Abstract
Background:
Relatively few studies have compared outcomes between helicopter transport (HT) and ground transport (GT) for the inter-facility transfer of trauma patients to tertiary trauma centers (TTC). Mixed results have been reported from these studies ranging from a slight increase in odds of survival for the severely injured to no evident benefit for HT patients. We hypothesized there was no adjusted difference in mortality between patients transported interfacility by HT or GT taking into account distance from TTC.
Methods:
Data from an inclusive statewide trauma registry was used to conduct a retrospective cohort study of adult (18+ years old) trauma patients who initially presented to a non-tertiary trauma center (NTC) before subsequent transfer by HT or GT to a TTC. Records from the NTC and TTC were linked (N=9880). We used propensity adjusted, multivariable Cox proportional hazards models to assess the association of HT on mortality at 72-hour and within the first 2 weeks of arrival at a TTC; these multivariable analyses were stratified by distance (miles) between NTC and TTC: 21-90, and greater than 90.
Results:
Mean distance between NTC and TTC was greater for HT patients, 96.7 miles versus 69.9 miles for GT. A higher proportion of patients among the HT group had an ISS of 16 or higher (24.6% vs 10.9%), an initial SBP<90 mmHg (7.3% vs 2.8%), and GCS<10 (12.5% vs 3.7%) than the GT group. HT was associated with significantly decreased 72-hour mortality (HR 0.65, 95%CI 0.48-0.90) for patients transferred from a NTC <90 miles from the TTC. No association was seen for patients transferred more than 90 miles to the TTC. No significant association of HT and 2-week mortality was seen at any distance from the TTC.
Conclusions:
Only for patients transferred from an NTC <90 miles from the receiving TTC was HT associated with a significantly decreased hazard of mortality in the first 72 hours. Many HT patients, especially from the most distant NTCs, had minor injuries and normal vital signs at both the NTC and TTC suggesting the decision to use HT for these patients was resource-driven rather than clinical.
Keywords: Helicopter ambulance, Trauma, Interfacility transfer
Background
Helicopter transport (HT) has become common place as an emergency medical transport tool in developed countries and in a rural state such as Oklahoma, helicopters may be the only means of rapid access to tertiary (Level I or II) trauma centers (TTC) for patients injured outside the metropolitan areas. A number of studies have found a reduction in in-hospital mortality for patients transported by helicopter ambulance from the scene of injury1-3. Moreover, some studies have found improved survival for patients initially seen in a non-tertiary trauma center (NTC) and subsequently transferred to a TTC4-5. However, relatively few studies have addressed the question of whether HT improves survival, over ground EMS transport (GT), among inter-facility transported patients.
Helicopter ambulances are expensive to maintain and operate and are often very costly to the patient and/or their insurance carrier. Helicopter transport can also be dangerous, particularly in certain circumstances such as nighttime missions and scene responses to unfamiliar locations6. These issues are more troubling when one considers studies of HT have invariably identified large numbers of patients where the expense and risk associated with HT did not appear warranted7-9.
A review of the literature has shown mixed results for benefits of HT when used for inter-facility transfer. One study using National Trauma Data Bank data found a significant, albeit very small (9%), increase in odds of survival with HT but only for patients with an ISS 16 or higher10. Borst et al compared HT patients to advanced life support (ALS) GT patients for whom HT had been requested but not used because of weather conditions and found no survival benefit of HT. Another study compared injury mortality before and after the loss of HT resources and found an increase mortality in the region that had lost HT services12. Two older studies also had conflicting results. Boyd et al, using a TRISS based method found a survival benefit for HT while a larger study by Arfken et al. found no difference in mortality for HT and GT patients. These previous studies did have notable limitations, the most significant being a lack of data from the NTC and no direct measure of distance between NTC and TTC.
We hypothesized there was no difference in in-hospital mortality between patients transported inter-facility by HT or GT after adjustment for propensity to be transferred, and other potentially confounding covariates as well as taking into account the potential effect modification of distance from TTC on observed outcomes.
Methods
This was a retrospective cohort study of trauma patients who initially presented to a NTC before subsequent transfer to a TTC. Data from 2005 to 2014 were obtained from the Oklahoma State Trauma Registry (OSTR). Oklahoma has a mandatory inclusive trauma system and all state licensed hospitals are required to report data to the OSTR and injured patients transferred inter-facility are required to be reported regardless of severity. As of December of 2014, was a total of 109 state-licensed hospitals in Oklahoma: one centrally (Oklahoma City) located American College of Surgeons (ACS) verified Level I TTC, 2 Level II TTCs (one ACS verified) in the northeast (Tulsa), 26 Level III NTCs, and 80 Level IV NTCs. Both the Oklahoma State Department of Health and University of Oklahoma Health Sciences Center Institutional Review Boards approved this study.
A total of 16171 inter-facility transferred adult (age 18+) patients treated at a TTC were identified from the OSTR. Patients TTC records were linked to their NTC records deterministically and probabilistically using SAS based LinkPro. Variables used for linkage included: first name, last name, age, Soundex of last name, date of birth, SSN, injury date, and emergency department arrival date. Additional conditional comparisons using the same variables were used as well (e.g. arrival date within 1 day). Probabilistically linked records were manually reviewed to ensure legitimate matches.
Road distance was determined by using the physical addresses of NTCs and TTCs and publicly available online navigation tools to create road distance lookup tables. Each patient was then matched to the corresponding NTC-TTC combination to find the transport distance.
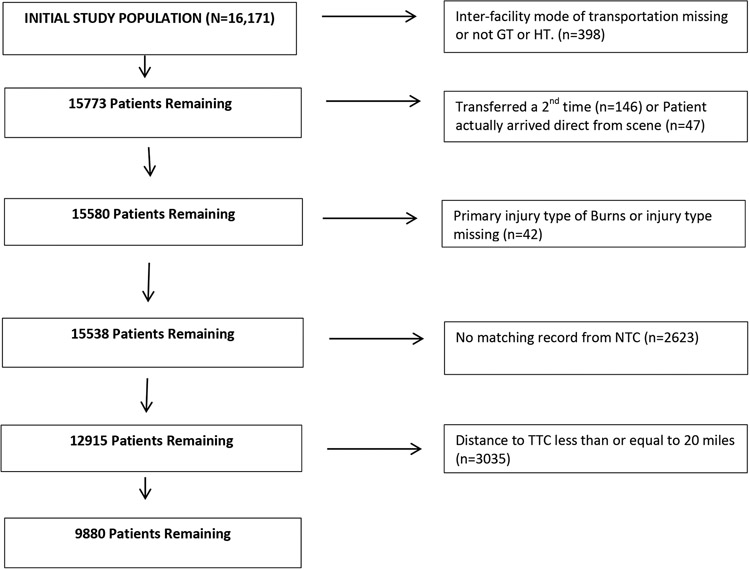
Patients not transported inter-facility by HT or GT or for whom mode of transport was unknown were excluded (n=398) as were patients transferred a second time (n=146) or were found to have arrived directly from the scene (n=42) (Figure 1). Patients without a matching NTC OSTR record (n=2623) were also excluded. Finally, patients arriving at a NTC 20 miles or closer to the receiving TTC were excluded (n=3035) due to the low probability of being transported by HT. After applying all exclusions 9880 patients were available for analysis (Figure 1).
Figure 1.
Study Population
Variables collected primarily from the NTC included age, sex, race, injury type, mechanism of injury, prehospital mode of transport, NTC trauma level, local ground EMS resources, elapsed time from arrival at NTC to arrival at TTC, weekend vs weekday transfer, and primary payer. Additional clinical and injury severity measures included EMS\NTC intubation, initial NTC vital signs, shock (SBP<90), GCS<10, comorbidities, injury severity score (ISS), severe injury (any AIS≥3), and length of stay (LOS). Multiple injury, defined as more than one body region with an AIS>=2 and again using AIS>=1, was also created for each patient.
Additional clinical factors collected at the TTC included initial vital signs (systolic blood pressure (SBP), heart rate (HR), respiratory rate (RR)), Glasgow Coma Score (GCS), weighted revised trauma score, severe head injury (AIS>=3), and final ISS. Emergency department (ED) disposition, minutes spent in the ED (EDMins), hospital length of stay in hours (LOS), hospital discharge disposition, and mortality were also collected. The primary outcome of interest, mortality, was considered at two different time points: within the first 72 hrs and within the first 2 weeks. The 2 week time point was chosen because it seemed unlikely mortality beyond that point could be related to inter-facility mode of transport.
Categorical variables were summarized using frequencies and proportions for HT and GT patients. Continuous variables were summarized using means and standard deviations. Bivariate assessments of association of transport mode (HT vs GT) with categorical variables was done using chi-square or Fisher’s exact tests. Bivariate tests of association with continuous variables were done using t-tests; or for non-normally distributed variables the Mann-Whitney U test, using an alpha level of p<0.05.
Multivariable Analyses
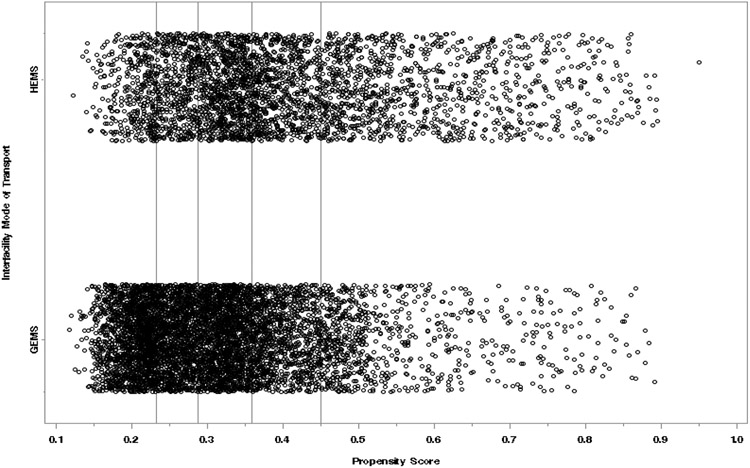
Patients are not randomly selected for transport by helicopter or ground EMS. The more severely injured patients are generally indicated for HEMS transport, therefore propensity-adjusted survival analyses were used to evaluate the effect of transport mode on mortality. The final propensity score model (Area Under the Curve [AUC] 0.67, 95%CI: 0.66–0.68) included the following variables: age, mechanism of injury, prehospital mode of transport, trauma level of transferring facility, intubation status, initial ED vital signs (SBP and GCS) and anatomical injuries (severe head, thorax, and abdomen) as recorded by the transferring facility as well as presence of multisystem injuries. A graphical evaluation of propensity score distribution indicated adequate overlap between the two groups across the range of propensity score with at least 10% representation of each group in each quintile (Figure 2.) Propensity adjusted, multivariable, Cox proportional hazards models were developed to assess the association of HT on 72-hour and within the first 2 weeks of arrival at a TTC. In addition, these multivariable analyses were stratified by distance between the NTC and TTC: 21-90, and >90 miles. The proportional hazards assumption was assessed both graphically and by testing a time-transport mode interaction term in the models. Excluded from the multivariable analyses were 307 patients that were missing ISS or SBP or GCS from the NTC. Among these excluded, there were 11 (11.2%) and 6 (2.9%) deaths among the HT and GT patients respectively.
Figure 2.
Propensity score distribution across quintiles by transport mode.
Results
Among the 9880 study eligible patients, 3424 (34.7%) were transported inter-facility to the TTC by HT. HT patients were slightly younger, more often male, more frequently injured in a traffic-related incident, more frequently transferred from a Level IV NTC, and more often arrived at the NTC via EMS. In addition, HT patients were on average transferred from NTCs farther from the TTC and were more frequently injured in areas served by basic or intermediate GT services. The median number of hours from arrival at the NTC to arrival at the TTC were 3.4 hours and 4.5 hours for HT and GT patients respectively. The median times were also shorter for HT within each distance strata (Table 1).
Table 1.
Demographic and Injury Characteristics by Inter-facility Mode of EMS Transport
| HT (n= 3424) |
GT (n=6456) |
P values |
|
|---|---|---|---|
| Variable | |||
| Mean Age (SD) | 45.2(20.1) | 47.5 (20.9) | <.0001 |
| Age ≥55 yrs, n (%) | 1091(31.9) | 2284(35.4) | 0.0005 |
| Male, n(%) | 2442(71.5) | 4318(67.0) | <.0001 |
| Race, n (%) | 0.0026 | ||
| White | 2799(81.8) | 5344(82.8) | |
| Black | 192(5.6) | 319(4.9) | |
| Native American/Alaskan Native | 283(8.3) | 582(9.0) | |
| Asian /Pac Island | 4(0.1) | 19(0.3) | |
| Other | 142(4.2) | 190(2.9) | |
| Penetrating Injury, n (%) | 479(14.0) | 646(10.0) | <.0001 |
| MOI, n (%) | <.0001 | ||
| MVC | 1297(37.9) | 1961(30.4) | |
| Motorcycle | 282(8.2) | 322(5.0) | |
| Pedestrian | 84(2.5) | 112(1.7) | |
| Gunshot | 240(7.0) | 221(3.4) | |
| Stabbing | 201(5.9) | 315(4.9) | |
| Falls | 675(19.7) | 1916(29.7) | |
| Other | 646(18.9) | 1613(25.0) | |
| Prehospital Mode of transport, n(%) | <.0001 | ||
| EMS | 2429(71.8) | 3784(59.5) | |
| POV | 927(27.4) | 2470(38.8) | |
| Other | 27(0.8) | 106(1.7) | |
| NTC Trauma Level, n(%) | <.0001 | ||
| Level3 | 1344(39.3) | 2854(44.2) | |
| Level4 | 2080(60.7) | 3602(55.8) | |
| Local GEMS Resources serving NTC, n (%) | <.0001 | ||
| Basic | 997(29.1) | 1616(25.0) | |
| Intermediate | 1364(39.9) | 2582(40.0) | |
| Paramedic | 1061(31.0) | 2255(35.0) | |
| Local GEMS Resources Serving NTC, Mean(SD) | |||
| Num of vehicles | 5.8(4.3) | 6.8(5.2) | <.0001 |
| Num of personnel | 31.4(24.4) | 38.1(28.0) | <.0001 |
| Num of Paramedics | 14.0(11.6) | 18.2(13.8) | <.0001 |
| Mean Distance toTTC, miles (SD) | 96.7(45.9) | 69.9(35.1) | <.0001 |
| Distance to TTC, n(%) | <.0001 | ||
| 21-59 miles | 773(22.6) | 3070(47.6) | |
| 60-90 miles | 868(25.4) | 1619(25.1) | |
| >90 miles | 1783(52.1) | 1767(27.4) | |
| Hrs Arrival NTC-Arrival TTC, Median(IQR) | 3.4(2.0) | 4.5(2.4) | <.0001 |
| Hrs Arrival NTC-Arrival TTC by Distance, Median (IQR) | <.0001 | ||
| 21-59 miles | 2.6(1.7) | 4.1(2.3) | |
| 60-90 miles | 3.0(1.9) | 4.4(2.2) | |
| >90 miles | 3.8(2.0) | 5.3(2.2) | |
| Weekend transfer, n(%) | 1706(50.1) | 3238(50.4) | 0.19 |
| Primary Payer, n(%) | 0.003 | ||
| Insurance | 987(28.9) | 1793(27.8) | |
| Self-pay | 1182(34.6) | 2050(31.8) | |
| Medicaid | 245(7.2) | 479(7.4) | |
| Medicare | 713(20.8) | 1562(24.2) | |
| Worker’s Comp | 164(4.8) | 298(4.6) | |
| Other | 130(3.8) | 264(4.1) |
HT patients had higher proportions of patients who were intubated or arrived with a SBP<90 mm Hg or had a GCS<10 (Table 2). Injury severity varied by transport mode with 24.6% of HT patients having ISS of 16 or higher versus 10.9% among GT patients. Overall, 40.6% of the HT group and 59.5% for the GT group had an ISS < 9. The HT group also had a higher proportion of patients with severe injury to the head (26.6% vs 17.9%) and chest (18.2% vs 9.6%) than the GT group. The mean LOS for HT patients was 3 days longer than GT patients.
Table 2.
Patients’ Clinical Characteristics and Outcomes by Inter-facility Mode of EMS Transport
| HT (n= 3424) |
GT (n=6456) |
P values | |
|---|---|---|---|
| Variable | |||
| EMS/Emergency Dept. Intubation, n(%) | 122(3.7) | 76(1.2) | <.0001 |
| Initial NTC Vital signs Mean (SD) | |||
| SBP | 133.3(30.7) | 138.4(27.2) | <.0001 |
| GCS | 13.3(3.4) | 14.4(2.0) | <.0001 |
| RR | 19.9(5.9) | 19.7(4.5) | 0.09 |
| HR | 91.8(23.5) | 88.3(19.3) | <.0001 |
| RTS | 7.4(1.2) | 7.7(0.6) | <.0001 |
| Shock (SBP <90mmHg), n(%) | 249(7.3) | 180(2.8) | <.0001 |
| TBI (GCS <10), n(%) | 417(12.5) | 229(3.7) | <.0001 |
| Overall comorbidity, n(%) | 995(29.1) | 1517(23.5) | <.0001 |
| Pulmonary Disease, n(%) | 207(6.1) | 471(7.3) | 0.02 |
| Diabetes, n(%) | 47(1.4) | 103(1.6) | 0.39 |
| Cardiac disease, n(%) | 517(15.1) | 866(13.4) | 0.02 |
| Coagulopathy, n(%) | 95(2.8) | 112(1.7) | 0.0006 |
| Liver disease, n(%) | 29(0.9) | 38(0.6) | 0.14 |
| Chronic renal failure, n(%) | 44(1.3) | 124(1.9) | 0.02 |
| Anemia 20 peripheral hemorrhage, n(%) | 363(10.6) | 276(4.3) | <.0001 |
| Cancer, n(%) | 14(0.4) | 30(0.5) | 0.69 |
| Mean ISS (SD) | 10.5 (8.4) | 7.6 (6.1) | <0.0001 |
| ISS Group, n (%) | <.0001 | ||
| <9 | 1337(40.6) | 3518(56.4) | |
| 9-14 | 1147(34.8) | 2041(32.7) | |
| 16-24 | 562(17.1) | 526(8.4) | |
| ≥25 | 248(7.5) | 155(2.5) | |
| Multisystem injury (AIS≥1), n(%) | 1757(51.3) | 2715(42.1) | <.0001 |
| Multisystem injury (AIS≥2), n(%) | 982(28.7) | 1227(19.0) | <.0001 |
| Severe Injury (AIS>=3), n (%) | |||
| Head/Neck/Face | 912(26.6) | 1154(17.9) | <.0001 |
| Chest | 623(18.2) | 621(9.6) | <.0001 |
| Abdomen | 128(3.7) | 120(1.9) | <.0001 |
| Extremity | 370(10.8) | 718(11.1) | 0.63 |
| Mean LOS (SD) | 8.2(11.0) | 5.1(11.2) | <.0001 |
| In-hospital Mortality, n (%) | 315(9.2) | 170(2.6) | <.0001 |
| Mortality by LOS Hours,n(%) | 0.63 | ||
| <24hrs | 118(37.5) | 56(32.9) | |
| 24hrs - <48hrs | 44(14.0) | 22(12.9) | |
| 48 hrs - <72hrs | 22(7.0) | 16(9.4) | |
| 72 hrs - <2weeks | 99(31.4) | 52(30.6) | |
| 2weeks - <30days | 23(7.3) | 19(11.2) | |
| ≥30days | 9(2.9) | 5(2.9) |
Overall, the crude mortality was significantly higher in patients transported by HEMS (9.2% vs 2.6%, p <0.0001). Upon multivariable analyses, a significant independent association between transport mode and 72-hour mortality was observed for patients within 90 miles of a tertiary trauma center (Table 3). After adjusting for the propensity to be transported by HEMS, male gender, pre-existing conditions, ISS, admission GCS at the TTC, presence of a serious head injury, and presence of a penetrating injury, transfer to a tertiary trauma center (Level I or II) by HEMS was associated with significantly lower 72-hour mortality (Hazard Ratio, 0.65; 95%CI:0.48-0.90). No independent association was observed between transport mode and 72-hour mortality for patients transported from greater than 90 miles from a tertiary trauma center. Additionally, there was no association between transport mode and 2-week mortality overall or stratified by distance (Table 4a). This lack of association was persistent whether patients who died or were discharged within 3 days of admission, were excluded (Table 4b).
Table 3.
Propensity-Adjusted Multivariable Analyses of the Impact of Inter-facility Mode of Transport on 72-hour Mortality in Trauma Patients Transferred to Tertiary Trauma Centers
| Variable | Overall 72-hour Mortality HR (95% CI) |
72-hour Mortality 21 – 90 Miles HR (95% CI) |
72-hour Mortality >90 Miles HR (95% CI) |
|---|---|---|---|
| HT | 0.79 (0.61-1.03) | 0.65 (0.48-0.90) | 1.49(0.86-2.60) |
| GT | ref | ref | ref |
| Male Gender | 0.7 (0.54 – 0.91) | 0.65 (0.47 – 0.91) | ˧ |
| Penetrating Injury | 1.99 (1.41-2.80) | 2.03 (1.29-3.18) | 2.07(1.21- 3.54) |
| Any Pre-existing Condition | 1.37 (1.05- 1.78) | 1.36 (0.98 – 1.89) | 1.48(0.95-2.31)* |
| TTC Initial ED SBP | 0.98 (0.97-0.99) | 0.98 (0.97-0.99) | 0.976(0.971-0.981) |
| TTC Initial GCS | 0.75 (0.72-0.78) | 0.72 (0.68 – 0.76) | 0.90 (0.75-0.86) |
| TTC Final ISS | 1.02 (1.01- 1.03) | 1.02 (1.00-1.03) | 1.03(1.02-1.04) |
| Severe Head Injury (AIS >=3) | 2.33(1.69 – 3.21) | 2.35 (1.55-3.57) | 2.25 (1.35-3.74) |
| Propensity Score | 3.16 (1.43-6.97) | 1.26 (0.45 – 3.49) | 15.60(4.05-60.15) |
HR=Hazard Ratio
dropped from model, p >0.05
p=0.08
TTC= Tertiary Trauma Center
Table 4a.
Propensity-Adjusted Multivariable Analyses of the Impact of Inter-facility Mode of Transport on 2-Week Mortality in Trauma Patients Transferred to Tertiary Trauma Centers
| Variable | Overall 2-Week Mortality HR (95% CI) |
2-Week Mortality 21 – 90 Miles HR (95% CI) |
2-Week Mortality >90 Miles HR (95% CI) |
|---|---|---|---|
| HT | 0.95 (0.77 – 1.18) | 0.90 (0.69 – 1.18) | 1.28 (0.86 – 1.92) |
| GT | ref | ref | ref |
| Age (Years) | 1.03 (1.02 – 1.04) | 1.04 (1.03 – 1.06) | 1.03 (1.02 – 1.03) |
| Penetrating Injury | 2.32 (1.71 – 3.15) | 2.86 (1.89 – 4.32) | 1.78 (1.12 – 2.81) |
| Any Pre-existing Condition | 1.27 (1.03 – 1.57) | ˧ | ˧ |
| TTC Initial GCS | 0.81 (0.79 – 0.83) | 0.80 (0.77 – 0.82) | 0.83 (0.80 – 0.87) |
| TTC Final ISS | 1.03 (1.02 – 1.05) | 1.03 (1.02 – 1.04) | 1.04 (1.02 – 1.05) |
| Severe Head Injury (AIS >=3) | 1.62 (1.23 – 2.09) | 1.59 (1.15 – 2.22) | 1.54 (1.03 – 2.29) |
| Propensity Score | 7.04 (3.65 – 13.58) | 3.92 (1.70 – 9.03) | 22.23 (7.50 – 66.16) |
HR=Hazard Ratio
dropped from model, p >0.05; TTC= Tertiary Trauma Center
Table 4b.
Propensity-Adjusted Multivariable Analyses of the Impact of Inter-facility Mode of Transport on *2-Week Mortality in Trauma Patients Transferred to Tertiary Trauma Centers
| Variable | Overall 2-Week Mortality HR (95% CI) |
2-Week Mortality 21 – 90 Miles HR (95% CI) |
2-Week Mortality >90 Miles HR (95% CI) |
|---|---|---|---|
| N (# of deaths) | 5350 (148) | 3320 (87) | 2030 (61) |
| HT | 1.27 (0.89 – 1.82) | 1.49 (0.93 – 2.37) | 1.07 (0.58 – 1.93) |
| GT | ref | ref | ref |
| Age (Years) | 1.05 (1.04 – 1.06) | 1.04 (1.03 – 1.06) | 1.04 (1.02 – 1.05) |
| Penetrating Injury | 2.10 (1.06 – 4.15) | 2.86 (1.17 – 6.97) | ˧ |
| Any Pre-existing Condition | 1.85 (1.30 – 2.63) | 1.94 (1.21 – 3.10) | ˧ |
| TTC Initial GCS | 0.88 (0.85 – 0.92) | 0.89 (0.84 – 0.93) | 0.87 (0.82 – 0.93) |
| TTC Final ISS | 1.03 (1.02 – 1.05) | 1.04 (1.01 – 1.06) | 1.03 (1.01 – 1.05) |
| Severe Head Injury (AIS >=3) | 1.90 (1.27 – 2.84) | 1.94 (1.15 – 3.27) | 1.77 (0.94 3.34) |
| Propensity Score | 3.71 (1.16 – 11.94) | 1.11 (0.22 – 5.58) | 18.42 (3.15 – 107.62) |
HR=Hazard Ratio
Excluding patients who died or were discharged within 3 days of admission
dropped from model, p >0.1; TTC= Tertiary Trauma Center
Discussion
Only for patients transferred from a NTC within 90 miles of the TTC was HT associated with a significantly reduced hazard of mortality in the first 72 hrs. Though the association with early mortality seems intuitive; that it was significant only for the patients closer to the TTC was somewhat surprising. The proportion of patients with an ISS≥16 was highest in the closest and most distant groups, however after further analyses, we found early physiologic derangements were more common in patients closest to the TTC. Based on previous experience with scene transports where a survival benefit for HT was most evident among patients with some early physiologic abnormalities this seems the most likely explanation for benefit among this select group2. Brown et al found a small increased odds of survival as well but only among patients with an ISS≥16. The vital signs information was not reported by ISS category in their paper but it is very likely abnormalities were more common among the ISS≥16 group.
Similar to Svenson et al, we found the overall times from arrival at the NTC to arrival at the TTC were shorter for HT within each distance strata. Unlike scene HT use where delays in helicopter arrival are very common, evaluation in the NTC gives the HT service time to arrive at the facility so the elapsed time at which GT and HT would depart the NTC would often be similar2. Nevertheless, it is important to note again that in previous research we found inter-facility transfers took an average of 3 times as long to reach the TTC when compared to scene transports from similar distances17.
A recent study by Nolan et al identified a wide array of causes of delay both related to EMS and the transferring facility. The most frequent helicopter-related delay was the need to refuel and for the transferring hospital, it was waiting for documentation18. So, though transport to a NTC may be necessary to provide temporizing intervention quickly if the intervention could not be provided in the field, it seems clear this will delay delivery of the patient to the TTC regardless of inter-facility mode of transport. Moreover, the beneficial effect of HT among scene transports is generally attributed to early access to an experienced advanced life support crew and rapid transport to a TTC1-3,11. With an average of 3-4 hours just from arrival at a NTC to arrival at the TTC neither of these proposed factors seem as relevant as they may be for scene transport. To minimize the delay to the TTC, the NTC should arrange transport very early on and avoid unnecessary testing that will not alter the immediate care of the patient.
Mortality as an outcome among inter-facility transfers is somewhat problematic because of an inherent survival bias. These patients have survived transport to the NTC, their time at the NTC, and inter-facility transport to the TTC making it more likely they will also survive to discharge. This has been discussed in studies of the effect of transfer to a TTC and is also tangentially reflected by Borst et al when they mention more than 200 (slightly over 5%) patients among their base cohort died before transfer4-5, 11. The true crude mortality for patients selected for inter-facility transfer is likely considerably higher if deaths at the NTC are considered and it is unfortunate, though understandable, these patients are often neglected in studies such as this one.
Here we found over 75% of the HT patients had an ISS<16 and mortality among this group was low (3.2%). The study by Brown et al found that, even with a very large group of patients in a NTDB study, a statistically significant survival benefit was not detected among patients with an ISS<1610. The seemingly high rate of overtriage to HT is somewhat surprising since one might expect triage of inter-facility patients would be more refined than that of scene patients given the controlled setting and additional hospital resources. It seems risk of mortality is often not the primary motivating factor for choosing HT and a lack of GT resources or lack of a GT resource willing to make lengthy transfers may be partially driving overuse of HT. In addition, there may be injuries, though not life threatening, which are considered time-sensitive and motivate HT use. One example is a study that looked at inter-facility transport of patients with spinal injury, however, they found GT to be just as safe as HT for moving these patients between hospitals19.
There are a number of limitations to this study worth noting. Though efforts were made to minimize the effects, bias and unmeasured factors may still be an issue with a retrospective design such as the one used here. Neither level/experience of the care provider nor specific treatments rendered at the NTC were available and these may have influenced survival of patients transported by either means. Location of HT and GT bases during the study period were not considered and might have had some influence on the times to definitive care, however, the data suggest it is likely less important than for scene transports. Data were also very limited with regard to patient stability and care rendered in transit between the NTC and TTC making it impossible to compare these factors for the two modes of transport. Finally, the focus on survival as the outcome may have neglected other important outcomes or reasons for HT.
In conclusion, using 10 years of data from a statewide trauma registry we found a survival advantage of HT for early mortality for a group of patients injured with 90 miles of a TTC. No survival advantage of HT was seen for any other group. Moreover, a large proportion of patients transported interfacility by HT did not have injury or vital sign indicators that would seem to warrant such an expensive and scarce resource.
Footnotes
Disclosure of Interest
The authors report no conflicts of interest.
References
- 1.Galvagno SM Jr, Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ Jr, Baker SP, Bowman SM, Pronovost PJ, Haider AH. Association between Helicopter vs Ground Emergency Medical Services and Survival for Adults with Major Trauma. JAMA. 2012; 307(15):1602–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart KE, Cowan LD, Thompson DM, Sacra JC, Albrecht R. Association of Direct Helicopter Transport versus Ground Transport and In-Hospital Mortality in Trauma Patients: A Propensity Score Analysis. Acad Emerg Med. 2011; 18(11):1208–1216. [DOI] [PubMed] [Google Scholar]
- 3.Thomas SH, Harrison TH, Buras WR, Ahmed W, Cheema F, Wedel SK. Helicopter Transport and Blunt Trauma Mortality: A Multicenter Trial. J Trauma. 2002; 52(1):136–145. [DOI] [PubMed] [Google Scholar]
- 4.Garwe T, Cowan LD, Neas B, Cathey T, Danford BC, Greenawalt P. Survival benefit of transfer to tertiary trauma centers for major trauma patients initially presenting to nontertiary trauma centers. Acad Emerg Med. 2010; 17(11): 1223–32. [DOI] [PubMed] [Google Scholar]
- 5.Newgard CD, McConnell KJ, Hedges JR, Mullins RJ. The benefit of higher level of care transfer of injured patients from nontertiary hospital emergency departments. J Trauma Acute Care Surg. 2007; 63(5):965–971. [DOI] [PubMed] [Google Scholar]
- 6.Baker SP, Grabowski JG, Dodd RS, Shanahan DF, Lamb MW, Li GH. EMS Helicopter Crashes: What Influences Fatal Outcome? Annals of Emergency Medicine. 2005; 47(4): 351–356. [DOI] [PubMed] [Google Scholar]
- 7.Vercruysse GA, Friese RS, Khalil M, Ibrahim-Zada I, Zangbar B, Hashmi A, Tang A, O’Keefe T, Kulvatunyou N, Green DJ, Gries L, Joseph B, Rhee PM. Overuse of helicopter transport in the minimally injured: A Healthcare System Problem that should be corrected. J Trauma Acute Care Surg. 2015; 78(3): 510–515. [DOI] [PubMed] [Google Scholar]
- 8.Cheung BH, Delgado MK, Staudenmayer KL. Patient and trauma center characteristics associated with helicopter emergency medical services transport for patients with minor injuries in the United States. Acad Emerg Med. 2014; 21(11):1232–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bledsoe BE, Wesley AK, Eckstein M, Dunn TM, O’Keefe MF. Helicopter Scene Transport of Trauma Patients with Non-Life Threatening Injuries: A Meta-Analysis. J Trauma. 2006; 60(6):1257–1265. [DOI] [PubMed] [Google Scholar]
- 10.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters Improve Survival in Seriously Injured Patients Requiring Interfacility Transfer for Definitive Care. J Trauma. 2011; 70(2):310–314. [DOI] [PubMed] [Google Scholar]
- 11.Borst GM, Davies SW, Waibel BH, Leonard KL, Rinehart SM, Newell MA, Goettler CE, Bard MR, Poulin NR, Toschlog EA. When Birds Can’t Fly: An Analysis of Interfacility Ground Transport using Advanced Life Support when Helicopter Emergency Medical Service is Unavailable. J Trauma Acute Care Surg. 2014; 77(2):331–337 [DOI] [PubMed] [Google Scholar]
- 12.Mann NC, Pinkney KA, Price DD, Rowland D, Arthur M, Hedges JR, Mullins RJ. Injury Mortality Following the Loss of Air Medical Support for Rural Interhospital Transport. Acad Emerg Med. 2002; 9(7):694–698. [DOI] [PubMed] [Google Scholar]
- 13.Arfken CL, Shapiro MJ, Bessey PQ, Littenberg B. Effectiveness of Helicopter versus Ground Ambulance Services for Interfacility Transport. J Trauma 1998; 45(4): 785–790. [DOI] [PubMed] [Google Scholar]
- 14.Boyd CR, Corse KM, Campbell RC. Emergency Interhospital Transport of the Major Trauma Patient: Air versus Ground. J Trauma. 1989; 29(6):789–793. [DOI] [PubMed] [Google Scholar]
- 15.Arfken C, Shapiro MJ, Bessey PQ, Littenberg B. Effectiveness of helicopter versus ground ambulance services for interfacility transport. J Trauma. 1998; 45(4): 785–790. [DOI] [PubMed] [Google Scholar]
- 16.Svenson JE, O’Conner JE, Lindsay MB. Is Air Transport Faster? A Comparison of Air versus Ground Transport Times for Interfacility Transfers in a Regional Referral System. Air Med J. 2005; 24(5):170–172. [DOI] [PubMed] [Google Scholar]
- 17.Stewart K, Garwe T, Bhandari N, Danford B, Albrecht R. Factors Associated with the Use of Helicopter Inter-Facility Transport of Trauma Patients to Tertiary Centers within an Organized Rural Trauma System. Prehosp Emerg Care. 2016; 20(5):601–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nolan B, Haas B, Tien H, Saskin R, Nathens A. Causes of delay during interfacility transports of injured patients transported by air ambulance. Prehosp Emerg Care. 2019; DOI: 10.1080/10903127.2019.1683662. [DOI] [PubMed] [Google Scholar]
- 19.Foster NA, Elfenbein DM, Kelley W, Brown CR, Foley C, Scarborough JE, Vaslef SN, Shapiro ML. Comparison of Helicopter Versus Ground Transport for the Interfacility Transport of Isolated Spinal Injury. The Spine Journal. 2014; 14:1147–1154. [DOI] [PubMed] [Google Scholar]