Abstract
Antibiotic use (ABU) plays an important role in the proliferation of antimicrobial resistance (AMR). Global antimicrobial consumption in food production is projected to rise by 67% from 2010 to 2030, but available estimates are limited by the scarcity of ABU data and absence of global surveillance systems. The WHO South-East Asia (WHO SEA) region is at high risk of emergence of AMR, likely driven by intensifying farm operations and worsening ABU hotspots. However, little is known about farm-level ABU practices in the region. To summarize emerging evidence and research gaps, we conducted a scoping review of ABU practices following the Arksey and O'Malley methodological framework. We included studies published between 2010 and 2021 on farm-level ABU/AMR in the 11 WHO SEA member states, and databases were last searched on 31 October 2021. Our search strategy identified 184 unique articles, and 25 publications underwent full-text eligibility assessment. Seventeen studies, reported in 18 publications, were included in the scoping review. We found heterogeneity in the categorizations, definitions, and ABU characterization methods used across studies and farm types. Most studies involved poultry, pig, and cattle farms, and only one study examined aquaculture. Most studies evaluated ABU prevalence by asking respondents about the presence or absence of ABU in the farm. Only two studies quantified antibiotic consumption, and sampling bias and lack of standardized data collection methods were identified as key limitations. Emerging evidence that farm workers had difficulty differentiating antibiotics from other substances contributed to the uncertainty about the reliability of self-reported data without other validation techniques. ABU for growth promotion and treatment were prevalent. We found a large overlap in the critically important antibiotics used in farm animals and humans. The ease of access to antibiotics compounded by the difficulties in accessing quality veterinary care and preventive services likely drive inappropriate ABU in complex ways.
Keywords: Antibiotic use, Antimicrobial resistance, Animal farms, Southeast Asia, One health, Farming practices
Highlights
-
•
The methods used to characterize antibiotic use in farm animals are heterogenous.
-
•
Studies characterizing antibiotic use are limited in number and validity.
-
•
The antibiotics used in farm animals are critically important to human medicine.
-
•
Easy antibiotic access and limited veterinary care likely drive inappropriate use.
1. Introduction
Antimicrobial resistance (AMR) presents a significant health and economic burden worldwide especially in low- and middle-income countries (LMICs). [1] One projection suggested that global AMR, estimated from studies on Klebsiella pneumonia, Escherichia coli, Staphylococcus aureus, HIV, tuberculosis, and malaria, could cause ten million deaths annually by 2050, mostly in Africa and Asia. [2] Alarmingly, as early as 2019 an estimated 4.95 million deaths globally were associated with bacterial AMR alone, with the highest mortality rate found in western sub-Saharan Africa. [3] While difficult to quantify, the impact of AMR extends beyond the clinical setting by compounding the burden of chronic illnesses and widening health inequities. [1,[4], [5], [6]]
As part of concerted efforts to address AMR, the World Health Organization (WHO) is implementing a global action plan that includes optimizing antibiotic use (ABU) in humans and animals. [7] The recommendations stem from the evidence that ABU drives the proliferation of AMR. [[8], [9], [10], [11], [12], [13]] While ABU in humans and farm animals appear comparable, the biomass of farm animals substantially exceeds human biomass. [14] There is also accumulating evidence of environmental contamination linked to ABU in humans and animals, suggesting the need for a One Health approach. [15] However, until recently most of the studies describing ABU have centered on in-hospital and community-dwelling humans. [16] Moreover, the effect of ABU in animals on AMR in humans at the population level is unclear. [[17], [18], [19]]
Van Boeckel and collaborators estimated the 2010 global antimicrobial consumption in food animal production at 57,290 t and projected a steady rise to 95,795 t by 2030. [20] A combination of regulatory caps in veterinary antimicrobial consumption, reduction in meat intake, and imposition of user fees on the price of veterinary antibiotics is projected to reduce global animal antimicrobial consumption by 80%. [14] However, these estimates are limited by the scarcity of ABU data, especially from LMICs, and the absence of a global veterinary antimicrobial sales database. [14,20]
Southeast Asia (SEA), a region of the world with rapidly growing economies, changing societal structures, and expanding socioeconomic inequities experiences a disproportionate burden of AMR. [21] Potentially important contributors include underdeveloped surveillance systems and limited antimicrobial stewardship practices. [22] The high risk of emergence of AMR among humans and animals in WHO-SEA is also attributed to increased ABU in intensive livestock production. [23] The region hosts key veterinary ABU hotspots including the northern suburbs of Bangkok and southern coasts of India. [20] Despite the large burden of ABU and AMR in SEA, a systematic review of ABU in animal production spanning the last three decades found that only 17 of the 89 included studies were conducted in LMICs, with only two studies coming from the WHO SEA region. [24]
We conducted a scoping review to summarize emerging evidence about ABU practices in animal farms in the WHO-SEA region. A scoping review is a tool used in identifying and mapping available evidence when specific questions addressed by a more precise systematic review are unclear. [25] Our aim was to summarize the current evidence regarding: i) practices and motivations for ABU in animal farms in the WHO SEA region; ii) access to antibiotics including types and amounts used in animal farms; iii) potential drivers of inappropriate ABU in animal farms; and iv) research gaps.
2. Materials and methods
We used the methodological framework elaborated by Arksey and O'Malley. [26] We applied key components of the Preferred Reporting Items for Systematic Review and Meta-analyses extension for Scoping Reviews checklist in the development of the manuscript. [27]
2.1. Information sources and search strategy
Two reviewers (GMM and NA) independently performed a systematic bibliographic database search of PubMed, Scopus, and Ovid including Embase, Medline, Applied and Complementary Medicine, Global Health, and Zoological Records. The search strategy was drafted by GMM and was duplicated and verified by NA. We used Boolean operators on permutations of the keywords related to the following terms: “antibiotic use”, “animal farming”, “practices”, “estimation”, and the 11 WHO-SEA member states. The databases were last searched on 31 October 2021. Supplementary Table S1 elaborates the full search strategy used for Ovid.
2.2. Study selection and eligibility criteria
Two reviewers (GMM and NA) independently performed study selection based on the following eligibility criteria.
Inclusion Criteria
-
-
Primary research on ABU or AMR in animal farms
-
-
Description or quantification of practices by farmers and other stakeholders (may include managers, veterinarians, and other personnel)
-
-
Conducted between 2010 and 2021 inclusive
-
-
Conducted in WHO SEA member states (i.e., Bangladesh, Bhutan, India, Indonesia, Korea DPRK, Maldives, Myanmar, Nepal, Sri Lanka, Timor-Leste, and Thailand) [28]
-
-
Available full text in English
Exclusion criteria
-
-
Studies not involving farm animals
-
-
Indirect quantification methods of ABU/AMR including modelling studies
-
-
Systematic, scoping, or literature reviews involving any of inclusion criteria
-
-
Clinical, health facility-based, or diagnostic research
-
-
Quality improvement projects
A two-step selection strategy was performed. First, the study title and abstract were screened for inclusion. Disagreements were settled by discussion, and a third reviewer (AM) was the designated adjudicator. Full text articles were subsequently assessed independently for inclusion using a similar procedure.
2.3. Data charting process
The data extraction tool was developed in Microsoft Excel [29] by one reviewer (NA) and validated by another (AM). Test extraction sessions were performed by both reviewers to calibrate the tool. Two other reviewers (GMM and NH) independently extracted data from each eligible article. Discussion sessions were held to resolve disagreements, to synthesize extracted data, and to elaborate on emerging themes. Any persisting disagreement was adjudicated by another reviewer (AM).
2.4. Data items
The extracted variables included study characteristics, ABU practices, and potential drivers of inappropriate ABU. The reviewers also extracted additional data and reported study outcomes deemed to be relevant in characterizing ABU in animal farming. Supplementary Table S2 outlines the definitions of each variable.
2.5. Synthesis of results
We synthesized characteristics of included studies narratively and described ABU practices. We tabulated the classes of antibiotics used by farms and their corresponding classification on the WHO list of Critically Important Antimicrobials for Human Medicine (WHO-CIA) [30], the WHO AWaRe list of antibiotics [31], and the World Organisation for Animal Health (OIE) List of Antimicrobial Agents of Veterinary Importance [32]. We synthesized the reported potential drivers of inappropriate ABU based on pre-specified levels. Finally, we discussed the gaps we identified in the existing body of evidence.
3. Results
3.1. Selection of sources of evidence
Our search strategy identified 184 publications that underwent title/abstract screening. (Fig. 1) We selected 25 reports for full-text eligibility assessment. Seven reports were excluded: one was a literature review of drivers of AMR [33]; one included domestic animals instead of farm animals [34]; three reports were indirect methods of quantification of ABU/AMR [20,35,36]; and two articles were conference reports [37,38]. Seventeen studies, described in 18 publications [[39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56]], were included in the scoping review.
Fig. 1.
PRISMA flow diagram.
3.2. Characteristics and results of sources of evidence
Of the 17 studies, 12 were quantitative cross-sectional surveys, and two were qualitative studies (Table 1). Three were mixed-method studies: one involved survey and direct observation [48]; one used in-depth interviews (IDI), surveys, and observation [49]; and one involved policy analysis, IDI, and secondary analysis of quantitative data [52] from a previously published cross-sectional survey [51]. Seven studies were conducted solely in Thailand, five in India, and four in Bangladesh; one was a transnational study involving Indonesia, Thailand, and Vietnam. Eight studies involved poultry farms; six studies included cattle and dairy farms; five studies involved pig farms; and only one study included fish farms. The study participants included farm operators and/or owners, veterinarians, and pharmacists. Four studies dichotomized study population based on farm size and ownership, and two studies categorized the population based on food products (e.g. broiler and layer poultry farms).
Table 1.
Characteristics of included studies.
| Author year country | Animal farms (n) | Study design | Prevalence of antibiotic use in animal farms (%) | Method of collection of antibiotic data | Sources of antibiotics | Indications for ABU (% of farms/respondents) | Antibiotics used (% of farms/respondents) |
|---|---|---|---|---|---|---|---|
| Brower et al. 2017 India [36] |
Poultry layer farms (9) Poultry broiler farms (9) |
Cross-sectional Survey | 100 | Questionnaire interview without validation | NR | Disease treatment Growth promotion |
Fluoroquinolones (50.0)
|
| Chauhan et al. 2018 India [37] |
Cattle and dairy farms (15) | Qualitative Study (Interviews, Observations) | NR | NR | Private drug companies Informal prescribers Government extension services |
NR | NR |
| Coyne et al. 2019 Indonesia, Thailand, and Vietnam [38] |
Small to medium commercial broiler farms (419) Small to medium commercial pig farms (51) |
Cross-sectional Survey and Document Review | Not clearly stated | Questionnaire interview without validation for Indonesia and Thailand | Animal pharmacies Private drug companies |
Disease prevention Growth promotion Increasing mortality rate in surrounding farms |
Penicillin Tetracyclines Aminoglycosides |
| Ferdous et al. 2019 Bangladesh [39] |
Small scale poultry layer farms (120) | Cross-sectional Survey | ~100 | Questionnaire interview with validation using leftover antibiotic packets and bottles | Veterinarians Informal prescribers Animal pharmacies |
Disease prevention and treatment (40.8) Disease treatment only (34.2) Disease prevention only (14.2) |
Ciprofloxacin (22.5) Enrofloxacin (17.5) Amoxicillin (16.6) |
| Hallenberg et al.a 2020 Thailand [40] |
Small scale pig farms (113) Medium scale pig farms (51) |
Cross-sectional Survey | 79.3 | Questionnaire interview For medium scale farms: model created for expenditure estimates based on information provided by company veterinarians |
Animal pharmacies Animal health workers Company veterinarians |
Disease treatment (small scale farms – 84.0) Disease prevention (medium scale farms – 94.0) |
Enrofloxacin Gentamicin Penicillin/Streptomycin Amoxicillin |
| Hassan et al. 2021 Bangladesh [41] |
Poultry layer farms (210) Poultry broiler farms (210) |
Cross-sectional Survey | Layer farms – 83.8 Broiler farms – 85.7 |
Questionnaire interview without validation | Registered veterinarians Animal feed seller Animal pharmacies |
Disease treatment
|
Layer Farms: Amoxicillin (36.4) Ciprofloxacin (34.1) Tetracyclines (12.5) Broiler Farms: Ciprofloxacin (30.0) Tetracyclines (20.6) Amoxicillin (11.7) |
| Hicks et al. 2021 Bangladesh [42] |
Small scale poultry husbandry (499) Small scale bovid husbandry (228) |
Cross-sectional Survey | Poultry – 24.0 Cattles – 36.0 |
Questionnaire interview without validation | Drug seller/pharmacist Government and/or private veterinarians Informal prescribers |
Growth promotion Disease treatment Poor egg production |
NR |
| Huber et al.a 2021 Thailand [43] |
Small scale pig farms (113) Medium scale pig farms (51) |
Cross-sectional Survey | 79.3 | Questionnaire interview For medium scale farms: model created for expenditure estimates based on information provided by company veterinarians |
Animal pharmacies Animal health workers Company veterinarians |
Disease treatment (small scale farms – 84.0) Disease prevention (medium scale farms – 94.0) |
Enrofloxacin Gentamicin Penicillin/Streptomycin Amoxicillin |
| Ingthamjitr et al. 2017 Thailand [44] |
Red tilapia cage culture farms (35) | Cross-sectional Survey | 100 | Questionnaire interview without validation | Direct from company | Disease prevention | NR |
| Kumar et al. 2021 India [45] |
Cattle dairy farms (491) | Mixed Methods (Surveys, Direct Observation) |
10.0 | Questionnaire interview Direct observation Milk residue testing |
Not clearly stated | Disease treatment
|
Beta-lactams Fluoroquinolones Sulfonamides Aminoglycosides |
| Lekagul et al. 2020 Thailand [46] |
Commercial pig farms (58) Small scale pig farms (26) |
Mixed Methods (Surveys, Direct Observation, Key Informant Interviews) |
73.8 | Questionnaire interview Estimation of antibiotic volume from feed production records |
Drug companies and pharmacies Feed stores Pharmacies |
Disease prevention Disease treatment |
Enrofloxacin Amoxicillin Penicillin and combination Tetracycline |
| Love et al. 2015 Thailand [47] |
Commercial pig farms (4) Small scale pig farms (16) |
Cross-sectional Survey | 65.0 | Questionnaire interview Pooled feed analysis |
Feed stores Animal pharmacies |
NR | Commercial farms:
|
| Nuangmek et al.b 2018 Thailand [48] |
Poultry layer farms (126) Pig farms (125) |
Cross-sectional Survey | 100 | Questionnaire interview without validation | Animal pharmacies Direct from company Private veterinarians |
Disease treatment Growth promotion |
NR |
| Nuangmek et al.b 2021 Thailand [49] |
Poultry layer farms (126) Pig farms (125) |
Mixed Methods (Policy Analysis, Key Informant Interviews, Survey) |
100 | Questionnaire interview without validation | Animal pharmacies Direct from company Private veterinarians |
Disease treatment Growth promotion |
NR |
| Raosaheb et al. 2020 India [50] |
Cattle dairy farms (4) | Cross-sectional Survey | 100 | Estimation using treatment records (5–10 years data) | NR | Disease treatment (mastitis, gastrointestinal tract disease,
|
Penicillin and combinations Tetracyclines Aminoglycosides Sulfonamides and combinations Fluoroquinolones |
| Roess et al. 2015 Bangladesh [51] |
Households with chicken and/or cattle (521) | Cross-sectional Survey | 58.0 | Questionnaire interview without validation | Animal pharmacies Informal prescribers Government source |
Growth promotion Disease treatment
|
NR |
| Sharma et al. 2020 India [52] |
Dairy cattle farms (28) | Qualitative Study (In-Depth Interviews and Focus Group Discussions) |
NR | NR | Private veterinarians Animal pharmacies Quack practitioners Government veterinarians Milk federations |
Disease treatment
|
Gentamicin Oxytetracycline Penicillin Dicrysticin Amoxicillin Ampicillin |
| Wongsuvan et al. 2018 Thailand [53] |
Broiler chicken farms (8) | Cross-sectional Survey | 100 | Questionnaire interview Direct observation |
Direct from company | Growth promotion Disease prevention |
Amoxicillin Colistin Doxycycline Oxytetracycline Tilmicosin |
NR Not reported.
Both records refer to the same study.
Nuangmek et al. 2021 includes quantitative data from Nuangmek et al. 2018.
Of the 15 studies that reported ABU data, nine used self-reported information without assessment of reliability. Validation methods used by the remaining studies were: i) direct observation for antibiotic packets and containers during visits [42,48,56]; ii) antibiotic expenditure estimation for contract farms based on information from company veterinarians [43,46]; iii) antibiotic residue testing in milk samples [48] and pooled feeds [50]; iv) estimation of antibiotic volume from feed production records [49]; and v) review of treatment records [50].
Fourteen studies described the prevalence of ABU at the farm level. Most of the studies outlined the sources of antibiotics used in farms (14/17) and the indications for ABU (15/17). Only 11 studies enumerated the types of antibiotics used, with some reporting frequency and stratifying results based on the relevant type of farm included. Finally, 14 studies presented an assessment of non-prescription antibiotic use, but only six explicitly assessed adherence to withdrawal periods.
3.3. Evidence synthesis
3.3.1. Animal farm types
We found heterogeneity in the definitions used in categorizing farms according to size. Five studies involving pig farms in Thailand applied varying classifications. One used the number of sows, pertaining to female pigs with litter [43,46]; two studies used the gross number of pigs kept with different thresholds [49,50]; and two studies expressed pig farm size based on livestock units [51,52]. In poultry farms, size categories were based on varying ranges of birds kept, likely reflecting the different definitions used in Bangladesh [44] and Thailand [51,52]. Lastly, one study reported the number of milking bovines as a descriptor of cattle farm size. [48]
Smallholder and small-scale farms (SSF) were associated with subsistence extensive practices, wherein animal farming was not the only source of income for the operators. [43,46] Often the operators were also the farm owners who practiced animal husbandry and kept different livestock in their properties. In contrast, most of the medium- (MSF) to large-scale farms (LSF) involved intensive farming, and many were contracted and/or effectively owned by commercial establishments. [51,52,56]
3.3.2. Antibiotic use prevalence
The studies reported ABU at the farm level (i.e., proportion of included farms reporting ABU) and not at livestock level (i.e., proportion of livestock given antibiotics per farm). Most studies described ABU by evaluating farm operators ever having used antibiotics or within a wide observation period (i.e., up to 1 year prior to the survey). Only two studies provided an estimation of antibiotic consumption. [49,56] Twelve studies indicated that >50% of farms had ABU, including eight studies in which 100% of the included farms reported ABU. A study involving 164 pig farms found that ABU was significantly higher in MSF (100% of farms) compared to SSF (69.9% of farms). [43,46] Antibiotics were more commonly used as feed additives in MSF (47% of farms) than in SSF (0.9% of farms). One study reported that 13.1% of pig farms used antibiotic medicated feed [49], and another study on red tilapia cage cultures found that 57% of farms used both antibiotics and feed premixes [47].
Of the two studies with <50% of farms reporting ABU, one was conducted in Bangladesh which sampled at the household level. [45] The study found that 24% of households keeping poultry and 36% of households farming cattle used antibiotics therapeutically. A study of 491 dairy farmers in India showed only 10% of farms reported ABU in the past year [48]; like other studies [43,46], ABU was more frequently found in MSF and LSF. During site inspection, researchers found 3% of surveyed farms routinely kept antibiotics onsite, with higher frequency in LSF (10%) compared to SSF (2%). Alarmingly, the study found that in the farms that stocked antibiotics, more than half of the respondents had never heard of the term antibiotics.
3.3.3. Types of antibiotics used
We found a large overlap between the antibiotics used in human and animal health. (Table 2) Many of the critically important drugs of highest priority for human use, including quinolones, cephalosporins, and macrolides, were used in animals in large quantities. Studies also reported farms using antibiotics under the Watch [39,[41], [42], [43], [44],46,[48], [49], [50],53,55] and Reserve [39,42,49,50,56] AWaRe groups. One study collected data between 2019 and 2020 in poultry farms in Bangladesh [44] and still reported ABU under the Watch AWaRe group despite the 2019–2023 country-level target of at least 60% total antibiotic consumption coming from Access AWaRe group [31].
Table 2.
Frequently reported antibiotics.
| Farm type | Reported antimicrobial class | WHO list category [27] | WHO AWaRe category [28] | OIE list category [29] |
|---|---|---|---|---|
| Aquaculture | Quinolones Sulfonamides Tetracyclines |
Highly Important Critically Important – Highest Highly Important |
Access Watch Access |
Critically Important Critically Important Critically Important |
| Cattle and Dairy-Producing | Aminoglycosides Beta-lactams Penicillin Quinolones Sulfonamides Tetracyclines |
Critically Important – High Critically Important – Highest Highly Important Critically Important – Highest Highly Important Highly Important |
Watch Watch Access Watch Access Access |
Critically Important Critically Important Critically Important Critically Important Critically Important Critically Important |
| Pig | Aminoglycosides Penicillin and combinations Quinolones Tetracyclines |
Critically Important – High Highly Important Critically Important – Highest Highly Important |
Watch Access Watch Access |
Critically Important Critically Important Critically Important Critically Important |
| Poultry | Aminoglycosides Amoxicillin and Penicillin Colistin Cotrimoxazole Macrolides Quinolones Tetracyclines |
Critically Important – High Critically Important – High Critically Important – Highest Highly Important Critically Important - Highest Critically Important – Highest Highly Important |
Watch Access Reserve Access Watch Watch Access |
Critically Important Critically Important Highly Important Critically Important Critically Important Critically Important Critically Important |
There was general concordance in the classes of antibiotics (e.g., aminopenicillins, tetracyclines, and quinolones) used in poultry layer and broiler types. [44] The antibiotics used in SSF and backyard pig farms were also comparable to those used in MSF and commercial farms. [43,46,50] In dairy-producing cattle, similar antibiotics were reported (e.g., penicillin, tetracyclines, and quinolones) in organized and unorganized farming. [53] In certain commercial poultry farms, prophylactic antibiotic regimens consisted of a cocktail of amoxicillin, colistin, tetracyclines, and tilmicosin. [56] Colistin, a critically important drug used in treating multidrug-resistant bacterial infection, was being used in poultry [39,42] and pig [49,50,56] farms. However, the studies that reported colistin use were conducted prior to country-level adoption of policies banning their use. [57,58]
3.3.4. Antibiotic consumption estimation
One study used data from 31 feed mills to estimate the volume of antibiotics added to pig feeds in Thailand. [49] A total of 843 t of antibiotics were mixed into feeds in 2017. Another study calculated the weight of active pharmaceutical ingredients (APIs) received by each bird through a review of company-provided antibiotic regimen. [56] In both studies, the researchers identified sampling biases and lack of standardized methods of ABU data collection as key limitations.
3.3.5. Sources of antibiotics
Antibiotics were accessed through written prescription and non-prescription routes. Operators who received professional advice from veterinarians and university-affiliated extension workers purchased antibiotics from veterinary pharmacies. [40,41,50] Commercial MSF-LSF had access to company veterinarians who directly provided prescriptions and medications. [47,51,52,56] Private animal health practitioners of unknown qualifications provided advice and prescription, especially in smallholders and SSF. [43,46,55]
Some farmers relied on old and invalid prescriptions to purchase new or similar antibiotics. [42] Various cadres of animal health workers (e.g., paraveterinarians and homeopaths) also provided farmers with medication guidance and antibiotics. [45,49,54] Across countries, most farms were able to access drugs from animal pharmacies and feed sellers without prescriptions. [[43], [44], [45], [46]]
3.3.6. Indications for antibiotic use
Antibiotics were used for disease treatment and prevention including growth promotion (AGP). Reported illnesses varied per animal type. In poultry layer farms, chronic respiratory disease, Newcastle disease, and avian influenza were treated with antibiotics. In poultry broiler farms, ABU was reported for gumboro, coccidiosis, and respiratory illnesses. [44] In pig farms, operators gave antibiotics for diarrhea, malaise, and fever. [43] In dairy farms, mastitis, postpartum uterine infections, and gastrointestinal diseases were treated with antibiotics. [53] Finally, red tilapias were given antibiotics for weakness, stress, and wounds. [47]
Antibiotics were overwhelmingly used as growth promoters. Reduced egg production prompted routine ABU. [42] In dairy farms, antibiotics were given to improve milk production. [48] Increasing mortality in surrounding farms also triggered operators to give antibiotics to the rest of the herd. [41] Farmers and other stakeholders viewed ABU as a means of increasing net profit, especially in commercial MSF. [43] Contract farmers were given regimented antibiotics and feeds to intensify livestock growth such as in tilapia cage cultures [47] and poultry farms [56].
3.3.7. Withdrawal period
Withdrawal period refers to the set interval between the last antibiotic dose and the production of foodstuff to reduce animal product residues. [59] Three studies characterized the respondents' awareness of the need for withdrawal. They found minimal awareness across farm types: 5.8% in poultry farms [42] and at most 2% in dairy farms, being more frequent in LSF (5%) than in SSF (1.4%) [48,55]. One study of contract broiler farms found 100% adherence to a protocolized withdrawal period at day 31 of life [56], and 92% adherence was seen for both layer and pig farms based on surveys [51,52].
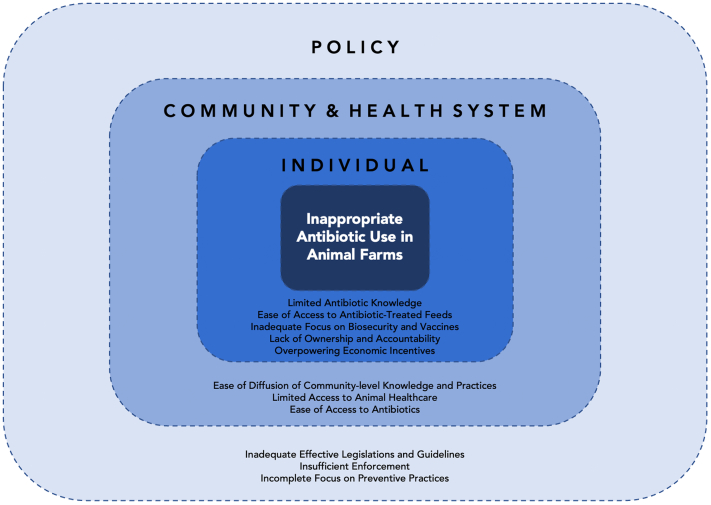
3.3.8. Drivers of inappropriate antibiotic use (Fig. 2)
Fig. 2.
Drivers of inappropriate antibiotic use in animal Farms. Potential drivers of inappropriate antibiotic use in animal farms are categorized according to individual, community and health system, and policy levels. Dashed lines in between the levels indicate the likely complex interactions between the drivers and across these levels.
3.3.8.1. Individual level drivers
3.3.8.1.1. Limited antibiotic knowledge
Evidence suggests limited farm-level knowledge on the role of antibiotics and effects of ABU. Farmers found difficulty differentiating antibiotics as a distinct class of drugs from other substances, adding uncertainty to the quality of collected data via cross-sectional interviews. [40,45,48,55] None of the studies reported on the language used in drug packaging or product inserts; however, one study included a figure of an empty tub of colistin from a rural poultry farm in Thailand in 2016, showing English text in the packaging. [56] Awareness of AMR was limited, especially in independent farms. [42,52] Farmers did not have the formal training to detect animal diseases, especially in SSF. [48] Even with appropriate training, translation to practice remained limited. [51] Farmers treated sick animals with multiple rounds of antibiotics before seeking care, regardless of etiology. [40,42] Finally, lack of understanding of the withdrawal period compounded inappropriate ABU. [42]
3.3.8.1.2. Ease of access to antibiotic-treated feed
Operators were unaware of the presence of antibiotics in feeds and their impact on AMR. [39,42,43] Contract farmers followed medicated feed guidelines set by companies, regardless of local disease epidemiology. [43,47,55] Similar to antibiotics, studies reported use of medicated feeds both for growth promotion [41,47,49] and treatment [41,54]. In an analysis of APIs from a medicated feed mill survey in Thailand, a majority of critically important antimicrobials of highest priority including colistin were mixed to enhance feeds for fatteners in pig production. [49]
3.3.8.1.3. Inadequate focus on biosecurity and vaccinations
There was low recognition of alternatives to antibiotics for growth promotion such as biosecurity and vaccinations. [39,41,43,45,46,50,51,54,55] Poor biosecurity practices were more frequent in smallholder and backyard farms, where use of open facilities was more common. [50] Some farmers and households shared enclosed spaces and water sources with farm animals [45], despite risks of zoonotic diseases [55]. Even in commercial farms, biosecurity was not prioritized despite rapid intensification [41], and ABU was used to mitigate poor housing conditions [46]. With poor growth, farms were likely driven to greater ABU.
3.3.8.1.4. Lack of ownership and accountability
Effective farm ownership dictated ABU practices by shaping healthcare access. Contract MSF-LSF were bound by company guidelines. This was beneficial in some cases by facilitating early targeted therapy. [41] However, overreliance on company guidelines perpetuated indiscriminate ABU practices such that a farm capable of raising 112,000 chickens annually would have used 34 kg of antibiotics in the same period just for growth promotion. [56] Intensive MSF was associated with higher AMR rates compared to extensive SSF due to larger ABU in pig production. [46] All MSFs in the study accessed drugs through their respective company. [43] Independent ownership could also propagate poor ABU practices by relying on unqualified prescribers. [41,44,[47], [48], [49]] Moreover, farmers did not feel accountable for monitoring farm-level ABU, viewing it as government responsibility. [41]
3.3.8.1.5. Overpowering economic incentives
Economic costs and benefits to the farm were perceived to be the most important consideration for choosing antimicrobials by a majority of farmers (63.7%) in a survey of layer and pig farms in Thailand. [51,52] A larger proportion of layer farms (73.8%) compared to pig farms (53.6%) agreed with this perception. Similarly, the majority (>75%) of farmers in poultry farms and pig farms in Indonesia and Thailand reported that antibiotics increased farm profitability and prevented livestock mortality. [41] In the same study, economic assessments of pig production in Thailand and poultry production in Indonesia showed that the cost of antimicrobials was small relative to other farm inputs. Fish cage operators, a majority of whom invested with their own savings (68.6%) and set up cages in front of their own residences (91.4%), used antibiotics to reduce disease and mortality in the farm. [47]
3.3.8.2. Community and health system level drivers
3.3.8.2.1. Ease of diffusion of community-level knowledge and practices
Community leaders influenced ABU practices especially in SSF. Groupthink and learning from other farmers could propagate inappropriate practices. [40,41] Farms belonging to cooperatives sought guidance from leaders who might not have had appropriate training [49] and had direct connections with drug sellers, presenting a conflict of interest [40]. Information regarding animal deaths and ABU from neighboring farms readily diffused in the community. [41,44,55] In contexts where livestock carried cultural significance as in cattle farming in Bangladesh, losing the herd carried severe consequences, including loss of respect in the community. This may have justified greater antibiotic spending to avoid death. [54]
3.3.8.2.2. Limited animal healthcare access
Farms had limited access to quality animal healthcare, impacting smaller farms more severely. [43] Veterinarian consults were too costly; hence, there was a proliferation of workers of varying credentials. [40,[44], [45], [46],55] Even when officially free, government services were associated with inconveniences and costs to farmers due to many potential reasons such as infrastructure deficiencies in remote areas. [54] In one study, up to 12% of cattle farms, mostly SSF, never received veterinary care. [48] Even when present, many veterinarians relied solely on their past treatment experiences due to unavailability of prescribing guidelines and diagnostic tests. [53]
Limited healthcare was also evident in MSF-LSF, where drug susceptibility testing at the farm level was deemed too costly, preventing its application during outbreaks. [51] Protocolized antibiotic regimens were not always grounded on best evidence because of lack of surveillance systems. [40,41,50] Lastly, healthcare workers trained for human healthcare were reportedly treating ill poultry. [45]
3.3.8.2.3. Ease of access to antibiotics
Antibiotics, medicated feeds, and other substances were deemed easily accessible. [48,50] In practice, prescriptions were not required for routine use [43,52], and especially when bought in bulk, antibiotics were cheaper [45].
3.3.8.3. Policy level drivers
3.3.8.3.1. Inadequate Effective Legislations and Guidelines
Studies identified inadequacy of treatment guidelines [43,53] and effective legislation regarding access to antibiotics and medicated feeds [41,43,47,49]. In certain areas, no legislation adequately covered monitoring of antibiotic residues in eggs [42] and meat products [50]. Oversight on rational ABU within large commercial farms was lacking. [43,46] Distribution of antibiotics by pharmaceutical companies was also poorly regulated or unregulated. [40,52] Among smallholder dairy farms in India, antibiotics were directly marketed by pharmaceutical representatives to the farmers with community elders serving as mediators. [40] In Thailand the regulations covering the distribution of veterinary products by pharmaceutical companies at the farm level were unclear, and procedures for sale of products including APIs were not systematically recorded. [52]
3.3.8.3.2. Insufficient enforcement
Despite the presence of comprehensive policies in some countries, effective enforcement remained inadequate. In Thailand, regulatory authorities did not have practical means of implementing laws, likely due to the large number of farms nationwide. [51,52] Specific rules were difficult to implement and resource-intensive. [46] For example, despite banning ABU in feeds in Bangladesh, poultry farmers found a loophole by adding antibiotics to water sources. [44] Enforcement demands were so large that a study even reported on health facilities being able to sell drugs without licenses. [52]
3.3.8.3.3. Incomplete focus on preventive practices
Farm biosecurity, vaccination, and other preventive measures were neither frequently promoted nor regulated. For instance, no rules covered egg tray management and routine personal protective equipment use in Bangladesh. [42] Farm zoning was also not discussed in Thailand. [50]
4. Discussion
The current body of evidence suffers from a deficiency of sustainable, standardized methods of ABU characterization. This may account for the heterogeneity of operational definitions used, the variety of the validation methods employed, and the uncertainties surrounding the quality of available data across farm types and countries.
Most of the included studies involve cross-sectional surveys; hence, estimates of ABU practices are based on self-reported data which are subject to respondents' comprehension of individual questions, recall ability, and truthfulness. The emerging evidence suggesting that respondents have difficulty differentiating antibiotics from other substances further raises concerns about the reliability of self-reported data. That we found only a small number of studies reporting on the types of antibiotics used in farms may be a manifestation of the limitations of these surveys. It highlights the importance of validating questionnaire interview data with production, treatment, and sales records. Moreover, due to the scarcity of updated farm registries in the region, many of the included cross-sectional studies employ convenience sampling and may not be representative of the target population. The underdeveloped data infrastructure and surveillance systems, especially in small and independent farms, are persisting problems worldwide. [[60], [61], [62]] This limits data aggregation, estimation, and comparison of results across contexts.
We did not find any longitudinal study on ABU practices in farms in the region, preventing characterization of changes and assessment of impact of interventions such as Thailand's National Strategic Plan on AMR. Instead, models are used to explore outcomes, but they are resource-intensive and lack reliable parameterization. [19]
We found only one study characterizing aquaculture in the region. This paucity in data is critical because the per capita consumption of aquaculture products is expanding more rapidly than meat and dairy consumption worldwide. Global antimicrobial consumption in aquaculture is projected to rise by 33% from 2017 to 2030, with the Asia-Pacific region having the largest ABU share (93.8%). [63] Furthermore, a review including the phenotypic prevalence of AMR in bacterial isolates from aquaculture products in SEA found high levels of resistance in Enterococcus spp. and Streptococcus dysgalactiae isolates in fish and in Klebsiella spp. isolates in shrimp. [64]
We found nominal reference to the One Health approach in the literature, whether in the analysis framework or the contextualization of results in the existing body of evidence. Most reference to ABU and AMR centered on animal-animal and animal-human transmission and interactions. The limited engagement with One Health-related literature suggests that further coordinated efforts by both government and non-governmental agencies in the area are needed.
Drawing on the emerging evidence, we propose the following recommendations. First, we recommend reviewing and developing sustainable and standardized methods of characterizing ABU in animals and the environment to support research and policy evaluation. These methods need to be grounded on the economic and logistic constraints in LMICs. Investments must be made to strengthen surveillance systems on antimicrobial consumption and resistance, like the Global Point Prevalence Survey used in human health [65]. Concerted efforts to evaluate livestock quantification methods and cross-validate consumption estimates based on sales data are also necessary to better characterize ABU.
Second, we recommend strengthening of veterinary health system in the region. While the drivers of inappropriate ABU likely interact with one another in complex ways, the lack of equitable access to qualified animal healthcare, the ease of access to antibiotics, and the paucity of preventive services are salient and recurring themes. Part of strengthening the veterinary health system is ensuring proper investments in water, sanitation, and hygiene (WASH) in both animal farms and surrounding communities are made. Reduction of AGP may be facilitated by improving biosecurity and WASH facilities and expediting herd vaccination. Public-private partnerships are likely necessary to capacitate the veterinary healthcare systems in the WHOSEA region.
Finally, we call for a collaborative research agenda examining the problems associated with inappropriate ABU from the vantage point of other actors including formal and informal veterinary workers, policy makers, and academic institutions. This could contribute to a more adequate characterization of ABU practices and ultimately inform the development of equitable interventions aimed at curbing AMR in the region.
5. Conclusions
In the WHO SEA region, many of the antibiotics used in animals for growth promotion and treatment are critically important for use in humans. The body of evidence is limited by the scarcity of surveillance systems and standardized ABU characterization and livestock quantification methods. The ease of access to poorly regulated antibiotic and drug products, compounded by the lack of access to quality animal healthcare and insufficient focus on preventive practices, likely drive inappropriate ABU.
Ethics statement
No ethical approval was required for this review work.
Funding
This work was funded by grant MR/S004769/1 from the Antimicrobial Resistance Cross Council Initiative supported by the seven United Kingdom research councils and the National Institute for Health Research.
Declarations of Competing Interests
The authors declare no competing interests.
CRediT authorship contribution statement
Greco Mark Malijan: Methodology, Data curation, Validation, Formal analysis, Writing – original draft, Visualization. Nopporn Howteerakul: Data curation, Validation, Formal analysis, Writing – original draft. Natasha Ali: Conceptualization, Methodology, Validation, Formal analysis, Writing – review & editing. Sukhontha Siri: Formal analysis, Writing – review & editing. Mondha Kengganpanich: Formal analysis, Writing – review & editing. OH-DART Study Group: Funding acquisition, Writing – review & editing. Roger Nascimento: Writing – review & editing. Ross D Booton: Writing – review & editing. Katherine M.E. Turner: Writing – review & editing, Funding acquisition. Ben S. Cooper: Conceptualization, Writing – review & editing. Aronrag Meeyai: Conceptualization, Methodology, Data curation, Validation, Supervision, Project administration, Funding acquisition, Writing – review & editing.
Acknowledgements
The authors acknowledge Prof. Kevin Marsh and Prof. Proochista Ariana for supporting the International Health and Tropical Medicine students' (GMM and NA) contribution to this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.onehlt.2022.100412.
Appendix A. Supplementary data
Search strategy and description of variables extracted
References
- 1.Naylor N.R., Atun R., Zhu N., Kulasabanathan K., Silva S., Chatterjee A., Knight G.M., Robotham J.V. Estimating the burden of antimicrobial resistance: a systematic literature review. Antimicrob. Resist. Infect. Control. 2018;7:1–17. doi: 10.1186/s13756-018-0336-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. Wellcome Trust; London, England: 2014. https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf (accessed May 26, 2022) [Google Scholar]
- 3.Murray C.J., Ikuta K.S., Sharara F., Swetschinski L., Aguilar G.R., Gray A., Han C., Bisignano C., Rao P., Wool E., Johnson S.C., Browne A.J., Chipeta M.G., Fell F., Hackett S., Haines-Woodhouse G., Hamadani B.H.K., Kumaran E.A.P., McManigal B., Agarwal R., Akech S., Albertson S., Amuasi J., Andrews J., Aravkin A., Ashley E., Bailey F., Baker S., Basnyat B., Bekker A., Bender R., Bethou A., Bielicki J., Boonkasidecha S., Bukosia J., Carvalheiro C., Castañeda-Orjuela C., Chansamouth V., Chaurasia S., Chiurchiù S., Chowdhury F., Cook A.J., Cooper B., Cressey T.R., Criollo-Mora E., Cunningham M., Darboe S., Day N.P.J., Luca M.D., Dokova K., Dramowski A., Dunachie S.J., Eckmanns T., Eibach D., Emami A., Feasey N., Fisher-Pearson N., Forrest K., Garrett D., Gastmeier P., Giref A.Z., Greer R.C., Gupta V., Haller S., Haselbeck A., Hay S.I., Holm M., Hopkins S., Iregbu K.C., Jacobs J., Jarovsky D., Javanmardi F., Khorana M., Kissoon N., Kobeissi E., Kostyanev T., Krapp F., Krumkamp R., Kumar A., Kyu H.H., Lim C., Limmathurotsakul D., Loftus M.J., Lunn M., Ma J., Mturi N., Munera-Huertas T., Musicha P., Mussi-Pinhata M.M., Nakamura T., Nanavati R., Nangia S., Newton P., Ngoun C., Novotney A., Nwakanma D., Obiero C.W., Olivas-Martinez A., Olliaro P., Ooko E., Ortiz-Brizuela E., Peleg A.Y., Perrone C., Plakkal N., Ponce-de-Leon A., Raad M., Ramdin T., Riddell A., Roberts T., Robotham J.V., Roca A., Rudd K.E., Russell N., Schnall J., Scott J.A.G., Shivamallappa M., Sifuentes-Osornio J., Steenkeste N., Stewardson A.J., Stoeva T., Tasak N., Thaiprakong A., Thwaites G., Turner C., Turner P., van Doorn H.R., Velaphi S., Vongpradith A., Vu H., Walsh T., Waner S., Wangrangsimakul T., Wozniak T., Zheng P., Sartorius B., Lopez A.D., Stergachis A., Moore C., Dolecek C., Naghavi M. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hay S.I., Rao P.C., Dolecek C., Day N.P.J., Stergachis A., Lopez A.D., Murray C.J.L. Measuring and mapping the global burden of antimicrobial resistance. BMC Med. 2018;16:78. doi: 10.1186/s12916-018-1073-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tacconelli E., Pezzani M.D. Public health burden of antimicrobial resistance in Europe. Lancet Infect. Dis. 2019;19:4–6. doi: 10.1016/S1473-3099(18)30648-0. [DOI] [PubMed] [Google Scholar]
- 6.Knight G.M., Glover R.E., McQuaid C.F., Olaru I.D., Gallandat K., Leclerc Q.J., Fuller N.M., Willcocks S.J., Hasan R., van Kleef E., Chandler C.I. Antimicrobial resistance and COVID-19: intersections and implications. ELife. 2021;10 doi: 10.7554/eLife.64139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO, Global Action Plan on Antimicrobial Resistance, n.d. https://apo.who.int/publications/i/item/global-action-plan-on-antimicrobial-resistance (accessed April 19, 2022).
- 8.Holmes A.H., Moore L.S.P., Sundsfjord A., Steinbakk M., Regmi S., Karkey A., Guerin P.J., Piddock L.J.V. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet Lond. Engl. 2016;387:176–187. doi: 10.1016/S0140-6736(15)00473-0. [DOI] [PubMed] [Google Scholar]
- 9.Andersson D.I., Hughes D. Selection and transmission of antibiotic-resistant Bacteria. Microbiol. Spectr. 2017;5:5.4.12. doi: 10.1128/microbiolspec.MTBP-0013-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christaki E., Marcou M., Tofarides A. Antimicrobial resistance in Bacteria: mechanisms, evolution, and persistence. J. Mol. Evol. 2020;88:26–40. doi: 10.1007/s00239-019-09914-3. [DOI] [PubMed] [Google Scholar]
- 11.Allen H.K., Stanton T.B. Altered egos: antibiotic effects on food animal microbiomes. Annu. Rev. Microbiol. 2014;68:297–315. doi: 10.1146/annurev-micro-091213-113052. [DOI] [PubMed] [Google Scholar]
- 12.Niehus R., van Kleef E., Mo Y., Turlej-Rogacka A., Lammens C., Carmeli Y., Goossens H., Tacconelli E., Carevic B., Preotescu L., Malhotra-Kumar S., Cooper B.S. Quantifying antibiotic impact on within-patient dynamics of extended-spectrum beta-lactamase resistance. ELife. 2020;9 doi: 10.7554/eLife.49206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beaber J.W., Hochhut B., Waldor M.K. SOS response promotes horizontal dissemination of antibiotic resistance genes. Nature. 2004;427:72–74. doi: 10.1038/nature02241. [DOI] [PubMed] [Google Scholar]
- 14.Van Boeckel T.P., Glennon E.E., Chen D., Gilbert M., Robinson T.P., Grenfell B.T., Levin S.A., Bonhoeffer S., Laxminarayan R. Reducing antimicrobial use in food animals. Science. 2017;357:1350–1352. doi: 10.1126/science.aao1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McEwen S.A., Collignon P.J. Antimicrobial resistance: a one health perspective. Microbiol. Spectr. 2018;6:6.2.10. doi: 10.1128/microbiolspec.ARBA-0009-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collignon P.J., McEwen S.A. One health—its importance in helping to better control antimicrobial resistance. Trop. Med. Infect. Dis. 2019;4:22. doi: 10.3390/tropicalmed4010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adda J. Preventing the spread of antibiotic resistance. AEA Pap. Proc. 2020;110:255–259. doi: 10.1257/pandp.20201014. [DOI] [Google Scholar]
- 18.Sharma C., Rokana N., Chandra M., Singh B.P., Gulhane R.D., Gill J.P.S., Ray P., Puniya A.K., Panwar H. Antimicrobial resistance: its surveillance, impact, and alternative management strategies in dairy animals. Front. Vet. Sci. 2018;4 doi: 10.3389/fvets.2017.00237. (accessed June 1, 2022) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Booton R.D., Meeyai A., Alhusein N., Buller H., Feil E., Lambert H., Mongkolsuk S., Pitchforth E., Reyher K.K., Sakcamduang W., Satayavivad J., Singer A.C., Sringernyuang L., Thamlikitkul V., Vass L., Avison M.B., Alhusein N., Booton R.D., Buller H., Chantong B., Charoenlap N., Couto N., Dulyayangkul P., Feil E., Gibbon M.J., Gould V.C., Lambert H., Meeyai A., Mongkolsuk S., Montrivade V., Pitchforth E., Phoonsawad K., Rangkadilok N., Ratanakorn P., Reyher K.K., Sakcamduang W., Satayavivad J., Singer A.C., Sirikanchana K., Sringernyuang L., Suriyo T., Suwanpakdee S., Thamlikitkul V., Turner K.M.E., Vass L., Wichuwaranan K., Wiratsudakul A., Avison M.B., Turner K.M.E. One Health drivers of antibacterial resistance: quantifying the relative impacts of human, animal and environmental use and transmission. One Health. 2021;12 doi: 10.1016/j.onehlt.2021.100220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Boeckel T.P., Brower C., Gilbert M., Grenfell B.T., Levin S.A., Robinson T.P., Teillant A., Laxminarayan R. Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. 2015;112:5649–5654. doi: 10.1073/pnas.1503141112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh P.K. One health approach to tackle antimicrobial resistance in South East Asia. BMJ. 2017;358 doi: 10.1136/bmj.j3625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zellweger R.M., Carrique-Mas J., Limmathurotsakul D., Day N.P.J., Thwaites G.E., Baker S., on behalf of the Southeast Asia Antimicrobial Resistance Network, Members of the Southeast Asia Antimicrobial Resistance Network A current perspective on antimicrobial resistance in Southeast Asia. J. Antimicrob. Chemother. 2017;72:2963–2972. doi: 10.1093/jac/dkx260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chereau F., Opatowski L., Tourdjman M., Vong S. Risk assessment for antibiotic resistance in South East Asia. BMJ. 2017;358 doi: 10.1136/bmj.j3393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cuong N.V., Padungtod P., Thwaites G., Carrique-Mas J.J. Antimicrobial usage in animal production: a review of the literature with a focus on low- and middle-income countries. Antibiotics. 2018;7:75. doi: 10.3390/antibiotics7030075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Munn Z., Peters M.D.J., Stern C., Tufanaru C., McArthur A., Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018;18:143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arksey H., O’Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 27.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., Hempel S., Akl E.A., Chang C., McGowan J., Stewart L., Hartling L., Aldcroft A., Wilson M.G., Garritty C., Lewin S., Godfrey C.M., Macdonald M.T., Langlois E.V., Soares-Weiser K., Moriarty J., Clifford T., Tunçalp Ö., Straus S.E. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization, WHO Southeast Asia, (n.d.). https://www.who.int/southeastasia/about (accessed April 19, 2022).
- 29.Microsoft Excel Spreadsheet Software | Microsoft 365, (n.d.). https://www.microsoft.com/en-ww/microsoft-365/excel (accessed April 5, 2022).
- 30.Critically Important Antimicrobials for Human Medicine: 6th Revision. World Health Organization; 2018. https://www.who.int/publications-detail-redirect/9789241515528 (accessed April 19, 2022) [Google Scholar]
- 31.2021 AWaRe Classification. World Health Organization; 2021. https://www.who.int/publications-detail-redirect/2021-aware-classification (accessed April 19, 2022) [Google Scholar]
- 32.OIE List of Antimicrobial Agents of Veterinary Importance. World Organisation for Animal Health; Paris: 2018. https://www.oie.int/en/document/a_oie_list_antimicrobials_june2019/ (accessed April 19, 2022) [Google Scholar]
- 33.Hinchliffe S., Butcher A., Rahman M.M. The AMR problem: demanding economies, biological margins, and co-producing alternative strategies. Palgrave Commun. 2018;4:1–12. doi: 10.1057/s41599-018-0195-4. [DOI] [Google Scholar]
- 34.Lucas P.J., Uddin M.R., Khisa N., Akter S.M.S., Unicomb L., Nahar P., Islam M.A., Nizame F.A., Rousham E.K. Pathways to antibiotics in Bangladesh: a qualitative study investigating how and when households access medicine including antibiotics for humans or animals when they are ill. PLoS One. 2019;14 doi: 10.1371/journal.pone.0225270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gräslund S., Holmström K., Wahlström A. A field survey of chemicals and biological products used in shrimp farming. Mar. Pollut. Bull. 2003;46:81–90. doi: 10.1016/S0025-326X(02)00320-X. [DOI] [PubMed] [Google Scholar]
- 36.Ting S., Pereira A., Alves A. de J., Fernandes S., Soares C. da C., Soares F.J., Henrique O. da C., Davis S., Yan J., Francis J.R., Barnes T.S., Jong J.B. da C. Antimicrobial use in animals in Timor-Leste based on veterinary antimicrobial imports between 2016 and 2019. Antibiotics. 2021;10:426. doi: 10.3390/antibiotics10040426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Islam S., Urmi U.L., Rana M., Sultana F., Jahan N., Hossain B., Iqbal S., Hossain M.M., Mosaddek A.S.M., Nahar S. High abundance of the colistin resistance gene mcr-1 in chicken gut-bacteria in Bangladesh. Sci. Rep. 2020;10:17292. doi: 10.1038/s41598-020-74402-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nugroho E., Isriyanthi N.M.R., Setyawan E., Arief R.A., McGrane J. Farmer perceptions of antimicrobial use (AMU) in small and medium-scale broiler farms in Indonesia. Int. J. Infect. Dis. 2020;101:84. doi: 10.1016/j.ijid.2020.09.247. [DOI] [Google Scholar]
- 39.C.H. Brower, S. Mandal, S. Hayer, M. Sran, A. Zehra, S.J. Patel, R. Kaur, L. Chatterjee, S. Mishra, B.R. Das, P. Singh, R. Singh, J.P.S. Gill, R. Laxminarayan, The prevalence of extended-spectrum beta-lactamase-producing multidrug-resistant Escherichia coli in poultry chickens and variation according to farming practices in Punjab, India, Environ. Health Perspect. 125 (n.d.) 077015. doi: 10.1289/EHP292. [DOI] [PMC free article] [PubMed]
- 40.Chauhan A.S., George M.S., Chatterjee P., Lindahl J., Grace D., Kakkar M. The social biography of antibiotic use in smallholder dairy farms in India. Antimicrob. Resist. Infect. Control. 2018;7:60. doi: 10.1186/s13756-018-0354-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coyne L., Arief R., Benigno C., Giang V.N., Huong L.Q., Jeamsripong S., Kalpravidh W., McGrane J., Padungtod P., Patrick I., Schoonman L., Setyawan E., Harja Sukarno A., Srisamran J., Ngoc P.T., Rushton J. Characterizing antimicrobial use in the livestock sector in three south east Asian countries (Indonesia, Thailand, and Vietnam) Antibiotics. 2019;8:33. doi: 10.3390/antibiotics8010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ferdous J., Sachi S., Al Noman Z., Hussani S.M.A.K., Sarker Y.A., Sikder M.H. Assessing farmers’ perspective on antibiotic usage and management practices in small-scale layer farms of Mymensingh district, Bangladesh. Vet. World. 2019;12:1441–1447. doi: 10.14202/vetworld.2019.1441-1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hallenberg G.S., Jiwakanon J., Angkititrakul S., Kang-air S., Osbjer K., Lunha K., Sunde M., Järhult J.D., Boeckel T.P.V., Rich K.M., Magnusson U. Antibiotic use in pig farms at different levels of intensification—farmers’ practices in northeastern Thailand. PLoS One. 2020;15 doi: 10.1371/journal.pone.0243099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hassan M.M., Kalam M.A., Alim M.A., Shano S., Nayem M.R.K., Badsha M.R., Al Mamun M.A., Hoque A., Tanzin A.Z., Nath C., Khanom H., Khan S.A., Islam M.M., Uddin M.B., Islam A. Knowledge, attitude, and practices on antimicrobial use and antimicrobial resistance among commercial poultry farmers in Bangladesh. Antibiotics. 2021;10:784. doi: 10.3390/antibiotics10070784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hicks J.P., Latham S.M., Huque R., Das M., Newell J., Abdullah S.M., Al Azdi Z., Jahan I., Rassi C., Hamade P., Shafique M., Islam M.S., King R. Antibiotic practices among household members and their domestic animals within rural communities in Cumilla district, Bangladesh: a cross-sectional survey. BMC Public Health. 2021;21:406. doi: 10.1186/s12889-021-10457-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huber L., Hallenberg G.S., Lunha K., Leangapichart T., Jiwakanon J., Hickman R.A., Magnusson U., Sunde M., Järhult J.D., Van Boeckel T.P. Geographic drivers of antimicrobial use and resistance in pigs in Khon Kaen Province, Thailand. Front. Vet. Sci. 2021;8 doi: 10.3389/fvets.2021.659051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ingthamjitr S., Paankhao N., Lueangtongkham W., Oopariktatipong K. Socio-economics and cage culture practices of red Tilapia (Tab Tim) at the Taasarn-Bangpla Canal, Nakhon Pathom Province, Thailand. J. Fish. Environ. 2017;41:50–59. [Google Scholar]
- 48.Kumar N., Sharma G., Leahy E., Shome B.R., Bandyopadhyay S., Deka R.P., Shome R., Dey T.K., Lindahl J.F. Understanding antibiotic usage on small-scale dairy farms in the Indian states of Assam and Haryana using a mixed-methods approach—outcomes and challenges. Antibiotics. 2021;10:1124. doi: 10.3390/antibiotics10091124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lekagul A., Tangcharoensathien V., Mills A., Rushton J., Yeung S. How antibiotics are used in pig farming: a mixed-methods study of pig farmers, feed mills and veterinarians in Thailand. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2019-001918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Love D.C., Tharavichitkul P., Arjkumpa O., Imanishi M., Hinjoy S., Nelson K., Nachman K.E. Antimicrobial use and multidrug-resistant Salmonella spp., Escherichia coli, and Enterococcus faecalis in swine from northern Thailand, Thai. J. Vet. Med. 2015;45:43–53. [Google Scholar]
- 51.Nuangmek A., Rojanasthien S., Patchanee P., Yano T., Yamsakul P., Chotinun S., Tadee P. Knowledge, attitudes and practices toward antimicrobial usage: a cross-sectional study of layer and pig farm owners/managers in Chiang Mai, Lamphun, and Chonburi provinces, Thailand, May 2014 to February 2016. Korean J. Vet. Res. 2018;58:17–25. doi: 10.14405/kjvr.2018.58.1.17. [DOI] [Google Scholar]
- 52.Nuangmek A., Rojanasthien S., Yamsakul P., Tadee P., Eiamsam-ang T., Thamlikitkul V., Tansakul N., Suwan M., Prasertsee T., Chotinun S., Patchanee P. Perspectives on antimicrobial use in pig and layer farms in Thailand: legislation, policy, regulations and potential. Vet. Integr. Sci. 2021;19:1–21. doi: 10.12982/VIS.2021.001. [DOI] [Google Scholar]
- 53.Raosaheb C.V., Manimaran A., Sivaram M., Sakthivel J. Antimicrobials use pattern under organized and unorganized dairy production conditions in southern India, Indian. J. Anim. Sci. 2020;90:362–366. [Google Scholar]
- 54.Roess A.A., Winch P.J., Akhter A., Afroz D., Ali N.A., Shah R., Begum N., Seraji H.R., El Arifeen S., Darmstadt G.L., Baqui A.H., the B.P.S. Group Household animal and human medicine use and animal husbandry practices in rural Bangladesh: risk factors for emerging zoonotic disease and antibiotic resistance. Zoonoses Public Health. 2015;62:569–578. doi: 10.1111/zph.12186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sharma G., Mutua F., Deka R.P., Shome R., Bandyopadhyay S., Shome B., Goyal Kumar N., Grace D., Dey T.K., Venugopal N., Sahay S., Lindahl J. A qualitative study on antibiotic use and animal health management in smallholder dairy farms of four regions of India. Infect. Ecol. Epidemiol. 2020;10:1792033. doi: 10.1080/20008686.2020.1792033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wongsuvan G., Wuthiekanun V., Hinjoy S., Day N.P., Limmathurotsakul D. Antibiotic use in poultry: a survey of eight farms in Thailand. Bull. World Health Organ. 2018;96:94–100. doi: 10.2471/BLT.17.195834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davies M., Stockton B. India bans use of “last hope” antibiotic on farms. Bur. Investig. J. En-GB. 2019 https://www.thebureauinvestigates.com/stories/2019-07-22/india-bans-use-of-last-hope-antibiotic-colistin-on-farms (accessed April 19, 2022) [Google Scholar]
- 58.Olaitan A.O., Dandachi I., Baron S.A., Daoud Z., Morand S., Rolain J.-M. Banning colistin in feed additives: a small step in the right direction. Lancet Infect. Dis. 2021;21:29–30. doi: 10.1016/S1473-3099(20)30915-4. [DOI] [PubMed] [Google Scholar]
- 59.P.O. of the E. Council of the European Union . Publications Office of the European Union; 1981. Council Directive 81/851/EEC of 28 September 1981 on the Approximation of the Laws of the Member States Relating to Veterinary Medicinal Products, CELEX1.http://op.europa.eu/en/publication-detail/-/publication/8f32cba4-c8fd-4e93-bcc0-5e855d63bda4/language-en (accessed April 19, 2022) [Google Scholar]
- 60.Sanders P., Vanderhaeghen W., Fertner M., Fuchs K., Obritzhauser W., Agunos A., Carson C., Borck Høg B., Dalhoff Andersen V., Chauvin C., Hémonic A., Käsbohrer A., Merle R., Alborali G.L., Scali F., Stärk K.D.C., Muentener C., van Geijlswijk I., Broadfoot F., Pokludová L., Firth C.L., Carmo L.P., Manzanilla E.G., Jensen L., Sjölund M., Pinto Ferreira J., Brown S., Heederik D., Dewulf J. Monitoring of farm-level antimicrobial use to guide stewardship: overview of existing systems and analysis of key components and processes. Front. Vet. Sci. 2020;7 doi: 10.3389/fvets.2020.00540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Landers T.F., Cohen B., Wittum T.E., Larson E.L. A review of antibiotic use in food animals: perspective, policy, and potential. Public Health Rep. 2012;127:4–22. doi: 10.1177/003335491212700103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khan X., Rymer C., Ray P., Lim R. Quantification of antimicrobial use in Fijian livestock farms. One Health. 2021;13 doi: 10.1016/j.onehlt.2021.100326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schar D., Klein E.Y., Laxminarayan R., Gilbert M., Van Boeckel T.P. Global trends in antimicrobial use in aquaculture. Sci. Rep. 2020;10:21878. doi: 10.1038/s41598-020-78849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nhung N.T., Cuong N.V., Thwaites G., Carrique-Mas J. Antimicrobial usage and antimicrobial resistance in animal production in Southeast Asia: a review. Antibiotics. 2016;5:37. doi: 10.3390/antibiotics5040037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Why a Global Point Prevalence Survey? Glob. PPS; 2021. https://www.global-pps.com/project/ (accessed April 19, 2022) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy and description of variables extracted