Highlights
-
•
Laparoscopic right hemicolectomy is performed only in 25% of cases in recent survey
-
•
The medial-to-lateral and the bottom-to-up are the most frequent approaches used to perform surgery
-
•
Top-to-down right hemicolectomy is an infrequent approach
-
•
Obesity is an evident aspect complicating surgical dissection
-
•
Top-to Down dissection could be an opportunity to use as alternative approach when classical dissection becomes intricate
Keywords: Laparoscopy, colon cancer, Colorectal, Right hemicolectomy, Right colon, Complete mesocolic excision, CME
Abstract
Introduction and importance
Right colon cancer represents 30 % of colonic malignancies worldwide, and a laparoscopic approach is recommended. Recent surveys show that only 25 % of surgeons perform right hemicolectomies by laparoscopy. Contemporary obesity is rising, and besides being a risk factor for colon cancer, it represents an objective difficulty in performing surgery. These two factors imply a constant and progressive issue facing surgeons.
Case presentation
We describe the case of a 61Y/o woman with 32BMI, a previous left nephrectomy, and neoformation of the right colonic. She underwent laparoscopic right hemicolectomy, using a hybrid top-to-down approach to overcome intraoperative difficulty, consequent to visceral obesity. The postoperative course was uneventful, and she was discharged after five days.
Clinical discussion
The medial-to-lateral approach is the main technique used in laparoscopic right hemicolectomy. Some other techniques are used to perform this intervention, and the top-to-down strategy is adopted only in 4 % of cases. In obese patients, difficulties could be found in vascular and plan dissection. The top-to-down strategy allowed us to deal with some objective difficulties during the procedure, efficiently bypassing them.
Conclusion
Laparoscopy for right colon cancer would be the standard procedure as recommended. Some objective difficulty could be found during interventions, especially in obese patients. The top-to-down dissection is not so frequent and could be considered to deal with intraoperative difficulty. The knowledge of all different strategies and their application might be a possible interchangeably way to solve difficult dissection and increase the spreading of laparoscopy.
1. Introduction
Colorectal cancer represents the third most common type of tumor worldwide. The World Health Organization estimates 1.93 million cases in 2020 and identifies it as the second cause of cancer death after lung cancer [1].
About 30 % of colon cancer are located in the right colon, 5,8 % in the transverse colon, and 64 % in the left colon [2]. Surgery remains the standard of care in treating colon cancer, with a strong recommendation (Level 1A) for a “minimally invasive approach” [3]. Still, a recent international survey underlines “the gap between guidelines and reality”, where over half of responders perform laparoscopic right hemicolectomy in less than 25 % of cases [4]. The most frequent technique used in the dissection is the medial-to-lateral (MTL) approach (74 %), followed by the inferior lateral-to-medial approach 20,5 %, and the superior lateral-to-medial in 4,1 %. Epidemiological studies show that obesity increases colorectal cancer risk, especially in men [5], and data from the Center of Disease Control and Prevention reveal an increasing prevalence of obesity in the last years from 30,5 % (1999–2000) to 41,9 % [6]. Obesity in laparoscopy does not seem to impact the lymph node retrieval [7], the minimally invasive procedure's feasibility and safety. Still, some objective difficulties could be found during interventions, like anastomosis time [8]. The persistent increase in obesity and simultaneous colorectal cancer implies an increase in laparoscopic procedures in these patients that surgeons need to deal with. We discuss the opportunity to use an alternative approach to overcome some technical difficulties during interventions.
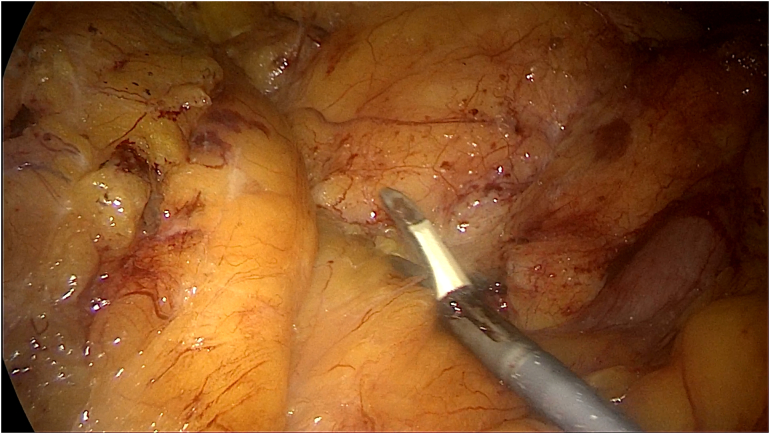
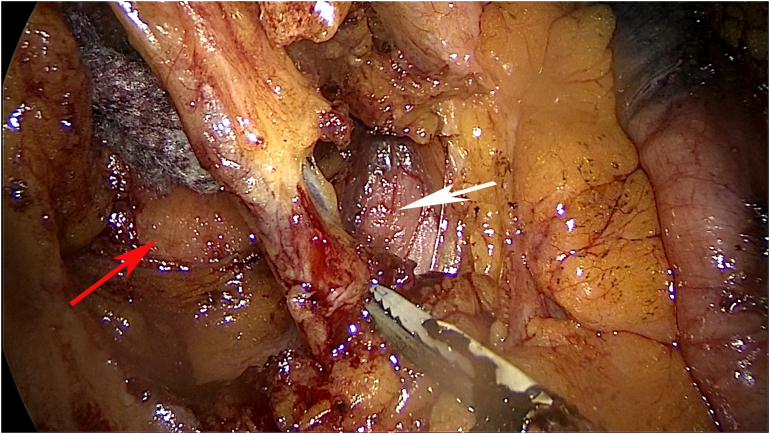
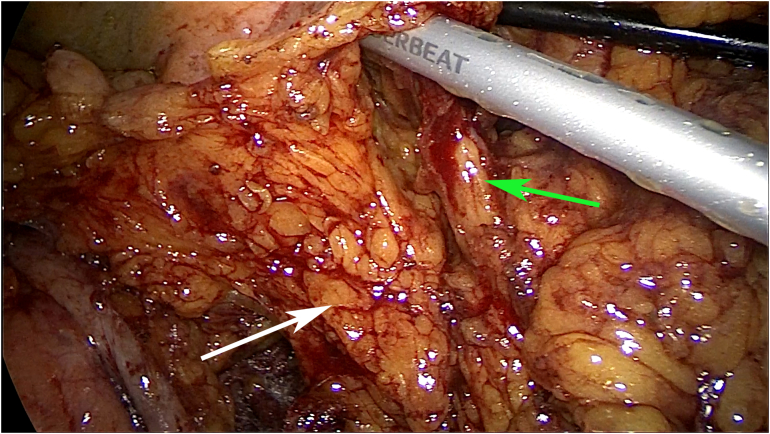
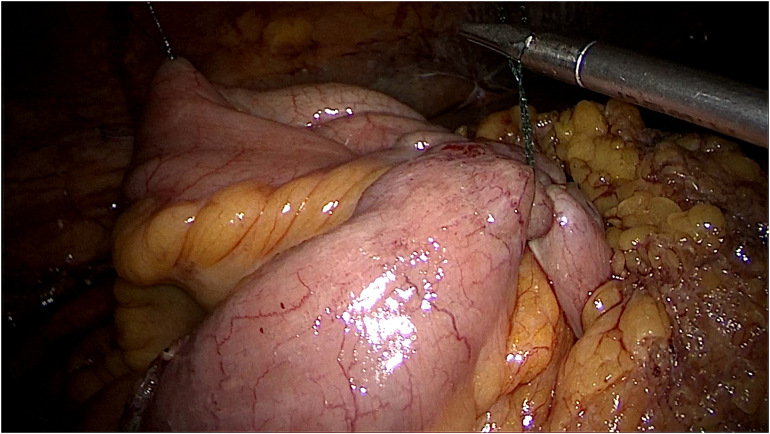
2. Case presentation
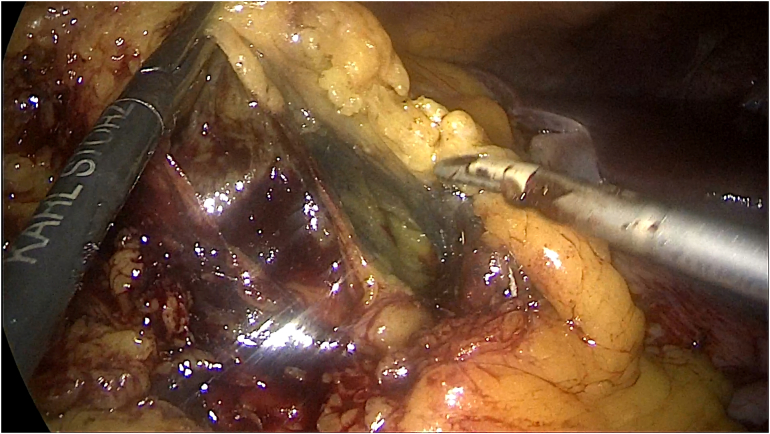
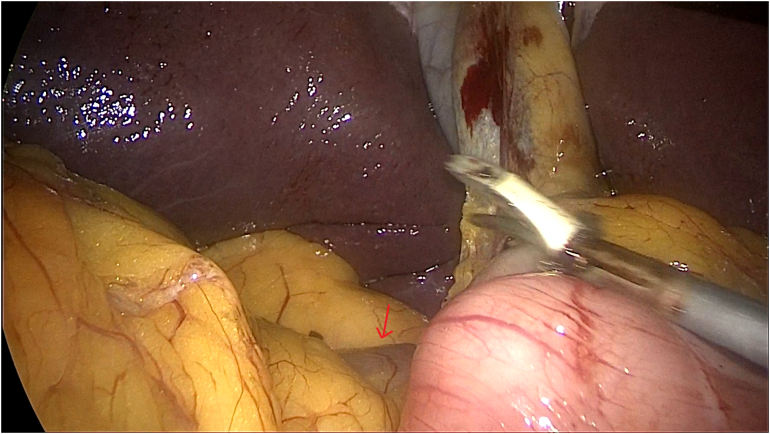
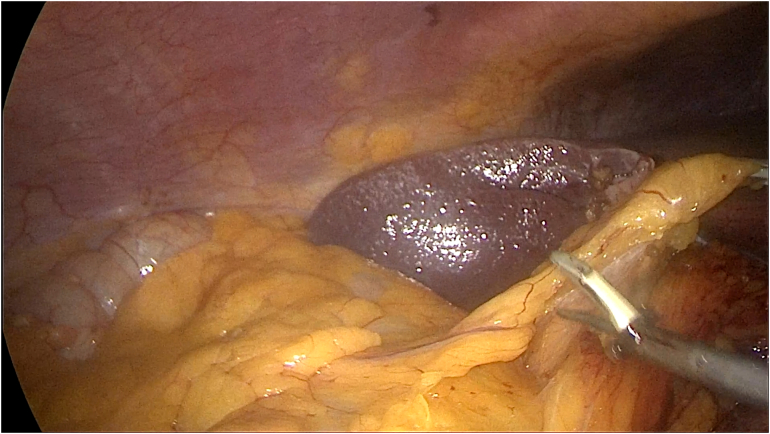
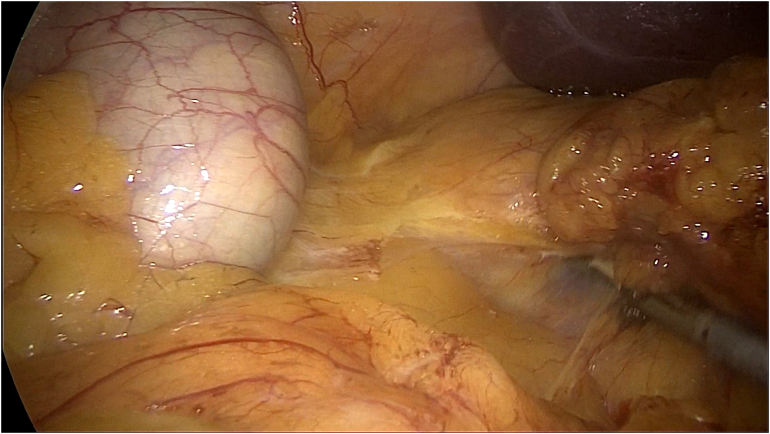
We describe the case of a 61Y/o woman with a history of left nephrectomy for chronic pyelonephritis, sleep apnoea treated with positive airway pressure therapy, obesity with a 32 BMI, hypothyroidism, and mild hypertension. During a follow-up colonoscopy, a 3,5 cm flat polyp of the right flexure was discovered with a pit-patter 3 s on Kudo Classification [9], and a preliminary biopsy showed high-grade dysplasia. A second colonoscopy was planned for an endoscopic submucosal dissection. Due to the impossibility of lifting the lesion, with the risk of non-en-block dissection and perforation [10], [11], the procedure was interrupted, and endoscopic marking was done 5 cm distal to the lesion. The multidisciplinary team discussed the patient and indicated a D2 right hemicolectomy for suspicious adenocarcinoma. A preoperative CT scan was negative for other lesions. Laparoscopy was performed with the patient in the supine position. Three 12 mm trocar and one 5 mm trocar were used: umbilical for the optic, left inferior, and left lateral; the smallest one at xiphoid. After dissection of omental adhesions to the abdominal wall, the first approach revealed difficulty moving the small bowel in the left abdominal quadrants due to the previous intervention and rugged traction to lift the right colon to expose the mesentery. The great omentum was separated until the marked colon (Fig. 1). Dissection of adhesions between transverse colon and gallbladder was achieved till the exposition of the duodenal bulb (Fig. 2). The omentum was dissected following the line joining the two mentioned points (Fig. 3). The duodenal bulb was used as a marker to start the separation of the right mesocolon from the Gerota fascia (Fig. 4). The dissection carried on from the top of the hepatic flexure down to the retrociecal area. This maneuver allowed a progressive detachment of the second and third duodenal portions and the pancreatic head (Fig. 5). Mobilizing the ileal mesentery allowed adequate traction with the easier exposition of the ileocolic pedicle. Mediolateral dissection of the ileocolic mesentery was done, directly joining the Toldt plane and the duodenum and sectioning the vascular pedicle (Fig. 6). Following the line of conjunction between the marked colon and the ileocolic pedicle allowed to expose the right colic pedicle and the right branch of the middle colic artery till the origin (Video demonstration) (Fig. 7). After the transverse colon and the terminal ileus stapler section, the specimen was inserted in an endobag. Intracorporal side-to-side anastomosis was done (Fig. 8), and drainage was placed. The specimen was extracted by Pfannenstiel incision. The postoperative course was uneventful, and the patient was discharged after five days. The histology showed high-grade dysplasia in flat adenoma with 22 lymph nodes harvested. The work has been reported in line with both SCARE and PROCESS Guidelines [12], [13], [14].
Fig. 1.
Separation of the omentum until the marked colon.
Fig. 2.
Duodenal bulb exposed: Red arrow = Duodenal bulb. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
omental dissection following the line joining the marked area of the transverse colon and the duodenum.
Fig. 4.
Dissection of the mesocolon from the Gerota fascia starting from duodenal bulb.
Fig. 5.
Mobilization of the right colon starting from the hepatic flexure down to the retrociecal area with contemporary detachment of the duodenum and pancreatic head.
Fig. 6.
Isolation of the ileocolic pedicle through the mesocolon with direct vision of Toldt-Gerota fascia and duodenum. Red arrow = Gerota fascia; White arrow = duodenum. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 7.
Exposition of the right colic pedicle and the right branch of the middle colic artery till the origin. White arrow = Right colic pedicle; Green arrow = Right branch of the middle colic pedicle. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 8.
Intracorporal side-to-side anastomosis.
3. Discussion
Colorectal interventions are the most frequent surgeries in the abdominal cavity. The majority of surgeons perform right hemicolectomy with the medial-to-lateral approach. Strey [15] well described this procedure by imagining the dissection as flipping through the “page of a book” to achieve a correct plan. The second most frequent type of dissection is the bottom-up (caudal-to-cranial) approach, first described by Zou [16] for laparoscopic resection and by Schulte [17] for robotic surgery. These letters describe a more accessible practice, particularly for complete mesocolic excision. The top-to-bottom procedure is an unusual procedure used only in 4 % of cases. Levard [18], in 2012, first described this technique to emphasize vascular variation and its approach, and other authors [19] described a hybrid medial approach in a top-to-down manner. This hybrid technique involves ligating the right mesenteric pedicle and right middle colic pedicle from above. Still, it reveals to be more dangerous compared to the medial-to-lateral approach. And again, more complications are reported in the MTL approach compared to the caudal-to-cranial one [20]. Debating the different approaches that could be used in the right laparoscopic hemicolectomy, some objective difficulties could be found, especially in obese patients [21]. During the dissection of the ileocolic pedicle in the MTL approach, difficulty in finding the correct plane between the Toldt and Gerota fascia and maintaining it could be frequent. Problems could be found in maintaining the suspension of the mesocolon during the dissection due to its redundancy. Moreover, the fat could hide the structures behind it in a dangerous manner. The case we describe wants to show a hybrid approach by using, in the beginning, the top-to-down dissection to separate the different plans, facilitating the vascular dissection. This first approach allows more accessible and immediate visualization of the Toldt-Gerota window and third duodenum in the following medial-to-lateral dissection. It also allows a more effective traction on the terminal ileus and transverse colon to pursue the dissection. Considering the continuous increase of obese patients, surgeons will have to deal more and more with this technical difficulty. The knowledge of all the strategies to facilitate and overcome critical issues could be an important way to spread laparoscopy.
4. Conclusion
Even if laparoscopy in the right hemicolectomy is considered the standard procedure, it is not as frequent as expected. Different approaches could be used to solve some intraoperative problems during the dissection or anastomotic creation. The knowledge of all different strategies and their application could be a possible interchangeably way to solve difficult dissection.
The following is the supplementary data related to this article.
Top to Down Right Hemicolectomy Banchini
Sources of funding
No found sources.
Ethical approval
No ethical approval is required, because it is a single case report and the patient signed consent form for publication.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Banchini* Filippo: Conceptualization, Performed surgical Itervention, Methodology, Software, Resources, Writing - Original Draft, Writing - Review & Editing, Visualization, Supervision, Project administration.@
Luzietti Enrico: Writing - Review & Editing.
Romboli Andrea: Writing - Review & Editing.
Palmieri Gerardo: Writing - Review & Editing.
Conti Luigi: Writing - Review & Editing.
Capelli Patrizio: Writing - Review & Editing.
Research registration
Not applicable.
Guarantor
Banchini Filippo.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors Banchini Filippo; Luzietti Enrico; Romboli Andrea; Palmieri Gerardo; Conti Luigi; Capelli Patrizio, all declare that thay have no conflict of interest.
References
- 1.https://www.who.int/news-room/fact-sheets/detail/cancer
- 2.Mangone L., Pinto C., Mancuso P., Ottone M., Bisceglia I., Chiaranda G., Michiara M., Vicentini M., Carrozzi G., Ferretti S., Falcini F., Hassan C., Rossi P.G. Colon cancer survival differs from right side to left side and lymph node harvest number matter. BMC Public Health. 2021;21:906. doi: 10.1186/s12889-021-10746-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vogel J.D., Felder S.I., Bhama A.R., Hawkins A.T., Langenfeld S.J., Shaffer V.O., Thorsen A.J., Weiser M.R., Chang G.J., Lightner A.L., Feingold D.L., Paquette I.M. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of colon cancer. Dis. Colon Rectum. 2022;65:148–177. doi: 10.1097/DCR.0000000000002323. [DOI] [PubMed] [Google Scholar]
- 4.Al-Taher M., Okamoto N., Mutter D., Stassen L.P.S., Marescaux J., Diana M., Dallemagne B. International survey among surgeons on laparoscopic right hemicolectomy: the gap between guidelines and reality. Surg. Endosc. 2022;36:5840–5853. doi: 10.1007/s00464-022-09044-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim H. Sex differences in the association of obesity and colorectal cancer risk. Cancer Causes Control. 2017;4 doi: 10.1007/s10552-016-0831-5. [DOI] [PubMed] [Google Scholar]
- 6.https://www.cdc.gov/obesity/data/adult.html#:~:text=The%20obesity%20prevalence%20was%2039.8,adults%20aged%2060%20and%20older
- 7.Linebarger J.H., Shapiro S.B. Does obesity impact lymph node retrieval in colon cancer surgery? Am. J. Surg. 2010;200:5. doi: 10.1016/j.amjsurg.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Manigrasso M. Safety and efficacy of totally minimally invasive right colectomy in the obese patients: a multicenter propensity score-matched analysis. Updat. Surg. 2022;10 doi: 10.1007/s13304-022-01298-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kudo S., Tamura S., Nakajima T., Yamano H., Kusaka H., Watanabe H. Diagnosis of colorectal tumorous lesions by magnifying endoscopy. Gastrointest. Endosc. 1996;44:8–14. doi: 10.1016/s0016-5107(96)70222-5. [DOI] [PubMed] [Google Scholar]
- 10.Hirasaki S., Kozu T., Yamamoto H., Sano Y., Yahagi N., Oyama T., Shimoda T., Sugano K., Tajiri H., Takekoshi T., Saito D. Usefulness and safety of 0.4% sodium hyaluronate solution as a submucosal fluid “cushion” for endoscopic resection of colorectal mucosal neoplasms: a prospective multi-center open-label trial. BMC Gastroenterol. 2009;9:1. doi: 10.1186/1471-230X-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pimentel-Nunes P., Dinis-Ribeiro M., Ponchon T., Repici A., Vieth M., De Ceglie A., Amato A., Berr F., Bhandari P., Bialek A., Conio M., Haringsma J., Langner C., Meisner S., Messmann H., Morino M., Neuhaus H., Piessevaux H., Rugge M., Saunders B., Robaszkiewicz M., Seewald S., Kashin S., Dumonceau J.-M., Hassan C., Deprez P. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2015;47:829–854. doi: 10.1055/s-0034-1392882. [DOI] [PubMed] [Google Scholar]
- 12.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Miguel D., Pagano D., Millham F.H., Roy G., Kadioglu H., Nixon I.J., Mukherjee I., McCaul J.A., Ngu J.Chi-Yong, Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., Wilde R.L.De, Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Kasivisvanathan V., Mei Z., Karanth V.K.L. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 13.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O'Neill N., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Pagano D., Roy G., Kadioglu H., Nixon I.J., Mukhejree I., McCaul J.A., Ngu J.Chi-Yong, Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Mei Z., Karanth V.K.L. The PROCESS 2020 guideline: updating consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guidelines. Int. J. Surg. 2020;84:231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P., Zhu H., Alsawadi A., Noureldin A., Rao A., Enam A., Thoma A., Bashashati M., Vasudevan B., Beamish A., Challacombe B., Wilde R.L.De, Machado-Aranda D., Laskin D., Muzumdar D., D’cruz A., Manning T., Healy D., Pagano D., Goel P., Ranganathan P., Pai P.S., Raja S., Ather M.H., Kadioäžlu H., Nixon I., Mukherjee I., Rivas J.Gómez, Raveendran K., Derbyshire L., Valmasoni M., Chalkoo M., Raison N., Muensterer O., Bradley P., Coppola R., Afifi R., Rosin D., Klappenbach R., Wynn R., Giordano S., Basu S., Surani S., Suman P., Thorat M., Kasi V. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 15.Strey C.W., Wullstein C., Adamina M., Agha A., Aselmann H., Becker T., Grützmann R., Kneist W., Maak M., Mann B., Moesta K.T., Runkel N., Schafmayer C., Türler A., Wedel T., Benz S. Laparoscopic right hemicolectomy with CME: standardization using the “critical view” concept. Surg. Endosc. 2018;32:5021–5030. doi: 10.1007/s00464-018-6267-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.L. Zou W. Xiong D. Mo Y. He H. Li P. Tan W. Wang J. Wan Laparoscopic Radical Extended Right Hemicolectomy Using a Caudal-to-Cranial Approach, (n.d.) 2. [DOI] [PubMed]
- 17.Schulte am Esch J., Iosivan S.-I., Steinfurth F., Mahdi A., Förster C., Wilkens L., Nasser A., Sarikaya H., Benhidjeb T., Krüger M. A standardized suprapubic bottom-to-up approach in robotic right colectomy: technical and oncological advances for complete mesocolic excision (CME) BMC Surg. 2019;19:72. doi: 10.1186/s12893-019-0544-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levard H., Denet C., Gayet B. Laparoscopic right colectomy from top to bottom. J.Visceral Surg. 2012;149:e34–e37. doi: 10.1016/j.jviscsurg.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Feng B., Ling T.-L., Lu A.-G., Wang M.-L., Ma J.-J., Li J.-W., Zang L., Sun J., Zheng M.-H. Completely medial versus hybrid medial approach for laparoscopic complete mesocolic excision in right hemicolon cancer. Surg. Endosc. 2014;7 doi: 10.1007/s00464-013-3225-8. [DOI] [PubMed] [Google Scholar]
- 20.Li F., Zhou X., Wang B., Guo L., Wang J., Wang W., Fu W. Comparison between different approaches applied in laparoscopic right hemi-colectomy: a systematic review and network meta-analysis. Int. J. Surg. 2017;48:74–82. doi: 10.1016/j.ijsu.2017.10.029. [DOI] [PubMed] [Google Scholar]
- 21.Franklin A., Patterson A., Taylor J., Avery M., Pullatt R. Laparoscopic right hemicolectomy in a morbidly obese patient using a medial approach with an intracorporeal anastomosis. Am. Surg. 2015;81:301–302. doi: 10.1177/000313481508100803. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Top to Down Right Hemicolectomy Banchini