E (2008). Gods or rituals? Relational faith, spiritual discontent, and religious practices as predictors of hope and optimism. The Journal of Positive Psychology, 3(2), 120–136. 10.1080/17439760701760666 [DOI] [Google Scholar]
- Ciarrochi J, Parker P, Kashdan TB, Heaven PCL, & Barkus E (2015). Hope and emotional well-being: A six-year study to distinguish antecedents, correlates, and consequences. The Journal of Positive Psychology, 10(6), 520–532. 10.1080/17439760.2015.1015154 [DOI] [Google Scholar]
- Cole MG, & Dendukuri N (2003). Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. American Journal of Psychiatry, 160(6), 1147–1156. 10.1176/appi.ajp.160.6.1147 [DOI] [PubMed] [Google Scholar]
- Cone JH (2010). A Black theology of liberation. Orbis Books. [Google Scholar]
- Cotton Bronk K, Hill PL, Lapsley DK, Talib TL, & Finch H (2009). Purpose, hope, and life satisfaction in three age groups. The Journal of Positive Psychology, 4(6), 500–510. 10.1080/17439760903271439 [DOI] [Google Scholar]
- Crego A, Yela JR, Gómez-Martínez MÁ, & Karim AA (2019). The contribution of meaningfulness and mindfulness to psychological well-being and mental health: A structural equation model. Journal of Happiness Studies, 21(8), 2827–2850. 10.1007/s10902-019-00201-y [DOI] [Google Scholar]
- Crego A, Yela JR, Gómez-Martínez MÁ, Riesco-Matías P, & Petisco-Rodríguez C (2021). Relationships between mindfulness, purpose in life, happiness, anxiety, and depression: Testing a mediation model in a sample of women. International Journal of Environmental Research and Public Health, 18(3), 925. 10.3390/ijerph18030925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damon W, Menon J, & Cotton Bronk K (2003). The development of purpose during adolescence. Applied Developmental Science, 7(3), 119–128. 10.1207/s1532480xads0703_2 [DOI] [Google Scholar]
- Davenport AD, & McClintock HF (2021). Let go and let god: A study of religiosity and depressive symptoms in the Black church. Community Mental Health Journal, 57(7), 1340–1347. 10.1007/s10597-020-00757-7 [DOI] [PubMed] [Google Scholar]
- Davidson CL, Wingate LR, Slish ML, & Rasmussen KA (2010). The great Black hope: Hope and its relation to suicide risk among African Americans. Suicide & Life-Threatening Behavior, 40(2), 170–180. 10.1521/suli.2010.40.2.170 [DOI] [PubMed] [Google Scholar]
- Ellison CG, & Levin JS (1998). The religion-health connection: Evidence, theory, and future directions. Health Education & Behavior, 25(6), 700–720. 10.1177/109019819802500603 [DOI] [PubMed] [Google Scholar]
- Everson SA, Goldberg DE, Kaplan GA, Cohen RD, Pukkala E, Tuomilehto J, & Salonen JT (1996). Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosomatic Medicine, 58(2), 113–121. 10.1097/00006842-199603000-00003 [DOI] [PubMed] [Google Scholar]
- Frazier C, Mintz LB, & Mobley M (2005). A multidimensional look at religious involvement and psychological well-being among urban elderly African Americans. Journal of Counseling Psychology, 52(4), 583–590. 10.1037/0022-0167.52.4.583 [DOI] [Google Scholar]
- Frazier EF, & Lincoln CE (1974). The Negro church in America. Schocken Books. [Google Scholar]
- Galek K, Flannelly KJ, Ellison CG, Silton NR, & Jankowski KRB (2015). Religion, meaning and purpose, and mental health. Psychology of Religion and Spirituality, 7(1), 1–12. 10.1037/a0037887 [DOI] [Google Scholar]
- Greene SM (1989). The relationship between depression and hopelessness: Implications for current theories of depression. The British Journal of Psychiatry, 154(5), 650–659. 10.1192/bjp.154.5.650 [DOI] [PubMed] [Google Scholar]
- Greenfield EA, & Marks NF (2004). Formal volunteering as a protective factor for older adults’ psychological well-being. The Journals of Gerontology.Series B, Psychological Sciences and Social Sciences, 59(5), S258–S264. 10.1093/geronb/59.5.S258 [DOI] [PubMed] [Google Scholar]
- Hajek A, & König H (2021). Do loneliness and perceived social isolation reduce expected longevity and increase the frequency of dealing with death and dying? Longitudinal findings based on a nationally representative sample. Journal of the American Medical Directors Association, 22(8), 1720–1725. 10.1016/j.jamda.2021.04.004 [DOI] [PubMed] [Google Scholar]
- Hedeker D, & Gibbons RD (1997). Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods, 2(1), 64–78. 10.1037/1082-989x.2.1.64. [DOI] [Google Scholar]
- Heisel MJ, & Flett GL (2016). Does recognition of meaning in life confer resiliency to suicide ideation among community-residing older adults? A longitudinal investigation. The American Journal of Geriatric Psychiatry, 24(6), 455–466. 10.1016/j.jagp.2015.08.007 [DOI] [PubMed] [Google Scholar]
- Hernandez SC, & Overholser JC (2021). A systematic review of interventions for hope/hopelessness in older adults. Clinical Gerontologist, 44(2), 97–111. 10.1080/07317115.2019.1711281 [DOI] [PubMed] [Google Scholar]
- Hirsch JK, & Sirois FM (2016). Hope and fatigue in chronic illness: The role of perceived stress. Journal of Health Psychology, 21(4), 451–456. 10.1177/1359105314527142 [DOI] [PubMed] [Google Scholar]
- Howell AJ, Jacobson RM, & Larsen DJ (2015). Enhanced psychological health among chronic pain clients engaged in hope-focused group counseling. The Counseling Psychologist, 43(4), 586–613. 10.1177/0011000014551421 [DOI] [Google Scholar]
- Hudson DL, Purnell JQ, Duncan AE, & Baker E (2015). Subjective religiosity, church attendance, and depression in the national survey of American life. Journal of Religion and Health, 54(2), 584–597. 10.1007/s10943-014-9850-2 [DOI] [PubMed] [Google Scholar]
- Ingersoll-Dayton B, Krause N, & Morgan D (2002). Religious trajectories and transitions over the life course. The International Journal of Aging and Human Development, 55(1), 51–70. 10.2190/297Q-MRMV-27TE-VLFK [DOI] [PubMed] [Google Scholar]
- Irving J, Davis S, & Collier A (2017). Aging with purpose: Systematic search and review of literature pertaining to older adults and purpose. International Journal of Aging & Human Development, 85(4), 403–437. 10.1177/0091415017702908 [DOI] [PubMed] [Google Scholar]
- Jang SJ, & Johnson BR (2004). Explaining religious effects on distress among African Americans. Journal for the Scientific Study of Religion, 43(2), 239–260. 10.1111/j.1468-5906.2004.00230.x [DOI] [Google Scholar]
- Karim J, Weisz R, Bibi Z, & ur Rehman S (2015). Validation of the eight-item center for epidemiologic studies depression scale (CES-D) among older adults. Current Psychology, 34(4), 681–692. 10.1007/s12144-014-9281-y [DOI] [Google Scholar]
- Kessler RC, Foster C, Webster PS, & House JS (1992). The relationship between age and depressive symptoms in two national surveys. Psychology and Aging, 7(1), 119–126. 10.1037//0882-7974.7.1.119 [DOI] [PubMed] [Google Scholar]
- Kim ES, Hershner SD, & Strecher VJ (2015). Purpose in life and incidence of sleep disturbances. Journal of Behavioral Medicine, 38(3), 590–597. 10.1007/s10865-015-9635-4 [DOI] [PubMed] [Google Scholar]
- Kim ES, Kawachi I, Chen Y, & Kubzansky LD (2017). Association between purpose in life and objective measures of physical function in older adults. JAMA Psychiatry, 74(10), 1039–1045. 10.1001/jamapsychiatry.2017.2145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Sun JK, Park N, Kubzansky LD, & Peterson C (2013a). Purpose in life and reduced risk of myocardial infarction among older U.S. adults with coronary heart disease: A two-year follow-up. Journal of Behavioral Medicine, 36(2), 124–133. 10.1007/s10865-012-9406-4 [DOI] [PubMed] [Google Scholar]
- Kim ES, Sun JK, Park N, & Peterson C (2013b). Purpose in life and reduced incidence of stroke in older adults: ‘The health and retirement study’. Journal of Psychosomatic Research, 74(5), 427–432. 10.1016/j.jpsychores.2013.01.013 [DOI] [PubMed] [Google Scholar]
- Kim G, Shin SH, Scicolone MA, & Parmelee P (2019). Purpose in life protects against cognitive decline among older adults. The American Journal of Geriatric Psychiatry, 27(6), 593–601. 10.1016/j.jagp.2019.01.010 [DOI] [PubMed] [Google Scholar]
- Koenig H, King D, & Carson VB (2012). Handbook of religion and health (2nd ed.). Oxford University Press. [Google Scholar]
- Krause N (2003). Religious meaning and subjective well-being in late life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58(3), S160–S170. 10.1093/geronb/58.3.S160 [DOI] [PubMed] [Google Scholar]
- Lachman ME (2004). Development in midlife. Annual Review of Psychology, 55(1), 305–331. 10.1146/annurev.psych.55.090902.141521. [DOI] [PubMed] [Google Scholar]
- Levin J, & Chatters LM (2008). Religion, aging, and health: Historical perspectives, current trends, and future directions: Public health. Journal of Religion, Spirituality & Aging, 20(1–2), 153–172. 10.1080/15528030801922103 [DOI] [Google Scholar]
- Levin JS, & Taylor RJ (1998). Panel analyses of religious involvement and well-being in African Americans: Contemporaneous vs. longitudinal effects. Journal for the Scientific Study of Religion, 37(4), 695–709. 10.2307/1388151 [DOI] [Google Scholar]
- Levin JS, Taylor RJ, & Chatters LM (1995). A multidimensional measure of religious involvement for African Americans. The Sociological Quarterly, 36(1), 157–173. 10.1111/j.1533-8525.1995.tb02325.x [DOI] [Google Scholar]
- Liang J, Xu X, Quiñones AR, Bennett JM, & Ye W (2011). Multiple trajectories of depressive symptoms in middle and late life: Racial/ethnic variations. Psychology and Aging, 26(4), 761–777. 10.1037/a0023945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln CE, & Mamiya LH (1990). The Black church in the African American experience. Duke University Press. [Google Scholar]
- Liwo ANN, Howard VJ, Zhu S, Martin MY, Safford MM, Richman JS, Cummings DM, & Carson AP (2020). Elevated depressive symptoms and risk of all-cause and cardiovascular mortality among adults with and without diabetes: The REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Journal of Diabetes and Its Complications, 34(10), 107672. 10.1016/j.jdiacomp.2020.107672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long KNG, Kim ES, Chen Y, Wilson MF, Worthington EL Jr, & VanderWeele TJ (2020). The role of hope in subsequent health and well-being for older adults: An outcome-wide longitudinal approach. Global Epidemiology, 2(November), 100018. 10.1016/j.gloepi.2020.100018 [DOI] [Google Scholar]
- Lynch SM, & George LK (2002). Interlocking trajectories of loss-related events and depressive symptoms among elders. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 57(2), S117–S125. 10.1093/geronb/57.2.s117 [DOI] [PubMed] [Google Scholar]
- Madan S, & Pakenham KI (2014). The stress-buffering effects of hope on adjustment to multiple sclerosis. International Journal of Behavioral Medicine, 21(6), 877–890. 10.1007/s12529-013-9384-0 [DOI] [PubMed] [Google Scholar]
- Mezuk B, Edwards L, Lohman M, Choi M, & Lapane K (2012). Depression and frailty in later life: a synthetic review. International Journal of Geriatric Psychiatry, 27(9), 879–892. 10.1002/gps.2807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkoff K, Bergman E, Beck AT, & Beck R (1973). Hopelessness, depression, and attempted suicide. American Journal of Psychiatry, 130(4), 455–459. 10.1176/ajp.130.4.455 [DOI] [PubMed] [Google Scholar]
- Mirowsky J, & Ross CE (1992). Age and depression. Journal of Health and Social Behavior, 33(3), 187–205. 10.2307/2137349 [DOI] [PubMed] [Google Scholar]
- Mitchell UA, Dellor ED, Sharif MZ, Brown LL, Torres JM, & Nguyen AW (2020). When is hope enough? hopefulness, discrimination and racial/ethnic disparities in allostatic load. Behavioral Medicine, 46(3–4), 189–201. 10.1080/08964289.2020.1729086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moazen-Zadeh E, & Assari S (2016). Depressive symptoms predict major depressive disorder after 15 years among whites but not blacks. Frontiers in Public Health, 4(2), 13. 10.3389/fpubh.2016.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagnier D, Dartigues J, Rouillon F, Pérès K, Falissard B, & Onen F (2014). Ageing and trajectories of depressive symptoms in community dwelling men and women. International Journal of Geriatric Psychiatry, 29(7), 720–729. 10.1002/gps.4054 [DOI] [PubMed] [Google Scholar]
- Mouzon DM (2017). Religious involvement and the black–white paradox in mental health. Springer Science and Business Media LLC. 10.1007/s12552-017-9198-9. [DOI] [Google Scholar]
- Nadimpalli SB, James BD, Yu L, Cothran F, & Barnes LL (2015). The association between discrimination and depressive symptoms among older African Americans: The role of psychological and social factors. Experimental Aging Research, 41(1), 1–24. 10.1080/0361073X.2015.978201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neville S, Adams J, Montayre J, Larmer P, Garrett N, Stephens C, & Alpass F (2018). Loneliness in men 60 years and over: The association with purpose in life. American Journal of Men’s Health, 12(4), 730–739. 10.1177/1557988318758807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen AW (2020). Religion and mental health in racial and ethnic minority populations: A review of the literature. Innovation in Aging, 4(5), igaa035. 10.1093/geroni/igaa035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen AW, Taylor RJ, Chatters LM, & Hope MO (2019). Church support networks of African Americans: The impact of gender and religious involvement. Journal of Community Psychology, 47(5), 1043–1063. 10.1002/jcop.22171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pargament KI (1997). The psychology of religion and coping: Theory, research, practice. Guilford press. [Google Scholar]
- Pargament KI, & Raiya HA (2007). A decade of research on the psychology of religion and coping: Things we assumed and lessons we learned. Psyke & Logos, 28(2), 742–766 [Google Scholar]
- Park CL, Knott CL, Williams RM, Clark EM, Williams BR, & Schulz E (2020). Meaning in life predicts decreased depressive symptoms and increased positive affect over time but does not buffer stress effects in a national sample of African-Americans. Journal of Happiness Studies, 21(8), 3037–3049. 10.1007/s10902-019-00212-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center (2015). America’s changing religious landscape. https://www.pewforum.org/2015/05/12/americas-changing-religious-landscape/
- Pickett YR, Bazelais KN, & Bruce ML (2013). Late life depression in older African Americans: A comprehensive review of epidemiological and clinical data. International Journal of Geriatric Psychiatry, 28(9), 903–913. 10.1002/gps.3908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M (2002). Creating and maintaining purpose in life in old age: A meta-analysis. Ageing International, 27(2), 90–114. 10.1007/s12126-002-1004-2 [DOI] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Ryff CD (1989). Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology, 57(6), 1069–1081. 10.1037/0022-3514.57.6.1069 [DOI] [Google Scholar]
- Ryff CD, & Singer BH (2008). Know thyself and become what you are: A eudaimonic approach to psychological well-being. Journal of Happiness Studies, 9(1), 13–39. 10.1007/s10902-006-9019-0 [DOI] [Google Scholar]
- Schieman S, & Plickert G (2007). Functional limitations and changes in levels of depression among older adults: A multiple-hierarchy stratification perspective. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62(1), S36–S42. 10.1093/geronb/62.1.s36 [DOI] [PubMed] [Google Scholar]
- Shiba K, Kubzansky LD, Williams DR, VanderWeele TJ, & Kim ES (2021). Associations between purpose in life and mortality by SES. American Journal of Preventive Medicine, 61(2), Article e53–e61. 10.1016/j.amepre.2021.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder CR (2002). Hope theory: Rainbows in the mind. Psychological Inquiry, 13(4), 249–275. 10.1207/s15327965pli1304_01 [DOI] [Google Scholar]
- Sonnega A, & Weir D (2014). The health and retirement study: A public data resource for research on aging. Open Health Data, 2(1), Article e7. 10.5334/ohd.am [DOI] [Google Scholar]
- Stearns M, Nadorff DK, Lantz ED, & McKay IT (2018). Religiosity and depressive symptoms in older adults compared to younger adults: Moderation by age. Journal of Affective Disorders, 238, 522–525. 10.1016/j.jad.2018.05.076 [DOI] [PubMed] [Google Scholar]
- Stoyles G, Chadwick A, & Caputi P (2015). Purpose in life and well-being: The relationship between purpose in life, hope, coping, and inward sensitivity among first-year university students. Journal of Spirituality in Mental Health, 17(2), 119–134. 10.1080/19349637.2015.985558 [DOI] [Google Scholar]
- Sutin AR, Terracciano A, Milaneschi Y, An Y, Ferrucci L, & Zonderman AB (2013). The trajectory of depressive symptoms across the adult life span. JAMA Psychiatry, 70(8), 803–811. 10.1001/jamapsychiatry.2013.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor HO, & Nguyen AW (2020). Depressive symptoms and loneliness among Black and White older adults: The moderating effects of race. Innovation in Aging, 4(5), igaa048. 10.1093/geroni/igaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, & Abelson JM (2012). Religious involvement and DSM IV 12 month and lifetime major depressive disorder among African Americans. The Journal of Nervous and Mental Disease, 200(10), 856–862. 10.1097/NMD.0b013e31826b6d65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, & Brown RK (2014). African American religious participation. Review of Religious Research, 56(4), 513–538. 10.1007/s13644-013-0144-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, & Joe S (2011). Religious involvement and suicidal behavior among African Americans and Black Caribbeans. The Journal of Nervous and Mental Disease, 199(7), 478–486. 10.1097/NMD.0b013e31822142c7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, & Levin J (2003). Religion in the lives of African Americans: Social, psychological, and health perspectives. Sage Publications. [Google Scholar]
- Taylor RJ, Mattis J, & Chatters LM (1999). Subjective religiosity among African Americans: A synthesis of findings from five national samples. Journal of Black Psychology, 25(4), 524–543. 10.1177/0095798499025004004 . [DOI] [Google Scholar]
- Taylor SE, & Broffman JI (2011). Psychosocial resources: Functions, origins, and links to mental and physical health. In Advances in experimental social psychology (pp. 1–57). Elsevier. 10.1016/b978-0-12-385522-0.00001-9 [DOI] [Google Scholar]
- Taylor SE, Burklund LJ, Eisenberger NI, Lehman BJ, Hilmert CJ, & Lieberman MD (2008). Neural bases of moderation of cortisol stress responses by psychosocial resources. Journal of Personality and Social Psychology, 95(1), 197–211. 10.1037/0022-3514.95.1.197 [DOI] [PubMed] [Google Scholar]
- Thomas K, Nilsson E, Festin K, Henriksson P, Lowén M, Löf M, & Kristenson M (2020). Associations of psychosocial factors with multiple health behaviors: A population-based study of middle-aged men and women. International Journal of Environmental Research and Public Health, 17(4), 1239. 10.3390/ijerph17041239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner AD, Capuano AW, Wilson RS, & Barnes LL (2015). Depressive symptoms and cognitive decline in older african americans: Two scales and their factors. The American Journal of Geriatric Psychiatry, 23(6), 568–578. 10.1016/j.jagp.2014.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Williams-Morris R (2000). Racism and mental health: The African American experience. Ethnicity & Health, 5(3–4), 243–268. 10.1080/713667453 [DOI] [PubMed] [Google Scholar]
- Wu Z, Schimmele CM, & Chappell NL (2012). Aging and late-life depression. Journal of Aging and Health, 24(1), 3–28. 10.1177/0898264311422599 [DOI] [PubMed] [Google Scholar]
- Xiang X, & An R (2015). Depression and onset of cardiovascular disease in the US middle-aged and older adults. Aging & Mental Health, 19(12), 1084–1092. 10.1080/13607863.2014.1003281 [DOI] [PubMed] [Google Scholar]
- Xiang X, & Cheng J (2019). Trajectories of major depression in middle aged and older adults: A population based study. International Journal of Geriatric Psychiatry, 34(10), 1506–1514. 10.1002/gps.5161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon E, Coburn C, & Spence SA (2019). Perceived discrimination and mental health among older African Americans: The role of psychological well-being. Aging & Mental Health, 23(4), 461–469. 10.1080/13607863.2017.1423034 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.