Abstract
Objectives
Heart rate (HR) is one of the physiological variables in the early assessment of trauma-related haemorrhagic shock, according to Advanced Trauma Life Support (ATLS). However, its efficiency as predictor of mortality is contradicted by several studies. Furthermore, the linear association between HR and the severity of shock and blood loss presented by ATLS is doubtful. This systematic review aims to update current knowledge on the role of HR in the initial haemodynamic assessment of patients who had a trauma.
Design
This study is a systematic review and meta-regression that follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations.
Data sources
EMBASE, MEDLINE, CENTRAL and Web of Science databases were systematically searched through on 1 September 2020.
Eligibility criteria
Papers providing early HR and mortality data on bleeding patients who had a trauma were included. Patient cohorts were considered haemorrhagic if the inclusion criteria of the studies contained transfusion and/or positive focused assessment with sonography for trauma and/or postinjury haemodynamical instability and/or abdominal gunshot injury. Studies on burns, traumatic spinal or brain injuries were excluded. Papers published before January 2010 were not considered.
Data extraction and synthesis
Data extraction and risk of bias were assessed by two independent investigators. The association between HR and mortality of patients who had a trauma was assessed using meta-regression analysis. As subgroup analysis, meta-regression was performed on patients who received blood products.
Results
From a total of 2017 papers, 19 studies met our eligibility criteria. Our primary meta-regression did not find a significant relation (p=0.847) between HR and mortality in patients who had a trauma with haemorrhage. Our subgroup analysis included 10 studies, and it could not reveal a linear association between HR and mortality rate.
Conclusions
In accordance with the literature demonstrating the multiphasic response of HR to bleeding, our study presents the lack of linear association between postinjury HR and mortality. Modifying the pattern of HR derangements in the ATLS shock classification may result in a more precise teaching tool for young clinicians.
Keywords: Trauma management, Bleeding disorders & coagulopathies, ORTHOPAEDIC & TRAUMA SURGERY, ACCIDENT & EMERGENCY MEDICINE
STRENGTHS AND LIMITATIONS OF THIS STUDY
The paper provides a systematic search of EMBASE, MEDLINE (via PubMed), Cochrane Controlled Register of Trials (CENTRAL) and Web of Science databases, uses rigorous study selection criteria, assesses each enrolled paper for bias and performs meta-regression analyses.
Studies focusing on special populations including pregnant, paediatric (<18 years of age), geriatric (≥55 years), burned and traumatic spinal-injured or brain-injured patients were excluded from the study.
The heterogeneity and the difference in patient number among the included studies prevented us from performing an adequate meta-analysis.
Although mortality is a highly objective outcome, the fact that in some cases haemorrhage might not been the direct cause of death even if bleeding was present is an important limitation of the study.
Introduction
Hypovolaemia caused by haemorrhage is the most common cause of shock in trauma. Delay in the recognition of shock has been linked to unfavourable outcomes such as organ dysfuntion and mortality.1 2 The initial assessment of trauma-related hypovolaemic shock is based on derangements of physiological variables according to the recommendations of Advanced Trauma Life Support (ATLS).3 Among these variables, heart rate (HR) is one of the most controversial when it comes to blood loss.4–7 As commonly criticised, HR is not only influenced by haemodynamic changes, but also by several other factors such as anxiety, pain and medications resulting in a low specificity for haemorrhage.4 8 9 Furthermore, ATLS suggests the continuously increasing tendency of HR in accordance with the severity of bleeding.3 However, in clinical reality, the HR response to haemorrhage is rather biphasic or triphasic than linear.8 10 11 Consequently, the utility of HR in the early management of bleeding patients who had a trauma was called into doubt during the past decades.4 5 8 9
The reliability of HR was already questioned in the early 2000s by a retrospective analysis on 14 325 patients who had a trauma. According to the results of this study, HR displayed insufficient sensitivity and specificity in predicting hypotension after trauma.9 A few years later, a registry analysis denoted further doubts in HR, as it had performed poorly in predicting the need for an emergent intervention and administration of packed red blood cells in the first 24 hours postinjury.4 In addition, as ATLS was progressively widespread, the role of HR in the classification of hypovolaemic shock sparked controversy. In 2013, 16 305 patients from the German trauma register (DGU) were allocated into shock severity classes (I–IV) according to ATLS guidance.12 Ultimately, no group displayed relevant tachycardia at all. According to these data, expecting tachycardia in case of hypovolaemia can be misleading in many instances. Moreover, a false sense of haemodynamic stability based on normal HR can lead to fatal consequences, since the lack of tachycardia in hypoperfusion is associated with poor prognosis.13
Despite criticism, increased HR has been known as a characteristic of hypovolaemic shock for a very long time. The utility of HR as a predictor of mortality is supported by several papers.14 15 An international, cross-sectional study using data from two large trauma cohorts was conducted to develop and validate a prognostic model to predict death due to bleeding. Although HR showed a significant relation to mortality, the curve was U-shaped as opposed to the linear model presented by ATLS.15
A notable limitation of previous studies is that trauma protocols have undergone several changes, which makes recent information incomparable with data from the past. In 2010, the CRASH-2 trial brought one of the most prominent findings of the past decades with the validation of the safeness and effectivity of tranexamic acid (TXA).16–18
The present systematic review investigates the role of HR in the initial assessment of patients who had a trauma with haemorrhage. Regarding the efficiency of HR as a predictor of outcome in trauma, there is contradictory data in the literature.4 5 15 Furthermore, the linear association between HR and blood loss presented by ATLS is questionable.8 15 Due to the developement of trauma care and a paradigm shift in the initial fluid resuscitation approach in the past decades,16 19 we aimed to update current knowledge on the effectivity of HR as predictor of mortality postinjury. For this purpose, a comprehensive database search has been conducted, data have been extracted and analysed through meta-regressions. As a primary outcome, the relationship between HR and mortality has been assessed. Since the severity of bleeding has a close relation to the risk for adverse outcomes including increased organ dysfunction and mortality, our study may be able to initiate further research reappraising the validity of HR in the ATLS classification of hypovolaemic shock.
Materials and methods
Protocol and search strategy
The present review is reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).20 The PRISMA checklist for our work is available in the supporting information (online supplemental table S1).
bmjopen-2021-059271supp001.pdf (53.2KB, pdf)
A systematic search of EMBASE, MEDLINE (via PubMed), Cochrane Controlled Register of Trials (CENTRAL) and Web of Science databases was performed on 1 September 2020 with the following search terms: “trauma” AND (“heart rate” OR “pulse rate” OR “tachycardia” OR “bradycardia” OR “vital sign” OR “vital signs” OR “vital parameter” OR “vital parameters”) AND “mortality” AND (“bleeding” OR “haemorrhage” OR “hemorrhage” OR “haemodynamic” OR “hemodynamic”). Articles published before 2010 were excluded from our study.
Eligibility criteria
Records on bleeding patients who had a trauma were considered for eligibility only if they provided initial HR values (prehospital (PH) or on admission (AD)) in addition to mortality data covering a time interval not exceeding 30 days from the time of injury. Only full-text articles were considered. Non-English language reports, reviews, conference abstracts and case reports with low patient number (<10) were excluded. Taking the development of trauma care in the past decade into consideration (eg, introduction of TXA,16 and paradigm shift in fluid resuscitation19) all studies that included data on patients treated before 2010 were also excluded.
To consider a patient cohort haemorrhagic, the inclusion criteria of the individual studies had to include transfusion of blood products and/or positive focused assessment with sonography for trauma (FAST) examination and/or haemodynamical instability after trauma and/or abdominal gunshot injury. Records on special populations such as pregnant, paediatric (<18 years of age) or geriatric (≥55 years) were not considered. Studies on patients suffering burns, traumatic spinal or brain injuries were excluded.
With excluding special populations and paediatric and older age groups we aimed to reduce the influence of confounding factors. Since studies of geriatric patients who had a trauma have used age cutoffs ranging from 55 to 80 years and there is no clear consensus in the literature,21 22 we decided to exclude study populations of 55 years of age or older to diminish the effects of age-related confounding factors.
Study selection
After having duplicates removed with the help of a reference manager software (EndNote V.X7), articles published before 2010 were also discarded. On the remaining studies, title and abstract screenings were performed by two review authors (PJ and IG). Thereafter, the full texts of the potentially eligible records were obtained and assessed based on the criteria described above. Disagreements were resolved by consensus.
Data extraction
The following information was extracted from the eligible studies: title, first author’s name, year of publication, study design, data origin (country, hospital database/registry), data collection period, inclusion criteria, subgroups, patient number of the subgroups, total patient number, HR (mean±SD or median (IQR)), phase of recording HR values (PH/AD), mortality within 30 days (n, %). In case of studies using overlapping data, the less comprehensive report with the smaller sample size was excluded.
Risk of bias assessment
Quality In Prognostic Studies (QUIPS) tool was used separately by two authors (TH and ZR) to assess the risk of bias for each study.23 Disagreements were resolved by consensus. QUIPS consists of six main domains: ‘study attrition’, ‘study participation’, ‘prognostic factor’, ‘outcome measurement’, ‘study confounding’ and ‘statistical analysis and reporting’. A rating for each domain was assigned as carrying ‘low’, ‘moderate’ or ‘high’ risk of bias. Based on the ratings of the individual domains, the overall risk of bias was evaluated by each study.
Statistical analysis
The association between HR and mortality of patients who had a trauma was assessed using meta-regression analysis. A result of p<0.05 was considered as significant. As a subgroup analysis, meta-regression was performed on patients who had a trauma who received blood products. Statistical analyses were performed with Stata V.16 (StataCorp). To convert median values to means, we used the method of Wan et al.24
Patient and public involvement
Patients and public were not specifically involved in designing the study.
Results
Results of systematic search and selection
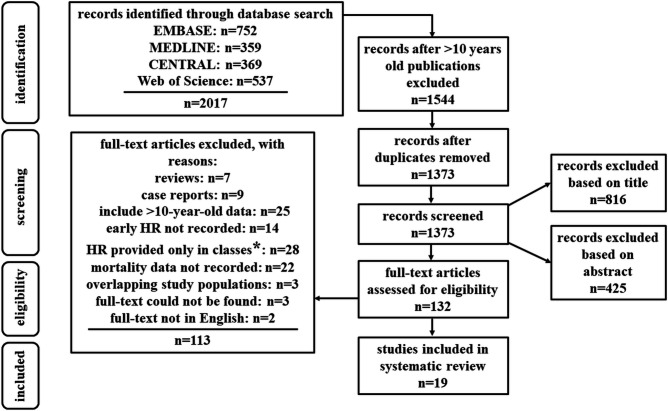
Two thousand and seventeen records were identified through our search strategy on 1 September 2020. One thousand three hundred and seventy-three articles were screened on title. Five hundred and fifty-seven abstracts were assessed, and 132 publications were enrolled into the final, comprehensive full text analysis. Ultimately, 19 records met our eligibility criteria. The flowchart of study enrolment is shown in figure 1.
Figure 1.
PRISMA flow diagram. Our search strategy resulted 2017 papers. After excluding articles published before 2010 and duplicates, 1373 papers were screened based on title and Abstract. In 79 cases the title clearly indicated non-eligible study design such as review or systematic review. Twenty-four title pointed out that the paper is a case report of a sole case. In 124 cases, the title clearly indicated non-eligible study population such as pregnant or paediatric. Five hundred and sixteen titles revealed that the study is not closely related to our research topic. In 73 cases, the title clearly indicated an animal experiment. Twenty-one records were excluded based on the Abstract section due to a non-eligible study design such as review or systematic review. The Abstract section indicated a non-eligible study population such as pregnant or paediatric in 94 cases. In 110 cases, the Abstract indicated that the study is not closely related to our research topic. Thirty-Nine animal experiments were filtered out based on Abstract. Eight studies did not have an English language Abstract. In 112 cases, the Abstract section revealed that the study includes data that is more than 10 years old. Forty-one case reports with a patient number <10 were excluded based on Abstract. After excluding a total of 816 papers based on title and 425 based on the Abstract section, 132 full-texts were assessed for eligibility. Reasons for non-inclusion of full-text articles are detailed above in the figure. Ultimately, 19 studies were enrolled to our meta-regression. *Heart rate (HR) was not provided in mean or median, only the number of patients in ranges of HR (eg, 100–120 bpm) was given. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Study characteristics
All publications processed data of patients who had a trauma with suspected haemorrhage from the past 10 years. From 19 studies yielding 3057 patients in total, 13 records collected data retrospectively and 6 prospectively. The number of participants in each dataset ranged from 15 to 428. Ten studies enrolled patients only if they received blood products as a part of the initial management. Seven publications used haemodynamic instability identified mainly by vital parameters as inclusion criteria. One study analysed patients with a positive result on FAST examination after blunt abdominal trauma. One research enrolled patients with abdominal gunshot injuries. Each of the inclusion criteria listed above entails a strong suspicion for significant bleeding. The main characteristics of the 19 eligible studies are summarised in table 1. The more comprehensive description of the papers is available in online supplemental table S2.
Table 1.
Baseline characteristics of the included studies
| First author, year | Country | Data collection | Patient characteristics | Patient no | HR mean±SD (PH/AD) | Mortality n, (%) |
| Bohonek 201929 | Czech Republic | Retrospective | Received blood products | 46 | 94.8±59.0 (AD) | 10 (21.7) |
| Boudreau 201930 | USA | Retrospective | Received blood products | 116 | 101.3±43.0 (PH) | 27 (23.3) |
| Duchesne 201931 | USA | Retrospective | Haemodynamic instability | 279 | 120.6±27.7 (AD) | 89 (32.0) |
| Montazer 201932 | Iran | prospective | Haemodynamic instability | 400 | 110.0±14.0 (AD) | 67 (16.7) |
| Priestley 201933 | USA | Retrospective | Received blood products | 283 | 104.0±24.0 (PH) | 88 (31.1) |
| Barmparas 201834 | USA | Retrospective | Received blood products | 120 | 101.1±39.7 (AD) | 59 (49.2) |
| Chaochankit 201835 | Thailand | Retrospective | Received blood products | 15 | 113.0±22.1 (AD) | 12 (80.0) |
| Moore 201836 | USA | Prospective | Haemodynamic instability | 125 | 110.0±15.9 (PH) | 16 (12.8) |
| Ng 201837 | Canada | Retrospective | Haemodynamic instability | 117 | 112.0±35.0 (AD) | 22 (19.0) |
| Guo 201738 | China | Prospective | Haemodynamic instability | 428 | 111.3±17.9 (AD) | 104 (23.4) |
| Heidari 201739 | Iran | Prospective | Blunt abdominal trauma with positive FAST | 168 | 105.3±23.4 (AD) | 57 (33.9) |
| Luehr 201740 | USA | Retrospective | Received blood products | 115 | 133.3±21.4 (PH) | 20 (17.4) |
| Naumann 201741 | UK | Retrospective | Received blood products | 17 | 108.0±16.2 (AD) | 3 (17.6) |
| Savage 201742 | USA | Retrospective | Received blood products | 330 | 108.2±55.3 (AD) | 82 (24.8) |
| Day 201643 | USA | Retrospective | Received blood products | 116 | 98.0±24.0 (PH) | 13 (11.0) |
| Ordoñez 201644 | Colombia | Retrospective | Haemodynamic instability | 171 | 112.6±23.5 (AD) | 26 (15.2) |
| Shah 201545 | Pakistan | Retrospective | Isolated abdominal gunshot wound | 70 | 99.8±30.3 (AD) | 11 (15.7) |
| Thurston 201546 | South Africa | Prospective | Haemodynamic instability | 50 | 123.3±13.1 (AD) | 11 (22.0) |
| Sisak 201347 | Australia | Prospective | Received blood products | 91 | 100.0±30.1 (AD) | 13 (14.0) |
The majority of the papers enrolled patients who had a trauma who received blood products (italics) and/or showed signs of haemodynamic instability. Haemodynamic instability was defined by vital parameters in most cases. most of the data was collected retrospectively. The number of participants in each dataset ranged from 15 to 428. There was a significant heterogeneity in mortality between datasets. The need for massive transfusion was accompanied by a prominently high mortality rate. A mean HR >120 bpm did not entail an outstanding mortality rate.
AD, on admission; FAST, focused assessment with sonography for trauma; HR, heart rate; PH, prehospital.
bmjopen-2021-059271supp002.pdf (123.6KB, pdf)
Study quality
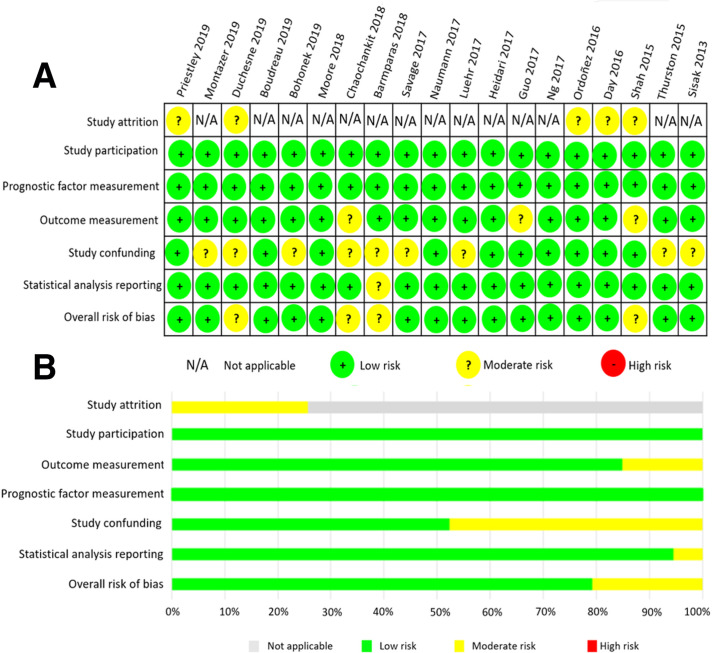
The methodological quality of the enrolled papers was investigated with QUIPS tool. The domain ‘study attrition’ was not suitable for the retrospective studies. In five prospective studies, a moderate risk for study attrition bias was identified. All papers were judged to carry a low risk of bias in ‘study participation’ and ‘prognostic factor measurement’ domains. In contrast, almost half of the records were accompanied by a moderate risk of bias with regards to ‘study confounding’, since the role of important confounders was not clarified in these reports. The results of the QUIPS assessment are shown in figure 2.
Figure 2.
Risk of bias assessment. (A) The figure shows the risk of bias in the six main domains of the quality in prognostic studies (QUIPS) assessment, in each paper. ‘Study attrition’ was not suitable for the retrospective studies. In five prospective studies, there was a moderate risk for study attrition bias. All studies were judged to carry a low risk of bias in ‘study participation’ and ‘prognostic factor measurement’ domains. ‘Study confounding’ was the worst rated domain: a moderate risk appeared in almost half of the records, in which the role of important confounders was not reported thoroughly. Based on the assessment of the six main domains, the overall risk of bias was determined for each study. (B) The summarised risk of bias is illustrated in percentages in the main domains. N/A, not available.
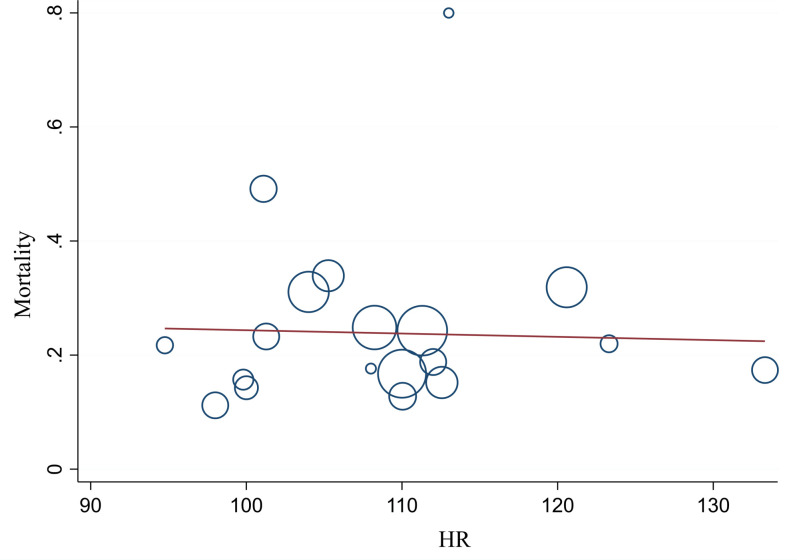
Primary meta-regression
Our primary meta-regression investigated the relation between HR and mortality in patients who had a trauma with haemorrhage based on all 19 datasets. We found no significant relation between HR and the outcome (p=0.847); thus, a linear association could not be confirmed. The results with the regression line are demonstrated in figure 3.
Figure 3.
Relation between heart rate (HR) and mortality of bleeding patients who had a trauma. Linear association between HR and mortality could not be identified.
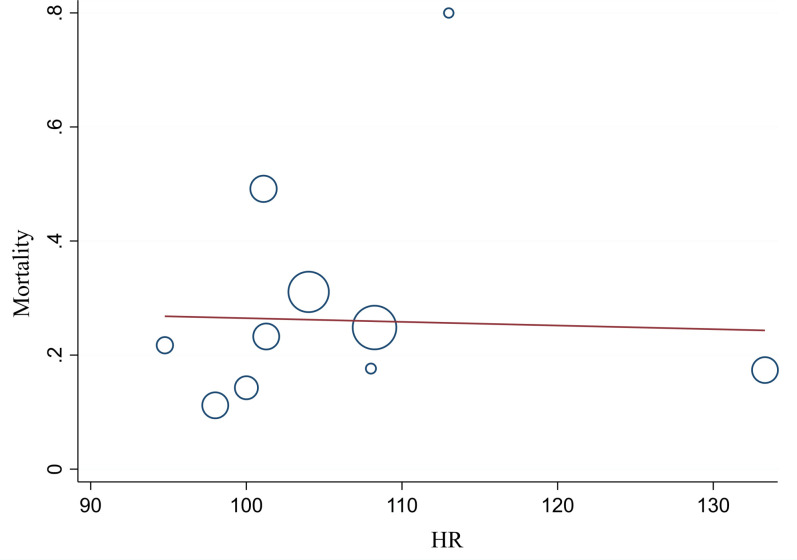
Subgroup analysis
Due to the relative heterogeneity of the patient enrolment criteria of the individual papers, a subgroup of 10 studies using the use of blood products in the initial management as inclusion criteria was formed and analysed separately. Again, our findings demonstrated no significant relation and linear association between HR and mortality rate (figure 4).
Figure 4.
Subgroup analysis of studies on patients who had a trauma who received blood products. Linear association between early heart rate (HR) and mortality rate of patients could not be identified.
Discussion
Interpretation of results
This study was designed to investigate and update current knowledge on the relation between HR and mortality in bleeding patients who had a trauma. We identified 19 studies providing early HR and mortality data on patients who had a trauma with haemorrhage from the past 10 years through database search. Due to the relative heterogeneity of the patient enrolment criteria of the individual papers, a subgroup of 10 records was created. Each of these 10 studies provided data on patients who had a trauma who received blood products. Meta-regressions were conducted on the data of all records and the subgroup, respectively.
No significant relation was found between HR and mortality in our meta-regressions. This result supports the evidence provided by studies doubting the value of HR in the initial assessment of potentially bleeding patients who had a trauma. In addition, our findings raise further concerns over the validiy of HR in the ATLS classification of hypovolaemic shock.
HR is an easily accessible vital parameter that indubitably reacts to circulatory volume depletion.5 6 However, the complexity of this reaction seems to contain too many possibilites for misinterpretation to be used in the simplified scheme presented by ATLS. The current classification of hypovolaemic shock suggests that HR increases continuously parallel to the severity of bleeding. The increase can stagnate between class I–II and III–IV according to ATLS.3 This scheme seems to be incongruent with the existing literature on the physiology of HR change during intravascular volume depletion. The HR response tends to follow a biphasic or triphasic pattern instead of continuous increase.8 10 11 If it comes to a decrease or stagnation in HR value, it is likely to occur at two separate stages of haemorrhage. First, due to increased vagal activity caused by a Bezold-Jarisch-like reflex just around 30% blood loss,5 10 between shock classes II and III, where ATLS suggests a clear increase in HR. Second, at the end stage of haemorrhage, bradycardia appears preceding cardiac arrest.15 25 26 Based on these observations, the pattern of HR alterations during haemorrhage suggested by ATLS may reflect the clinical condition more accurately after minor modifications (table 2).
Table 2.
Advanced Trauma Life Support (ATLS) classification of hypovolaemic shock including suggested modifications in the pattern of heart rate (HR) derangements
| Severity classes Estimated blood loss |
Class I <15% |
Class II 15%–30% |
Class III 31%–40% |
Class IV >40% |
|
| Physiological variables | HR | ↔ | ↔/↑ | ↑ | ↑/↑↑ |
| HR* | ↔ | ↑ | ↔/↑ | ↓/↑ | |
| SBP | ↔ | ↔ | ↔/↓ | ↓ | |
| GCS | ↔ | ↔ | ↓ | ↓ | |
| Pulse pressure | ↔ | ↓ | ↓ | ↓ | |
| Respiratory rate | ↔ | ↔ | ↑ | ↑ | |
| Urine output | ↔ | ↔ | ↓ | ↓↓ | |
| BD | 0–2 mEq | 2–6 mEq | 6–10 mEq | ≥10 mEq | |
| Transfusion | Monitor | Possible | Yes | Massive transfusion | |
The table is based on the 10th edition of ATLS. Estimated blood loss is shown as percentage of total blood volume.
*The suggested modifications are highlighted in bold: possible stagnation in HR value is indicated around 30% blood loss due to increased vagal activity. The possibility of bradycardia in profound bleeding in Class IV is highlighted.
BD, base deficit; GCS, Glasgow Coma Scale; HR, heart rate SBP, systolic blood pressure.
Despite criticism, HR is a promptly available vital sign that may lead physicians in the right direction in a relatively high percentage of cases when it comes to the initial management of potentially bleeding patients who had a trauma. However, the question remains if it is effective enough to be taken into consideration when we can also rely on parameters with higher sensitivity and specificity for bleeding—such as base deficit (BD). Multiple studies have presented the inferiority of HR as compared with other predictors included in the ATLS criteria such as systolic blood pressure, Glasgow Coma Scale and BD.27 28 Based on these concerns, the role of HR in the classification of hypovolaemic shock and the initial management of the severely injured should be re-evaluated.
Strenghts and limitations
Our study focuses on injury-related severe haemorrhage, a condition carrying high clinical importance. In the previous decades, trauma care has gone through remarkable development. On that note, we decided to use scientific data only from January 2010 to September 2020 (date of database search). The included papers were judged to carry a relatively low risk of bias.
Naturally, our study also has its limitations. Although mortality is a highly objective outcome and we included patients only with significant haemorrhage, the direct cause of death may be difficult to determine in some cases. Although studies on special populations have been excluded from our analysis, it is important to emphasise that the presence of potential confounding factors affecting HR values could not be ruled out completely. PH measures may have affected the HR values registered on AD. There is a notable difference in patient number among some of the included studies. The characteristics of the patient population by the individual records show a significant heterogeneity. To minimise this, a subgroup analysis was performed on patients who received blood products during initial in-hospital trauma care. These limitations prevented us from performing an adequate meta-analysis; however, we believe that we managed to raise attention on a clinically important issue.
Conclusions
The legitimity of HR in the initial assessment of hypovolaemic shock seems to be obvious, but in fact, its usefulness is questionable due to unsatisfactory sensitivity and specificity. The complexity of HR response during haemorrhage leads to the possibility of misinterpretation, false sense of haemodynamic stability and consequent delay in adequate therapy.
Further research is required to reappraise HR as a physiological variable in the ATLS classification of hypovolaemic shock. As a reaction frequently associated with bleeding, tachycardia should raise suspicion for haemorrhage, but it might not be appropriate as one of the determining factors of therapeutic decisions, such as administration of blood products. In addition to the literature demonstrating the multiphasic response of HR to bleeding, our study presents the lack of linear association with mortality. Considering these, modifying the pattern of HR derangements in the ATLS shock classification may make this pragmatic guide even more precise.
Supplementary Material
Acknowledgments
The authors are thankful to Hanne Sofie Solli for her skillful assisstance.
Footnotes
Contributors: PJ preparation of the draft of the manuscript, contribution in study design, selection of studies, data extraction; LH: statistical analysis, interpretation of data; PHe: expert in the field of internal medicine, provided revisions to the scientific content of the manuscript; EC: expert in the field of traumatology, substantial contribution in study design and interpretation of data, provided revisions to the scientific content of the manuscript; EB: data extraction, preparation of the standardised data collection sheet; TH: risk of bias assessment, stylistic and grammatical revision of the manuscript; IG: substantial contribution in study design, selection of studies, data extraction; AL: formatting the manuscript, stylistic revision of the manuscript; AS: statistical analysis, interpretation of data; ZR: risk of bias assessment, preparation of the manuscript; EP: participation in the design of the study and its coordination; JT: provided revisions to the scientific content of the manuscript, validation of data extraction; PHa: guarantor of the study, contribution in study design, preparation of the manuscript, provided revisions to the scientific content of the manuscript.
Funding: The study was funded by the following National Research Development and Innovation Office grants: FK138839; EFOP- 3.6.3-VEKOP-16-2017-00009. PHa was further supported by the Bolyai János Grant of the Hungarian Science Academy: BO/00605/21/5.
Disclaimer: Funders did not influence the design and scientific content of our paper in any way.
Competing interests: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Our study uses published data only. The original contributions presented in the study are included in the article and online supplemental material, further inquiries can be directed to the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Mutschler M, Paffrath T, Wölfl C, et al. The ATLS(®) classification of hypovolaemic shock: a well established teaching tool on the edge? Injury 2014;45 Suppl 3:S35–8. 10.1016/j.injury.2014.08.015 [DOI] [PubMed] [Google Scholar]
- 2.Evans JA, van Wessem KJP, McDougall D, et al. Epidemiology of traumatic deaths: comprehensive population-based assessment. World J Surg 2010;34:158–63. 10.1007/s00268-009-0266-1 [DOI] [PubMed] [Google Scholar]
- 3.Henry S, Brasel K, Stewart RM. American College of Surgeons. ”Shock”. In: Henry S, Brasel K, Stewart RmAdvanced trauma life support: student course manual. Chicago, IL, 2018: 42–61. [Google Scholar]
- 4.Brasel KJ, Guse C, Gentilello LM, et al. Heart rate: is it truly a vital sign? J Trauma 2007;62:812–7. 10.1097/TA.0b013e31803245a1 [DOI] [PubMed] [Google Scholar]
- 5.Secher NH and van Lieshout JJ. heart rate during haemorrhage: time for reappraisal. J Physiol 2010;588:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guyton AC. Textbook of medical physiology. Philadelphia, 1986: 332–43. [Google Scholar]
- 7.editor.. Braunwald E, Williams GH. ”Alterations in arterial pressure and the shock syndrome”. In: Jameson JLHarrison’s principles of internal medicine, 1987: 153–6. [Google Scholar]
- 8.Guly HR, Bouamra O, Spiers M, et al. Vital signs and estimated blood loss in patients with major trauma: testing the validity of the ATLS classification of hypovolaemic shock. Resuscitation 2011;82:556–9. 10.1016/j.resuscitation.2011.01.013 [DOI] [PubMed] [Google Scholar]
- 9.Victorino GP, Battistella FD, Wisner DH. Does tachycardia correlate with hypotension after trauma? J Am Coll Surg 2003;196:679–84. 10.1016/S1072-7515(03)00128-5 [DOI] [PubMed] [Google Scholar]
- 10.Jacobsen J, Secher NH. Heart rate during haemorrhagic shock. Clin Physiol 1992;12:659–66. 10.1111/j.1475-097X.1992.tb00369.x [DOI] [PubMed] [Google Scholar]
- 11.Little RA, Kirkman E, Driscoll P, et al. Preventable deaths after injury: why are the traditional 'vital' signs poor indicators of blood loss? J Accid Emerg Med 1995;12:1–14. 10.1136/emj.12.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mutschler M, Nienaber U, Brockamp T, et al. Renaissance of base deficit for the initial assessment of trauma patients: a base deficit-based classification for hypovolemic shock developed on data from 16,305 patients derived from the TraumaRegister DGU®. Crit Care 2013;17:R42. 10.1186/cc12555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mizushima Y, Ueno M, Watanabe H, et al. Discrepancy between heart rate and makers of hypoperfusion is a predictor of mortality in trauma patients. J Trauma 2011;71:789–92. 10.1097/TA.0b013e31822f7bbd [DOI] [PubMed] [Google Scholar]
- 14.Ley EJ, Singer MB, Clond MA, et al. Admission heart rate is a predictor of mortality. J Trauma Acute Care Surg 2012;72:943–7. 10.1097/TA.0b013e3182465527 [DOI] [PubMed] [Google Scholar]
- 15.Ageron F-X, Gayet-Ageron A, Steyerberg E, et al. Prognostic model for traumatic death due to bleeding: cross-sectional International study. BMJ Open 2019;9:e026823–6055. 10.1136/bmjopen-2018-026823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16., Shakur H, Roberts I, et al. , CRASH-2 trial collaborators . Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet 2010;376:23–32. 10.1016/S0140-6736(10)60835-5 [DOI] [PubMed] [Google Scholar]
- 17.Boling B, Moore K. Tranexamic acid (TXA) use in trauma. J Emerg Nurs 2012;38:496–7. 10.1016/j.jen.2012.06.001 [DOI] [PubMed] [Google Scholar]
- 18.Cole E, Davenport R, Willett K, et al. Tranexamic acid use in severely injured civilian patients and the effects on outcomes: a prospective cohort study. Ann Surg 2015;261:390–4. 10.1097/SLA.0000000000000717 [DOI] [PubMed] [Google Scholar]
- 19.Kutcher ME, Kornblith LZ, Narayan R, et al. A paradigm shift in trauma resuscitation: evaluation of evolving massive transfusion practices. JAMA Surg 2013;148:834–40. 10.1001/jamasurg.2013.2911 [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGwin G, MacLennan PA, Fife JB, et al. Preexisting conditions and mortality in older trauma patients. J Trauma 2004;56:1291–6. 10.1097/01.TA.0000089354.02065.D0 [DOI] [PubMed] [Google Scholar]
- 22.Meldon SW, Reilly M, Drew BL, et al. Trauma in the very elderly: a community-based study of outcomes at trauma and nontrauma centers. J Trauma 2002;52:79–84. 10.1097/00005373-200201000-00014 [DOI] [PubMed] [Google Scholar]
- 23.Hayden JA, van der Windt DA, Cartwright JL, et al. Assessing bias in studies of prognostic factors. Ann Intern Med 2013;158:280–6. 10.7326/0003-4819-158-4-201302190-00009 [DOI] [PubMed] [Google Scholar]
- 24.Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barriot P, Riou B. Hemorrhagic shock with paradoxical bradycardia. Intensive Care Med 1987;13:203–7. 10.1007/BF00254705 [DOI] [PubMed] [Google Scholar]
- 26.Hooper N, Armstrong TJ, Shock H. Hemorrhagic Shock. In: StatPearls [Internet, 2020. https://www.ncbi.nlm.nih.gov/books/NBK470382/ [Google Scholar]
- 27.Perel P, Prieto-Merino D, Shakur H, et al. Predicting early death in patients with traumatic bleeding: development and validation of prognostic model. BMJ 2012;345:e5166. 10.1136/bmj.e5166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jávor P CE, Butt E, Rárosi F. Comparison of the previous and current trauma-related shock classifications – a retrospective cohort study from a level I trauma centre. Eur Surg Res 2021. [DOI] [PubMed] [Google Scholar]
- 29.Bohonek M, Kutac D, Landova L, et al. The use of cryopreserved platelets in the treatment of polytraumatic patients and patients with massive bleeding. Transfusion 2019;59:1474–8. 10.1111/trf.15177 [DOI] [PubMed] [Google Scholar]
- 30.Boudreau RM, Deshpande KK, Day GM, et al. Prehospital tranexamic acid administration during aeromedical transport after injury. J Surg Res 2019;233:132–8. 10.1016/j.jss.2018.07.074 [DOI] [PubMed] [Google Scholar]
- 31.Duchesne J, Costantini TW, Khan M, et al. The effect of hemorrhage control adjuncts on outcome in severe pelvic fracture: a multi-institutional study. J Trauma Acute Care Surg 2019;87:117–24. 10.1097/TA.0000000000002316 [DOI] [PubMed] [Google Scholar]
- 32.Montazer SH, Jahanian F, Khatir IG, et al. Prognostic value of cardiac troponin I and T on admission in mortality of multiple trauma patients admitted to the emergency department: a prospective follow-up study. Med Arch 2019;73:11–14. 10.5455/medarh.2019.73.11-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Priestley EM, Inaba K, Byerly S, et al. Pulse pressure as an early warning of hemorrhage in trauma patients. J Am Coll Surg 2019;229:184–91. 10.1016/j.jamcollsurg.2019.03.021 [DOI] [PubMed] [Google Scholar]
- 34.Barmparas G, Dhillon NK, Smith EJT, et al. Patterns of vasopressor utilization during the resuscitation of massively transfused trauma patients. Injury 2018;49:8–14. 10.1016/j.injury.2017.09.021 [DOI] [PubMed] [Google Scholar]
- 35.Chaochankit W, Akaraborworn O, Sangthong B, et al. Combination of blood lactate level with assessment of blood consumption (ABC) scoring system: A more accurate predictor of massive transfusion requirement. Chin J Traumatol 2018;21:96–9. 10.1016/j.cjtee.2017.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moore HB, Moore EE, Chapman MP, et al. Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial. Lancet 2018;392:283–91. 10.1016/S0140-6736(18)31553-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ng M, Perrott J, Burgess S. Evaluation of tranexamic acid in trauma patients: a retrospective quantitative analysis. Am J Emerg Med 2019;37:444–9. 10.1016/j.ajem.2018.06.010 [DOI] [PubMed] [Google Scholar]
- 38.Guo S-B, Chen Y-X, Yu X-Z. Clinical characteristics and current interventions in shock patients in Chinese emergency departments: a multicenter prospective cohort study. Chin Med J 2017;130:1146–54. 10.4103/0366-6999.205862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heidari K, Taghizadeh M, Mahmoudi S, et al. Fast for blunt abdominal trauma: correlation between positive findings and admission acid-base measurement. Am J Emerg Med 2017;35:823–9. 10.1016/j.ajem.2017.01.035 [DOI] [PubMed] [Google Scholar]
- 40.Luehr E, Grone G, Pathak M, et al. Administration of tranexamic acid in trauma patients under stricter inclusion criteria increases the treatment window for stabilization from 24 to 48 hours-a retrospective review. Int J Burns Trauma 2017;7:115–9. [PMC free article] [PubMed] [Google Scholar]
- 41.Naumann DN, Hazeldine J, Dinsdale RJ, et al. Endotheliopathy is associated with higher levels of cell-free DNA following major trauma: a prospective observational study. PLoS One 2017;12:e0189870. 10.1371/journal.pone.0189870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Savage SA, Zarzaur BL, Brewer BL, et al. 1: 1 transfusion strategies are right for the wrong reasons. J Trauma Acute Care Surg 2017;82:845–52. 10.1097/TA.0000000000001402 [DOI] [PubMed] [Google Scholar]
- 43.Day DL, Anzelon KM, Conde FA. Association of prehospital shock index and trauma Bay Uncrossmatched red blood cell transfusion with multiple transfusion. J Trauma Nurs 2016;23:89–95. 10.1097/JTN.0000000000000192 [DOI] [PubMed] [Google Scholar]
- 44.Ordoñez CA, Herrera-Escobar JP, Parra MW, et al. Computed tomography in hemodynamically unstable severely injured blunt and penetrating trauma patients. J Trauma Acute Care Surg 2016;80:597–603. 10.1097/TA.0000000000000975 [DOI] [PubMed] [Google Scholar]
- 45.Shah AA, Rehman A, Shah SJ, et al. Abdominal gunshot wounds-a comparative assessment of severity measures. J Surg Res 2015;198:334–9. 10.1016/j.jss.2015.03.061 [DOI] [PubMed] [Google Scholar]
- 46.Thurston B, Chowdhury S, Edu S, et al. Time since injury is the major factor in preventing tranexamic acid use in the trauma setting: an observational cohort study from a major trauma centre in a middle-income country. S Afr J Surg 2015;53:13–18. 10.7196/sajs.2250 [DOI] [PubMed] [Google Scholar]
- 47.Sisak K, Manolis M, Hardy BM, et al. Acute transfusion practice during trauma resuscitation: who, when, where and why? Injury 2013;44:581–6. 10.1016/j.injury.2012.08.031 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059271supp001.pdf (53.2KB, pdf)
bmjopen-2021-059271supp002.pdf (123.6KB, pdf)
Data Availability Statement
Our study uses published data only. The original contributions presented in the study are included in the article and online supplemental material, further inquiries can be directed to the corresponding author.