Abstract
Background
Although non-motor symptoms of Parkinson’s disease (PD) are serious, effective treatments are still lacking. Acupuncture may have clinical benefits for non-motor symptoms of PD patients, but high-quality evidence supporting this possibility is still limited. Hence, we conducted this meta-analysis to evaluate the effect of acupuncture treatment on non-motor symptoms in patients with PD.
Methods
Randomized controlled trials (RCTs) of acupuncture treatment for PD were retrieved from the following electronic databases: Medline (OVID), Embase (OVID), Cochrane Library, Web of Science, China National Knowledge Infrastructure, Chinese BioMedical Literature Database, Chonqing VIP (CQVIP), and Wangfang database. Studies evaluating non-motor symptoms of PD were retrieved. Methodological quality was assessed using the Cochrane Handbook for Systematic Reviews of Interventions.
Results
A total of 27 RCTs were included, among which 8 outcomes related to non-motor symptoms were evaluated. The results showed that acupuncture combined with medication had benefits for PD-related insomnia relative to medication alone or sham acupuncture [standardized mean difference (SMD) = 0.517; 95% confidence interval (CI) = 0.242–0.793; p = 0.000], and acupuncture treatment had benefits at 8 weeks (SMD = 0.519; 95% CI = 0.181–0.857; p = 0.003). Regarding depression, acupuncture treatment was more effective (SMD = −0.353; 95% CI = −0.669 to −0.037; p = 0.029) within 2 months (SMD = −0.671; 95% CI = −1.332 to −0.011; p = 0.046). Regarding cognition, quality of life, and Unified Parkinson’s Disease Rating Scale (UPDRS) I and II scores, acupuncture treatment was effective [SMD = 0.878, 95% CI = 0.046–1.711, p = 0.039; SMD = −0.690, 95% CI = −1.226 to −0.155, p = 0.011; weighted mean difference (WMD) = −1.536, 95% CI = −2.201 to −0.871, p = 0.000; WMD = −2.071, 95% CI = −3.792 to −0.351, p = 0.018; respectively]. A significant difference was not found in terms of PD-related constipation. Only one study evaluated PD-related fatigue.
Conclusion
The results of the analysis suggested that acupuncture treatment could ameliorate the symptoms of depression, quality of life, cognition, total mentation, behavior and mood, and activities of daily living in PD patients. Nevertheless, more prospective, well-designed RCTs with larger sample sizes are required to confirm our findings.
Keywords: Parkinson’s disease, non-motor symptoms, acupuncture, meta-analysis, randomized controlled trial
Introduction
Parkinson’s disease (PD) is a neurodegenerative disorder characterized by a myriad of motor symptoms and non-motor symptoms affecting approximately 6.1 million individuals worldwide in 2016, 2.4 times higher than in 1990 (GBD 2016 Neurology Collaborators, 2019). The duration of symptoms can span decades, and the accumulating disability can lower quality of life. For society, PD has caused a global burden, especially in terms of deaths and disability, which has been rapidly rising in the past two decades (Deuschl et al., 2020). Therapies such as dopamine agonists and dopaminergic medications are the most effective therapies for PD but have a limited effect on non-motor symptoms (Kim et al., 2009; Connolly and Lang, 2014; Armstrong and Okun, 2020). In addition, non-motor symptoms have often been neglected in clinical practice, although some researchers in the last decade have called for more attention because they are the main key to quality of life of patients (Poewe, 2010; Asakawa et al., 2016; Chaudhuri and Sauerbier, 2016). Some non-motor symptoms of PD patients precede the motor symptoms by several years, are present early in the disease course and could be the drivers of significant disability as the disease progresses (Haehner et al., 2007; Seppi et al., 2019; Gilbert and Khemani, 2022). Moreover, some researchers have emphasized the disparities between the need for treatment for non-motor symptoms and the lack of clinical trial data evaluating these symptoms (Zesiewicz et al., 2010). Although the number of convincing studies have been increasing in recent years, evidence-based treatments remain limited (Seppi et al., 2019). Therefore, it is important to prioritize the development of an analysis of the management of non-motor symptoms.
Non-motor symptoms of PD include symptoms such as constipation, fatigue, cognitive impairment, and sleep and affective disturbances. Symptomatic therapies for non-motor symptoms of PD are similar to those for general populations (those without PD), while evidence for the efficacy of these therapies, specifically in individuals affected by PD varies (Armstrong and Okun, 2020). Multidisciplinary approaches and non-pharmacologic treatment strategies have been encouraged (Goldman and Guerra, 2020; Bloem et al., 2021). Acupuncture as a non-invasive procedure and an alternative therapy has received increasing attention in recent years. Accumulating studies investigating the effectiveness of acupuncture targeting PD or other disorders, such as depression, insomnia, cognitive impairment and so on, have had some positive results (Lee and Lim, 2017; Goldman and Guerra, 2020; Yeung et al., 2021). However, high-quality evidence supporting significant effects of acupuncture on non-motor symptoms of PD is lacking. Therefore, we carried out a meta-analysis of randomized controlled trials (RCTs) to reach a solid conclusion with a larger sample size. We aimed to determine the effects of acupuncture on the non-motor symptoms of PD and provide evidence-based recommendations for PD patients with non-motor symptoms.
Materials and methods
This meta-analysis (registration No. CRD42022295938) focused on RCTs involving acupuncture and acupuncture combined with medication interventions on non-motor symptoms in PD patients, which abided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Page et al., 2021).
Search strategy
We searched Medline (OVID), Embase (OVID), the Cochrane Library, Web of Science, China National Knowledge Infrastructure (CNKI), Chinese BioMedical Literature Database (CBM), Chonqing VIP (CQVIP), and Wangfang database from their inception through November 2021. Databases were searched using three main components: disease (PD), intervention (acupuncture), and study type (randomized clinical trial). The complete search strategy is shown in Supplementary Appendix.
Inclusion criteria/exclusion criteria
Articles meeting the following criteria were included: (1) population: patients diagnosed as PD using any recognized diagnostic criteria (UK Parkinson’s Disease Society Brain Bank Criteria for the diagnosis of PD) (Hughes et al., 2001), MDS clinical diagnostic criteria for PD (Postuma et al., 2015), diagnostic criteria for PD in China (2016) (Parkinson’s Disease and Movement Disorders Group of Neurology Branch of Chinese Medical Association, 2016); (2) intervention: acupuncture treatment including acupuncture alone or acupuncture combined with conventional treatment; (3) comparators: no treatment, sham acupuncture, sham acupuncture combined with conventional treatment or conventional treatment alone (conventional treatment included Antiparkinson drug and other drugs for the non-motor symptoms of PD); (4) outcome measure: involving some metric related to non-motor symptoms, for instance: the primary outcomes of this meta-analysis were insomnia [assessed by the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989) and Parkinson’s Disease Sleep Scale (PDSS) (Chaudhuri et al., 2002)], depression [assessed by the Hamilton Depression Scale (HAMD) (Hamilton, 1980) and Hospital Anxiety Depression Scale (HADS, depression)] (Zigmond and Snaith, 1983), cognition [measured by the Montreal Cognitive Assessment (MoCA)] (Nasreddine et al., 2005), constipation and fatigue as non-motor outcomes. Unified Parkinson’s Disease Rating Scale (UPDRS) I and II scores (Ramaker et al., 2002), evaluating behavioral and emotional problems and activities of daily living, respectively, were used as secondary outcome indices. Quality of life [the Parkinson’s Disease Questionnaire (PDQ-39)] was also assessed and included as a secondary outcome index; (5) study design: randomized control trials. And language was not restricted.
Studies were excluded if they reported only the response rate or did not have data available for effect size estimates. Duplicate or secondary publications on the same sample were excluded. Conference abstracts, protocols or presentations were also excluded. Two authors (XW and ML) screened the articles on the basis of titles and abstracts. If they could not determine eligibility of a study through this procedure, they selected the article for a subsequent full-text assessment.
Data extraction
Two reviewers (LZ and ZL) extracted and checked the data, and disagreements were resolved by a third-party expert (C W). Clinical characteristics (population, interventions, comparators, and outcome measures), details of the interventions and comparators, time points of measurement and the results before and after the treatments were extracted from each article.
Quality assessment
Two reviewers (QL and XH) independently assessed the quality of the included trials using the revised Cochrane risk of bias, version 2 (RoB 2) tool (Sterne et al., 2019). Disagreements were settled by discussion with another reviewer, CW. Each trial was assessed as having a low or high or some concerns of bias in terms of randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, selection of the reported result.
Statistical analysis
Data were synthesized and analyzed through STATA (version 13). We calculated I2 statistics and Q statistics to determine which effect model was appropriate (Higgins et al., 2003). If the p-value was ≤0.05 or I2 was >40%, this was taken as an indicator of notable heterogeneity among the trials, and a random effect model was chosen (Deeks et al., 2022). The sources of heterogeneity were further explored using subgroup analyses. If the p-value was greater than 0.05 or I2 was no more than 40%, indicating that heterogeneity was low, a fixed effects model was applied. The weighted mean difference (WMD) or standardized mean difference (SMD) with 95% confidence intervals (CIs) was calculated to analyze continuous outcomes. If the assessment tool was the same, WMD was applied to analyze continuous data; otherwise, SMD was used. If necessary, sensitivity analyses were performed to test the stability of the results. Moreover, the risk of publication bias was evaluated by funnel plots or Egger’s test.
Results
Study identification and selection
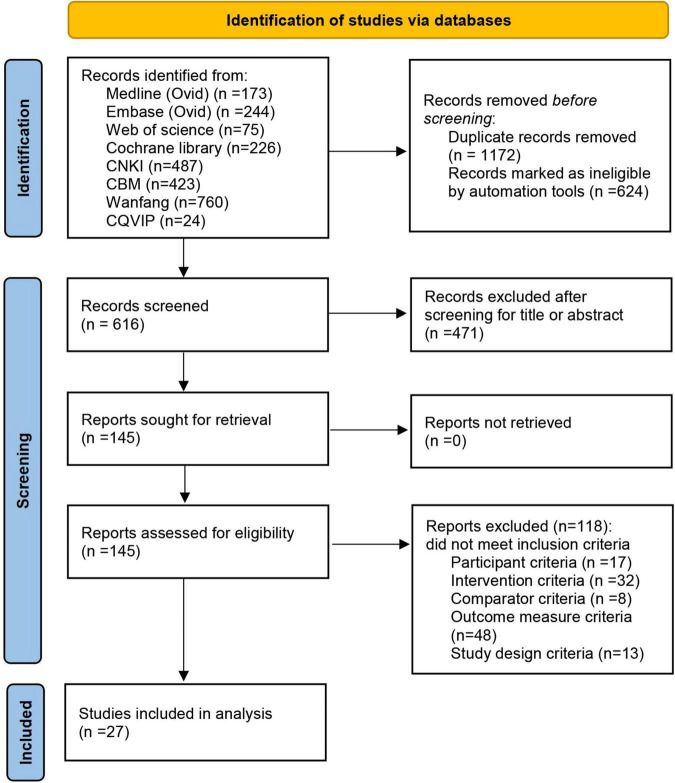
In total, 2,412 potentially eligible articles were identified through database searches, from which 1,172 duplicate articles were removed. After screening the titles and abstracts, we selected 145 articles for full-text dual review after excluding 1,095 articles on the basis of the inclusion criteria. A total of 118 of 145 articles were excluded, and the detailed reasons are shown in the flow diagram (Figure 1). Finally, 27 articles were included in this meta-analysis (Yang, 2009; Cho et al., 2012, 2018; Xia et al., 2013; Liang, 2014; Chen, 2015; Toosizadeh et al., 2015; Wang et al., 2015, 2019; Kluger et al., 2016; Li, 2016; Tian et al., 2016; Zhou et al., 2016; Aroxa et al., 2017; Dong et al., 2018; Li L. et al., 2018; Li Z. et al., 2018; Liu et al., 2018; Luo and Zhang, 2019; Zhan and Wang, 2019; Li et al., 2020, 2021; Wu, 2020; Xu et al., 2020; Yuan et al., 2020; Zhang, 2020; Wu et al., 2021). The specific screening procedure is summarized in Figure 1.
FIGURE 1.
Flowchart.
Study characteristics
Among the 27 eligible articles, 9 studies focused on insomnia (Liang, 2014; Wang et al., 2015; Kluger et al., 2016; Zhou et al., 2016; Aroxa et al., 2017; Dong et al., 2018; Wu, 2020; Xu et al., 2020; Li et al., 2021), 9 studies focused on depression (Cho et al., 2012, 2018; Xia et al., 2013; Wang et al., 2015; Kluger et al., 2016; Tian et al., 2016; Xu et al., 2020; Yuan et al., 2020; Li et al., 2021), 5 studies focused on cognition (Liang, 2014; Wang et al., 2015, 2019; Kluger et al., 2016; Wu et al., 2021), 4 studies focused on constipation (Li L. et al., 2018; Luo and Zhang, 2019; Zhan and Wang, 2019; Zhang, 2020), one study focused on fatigue (Kluger et al., 2016), 9 studies focused on quality of life (Yang, 2009; Cho et al., 2012, 2018; Liang, 2014; Chen, 2015; Kluger et al., 2016; Li, 2016; Liu et al., 2018; Li et al., 2020), 9 studies focused on UPDRS I scores (Yang, 2009; Cho et al., 2012; Chen, 2015; Toosizadeh et al., 2015; Li L. et al., 2018; Luo and Zhang, 2019; Wang et al., 2019; Xu et al., 2020; Yuan et al., 2020) focused on UPDRS I, and 12 studies focused on UPDRS II scores (Yang, 2009; Cho et al., 2012, 2018; Liang, 2014; Chen, 2015; Toosizadeh et al., 2015; Li, 2016; Li L. et al., 2018; Li Z. et al., 2018; Luo and Zhang, 2019; Wang et al., 2019; Xu et al., 2020). A total of 23 studies used a 2-group parallel design, 3 of which compared real acupuncture with sham acupuncture, 7 of which compared acupuncture with conventional treatments, and 13 of which compared the combination of acupuncture and conventional treatments (such as Madopar or Levodopa) with conventional treatments. A total of four studies used a three-arm study design. The parameters of electroacupuncture involved a continuous wave and dilatational wave, and the frequency varied from 1.5 to 100 Hz. The acupuncture intervention duration ranged from 15 to 40 min per session, with one to seven sessions per week. The intervention courses ranged from 4 to 24 weeks. A total of 2 studies were completed in America, 2 in Korea, 1 in Brazil, and the remaining 22 in China. The details of the study characteristics are exhibited in Table 1.
TABLE 1.
Basic characteristics.
| References | Study population | Intervention | Control 1 | Control 2 | Outcomes measured | Measurement time points |
| Li L. et al., 2018 | PD H-Y stage 1–3 | Electroacupuncture Freq: dilatational wave 2/15 Hz, once/d Duration: 30 min Course: 4 w |
Polyethylene glycol | UPDRS I, UPDRS II, anal rectum dynamics | 4 w | |
| Luo and Zhang, 2019 | PD (H-Y stage not mentioned) | Electroacupuncture Freq: continuous wave 1.5 Hz, once/d Duration: 20 min Course: 4 w |
Phenolphthalein tablets | UPDRS I, UPDRS II, anal rectum dynamics | 4 w | |
| Zhan and Wang, 2019 | PD (H-Y stage not mentioned) | Acupuncture Freq: once/d, 6 d/w Duration: 40 min Course: 8 w |
Maren Wan | BSFS, PAC-QOL | 8 w | |
| Zhang, 2020 | PD (H-Y stage not mentioned) | Acupuncture Freq: 3 times/w Duration: 30 min Course: 4 w |
Maren soft capsules | PAC-QOL, Bristol | 4 w | |
| Aroxa et al., 2017 | PD H-Y stage 1–3 | Acupuncture + Antiparkinson drug Freq: 8 times/w Duration: 30 min Course: 8 w |
Antiparkinson drug | PDSS, MMSE | 8 w | |
| Wang et al., 2015 | PD (H-Y stage not mentioned) | Acupuncture + Antiparkinson drug Freq: 100 Hz, 3 d/time Duration: 30 min Course: 2 m |
Antiparkinson drug | PSQI, HAMD, MMSE, MoCA, | 2 m | |
| Xu et al., 2020 | PD H-Y stage 1–4 | Electroacupuncture + Levodopa and Benserazide Freq: continuous waves 100 Hz, 4 times/week Duration: 30 min Course: 8 w |
Levodopa and Benserazide | UPDRS I, UPDRS II, PDSS, SDS | 4, 8, 12 w | |
| Dong et al., 2018 | PD H-Y stage 1–3 | Electroacupuncture Freq: continuous waves 2 Hz, once/day Duration: 30 min Course: 30 d |
Madopar | PDSS | 30 d | |
| Li et al., 2021 | PD (H-Y stage not mentioned) | Electroacupuncture + Madopar Freq: dilatational wave 2/15 Hz, once/d Duration: 30 min Course: 8 w |
Madopar | PDSS, PSQI, SDS, UPDRS | 8 w | |
| Wu, 2020 | PD H-Y stage 1.5–4 | Acupuncture Freq: once/day, 6 times/week Duration: 40 min Course: 4 w |
Estazolam | PDSS, PSQI | 4 w | |
| Zhou et al., 2016 | PD (H-Y stage not mentioned) | Electroacupuncture + Madopar Freq: continuous waves 2 Hz, once/d Duration: 20 min Course: 8 w |
Madopar | PDSS, UPDRS II | 8 w | |
| Kluger et al., 2016 | PD (H-Y stage not mentioned) | Acupuncture Freq: twice/week Duration: 30 min Course: 6 w |
Sham acupuncture | MFIS, HADS depression, PDSS, PDQ-39 | 6 w | |
| Cho et al., 2018 | PD H-Y stage 1–4 | Acupuncture Freq: twice/week Duration: 15 min Course: 12 w |
Sham acupuncture | Antiparkinson drug | BDI, PDQL, UPDRS II | 12 w |
| Chen, 2015 | PD H-Y stage 1–5 | Acupuncture + Madopar Freq: 2 consecutive d, followed by a 2-d rest Duration: 30 min Course: 24 w |
Madopar | UPDRS I, UPDRS II | 24 w | |
| Li et al., 2020 | PD H-Y stage 1–4 | Electroacupuncture + Antiparkinson drug Freq: 10/50 Hz, 3 times/w Duration: 30 min Course: 12 w |
Antiparkinson drug | PDQ-39 | 8, 12 w | |
| Li, 2016 | PD H-Y stage 1–3 | Acupuncture + Antiparkinson drug Freq: 2 times/w Duration: 30 min Course: 12 w |
Antiparkinson drug | Sham acupuncture + Antiparkinson drug | UPDRS II, PDQ-39 | 4, 8, 12 w |
| Liang, 2014 | PD H-Y stage 1–3 | Acupuncture Freq: every other day, 3 times/w Duration: 30 min Course: 6 m |
Madopar | PDQ-39, PDSS, UPDRS II | 1, 3, 6 m | |
| Liu et al., 2018 | PD H-Y stage 1–3 | Electroacupuncture + compound Carbidopa tablet Freq: continuous waves, 1.5 Hz, once/d Duration: 20 min Course: 3 m |
Compound Carbidopa tablet | PDQ-39 | 3 m | |
| Yang, 2009 | PD (H-Y stage not mentioned) | Acupuncture Freq: 5 times/w Duration: 30 min Course: 4 w |
Madopar | UPDRS I, UPDRS II | 4 w | |
| Cho et al., 2012 | PD (H-Y stage not mentioned) | Acupuncture Freq: twice/w Duration: 20 min Course: 8 w |
Not treatment | UPDRS I, UPDRS II, PDQL, BDI | 8 w | |
| Tian et al., 2016 | PD (H-Y stage not mentioned) | Electroacupuncture + Madopar and Fluoxetine Freq: dilatational wave, every other 2 d Duration: 30 min Course: 3 m |
Madopar and Fluoxetine | HAMD17 | 3 m | |
| Xia et al., 2013 | PD (H-Y stage not mentioned) | Electroacupuncture + Madopar and Fluoxetine Freq: dilatational wave, every other day Duration: 30 min Course: 3 m |
Madopar and Fluoxetine | HAMD17 | 3 m | |
| Yuan et al., 2020 | PD (H-Y stage not mentioned) | Acupuncture Freq: once/d, every other day Duration: 30 min Course: 3 m |
Escitalopram Oxalate | HAMD17, UPDRS I | 3 m | |
| Toosizadeh et al., 2015 | PD (H-Y stage not mentioned) | Electroacupuncture Freq: 4/100 Hz, once/w Duration: 30 min Course: 3 w |
Sham acupuncture | UPDRS I, UPDRS II | 3 w | |
| Wang et al., 2019 | PD (H-Y stage not mentioned) | Acupuncture + Madopar Freq: once/d Duration: 30 min Course: 30 days |
Acupuncture | Madopar | UPDRS I, UPDRS II, MMSE, MoCA | 30 d |
| Li Z. et al., 2018 | PD H-Y stage 1–3.5 | Acupuncture + Levodopa Duration: 30 min Course: 12 w |
Sham acupuncture + Levodopa | Levodopa | UPDRS II | 12 w |
| Wu et al., 2021 | PD H-Y stage 2–3 | Acupuncture + Madopar Freq: once/d, 5 times/w Duration: 30 min Course: 12 w |
Madopar | MoCA | 12 w |
BDI, Beck Depression Rating Scale; BSFS, Bristol Stool Form Scale; d, day; m, months; H-Y, Hoehn–Yahr; MFIS, Modified Fatigue Impact Scale; min, minute; MMSE, Mini-Mental State Examination; PAC-QOL, Patient Assessment of Constipation Quality of Life Questionnaire; PDQL, Parkinson’s Disease Quality of Life Questionnaire; SDS, Self-Rating Depression Scale; w, week.
Quality assessment of included studies
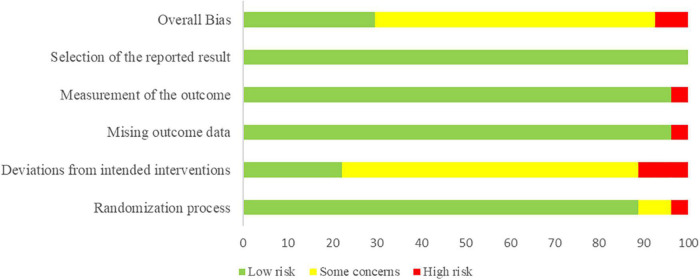
Risk of bias, version 2 indicated low risk for 5 studies (Kluger et al., 2016; Li, 2016; Li Z. et al., 2018; Luo and Zhang, 2019; Zhang, 2020), high risk for 5 studies (Cho et al., 2012; Liang, 2014; Wang et al., 2015; Li et al., 2020; Wu, 2020), and some concerns for 17 studies (Yang, 2009; Xia et al., 2013; Chen, 2015; Toosizadeh et al., 2015; Tian et al., 2016; Zhou et al., 2016; Aroxa et al., 2017; Cho et al., 2018; Dong et al., 2018; Li L. et al., 2018; Liu et al., 2018; Wang et al., 2019; Zhan and Wang, 2019; Xu et al., 2020; Yuan et al., 2020; Li et al., 2021; Wu et al., 2021). Twenty-one studies reported random sequence generation using proper approaches such as a random number table, computer-generated random numbers, or central stochastic distribution, while the remaining 6 studies did not interpret this procedure. Allocation concealment was performed using opaque, sealed envelopes or was sequentially numbered in 10 studies, whereas 17 studies did not report a specific approach for how allocation concealment was conducted. Overall, 19 studies were judged as some concerns risk of bias in deviations from intended interventions domain because most studies failed to blind the participants and personnel, and only 5 studies reported blinding. Only one study was judged as high risk of bias in missing outcome data domain because some participants were lost to follow-up. Besides, one study was judged as high risk of bias in measurement of the outcome. All studies were judged as low risk of bias in selection of the reported result. Figure 2 provided explicit details methodological quality assessment.
FIGURE 2.
Risk of bias graph.
Primary outcomes
Insomnia
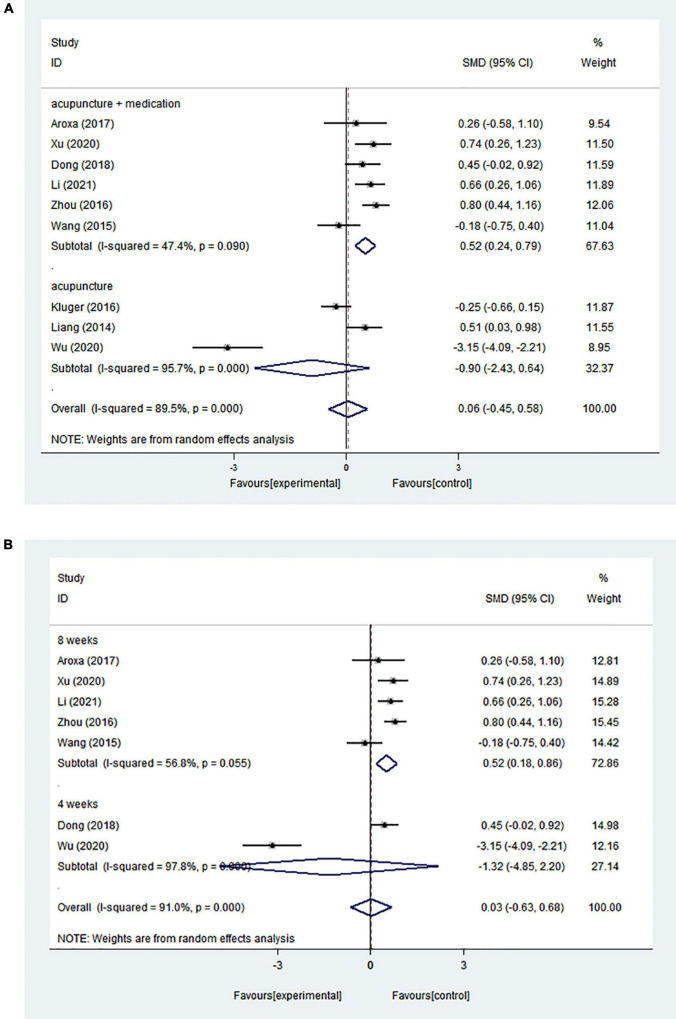
A random effects model was used because of the high statistical heterogeneity of the pooled results (I2 = 89.5%). Nine RCTs showed no significant intervention effect (SMD = 0.064; 95% CI = −0.447 to 0.576; p = 0.805) (Figure 3A).
FIGURE 3.
(A) Forest plot of effects of acupuncture treatment on PD-related insomnia according to intervention types. (B) Forest plot of effects of acupuncture treatment on PD-related insomnia according to course.
Because of the high heterogeneity of the pooled results, we conducted subgroup analyses to explore sources of heterogeneity. Based on different interventions, studies were separated into those evaluating acupuncture combined with medication and those evaluating acupuncture alone. Six studies assessed the effect of acupuncture combined with medication and showed that acupuncture combined with medication could significantly improve insomnia compared with the control group (medication alone) (SMD = 0.517; 95% CI = 0.242–0.793; p = 0.000) (I2 = 47.4%). Three studies examined the effect of acupuncture alone and demonstrated that there was no significant difference between the acupuncture group and the control group (medication alone or sham acupuncture) (SMD = −0.898; 95% CI = −2.432 to 0.636; p = 0.251) (I2 = 95.7%) (Figure 3A). It was clear that heterogeneity was influenced by intervention type, which may be one of the sources of heterogeneity.
The studies included varying courses of treatment, with five trials assessing insomnia at 8 weeks, and two trials assessing insomnia at 4 weeks. The effect of the intervention treatment for improving PD-related insomnia at 4 weeks was similar to that of the control treatment (SMD = −1.325; 95% CI = −4.853 to 2.204; p = 0.462) (I2 = 97.8%). However, there was a significant difference when the treatment occurred over 8 weeks (SMD = 0.519; 95% CI = 0.181–0.857; p = 0.003) (I2 = 56.8%) (Figure 3B).
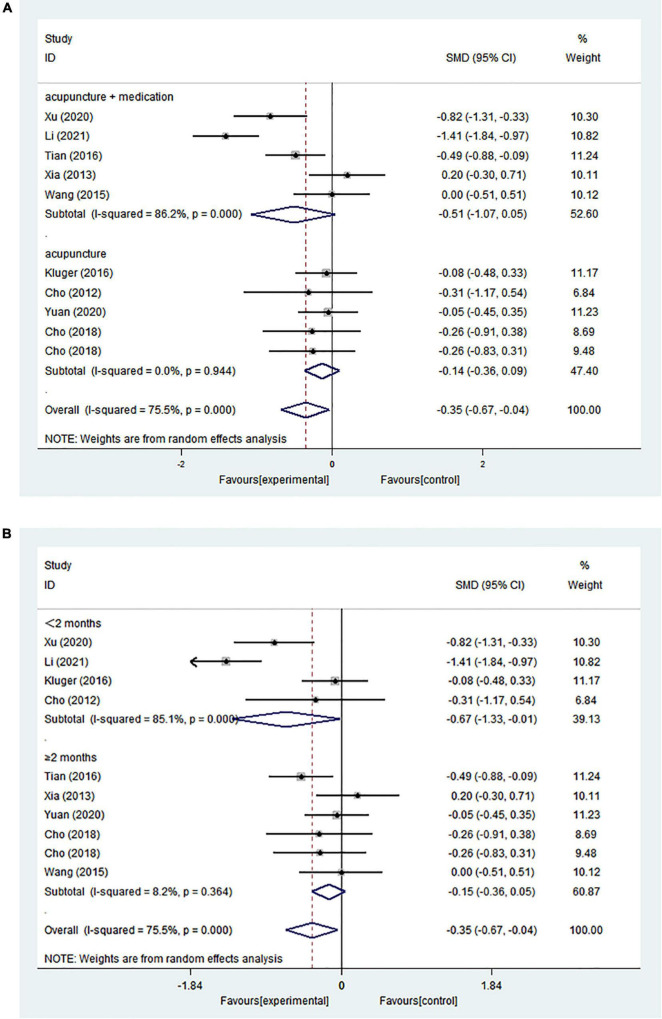
Depression
The pooled results from ten comparisons showed that acupuncture treatment had an overall significant positive intervention effect (SMD = −0.353; 95% CI = −0.669 to −0.037; p = 0.029) (Figure 4).
FIGURE 4.
(A) Forest plot of effects of acupuncture treatment on PD-related depression according to intervention types. (B) Forest plot of effects of acupuncture treatment on PD-related depression according to course.
A subgroup analysis was performed on the basis of the intervention treatment because of significant heterogeneity (I2 = 75.5%). Meta-analysis revealed high heterogeneity (I2 = 86.2%) in the acupuncture combined with medication groups but no heterogeneity in the acupuncture alone group (I2 = 0%). However, both subgroups showed no statistically significant differences in efficacy for improving depression (acupuncture combined with medication: SMD = −0.509; 95% CI = −1.067 to 0.049; p = 0.074) (acupuncture alone: SMD = −0.136; 95% CI = −0.364 to 0.092; p = 0.241) (Figure 4A).
We further performed a subgroup analysis based on the intervention course; studies were separated into those evaluating outcomes within 2 months and those with evaluations after no less than 2 months. Statistically significant heterogeneity (I2 = 85.1%) and a statistically significant advantage (SMD = −0.671; 95% CI = −1.332 to −0.011; p = 0.046) were demonstrated in the studies with courses within 2 months. However, the other subgroup had lower heterogeneity (I2 = 8.2%) and showed no statistically significant differences in treatment efficacy (SMD = −0.153; 95% CI = −0.360 to 0.053; p = 0.145) (Figure 4B). Subgroup analyses showed that the intervention treatment or intervention course explained part of the heterogeneity.
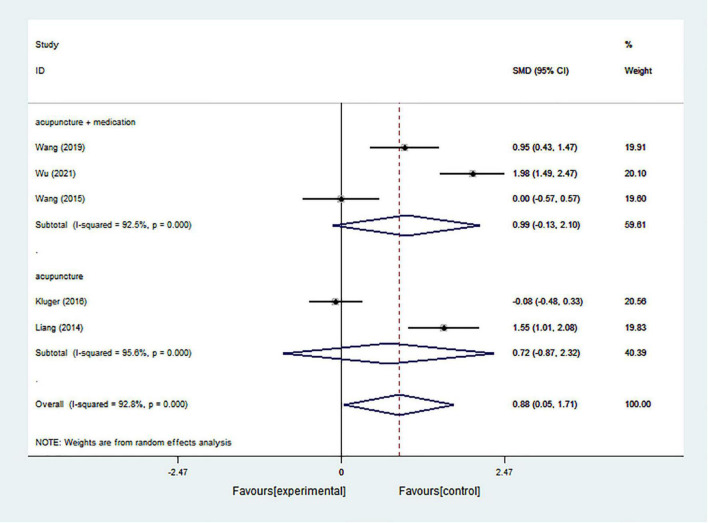
Cognition
The pooled results from 5 studies indicated that acupuncture had an overall significant positive intervention effect in improving cognition in PD patients (SMD = 0.878; 95% CI = 0.046–1.711; p = 0.039) with significant heterogeneity (I2 = 92.8%) (Figure 5). According to the subgroup analysis based on intervention types, both acupuncture alone and acupuncture combined with medication showed no statistically significant effect (acupuncture combined with medication: SMD = 0.985; 95% CI = −0.130 to 2.101; p = 0.083) (acupuncture alone: SMD = 0.724; 95% CI = −0.868 to 2.316; p = 0.373) with significant heterogeneity (I2 = 92.5% and I2 = 95.6%, respectively) (Figure 5).
FIGURE 5.
Forest plot of effects of acupuncture treatment on PD-related cognition according to intervention types.
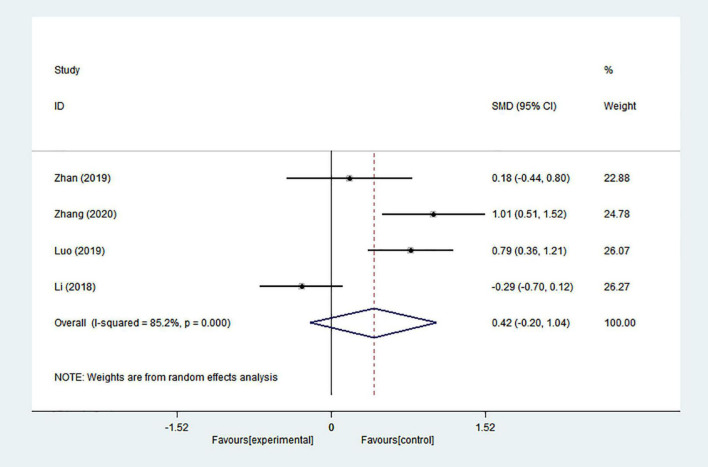
Constipation
Substantial heterogeneity was present in the comparison between acupuncture and medication in four studies (I2 = 65.5%). Statistically significant differences were not found in the pooled results (SMD = 0.422; 95% CI = −0.201 to 1.044; p = 0.185) (Figure 6).
FIGURE 6.
Forest plot of effects of acupuncture treatment on PD-related constipation.
Fatigue
Only one study provided information on fatigue, so a quantitative synthesis could not be performed. This trial included 94 PD patients who were randomized to receive 6 weeks of biweekly real or sham acupuncture. Both acupuncture and sham acupuncture showed significant improvements in the modified Fatigue Impact Scale scores, but no significant difference between the groups was found. The authors suggested that acupuncture improved PD-related fatigue through non-specific or placebo effects.
Secondary outcomes
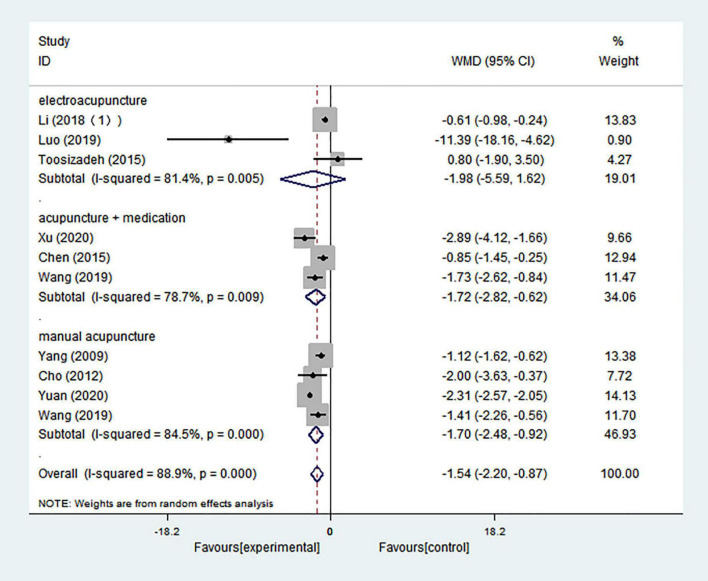
Unified Parkinson’s Disease Rating Scale I
In this analysis, 10 comparisons indicated that UPDRS I scores in PD patients could be significantly decreased by acupuncture treatment (WMD = −1.536; 95% CI = −2.201 to −0.871; p = 0.000), and there was high heterogeneity (I2 = 88.9%) (Figure 7). Intervention types were divided into manual acupuncture, electroacupuncture, and acupuncture combined with medication. Both manual acupuncture and acupuncture combined with medication performed significantly better in decreasing UPDRS I scores than the control treatment (WMD = −1.697; 95% CI = −2.476 to −0.918; p = 0.000; WMD = −1.718; 95% CI = −2.820 to −0.616; p = 0.002; respectively), and there was high heterogeneity (I2 = 84.5% and I2 = 78.7%, respectively). However, three studies evaluating an electroacupuncture intervention showed no significant effect (WMD = −1.984; 95% CI = −5.586 to 1.619; p = 0.280), and there was high heterogeneity (I2 = 81.4%) (Figure 7).
FIGURE 7.
Forest plot of effects of acupuncture treatment on scores of UPDRS I according to intervention types.
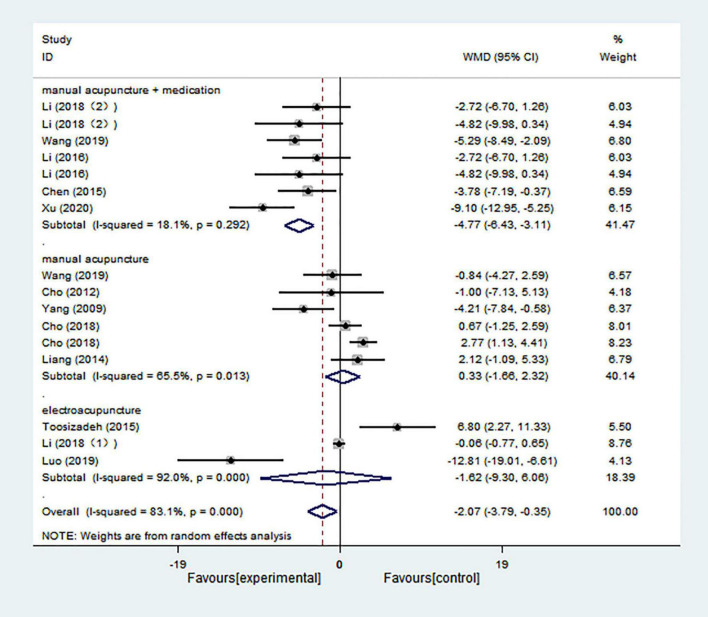
Unified Parkinson’s Disease Rating Scale II
The overall results based on 16 comparisons showed that acupuncture treatment had a better effect in decreasing UPDRS II scores than control treatment (WMD = −2.071; 95% CI = −3.792 to −0.351; p = 0.018), and there was high heterogeneity (I2 = 83.1%) (Figure 8). Both manual acupuncture and electroacupuncture had no significant effect in decreasing UPDRS II scores compared with control treatment (WMD = 0.333; 95% CI = −1.659 to 2.324; p = 0.743; WMD = −1.618; 95% CI = −9.301 to 6.065; p = 0.680, respectively), and there was high heterogeneity (I2 = 65.5% and I2 = 92.0%, respectively). Only manual acupuncture combined with medication was significantly better in decreasing UPDRS II scores (WMD = −4.768; 95% CI = −6.426 to −3.110; p = 0.000), and there was low heterogeneity (I2 = 18.1%) (Figure 8).
FIGURE 8.
Forest plot of effects of acupuncture treatment on scores of UPDRS II according to intervention types.
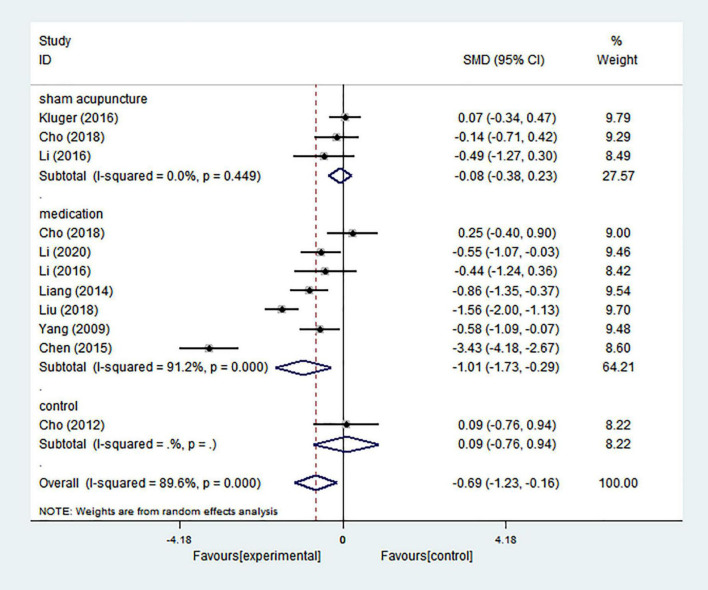
Quality of life
Pooling the results of 11 comparisons showed that acupuncture treatment could improve quality of life in patients with PD (SMD = −0.690; 95% CI = −1.226 to −0.155; p = 0.011), and there was high heterogeneity (I2 = 89.6%) (Figure 9). Based on the differences in control groups, we carried out a subgroup analysis (Figure 9). Meta-analysis of three comparisons showed no significant improvement in quality of life compared with sham acupuncture (SMD = −0.076; 95% CI = −0.380 to 0.227; p = 0.622), and there was no heterogeneity (I2 = 0.00%). Seven comparisons with medication indicated that quality of life could be improved (SMD = −1.013; 95% CI = −1.734 to −0.292; p = 0.006), and there was high heterogeneity (I2 = 91.2%). Only one comparison showed that there was no significant difference in improving quality of life between acupuncture alone and no treatment (SMD = 0.089; 95% CI = −0.761 to 0.939; p = 0.837). It was found that heterogeneity greatly decreased when the control group subgroup analysis was performed, which demonstrated that this may be one of the reasons for high heterogeneity.
FIGURE 9.
Forest plot of effects of acupuncture treatment on PD-related quality of life according to control types.
Sensitive analysis
A sensitivity analysis was conducted by excluding one study at a time, and this exclusion of studies one by one demonstrated that the results were not robust. Stable effects were present in the pooled results regarding quality of life and UPDRS I scores, while other pooled results, including PD-related insomnia, depression, cognition, and constipation were not stable. More details are shown in Supplementary Figures 1–7.
Publication bias
Egger’s test based on different primary outcomes showed no significant publication bias of the included studies (insomnia outcome: Egger’s test p = 0.053; depression outcome: Egger’s test p = 0.816; cognition: Egger’s test p = 0.538; constipation: Egger’s test p = 0.793; UPDRS I: Egger’s test p = 0.918; UPDRS II: Egger’s test p = 0.067; and quality of life: Egger’s test p = 0.783).
Discussion
Summary of findings
Medication treatment is the main treatment for PD, but its long-term use may increase potential complications. Dopaminergic therapies have some limitations regarding treatment of the non-motor symptoms of PD (Muhammed et al., 2016). Adverse effects should also be considered alongside benefits when these drugs are prescribed, and alternative treatments should certainly be explored. In this study, we included 27 trials to evaluate whether acupuncture treatment is an effective option for treating the non-motor symptoms of PD.
In terms of PD-related insomnia, the subgroup results by type of intervention indicated that only acupuncture combined with medication but not acupuncture alone showed benefits. In some studies, it was found that acupuncture combined with medication was more effective, which was consistent with our findings (Cao et al., 2009, 2019; Dong et al., 2017; Zhao et al., 2021). In addition, subgroup analysis based on the intervention course indicated that 8 weeks may be the optimal course for improving PD-related insomnia. Moreover, some studies suggested that acupuncture may more effectively improve insomnia at 8 weeks (Garland et al., 2019). In addition, acupuncture has been shown to be effective for various types of insomnia, including primary insomnia, insomnia after stroke, depression-related insomnia, and chronic pain-related insomnia (Lee and Lim, 2016; Dong et al., 2017; Yin et al., 2017; Liu et al., 2019). It seemed that acupuncture worked on this symptom but not only PD-related insomnia specific, which still needed to be further studied and discussed.
Depression is a common feature in PD, with an estimated prevalence of 30–50% of individuals (Goodarzi et al., 2016). Our findings demonstrated that acupuncture treatment compared with the control treatments resulted in an overall statistically significant improvement in depression. This result was consistent with some previous studies (Xia et al., 2012; Liu et al., 2017; Subramanian, 2017). A previous review focusing on PD-related depression conducted a qualitative analysis of three trials and suggested that acupuncture had a positive effect on PD-related depression (Subramanian, 2017), which was consistent with our findings. Subgroup analysis based on the course showed that an intervention course within 2 months may be the optimal course for improving PD-related depression. Some associations were found in previous studies that demonstrated that the onset of acupuncture treatment effects occurred within 2 months (Andreescu et al., 2011; Wang Z. et al., 2017; Zhao et al., 2019). Although acupuncture could effectively ameliorate PD-related depressive symptoms, more evidence is needed because the sensitivity analysis was unstable to an extent. The unstable results might be ascribed to the stimulation parameters and duration of acupuncture in Xu and Tian’s studies. Besides, acupuncture treatment also had positive effect on patients with depression but without PD (Zeng et al., 2018; Li et al., 2019; Tu et al., 2021).
In terms of cognition, we found evidence of an overall greater effect of acupuncture treatment. A few studies focusing on PD-related cognition showed results consistent with this finding (Arankalle and Nair, 2013; Yeo et al., 2018). Other studies also indicated that acupuncture exerts a positive effect in improving global cognitive function, in conditions involving vascular cognition impairment, mild cognitive impairment, and Alzheimer’s disease-related cognitive impairment (He et al., 2021; Su et al., 2021; Zheng et al., 2021).
Constipation is one of the predominant early non-motor manifestations in PD, and there is pathological evidence to support the hypothesis that PD starts in the gut (Klingelhoefer and Reichmann, 2015). Our pooled results regarding constipation did not show the effect of acupuncture for PD-related constipation, which contradicted a previous study (Cheng, 2017). This result should be examined with caution due to the significant heterogeneity and small sample size. In fact, acupuncture was considered an effective or safe treatment for constipation in those without PD in some randomized trials (Liu et al., 2016; Lv et al., 2017; Wang B. et al., 2017). It is necessary to fill this gap by conducting high-quality evidence-based studies to confirm the effectiveness of acupuncture on constipation, especially on PD-related constipation.
Approximately 50% of PD patients report fatigue (Elbers et al., 2015). Among the studies included in this analysis, only one trial reported PD-related fatigue. This trial recruited 94 patients and suggested that acupuncture treatment may have a placebo effect on PD-related fatigue. In fact, holistic approaches (including acupuncture) are often advised for the treatment of fatigue (Dantzer et al., 2014). Acupuncture treatment had been showed in cancer-related fatigue, chronic fatigue syndrome (Zhang et al., 2018, 2019; Yin et al., 2021). In the absence of enough data allowing a quantitative analysis, the effect of acupuncture on PD-related fatigue remains uncertain based on the present evidence (Elbers et al., 2016).
Our results showed that manual acupuncture combined with medication or acupuncture alone might significantly decrease UPDRS I and II scores, which indicated that acupuncture could totally mitigate the non-motor symptoms of PD. The positive results from previous meta-analyses suggested the efficacy of acupuncture in reducing UPDRS I and II scores (Zhang et al., 2015; Noh et al., 2017). In terms of quality of life, our findings demonstrated that acupuncture treatment had statistically significant overall improvements. Consistent with findings of previous studies, acupuncture was associated with significant reductions in PDQ39 scores (Eng et al., 2006; Arankalle and Nair, 2013; Subramanian, 2017). The results of a subgroup analysis based on comparator types were in line with the finding obtained by Doo et al. (2015) that suggested that acupuncture treatment was more effective than medication in regard to PD-related quality of life (Doo et al., 2015).
Limitations and strengths
To our knowledge, this study is the first to comprehensively examine acupuncture for non-motor symptoms of PD, although some symptoms (such as dizziness, bladder urgency, and apathy) were not reviewed because of the lack of original data. This study combined data from 27 eligible studies that covered an array of common non-motor symptoms and might provide potential evidence for one of non-pharmaceutical therapies for PD-related non-motor symptoms. Previous studies have mostly focused on motor symptoms (Chou et al., 2015; Lee and Lim, 2017). Other studies reviewed the effects of complementary therapies, including acupuncture, for motor and non-motor symptoms but did not provide a quantitative analysis (Subramanian, 2017; Deuel and Seeberger, 2020). Therefore, our study represents a comprehensive assessment of currently available evidence regarding PD non-motor symptoms.
As acupuncture is a manipulated intervention and an invasive non-drug therapy, blinding for acupuncturists is hard to implement in most studies, even in the studies outside of PD (He et al., 2020; Wang et al., 2022). Some concerns risk of bias mostly existed in the domains of blinding in our study, particularly in participant and personnel blinding, which weakened the strength of the evidence and our conclusions. Potential bias may be produced and placebo effect in acupuncture may confound these analyses. In an analysis of acupuncture for depression, it showed that acupuncture treatment had placebo effect (Smith et al., 2018). However, placebo effect of acupuncture treatment was conflicting in other studies (Sunay et al., 2011; Zhang et al., 2019). And trials using sham acupuncture may underestimate acupuncture’s treatment effect in some cases (Fei et al., 2022). Moreover, some of the pooled results continued to exhibit high levels of heterogeneity and were unstable in the sensitivity analysis, although we restricted the criteria for study enrollment and performed subgroup analyses. And most of the trials were conducted in China is one of the major limitations, which may affect the generalizability of the findings. Therefore, the effectiveness of acupuncture in PD-related non-motor symptoms should be interpreted with caution.
Implications for clinical practice
Some results of this study may help provide guidance for clinical application. First, for patients with PD-related depression or decreased quality of life or cognition, acupuncture treatment may be a good choice for health care workers. Second, among acupuncture treatment types, acupuncture combined with medications may be more suitable for PD-related insomnia, and manual acupuncture combined with medication could be recommended for improving total mentation, behavior and mood (UPDRS I) or activities of daily living (UPDRS II). Third, 8 weeks may be the optimal course for improving PD-related insomnia and within 2 months for PD-related depression.
Conclusion
In conclusion, this meta-analysis demonstrated that acupuncture treatment may be associated with improvements in PD-related depression, quality of life, cognition, total mentation, behavior and mood, and activities of daily living. However, more evidence, especially a higher level of evidence from large-scale clinical trials, is still needed to support these clinical recommendations.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CW and MZ designed this study, supervised the research, and reviewed the manuscript. XW, ML, LZ, and ZL performed the articles screening and data extracting. QL and XH performed the quality assessment. QL contributed to data analysis, and wrote and reviewed the manuscript. XW, LZ, and ZL edited the figures and table. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Natural Science Foundation of Guangdong Province (2022A1515010450), Natural Science Foundation of Shenzhen (JCYJ20210324123614040), Traditional Chinese Medicine Bureau of Guangdong Province, China (Grant No. 20221348), Bao’an TCM Development Foundation (2020KJCX-KTYJ-130, 2020KJCX-KTYJ-131, and 2020KJCX-KTYJ-134), and Sanming Project of Medicine in Shenzhen (No. SZZYSM202106009).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2022.995850/full#supplementary-material
References
- Andreescu C., Glick R., Emeremni C., Houck P., Mulsant B. (2011). Acupuncture for the treatment of major depressive disorder: A randomized controlled trial. J. Clin. Psychiatr. 72 1129–1135. 10.4088/JCP.10m06105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arankalle D., Nair P. (2013). Effect of electroacupuncture on function and quality of life in Parkinson’s disease: A case report. Acupunct. Med. 31 235–238. 10.1136/acupmed-2012-010285 [DOI] [PubMed] [Google Scholar]
- Armstrong M., Okun M. (2020). Diagnosis and treatment of Parkinson disease: A review. JAMA 323 548–560. 10.1001/jama.2019.22360 [DOI] [PubMed] [Google Scholar]
- Aroxa F. H., Gondim I. T., Santos E. L., Coriolano M. D., Asano A. G., Asano N. M. (2017). Acupuncture as adjuvant therapy for sleep disorders in Parkinson’s disease. J. Acupunct. Meridian Stud. 10 33–38. 10.1016/j.jams.2016.12.007 [DOI] [PubMed] [Google Scholar]
- Asakawa T., Fang H., Sugiyama K., Nozaki T., Kobayashi S., Hong Z., et al. (2016). Human behavioral assessments in current research of Parkinson’s disease. Neurosci. Biobehav. Rev. 68 741–772. 10.1016/j.neubiorev.2016.06.036 [DOI] [PubMed] [Google Scholar]
- Bloem B., Okun M., Klein C. (2021). Parkinson’s disease. Lancet 397 2284–2303. 10.1016/S0140-6736(21)00218-X [DOI] [PubMed] [Google Scholar]
- Buysse D., Reynolds C. F., III, Monk T., Berman S., Kupfer D. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 28 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Cao H., Pan X., Li H., Liu J. (2009). Acupuncture for treatment of insomnia: A systematic review of randomized controlled trials. J. Altern. Complement. Med. 15 1171–1186. 10.1089/acm.2009.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao H., Yu M., Wang L., Fei Y., Xu H., Liu J. (2019). Acupuncture for primary insomnia: An updated systematic review of randomized controlled trials. J. Altern. Complement. Med. 25 451–474. 10.1089/acm.2018.0046 [DOI] [PubMed] [Google Scholar]
- Chaudhuri K. R., Pal S., DiMarco A., Whately-Smith C., Bridgman K., Mathew R., et al. (2002). The Parkinson’s disease sleep scale: A new instrument for assessing sleep and nocturnal disability in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 73 629–635. 10.1136/jnnp.73.6.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri K., Sauerbier A. (2016). Parkinson disease. Unravelling the nonmotor mysteries of Parkinson disease. Nat. Rev. Neurol. 12 10–11. 10.1038/nrneurol.2015.236 [DOI] [PubMed] [Google Scholar]
- Chen Y. (2015). Clinical Observation of Treatment of Parkinson’s Disease with Trembling Three Needles. Guangzhou: Guangzhou University of Chinses Medicine. [Google Scholar]
- Cheng F. K. (2017). The use of acupuncture in patients with Parkinson’s disease. Geriatr. Nurs. 38 302–314. 10.1016/j.gerinurse.2016.11.010 [DOI] [PubMed] [Google Scholar]
- Cho S. Y., Lee Y. E., Doo K. H., Lee J. H., Jung W. S., Moon S. K., et al. (2018). Efficacy of combined treatment with acupuncture and bee venom acupuncture as an adjunctive treatment for Parkinson’s disease. J. Altern. Complement. Med. 24 25–32. 10.1089/acm.2016.0250 [DOI] [PubMed] [Google Scholar]
- Cho S. Y., Shim S. R., Rhee H. Y., Park H. J., Jung W. S., Moon S. K., et al. (2012). Effectiveness of acupuncture and bee venom acupuncture in idiopathic Parkinson’s disease. Parkinsonism Relat. Disord. 18 948–952. 10.1016/j.parkreldis.2012.04.030 [DOI] [PubMed] [Google Scholar]
- Chou Y. H., Hickey P. T., Sundman M., Song A. W., Chen N. K. (2015). Effects of repetitive transcranial magnetic stimulation on motor symptoms in Parkinson disease: A systematic review and meta-analysis. JAMA Neurol. 72 432–440. 10.1001/jamaneurol.2014.4380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly B., Lang A. (2014). Pharmacological treatment of Parkinson disease: A review. JAMA. 311 1670–1683. 10.1001/jama.2014.3654 [DOI] [PubMed] [Google Scholar]
- Dantzer R., Heijnen C. J., Kavelaars A., Laye S., Capuron L. (2014). The neuroimmune basis of fatigue. Trends Neurosci. 37 39–46. 10.1016/j.tins.2013.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks J. J., Higgins J. P. T., Altman D. G. (eds) (2022). “Chapter 10: Analysing data and undertaking meta-analyses,” in Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022), eds Higgins J. P. T., Thomas J., Chandler J., Cumpston M., Li T., Page M. J., et al. (London: Cochrane; ). [Google Scholar]
- Deuel L. M., Seeberger L. C. (2020). Complementary therapies in Parkinson disease: A review of acupuncture, Tai Chi, Qi Gong, Yoga, and Cannabis. Neurotherapeutics 17 1434–1455. 10.1007/s13311-020-00900-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deuschl G., Beghi E., Fazekas F., Varga T., Christoforidi K., Sipido E., et al. (2020). The burden of neurological diseases in Europe: An analysis for the Global Burden of Disease Study 2017. Lancet Public Health 5 e551–e567. 10.1016/S2468-2667(20)30190-0 [DOI] [PubMed] [Google Scholar]
- Dong B., Chen Z., Yin X., Li D., Ma J., Yin P., et al. (2017). The efficacy of acupuncture for treating depression-related insomnia compared with a control group: A systematic review and meta-analysis. Biomed. Res. Int. 2017:9614810. 10.1155/2017/9614810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Q., Li X., Tang M., Wan J., Zhong L. A. (2018). Randomized controlled study on scalp electro-acupuncture for the treatment of sleep disorders in Parkinson’s disease. Clin. J. Pract. Hosp. 15 214–216. [Google Scholar]
- Doo K. H., Lee J. H., Cho S. Y., Jung W. S., Moon S. K., Park J. M., et al. (2015). A prospective open-label study of combined treatment for idiopathic Parkinson’s disease using acupuncture and bee venom acupuncture as an adjunctive treatment. J. Altern. Complement. Med. 21 598–603. 10.1089/acm.2015.0078 [DOI] [PubMed] [Google Scholar]
- Elbers R. G., Berendse H. W., Kwakkel G. (2016). Treatment of fatigue in Parkinson disease. JAMA 315 2340–2341. 10.1001/jama.2016.5260 [DOI] [PubMed] [Google Scholar]
- Elbers R. G., Verhoef J., van Wegen E. E., Berendse H. W., Kwakkel G. (2015). Interventions for fatigue in Parkinson’s disease. Cochrane Database Syst. Rev. 2015:Cd010925. 10.1002/14651858.CD010925.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng M. L., Lyons K. E., Greene M. S., Pahwa R. (2006). Open-label trial regarding the use of acupuncture and yin tui na in Parkinson’s disease outpatients: A pilot study on efficacy, tolerability, and quality of life. J. Altern. Complement. Med. 12 395–399. 10.1089/acm.2006.12.395 [DOI] [PubMed] [Google Scholar]
- Fei Y. T., Cao H. J., Xia R. Y., Chai Q. Y., Liang C. H., Feng Y. T., et al. (2022). Methodological challenges in design and conduct of randomised controlled trials in acupuncture. BMJ 376:e064345. 10.1136/bmj-2021-064345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland S., Xie S., DuHamel K., Bao T., Li Q., Barg F., et al. (2019). Acupuncture versus cognitive behavioral therapy for insomnia in cancer survivors: A randomized clinical trial. J. Natl. Cancer Inst. 111 1323–1331. 10.1093/jnci/djz050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2016 Neurology Collaborators (2019). Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18 459–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert R., Khemani P. (2022). Treatment of advanced Parkinson’s disease. J. Geriatr. Psychiatry Neurol. 35 12–23. 10.1177/0891988720988904 [DOI] [PubMed] [Google Scholar]
- Goldman J., Guerra C. (2020). Treatment of nonmotor symptoms associated with Parkinson disease. Neurol. Clin. 38 269–292. 10.1016/j.ncl.2019.12.003 [DOI] [PubMed] [Google Scholar]
- Goodarzi Z., Mrklas K., Roberts D., Jette N., Pringsheim T., Holroyd-Leduc J. (2016). Detecting depression in Parkinson disease: A systematic review and meta-analysis. Neurology 87 426–437. 10.1212/WNL.0000000000002898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haehner A., Hummel T., Hummel C., Sommer U., Junghanns S., Reichmann H. (2007). Olfactory loss may be a first sign of idiopathic Parkinson’s disease. Mov. Disord. 22 839–842. 10.1002/mds.21413 [DOI] [PubMed] [Google Scholar]
- Hamilton M. (1980). Rating depressive patients. J. Clin. Psychiatry 41(12 Pt. 2), 21–24. [PubMed] [Google Scholar]
- He W., Li M., Han X., Zhang W. (2021). Acupuncture for mild cognitive impairment and dementia: An overview of systematic reviews. Front. Aging Neurosci. 13:647629. 10.3389/fnagi.2021.647629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Y., Guo X., May B., Zhang A., Liu Y., Lu C., et al. (2020). Clinical evidence for association of acupuncture and acupressure with improved cancer pain: A systematic review and meta-analysis. JAMA Oncol. 6 271–278. 10.1001/jamaoncol.2019.5233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J., Thompson S., Deeks J., Altman D. (2003). Measuring inconsistency in meta-analyses. BMJ 327 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes A. J., Daniel S. E., Lees A. J. (2001). Improved accuracy of clinical diagnosis of Lewy body Parkinson’s disease. Neurology 57 1497–1499. 10.1212/WNL.57.8.1497 [DOI] [PubMed] [Google Scholar]
- Kim H., Park S., Cho Y., Hong K., Cho J., Seo S., et al. (2009). Nonmotor symptoms in de novo Parkinson disease before and after dopaminergic treatment. J. Neurol. Sci. 287 200–204. 10.1016/j.jns.2009.07.026 [DOI] [PubMed] [Google Scholar]
- Klingelhoefer L., Reichmann H. (2015). Pathogenesis of Parkinson disease–the gut-brain axis and environmental factors. Nat. Rev. Neurol. 11 625–636. 10.1038/nrneurol.2015.197 [DOI] [PubMed] [Google Scholar]
- Kluger B. M., Rakowski D., Christian M., Cedar D., Wong B., Crawford J., et al. (2016). Randomized, controlled trial of acupuncture for fatigue in Parkinson’s disease. Mov. Disord. 31 1027–1032. 10.1002/mds.26597 [DOI] [PubMed] [Google Scholar]
- Lee S. H., Lim S. M. (2016). Acupuncture for insomnia after stroke: A systematic review and meta-analysis. BMC Complement. Altern. Med. 16:228. 10.1186/s12906-016-1220-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Lim S. (2017). Clinical effectiveness of acupuncture on Parkinson disease: A PRISMA-compliant systematic review and meta-analysis. Medicine 96:e5836. 10.1097/MD.0000000000005836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li K., Xu S., Li J., Chen L., Li G., Dai M., et al. (2020). Clinical study of electroacupuncture combined with medication for Parkinson’s disease. Shanghai J. Acu-Mox. 39 1564–1569. [Google Scholar]
- Li L., Jin X., Wang X., Yin J., Chen C. (2018). Effect of electroacupuncture on bilateral TianShu for dynamics of anal rectum and UPDRS scores in Parkinson’s disease with constipation. Zhejiang Med. J. 40 1367–1370. [Google Scholar]
- Li L., Tian Z., Zhang X. (2021). Clinical study on electroacupuncture combined with madopar for sleep disorders in Parkinson disease. J. N. Chin. Med. 53 113–116. [Google Scholar]
- Li W., Yin P., Lao L., Xu S. (2019). Effectiveness of acupuncture used for the management of postpartum depression: A systematic review and meta-analysis. Biomed. Res. Int. 2019:6597503. 10.1155/2019/6597503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z. (2016). Clinical Study of Acupuncture Paratherapy for Parkinson’s Disease Tremor and Its Underlying Neuromechanism Based on Functional Magnetic Resonance Imaging. Guangzhou: Guangzhou University of Chinses Medicine. [Google Scholar]
- Li Z., Chen J., Cheng J., Huang S., Hu Y., Wu Y., et al. (2018). Acupuncture modulates the cerebello-thalamo-cortical circuit and cognitive brain regions in patients of Parkinson’s disease with tremor. Front. Aging Neurosci. 10:206. 10.3389/fnagi.2018.00206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang X. (2014). The Effect of “the Seven Acupoints of the Cranial Base” on Health Related Quality of Life for Patients with Parkinson’s Disease: A Randomzied Controlled Trial. Beijing: China Academy of Chinese Medical Sciences. [Google Scholar]
- Liu A., Wu X., Xu J., Lu B. (2018). Influence of acupuncture on serum MDA, SOD and Cystatin C in Parkinson’s disease patients. Chin. Med. Guide 24 104–106. [Google Scholar]
- Liu F., You J., Li Q., Fang T., Chen M., Tang N., et al. (2019). Acupuncture for chronic pain-related insomnia: A systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2019:5381028. 10.1155/2019/5381028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Chen L., Zhang Z., Geng G., Chen W., Dong H., et al. (2017). Effectiveness and safety of acupuncture combined with Madopar for Parkinson’s disease: A systematic review with meta-analysis. Acupunct. Med. 35 404–412. [DOI] [PubMed] [Google Scholar]
- Liu Z., Yan S., Wu J., He L., Li N., Dong G., et al. (2016). Acupuncture for chronic severe functional constipation: A randomized trial. Ann. Intern. Med. 165 761–769. 10.7326/M15-3118 [DOI] [PubMed] [Google Scholar]
- Luo S., Zhang Y. (2019). Clinical effect of electro-acupuncture zusanli combined with conventional western medicine in the traetment of Parkinson’s disease and constipation. TCM Chin. Med. 4 136–138. [Google Scholar]
- Lv J. Q., Wang C. W., Liu M. Y., Zhao Y., Wen Q., Li N. (2017). Observation on the efficacy of electroacupuncture for functional constipation. Zhen Ci Yan Jiu 42 254–258. [PubMed] [Google Scholar]
- Muhammed K., Manohar S., Ben Yehuda M., Chong T., Tofaris G., Lennox G., et al. (2016). Reward sensitivity deficits modulated by dopamine are associated with apathy in Parkinson’s disease. Brain 139 2706–2721. 10.1093/brain/aww188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasreddine Z. S., Phillips N. A., Bédirian V., Charbonneau S., Whitehead V., Collin I., et al. (2005). The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53 695–699. 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- Noh H., Kwon S., Cho S. Y., Jung W. S., Moon S. K., Park J. M., et al. (2017). Effectiveness and safety of acupuncture in the treatment of Parkinson’s disease: A systematic review and meta-analysis of randomized controlled trials. Complement. Ther. Med. 34 86–103. 10.1016/j.ctim.2017.08.005 [DOI] [PubMed] [Google Scholar]
- Page M., McKenzie J., Bossuyt P., Boutron I., Hoffmann T., Mulrow C., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. 74 790–799. 10.1016/j.recesp.2021.06.016 [DOI] [PubMed] [Google Scholar]
- Parkinson’s Disease and Movement Disorders Group of Neurology Branch of Chinese Medical Association (2016). Diagnostic criteria for Parkinson’s disease in China. Chin. J. Neurol. 49 268–271. [Google Scholar]
- Poewe W. (2010). Parkinson disease: Treatment of the nonmotor symptoms of Parkinson disease. Nat. Rev. Neurol. 6 417–418. 10.1038/nrneurol.2010.87 [DOI] [PubMed] [Google Scholar]
- Postuma R. B., Berg D., Stern M., Poewe W., Olanow C. W., Oertel W., et al. (2015). MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 30 1591–1601. 10.1002/mds.26424 [DOI] [PubMed] [Google Scholar]
- Ramaker C., Marinus J., Stiggelbout A. M., Van Hilten B. J. (2002). Systematic evaluation of rating scales for impairment and disability in Parkinson’s disease. Mov. Disord. 17 867–876. 10.1002/mds.10248 [DOI] [PubMed] [Google Scholar]
- Seppi K., Ray Chaudhuri K., Coelho M., Fox S., Katzenschlager R., Perez Lloret S., et al. (2019). Update on treatments for nonmotor symptoms of Parkinson’s disease-an evidence-based medicine review. Mov. Disord. 34 180–198. 10.1002/mds.27602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C., Armour M., Lee M., Wang L., Hay P. (2018). Acupuncture for depression. Cochrane Database Syst. Rev. 3:CD004046. 10.1002/14651858.CD004046.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne J., Savović J., Page M., Elbers R., Blencowe N., Boutron I., et al. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- Su X., Sun N., Zhang N., Wang L., Zou X., Li J., et al. (2021). Effectiveness and safety of acupuncture for vascular cognitive impairment: A systematic review and meta-analysis. Front. Aging Neurosci. 13:692508. 10.3389/fnagi.2021.692508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian I. (2017). Complementary and alternative medicine and exercise in nonmotor symptoms of Parkinson’s disease. Int. Rev. Neurobiol. 134 1163–1188. 10.1016/bs.irn.2017.05.037 [DOI] [PubMed] [Google Scholar]
- Sunay D., Sunay M., Aydoǧmuş Y., Baǧbancı S., Arslan H., Karabulut A., et al. (2011). Acupuncture versus paroxetine for the treatment of premature ejaculation: A randomized, placebo-controlled clinical trial. Eur. Urol. 59 765–771. 10.1016/j.eururo.2011.01.019 [DOI] [PubMed] [Google Scholar]
- Tian Y., Dong Q., Liu H. (2016). Efficacy of electro-acupuncture combined with drug therapy on Parkinson’s disease with depression and its influence on serum BDNF. Res. Integr. Tradit. Chin. West. Med. 8 289–291. [Google Scholar]
- Toosizadeh N., Lei H., Schwenk M., Sherman S. J., Sternberg E., Mohler J., et al. (2015). Does integrative medicine enhance balance in aging adults? Proof of concept for the benefit of electroacupuncture therapy in Parkinson’s disease. Gerontology 61 3–14. 10.1159/000363442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu M., Jiang Y., Yu J., Hu H., Liao B., He X., et al. (2021). Acupuncture for treating chronic stable angina pectoris associated anxiety and depression: A systematic review and meta-analysis. Complement. Ther. Clin. Pract. 45:101484. 10.1016/j.ctcp.2021.101484 [DOI] [PubMed] [Google Scholar]
- Wang B., Chen Y., Chen S. (2017). Clinical observation of slow transit constipation treated with acupuncture and modified weitong xiaopi formula. Zhongguo Zhen Jiu 37 130–134. 10.13703/j.0255-2930.2017.02.006 [DOI] [PubMed] [Google Scholar]
- Wang F., Sun L., Zhang X. Z., Jia J., Liu Z., Huang X. Y., et al. (2015). Effect and potential mechanism of electroacupuncture add-on treatment in patients with Parkinson’s disease. Evid. Based Complement. Alternat. Med. 2015:692795. 10.1155/2015/692795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Xia Q., Zhu F., Huang W., Meng Y., Wang Y., et al. (2022). Effects of acupuncture on adverse events in colonoscopy: A systematic review and meta-analysis of randomized controlled trials. Pain Ther. [Epub ahead of print]. 10.1007/s40122-022-00415-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Wang X., Liu J., Chen J., Liu X., Nie G., et al. (2017). Acupuncture treatment modulates the corticostriatal reward circuitry in major depressive disorder. J. Psychiatr. Res. 84 18–26. 10.1016/j.jpsychires.2016.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Zhang H., Zhang D. (2019). Clinical effect evaluation of acupuncture combined with benserazide in treatment of Parkinson syndrome. J. Hubei Univ. Chin. Med. 21 82–85. 10.13703/j.0255-2930.20210605-0001 [DOI] [PubMed] [Google Scholar]
- Wu L., Zhang G., Zhou X., Feng Q. (2021). Effects of acupuncture combined with western medication on the levels of NT-3, IGF-1, DA and inflammatory cytokines in patients with Parkinson’s disease of liver-kidney yin deficiency pattern. Shanghai J. Acu-Mox. 40 814–819. [Google Scholar]
- Wu M. (2020). Treatment of Insomnia in Parkinson’s Disease with Liver Depression and Spleen Deficiency by Different Methods Clinical Effect Observation. Anhui: Anhui University of Chinese Medicine. [Google Scholar]
- Xia Y., Ding Y., Wang H., Liu W., Qiao F., Pan Q., et al. (2013). Clinical study of electroacupuncture for Parkinson disease with depression. J. Shandong Univ. TCM 37 29–31. 23301468 [Google Scholar]
- Xia Y., Wang H., Ding Y., Kang B., Liu W. (2012). Parkinson’s disease combined with depression treated with electroacupuncture and medication and its effect on serum BDNF. Zhongguo Zhen Jiu 32 1071–1074. [PubMed] [Google Scholar]
- Xu Y., Cai X., Qu S., Zhang J., Zhang Z., Yao Z., et al. (2020). Madopar combined with acupuncture improves motor and non-motor symptoms in Parkinson’s disease patients: A multicenter randomized controlled trial. Eur. J. Integr. Med. 34:101049. 10.1016/j.eujim.2019.101049 [DOI] [Google Scholar]
- Yang S. (2009). The Clinical Study of Using Tremor Three Needles in the Treatment of Parkinson’s Disease. Guangzhou: Guangzhou University of Chinses Medicine. [Google Scholar]
- Yeo S., van den Noort M., Bosch P., Lim S. (2018). A study of the effects of 8-week acupuncture treatment on patients with Parkinson’s disease. Medicine 97:e13434. 10.1097/MD.0000000000013434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung W., Yu B., Yuen J., Ho J., Chung K., Zhang Z., et al. (2021). Semi-individualized acupuncture for insomnia disorder and oxidative stress: A randomized, double-blind, sham-controlled trial. Nat. Sci. Sleep 13 1195–1207. 10.2147/NSS.S318874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin X., Gou M., Xu J., Dong B., Yin P., Masquelin F., et al. (2017). Efficacy and safety of acupuncture treatment on primary insomnia: A randomized controlled trial. Sleep Med. 37 193–200. 10.1016/j.sleep.2017.02.012 [DOI] [PubMed] [Google Scholar]
- Yin Z. H., Wang L. J., Cheng Y., Chen J., Hong X. J., Zhao L., et al. (2021). Acupuncture for chronic fatigue syndrome: An overview of systematic reviews. Chin. J. Integr. Med. 27 940–946. 10.1007/s11655-020-3195-3 [DOI] [PubMed] [Google Scholar]
- Yuan Y., Cai X., Chen F. (2020). Clinical observation on treatment of Parkinson’s disease with depression by the“Seven Acupoints of Cranial Base”. Chin. J. Geriatr. Care 18 27–30. [Google Scholar]
- Zeng L., Tao Y., Hou W., Zong L., Yu L. (2018). Electro-acupuncture improves psychiatric symptoms, anxiety and depression in methamphetamine addicts during abstinence: A randomized controlled trial. Medicine 97:e11905. 10.1097/MD.0000000000011905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zesiewicz T., Sullivan K., Arnulf I., Chaudhuri K., Morgan J., Gronseth G., et al. (2010). Practice parameter: Treatment of nonmotor symptoms of Parkinson disease: Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 74 924–931. 10.1212/WNL.0b013e3181d55f24 [DOI] [PubMed] [Google Scholar]
- Zhan X., Wang Y. (2019). Therapeutic effect of acupuncture on constipation of Parkinson’s disease. Asia-Pacif. Tradit. Med. 15 128–130. [Google Scholar]
- Zhang G., Xiong N., Zhang Z., Liu L., Huang J., Yang J., et al. (2015). Effectiveness of traditional Chinese medicine as an adjunct therapy for Parkinson’s disease: A systematic review and meta-analysis. PLoS One 10:e0118498. 10.1371/journal.pone.0118498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H. (2020). The Clinical Research of Treating Parkinson’s Disease Patients with Functional Constipation by Abdominal Acupuncture. Guangzhou: Guangzhou University of Chinese Medicine. [Google Scholar]
- Zhang Q., Gong J., Dong H., Xu S., Wang W., Huang G. (2019). Acupuncture for chronic fatigue syndrome: A systematic review and meta-analysis. Acupunct. Med. 37 211–222. 10.1136/acupmed-2017-011582 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Lin L., Li H., Hu Y., Tian L. (2018). Effects of acupuncture on cancer-related fatigue: A meta-analysis. Support. Care Cancer 26 415–425. 10.1007/s00520-017-3955-6 [DOI] [PubMed] [Google Scholar]
- Zhao B., Li Z., Wang Y., Ma X., Wang X., Wang X., et al. (2019). Can acupuncture combined with SSRIs improve clinical symptoms and quality of life in patients with depression? Secondary outcomes of a pragmatic randomized controlled trial. Complement. Ther. Med. 45 295–302. 10.1016/j.ctim.2019.03.015 [DOI] [PubMed] [Google Scholar]
- Zhao F., Fu Q., Kennedy G., Conduit R., Wu W., Zhang W., et al. (2021). Comparative utility of acupuncture and western medication in the management of perimenopausal insomnia: A systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2021:5566742. 10.1155/2021/5566742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X., Lin W., Jiang Y., Lu K., Wei W., Huo Q., et al. (2021). Electroacupuncture ameliorates beta-amyloid pathology and cognitive impairment in Alzheimer disease via a novel mechanism involving activation of TFEB (transcription factor EB). Autophagy 17 3833–3847. 10.1080/15548627.2021.1886720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou C., Pang W., Wu L. (2016). Analysis of clinical efficacy and safety of acupuncture combined with madopar in the treatment of Parkinson’s disease. China Med. Pharm 6 11–18. 29180347 [Google Scholar]
- Zigmond A. S., Snaith R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67 361–370. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.