Abstract
Background:
Castor oil is used in some countries to induce labor, but results on its effectiveness and safety is controversial. This systematic review and meta-analysis aimed to evaluate the effect of castor oil on labor induction and prevalence of vaginal delivery along with investigating its safety.
Materials and Methods:
PubMed, Scopus, Web of Science, and Google Scholar were searched systematically up to September 2020. Observational studies and Randomized Clinical Trials (RCTs), which assessed the effect of castor oil on labor induction in English and Persian languages using different combinations of the related key terms and Medical Subject Headings (MeSH) terms were collected and analyzed independently by two authors. Random effect model was used for meta-analysis. The studies were included in which the Relative Risk (RR) had been reported with 95% Confidence Intervals (CIs).
Results:
A total of 12 studies consisting 1653 pregnant women were included. The mean age of women who used castor oil was 24.72 years and in control group was 24.67 years. Results showed that labor induction was significantly higher in castor oil group than control group (RR: 3.27; 95% CI (1.96, 5.46)). Prevalence of vaginal delivery was 81% in the castor oil group and 69% in the control group.
Conclusions:
It can be concluded that use of castor oil has positive effect on labor induction and increases the prevalence of vaginal delivery. None of the studies considered in this meta-analysis reported any serious harmful effects for the use of castor oil.
Keywords: Castor, Labor, Induced, obstetric labor, oil
Introduction
Induction of Labour (IOL) is one of the main problems in maternal care and is defined as a desire to induce labor in order to end the pregnancy. It might be recommended for various reasons, mainly medical concern such as baby's health or mother's health or for social reasons.[1,2] A variety of methods are used for IOL, such as amniotomy, membrane sweep or artificial rupture of membranes and use of chemical drugs such as prostaglandins and oxytocin which could be applied either alone or in combination. However, some pregnant women prefer traditional methods such as acupuncture or medicinal herbs.[3,4] Castor oil is a natural triglyceride obtained from the seeds of Ricinus communis L. plant (Euphorbiaceae), commonly known as castor oil plant, and contains mainly ricinoleic acid (9Z,12R)-12-hydroxyoctadec-9-enoic acid.[5] It is used in some parts of the world in pregnant women for inducing labor.[6]
A study showed that over 50% of those subjected to intervention with castor oil went into active labor within 24 h while in the control group labor percentage was only 4%.[7] On the other hand another observational study which was carried out on data of 10-year follow-up duration with larger population found no beneficial effect for castor oil on labor induction.[8] A double-blind RCT also showed that the percentage of the IOL in castor oil group was significantly higher than the control group (almost three times).[9] Many midwives showed much interest in using “labour cocktail” especially castor oil, as a potent cathartic, to induce labor, however their efficiency and safety for IOL is poorly understood.[6,10,11] A comprehensive systematic review found that castor oil increases the prevalence of cesarean,[12] but[13,14,15] were not agreeing. Currently use of castor oil for IOL is on the basis of traditional knowledge and recommendations, rather than scientific records and it is not possible to make firm conclusions based on scattered clinical evidences with different results. Also, the results about the effect of castor oil on IOL and its effect on the prevalence of vaginal delivery compared to cesarean are contradictory and controversial. To our knowledge so far only one systematic review and meta-analysis evaluated the effect of herbal medicine on labor induction generally which included raspberry, castor oil, and general use of herbal medicine all together[16] and since it was not done specifically on castor oil, it was confusing and difficult to find the effect of castor oil on labor induction by primary searching of the databases. Therefore in the present systematic review and meta-analysis we aimed to study the effectiveness of castor oil on labor induction and prevalence of vaginal delivery along with investigating its safety.
Materials and Methods
Present systematic review and meta-analysis was performed in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement recommendations for published articles with no date limitation for beginning until September 2020.[17] We conducted a comprehensive search of both observational and Randomized Clinical Trials (RCTs) covering PubMed, Scopus, Web of Sciences, and Google scholar up to September 2020. English and Persian language articles were considered. Moreover, we reviewed reference list of retrieved articles for additional studies. We used different combinations of the following search key terms and MeSH terms: labor, labour, induction, inducing, and castor oil. Operations within each component used “OR” Boolean operator, and operations between components used “AND”. All articles were uploaded in EndNote software and then analyzed for duplication, screening, and data extraction. Next the titles and abstracts were reviewed for possible exclusion. The following data were recorded independently by two authors (Atefeh Amerizadeh and Ziba Farajzadegan): first author's surname, publication year, country, sample size in test and control groups, age, gestational age, number of induced labor in control and test groups, study type, complications, and the percentage of vaginal delivery with and without use of castor oil. All these steps were performed by two reviewers (Amerizadeh and Farajzadegan) at the same time and independently. RCTs and observational studies (cohort or case-control) were eligible for inclusion.
Patient/Problem/Population; Intervention/Exposure; Comparison and Outcomes (PICO) in our study was: study population of pregnant women at term or post-term pregnancy (37–42 weeks)/use of castor oil as an intervention for IOL/comparison of induced labor in either pregnant woman who use castor oil or those who did not use castor oil/induced labor (if active labor began 24 h after using castor oil), vaginal delivery, complications, and safety issues were reported as outcomes. In all studies, the method of consumption of castor oil was the same and it was consumed orally.
To evaluate the quality of the observational studies, the Newcastle-Ottawa Scale (NOS) was used.[18] To evaluate risk of bias of included RCTs in the present meta-analysis, the Cochrane Collaboration's tool was used. The risk of bias tool covers six main domains of bias: performance bias, selection bias, attrition bias, detection bias, reporting bias, and other bias. Within each domain, assessments are made for one or more items, which may cover different aspects of the domain, or different outcomes. Each RCT was given one of three rankings, “high risk”, “low risk”, or “unclear risk”, in each of the these domains. Low risk of bias meant that the bias is unlikely to change the outcomes. Unclear risk of bias meant that insufficient information is provided about the main areas and this raised some doubts about the results. High-risk of bias meant that the bias might change the outcomes.[19]
We extracted the number of events in both the cases: castor oil and control groups, from each article and reported the Risk Ratio (RR) with a 95% CI as the overall effect size. Also the proportion with 95% CI was used to report the number of vaginal delivery in each group. Heterogeneity between the studies was assessed using I2 and Q statistic.[20] In case of heterogeneity (I2 > 50 and p < 0.05), random effect model was used and otherwise, fixed effect model was applied to combine the results of the studies. Publication bias was assessed using the Egger's regression test[21] and the “trim and fill” method was used if any publication bias was significant.[22] All statistical analyses were performed in Stata version 14.
Ethical considerations
This manuscript has no plagiarism. The results of the analysis were completely honest. Any data fabrication has been avoided. This article does not contain any studies with human participants performed by any of the authors.
Results
Labor induction
The detailed procedure of literature search and study selection is shown in Figure 1. Searches in the PubMed, Scopus, Web of Sciences, EMBASE, and Google scholar databases returned a total of 436 papers. Finally, after removing duplication and undesired title, and those with not-sufficient data 14 papers were remaining. Of the 14 eligible studies 2 were excluded because 1 had no control group[23] and 1 only reported results on the percentage of vaginal delivery after IOL and did not report results on the number of induced labor after use of castor oil in the control and the intervention groups.[24] Finally 12 studies were remained which included in our study to evaluate the effect of castor oil on labor induction and prevalence of vaginal delivery.[7,8,13,14,15,25,26,27,28,29,30,31]
Figure 1.
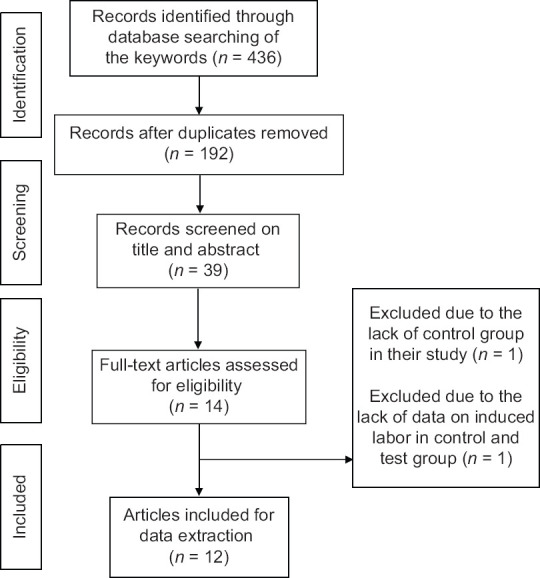
Flow chart of detailed procedure of literature search and study selection
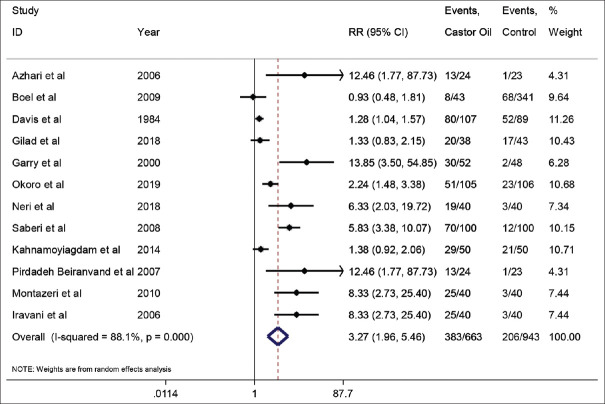
The main characteristics of the selected studies have been summarized in Table 1. Totally 1653 pregnant women cases were involved in these studies. Figure 2 shows the mean age of pregnant women in the castor oil group which was 24.72 years and Figure 3 shows the mean age of pregnant women in the control group which was 24.67 years old. These results showed that there were no significant differences between the two groups in terms of age range. The pooled results of the 12 studies showed that labor induction was significantly higher in castor oil group than control group. Figure 4 shows the forest plot of the effect of castor oil on labor induction, with risk ratio (RR: 3.27; 95% CI (1.96, 5.46).
Table 1.
Characteristics of studies included in this meta-analysis
| First author’s surname | Year | Type of study | Age: year | Gestational age | Total no=test and control (n) | Pregnancy | IOL in test group n(%) | IOL* in control group n(%) | Significant complications/safety | Explanations and/or other outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| Azhari et al.[25] | 2006 | RCT** | 19-35 | 40-42 weeks | 47=24 and 23 | Term/singleton | 13/24 (54.20%) | 1/23 (4.30%) | Nausea was 48% in castor oil group vs 0% in control group | The mean bishop score in the castor oil group increased from 2.50±1.29 to 6.79±3.20 [p<0.001]. The differences in terms of 5 min Apgar score, neonate birth weight, meconium amniotic fluid staining was not significant between control and castor oil groups |
| Boel et al.[8] | 2009 | retrospective cohort (history cohort) | 28±7 | 40-41 weeks | 384=43 and 341 | Term | 8/43 (27.90%) | 68/341 (41.60%) | No | No evidence for harm of castor oil on mother or baby and also no beneficial effect of castor oil on mother or baby was seen |
| Davis[13] | 1984 | Retrospective cohort (history cohort) | 28.60 | 37-42 weeks | 196=107 & 89 | Term/singleton | 80/107 (75%) | 52/89 (58%) | No | The effect of castor oil was more pronounced in primiparas; 75% in castor oil vs 54% in control groups. Caesarean incidence was three times in control vs castor oil group (p<0.001) |
| Gilad et al.[26] | 2018 | Prospective, randomized, double-blind, placebo-controlled clinical trial | 29±5 | 40-42 weeks | 81=38 and 43 | low-risk/post-date singleton | 20/38 (52.60%) | 17/43 (39.50%) | Bowel movement-no serious adverse effect | There were no differences in terms of rates of meconium staining of amniotic fluid, abnormal fetal heart rate tracing, cesarian section and instrumental deliveries, 5 min Apgar score, and the rate of chorio amnionitis, hypertensive complications of pregnancy, retained placenta and PPH between groups. Castor oil is effective for labor induction, in post-date multiparous women but not in primiparous women |
| Garry et al.[7] | 2000 | RCT | 24.80±6.70 | 40-42 weeks | 100=52 and 48 | Term/singleton | 30/52 (57.70%) | 2/48 (4.20%) | No | 5-min Apgar score, neonate birth weight, meconium amniotic fluid staining was same between control and intervention groups |
| Okoro et al.[28] | 2019 | RCT | 28.7±3.9 | 40-41 weeks | 211=105 and 106 | 51/105 (48.6%) | 23/106 (21.70%) | No | Complications were also similar in the two groups and were mainly “presumed” fetal distress, prolonged labor, maternal exhaustion and prolonged second stage labor | |
| Neri et al.[15] | 2018 | Retrospective observational case-control study | 32.8±4.7 | 40-41 weeks | 80=40 and 40 | singleton/low-risk | 19/40 (47.50%) | 3/40 (7.50%) | Mild nausea and diarrhoea which treated with common medicaments, no need for special care | Women in castor oil group showed a higher incidence of vaginal delivery and lower caesarean rate but the difference was not statistically significance |
| Saberi et al.[30] | 2008 | RCT | 26.4±4.93 | 40-42 weeks | 200=100 and 100 | Term/singleton | 70/100 (70%) | 30/100 (30%) | No | 5-min Apgar score, neonate birth weight, meconium amniotic fluid staining was same between control and intervention groups |
| Kahnamoyiagdam et al.[14] | 2014 | RCT | 22.64 | 41 week | 100=50 & 50 | Term/singleton | 29/50 (58%) | 21/50 (42%) | No | Caesarean rate was lower in castor oil group (36%) vs control (44%) but it was not significant |
| Pirdadeh Beiranvand et al.[29] | 2007 | RCT | 25.4±4.4 | 40-42 weeks | 47=24 and 23 | Term/primigravida | 13/24 (54.20%) | 1/23 (4%) | No | The mean Bishop score in the castor oil group increased from 2.50±1.29 (at first) to 6.79±3.20 (at the end) (p<0.001) |
| Montazeri et al.[27] | 2010 | RCT | 40-42 weeks | 80=40 and 40 | Term/singleton | 25/40 (62.50%) | 3/40 (7.50%) | No | 5-min Apgar score, neonate birth weight, meconium amniotic fluid staining was same between control and intervention groups | |
| Iravani et al.[31] | 2006 | RCT | 80=40 and 40 | post-term/singleton | 25/40 (62.50%) | 3/40 (7.50%) | No | 5-min Apgar score, neonate birth weight, meconium amniotic fluid staining was same between control and intervention groups |
*Induction of Labour, **Randomized Clinical Trials
Figure 2.
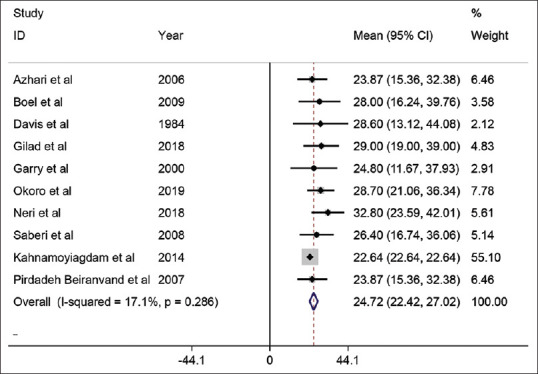
The mean age of pregnant women in castor oil group
Figure 3.
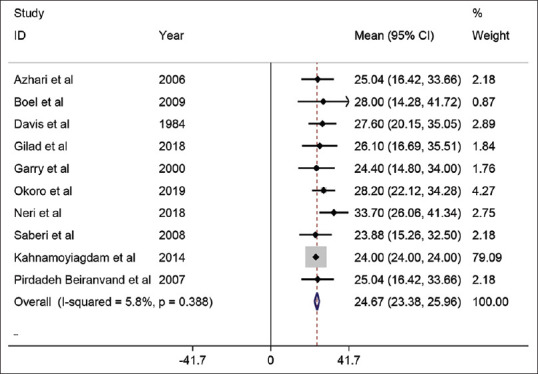
The mean age of pregnant women in control group
Figure 4.
Forest plot of effect of castor oil on labor induction RR(risk ratio)
Vaginal delivery
Pooled results of ten studies on the prevalence of vaginal delivery showed that the proportion of vaginal delivery was higher in castor oil group compared to the control group 81% vs 69%. Figure 5 shows the prevalence of vaginal delivery in the castor oil group and Figure 6 shows the prevalence of vaginal delivery in the control group.
Figure 5.
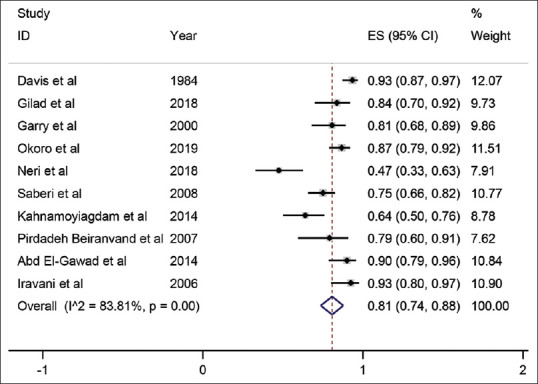
Prevalence of vaginal delivery in castor oil group
Figure 6.
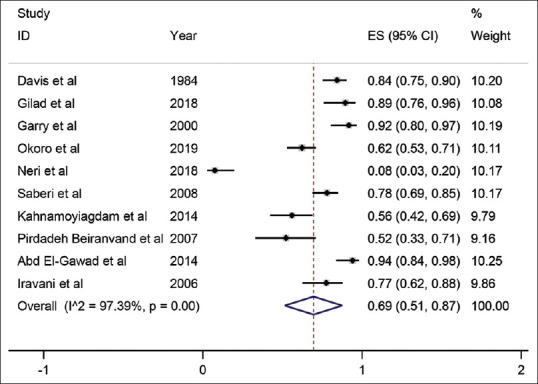
Prevalence of vaginal delivery in control group
Possible side effects
The possible side effects of consuming castor oil in each article were collected and listed in Table 1. Nine studies reported no side effects for applying castor oil. Two studies reported mild nausea and diarrhoea which were treated with common medicaments, and one study reported only more bowel movement.
Publication bias
The result of Egger test for checking the publication bias was significant (p < 0.001). Therefore, the Trim and Fill method was used to modify the result which showed that the result was still significant and only numerically different (RR: 5.38; 95% CI (3.81, 6.94)).
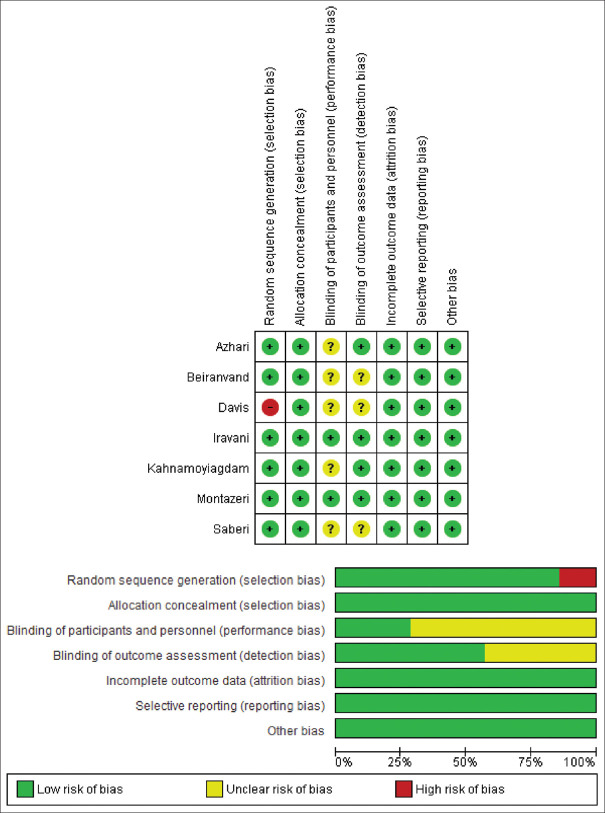
Quality assessment
To assess the quality of the included RCTs, we used the risk of bias table. In this table, the bias of each study was evaluated in some area such as selection bias, performance bias, etc., From seven RCTs, only one study had limitations on randomization and three studies did not explain blindness and had an unknown risk. In general, all studies were out of bias. This table was designed according to Review Manager 5.3 [Figure 7]. To assess the quality of the observational studies, their methodological quality was assessed by the nine-star Newcastle Ottawa Scale (NOS),[18] which consists of three major aspects: selection, comparability, and exposure or outcome. All included observational studies were more than 7 score and were considered high-quality.
Figure 7.
Percentage of risk of bias in each domain in all included RCTs
Discussion
Considering the results of the present systematic review and meta-analysis, use of castor oil in laboring women could be propounded as a safe and effective non-pharmacological method to induce labor. It also can increase the prevalence of vaginal delivery without any complications. Reasons to explain why use of herbal medicines such as castor oil for labor induction is important and how useful, effective, and safe it can be will be discussed in this section.
Labor induction
Labor induction is often necessary for patients with premature rupture of membranes. Effective use of oxytocin for IOL is well documented; however, it is not totally safe for both the mother and the infant.[13] Use of herbal medicines such as castor oil has a long history from mid-1950s.[15] Our results in accordance with another study showed that castor oil can induce labor significantly compared to the control group.[16] A prospective case control study showed that women who received castor oil have an increased probability of initiation of labor within 24 h after consumption of castor oil compared to women who receive no treatment and this increased percentage of IOL was completely independent of maternal age and neonate weight.[7] Another study also confirmed that there was a higher probability of IOL after the use of 60 ml of castor oil in their study[25]; however, a retrospective study reported that the time of birth was not significantly different between those who received castor oil and the control.[8] Significant difference in the rate of spontaneous labour onset between castor oil group and the control group was reported by Azhari et al. (54.20% versus 4.30%; p <0.001), by Garry et al. (57.70% versus 4.20%; p<0.001), and by Davis (75 versus 58; p<0.02). Based on the results of the previous studies,[7,13,15,16,25] and our study, and according to potential side effects of oxytocin, it seems logical to use castor oil in low-risk pregnant women. According to a study, oxytocin infusion after prostaglandins was needed in nine cases in the control group and none of the cases in the castor oil group.[15] Five studies found no significant differences between the two groups in terms of the age, pre-recruitment Bishop Score, parity, previous post-dates as well as previous labor induction.[7,8,13,25,28] A study from Nigeria, has argued that the use of castor oil to induce labor largely reduces the need for hospitalization and care by hospital staff.[28] Therefore, this could be useful in conditions of low resources and poor countries where maternal and infant health care services are often difficult for most people.
The possible mechanism for labor induction after oral ingestion of castor oil could be that ricinoleic acid is released by lipases in the intestinal lumen, and considerable amounts of ricinoleic acid are absorbed in the intestine which results in a strong laxative effect.[32,33] Ricinoleic acid affects intestinal smooth muscle and thus alters the intestinal ion transport and water flux.[34] Based on cellular signaling studies and small interfering RNA (siRNA) screening it has been observed that prostaglandin E2 receptors is the target of ricinoleic acid and EP3 receptor mediates the effects of castor oil on the motility of the uterus and the intestine. Using mice with constitutive and conditional EP3 or EP4 receptor deficiency showed that the pharmacological effects of castor oil are mediated by activation of EP3 receptors on smooth-muscle cells.[35]
According to the results of the present meta-analysis, in terms of vaginal delivery a significant increase was seen in the castor oil group (81% vs 69%). Davis[13] showed that number of vaginal delivery in castor oil group was significantly higher than control. Another report from Iran also reported higher percentage of vaginal delivery in castor oil group.[31] A more incidence of vaginal delivery in castor oil group was reported although this difference was not significant by others.[15] The clinical implication of this fact is that the consumption of castor oil does not seem to increase the rate of cesarean, and this fact can be an important and practical issue in environments where women hate cesarean.
Besides the well-documented labor-inducing effect of castor oil in pregnant females, use of this natural product for labor induction after 1950s was not recommended anymore because of its unwanted reported side effects, such as nausea and serious diarrhoea.[15] Since the issue of maternal and neonatal safety is of a great importance we evaluated the safety of castor oil in our systematic review. It was seen that only one study reported higher incidence of nausea (48% in castor oil group vs 0% in control group) and higher incidence of meconium-stained amniotic fluid (three times higher in control group).[25] Another study reported more bowel movement.[26] Three studies also reported higher percentage of post-partum hemorrhage in castor oil group[8,15,26]; however, the differences were not significant compared to the control. In an RCT on 81 women with a low-risk post-date singleton pregnancy some complications were reported for castor oil group such as retained placenta and hemorrhage, but overall the incidence of complications in castor oil group was lower compared to the control group.[26] The good infant results with no significant maternal morbidity and deaths has been reported.[13] The expected side effect of castor oil such as diarrhea in their study did occur in almost every pregnant woman in both groups. A Nigerian study documented that labor complications were almost similar between these two groups and were mainly maternal exhaustion, and prolonged labor time.[28]. In total no mother death was recorded in each group and only one case of stillbirth was reported which was in the control group.[8] Only mild side effects were reported for the use of castor oil in the intervention group compared to the control group, which could be controlled with conventional drugs and no special care was required.
Given the vitality of maternal and infant health, the result of higher quality studies involving a wide range of outcomes of neonatal and maternal mortality are needed to assess the safety of castor oil in pregnant women for induction of labor. Also the recommendation on the use of this drug should be done only after consulting with the doctor. In this review, no time and language restrictions were applied in searching mentioned databases; however, the possibility of missing some related articles cannot be ruled out.
Conclusion
According to the results of this study it can be concluded that use of castor oil can increase the rate of labor induction and also the prevalence of vaginal delivery in pregnant women with no serious harmful effects. More high-quality studies are needed to confirm the safety of this compound. This systematic review shows the need to develop guidelines for the use of herbal medicines specially castor oil in pregnant women. There is also a need for more clinical trials and also experimental studies in this regard in different countries of the world, based on which a definite and reliable result can be obtained.
Financial support and sponsorship
Nil.
Conflicts of interest
Nothing to declare.
Acknowledgments
The first author received finical support from Isfahan University of Medical Sciences as postdoctoral researcher.
References
- 1.Caughey AB, Sundaram V, Kaimal AJ, Cheng YW, Gienger A, Little SE, et al. Maternal and neonatal outcomes of elective induction of labor. Evid Rep Technol Assess (Full Rep) 2009:1–257. [PMC free article] [PubMed] [Google Scholar]
- 2.Marconi AM. Recent advances in the induction of labor. F1000Res. 2019:8. doi: 10.12688/f1000research.17587.1. F1000 Faculty Rev-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hall HG, McKenna LG, Griffiths DL. Complementary and alternative medicine for induction of labour. Women Birth. 2012;25:142–8. doi: 10.1016/j.wombi.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 4.Vogel JP, Osoti AO, Kelly AJ, Livio S, Norman JE, Alfirevic Z. Pharmacological and mechanical interventions for labour induction in outpatient settings. Cochrane Database Syst Rev. 2017;9:CD007701. doi: 10.1002/14651858.CD007701.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKeon T. Castor (Ricinus communis L.) USA AOCS Press; 2016. pp. 75–112. [Google Scholar]
- 6.Kelly AJ, Kavanagh J, Thomas J. Castor oil, bath and/or enema for cervical priming and induction of labour. Cochrane Database Syst Rev. 2013;2013:CD003099. doi: 10.1002/14651858.CD003099. [DOI] [PubMed] [Google Scholar]
- 7.Garry D, Figueroa R, Guillaume J, Cucco V. Use of castor oil in pregnancies at term. Altern Ther Health Med. 2000;6:77–9. [PubMed] [Google Scholar]
- 8.Boel ME, Lee SJ, Rijken MJ, Paw MK, Pimanpanarak M, Tan SO, et al. Castor oil for induction of labour: Not harmful, not helpful. Aust N Z J Obstet Gynaecol. 2009;49:499–503. doi: 10.1111/j.1479-828X.2009.01055.x. [DOI] [PubMed] [Google Scholar]
- 9.Gilad R, Hochner H, Vinograd O, Saam R, Hochner-Celnikier D, Porat S. 148: The CIC Trial–castor oil for induction of contractions in post-term pregnancies. Am J Obstetr Gynecol. 2012;206:S77–8. [Google Scholar]
- 10.Kozhimannil KB, Johnson PJ, Attanasio LB, Gjerdingen DK, McGovern PM. Use of nonmedical methods of labor induction and pain management among U.S. women. Birth. 2013;40:227–36. doi: 10.1111/birt.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall HG, McKenna LG, Griffiths DL. Midwives’ support for complementary and alternative medicine: A literature review. Women Birth. 2012;25:4–12. doi: 10.1016/j.wombi.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Boltman-Binkowski H. A systematic review: Are herbal and homeopathic remedies used during pregnancy safe? Curationis. 2016;39:1514. doi: 10.4102/curationis.v39i1.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis L. The use of castor oil to stimulate labor in patients with premature rupture of membranes. J Nurse-Midwifery. 1984;29:366–70. doi: 10.1016/0091-2182(84)90166-6. [DOI] [PubMed] [Google Scholar]
- 14.Kahnamoyiagdam F, Aghamohammadi M, Rostamnejad M. The effect of castor oil on the induction of labor: A clinical trial. Nurs Midwifery J. 2014;12:348–53. [Google Scholar]
- 15.Neri I, Dante G, Pignatti L, Salvioli C, Facchinetti F. Castor oil for induction of labour: A retrospective study. J Matern Fetal Neonatal Med. 2018;31:2105–8. doi: 10.1080/14767058.2017.1336223. [DOI] [PubMed] [Google Scholar]
- 16.Zamawe C, King C, Jennings HM, Mandiwa C, Fottrell E. Effectiveness and safety of herbal medicines for induction of labour: A systematic review and meta-analysis. BMJ Open. 2018;8:e022499. doi: 10.1136/bmjopen-2018-022499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.DeMaria AL, Sundstrom B, Moxley GE, Banks K, Bishop A, Rathbun L. Castor oil as a natural alternative to labor induction: A retrospective descriptive study. Women Birth. 2018;31:e99–104. doi: 10.1016/j.wombi.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Abd El-Gawad S. Castor oil safety and effectiveness on labour induction and neonatal outcome. J Biol Agric Healthcare. 2014;4:1–10. [Google Scholar]
- 25.Azhari S, Pirdadeh S, Lotfalizadeh M, Shakeri MT. Evaluation of the effect of castor oil on initiating labor in term pregnancy. Saudi Med J. 2006;27:1011–4. [PubMed] [Google Scholar]
- 26.Gilad R, Hochner H, Savitsky B, Porat S, Hochner-Celnikier D. Castor oil for induction of labor in post-date pregnancies: A randomized controlled trial. Women Birth. 2018;31:e26–31. doi: 10.1016/j.wombi.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 27.Montazeri S, Afshary P, Souri H, Iravani M. Efficacy of castor oil for induction and augmentation of labor. Iran J Pharm Res. 2010;3(Suppl 2):38–9. [Google Scholar]
- 28.Okoro O, Ugwu E, Dim C, Ozumba B, Nkwo P, Leonard A, et al. Effectiveness of castor oil in preventing post-term pregnancy in low resource setting: A randomized controlled trial. Am J Clin Med Res. 2019;7:37–43. [Google Scholar]
- 29.Pirdadeh Beiranvand S, Azhari S, Lotfalizadeh M, Shakeri M. The effect of castor oil on initiating labor in 40-42 weeks pregnancy. J Babol Univ Med Sci. 2007;9:33–8. [Google Scholar]
- 30.Saberi F, Abedzadeh M, Sadat Z, Eslami A. Effect of castor oil on induction of labor. KAUMS J (FEYZ) 2008;11:19–23. [Google Scholar]
- 31.Iravani M, Montazeri S, Afshari P, Souri H. A study on the safety and efficacy of castor oil for cervical ripening and labour induction. Jundishapur Sci Med J. 2006;5:398–404. [Google Scholar]
- 32.Mathias JR, Martin JL, Burns TW, Carlson GM, Shields RP. Ricinoleic acid effect on the electrical activity of the small intestine in rabbits. J Clin Invest. 1978;61:640–4. doi: 10.1172/JCI108975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burdock GA, Carabin IG, Griffiths JC. Toxicology and pharmacology of sodium ricinoleate. Food Chem Toxicol. 2006;44:1689–98. doi: 10.1016/j.fct.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 34.Ammon HV, Thomas PJ, Phillips SF. Effects of oleic and ricinoleic acids on net jejunal water and electrolyte movement. Perfusion studies in man. J Clin Invest. 1974;53:374–9. doi: 10.1172/JCI107569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tunaru S, Althoff TF, Nüsing RM, Diener M, Offermanns S. Castor oil induces laxation and uterus contraction via ricinoleic acid activating prostaglandin EP3 receptors. Proc Natl Acad Sci U S A. 2012;109:9179–84. doi: 10.1073/pnas.1201627109. [DOI] [PMC free article] [PubMed] [Google Scholar]