Abstract
Hypertension is a major cause of cardiovascular disease and related mortality worldwide. The presence of general and abdominal obesity in hypertensive individuals increases the risk of cardiovascular mortality. However, evidence on the burden of obesity and hypertension and associated factors are lacking or limited among young adult students in Bangladesh. This study measured the prevalence and factors associated with general and abdominal obesity and hypertension among university students in Bangladesh. In this study, a total of 1011 students (647 males and 364 females) were enrolled on nine public universities in eight divisional regions of Bangladesh. Data were collected on socio‐demographic, anthropometric, and lifestyle in a questionnaire form. Unadjusted and adjusted logistic regression analyses were performed to evaluate the association of general obesity, abdominal obesity and hypertension with different factors. The prevalence of general obesity, abdominal obesity and hypertension was 8.3%, 20.7%, and 10.2%, respectively. The females had a higher prevalence of general obesity (8.8%) and abdominal obesity (26.3%) compared to the males (8.0% and 17.7%, respectively). However, a higher prevalence of hypertension was observed in males (12.2%) than in the female (6.1%) patients. In regression analysis, age showed a significant association with general obesity, whereas, age and female sex were significantly associated with abdominal obesity. The analysis also identified the male sex and high BMI as the increased risk factors for hypertension. Our study suggests a comprehensive screening program and campaigns to increase awareness about obesity and hypertension and its risk factors among young adults in Bangladesh.
Keywords: abdominal obesity, Bangladesh, general obesity, hypertension, risk factors, students, young adults
1. INTRODUCTION
The prevalence of general obesity is increasing globally both in developing and developed nations. 1 According to the world health organization (WHO), 11% of males and 15% of females aged 18 years and older were obese in 2014. 2 Abdominal obesity, another form of obesity, is considered an important predictor of general obesity‐associated diseases. 3 , 4 Both general and abdominal obesity is linked to metabolic abnormalities including diabetes, hypertension, and cardiovascular diseases. 5 On the other hand, hypertension is a serious public health concern worldwide. Hypertension increases the risk of cardiovascular diseases and related mortality. 6 It has been referred to as a “silent killer” and is responsible for approximately 9.4 million deaths and 7% of the disease burden as estimated in disability‐adjusted life years in 2010. 2 One of the concerning issues is that obesity and hypertension are occurred often together 7 and increased the risk of all‐cause and cardiovascular mortality. 8 , 9 It has been indicated that excess weight gain increases 65%–75% of essential hypertension risk and also increases the risk of renal disease. 10
Bangladesh a developing country in South Asia, is experiencing a rapid socioeconomic and demographic transition. 11 The population of this country is expected to proliferate to 218 million in 2050. 12 This high increasing pattern of the population in the country has been found to be linked with rapid urbanization and an epidemiological changing pattern from communicable to non‐communicable diseases. 12 With the rapid urbanization and industrialization in recent decades, the prevalence of obesity and hypertension has increased remarkably in the Bangladeshi population. Although some early studies reported the prevalence of obesity and hypertension in Bangladeshi adults, 13 , 14 , 15 , 16 , 17 most of the studies were small‐scale and regions specific and investigated either obesity or hypertension prevalence in general adults. Moreover, evidence on the burden of both obesity and hypertension and associated factors are lacking or insufficient, especially among young adults in Bangladesh. Therefore, we aimed to measure the prevalence and related risk factors of general and abdominal obesity and hypertension among public university students of all divisional regions in Bangladesh.
2. METHODOLOGY
2.1. Study areas and participants
We conducted this cross‐sectional study between August 2017 and February 2018 at the Department of Biochemistry and Molecular Biology of Shahjalal University of Science and Technology, Bangladesh. A total of 1011 students (647 males and 364 females from undergraduate and graduate programs, aged 18–28 years) participated from nine public universities in eight divisional regions (i) Barisal division (University of Barisal), (ii) Chittagong division (Chittagong University of Engineering and Technology, Noakhali Science and Technology University), (iii) Dhaka division (University of Dhaka), (iv) Khulna division (Khulna University), (v) Mymensingh division (Bangladesh Agricultural University), (vi) Rajshahi division (University of Rajshahi), (vii) Rangpur division (Begum Rokeya University), and (viii) Sylhet division (Shahjalal University of Science and Technology) of Bangladesh. The participants were selected by random sampling procedure and in a few cases in a convincing way. All participants were informed about the study aims and they provided written informed consent. This study protocol was reviewed and approved by the Internal Ethics Review Committee at the Department of Biochemistry and Molecular Biology, SUST. The inclusion criteria were both sex, age ≥18 years, willingness to participate and free from severe chronic illness. As the exclusion criteria, pregnant women, nursing mothers, and participants who had cardiac disease or malignant disease were not included in the study. The individuals with missing any demographic information were also excluded from the study.
2.2. Data collection
A pre‐structured questionnaire was used for detailed information collection regarding demographic, socio‐economic and lifestyle factors by trained personnel. Anthropometric data like height, weight, waist circumference (WC) and hip circumference (HC), were measured following the standard procedure described elsewhere. 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 Measurements were done without shoes and with minimal clothing. We advised the participants to avoid tea, coffee, beverages, eating, smoking and heavy physical work at least 10 min prior to blood pressure (BP) measurement. The participants were also allowed 5 min rest before measuring BP (two times at 5 min intervals) on the left arm in a comfortable sitting position using a digital BP machine (Omron M10, Tokyo, Japan). At the end of height, weight and BP measurement, we informed all the participants about their body mass index (BMI, weight in kg divided by height in meter squared) and BP status with some health messages (information on risk factors of obesity and hypertension) in Bengali, the local language.
2.3. Definitions
BMI (kg/m2) values were divided as underweight (BMI < 18.5), normal (BMI 18.5–23.5), overweight (BMI 23.5–27.5) and obese (BMI > 27.5) according to the WHO guidelines for the Asian population. 26 , 27 Abdominal obesity was defined as a WC ≥ 80 cm for females and ≥ 90 cm for males. 26 , 28 Hypertension was defined by systolic blood pressure (SBP)≥140 mm Hg and/or, diastolic blood pressure (DBP)≥90 mm Hg and/or, intake of anti‐hypertensive drugs at the time of data collection. 29 , 30 , 31 Family socioeconomic status was grouped as low, medium and high based on their monthly income. Physical activity was categorized as low (easy housework), medium (swimming and walking) and adequate/high (jogging, carrying, lifting, and/or sports). Smoking habits were classified as a present smoker and never smoker.
2.4. Statistical analysis
The results are presented as mean ± standard deviation (SD) for the continuous variables and percentages for the categorical variables. A chi‐square test was applied to assess the proportional differences in obesity and hypertension status in the categorical variables. Differences in the socio‐demographic and anthropometric variables were analyzed by independent sample t‐test and one‐way ANOVA. Bivariate and multivariable logistic regression models were used to identify the significant risk factors for obesity and hypertension. In the multivariable regression analysis, we have adjusted for the covariates age, sex, place of living region, BMI, education, Socioeconomic status, physical activity, family history of obesity and hypertension, intake of fat‐rich food, and smoking. All statistical analyzes were conducted using the IBM SPSS Statistics version 23. A P‐value < 0.05 was considered as the level of significance.
3. RESULTS
3.1. Characteristics of the participants
The socio‐demographic information of the participants by region are summarized in Table 1. Our study comprised 1011 patients, 647(63.9%) males and 364(36.1%) females, aged 18–28 years. The mean age, BMI and WC of the participants were 22.2 ± 2.3 years, 22.6 ± 3.7 kg/m2, and 78.8 ± 9.9 cm, respectively. The mean SBP and DBP were 119.3 ± 12.3 mm Hg and 75.0 ± 9.9 mm Hg, respectively. Regarding family socioeconomic status, 7.1%, 78.4% and 14.5 of the participants were in the low, medium and high category groups, respectively. About 37% of the students were not aware of obesity and hypertension. Regarding physical activity, only 2.1% of students were in the adequate or recommended physical activity group. Our data also showed that about 46% of the participants were used to intake of fat‐rich diet and 16.1% were used to smoking.
TABLE 1.
Descriptive characteristics for socio‐demographic and anthropometric data for the participants by regions
| Measure | Total | Barisal | Chittagong | Dhaka | Khulna | Mymensingh | Rajshahi | Rangpur | Sylhet |
|---|---|---|---|---|---|---|---|---|---|
| N | 1011 | 85 | 106 | 97 | 85 | 115 | 109 | 93 | 321 |
| Sex (m/f) | 647/364 | 48/37 | 78/28 | 53/44 | 47/38 | 85/30 | 47/62 | 72/21 | 217/104 |
| Age (years) | 22.2 ± 2.3 | 21.8 ± 1.6 | 21.4 ± 2.2 | 23.1 ± 2.6 | 23.1 ± 1.8 | 21.3 ± 3.5 | 22.1 ± 1.7 | 21.1 ± 1.8 | 22.7 ± 1.6 |
| BMI (kg/m2) | 22.6 ± 3.7 | 22.7 ± 3.7 | 23.0 ± 3.9 | 23.4 ± 2.8 | 22.3 ± 4.2 | 22.2 ± 2.9 | 21.4 ± 2.7 | 21.6 ± 3.0 | 23.4 ± 4.1 |
| WC (cm) | 78.8 ± 9.9 | 74.6 ± 8.8 | 81.7 ± 11.8 | 78.9 ± 7.6 | 77.5 ± 9.9 | 77.3 ± 8.3 | 72.6 ± 9.6 | 78.7 ± 7.7 | 81.1 ± 9.8 |
| HC (cm) | 87.7 ± 17.6 | 80.8 ± 10.9 | 90.9 ± 14.7 | 88.6 ± 6.0 | 92.7 ± 8.7 | 81.5 ± 24.5 | 85.4 ± 14.4 | 69.7 ± 37.1 | 93.1 ± 8.7 |
| WHR | 0.86 ± 0.30 | 0.92 ± 0.5 | 0.87 ± 0.1 | 0.89 ± 0.1 | 0.83 ± 0.1 | 0.81 ± 0.2 | 0.83 ± 0.1 | 0.72 ± 0.4 | 0.89 ± 0.4 |
| SBP (mmHg) | 119.3 ± 12.3 | 117.5 ± 11.0 | 120.2 ± 11.2 | 117.4 ± 11.6 | 119.2 ± 14.1 | 122.8 ± 10.8 | 118.0 ± 10.2 | 131.4 ± 13.1 | 116.8 ± 11.8 |
| DBP (mmHg) | 75.0 ± 9.9 | 75.5 ± 7.3 | 75.0 ± 10.9 | 74.7 ± 8.1 | 73.4 ± 13.4 | 76.9 ± 9.8 | 76.3 ± 8.1 | 84.6 ± 9.7 | 72.4 ± 8.8 |
| PP (mmHg) | 75.5 ± 20.9 | 71.0 ± 15.4 | 71.2 ± 14.5 | 76.7 ± 12.4 | 82.6 ± 11.8 | 77.3 ± 14.1 | 80.9 ± 14.0 | 88.1 ± 15.4 | 78.6 ± 12.4 |
| Family Socioecono. status | |||||||||
| Low (%) | 7.1 | 12.5 | 1.3 | 7.5 | 8.3 | 3.3 | 5.6 | 33.3 | 3.5 |
| Medium (%) | 78.4 | 79.2 | 82.9 | 67.2 | 64.6 | 88 | 86.1 | 50.8 | 82.2 |
| High (%) | 14.5 | 8.3 | 15.8 | 25.4 | 27.1 | 8.7 | 8.3 | 15.9 | 13.8 |
| Family hist. of hypertension | |||||||||
| Yes (%) | 42.9 | 64.0 | 27.6 | 39.4 | 34.0 | 21.5 | 36.4 | 44.0 | 56.0 |
| No (%) | 57.1 | 36.0 | 72.4 | 60.6 | 66.0 | 78.5 | 63.6 | 56.0 | 44.0 |
| Physical activity | |||||||||
| Low (%) | 50.9 | 97.2 | 98.3 | 97.6 | 98.1 | 98.8 | 40.3 | 21.1 | 13.1 |
| Moderate (%) | 42.9 | 2.8 | 1.7 | 3.2 | 1.9 | 1.2 | 59.7 | 63.2 | 84.0 |
| Adequate (%) | 2.1 | 0 | 0 | 0 | 0 | 0 | 0 | 15.8 | 2.9 |
| Aware about hypertension | |||||||||
| Yes (%) | 62.7 | 75.9 | 68.9 | 69.0 | 59.5 | 65.1 | 60.9 | 68.3 | 57.7 |
| No (%) | 37.3 | 24.1 | 31.1 | 31.0 | 40.5 | 34.9 | 39.1 | 31.7 | 42.3 |
| Aware about obesity | |||||||||
| Yes (%) | 62.9 | 80.6 | 63.3 | 70.7 | 56.1 | 69.5 | 59.8 | 61.9 | 59.1 |
| No (%) | 37.1 | 19.4 | 36.7 | 29.3 | 43.9 | 30.5 | 40.2 | 38.1 | 40.9 |
| Sleeping duration (h/day) | |||||||||
| ≤6 (%) | 19.4 | 15.7 | 11.8 | 26.9 | 38.0 | 16.1 | 14.6 | 20.8 | 19.5 |
| 7–8 (%) | 73.7 | 82.4 | 82.9 | 68.7 | 54.0 | 82.8 | 76.4 | 75.0 | 70.5 |
| >8 (%) | 6.9 | 2.0 | 5.3 | 4.5 | 8.0 | 1.1 | 9.0 | 4.2 | 10.1 |
| Intake of fat rich food | |||||||||
| Yes (%) | 45.8 | 53.1 | 34.7 | 46.8 | 46.9 | 51.2 | 61.5 | 57.6 | 39.8 |
| No (%) | 11.9 | 8.2 | 13.3 | 14.5 | 18.4 | 15.1 | 9.2 | 15.3 | 9.5 |
| Occasionally (%) | 42.3 | 38.8 | 52.0 | 38.7 | 34.7 | 33.7 | 29.2 | 27.1 | 50.7 |
| Intake of soft drinks | |||||||||
| Daily (%) | 18.8 | 31.7 | 13.6 | 21.1 | 19.7 | 25.0 | 20.3 | 14.8 | 16.1 |
| Weekly (%) | 36.6 | 17.1 | 28.8 | 38.6 | 27.8 | 34.2 | 45.6 | 37.0 | 39.8 |
| Monthly/rarely (%) | 44.6 | 52.2 | 57.6 | 40.4 | 52.8 | 40.8 | 34.2 | 48.1 | 44.1 |
| Smoking status | |||||||||
| Yes (%) | 16.1 | 6.1 | 11.8 | 25.8 | 14.0 | 9.7 | 19.3 | 12.0 | 15.4 |
| No (%) | 83.9 | 93.9 | 88.2 | 74.2 | 86.0 | 90.3 | 80.7 | 88.0 | 84.6 |
Data are presented as mean ± SD for the continuous variables and percentages for the categorical variables.
3.2. Body mass index and waist circumference data
The characteristics of the participants by BMI and WC are shown in Table 2 and Figure 1. Overall, the prevalence of general and abdominal obesity was 8.3% and 20.7%, respectively. About 12% of the participants were underweight, and 26% were overweight. No significant difference was found for general obesity prevalence between male (8.0%) and female (8.8%) participants. However, females had a higher prevalence of being underweight (14.1%) compared to males (10.6%). In WC‐based data analysis, a significant difference (P < 0.01) was observed in abdominal obesity between male (17.7%) and female (26.3%) patients. A high prevalence of general obesity (13.7%) and abdominal obesity (37.3%) was found among patients recruited from Barisal and Chittagong regions, respectively. The lowest prevalence of general obesity (1.5%) and abdominal obesity (3.9%) was observed among participants in Dhaka and Barisal regions, respectively.
TABLE 2.
Characteristics of the study patients according to BMI, WC, and blood pressure data
| Body mass index | Waist circumference | Blood pressure | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Divisions | Sex | Underweight (%) | Normal (%) | Overweight (%) | Obesity (%) | Normal (%) | Obesity (%) | Normal (%) | Pre‐hypertensive (%) | Hypertensive (%) |
| Barisal | Male | 3.4 | 55.2 | 27.6 | 13.8 | 93.1 | 6.3 | 31.0 | 69.0 | 0.0 |
| Female | 22.7 | 54.5 | 9.1 | 13.6 | 100 | 0.0 | 68.2 | 27.3 | 4.5 | |
| Total | 11.8 | 54.9 | 19.6 | 13.7 | 96.1 | 3.9 | 47.1 | 26 (51) | 1.9 | |
| Chittagong | Male | 8.9 | 46.4 | 30.4 | 14.3 | 60.7 | 39.3 | 33.9 | 46.4 | 19.6 |
| Female | 15.0 | 40.0 | 45.0 | 0.0 | 65.0 | 35.0 | 65.0 | 35.0 | 0.0 | |
| Total | 10.5 | 44.7 | 34.2 | 10.5 | 62.7 | 37.3 | 42.1 | 43.4 | 14.5 | |
| Dhaka | Male | 32.4 | 48.6 | 16.2 | 2.7 | 89.2 | 10.8 | 29.7 | 67.6 | 2.7 |
| Female | 0.0 | 80.0 | 20.0 | 0.0 | 53.3 | 46.7 | 86.7 | 13.3 | 0.0 | |
| Total | 17.9 | 62.7 | 17.9 | 1.5 | 73.1 | 26.9 | 55.2 | 43.3 | 1.5 | |
| Khulna | Male | 6.9 | 58.6 | 34.5 | 0.0 | 79.3 | 20.7 | 37.9 | 62.1 | 0.0 |
| Female | 18.2 | 50.0 | 18.2 | 13.6 | 81.8 | 18.2 | 72.7 | 22.7 | 4.5 | |
| Total | 11.8 | 54.9 | 27.5 | 5.9 | 80.4 | 19.6 | 52.9 | 45.1 | 2.0 | |
| Mymensingh | Male | 11.6 | 62.3 | 20.3 | 5.8 | 92.8 | 7.2 | 37.3 | 46.4 | 15.9 |
| Female | 0.0 | 62.5 | 37.5 | 0.0 | 70.6 | 29.4 | 58.3 | 25.0 | 16.7 | |
| Total | 8.6 | 62.4 | 24.7 | 4.3 | 88.4 | 11.6 | 43.0 | 40.9 | 16.1 | |
| Rajshahi | Male | 5.3 | 68.4 | 23.7 | 2.6 | 91.7 | 8.3 | 47.4 | 42.1 | 10.5 |
| Female | 23.5 | 58.8 | 13.7 | 3.9 | 94.1 | 5.9 | 62.7 | 23.5 | 13.7 | |
| Total | 15.7 | 62.9 | 18.0 | 3.4 | 93.1 | 6.9 | 56.2 | 31.4 | 12.4 | |
| Rangpur | Male | 17.3 | 57.7 | 19.2 | 5.8 | 92.7 | 7.3 | 27.5 | 48.5 | 25.0 |
| Female | 36.4 | 54.5 | 0.0 | 9.1 | 88.9 | 11.1 | 49.0 | 23.7 | 27.3 | |
| Total | 20.6 | 57.1 | 15.9 | 6.3 | 92.0 | 8.0 | 34.8 | 41.4 | 23.8 | |
| Sylhet | Male | 7.8 | 46.1 | 36.4 | 9.7 | 78.8 | 21.2 | 49.3 | 40.6 | 10.1 |
| Female | 11.5 | 48.1 | 25.0 | 15.4 | 62.5 | 37.5 | 88.5 | 11.5 | 0.0 | |
| Total | 9.0 | 46.7 | 32.7 | 11.5 | 73.5 | 26.5 | 62.0 | 31.1 | 6.9 | |
| Overall | Male | 10.6 | 52.4 | 29.0 | 8.0 | 82.3 | 17.7 | 39.9 | 47.8 | 12.2 |
| Female | 14.1 | 55.6 | 21.5 | 8.8 | 73.7 | 26.3 | 74.6 | 19.2 | 6.1 | |
| Total | 11.8 | 53.5 | 26.4 | 8.3 | 79.3 | 20.7 | 51.9 | 37.8 | 10.2 | |
Data are presented as percentages for the categorical variables. BMI (kg/m2) was categorized as underweight (BMI < 18.5), normal (BMI 18.5–23.5), overweight (BMI 23.5–27.5) and obese (BMI > 27.5). 26 , 27 Abdominal obesity was defined as a WC ≥ 80 cm for females and ≥ 90 cm for males. 26 , 28 Hypertension was defined by as SBP≥140 mm Hg and/or, DBP≥90 mm Hg and/or, intake of an anti‐hypertensive drugs. 30 , 31
FIGURE 1.
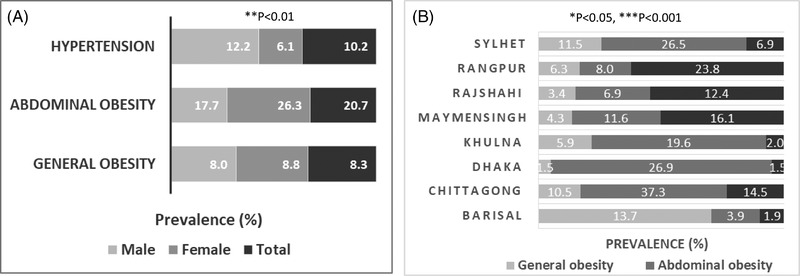
Prevalence of general obesity, abdominal obesity and hypertension among Bangladeshi young adults by sex (A) and region (B). *P < 0.05 when the prevalence of general obesity is compared within regions, **P < 0.01 when the prevalence of abdominal obesity and hypertension is compared between sex groups, and ***P < 0.001 when the prevalence of abdominal obesity and hypertension is compared within regions. P‐values were obtained from the chi‐square test
3.3. Blood pressure data
Table 2 and Figure 1 show the category of blood pressure data for all participants by sex and region. The overall prevalence of prehypertension and hypertension was 37.8% and 10.2%, respectively. Males were more prehypertensive and hypertensive (47.8% and 12.2%, respectively) than females (19.2% and 6.1%, respectively) (P < 0.01). A variation was observed in obesity and hypertension prevalence within the regions. The lowest prevalence of hypertension was observed in the Dhaka region (1.5%) and the highest prevalence was found in Rangpur (23.8%) region. Both prehypertension and hypertension rates were significantly higher (53.7% and 19.7%, respectively) in BMI based obesity group compared to the normal and overweight group (P < 0.05) (Figure 2). Similarly, both prehypertension and hypertension prevalence was significantly higher (38% and 15.3%, respectively) in WC based abdominal obesity group (Figure 2) compared to the normal group (P < 0.05).
FIGURE 2.
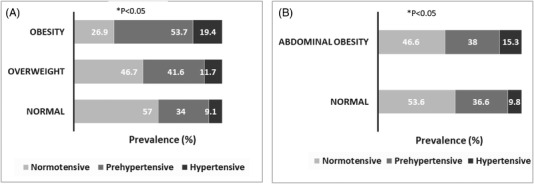
Prevalence of prehypertension and hypertension in the BMI (A) and WC (B) groups *P < 0.05 when prehypertension and hypertension prevalence is compared within the BMI and WC groups
3.4. Logistic regression analysis to assess the risk factors
In multivariable logistic regression analysis, increased age was found to be an independent risk factor for general obesity (Table 3). Whereas, increased age and female sex were the significant risk factors for abdominal obesity (Table 4). Moreover, the patients with medium family socioeconomic status had a higher odds of having abdominal obesity than the patients with lower family socioeconomic status. Male sex and high BMI also showed an association with the risk of hypertension among participants (Table 5).
TABLE 3.
Evaluation of the factors associated with general obesity by bivariate and multivariable logistic regression analysis
| Variables | COR (95% Cl) | P‐value | AOR (95% Cl) | P‐value |
|---|---|---|---|---|
| Sex | ||||
| Male | Ref. | Ref. | ||
| Female | 1.12 (0.66–1.87 | 0.861 | 0.76 (0.42–1.38) | 0.361 |
| Age (years) | ||||
| 18–21 | Ref | Ref | ||
| 22–24 | 3.83 (1.83–8.00) | 0.000 | 2.48 (1.13–5.46) | 0.024 |
| 25–28 | 5.23 (2.23–12.16) | 0.000 | 2.93 (1.16–7.42) | 0.023 |
| WC (cm) | ||||
| Normal | Ref. | Ref. | ||
| Obese | 19.31 (10.33–36.10) | 0.000 | 17.36 (9.18–32.86) | 0.000 |
| Family socioeconomic status | ||||
| Low | Ref. | Ref. | ||
| Medium | 1.50 (0.45–4.98) | 0.507 | 2.01 (0.43–9.39) | 0.376 |
| High | 2.04 (0.55–7.55) | 0.286 | 1.46 (0.28–7.63) | 0.652 |
| Physical activity | ||||
| Adequate/Moderate | Ref. | Ref. | ||
| Low | 0.63 (0.36–1.12) | 0.113 | 0.66 (0.33–1.32) | 0.243 |
| Aware about obesity | ||||
| Yes | Ref. | Ref. | ||
| No | 0.63 (0.35–1.13) | 0.121 | 0.53 (0.27–1.03) | 0.062 |
| Division | ||||
| Dhaka | Ref | Ref | ||
| Barisal | 10.50 (1.25–88.33) | 0.030 | 65.23 (6.63–642‐04) | 0.000 |
| Chittagong | 7.76 (0.94–63.81) | 0.056 | 6.56 (0.73–58.65) | 0.093 |
| Khulna | 4.12 (0.42–40.88) | 0.226 | 4.92 (0.45–54.23) | 0.193 |
| Mymensingh | 2.97 (0.32–27.16) | 0.336 | 7.50 (0.73–76.61) | 0.089 |
| Rajshahi | 2.30 (0.23–22.64) | 0.475 | 2.34 (0.13–41.95) | 0.564 |
| Rangpur | 4.47 (0.49–41.17) | 0.186 | 8.84 (0.66–119.05) | 0.101 |
| Sylhet | 8.60 (1.16–63.81) | 0.035 | 9.93 (1.26–78.32) | 0.029 |
| Intake of fat rich food | ||||
| No | Ref. | Ref. | ||
| Occasionally | 1.22 (0.52–2.89) | 0.644 | 1.70 (0.62–4.68) | 0.301 |
| Yes | 0.92 (0.39–2.20) | 0.853 | 1.17 (0.42–3.26) | 0.765 |
| Intake of soft drinks | ||||
| No | Ref. | Ref. | ||
| Occasionally | 0.55 (0.23–1.29) | 0.168 | 0.44 (0.16–1.19) | 0.106 |
| Yes | 0.92 (0.51–1.64) | 0.776 | 0.73 (0.37–1.43) | 0.354 |
Abbreviations: COR, Crude odds ratio; AOR, Adjusted odds ratio; CI, Confidence Interval.
TABLE 4.
Evaluation of the factors associated with abdominal obesity by bivariate and multivariable logistic regression analysis
| Variables | COR (95% Cl) | P‐value | AOR (95% Cl) | P‐value |
|---|---|---|---|---|
| Sex | ||||
| Male | Ref. | Ref. | ||
| Female | 1.66 (1.17–2.36) | 0.005 | 2.71 (1.69–4.34) | 0.000 |
| Age (years) | ||||
| 18–21 | Ref. | Ref. | ||
| 22–24 | 2.25 (1.48–3.42) | 0.000 | 1.84 (1.12–3.03) | 0.017 |
| 25–28 | 2.85 (1.67–4.87) | 0.000 | 2.32 (1.19–4.53) | 0.013 |
| BMI (kg/m2) | ||||
| Normal | Ref. | Ref. | ||
| Overweight | 12.77 (7.93–20.54) | 0.000 | 16.03 (9.65–26.63) | 0.000 |
| Obese | 64.68 (31.86–131.31) | 0.000 | 68.28 (32.45–143.67) | 0.000 |
| Family socioeconomic status | ||||
| High | Ref. | Ref. | ||
| Medium | 0.42 (0.27–0.65) | 0.000 | 0.46 (0.26–0.81) | 0.007 |
| Low | 0.42 (0.19–0.96) | 0.039 | 1.18 (0.41–3.40) | 0.750 |
| Physical activity | ||||
| Adequate/moderate | Ref. | Ref. | ||
| Low | 0.83 (0.55–1.23) | 0.345 | 1.31 (0.76–2.26) | 0.325 |
| Division | ||||
| Barisal | Ref. | Ref. | ||
| Chittagong | 14.60 (3.29–64.72) | 0.000 | 57.98 (9.67–347.57) | 0.000 |
| Dhaka | 9.00 (1.98–40.89) | 0.004 | 75.47 (12.12–469.87) | 0.000 |
| Khulna | 5.98 (1.24–28.83) | 0.026 | 16.41 (2.44–110.20) | 0.004 |
| Mymensingh | 3.22 (0.68–15.34) | 0.141 | 12.81 (2.02–81.37) | 0.007 |
| Rajshahi | 1.81 (0.35–9.35) | 0.476 | 5.76 (0.80–41.28) | 0.082 |
| Rangpur | 2.13 (0.37–12.19) | 0.395 | 12.26 (1.55–97.13) | 0.018 |
| Sylhet | 8.82 (2.10–37.08) | 0.003 | 20.93 (3.86–113.48) | 0.000 |
| Intake of fat rich food | ||||
| No | Ref. | Ref. | ||
| Occasionally | 0.83 (0.47–1.47) | 0.519 | 0.65 (0.31–1.33) | 0.233 |
| Yes | 0.86 (0.49–1.52) | 0.609 | 0.86 (0.42–1.75) | 0.673 |
| Intake of soft drinks | ||||
| No | Ref. | Ref. | ||
| Occasionally | 0.87 (0.51–1.49) | 1.09 (0.56–2.11) | 0.798 | |
| Yes | 1.07 (0.71–1.62) | 1.21 (0.72–2.01) | 0.477 |
Abbreviations: COR, Crude odds ratio; AOR, Adjusted odds ratio; CI, Confidence Interval.
TABLE 5.
Evaluation of the factors associated with hypertension by bivariate and multivariable logistic regression analysis
| Variables | COR (95% Cl) | P‐value | AOR (95% Cl) | P‐value |
|---|---|---|---|---|
| Sex | ||||
| Female | Ref. | Ref. | ||
| Male | 2.19 (1.27–3.76) | 0.005 | 2.10 (1.22–3.63) | 0.008 |
| Age (years) | ||||
| 18–21 | Ref. | Ref. | ||
| 22–24 | 0.77 (0.48–1.24) | 0.285 | 0.73 (0.45–1.19) | 0.205 |
| 25–28 | 0.58 (0.27–1.25) | 0.166 | 0.52 (0.24–1.14) | 0.104 |
| BMI (kg/m2) | ||||
| Normal | Ref. | Ref. | ||
| Overweight | 1.33 (0.80–2.22) | 0.277 | 1.27 (0.76–2.13) | 0.369 |
| Obese | 2.42 (1.23–4.74) | 0.010 | 2.80 (1.39–5.65) | 0.004 |
| Family socioeconomic status | ||||
| Low | Ref. | Ref. | ||
| Medium | 0.64 (0.29–1.41) | 0.263 | 0.67 (0.30–1.51) | 0.339 |
| High | 0.89 (0.35–2.25) | 0.805 | 1.08 (0.41–2.81) | 0.878 |
| Physical activity | ||||
| Adequate/moderate | Ref. | Ref | ||
| Low | 0.85 (0.51–1.42) | 0.531 | 0.66 (0.38–1.15) | 0.143 |
| Family history of hypertension | ||||
| No | Ref. | Ref. | ||
| Yes | 1.14 (0.71–1.81) | 0.589 | 1.13 (0.70–1.81) | 0.618 |
| Aware about hypertension | ||||
| Yes | Ref. | Ref. | ||
| No | 0.79 (0.48–1.30) | 0.350 | 0.79 (0.48–1.32) | 0.373 |
| Division | ||||
| Barisal | Ref. | Ref. | ||
| Chittagong | 8.46 (1.06–67.73) | 0.044 | 8.10 (1.00–65.88) | 0.050 |
| Dhaka | 0.76 (0.05–12.41) | 0.846 | 1.03 (0.06–17.33) | 0.984 |
| Khulna | 1.00 (0.06–16.43) | 1.000 | 1.15 (0.07–19.19) | 0.922 |
| Mymensingh | 9.62 (1.23–75.08) | 0.031 | 10.98 (1.37–87.75) | 0.024 |
| Rajshahi | 7.05 (0.88–56.31) | 0.065 | 10.06 (1.23–82.12) | 0.031 |
| Rangpur | 16.77 (2.99–117.52) | 0.001 | 19.24 (3.34–140) | 0.001 |
| Sylhet | 3.68 (0.48–27.91) | 0.208 | 3.48 (0.45–26.74) | 0.230 |
| Intake of fat rich food | ||||
| No | Ref. | Ref. | ||
| Occasionally | 1.10 (0.68–1.78) | 0.703 | 1.02 (0.48–2.18) | 0.957 |
| Yes | 1.05 (0.50–2.23) | 0.891 | 1.20 (5.57–2.52) | 0.641 |
| Intake of soft drinks | ||||
| Monthly/rarely | Ref. | Ref. | ||
| Weekly | 1.09 (0.57–2.09) | 0.794 | 1.25 (0.64–2.42) | 0.511 |
| Daily | 0.80 (0.45–1.40) | 0.430 | 082 (0.46–1.46) | 0.500 |
| Smoking | ||||
| No | Ref. | Ref. | ||
| Yes | 1.19 (0.65–2.20) | 0.576 | 1.23 (0.66–2.31) | 0.511 |
Abbreviations: COR, Crude odds ratio; AOR, Adjusted odds ratio; CI, Confidence Interval.
4. DISCUSSION
The prevalence rate of obesity and hypertension in different age groups has been investigated widely in many developed countries, while similar data are limited in Bangladesh, especially for young adults. To our knowledge, this study is the first that reports on the prevalence of general and abdominal obesity and hypertension and associated risk factors among university students from all divisional regions of Bangladesh.
In this cross‐sectional study, the overall prevalence of general obesity, abdominal obesity and hypertension was 18.2%, 41.9%, and 25.5%, respectively. A previous study conducted in the Dhaka region, reported a lower prevalence of general obesity (2%) among university students with a higher rate of prevalence in females than males (0.8% vs. 3.2%). 32 A higher prevalence of combined overweight and obesity was found in males (14.8%) than in the female students (11.8%) selected from three public universities in Bangladesh. 33 In our study, the prevalence rate of general obesity was slightly higher in females but the difference was not significant between the sex, however, the prevalence of abdominal obesity was significantly higher in females than in males. An increased rate of general and abdominal obesity in females was also found in studies conducted in India 34 and China. 35
This higher prevalence of obesity in females may be caused by an imbalance of excessive caloric intake and inadequate activity. In Bangladesh, females are generally used to less physical activity which may influence excess weight gain. In risk factors analysis, age was a significant determinant of general obesity, whereas, female sex, age and medium family socioeconomic status were significant determinants of abdominal obesity. A previous study also found the female sex, increased age and less physical activity as significant risk factors of obesity in the South Asian population. 36
In the present study, males had a 2‐fold higher hypertension prevalence than females (12.2% vs. 6.1%). A higher level of hypertension prevalence has also been found among university male students (9.2% vs. 2%) in a previous study conducted in the Dhaka region. 32 Another study reported a similar finding for hypertension prevalence among medical students (12.1% vs. 3.4%), in the Dhaka region of Bangladesh. 13 In Saudi Arabia, a higher prevalence of hypertension was also found among male (18.5%) students than in female (5.3%) students. 37 The mechanism underlying this sex difference remains unclear; however, there is reliable evidence about the role of androgens in the regulation of blood pressure differences between the sex groups. 38 Furthermore, during the premenopausal stage in females, estrogen production with higher nitric oxide and vasodilation may also act as a protection against hypertension development. 39 In a study in neighboring country, India, about 13.8% of undergraduate medical students were found to be hypertensive where increased age, sex, high BMI and some dietary habits were identified as important predictors of hypertension among the participants. 40 In our study, male sex and high BMI showed a significant association with hypertension. Smoking, intake of fatty food and physical activity did not show a significant association with hypertension in our study, which might be a reason that the participants were at a younger age, do some physical work and a major portion of them were nonsmokers.
We observed a wide variation in the prevalence of obesity and hypertension among study patients. The highest risk of general obesity, abdominal obesity and hypertension was observed among students selected from Barisal division (south‐central part), Dhaka division (central part), and Rangpur division (northwestern part), respectively, whereas the lowest risk was found in Rajshahi (west‐central part; both general and abdominal obesity), and in Dhaka region, respectively. These prevalence differences might be influenced by dietary food habits and malnutrition. Overall, the variation in results between the studies may be related to differences in sampling time points, dietary habits, region‐specific studies, and socioeconomic and demographic transition in the last few decades.
Both obesity and hypertension are global health problems and there is a linear relationship between them. In our survey, we found a higher percentage of hypertension in both BMI and WC‐based obesity groups compared to the normal group. Although the prevalence of general and abdominal obesity in our study is moderate, this prevalence rate could also contribute to the development of hypertension in their later life and increase the risk of cardiovascular mortality. Therefore, in order to control hypertension in this important group of the national population, it is necessary to check blood pressure regularly in patients, especially those who have high BMI and WC. The pathophysiology of obesity‐related hypertension is not clear yet, however, several factors may be associated such as leptin, elevated aldosterone, insulin resistance, inappropriate activation of the renin‐angiotensin‐aldosterone system and sympathetic nervous system and renal compression. 41 , 42 , 43 , 44 In addition to obesity and hypertension, we also found a high prevalence of overweight (26.4%) and prehypertension (37.8%) in our study patients which may influence the future development of obesity and hypertension. Therefore, to maintain a healthy life, the students should maintain their normal body weight and blood pressure, do regular exercise and reduce excess fatty and sugar‐containing food from their daily diet menu.
The major strength of this study was that we collected data on both sexes from the public university of each of the eight divisional regions in Bangladesh. Furthermore, we included information on most of the demographic and anthropometric factors that may be related to obesity and hypertension. However, our study had also some limitations. First, the study was a cross‐sectional design and the individual's BMI, WC and blood pressure data recorded in the survey were from one‐day measurement only, therefore a longitudinal study might be more effective to identify all the factors associated with obesity and hypertension in young adults in Bangladesh. Second, we could not collect data on detailed food habits and lipid levels that may also influence the development of obesity and hypertension.
5. CONCLUSIONS
This study indicates a moderate prevalence of general and abdominal obesity and hypertension among young adults in Bangladesh. We found that about 1 in 5 subjects we abdominally obese and 1 in 10 subjects were general obese and hypertensive. In our analysis, several factors were identified as risk factors for obesity and hypertension. Increased age showed a significant association with general obesity; whereas increased age, female sex and medium family socioeconomic status showed a significant association with abdominal obesity. On the other hand, male sex and high BMI were significant predictors of hypertension. Even though the prevalence of obesity and hypertension in our study patients is moderate, for the related disease‐free future life, a comprehensive national screening program and campaigns are required to increase awareness about obesity and hypertension and its risk factors in this significant group of the population of the nation.
CONFLICTS OF INTEREST
All authors declare no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Study conception and design and drafting of manuscript: Nurshad Ali. Data collection, analysis and interpretation: Firoz Mahmud, Syeda Ayshia Akter, Shiful Islam, Abu Hasan Sumon, Dhirendra Nath Barman and Farjana Islam. Revision of the manuscript: Nurshad Ali and Farjana Islam. Final approval of the manuscript: All authors.
ACKNOWLEDGMENTS
The authors would like to thank all volunteers for their active participation in the study. This study did not receive any external funding. It was conducted with small support internally.
Ali N, Mahmud F, Akter SA, et al. The prevalence of general obesity, abdominal obesity, and hypertension and its related risk factors among young adult students in Bangladesh. J Clin Hypertens. 2022;24:1339–1349. 10.1111/jch.14560
REFERENCES
- 1. Abarca‐Gómez L, Abdeen ZA, Hamid ZA, et al. Worldwide trends in body‐mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population‐based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627‐2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO . Global Status Report on Noncommunicable Diseases 2014. World Health Organization; 2014. [Google Scholar]
- 3. Bigaard J, Frederiksen K, Tjønneland A, et al. Waist circumference and body composition in relation to all‐cause mortality in middle‐aged men and women. Int J Obes. 2005;29(7):778‐784. [DOI] [PubMed] [Google Scholar]
- 4. Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity‐related health risk. Am J Clin Nutr. 2004;79(3):379‐384. [DOI] [PubMed] [Google Scholar]
- 5. Casanueva FF, Moreno B, Rodríguez‐Azeredo R, et al. Relationship of abdominal obesity with cardiovascular disease, diabetes and hyperlipidaemia in Spain. Clin Endocrinol (Oxf). 2009;73(1):35‐40. 10.1111/j.1365-2265.2009.03727.x [DOI] [PubMed] [Google Scholar]
- 6. Bonita R, De Courten M, Dwyer T, Jamrozik K, Winkelmann R. Surveillance of risk factors for noncommunicable diseases: the WHO STEPwise approach: summary. Published online 2001.
- 7. Jordan J, Yumuk V, Schlaich M, et al. Joint statement of the European Association for the Study of Obesity and the European Society of Hypertension: obesity and difficult to treat arterial hypertension. J Hypertens. 2012;30(6):1047‐1055. [DOI] [PubMed] [Google Scholar]
- 8. Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body‐mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211‐2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Prospective Studies Collaboration . Body‐mass index and cause‐specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083‐1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wofford MR, Hall JE. Pathophysiology and treatment of obesity hypertension. Curr Pharm Des. 2004;10(29):3621‐3637. [DOI] [PubMed] [Google Scholar]
- 11. Ahsan Karar Z, Alam N, Kim Streatfield P. Epidemiological transition in rural Bangladesh, 1986–2006. Glob Health Action. 2009;2(1):1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Streatfield PK, Karar ZA. Population challenges for Bangladesh in the coming decades. J Health Popul Nutr. 2008;26(3):261‐272. [PMC free article] [PubMed] [Google Scholar]
- 13. Ali N, Mahmood S, Manirujjaman M, et al. Hypertension prevalence and influence of basal metabolic rate on blood pressure among adult students in Bangladesh. BMC Public Health. 2017;18(1):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chowdhury MAB, Uddin M, Haque M, Ibrahimou B. Hypertension among adults in Bangladesh: evidence from a national cross‐sectional survey. BMC Cardiovasc Disord. 2016;16(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Islam S, Rahman S, Haque T, Sumon AH, Ahmed AM, Ali N. Prevalence of elevated liver enzymes and its association with type 2 diabetes: a cross‐sectional study in Bangladeshi adults. Endocrinol Diabetes Metab. 2020;3(2):e00116. 10.1002/edm2.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moni MA, Rahman MA, Haque MA, Islam MS, Ahmed K. Blood pressure in relation to selected anthropometric measurements in senior citizens. Mymensingh Med J. 2010;19(2):254‐258. [PubMed] [Google Scholar]
- 17. Siddiquee T, Bhowmik B, Da Vale Moreira NC, et al. Prevalence of obesity in a rural Asian Indian (Bangladeshi) population and its determinants. BMC Public Health. 2015;15(1):860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ali N, Miah R, Hasan M, et al. Association between serum uric acid and metabolic syndrome: a cross‐sectional study in Bangladeshi adults. Sci Rep. 2020;10(1):7841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ali N, Mahmood S, Islam F, et al. Relationship between serum uric acid and hypertension: a cross‐sectional study in Bangladeshi adults. Sci Rep. 2019;9(1):9061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ali N, Rahman S, Islam S, et al. The relationship between serum uric acid and lipid profile in Bangladeshi adults. BMC Cardiovasc Disord. 2019;19(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ali N, Perveen R, Rahman S, et al. Prevalence of hyperuricemia and the relationship between serum uric acid and obesity: a study on Bangladeshi adults. PLoS ONE. 2018;13(11):e0206850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Haque T, Rahman S, Islam S, Molla NH, Ali N. Assessment of the relationship between serum uric acid and glucose levels in healthy, prediabetic and diabetic individuals. Diabetol Metab Syndr. 2019;11:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kathak RR, Sumon AH, Molla NH, et al. The association between elevated lipid profile and liver enzymes: a study on Bangladeshi adults. Sci Rep. 2022;12(1):1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Molla NH, Kathak RR, Sumon AH, et al. Assessment of the relationship between serum uric acid levels and liver enzymes activity in Bangladeshi adults. Sci Rep. 2021;11(1):20114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Saadi MM, Roy MN, Haque R, Tania FA, Mahmood S, Ali N. Association of microalbuminuria with metabolic syndrome: a cross‐sectional study in Bangladesh. BMC Endocr Disord. 2020;20(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ali N, Sumon AH, Fariha KA, et al. Assessment of the relationship of serum liver enzymes activity with general and abdominal obesity in an urban Bangladeshi population. Sci Rep. 2021;11(1):6640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. WHO . Appropriate body‐mass index for Asian populations and its implications for policy and intervention strategies. Lancet Lond Engl. 2004;363(9403):157‐163. [DOI] [PubMed] [Google Scholar]
- 28. WHO . International association for the study of obesity, International Obesity Taskforce. Asia‐Pac Perspect Redefining Obes Its Treat. 2000:15‐21. [Google Scholar]
- 29. Mou AD, Barman Z, Hasan M, et al. Prevalence of preeclampsia and the associated risk factors among pregnant women in Bangladesh. Sci Rep. 2021;11(1):21339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206‐1252. [DOI] [PubMed] [Google Scholar]
- 31. Rahman S, Islam S, Haque T, Kathak RR, Ali N. Association between serum liver enzymes and hypertension: a cross‐sectional study in Bangladeshi adults. BMC Cardiovasc Disord. 2020;20(1):128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Paul S, Solayman BP, Saha M, Hossain S. Obesity and hypertension in students of Jahangirnagar University: alarming issues. Int J Public Health Sci. 2015;4(3):164‐171. [Google Scholar]
- 33. Zamsad M, Banik S, Ghosh L. Prevalence of overweight, obesity and abdominal obesity in Bangladeshi university students: a cross‐sectional study. Diabetes Metab Syndr Clin Res Rev. 2019;13(1):480‐483. [DOI] [PubMed] [Google Scholar]
- 34. Kaur P, Rao SR, Radhakrishnan E, Rajasekar D, Gupte MD. Prevalence, awareness, treatment, control and risk factors for hypertension in a rural population in South India. Int J Public Health. 2012;57(1):87‐94. [DOI] [PubMed] [Google Scholar]
- 35. Zhang X, Sun Z, Zhang X, et al. Prevalence and associated factors of overweight and obesity in a Chinese rural population. Obesity. 2008;16(1):168‐171. [DOI] [PubMed] [Google Scholar]
- 36. Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Hills AP. Prevalence, trends and associated socio‐economic factors of obesity in South Asia. Obes Facts. 2013;6(5):405‐414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. AlWabel AH, Almufadhi MA, Alayed FM, Aloraini AY, Alobaysi HM, Alalwi RM. Assessment of hypertension and its associated risk factors among medical students in Qassim University. Saudi J Kidney Dis Transplant. 2018;29(5):1100. [DOI] [PubMed] [Google Scholar]
- 38. Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension. 2001;37(5):1199‐1208. [DOI] [PubMed] [Google Scholar]
- 39. Sudhir K, Jennings GL, Funder JW, Komesaroff PA. Estrogen enhances basal nitric oxide release in the forearm vasculature in perimenopausal women. Hypertension. 1996;28(3):330‐334. [DOI] [PubMed] [Google Scholar]
- 40. Chattopadhyay A, Taraphdar P, Kumar Sahu B, et al. A study on prevalence of hypertension and its related risk factors among undergraduate medical students in Kolkata. IOSR J Dent Med Sci. 2014;13(11):1‐7. [Google Scholar]
- 41. Chrysant SG. Pathophysiology and treatment of obesity‐related hypertension. J Clin Hypertens. 2019;21(5):555‐559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. DeMarco VG, Aroor AR, Sowers JR. The pathophysiology of hypertension in patients with obesity. Nat Rev Endocrinol. 2014;10(6):364‐376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Engeli S, Sharma AM. The renin‐angiotensin system and natriuretic peptides in obesity‐associated hypertension. J Mol Med Berl Ger. 2001;79(1):21‐29. [DOI] [PubMed] [Google Scholar]
- 44. Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity‐induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116(6):991‐1006. [DOI] [PMC free article] [PubMed] [Google Scholar]


