Abstract
The early detection of Francisella tularensis, the causative agent of tularemia, is important for adequate treatment by antibiotics and the outcome of the disease. Here we describe a new capture enzyme-linked immunosorbent assay (cELISA) based on monoclonal antibodies specific for lipopolysaccharide (LPS) of Francisella tularensis subsp. holarctica and Francisella tularensis subsp. tularensis. No cross-reactivity with Francisella tularensis subsp. novicida, Francisella philomiragia, and a panel of other possibly related bacteria, including Brucella spp., Yersinia spp., Escherichia coli, and Burkholderia spp., was observed. The detection limit of the assay was 103 to 104 bacteria/ml. This sensitivity was achieved by solubilization of the LPS prior to the cELISA. In addition, a novel immunochromatographic membrane-based handheld assay (HHA) and a PCR, targeting sequences of the 17-kDa protein (TUL4) gene of F. tularensis, were used in this study. Compared to the cELISA, the sensitivity of the HHA was about 100 times lower and that of the PCR was about 10 times higher. All three techniques were successfully applied to detect F. tularensis in tissue samples of European brown hares (Lepus europaeus). Whereas all infected samples were recognized by the cELISA, those with relatively low bacterial load were partially or not detected by PCR and HHA, probably due to inhibitors or lack of sensitivity. In conclusion, the HHA can be used as a very fast and simple approach to perform field diagnosis to obtain a first hint of an infection with F. tularensis, especially in emergent situations. In any suspect case, the diagnosis should be confirmed by more sensitive techniques, such as the cELISA and PCR.
Within the genus Francisella there are two known species, Francisella tularensis and Francisella philomiragia, which have a 16S rRNA gene sequence similarity of more than 98% (6). F. tularensis, a gram-negative, small (0.2 to 0.7 by 0.2 μm) facultative intracellular bacterium, is distributed on all continents of the northern hemisphere. At least four subspecies of F. tularensis are known. Francisella tularensis subsp. tularensis (or type A; predominantly found in North America), Francisella tularensis subsp. holarctica, and Francisella tularensis subsp. mediaasiatica (both referred to as type B) cause the zoonotic disease tularemia in humans and animals (5, 11, 17). Only a few cases of human tularemia-like disease caused by the fourth subspecies, Francisella tularensis subsp. novicida, have been described (10). Depending on the site of entry and the predominant infectious or pathogenic process, tularemia can clinically manifest as an ulceroglandular, glandular, pulmonary, typhoidal, or ocular form. High fever and enlarged lymph nodes are predominant symptoms.
More than 250 different animal species can be infected by F. tularensis. Small rodents are the main natural hosts (reservoir), and blood-sucking ectoparasites are the most important vectors. In addition, the bacteria are quite stable in the environment under humidified and cold conditions. Humans can acquire the infection through the bites of infected arthropods or after contact with infected animals or contaminated water, food, dust, and aerosols (15, 17).
The detection of specific antibodies in serum is the most widely used approach for routine laboratory diagnosis of tularemia. However, antibodies to F. tularensis are not detected until 2 weeks or more after infection (2, 12). An early identification of the pathogen is important, as the course and the outcome of the disease is mainly dependent on early and adequate antibiotic treatment. The classical methods for identification of F. tularensis are the isolation of the pathogen by cultivation with subsequent identification by agglutination or immunofluorescence assay. These methods are time-consuming and require intensive handling of the infectious agent. Antigen detection in urine and RNA hybridization of wound specimens have also been used as diagnostic methods (7, 16). More recently, PCR has been applied for the detection of F. tularensis (6, 13, 18).
In this study we describe a highly sensitive capture enzyme-linked immunosorbent assay (cELISA) based on monoclonal antibodies (MAbs) and compare it with an immunochromatographic membrane-based handheld assay (HHA) and a PCR for detection of F. tularensis in naturally infected hare tissues.
MATERIALS AND METHODS
Bacteria.
The F. tularensis live vaccine strain (LVS; ATCC 29684) was cultivated on cysteine-heart agar (Difco, Augsburg, Germany) supplemented with 10% sheep blood. The bacterial isolates from European brown hares (Lepus europaeus) were obtained by direct cultivation on cysteine-heart agar as described previously (9). The bacteria were identified as F. tularensis by specific antisera. The classification of these isolates as F. tularensis subsp. holarctica was done on the basis of resistance to erythromycin and acid formation from glucose and maltose, as well as by the absence of utilization of glycerol and saccharose (4, 14). The sources of other bacteria used in this study are listed in Table 1. All bacterial isolates used were inactivated by 0.5 to 1.0% formalin at room temperature for 20 min, washed in phosphate-buffered saline (PBS; pH 7.4) and adjusted to an optical density at 560 nm (OD560) of 1.0. In the case of F. tularensis, this OD corresponded to approximately 109 CFU/ml (data not shown).
TABLE 1.
Sensitivity and cross-reactivity of cELISA for F. tularensisa
| Species | Source or strain | No. of strains | Reactivity (bacteria/ml) |
|---|---|---|---|
| F. tularensis subsp. holarctica | ATCC 29684 (LVS) | 1 | <104 |
| WIS 140, 202 | 2 | <104 | |
| BTB | 8 | <104 | |
| F. tularensis subsp. tularensis | ATCC 6223 | 1 | <104 |
| FOA | 12 | <104 | |
| F. tularensis subsp. novicida | ATCC 15482 | 1 | >107 |
| WIS 223 | 1 | >107 | |
| F. philomiragia | ATCC 25015, 25016, 25017 | 3 | >107 |
| Brucella melitensis | WIS 163, 165, 166, 167 | 4 | >107 |
| Brucella abortus | ATCC 23448; WIS 181, 182 | 3 | >107 |
| Brucella suis | ATCC 23444, 23 445, 23446, 23447 | 4 | >107 |
| Brucella canis | WIS 51 | 1 | >107 |
| Brucella neotomae | WIS 225 | 1 | >107 |
| Yersinia pestis | ATCC 19428 | 1 | >107 |
| Yersinia pseudotuberculosis | WIS 171, 175, 179 | 3 | >107 |
| Burkholderia cepacia | DSM P 154 | 1 | >107 |
| Burkholderia pseudomallei | WIS 203 | 1 | >107 |
| Burkholderia mallei | WIS 204 | 1 | >107 |
| Klebsiella ozaneae | IMB B 246, 248 | 2 | >107 |
| Klebsiella pneumoniae | IMB B 235, 245 | 2 | >107 |
| E. coli | |||
| O:26; O:91; O:111; O:118 | IMB B239, 237, 238, 241 | 1 | >107 |
| O:157 | IMB B240, 243, 244; ATCC 11775 | 4 | >107 |
| Staphylococcus aureus | WIS B115 | 1 | >107 |
Bacteria were adjusted to an OD560 of 1.0 (approximately 109 bacteria/ml), and LPS was solubilized as described in Materials and Methods. Dilutions of the antigen corresponding to 10 to 107 bacteria/ml were studied for reactivity in cELISA. An OD450 of >0.1 in cELISA was considered positive. WIS, Federal Armed Forces Scientific Institute for Protection Technologies and NBC Protection, Munster, Germany; BTB, Federal Institute for Control of Infectious Diseases of Animals, Mödling, Austria; FOA, National Defence Research Establishment, Umea, Sweden; DSM, German Collection of Microorganisms and Cell Cultures, Braunschweig, Germany; IMB, Institute of Microbiology, Federal Armed Forces Medical Academy, Munich, Germany.
Tissue samples.
Spleen, lung, and kidney specimens from European brown hares found dead or ill during an F. tularensis epizootic period of tularemia in northeast Austria during the spring of 1997 were investigated. The primary identification of the bacteria was performed by direct cultivation and indirect immunofluorescence assays, as well as by a slide agglutination assay with a specific polyclonal antiserum as described elsewhere (9).
Tissue samples (about 0.5 to 1.0 cm3) from the hares were transferred to a fivefold volume of PBS and cut with scissors into small pieces. After a 5-min sedimentation of the remaining larger tissue particles, the supernatants were removed and stored frozen.
Extraction of LPS of F. tularensis.
The lipopolysaccharide (LPS) antigen was solubilized by incubating isolated bacteria (Table 1) or 0.5 ml of cut tissue samples in extraction buffer (Abbott, Solna, Sweden) at a ratio of 1:5 and boiling them for 15 min. Insoluble material was removed either by passing the suspension through 0.2-μm-pore-size filters or by centrifugation at 1,000 × g for 10 min. To create a standard curve, LPS was extracted from 109 bacteria (LVS) and serial dilutions were prepared corresponding to an LPS content of 107 to 103 bacteria/ml.
Antibodies.
The MAbs directed against F. tularensis had been developed as described previously (8). Selected MAbs were produced in serum-free medium at concentrations of approximately 500 to 1,000 μg/ml with a Miniperm bioreactor (Heraeus, Hanau, Germany). The MAb Ft-11 of immunoglobulin G1 (IgG1) isotype was purified by protein A affinity chromatography by a standard protocol and biotinylated with the Biotin Labeling kit (Boehringer, Mannheim, Germany). The MAb Ft-27 of IgM isotype was concentrated to 2 mg/ml by stirring it in a concentrator chamber containing a 100-kDa cutoff filter membrane (Amicon, Gloucestershire, United Kingdom) and was extensively dialyzed against PBS.
Western blotting.
Inactivated LVS samples were adjusted to an OD560 of 2.5. The samples were mixed at a 1:2 ratio with electrophoresis sample buffer (Novex, Frankfurt, Germany) and 5% mercaptoethanol. After 15 min of boiling, the solution was centrifuged for 20 min at 400 × g and submitted to sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis with a 4 to 20% separating Tris-glycine gel (Novex). The gel was electrotransferred onto a nitrocellulose membrane (0.45 μm) at 30 V for 1 h (Novex). The membrane was blocked with 5% skim milk in Tris-buffered saline (pH 8.1) overnight at 4°C. MAbs were incubated with membrane strips at 5 μg/ml in PBS–10% goat serum at room temperature for 2 h. For specificity control, the MAbs were preincubated with PBS or extracted LPS from various numbers of F. tularensis LVS overnight at room temperature. After three washes, the membranes were incubated with goat anti-mouse immunoglobulin-peroxidase (Dako, Glostrup, Denmark) or goat anti-human immunoglobulin-peroxidase (Sigma, St. Louis, Mo.) at room temperature for 1 h followed by substrate reaction with precipitating tetramethylbenzidine (Seramun, Dolgenbrodt, Germany).
cELISA.
For cELISA, a 96-well microplate (Maxisorb; Nunc, Roskilde, Denmark) was coated with 100 μl of the MAb Ft-27 at 10 μg/ml in carbonate buffer (pH 9.0) overnight. The plate was washed and blocked at 37°C for 30 min with PBS containing 0.05% Tween 20 and 4% skim milk powder. Antigen was diluted in dilution buffer (PBS with 0.05% Tween 20 and 2% skim milk) and incubated at 37°C for 60 min. After being washed, the bound antigen was incubated with 100 μl of biotinylated Ft-11 per well at 2 μg/ml at 37°C for 60 min. After being washed, 100 μl of streptavidin-peroxidase (Dako) diluted in dilution buffer at 1:4,000 was added and incubated at 37°C for another 60 min. The plate was washed, and 100 μl of tetramethylbenzine substrate (Seramun) was added and incubated at 37°C for 10 min. The OD was read with a photometer (Digiscan; AsysHitech, Eugendorf, Austria) at wavelengths of 450 and 620 nm as references.
Immunochromatographic HHA.
The HHAs and the antibodies used to manufacture them were produced at the Naval Medical Research Institute. This assay employs an affinity-purified polyclonal antibody and a MAb with an isotype of IgG3. The specificity of the MAb is for LPS of F. tularensis LVS.
The HHA used the same antigen preparations as were used for the cELISA. Diluted samples were mixed at 1:2 in PBS containing 0.1% Triton X-100 and 0.1% sodium azide (pH 7.4). Two hundred microliters of the sample was pipetted into the starting chamber of the device, where specific gold-labeled MAbs were placed, and reacted with the F. tularensis antigen. Complexed and free antibodies migrated through a nitrocellulose membrane by capillary forces. The detection window contained a line of coated specific anti-F. tularensis rabbit antibody and further downstream a control line of coated anti-mouse immunoglobulin. The result was visually determined as a relative intensity of the specific line after 15 min, when the control line was completely developed (1).
Preparation of DNA and PCR.
In order to isolate DNA, two different protocols for treatment of tissue and spiked serum samples prior to PCR were assessed. For method A, a 400-μl aliquot of ground tissue slurry or of spiked serum was mixed with 50 μl of TEN buffer (100 mM Tris, 10 mM EDTA, 1 M NaCl, pH 8.0), 20 μl of SDS (20% [wt/vol]), and 50 μl of proteinase K (1 mg/ml) and incubated at 56°C for 3 to 5 h. After two phenol extractions followed by two extractions with chloroform-isoamyl alcohol (24:1), the DNA was ethanol precipitated. The pellet was washed twice with 70% ethanol and resuspended in 20 μl of water. Method B was applied for spiked serum samples only. Lysis buffer (50 mM Tris, 1 mM EDTA, 0.5% Tween 20 [pH 8.0]; 190 μl) and 10 μl of proteinase K (1 mg/ml) were added to 200 μl of spiked serum. Incubation at 56°C for 3 h was followed by 10 min at 95°C to inactivate the proteinase K. The PCR was performed as described by Sjöstedt (18) with 1 μl of DNA template prepared by either method A or B and 40 cycles of amplification with primers specific for sequences of the gene encoding a 17-kDa lipoprotein, TUL 4 (13). After amplification, 5 μl of each reaction mixture was analyzed on a 2% agarose gel.
RESULTS AND DISCUSSION
Development and evaluation of the cELISA.
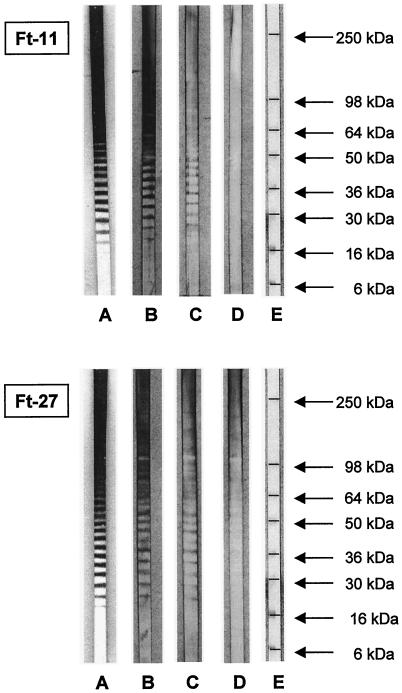
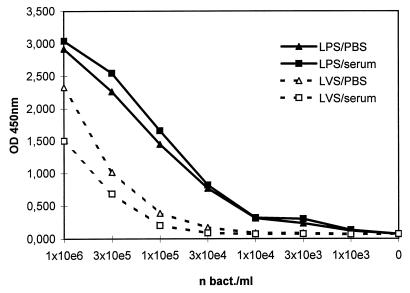
Two specific murine MAbs to F. tularensis (8), Ft-11 (IgG1) and Ft-27 (IgM), were utilized for the cELISA. Both MAbs reacted strongly with the LPS of F. tularensis as shown by Western blot analysis (Fig. 1). The reactivity of the MAbs could be blocked by free LPS of F. tularensis in a concentration-dependent fashion, indicating the specificity of the binding. A key step in the configuration of the assay was the extraction of the LPS from the bacteria. Compared to the crude bacterial preparation, a 10-fold increase in sensitivity was achieved with cELISA (Fig. 2). Furthermore, the handling of infectious material was reduced by this first step of the assay, as the LPS extraction was accompanied by inactivation of the bacteria. This procedure was the method of choice, as it also allowed the lysis of eukaryotic cells, which is important for the availability of intracellularly localized bacteria.
FIG. 1.
Western blot of LPS-specific MAbs to F. tularensis. Whole bacterial antigen of F. tularensis was separated by SDS-polyacrylamide gel electrophoresis with 4 to 20% Tris-glycine gel and blotted onto a nitrocellulose membrane. The MAbs Ft-27 and Ft-11 were used at 5 μg/ml in PBS (A). For specificity control, the MAbs were preincubated with extracted LPS from 104 (B), 106 (C), and 108 (D) bacteria/ml (lane E, molecular mass markers).
FIG. 2.
Comparison of detection of whole bacteria and extracted LPS of F. tularensis by cELISA. Serial dilutions of whole bacteria and extracted LPS antigen of F. tularensis LVS from spiked PBS and pooled human sera were tested in the LPS-specific cELISA. The results are given as OD450.
The sensitivity of the cELISA was proven with 26 strains of F. tularensis, including 3 reference strains obtained from the American Type Culture Collection (ATCC), 8 strains of F. tularensis subsp. holarctica isolated from European brown hares, and 13 strains of F. tularensis subsp. tularensis (type A [Table 1]). All tested isolates of F. tularensis except F. tularensis subsp. novicida were recognized. This underlines the unique LPS composition of both F. tularensis subsp. holarctica and F. tularensis subsp. tularensis, which is different from that of F. tularensis subsp. novicida (3, 19). No cross-reactivity with other tested bacteria, including Brucella spp., E. coli serotypes O:118 and O:157, and Yersinia spp., was observed. Therefore, a highly sensitive and specific cELISA for the diagnosis of tularemia was developed.
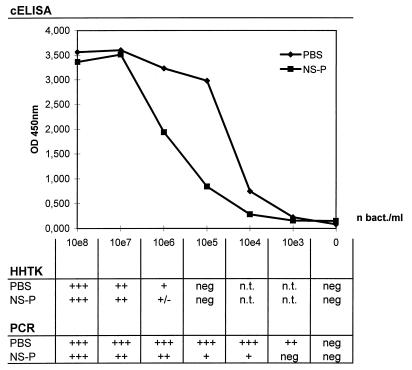
Detection limits of cELISA, HHA, and PCR.
In order to compare the sensitivities of the different assays used in this study, serial dilutions of F. tularensis LVS were prepared in PBS and in human sera from healthy donors, representing biological fluids which could contain inhibiting factors for the assays. The detection limit of the cELISA was 103 bacteria/ml in PBS and 104 bacteria/ml in human serum (Fig. 3). This represents detecting 102 and 103 bacteria/100 μl of sample. Further evaluation of the assay has revealed that the bacteria and the LPS antigen, respectively, could be detected in spiked human urine, sputum, and stool with nearly the same sensitivity (data not shown).
FIG. 3.
Sensitivity of cELISA, HHA, and PCR for the detection of F. tularensis. Serial dilutions of the solubilized LPS antigen of F. tularensis in PBS and in pooled human normal sera (NS-P) were tested in the specific cELISA (upper diagram). The results are given as OD450. The same dilutions of bacteria were tested in the immunochromatographic HHA and in the PCR (lower table). The results are expressed as relative intensity of obtained visible bands. +, light; ++, medium; +++, dark; neg, negative; n.t., not tested.
Using the same samples, the detection limit of the immunochromatographic assay was 106 and 106 to 107 bacteria per ml of PBS or human serum, respectively (Fig. 3). The required sample volume was 200 μl for this assay. The sensitivity could be increased to about 1 log10 unit after an extraction of LPS from bacteria, as used with the cELISA. Although the assay was completed within 15 min, specimens containing a high bacterial load produced a positive signal in less than 1 min. A longer incubation time did not increase the sensitivity of the assay. This assay is principally applicable to field diagnostic use due to its fast and easy performance.
In comparison, 102 bacteria/ml of PBS and 103 to 104 bacteria/ml of spiked serum, respectively, could be detected with the TUL4-specific PCR (Fig. 3).
Detection of F. tularensis in tissue specimens.
For further evaluation, the assays were applied to detect and quantify F. tularensis in tissue samples from dead or sick and killed European brown hares (Table 2). The bacteria were isolated by direct cultivation or were detected by immunofluorescence from 14 samples from hares (no. 3 to 16) and were classified as F. tularensis subsp. holarctica. In one case (no. 17) tularemia was diagnosed serologically by a slide agglutination assay. In two cases (no. 1 and 2) the bacteriological and serological studies remained negative. Eleven of the animals (no. 3 to 13) showed pathomorphologic signs of an acute septicemic tularemia with enlarged spleen. Pneumonia, pericarditis, or nephritis was observed in four animals (no. 14 to 17) and was considered to represent chronic forms of the disease. In 15 cases, spleen tissues were studied; in two cases, kidney or lung, respectively, was available.
TABLE 2.
Detection of F. tularensis in tissue samples of European brown haresa
| No. | Diagnosis | Course | Tissue | cELISA (106 bact/ml) | cELISA titer | HHA titer | PCR titer |
|---|---|---|---|---|---|---|---|
| 1 | Neg | Control | Spleen | Neg | Neg | Neg | Neg |
| 2 | Neg | Control | Spleen | Neg | Neg | Neg | Neg |
| 3 | Cult. | Acute-sept. | Spleen | 135.0 | 3.0 × 10−5 | 10−3 | 10−5 |
| 4 | Cult. | Acute-sept. | Spleen | 2.9 | 3.0 × 10−3 | 10−1 | 10−2 |
| 5 | Cult. | Acute-sept. | Lung | 3.0 | 5.0 × 10−3 | 10−2 | 10−6 |
| 6 | Cult. | Acute-sept. | Spleen | 140.3 | 1.6 × 10−5 | 10−4 | 10−6 |
| 7 | Cult. | Acute-sept. | Spleen | 3.9 | 5.0 × 10−3 | 10−2 | 10−5 |
| 8 | Cult. | Acute-sept. | Spleen | 66.5 | 1.0 × 10−4 | 10−3 | 10−5 |
| 9 | Cult. | Acute-sept. | Spleen | 55.2 | 1.0 × 10−4 | 10−3 | 10−5 |
| 10 | Cult. | Acute-sept. | Spleen | 57.5 | 8.0 × 10−4 | 10−3 | 10−7 |
| 11 | IFA | Acute-sept. | Spleen | 1.1 | 3.0 × 10−3 | 10−1 | 10−3 |
| 12 | IFA | Acute-sept. | Spleen | 3.0 | 1.0 × 10−3 | 10−2 | 10−4 |
| 13 | IFA | Acute-sept. | Spleen | 7.0 | 1.0 × 10−4 | 10−2 | 10−3 |
| 14 | Cult. | Chron. | Spleen | 0.1 | 1.0 × 10−2 | Neg | Neg |
| 15 | Cult. | Chron. | Kidney | 0.3 | 1.6 × 10−2 | Neg | 10−4 |
| 16 | IFA | Chron. | Spleen | 0.3 | 3.0 × 10−2 | Neg | Neg |
| 17 | Serol. | Chron. | Spleen | 0.1 | 3.0 × 10−2 | Neg | 10−1 |
Diagnosis of tularemia was made by culturing bacteria (cult.), by immunofluorescence assay (IFA), or by antibody detection in serum (serol.). Depending on the pathomorphological picture, acute-septicemic (acute-sept.) and chronic (chron.) courses of the infection were identified. The number of bacteria per milliliter (bact./ml) was calculated from the standard curve of the cELISA. The results of the HHA and the PCR were obtained by registration of the last visible band in the assays. Neg, negative.
Two samples (no. 1 and 2) found to be negative after cultivation or by the immunofluorescence technique were also found to be negative in all three assays evaluated in this study. Fifteen of 15 tissue samples from infected hares were also identified as positive in cELISA, revealing a 100% agreement with the first diagnosis. Eleven of 15 samples were found to be positive with the HHA, and 13 of 15 samples were detected by PCR. The bacterial load, calculated from the standard curve of LVS created by the cELISA, had a broad range, between 108 bacteria and 105 bacteria/ml of suspended tissue. Negative results with the HHA and PCR were obtained for tissue samples with a low bacterial load from hares suffering from a chronic form of the disease. The endpoint titers for the cELISA and PCR were quite similar, whereas those of the HHA were significantly lower. The reason for the high sensitivity of the cELISA might be the high stability of LPS, as has been previously experienced with long-term storage of LPS and from studies of autolysated tissues (data not shown).
In conclusion, the HHA could be used as a field approach for the diagnosis of tularemia in emergent situations due to its simple application. However, because of its relatively low sensitivity, negative results obtained with this assay do not allow the exclusion of tularemia. Therefore, each suspect sample should be investigated by more sensitive laboratory methods, such as the highly sensitive cELISA and PCR. Conventional diagnostic tools, such as cultivation, immunofluorescence, and agglutination assays, are less sensitive, more time-consuming, and hazardous.
ACKNOWLEDGMENTS
As listed in Table 2, bacteria were kindly provided by A. Sjöstedt (FOA, Umea, Sweden) and B. Niederwöhrmeier (WIS, Munster, Germany). We also thank Gudrun Zöller, Mandy Macholeth, Ulli M. Hohenester, and Rudi Kühn for excellent technical assistance, as well as Gale Brightwell and David Pulford (DERA Porton Down, United Kingdom) for reviewing the English language.
REFERENCES
- 1.Burans J, Keleher A, O'Brien T, Hager-Aldrich J, Plummer A, Morgan C. Rapid method for the diagnosis of Bacillus anthracis infection in clinical samples using a hand-held assay. Salisbury Med Bull Special Suppl. 1996;87:36–37. [Google Scholar]
- 2.Carlsson H E, Lindberg A A, Lindberg G, Hederstedt B, Karlsson K A, Agell B O. Enzyme-linked immunosorbent assay for immunological diagnosis of human tularemia. J Clin Microbiol. 1979;10:615–621. doi: 10.1128/jcm.10.5.615-621.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cowley S C, Myltseva S V, Nano F E. Phase variation in Francisella tularensis affecting intracellular growth, lipopolysaccharide antigenicity and nitric oxide production. Mol Microbiol. 1996;20:867–874. doi: 10.1111/j.1365-2958.1996.tb02524.x. [DOI] [PubMed] [Google Scholar]
- 4.Downs C M, Bond G C. Studies on the cultural characterization of Pasteurella tularense. J Bacteriol. 1935;30:485–490. doi: 10.1128/jb.30.5.485-490.1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Evans M E, Gregory D W, Schaffner W, McGee Z A. Tularemia. A 30-year experience with 88 cases. Medicine. 1985;64:251–269. [PubMed] [Google Scholar]
- 6.Forsman M, Sandström G, Sjöstedt A. Analysis of 16S ribosomal DNA sequences of Francisella strains and utilization for determination of the phylogeny of the genus and for identification of strains by PCR. Int J Syst Bacteriol. 1994;44:38–46. doi: 10.1099/00207713-44-1-38. [DOI] [PubMed] [Google Scholar]
- 7.Forsman M, Kuoppa K, Sjöstedt A, Tärnvik A. Use of RNA hybridization in the diagnosis of a case of ulceroglandular tularemia. Eur J Microbiol Infect Dis. 1990;9:784–785. doi: 10.1007/BF02184697. [DOI] [PubMed] [Google Scholar]
- 8.Greiser-Wilke I, Soine C, Moenning V. Monoclonal antibodies reacting specifically with Francisella sp. J Vet Med. 1989;36:593–600. doi: 10.1111/j.1439-0450.1989.tb00650.x. [DOI] [PubMed] [Google Scholar]
- 9.Hofer E, Schildorfer H, Flatscher J, Müller M. Detection of tularemia in European brown hares (Lepus europaeus) in Austria. Wien Tierärztl Monatsschr. 1997;84:301–306. [Google Scholar]
- 10.Hollis D G, Weaver R E, Steigerwalt A G, Wenger J D, Moss C W, Brenner D J. Francisella philomiragia comb. nov. (formerly Yersinia philomiragia) and Francisella tularensis biogroup novicida (formerly Francisella novicida) associated with human disease. J Clin Microbiol. 1989;27:1601–1608. doi: 10.1128/jcm.27.7.1601-1608.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hornick R B, Eigelsbach H T. Aerogenic immunization of man with live tularemia vaccine. Bacteriol Rev. 1966;30:532–538. doi: 10.1128/br.30.3.532-538.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koskela P, Salminen A. Humoral immunity against Francisella tularensis after natural infection. J Clin Microbiol. 1985;22:973–979. doi: 10.1128/jcm.22.6.973-979.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Long G W, Oprandy J J, Narayanan R B, Fortier A H, Portier K R, Nacy C A. Detection of Francisella tularensis in blood by polymerase chain reaction. J Clin Microbiol. 1993;31:152–154. doi: 10.1128/jcm.31.1.152-154.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olsufjev N G, Meshcheryakova I S. Subspecific taxonomy of Francisella tularensis McCoy and Chapin 1912. Int J Syst Bacteriol. 1983;33:872–874. [Google Scholar]
- 15.Olsufjev N G. Tularemia. 1974. Presented at the WHO Inter-regional traveling seminar on natural foci of zoonoses. Moscow, USSR. [Google Scholar]
- 16.Sandström G E, Wolf-Watz H, Tärnvik A. Duct ELISA for detection of bacteria in fluid samples. J Microbiol Methods. 1986;5:41–47. [Google Scholar]
- 17.Sandström G. The tularemia vaccine. J Chem Tech Biotechnol. 1994;59:315–320. doi: 10.1002/jctb.280590402. [DOI] [PubMed] [Google Scholar]
- 18.Sjöstedt A, Eriksson U, Berglund L, Tärnvik A. Detection of Francisella tularensis in ulcers of patients with tularemia by PCR. J Clin Microbiol. 1997;35:1045–1048. doi: 10.1128/jcm.35.5.1045-1048.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vinogradov E V, Shashkov A S, Knirel Y A, Kochetkov N K, Tochtamysheva N V, Averin S F, Goncharova O V, Khlebnikov V S. Structure of O-antigen of Francisella tularensis strain 15. Carbohydr Res. 1991;214:289–297. doi: 10.1016/0008-6215(91)80036-m. [DOI] [PubMed] [Google Scholar]