Abstract
IMPORTANCE
Approximately 80% of US adults and adolescents are insufficiently active. Physical activity fosters normal growth and development and can make people feel, function, and sleep better and reduce risk of many chronic diseases.
OBJECTIVE
To summarize key guidelines in the Physical Activity Guidelines for Americans, 2nd edition (PAG).
PROCESS AND EVIDENCE SYNTHESIS
The 2018 Physical Activity Guidelines Advisory Committee conducted a systematic review of the science supporting physical activity and health. The committee addressed 38 questions and 104 subquestions and graded the evidence based on consistency and quality of the research. Evidence graded as strong or moderate was the basis of the key guidelines. The Department of Health and Human Services (HHS) based the PAG on the 2018 Physical Activity Guidelines Advisory Committee Scientific Report.
RECOMMENDATIONS
The PAG provides information and guidance on the types and amounts of physical activity to improve a variety of health outcomes for multiple population groups. Preschool-aged children (3 through 5 years) should be physically active throughout the day to enhance growth and development. Children and adolescents aged 6 through 17 years should do 60 minutes or more of moderate-to-vigorous physical activity daily. Adults should do at least 150 minutes to 300 minutes a week of moderate-intensity, or 75 minutes to 150 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. They should also do muscle-strengthening activities on 2 or more days a week. Older adults should do multicomponent physical activity that includes balance training as well as aerobic and muscle-strengthening activities. Pregnant and postpartum women should do at least 150 minutes of moderate-intensity aerobic activity a week. Adults with chronic conditions or disabilities, who are able, should follow the key guidelines for adults and do both aerobic and muscle-strengthening activities. Recommendations emphasize that moving more and sitting less will benefit nearly everyone. Individuals performing the least physical activity benefit most by even modest increases in moderate-to-vigorous physical activity. Additional benefits occur with more physical activity. Both aerobic and muscle-strengthening physical activity are beneficial.
CONCLUSIONS AND RELEVANCE
The Physical Activity Guidelines for Americans, 2nd edition, provides information and guidance on the types and amounts of physical activity that provide substantial health benefits. Health professionals and policy makers should facilitate awareness of the guidelines and promote the health benefits of physical activity and support efforts to implement programs, practices, and policies to facilitate increased physical activity and to improve the health of the US population.
Being physically active is one of the most important actions individuals of all ages can engage in to improve their health. In the United States, an estimated $117 billion in annual health care costs and about 10% of premature mortality are associated with inadequate physical activity (not meeting the existing aerobic physical activity guideline).1-3 The evidence reviewed by the Physical Activity Guidelines Advisory Committee4 for the newly released Physical Activity Guidelines for Americans, 2nd edition5 (PAG) is clear–physical activity fosters normal growth and development and can make people feel better, function better, sleep better, and reduce the risk of many chronic diseases. Health benefits newly identified since the release of the previous 2008 Physical Activity Guidelines for Americans6 are listed in Box 1.
Box 1. New Evidence for Health Benefits of Physical Activity.
Improved bone health and weight status for children aged 3 through 5 years
Improved cognitive function for youth aged 6 to 13 years
Reduced risk of cancer at additional sites
Brain health benefits, including improved cognitive function, reduced anxiety and depression risk, and improved sleep and quality of life
Reduced risk of fall-related injuries for older adults
For pregnant women, reduced risk of excessive weight gain, gestational diabetes, and postpartum depression
For people with various chronic medical conditions, reduced risk of all-cause and disease-specific mortality, improved function, and improved quality of life
Some health benefits begin immediately after exercising, and even short episodes or small amounts of physical activity are beneficial. In addition, research shows that virtually everyone benefits: men and women of all races and ethnicities, young children to older adults, women who are pregnant or postpartum, people living with a chronic condition or a disability, or people who want to reduce their risk of disease. The evidence about the health benefits of regular physical activity is well established (Box 2), and research continues to provide insights into what works to increase physical activity, at both the individual and the community level.
Box 2. Health Benefits Associated With Regular Physical Activity.
Children and Adolescents
Improved bone health (ages 3 through 17 years)
Improved weight status (ages 3 through 17 years)
Improved cardiorespiratory and muscular fitness (ages 6 through 17 years)
Improved cardiometabolic health (ages 6 through 17 years)
Improved cognition (ages 6 to 13 years)
Reduced risk of depression (ages 6 to 13 years)
Adults and Older Adults
Lower risk of all-cause mortality
Lower risk of cardiovascular disease mortality
Lower risk of cardiovascular disease (including heart disease and stroke)
Lower risk of hypertension
Lower risk of type 2 diabetes
Lower risk of adverse blood lipid profile
Lower risk of cancers of the bladder, breast, colon, endometrium, esophagus, kidney, lung, and stomach
Improved cognition
Reduced risk of dementia (including Alzheimer disease)
Improved quality of life
Reduced anxiety
Reduced risk of depression
Improved sleep
Slowed or reduced weight gain
Weight loss, particularly when combined with reduced calorie intake
Prevention of weight regain after initial weight loss
Improved bone health
Improved physical function
Lower risk of falls (older adults)
Lower risk of fall-related injuries (older adults)
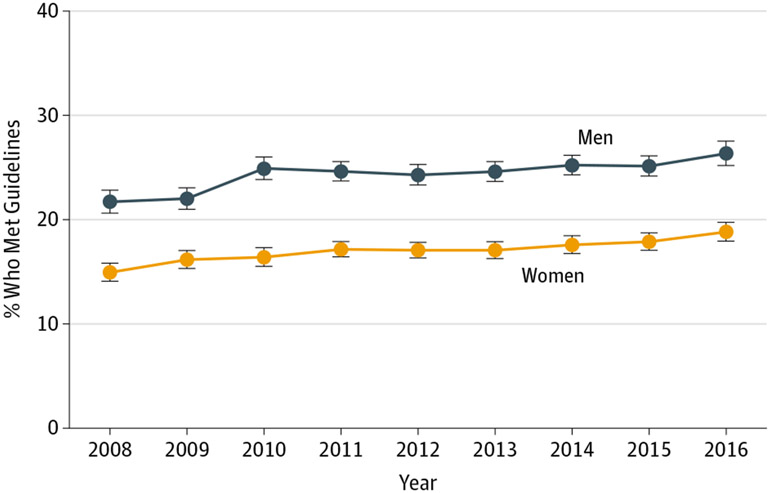
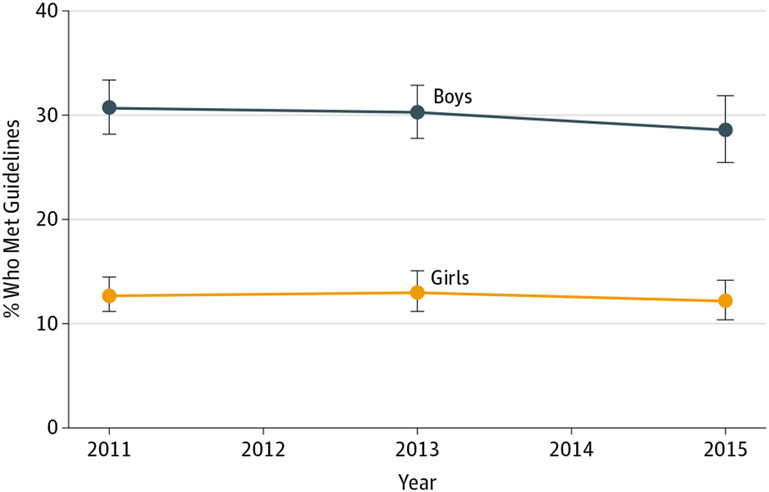
The information in the PAG is necessary because of the importance of physical activity to the health of people living in the United States, whose current inactivity puts them at unnecessary risk for chronic diseases and conditions. Healthy People 2020 established objectives for increasing the level of physical activity among US residents over the decade from 2010 to 2020.7 Although the latest federal monitoring data shows some improvements in physical activity levels among US adults (Figure 1), as of 2016 (adults) and 2015 (adolescents), only 26% of men, 19% of women, and 20% of adolescents report performing sufficient activity. Sufficient physical activity is defined as at least 150 minutes of moderate-intensity aerobic physical activity and 2 days per week of muscle-strengthening activity for adults and at least 60 minutes of moderate-intensity aerobic physical activity and 3 days per week of muscle-strengthening activity for youth (Figure 2).8
Figure 1. Percentage of US Adults 18 Years or Older Who Met the Aerobic and Muscle-Strengthening Guidelines, 2008-2016.
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey (NHIS). Estimates are age-adjusted to the 2000 US standard population using 5 age groups: 18-24 years, 25-34 years, 35-44 years, 45-64 years, and 65 years and older. Annual sample sizes ranged from 9188 (2008) to 16 032 (2014) for men and from 11 955 (2008) to 19 904 (2014) for women. NHIS questions ask about frequency and duration of light-intensity to moderate-intensity and vigorous-intensity leisure-time physical activities, as well as the frequency of muscle-strengthening activities. Meeting the aerobic component of the 2008 Physical Activity Guidelines for Americans for this population is defined as reporting at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic physical activity per week, or an equivalent combination. Meeting the muscle-strengthening component is defined as reporting muscle-strengthening activities at least 2 days per week. Error bars indicate 95% CIs.
Figure 2. Percentage of US High School Students Who Met the Aerobic Physical Activity and Muscle-Strengthening Guidelines, 2011-2015.
Source: Centers for Disease Control and Prevention, Youth Risk Behavior Surveillance System. Annual sample sizes ranged from 6599 (2013) to 6950 (2011) for boys and from 6448 (2013) to 7312 (2015) for girls. Meeting the aerobic component of the 2008 Physical Activity Guidelines for Americans for this population is defined as reporting at least 60 minutes of “any kind of physical activity that increases your heart rate and makes you breathe hard some of the time” on all days during the 7 days before the survey. Meeting the muscle-strengthening component is defined as reporting at least 3 days of “exercises to strengthen or tone your muscles” during the 7 days before the survey. Error bars indicate 95% CIs.
Although the key guidelines are provided for all people in the United States, the primary audience for the PAG is health professionals and policy makers. However, the document may also be useful to individuals. The principal concept of the PAG is that regular physical activity over months and years can produce long-term health benefits. This Special Communication provides an overview of the Physical Activity Guidelines for Americans, 2nd edition5 and explains how health professionals can help patients increase physical activity and improve health.
Process for Developing the Physical Activity Guidelines for Americans
The PAG was developed with 2 major steps: a review of the science by a federal advisory committee and the development of the PAG by the Department of Health and Human Services (HHS) writing team. In June 2016, 17 academic experts were appointed to the 2018 Physical Activity Guidelines Advisory Committee by former HHS Secretary Sylvia Mathews Burwell. The committee was charged with reviewing the current science related to physical activity and health and providing recommendations to the HHS to inform the second edition of the PAG. The members of the committee were asked to focus particularly on new results not reflected in the 2008 Physical Activity Guidelines for Americans.6
At the first public meeting, in July 2016, the committee was organized into 9 subcommittees–Aging, Brain Health, Cancer, Cardiometabolic and Weight Management, Exposure, Individuals With Chronic Conditions, Sedentary Behavior, Physical Activity Promotion, and Youth–and began discussing which key topics to address. The Pregnancy and Postpartum Work Group was added later. At the second public meeting, in October 2016, after discussing the scope of the topics to consider, the committee identified and prioritized 38 literature review questions, including 104 subquestions. Working with a contractor, each subcommittee conducted a series of systematic reviews of the scientific literature on the selected questions and began searching for existing meta-analyses and systematic reviews.
At subsequent public meetings, in March, July, and October 2017, the committee deliberated on the findings from each subcommittee, including the evidence grades and conclusions for each question. The committee agreed on a grading system modified from the 2015 Dietary Guidelines Advisory Committee.9 Evidence for each question and subquestion was graded as strong, moderate, limited, or not assignable based on the applicability, generalizability to the US population of interest, risk of bias or study limitations, quantity or consistency of results, and magnitude and precision of effect. The committee summarized its work in an extensive scientific report, the 2018 Physical Activity Guidelines Advisory Committee Scientific Report.4 For each question, the report outlined the methodology used for the literature search, the evidence grades and conclusion statements, public health importance, and research recommendations. The Scientific Report, which was submitted to HHS Secretary Alex Azar in February 2018, concluded the work of the committee.
A federal writing team with expertise in physical activity and public health who supported the committee during its 21-month tenure used the scientific report, along with public and federal agency comments, to draft the second edition of the PAG.5
Key Concepts for the Physical Activity Guidelines
The types and intensity of physical activity are summarized in Box 3.
Box 3. Types and Intensity of Physical Activity.
Aerobic Activity
An activity in which the body’s large muscles move for a sustained amount of time, therefore improving cardiorespiratory fitness. Aerobic activity is also called endurance or cardio activity. Examples include brisk walking, running, or bicycling.
Muscle-Strengthening Activity
An activity that increases skeletal muscle strength, power, endurance, and mass. Examples include weight lifting or resistance training.
Bone-Strengthening Physical Activity
An activity that produces a force on the bones, which promotes bone growth and strength. Examples include jumping rope or running.
Balance Activity
An activity designed to improve individuals’ ability to resist forces within or outside of the body that cause falls while a person is stationary or moving. Examples include lunges or walking backward.
Multicomponent Physical Activity
An activity that includes more than 1 type of physical activity, such as aerobic, muscle strengthening, and balance training. Examples include some dancing or sports.
Absolute Intensity
Refers to the rate of work being performed and does not consider the physiologic capacity of the individual. This is often expressed in metabolic equivalent of task (MET) units. Moderate-intensity physical activities such as walking briskly or raking the yard have a MET level of 3 to 5.9 METs.
Relative Intensity
Takes into account or adjusts for a person’s cardiorespiratory fitness. Someone who is more fit will perceive an exercise to be easier and thus rate it as of lower relative intensity than someone who is less fit.
Types of Physical Activity
Aerobic Activity
In aerobic activity (also called endurance or cardio activity), the large muscles move in a rhythmic manner for a sustained period. Aerobic activity causes the heart rate to increase and breathing to become more labored.
Aerobic physical activity has 3 components: intensity, frequency, and duration. Intensity describes how hard a person works to do the activity. The intensities most often studied are moderate (equivalent in effort to brisk walking) and vigorous (equivalent in effort to running or jogging). Frequency describes how often a person does aerobic activity. Duration describes how long a person does an activity in any 1 session.
Muscle-Strengthening Activity
Muscle-strengthening activities, which include resistance training and weight lifting, cause the body’s muscles to work or hold against an applied force or weight. These activities often involve lifting relatively heavy objects, such as weights, multiple times to strengthen various muscle groups. Muscle-strengthening activity can also involve using elastic bands or body weight for resistance.
Muscle-strengthening activity has 3 components: intensity, frequency, and sets and repetitions. Intensity describes how much weight or force is used relative to how much a person is able to lift. Frequency describes how often a person does muscle-strengthening activity. Sets and repetitions describes how many times a person does the muscle-strengthening activity, like lifting a weight or doing a push-up (comparable to duration for aerobic activity).
The effects of muscle-strengthening activity are limited to the muscles doing the work. It is important to work all the major muscle groups of the body–the legs, hips, back, abdomen, chest, shoulders, and arms.
Bone-Strengthening Activity
Bone-strengthening (also called weight-bearing or weight-loading) activities produce a force on the bones of the body that promotes bone growth and strength. This force is commonly produced by impact with the ground. Bone-strengthening activities can also be aerobic and muscle-strengthening.
Balance Activities
These kinds of activities can improve the ability to resist forces within or outside of the body that cause falls while a person is stationary or moving. Strengthening muscles of the back, abdomen, and legs also improves balance.
Multicomponent Physical Activity
Multicomponent physical activity programs include a combination of balance, muscle-strengthening, and aerobic physical activity. In addition, these programs also may include gait, coordination, and physical function training. Recreational activities such as dancing, yoga, tai chi, gardening, or sports can also be considered multicomponent because they often incorporate multiple types of physical activity.
Physical Activity Intensity
The key guidelines discussed in the next section focus on 2 levels of intensity–moderate-intensity activity and vigorous-intensity activity. The intensity of aerobic activity can be tracked in 2 ways–absolute intensity and relative intensity. Absolute intensity is the amount of energy expended during the activity, without considering a person’s cardiorespiratory fitness or aerobic capacity. Absolute intensity is expressed in metabolic equivalent of task (MET) units; 1 MET is equivalent to the resting metabolic rate or the energy expenditure while awake and sitting quietly. Moderate-intensity activities have a MET value of 3 to 5.9 METs; vigorous-intensity activities have a MET value of 6 or greater.
Examples of moderate-intensity activities (defined using absolute intensity) include walking briskly at 2.5 to 4.0 mph, playing volleyball, or raking the yard. Examples of vigorous-intensity activities include jogging or running, carrying heavy groceries, or participating in a strenuous fitness class. Some activities, such as swimming or riding a bicycle, can be either moderate or vigorous intensity, depending on the effort. Light-intensity physical activity, such as walking slowly at 2 mph or less or doing light household chores, may also provide some health benefits, especially if a person replaces sedentary behavior with light-intensity activity. However, the greatest benefit occurs when sedentary behavior is replaced with moderate-to-vigorous physical activity.
In contrast to absolute intensity, relative intensity is the level of effort required to do an activity compared with a person’s capacity. For an activity of a given absolute intensity, relative intensity will be higher for a person with lower aerobic capacity than for a person who is more fit. Relative intensity can be estimated using a scale of 0 to 10, where sitting is 0 and the highest level of effort possible is 10. On this scale, moderate-intensity activity is a 5 or 6; vigorous-intensity activity begins at a level of 7 or 8.
When describing physical activity to an individual (such as a patient), the “talk test” is helpful to determine whether an activity is moderate or vigorous intensity. Generally, a person doing moderate-intensity aerobic activity can talk, but not sing, during the activity. A person doing vigorous-intensity activity generally cannot say more than a few words without pausing for a breath.
It takes less time to obtain the same benefit from vigorous-intensity activities than from moderate-intensity activities. For adults, a general rule is that 2 minutes of moderate-intensity activity counts the same as 1 minute of vigorous-intensity activity. For example, 30 minutes of moderate-intensity (3-4 METs) activity is roughly the same as 15 minutes of vigorous-intensity (6-8 METs) activity.
Either absolute or relative intensity can be used to monitor progress in meeting the key guidelines described below. Aerobic capacity changes with age, peaking in young adulthood.10 Because older adults generally have a decreased aerobic capacity compared with younger adults, relative intensity is a better guide for older adults than absolute intensity. Certain activities, such as some types of yoga or tai chi, that are considered light intensity on an absolute scale may be perceived as moderate or vigorous intensity for older adults. Children and adults who are inactive or have low fitness levels can also use relative intensity to help determine their level of effort.
Progression and Overload
Whether absolute or relative intensity is used to assess level of effort, for anyone beginning physical activity, walking is usually a good first activity because it does not require special skills or equipment and can generally be done indoors or outside. Over time, physical activity will get easier as the body adapts to performing physical activity that is greater in amount or intensity than usual. People should be encouraged to progress to higher levels of physical activity as they become more fit. People can work toward meeting the key guidelines by increasing the amount of time they perform an activity, the intensity of the activity, or the number of times a week they are physically active. Small, progressive changes in activity level and amount help the body adapt to the additional stresses while minimizing the risk of injury. A health professional or physical activity specialist can help tailor physical activity to meet the needs and goals of individuals.
The Key Guidelines
Strong evidence demonstrates that regular physical activity has health benefits for everyone, regardless of age, sex, race, ethnicity, or body size. Some benefits occur immediately, such as reduced feelings of anxiety, reduced blood pressure, and improved sleep, cognitive function, and insulin sensitivity. Other benefits, such as increased cardiorespiratory fitness, increased muscular strength, decreased depressive symptoms, and sustained reduction in blood pressure, accrue over months or years of physical activity. The key guidelines below highlight the amounts and types of physical activity recommended for 3 age groups (children and adolescents, adults, and older adults), for women who are pregnant or postpartum, and for adults with chronic diseases or adults with disabilities. The PAG also discusses doing physical activity safely.
The PAG has some new features, reflecting the evolution of research summarized in the 2018 Physical Activity Guidelines Advisory Committee Scientific Report.4 For example, the PAG emphasizes increasing the amount of moderate-to-vigorous physical activity and decreasing sitting time for adults. Most people are not meeting the current key guidelines, so shifting from sitting time to being more active, ideally by doing moderate- or even vigorous-intensity physical activity, would have significant health benefits for many people in the United States. Guidance for adults no longer requires physical activity to occur in bouts of at least 10 minutes. Also new in this edition of the PAG is guidance for children younger than 6 years.
The PAG also identifies numerous benefits of physical activity for specific populations, which are listed below.
Physical Activity for Preschool-aged Children
Children younger than 6 years undergo periods of rapid growth and development. Physical activity can enhance growth and development and teach important movement skills. Parents and caregivers can have a critical role in supporting and encouraging young children to be physically active and in modeling participation in regular physical activity (Box 4). Although a quantitative key guideline for daily physical activity is not well defined for this age group, a reasonable target may be 3 hours per day of activity of all intensities: light, moderate, or vigorous. This is the average amount of activity observed among children of this age11,12 and is consistent with guidelines from Canada,13 the United Kingdom,14 and the Commonwealth of Australia.15
Box 4. Key Guidelines for Preschool-aged Children and for School-aged Children and Adolescents.
Preschool-aged Children
Preschool-aged children (3 through 5 years) should be physically active throughout the day to enhance growth and development.
Adult caregivers of preschool-aged children should encourage active play that includes a variety of activity types.
School-aged Children and Adolescents
It is important to provide young people opportunities and encouragement to participate in physical activities that are appropriate for their age, that are enjoyable, and that offer variety.
Children and adolescents aged 6 through 17 years should do 60 minutes (1 hour) or more of moderate-to-vigorous physical activity daily
Aerobic:
Most of the 60 minutes or more per day should be either moderate- or vigorous-intensity aerobic physical activity and should include vigorous-intensity physical activity on at least 3 days a week.
Muscle-strengthening:
As part of their 60 minutes or more of daily physical activity, children and adolescents should include muscle-strengthening physical activity on at least 3 days a week.
Bone-strengthening:
As part of their 60 minutes or more of daily physical activity, children and adolescents should include bone-strengthening physical activity on at least 3 days a week.
Physical Activity for School-aged Children and Adolescents
Childhood and adolescence are critical periods for developing movement skills, learning healthy habits, and establishing a firm foundation for lifelong health and well-being. Similar to younger children, parents and caregivers can have a crucial supportive role to foster positive relationships with physical activity and to encourage and support their children to be active daily. For youth aged 6-17 years, vigorous-intensity, bone-strengthening, and muscle-strengthening physical activities are important components to include on 3 or more days a week (Box 4). Unlike adults, youth typically do not develop chronic diseases, but risk factors such as obesity, elevated insulin and blood lipids levels, and elevated blood pressure can develop in childhood and adolescence. Youth who are regularly active have a better chance of a healthy adulthood by lowering the likelihood that these risk factors will develop, both now and in the future.
Physical Activity for Adults
The link between physical activity and better health is well established in adults. Physical activity has myriad benefits, ranging from those occurring after a single bout of physical activity, to long-term benefits such as reduced risk of development or progression of a chronic condition, to improvement of an existing chronic condition. Most healthy adults do not need to consult a health care professional before beginning physical activity. Starting with low amounts and gradually increasing the amount of time or intensity of physical activity is a good way to build toward meeting the key guidelines (Box 5). Bouts, or episodes, of moderate-to-vigorous physical activity of any duration may be included in the accumulated total volume of physical activity. Benefits continue to accumulate with additional physical activity, and both aerobic and muscle-strengthening physical activity provide important benefits.
Box 5. Key Guidelines for Adults.
Adults should move more and sit less throughout the day. Some physical activity is better than none. Adults who sit less and do any amount of moderate-to-vigorous physical activity gain some health benefits.
For substantial health benefits, adults should do at least 150 minutes (2 hours and 30 minutes) to 300 minutes (5 hours) a week of moderate-intensity, or 75 minutes (1 hour and 15 minutes) to 150 minutes (2 hours and 30 minutes) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Preferably, aerobic activity should be spread throughout the week.
Additional health benefits are gained by doing physical activity beyond the equivalent of 300 minutes (5 hours) of moderate-intensity physical activity a week.
Adults should also do muscle-strengthening activities of moderate or greater intensity that involve all major muscle groups on 2 or more days a week, as these activities provide additional health benefits.
Physical Activity for Older Adults
The benefits of regular physical activity occur throughout life and are essential for healthy aging. Adults 65 years and older gain substantial health benefits from regular physical activity, even if they do not meet the key guidelines. Older adults who are physically active can engage in activities of daily living more easily and have improved physical function (even if they are frail). They are less likely to fall, and if they do fall, the risk of injury is lower. Most older adults spend a substantial portion of their day being sedentary, so the key guidelines start in a similar fashion as those for adults–move more and sit less throughout the day (Box 6). Replacing sitting with light-intensity physical activity or, ideally, moderate-intensity physical activity may provide significant benefits. For older adults, multicomponent physical activity is important. Multicomponent physical activity combines aerobic, muscle-strengthening, and balance exercises. All 3 aspects are important for this population because older adults are at an increased risk of falls, and strength and balance are needed to prevent falls.
Box 6. Key Guidelines for Older Adults.
The key guidelines for adults also apply to older adults. In addition, the following key guidelines are just for older adults:
As part of their weekly physical activity, older adults should do multicomponent physical activity that includes balance training as well as aerobic and muscle-strengthening activities.
Older adults should determine their level of effort for physical activity relative to their level of fitness.
Older adults with chronic conditions should understand whether and how their conditions affect their ability to do regular physical activity safely.
When older adults cannot do 150 minutes of moderate-intensity aerobic activity a week because of chronic conditions, they should be as physically active as their abilities and conditions allow.
Physical Activity During Pregnancy and During Postpartum
Physical activity during pregnancy benefits a woman’s overall health without increasing the risk of adverse pregnancy outcomes, such as low birth weight, preterm delivery, or early pregnancy loss. Benefits include maintenance of, or increases in, cardiorespiratory fitness, reduced risk of excessive weight gain and gestational diabetes, and reduced symptoms of postpartum depression. Some evidence suggests that physical activity may reduce the risk of pregnancy complications such as preeclampsia, reduce the length of labor and postpartum recovery, and reduce the risk of having a cesarean delivery. Pregnant women should be under the care of a health care practitioner (such as a physician, nursing professional, or physician assistant), who can help them to adjust their physical activity levels if needed; most women who were active before becoming pregnant can safety continue their activity level during pregnancy. Key guidelines are described in Box 7.
Box 7. Key Guidelines for Women During Pregnancy and the Postpartum Period.
Women should do at least 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity a week during pregnancy and the postpartum period. Preferably, aerobic activity should be spread throughout the week.
Women who habitually engaged in vigorous-intensity aerobic activity or who were physically active before pregnancy can continue these activities during pregnancy and the postpartum period.
Women who are pregnant should be under the care of a health care practitioner who can monitor the progress of the pregnancy. Women who are pregnant can consult their health care practitioner about whether or how to adjust their physical activity during pregnancy and after the child is born.
Physical Activity for Adults With a Chronic Health Condition or a Disability
Regular physical activity is recommended for adults with a chronic health condition or a disability and can provide both physical and cognitive benefits. For many chronic conditions, physical activity provides therapeutic benefits and is part of recommended treatment for the condition (Box 8). The benefits of physical activity for people with disabilities have been studied in diverse groups with disabilities related to traumatic events or to chronic health conditions. These groups include people with previous stroke, spinal cord injury, multiple sclerosis, Parkinson disease, muscular dystrophy, cerebral palsy, traumatic brain injury, limb amputations, mental illness, intellectual disability, and Alzheimer disease and other dementias. If possible, those with a chronic condition or disability should try to meet the adult key guidelines. However, the type and amount of physical activity should be determined by a person’s abilities and the severity of the chronic condition or disability, which may change over time. Health care professionals and physical activity specialists can support and guide patients in choosing appropriate types and amounts of physical activities for their abilities.
Box 8. Key Guidelines for Adults With Chronic Health Conditions and Adults With Disabilities.
Adults with chronic conditions or disabilities, who are able, should do at least 150 minutes (2 hours and 30 minutes) to 300 minutes (5 hours) a week of moderate-intensity, or 75 minutes (1 hour and 15 minutes) to 150 minutes (2 hours and 30 minutes) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Preferably, aerobic activity should be spread throughout the week.
Adults with chronic conditions or disabilities, who are able, should also do muscle-strengthening activities of moderate or greater intensity that involve all major muscle groups on 2 or more days a week, as these activities provide additional health benefits.
When adults with chronic conditions or disabilities are not able to meet the above key guidelines, they should engage in regular physical activity according to their abilities and should avoid inactivity.
Adults with chronic conditions or symptoms should be under the care of a health care practitioner. People with chronic conditions can consult a health care professional or physical activity specialist about the types and amounts of activity appropriate for their abilities and chronic conditions.
Physical Activity and Risk of Injury
Physical activity is safe for almost everyone, and the health benefits of physical activity outweigh the risks for most people. Injuries can occur, but individuals can minimize the risk of injury by wearing protective equipment and gear, choosing safe environments in which to be physically active, following rules and policies that promote safety, and making sensible choices about when and how to be active (Box 9). People who are physically fit have a lower risk of injury than people who are not. Therefore, engaging in regular physical activity over time can reduce risk of injury. It is also recommended that physical activity be gradually increased over time through increasing the frequency, duration, or intensity to minimize the risk of injury.
Box 9. Key Guidelines for Safe Physical Activity.
To do physical activity safely and reduce risk of injuries and other adverse events, people should
Understand the risks, yet be confident that physical activity can be safe for almost everyone.
Choose types of physical activity appropriate for their current fitness level and health goals, because some activities are safer than others.
Increase physical activity gradually over time to meet key guidelines or health goals. Inactive people should “start low and go slow” by starting with lower-intensity activities and gradually increasing how often and how long activities are done.
Protect themselves by using appropriate gear and sports equipment, choosing safe environments, following rules and policies, and making sensible choices about when, where, and how to be active.
Be under the care of a health care practitioner if they have chronic conditions or symptoms. People with chronic conditions and symptoms can consult a health care professional or physical activity specialist about the types and amounts of activity appropriate for them.
Promoting Physical Activity
In addition to providing specific recommendations for health-enhancing physical activity, the PAG also addresses evidence-based strategies to promote and support physical activity. These strategies include those that focus on individuals or small groups as well as programs and policies that can make physical activity easier for entire communities. Of particular relevance for health care professionals is evidence that groups led by professionals or peers can help improve physical activity levels. These groups usually incorporate some form of counseling or guidance from a health professional or physical activity specialist to help participants set physical activity goals, monitor their progress toward these goals, seek social support to maintain physical activity, and use self-reward and positive self-talk to reinforce progress. They also use structured problem solving to prevent relapse to a less active lifestyle. To reduce staff burden and costs, groups can also be led by trained peers who deliver the intervention in full or in part and often share similar characteristics or experiences as group members. Youth, adults, and older adults can benefit from individual or group approaches as well as community-level programs, practices, and policies to achieve an active lifestyle. The role of health care professionals in community approaches is discussed below.
Technology, such as step counters or other wearable devices or fitness apps, can provide physical activity feedback directly to the user. Technology can be used alone or combined with other strategies, such as goal setting and coaching, to encourage and maintain increased physical activity. Technological approaches can also be used to provide guidance remotely to individuals through text messaging, by telephone, or through the internet. Telephone and internet delivery strategies can offer guidance to individuals from trained peers or through interactive voice-response systems.
Discussion
The PAG5 represents a significant evolution from the 2008 Physical Activity Guidelines for Americans.6 The scientific evidence for the health benefits of being physically active has continued to expand beyond primary prevention of chronic disease, with new evidence of benefits for multiple aspects of brain health, healthy development of preschool children, and benefits for persons with chronic disease or various disabilities. In addition, new evidence about the interrelationship between sedentary behavior and physical activity has expanded understanding of the importance of being active throughout the day.
New evidence also shows that obtaining health benefits associated with physical activity may be easier than previously thought. A single episode of moderate-to-vigorous physical activity can improve sleep, reduce anxiety symptoms, improve cognition, reduce blood pressure, and improve insulin sensitivity on the day the activity is performed. Most of these improvements increase, and additional benefits occur, with the regular performance of moderate-to-vigorous physical activity.
A significant change since the 2008 Physical Activity Guidelines for Americans6 is that previously, aerobic physical activity for adults had to be accumulated in bouts, or sessions, that lasted at least 10 minutes to count toward meeting the key guidelines. Current evidence shows that the total volume of moderate-to-vigorous physical activity is related to many health benefits; bouts of a prescribed duration are not essential. This finding is consistent with the type of recommendations made to increase routine daily physical activity, such as parking farther away from a destination and walking, or taking the stairs rather than the elevator, and will allow health care professionals to promote small increases in physical activity that do not take 10 minutes. These small changes can contribute to providing increases in health-enhancing physical activity.
Sedentary behavior has recently become a topic of considerable interest. The PAG addresses the risks of too much sitting for adults but does not prescribe a quantitative key guideline for sitting time or how to break up sitting duration throughout the day. This is because recent evidence shows a complex relationship between the effects of sitting time and duration of moderate-to-vigorous physical activity on all-cause and cardiovascular disease mortality.4 With greater amounts of moderate-to-vigorous physical activity, the risk of a given amount of sitting time is reduced. However, given the low amount of moderate-to-vigorous physical activity currently performed by most people in the United States, increasing physical activity and decreasing sitting are both likely to provide benefits.
Physicians and other health care professionals are members of the key audience for the PAG and are ideally situated to facilitate awareness of the PAG and to promote the health benefits of physical activity. Many of the target populations of the PAG–pregnant women, preschool and school-aged children and adolescents, older adults, and persons with chronic diseases or disabilities–have regular health care encounters that provide opportunities to inquire about and promote physical activity. Many tools and resources are available to help facilitate physical activity counseling, such as the American Academy of Pediatrics’ Bright Futures Guidelines16 and the Exercise Is Medicine Healthcare Providers’ Action Guide.17 Large health care systems, including Kaiser Permanente, Intermountain Healthcare, and Greenville Health System, have incorporated monitoring physical activity as a vital sign.18-20
Health care professionals can also partner with other sectors to promote physical activity. The 2016 National Physical Activity Plan21 identified 9 sectors of society that have a role to play in promoting physical activity (Table). For example, health care professionals can link patients or clients to physical activity programs within the Community, Recreation, Fitness, and Parks sector. Implementing population-level approaches to improve physical activity requires collaboration across these sectors at local, state, and national levels. Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities22 addresses how partnerships can be used to promote walking, an easy and common physical activity that most people can perform. Although all groups can benefit from efforts to make physical activity easier, attention to underserved groups or those with barriers to physical activity is particularly needed.
Table.
Sectors in the 2016 National Physical Activity Plan (NPAP) and Their Potential Role in Supporting Physical Activity
| NPAP Sector | Role |
|---|---|
| Business and industry | Employers can encourage workers to be physically active. They can provide access to facilities and encourage their use through outreach activities. Businesses can consider access to opportunities for active transportation and public transit when selecting new locations. |
| Community, recreation, fitness, and parks | This sector plays a leading role in providing access to places for active recreation, such as playgrounds, hiking and biking trails, senior centers, sports fields, and swimming pools. This sector can also provide access to exercise programs and equipment for a broad range of people, including underserved populations and people with disabilities. |
| Education | This sector can take a lead role in providing opportunities for age-appropriate physical activity in all educational settings. Opportunities include offering physical education, after-school sports, and public access to school facilities during after-school hours, and expanded intramural sports and campus recreation opportunities. |
| Faith-based settings | Faith-based organizations can be important partners in providing access to places for physical activity and promotion through outreach activities that can be tailored for diverse faith-based groups. |
| Health care | Health care professionals can assess, counsel, and advise patients on physical activity and how to do it safely. Health care systems can partner with other sectors to promote access to community-based physical activity programs. |
| Mass media | Media outlets can provide easy-to-understand messages about the health benefits of physical activity as part of community promotion efforts. Messages can also provide information about facilities or outlets where individuals can be active. |
| Public health | Public health departments can monitor community progress in providing places and opportunities to be physically active and track changes in the proportion of the population meeting the Physical Activity Guidelines for Americans. They can also take the lead in setting objectives and coordinating activities among sectors. Public health departments and organizations can disseminate appropriate messages and information to the public about physical activity. |
| Sports | This sector can provide organized opportunities for people to be active. Youth sports can expose children and adolescents to a variety of age-appropriate activities that can set the basis for a lifetime of activity. Sports organizations can also ensure that sports programs are conducted in a manner that minimizes risk of injuries. |
| Transportation, land use, and community design | This sector plays a lead role in designing and implementing options that provide areas for safe walking, bicycling, and wheelchair walking. Public transit systems also promote walking, as people typically walk to and from transit stops. Community planners and designers can implement design principles to create communities with activity-friendly routes to everyday destinations for people of all ages and abilities. They can also help create or improve access to places for physical activity, such as parks and other green spaces. |
The federal government provides a number of resources to support individuals, organizations, and sectors in promoting physical activity. A list of useful websites is provided in the Appendix of the PAG5 and at https://health.gov/paguidelines. Communication tools to support and disseminate PAG messages are also available at this website.
Realizing a shared vision of a more physically active and healthy United States will require dedication, ingenuity, skill, and commitment from many partners working across many different sectors. As clearly demonstrated by the scientific evidence supporting the PAG, being physically active is one of the best investments individuals and communities can make in their health and welfare. Now is the time to take action and help more individuals in the United States attain the numerous benefits of physical activity.
Conclusions
The Physical Activity Guidelines for Americans, 2nd edition, provides information and guidance on the types and amounts of physical activity that provide substantial health benefits. Health professionals and policy makers should facilitate awareness of the guidelines and promote the health benefits of physical activity and support efforts to implement programs, practices, and policies to facilitate increased physical activity and to improve the health of the US population.
Funder/Sponsor:
This study was funded by the US Department of Health and Human Services (HHS).
Role of the Funder/Sponsor:
The HHS is responsible of all aspects of the development of the Physical Activity Guidelines for Americans, 2nd edition (PAG). This includes appointing an advisory committee, funding contracts for the advisory committee literature review, and writing the PAG. HHS had no role in the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
Contributor Information
Katrina L. Piercy, Office of Disease Prevention and Health Promotion, US Department of Health and Human Services, Rockville, Maryland.
Richard P. Troiano, National Cancer Institute, National Institutes of Health, US Department of Health and Human Services, Bethesda, Maryland.
Rachel M. Ballard, Office of Disease Prevention, National Institutes of Health, US Department of Health and Human Services, Bethesda, Maryland.
Susan A. Carlson, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, US Department of Health and Human Services, Atlanta, Georgia.
Janet E. Fulton, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, US Department of Health and Human Services, Atlanta, Georgia.
Deborah A. Galuska, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, US Department of Health and Human Services, Atlanta, Georgia..
Stephanie M. George, Office of Disease Prevention, National Institutes of Health, US Department of Health and Human Services, Bethesda, Maryland.
Richard D. Olson, Office of Disease Prevention and Health Promotion, US Department of Health and Human Services, Rockville, Maryland.
REFERENCES
- 1.Carlson SA, Adams EK, Yang Z, Fulton JE. Percentage of deaths associated with inadequate physical activity in the United States. Prev Chronic Dis. 2018;15:E38. doi: 10.5888/pcd18.170354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carlson SA, Fulton JE, Pratt M, et al. Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis. 2015;57(4):315–323. doi: 10.1016/j.pcad.2014.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: US Dept of Health and Human Services; 2018. [Google Scholar]
- 5.US Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. Wasington, DC: US Dept of Health and Human Services; 2018. [Google Scholar]
- 6.US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: US Dept of Health and Human Services; 2008. [Google Scholar]
- 7.Office of Disease Prevention and Health Promotion, US Dept of Health and Human Services. Healthy People 2020: Topics & Objectives–Physical Activity. HealthyPeople.gov website. https://www.healthypeople.gov/2020/topics-objectives/topic/physical-activity. Updated September 13, 2018. Accessed September 13, 2018. [Google Scholar]
- 8.Office of Disease Prevention and Health Promotion, US Dept of Health and Human Services. Healthy People 2020: Data Search–Physical Activity. HealthyPeople.gov website. https://www.healthypeople.gov/2020/data-search/search-the-data#topic-area=3504. Updated September 13, 2018. Accessed September 13, 2018. [Google Scholar]
- 9.Dietary Guidelines Advisory Committee; Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. Washington, DC: US Dept of Agriculture, Agricultural Research Service; 2015. [Google Scholar]
- 10.American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 7th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 11.Pate RR, O’Neill JR. Physical activity guidelines for young children: an emerging consensus. Arch Pediatr Adolesc Med. 2012;166(12):1095–1096. doi: 10.1001/archpediatrics.2012.1458 [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine. Early Childhood Obesity Prevention Policies. Washington, DC: National Academies Press; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Canadian Society for Exercise Physiology (CSEP). Canadian 24-hour movement guidelines for the early years (0-4 years): an integration of physical activity, sedentary behaviour and sleep. CSEP; website. http://csepguidelines.ca/early-years-0-4/. 2018. Accessed August 16, 2018. [Google Scholar]
- 14.Department of Health, Physical Activity, Health Improvement and Protection. Start Active, Stay Active: A Report on Physical Activity for Health From the Four Home Countries’ Chief Medical Officers. London, United Kingdom: Dept of Health, Physical Activity, Health Improvement and Protection; 2011. [Google Scholar]
- 15.Commonwealth of Australia. National Physical Activity Guidelines for Australians: Physical Activity Recommendations for 0-5 Year Olds. Canberra: Commonwealth of Australia; 2010. [Google Scholar]
- 16.Hagan J, Shaw J, Duncan P. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 17.American College of Sports Medicine. Exercise Is Medicine: Healthcare Providers’ Action Guide. Indianapolis, IN: American College of Sports Medicine; 2014. [Google Scholar]
- 18.Kaiser Permanente. Exercise as a vital sign. Kaiser Permanente Center for Total Health website. https://centerfortotalhealth.org/exercise-vital-sign. May 18, 2017. Accessed August 6, 2018. [Google Scholar]
- 19.Schroder MO. Treating exercise as a vital sign: why some health providers are asking about physical activity, and how to join the discussion. US World News & World Report. https://health.usnews.com/health-care/articles/2016-11-15/treating-exercise-as-a-vital-sign. Published November 15, 2016. Accessed August 6, 2018. [Google Scholar]
- 20.Ball TJ, Joy EA, Gren LH, Shaw JM. Concurrent validity of a self-reported physical activity “vital sign” questionnaire with adult primary care patients. Prev Chronic Dis. 2016;13:E16. doi: 10.5888/pcd13.150228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Physical Activity Plan Alliance. US National Physical Activity Plan. National Physical Activity Plan Alliance; website. http://physicalactivityplan.org/docs/2016NPAP_Finalforwebsite.pdf. Published 2016. Accessed September 25, 2018. [Google Scholar]
- 22.US Dept of Health and Human Services. Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities. Washington, DC: US Dept of Health and Human Services, Office of the Surgeon General; 2015. [PubMed] [Google Scholar]