Abstract
Objective
To document the recovery of vascular services in Europe following the first COVID-19 pandemic peak.
Methods
An online structured vascular service survey with repeated data entry between 23 March and 9 August 2020 was carried out. Unit level data were collected using repeated questionnaires addressing modifications to vascular services during the first peak (March – May 2020, “period 1”), and then again between May and June (“period 2”) and June and July 2020 (“period 3”). The duration of each period was similar. From 2 June, as reductions in cases began to be reported, centres were first asked if they were in a region still affected by rising cases, or if they had passed the peak of the first wave. These centres were asked additional questions about adaptations made to their standard pathways to permit elective surgery to resume.
Results
The impact of the pandemic continued to be felt well after countries’ first peak was thought to have passed in 2020. Aneurysm screening had not returned to normal in 21.7% of centres. Carotid surgery was still offered on a case by case basis in 33.8% of centres, and only 52.9% of centres had returned to their normal aneurysm threshold for surgery. Half of centres (49.4%) believed their management of lower limb ischaemia continued to be negatively affected by the pandemic. Reduced operating theatre capacity continued in 45.5% of centres. Twenty per cent of responding centres documented a backlog of at least 20 aortic repairs. At least one negative swab and 14 days of isolation were the most common strategies used for permitting safe elective surgery to recommence.
Conclusion
Centres reported a broad return of services approaching pre-pandemic “normal” by July 2020. Many introduced protocols to manage peri-operative COVID-19 risk. Backlogs in cases were reported for all major vascular surgeries.
Keywords: AAA, COVID-19, PAD, Survey, Vascular surgery
Highlights
-
•
By July 2020 a high proportion of centres had not returned to their pre-pandemic aneurysm screening programme or thresholds for surgery.
-
•
At least one negative swab and 14 days of isolation were the most common strategies for permitting elective surgery to recommence on ‘green’ pathways.
-
•
Large backlogs of cases for aortic aneurysm, lower limb, and varicose vein surgery were reported.
-
•
Vascular surgeons will face significant competition with other specialties facing similar backlogs.
Introduction
In recent times, the effect of the COVID-19 pandemic on the availability of healthcare resources has been widely reported.1,2 In the early stages of the pandemic, healthcare professionals documented dwindling resources,3 staff illness and self quarantine, and problems with the availability of personal protective equipment (PPE).4,5 In response, several national vascular societies released guidance for surgeons on what operative case mix should, or should not, be undertaken during the pandemic.6, 7, 8
The Vascular and Endovascular Research Network (VERN; www.vascular-research.net) is an established vascular trainee research collaborative.9, 10, 11 In response to the evolving crisis VERN launched the COVID-19 Vascular SERvice (COVER) study in March 2020. The aim of the first tier of the study (tier 1) was to document fluctuations in global vascular services during and after the first peak of the pandemic.
From early May 2020, many European countries had begun to ease various aspects of national lockdowns, devolving responsibility for implementing restrictions to local governments.12 Ongoing feedback to the COVER tier 1 survey by participating centres indicated that key structural changes made to services were updated in response to a reduction in local cases and pressure on local hospital services. Here, the focus is on those centres within Europe, and their experience of resumption of services and surgery in the aftermath of the first wave. The aim of this paper was to document changes in vascular practice during the first peak of the pandemic, and the adaptations made to practice in the months following the greatest pressure on services. This will permit ongoing comparison with repeated surveys of practice in the future.
Materials and methods
International guidelines on designing and reporting of surveys were used.13 The full study protocol is available at https://medrxiv.org/cgi/content/short/2020.05.27.20114322v1.
An online survey (SurveyMonkey) was developed by the VERN committee, and piloted and refined in response to rolling feedback from users. The survey contained closed and open questions, and free text for detailed comments regarding local challenges. The study is registered with the ISRCTN Registry (80453162).
Descriptive analysis
The survey was divided into two sections. The first period contained a descriptive analysis of the evolution of centres’ provision of common vascular services: threshold for treatment; imaging and screening; staff availability; theatre availability; multidisciplinary team input; clinics and PPE; and progression over time.
These data comprised three time periods of approximately seven weeks each. Period 1 was from 23 March to 8 May 2020. These data had already been gathered and published.2 The period for the first peak was estimated to have occurred between March and May 2020 for all countries included in this paper. It was also the period in which centres were mostlikely to see significant changes due to rapidly published national and international guidance and changes to working practice based on systemic shutdowns.
Period 2 was from 9 May to 24 June. This was considered to be a period during which guidance was released,6 and regions were beginning to develop resources to permit continuing care for their vascular patients. Period 3 was from 25 June to 8 August 2020. Around this time, more reports were being released about lockdowns being lifted across Europe.12 This division was also established so that each period was of a similar length.
Management of vascular work in centres that described themselves as having passed the initial peak of new cases in the initial survey filter question
The aim of these questions was to identify strategies used to permit the return of elective vascular surgery in only those centres in regions which had reached this stage of the pandemic.
This was a data collection period that occurred during periods 2 and 3, from 2 June to 8 August 2020. Centres that still felt they were in a region still experiencing a peak of cases were excluded from the analysis.
No formal statistical analysis was performed. Percentages represent the proportion of centres of a total of 53 (period 1), or 51 (period 2).
The full survey is detailed in Supplementary Appendix S1. Initial survey completion asked for permission to use contact details for future work. Using these details, centres were asked, through regular repeated advertisement via social media, e-newsletters, and established international collaborative networks, to complete the survey regularly to update their current practice over the stated period. Survey data from centres outside of Europe were excluded for the purposes of this analysis.
Data cleaning
The raw survey data were carefully scrutinised and cleaned prior to analysis. Responses from non-European centres were removed. Duplicate responses (defined as responses from the same unit on the same day), and responses that contained no useable data (e.g., where the responder had entered no more than the name and or size of the unit without answering any of the questions about service provision) were removed. If there were multiple responses from a single unit, the latest response during the specified period was used as the most contemporary representation of the practice in the centre at that time.
Calculating overall practice change over time
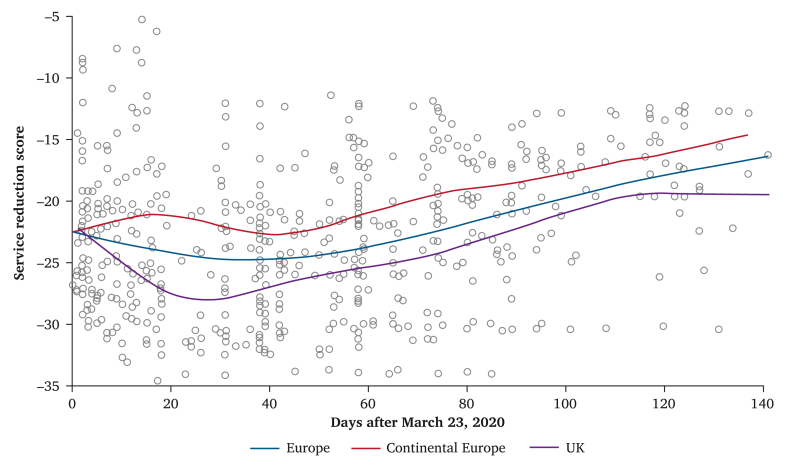
A scoring system was developed to enable calculation of overall relative changes in practice from normal. This was achieved by allocating a score of 0, 1, 2, or 3 to each possible answer for each service evaluation question asked in the questionnaire (Appendix S1). A score was allocated to each possible answer based on the perceived relative service reduction (with “0” representing no change and “3” representing the most significant change). The results, including mean values and standard deviations are included in Supplementary Table S1. A visual chart (Fig. 2) of mean scores for each time point was created using these scores by plotting centre responses with smoothing splines, used to fit the trend in the average response. Generalised cross validation was used to choose automatically the optimal smoothing parameters.
Figure 2.
Overall relative mean reductions in service throughout the study period. Results of the service reduction scores for all European (including UK for the purposes of this analysis, which remained in the transition period until December 2020) centres represented in the survey (purple), continental Europe alone (blue), and the UK (red). Each grey dot represents a centre response.
Results
Evolution of practice change during the three time periods
The results presented here are combined data from all centres and report the evolution of practice during the three stated study time periods in 2020, during which responses were received from 53 units across Europe (Table 1).
Table 1.
Breakdown of the location of the centres whose responses are included in the report.
| Country | Number of centres providing at least two complete responses during the mandated survey period | First confirmed case |
|---|---|---|
| Austria | 1 | 25 February 2020 |
| Belgium | 1 | 3 February 2020 |
| Switzerland | 1 | 25 February 2020 |
| Germany | 2 | 27 January 2020 |
| Spain | 2 | 31 January 2020 |
| UK | 28 | 31 January 2020 |
| Greece | 9 | 26 February 2020 |
| Republic of Ireland | 1 | 29 February 2020 |
| Italy | 3 | 30 January 2020 |
| The Netherlands | 1 | 27 February 2020 |
| Portugal | 2 | 2 March 2020 |
The table contains all centres included in section 1. Two centres reported they were still experiencing a spike in cases and were not included in the past the peak questions (one centre from the UK and one from Poland).
Provision of vascular services
The reported loss of dedicated inpatient vascular beds compared with each centre's baseline is shown in Fig. 1. Although centres reported a gradual improvement in the availability of dedicated vascular beds over time, the overall number remained below pre-pandemic levels even up to several months after the reported peak of cases. Fig. 2 shows the results of the scoring system used to calculate mean service reductions during the study period. The most significant service reductions were observed during the earliest phase of the study during the first peak of the pandemic, in most European countries. Although, overall, the centres providing data experienced a recovery of services towards normal pre-pandemic practice, levels of service remained below baseline by the time the study period had been completed at the end of July 2020.
Figure 1.
Reported change in the number of inpatient dedicated vascular beds during the survey period. A negative number on the y axis indicates a drop in the number of beds compared with the centre's baseline. The smoothed line (blue) represents mean changes over five days to demonstrate the overall change. The responses suggest that bed levels for vascular patients has not returned to baseline by the end of the survey period.
Carotid surgery
During period 1, 68% of centres described a change in approach to the management of carotid patients (i.e., a reduction in the number of patients offered surgery). This decreased to 54% during period 2; during period 3, 34% of centres were still offering surgery at reduced frequency vs. their normal practice. The remaining centres approached carotids on a case by case basis and none was automatically limiting surgery to crescendo transient ischaemic attacks only.
Abdominal aortic aneurysm screening programmes
Of those responding units with an active screening programme (either as part of the UK national screening programme or their own centre led programme), 52% of centres had stopped screening during the peak. By period 3, 22% of responding centres continued to halt their programme.
Aortic aneurysm treatment threshold
During period 1, only 25% of centres had been able to maintain their standard abdominal aortic aneurysm (AAA) practice, compared with most centres that documented increased thresholds for treatment of AAA to >6.5 cm or symptomatic patients, where baseline practice was in line with international standards. In contrast, during the final period, 53% of centres had returned to their normal practice.
Endovascular aortic aneurysm repair
Initially, only 15% of centres previously able to offer 24/7 endovascular aortic aneurysm repair (EVAR) were maintaining this standard. By the end of period 3 this had recovered to 43% of centres, with 40% able to offer EVAR during normal working hours only.
Post-EVAR surveillance
Surveillance following EVAR had been reduced or halted in 73% of centres during period 1; however, by the third period 32% of centres documented that they had not yet returned to their “normal” service.
Acute aortic syndrome
The majority of responding centres (65%) maintained their usual pathways for the treatment of acute aortic syndrome (AAS) (however, individual centre baselines of usual practice were not documented); by period 3 only 22% of centres were offering a reduced service. A small proportion of centres (2%) adopted early endovascular treatment of AAS during the pandemic peak, compared with their standard practice; this was not seen in the later time periods.
Lower limb ischaemia
In period 1, 87% of centres had altered their approach to patients presenting with limb ischaemia, with 49% still not offering pre-pandemic pathways by period 3. Of those centres, 36% of centres documented that they were being more conservative in their treatment than usual, with many limiting interventions to patients with only the most severe limb ischaemia (i.e., rest pain and/or tissue loss).
Throughout the study period, centres stated that they were using an “endovascular first” strategy more often than before the pandemic, with 66% of centres adopting this approach during the height of the pandemic and 53% of centres continuing to use a more “endovascular first” compared with their pre-pandemic approach in the final study period.
Access to operating theatres
During the first study period, many centres (57%) reported that there were no dedicated elective vascular surgical slots, or that access to theatres was only available for emergency cases. An assumption was made that these centres had dedicated elective vascular theatre lists before the pandemic.
By the later stages, 51% reported a return to normal operating capacity, while 45% continued to work with reduced or emergency operating theatre capacity compared with their normal service. By the end of the survey period only 3% continued to report a lack of dedicated vascular surgery slots.
Elective outpatient clinics
Initially, almost no centres were running normal clinics (only 2%), where 31% had moved to a pre-clinic triage system and 25% had cancelled all clinics outright. Centres adapted and, in the latest study period, 30% of centres had returned to their normal outpatient services, with 43% of centres continuing to triage patients.
Outpatient hot clinics
The use of hot clinics (i.e., clinics reserved for acute and urgent patients seen directly by a vascular surgeon) increased during the study period, despite a lower case incidence in the latter stages, and only 26% of centres did not have some form of hot clinic set up. Of note, the data collected did not include the number of centres with hot clinics pre-pandemic.
Multidisciplinary team meetings
Although a small proportion of centres did not run any form of multidisciplinary team (MDT) even before the pandemic, face to face meetings remained absent in almost half (46%) of centres even in the final study period, replaced by an MDT with reduced staff in 41% of centres and video MDTs in a further 30% of centres.
Staff redeployment
The redeployment of junior staff from their usual vascular team to other specialties during the peak of the pandemic was most marked in the initial weeks (55% of junior team members). Even during the later study period, 32% of centres reported an ongoing loss of medical staff to intensive care (22%), other surgical specialties (6%), or medical teams, including accident and emergency (4%).
Imaging
A quarter (26%) of centres documented reduced access to their usual pre-pandemic imaging in period 1; however, by period 3 this had reduced to 6% and most centres had documented a return to their first line imaging modality.
Personal protective equipment
During period 1, PPE was unavailable to staff in 25% of centres. Even during period 3, 12% reported that recommended PPE was not available at the level recommended by local guidelines.
Management of elective cases in the new era
During the period from the 2 June to 9 August, two of the 53 units felt they were still in the middle of a local peak in cases and were therefore excluded from this analysis (one in the UK and one in Poland). The rest indicated that their centre was in a region that had documented a reduction in the number of new cases being reported (i.e., past the peak).
The following section reports the data from the 51 of 53 unit responses from the UK (28 centres), Greece (nine centres), Italy (three centres), Spain and Germany (two centres), and Portugal, Austria, Belgium, Switzerland, Ireland, and the Netherlands (one centre each).
The survey asked centres what category they considered their centre to be in, using a colour coding system: blue, dedicated to COVID-19 patients; amber, mixed patient cohorts (i.e., caring for patients with suspected or confirmed COVID-19 alongside patients admitted for elective surgery); and green, only admitting and managing patients screened as negative for COVID-19 being admitted for elective surgery.
Most centres (81%) were designated amber sites. Seventy-six per cent of amber or blue centres reported a local green centre allied to their hospital, although 32% reported access for day case patients only, and 29% did not have access for their vascular cases. At least 24% of centres did not have a designated green hospital site within their region at all.
Patient testing in elective surgery
The majority of centres had begun to test all patients ahead of elective surgery (74%), with all centres testing at least a subset of elective patients. Although a small number of centres required two negative swabs before surgery, 90% had set a requirement of one negative swab.
Antigen testing using a swab was reported as the most common form of testing employed in this cohort. Pre-operative chest computed tomography was used in 31% of centres for some or all pre-operative patients. The majority of centres reported that they asked their patients to self isolate before surgery (67%), with the most frequent duration being 14 days (71%), followed by seven days (21%). Of these patients, 41% were being asked to self isolate with their whole household.
Management after confirmed COVID-19 infection
Fifty-nine per cent considered an unspecified length of time and a negative test necessary, whereas others relied on a period of time having passed, or a negative test. The majority of centres maintained their own usual practice with regard to post-operative thromboembolism prophylaxis.
Testing of healthcare workers
The practice of testing healthcare workers varied between testing all (31%), some (17%), those who were symptomatic (40%), and none (12%).
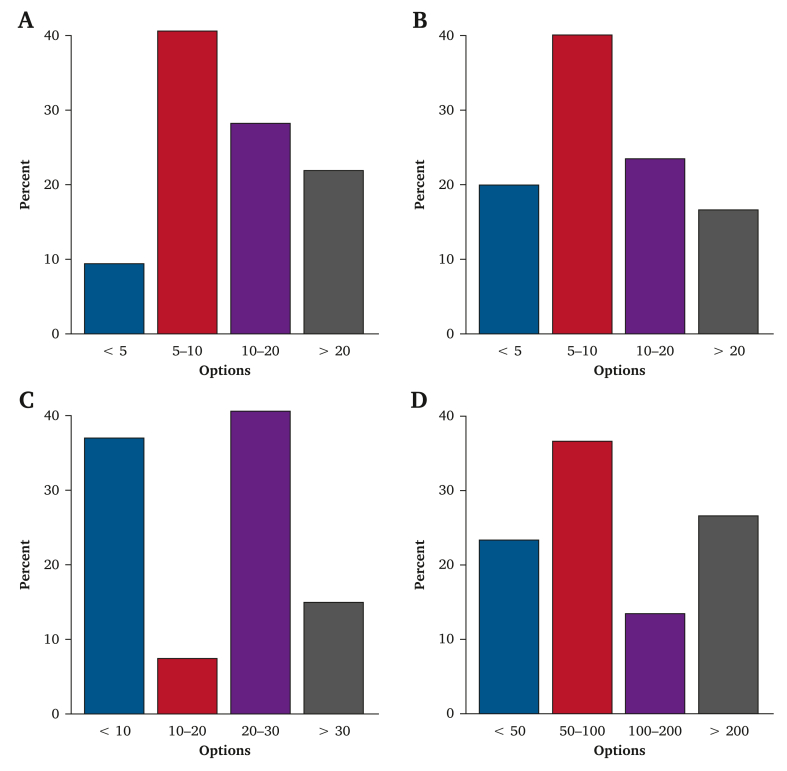
Waiting lists
Respondents aware of the status of their centre's elective waiting list (76%) reported that, in some centres, > 20 patients with an AAA were waiting for surgery due to backlogs caused by the pandemic. Similar numbers were reported for lower limb revascularisations (open and endovascular management) and superficial venous disease (Fig. 3).
Figure 3.
Reported estimated waiting list figures for key vascular conditions and associated surgery. Figures were taken from centres that had access to their waiting lists. The x axis represents the estimated number of patients on the waiting list for each procedure. The y axis indicates the percentage of responding centres in each category. (A) Abdominal aortic aneurysm repair. (B) Open surgery for peripheral arterial disease. (C) Endovascular procedure for peripheral arterial disease. (D) Treatment for varicose vein treatment.
Research
Although nearly 100% of centres were involved in research during the reported “recovery” phase, 50% were only open to COVID related studies, compared with 35% continuing with all types of research. Of the centres with academic surgeons on the team, 60% had not been able to resume their research, or had returned only partly.
Discussion
This paper has presented the initial recovery efforts of vascular teams around Europe as reported case numbers fell and the pressure on medical and surgical services eased after the initial peak of the COVID-19 pandemic. It represents a pattern of service reductions that may repeat during subsequent rises in cases and repeated lockdowns.
The initial report from the COVER study provided the first international collaborative reports of unit level vascular surgical practice at the start of the COVID-19 pandemic in 2020 and the period following the first international lockdowns.2
By focusing the data and reports of “recovery” to UK and European centres, the changes have been examined more comprehensively, including bed availability and the peri-operative pathway. It has also permitted a focus on countries considered to be “high income” and that share similar practices under the same pan-Europe guidelines (e.g., those from the European Society of Vascular Surgery).14
Despite the adaptations described by vascular centres to permit as much elective surgery to proceed as possible across a breadth of vascular services, including aortic aneurysm surgery, limb threatening ischaemia, and venous insufficiency, waiting lists have increased. The financial resources, operating time, patient prioritisation, and staffing that will be needed to “catch up” will be a challenge that requires multistakeholder input. An estimate of the backlog of AAA repairs in the UK alone, using results from the UK National AAA Screening Programme,15 that 809 size threshold aneurysms are identified annually, implies a backlog of approximately 130 AAAs from the initial peak alone. This does not consider the slow return to normal practice, and the patients diagnosed in the months subsequent to this. Following only 12 weeks of COVID-19 disruption, global predictive modelling from reported elective cancellations across a range of surgical specialties estimated it would take between 43 and 48 weeks for services to catch up, and that was based on a 20% increase in surgical volume.16
Few centres surveyed here had fully returned to their pre-pandemic practice by July 2020, and the most recent results of service availability and methods for ensuring COVID safe pathways may now represent the new normal. The demands made on teams to change their way of practising may have been found to suit their population and regional needs. Positive changes in practice may have been found to be favourable and are now continuing. One example is the use of remote MDTs in those centres that use them. Not all centres will have a space large enough to accommodate all members of a MDT in a COVID safe manner (i.e., with adequate social distancing). Therefore, the addition of video and teleconference software may now permit all members of the team to attend and contribute, whereas without it they would not be able to do so.
The use of hot clinics also increased during the pandemic. Although many centres required them to replace the lost regular outpatient clinics, many report continuing the practice into the recovery period.
The routine use of pre-operative COVID-19 tests shortly before admission for surgery, and after a set period of self isolation, has been reported by many of the centres surveyed here. Evidence from other studies demonstrate that contracting COVID-19 during or after surgery is detrimental to patient survival.17 However, even during the peak of the pandemic, the reported rate of suspected or confirmed infection among patients operated on for a vascular condition was very low.18 Vascular conditions are commonly associated with the comorbidities linked to COVID-19 mortality (i.e., hypertension, increasing age, and male sex). Therefore, many patients were likely to be practising a degree of social isolation before their acute presentation to vascular services, which will have provided some protection to those requiring surgery.
Tier 1 of the COVER study remains a pragmatic survey of evolving practice changes in a mix of district and tertiary vascular centres. Surveys have known limitations (e.g., duplicates and validation of results). Duplications were matched and resolved. The time periods were not correlated exactly with individual country lockdown dates. However, the countries of all centres included in this paper entered lockdown in March 2020 and were in lockdown when the survey began. Most centres that responded in a repeated way were from the UK. The data have been presented as received from centres, and the bias this displays must be accepted, while acknowledging that, across the countries included, available technologies and guidelines used for best practice are the same. Therefore, perceived changes from best guided care will have been broadly similar. Blanket coverage was not achieved for all countries involved and therefore no comment can be made on any bias introduced into the results due to the types of centres that responded.
Conclusion
In the months following the first peak of COVID-19 cases, many centres did not return to their previous levels of care provision. Since these data were collected, global rises in cases have led to rolling lockdowns and repeated hospital shutdowns due to pressures on services. Although these data are historical, they represent a pattern of service reductions that many countries may be forced to repeat in the future.
Conflict of interest
None.
Funding
The study has received financial grant support from the Circulation Foundation (Vascular charity, no grant reference). The National Institute for Health Research (NIHR) has provided salary support for the co-chief investigators (reference: NIHR000359) and co-study leads (reference: NIHR202011). The funders have not played any role in study design, analysis, or writing of the report.
Acknowledgements
The VERN executive committee would like to formally acknowledge the support and collaboration with the following international groups and networks: Vascular Society of Great Britain and Ireland (VSGBI); Rouleaux Club (RC); GLOBALSurg; British Society of Endovascular Therapy (BSET); Singapore Vascular Surgical Collaborative (SingVasc); Vascupedia (European vascular education platform); VASCUNET (global collaboration of International Vascular Registries); Australian and New Zealand Vascular Trials Network (ANZVTN); Audible Bleeding (evidence based podcast, USA); British Society of Interventional Radiology (BSIR); BSIR Trainees (BSIRT); International Working Group in the Diabetic Foot (IWGDF); the European Society of Vascular Surgery (ESVS); European Vascular Surgeons in Training (EVST); and STARSurg (UK based student surgical research network). We would also like to thank Sonia Kandola and the Department of Research and Development at the University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK (study sponsor site), and Irene Cruikshanks and Thomas Koller for Spanish and German translations. These partner groups and colleagues have enabled dissemination of the study and participation from multiple nations worldwide, which has been invaluable in the success of the COVER study to date.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ejvsvf.2022.10.002.
Contributor Information
Ruth A. Benson, Email: ruth.benson@gmail.com, vern.arterial.disease@gmail.com.
The VERN COVER study collaborative:
Maria Antonella Ruffino, Sharon Chan, Patrick Coughlin, Ayoola Awopetu, Philip Stather, Tristan Lane, Dimitrios Theodosiou, Mohamed Abozeid Ahmed, Thodur Vasudevan, Mohammed Ibrahim, Faraj Al Maadany, Mohamed Eljareh, Fatimah Saad Alkhafeefi, Raphael Coscas, Ertekin Utku Ünal, Raffaele Pulli, Sergio Zacà, Domenico Angiletta, Thomas Kotsis, Magdy Moawad, Matteo Tozzi, Nikolaos Patelis, Andreas M. Lazaris, Jason Chuen, Alexander Croo, Elpiniki Tsolaki, Gladiol Zenunaj, Dhafer Kamal, Mahmoud MH. Tolba, Martin Maresch, Vipul Khetarpaul, Joseph Mills, Gaurav Gangwani, Mohamed Elahwal, Rana Khalil, Mohammed A. Azab, Anver Mahomed, Richard Whiston, Ummul Contractor, Davide Esposito, Carlo Pratesi, Elena Giacomelli, Martín Veras Troncoso, Stephane Elkouri, Flavia Gentile Johansson, Ilias Dodos, Marie Benezit, José Vidoedo, João Rocha-Neves, António Henrique Pereira-Neves, Marina Felicidade Dias-Neto, Ana Filipa Campos Jácome, Luis Loureiro, Ivone Silva, Rodrigo Garza-Herrera, Victor Canata, Charlotte Bezard, Kathryn Bowser, Jorge Felipe Tobar, Carlos Gomez Vera, Carolina Salinas Parra, Eugenia Lopez, Yvis Gadelha Serra, Juan Varela, Vanessa Rubio, Gerardo Victoria, Adam Johnson, Leigh Ann O’Banion, Ragai Makar, Tamer Ghatwary Tantawy, Martin Storck, Vincent Jongkind, Orwa falah, Olivia McBride, Arda Isik, Athanasios Papaioannou, Paulo Eduardo Ocke Reis, Umberto Marcello Bracale, Ellie Atkins, Giovanni Tinelli, Emma Scott, Lucy Wales, Ashwin Sivaharan, Georgia Priona, Craig Nesbitt, Tabitha Grainger, Lauren Shelmerdine, Patrick Chong, Adnan Bajwa, Luke Arwynck, Nancy Hadjievangelou, Ahmed Elbasty, Oscar Rubio, Michael Ricardo, Jorge H. Ulloa, Marcos Tarazona, Manuel Pabon, Georgios Pitoulias, Kevin Corless, Orestis Ioannidis, Oliver Friedrich, Isabelle Van Herzeele, Badri Vijaynagar, Tina Cohnert, Rachel Bell, Hayley Moore, Prakash Saha, Edward Gifford, Matti Laine, Adel Barkat, Christos Karkos, Lenny Suryani Binti Safri, Gabriel Buitron, Javier Del Castillo, Paul Carrera, Nilson Salinas, Rodrigo Bruno Biagioni, Sergio Benites, César Andrés Mafla, Putera Mas Pian, Pereira Albino, Ernesto Serrano, Andres Marin, Marco González, Marsha Foreroga, Alejandro Russo, Andrés Reyes, Daniel Guglielmone, Lorena Grillo, Ronald Flumignan, Francisco Gomez Palones, Pierre Galvagni Silveira, Rosnelifaizur Bin Ramely, Sara Edeiken, Ian Chetter, Lucy Green, Abhilash Sudarsanam, Oliver Lyons, Gary Lemmon, Richard Neville, Mariano Castelli, Carlos A. Hinojosa, Rubén Rodríguez Carvajal, Aksim Rivera, Peng Wong, Laura Drudi, Jeremy Perkins, Kishore Sieunarine, Doaa Attia, Mahmoud Atef, Lostoridis Eftychios, Fred Weaver, Leong Chuo Ren, Mohannad Alomari, Reda Jamjoom, Qusai Aljarrah, Ayman Abbas, Faris Alomran, Ambrish Kumar, Abdulmajeed Altoijri, Kareem T. ElSanhoury, Ahmed Alhumaid, Tamer Fekry, Raghuram Sekhar, Panagiotis Theodoridis, Theodoridis Panagiotis, Konstantinos Roditis, Paraskevi Tsiantoula, Afroditi Antoniou, Raphael Soler, Natasha Hasemaki, Efstratia Baili, Eustratia Mpaili, Bella Huasen, Tom Wallace, Andrew Duncan, Matthew Metcalfe, Kristyn Mannoia, Carlos F. Bechara, Nikolaos Tsilimparis, Nathan Aranson, David Riding, Mariano Palena, Ciarán McDonnell, Nicolas J. Mouawad, Shonda Banegas, Peter Rossi, Taohid Oshodi, Rodney Diaz, Rana Afifi, Shiva Dindyal, Ankur Thapar, Ali Kordzadeh, Gonzalo Pullas, Stephanie Lin, Chris Davies, Katy Darvall, Akio Kodama, Thushan Gooneratne, Nalaka Gunawansa, Alberto Munoz, Ng Jun Jie, Nicholas Bradley, Wissam Al-Jundi, Felicity Meyer, Cheong Lee, Martin Malina, Sophie Renton, Dennis Lui, Andrew Batchelder, Grzegorz Oszkinis, Antonio Freyrie, Jacopo Giordano, Nikolaos Saratzis, Konstantinos Tigkiropoulos, Stavridis Kyriakos, Guriy Popov, Muhammad Usman Cheema, Pierfrancesco Lapolla, Yih Chun Ling Patricia, Raed Ennab, Brant W. Ullery, Ketino Pasenidou, Jacky Tam, Gabriel Sidel, Vivek Vardhan Jayaprakash, Lisa Bennett, Simon Hardy, Emma Davies, Sara Baker, Lasantha Wijesinghe, Adam Tam, Ken McCune, Manik Chana, Chris Lowe, Aaron Goh, Katarzyna Powezka, Ioanna Kyrou, Nishath Altaf, Denis Harkin, Hannah Travers, James Cragg, Atif sharif, Tasleem Akhtar, José Antonio Chávez, Claudia Ordonez, Martin Mazzurco, Edward Choke, Imran Asghar, Virginia Summerour, Paul Dunlop, Rachel Morley, Thomas Hardy, Paul Bevis, Robert Cuff, Konstantinos Stavroulakis, Efthymios Beropoulis, Angeliki Argyriou, Ian Loftus, Bilal Azhar, Sharvil Sheth, Marco Virgilio Usai, Asad Choudhry, Kira Nicole, Emily Boyle, Doireann Joyce, Mohammed Hassan Abdelaty Hassan, Alberto Saltiel, Gert Frahm-Jensen, George Antoniou, Muhammed Elhadi, Ali Kimyaghalam, Rafael Malgor, Leigh Ann O'Banion, Diego Telve, Andrej Isaak, Jürg Schmidli, Kevin McKevitt, Tam Siddiqui, Giuseppe Asciutto, Nikolaos Floros, George Papadopoulos, Alexandros Kafetzakis, Stylianos G. Koutsias, Petroula Nana, Athanasios Giannoukas, Stavros Kakkos, Konstantinos G. Moulakakis, Natasha Shafique, Arkadiusz Jawien, Matthew Popplewell, Chris Imray, Kumar Abayasekara, Timothy Rowlands, Ganesh Kuhan, Sriram Rajagopalan, Anthony Jaipersad, Uzma Sadia, Isaac Kobe, Devender Mittapalli, Ibrahim Enemosah, Christian-Alexander Behrendt, Adam Beck, Muayyad Almudhafer, Stefano Ancetti, Donald Jacobs, Priya Jayakumar, Fatemeh Malekpour, Sherene Shalhub, Boboyor Keldiyorov, Meryl Simon, Manar Khashram, Nicole Rich, Amanda Shepherd, Lewis Meecham, and Daniel Doherty
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.COVIDSurg Collaborative Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;107:1097–1103. doi: 10.1002/bjs.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Vascular and Endovascular Research Network (VERN) COVER study collaborative. Global impact of the first coronavirus disease 2019 (COVID-19) pandemic wave on vascular services. Br J Surg. 2020;107:1396–1400. doi: 10.1002/bjs.11961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng J.J., Ho P., Dharmaraj R.B., Wong J.C.L., Choong A.M.T.L. The global impact of COVID-19 on vascular surgical services. J Vasc Surg. 2020;71:2182–2183. doi: 10.1016/j.jvs.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Misra A. Doctors and healthcare workers at frontline of COVID 19 epidemic: admiration, a pat on the back, and need for extreme caution. Diabetes Metab Syndr. 2020;14:255–256. doi: 10.1016/j.dsx.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson R. Lack of protective gear disrupts oncology care. Lancet Oncol. 2020;21:631–632. doi: 10.1016/S1470-2045(20)30223-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imray CHE. COVID-19 virus and vascular surgery. Available at: https://www.vascularsociety.org.uk/professionals/news/113/covid19_virus_and_vascular_surgery [Accessed 5 May 2020].
- 7.https://vascular.org/news-advocacy/covid-19-resources#Guidelines&Tools [Accessed 7 July 2020].
- 8.American College of Surgeons. COVID-19 guidelines for triage of vascular surgery patients. Available at: https://www.facs.org/covid-19/clinical-guidance/elective-case/vascular-surgery [Accessed 8 July2020].
- 9.VERN Executive Committee The COvid-19 Vascular sERvice (COVER) Study: an international Vascular and Endovascular Research Network (VERN) collaborative study assessing the provision, practice, and outcomes of vascular surgery during the COVID-19 pandemic. Eur J Vasc Endovasc Surg. 2020;60:156–157. doi: 10.1016/j.ejvs.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benson R.A., Nandhra S., on behalf of the Vascular and Endovascular Research Network Study protocol for COvid-19 Vascular sERvice (COVER) study: the impact of the COVID-19 pandemic on the provision, practice and outcomes of vascular surgery. PLoS One. 2020;15 doi: 10.1371/journal.pone.0243299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saratzis A., Jaspers N.E.M., Gwilym B., Thomas O., Tsui A., Lefroy R., et al. Observational study of the medical management of patients with peripheral artery disease. Br J Surg. 2019;106:1168–1177. doi: 10.1002/bjs.11214. [DOI] [PubMed] [Google Scholar]
- 12.BBC. Coronavirus: How lockdown is being lifted across Europe. Available at: https://www.bbc.com/news/explainers-52575313 [Accessed 20 August 2020].
- 13.Kelley K., Clark B., Brown V., Sitzia J. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15:261–266. doi: 10.1093/intqhc/mzg031. [DOI] [PubMed] [Google Scholar]
- 14.European Society of Vascular Surgery. Guidelines. Available at: https://esvs.org/guidelines/ [Accessed 16 September 2022].
- 15.Vascular Society Quality Improvement Programme Annual report. 2018. https://www.vsqip.org.uk/reports/2018-annual-report/ Available at:
- 16.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Vascular and Endovascular Research Network VERN COVER Study Collaborative Outcomes of vascular and endovascular interventions performed during the COronaVIrus disease 2019 (COVID-19) pandemic: the vascular and endovascular research network (VERN) COvid-19 vascular sERvice (COVER) tier 2 study. Ann Surg. 2021;273:630–635. doi: 10.1097/SLA.0000000000004722. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.