Abstract
Langerhans histiocytosis or Langerhans cell histiocytosis (LCH) is a rare benign pathology representing less than 1% of orbital tumors. It can cause either localized or generalized lesions, leading to the destruction of hard and soft tissues. Eosinophilic granuloma is the most benign form and the predominant clinical presentation of LCH. We report a case of eosinophilic granuloma with orbital involvement in an 18-year-old male patient. Orbital radiotherapy was initially planned, but finally it was not performed due to a spontaneous regression of the lesion after the incisional biopsy. The presented case supports an expectant attitude given the possibility of a spontaneous regression after the biopsy, especially in small lesions. However, long-term follow-up is essential given the risk of recurrence.
Keywords: Langerhans cell histiocytosis, orbital tumors, spontaneous regression, biopsy
Background
Langerhans histiocytosis or Langerhans cell histiocytosis (LCH), previously known as Histiocytosis X, is a rare pathology that affects children, and more rarely young adults.1 It represents less than 1% of orbital tumors.2 It’s a benign disease characterized by a proliferation of bone marrow-derived myeloid dendritic cells.3 It can cause either localized or generalized lesions, leading to the destruction of hard and soft tissues. The localized alternative of langerhans cell histiocytosis (LLCH), known as eosinophilic granuloma (EG), is the predominant clinical presentation of LCH. Clinical course and prognosis are unpredictable but some cases of spontaneously resolved LCH have been reported especially in localized forms.4
In this clinical case report, it is described a case of an 18-year-old male patient with EG of the left orbital roof that showed a spontaneous regression after biopsy without any additional treatment.
Case report
An 18 year-old patient had been referred to our center after discovering a left orbital mass. The physical examination found a tumor of the left superolateral orbit involving bone and dura associated to left exophthalmia. The cerebral computed tomography (CT) and magnetic resonance imaging (MRI) showed a superolateral extraconal tissular mass extending through the superior orbital fissure and along the dura mater, measuring 36.6 mm x 32.7 mm (Figure 1). A biopsy was performed. The histopathological examination disclosed clusters of Langerhans cells admixed with numerous eosinophils and osteoclast-like giant cells. Langerhans cells have grooved, indented and lobed nuclei with inconspicuous nucleoli. The cytoplasm is moderately abundant and slightly eosinophilic. On immunohistochemistry, Langerhans cells express S100 and CD1a (Figure 2). To assess the disease extension, a bone scintigraphy and a total body scan were performed and it did not show abnormalities. After a discussion in multidisciplinary consultation meeting and agreement of the patient and his parents, low dose localized radiotherapy was decided in view of the risk of mutilating surgery, the young age and the troublesome exophthalmos. CT was taken to plan radiation therapy, and had shown no infiltrative lesion or abnormalities of the orbital bone to delineate. On account of this CT-MRI discordance, we performed an Orbital MRI which revealed no abnormalities compared with the first one (Figure 3). So, we decided to follow up with the patient without any additional treatment. Nine months after biopsy, the patient showed no evidence of clinical or radiological recurrence. In fact, the lesion had completely disappeared in the later orbital MRI, the one at 9 months. And even after a follow-up of 4 years, there was no clinical or radiological evidence of disease.
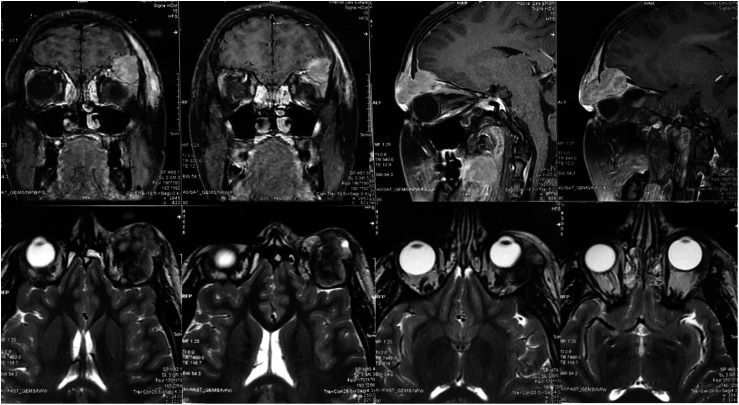
Figure 1.
Cerebral MRI in coronal, sagittal and axial section showing a superolateral extraconal tissular mass extending through the superior orbital fissure and along the dura mater measuring 36.6 mm x 32.7 mm.
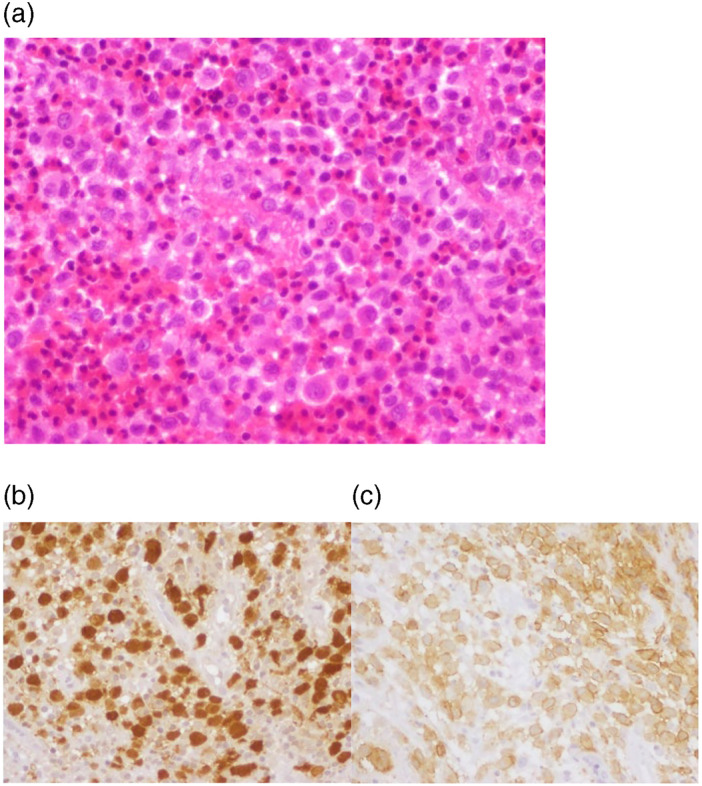
Figure 2.
(a) Langerhans cell histiocytosis showing intermediate-sized cells with grooved, indented and lobed nuclei and pale eosinophilic cytoplasm surrounded by large numbers of eosinophils (HEx400). Langerhans cell histiocytosis with S100 (b) and CD1a (c) immunoreactivity on the majority of cells (IHCx400).
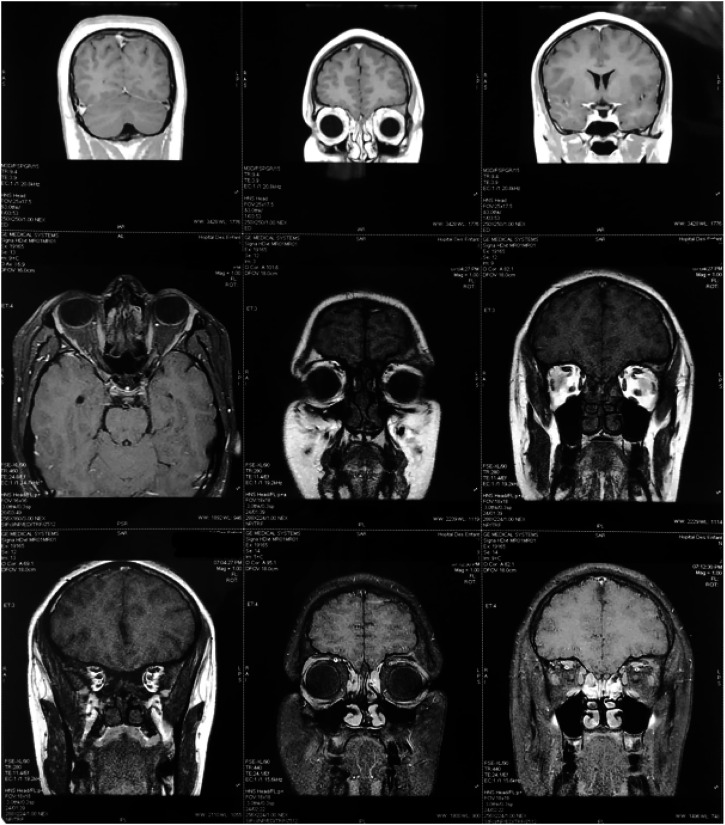
Figure 3.
Orbital MRI revealing no abnormalities 9 months after diagnosis.
Discussion
Langerhans cell histiocytosis is a rare disease affection mainly children and young adult with a frequency peak between 1 and 4 years with a male predominance.5 The etiology of LCH is unknown. The rarity of mitosis and the absence of cellular atypia are against the malignant etiology, however, cancer associated mutation (BRAFV600 E) was found in more than half of investigated specimens, indicating that LCH may be more a neoplastic disease than a reactive disorder.6
LCH is characterized by a wide spectrum of clinical presentation including solitary bone lesions with excellent prognosis, known as EG, and other systemic presentations with a multi-organic form known as Hand-Schüller-Christian syndrome and disseminated form, previously termed Letterer-Siwe’s disease with a very poor prognosis.7
In the orbit, GE sits preferentially in the superolateral quadrant and is often manifested by an exophthalmia, an infiltration of the eyelid, a tumor or fracture syndrome. In our case the diagnosis was revealed by appearance of exophthalmia. Standard radiographs of the skeleton, chest X-ray and skull CT should be practiced within the framework of the radiologic assessment. MRI can also be indicated in particular locations such as the orbit, the skull base and the spine. The diagnosis of LCH should be based on histologic and immunophenotypic examination of a lesional biopsy and it’s defined by the positivity for S100 protein and for CD1a antigens and the presence of Birbeck granules on electronic microscopy.8
Due to incomplete understanding of the pathogenesis and the rarity of this pathology treatment has been based on different empirical strategies. Treatment recommendations are based on the location, the extension of the disease and the age of the patient. The reference treatment according to the international histiocyte society is mainly based on curettage with or without intralesional steroid, PO prednisone, and/or PO vinblastine. Excision of bone lesions may be indicated for small lesions less than 2 cm in diameter and for lesions with a diameter of 2–5 cm, particularly in cases of orbital location. Local corticosteroid injection can provide immediate pain relief and first radiographic signs of healing within 2 months of injection. The international histiocyte society also recommends chemotherapy for “high-risk” lesions, in or near the central nervous system (e.g. orbit), although this is a subject of controversy, of many orbital surgeons advocating local treatment for solitary orbital lesions. Low-dose localized radiotherapy is an interesting therapeutic alternative in locally threatening forms close to the optic pathways which can lead to compression of the optic nerve or the spinal cord responsible for spinal cord compression. It is a treatment that has proven to provide sufficient local control. Given the benign nature of EG, the risk of acquired abnormalities of maxillofacial and dental development in growing children, some treatments may be unjustified. This risk is predominant especially with radiotherapy which can give facial dysmorphisms and secondary cancers.9,10
The clinical course of this affection is very variable and unpredictable and depends on the age of the patient, clinical form, location, tumor size and degree of infiltration of surrounding tissues. But, usually has a favorable prognosis and cases of spontaneous remission have been reported. This form can spontaneously regress or be followed by several outbreaks of the disease with the appearance of visceral localization.
Indeed, similar to this present case, in the literature, some authors have reported few cases of spontaneous resolution after biopsy without additional treatment.11–21 Through Table 1tbl1, among the cases found in the literature, we noticed a predominance of the orbital localization. In fact, five out of the 12 cases found were located in orbit. The age of the patients at the time of diagnosis varied between 2 and 45 years. The time to total spontaneous regression varied between 3 months and 4 years.
Table 1.
Summary of localized reported cases that have undergone spontaneous regression in the literature.
| Authors | Number of cases | Age | Gender | Localisation | Time to spontaneous regression |
|---|---|---|---|---|---|
| Lachkar R et al. (2008)8 | 4 patients including one with spontaneous regression | 3 years old | Female | Orbital localisation | 4 years |
| Smith JH et al. (1999)9 | 1 | 3 years old | Female | Orbital localisation | 1 6 months |
| Namai T et al. (2001)10 | 1 | 17 years old | Male | Mandible | 10 months |
| Silva de Paula J et al. (2003)11 | 1 | 17 years old | Male | Orbital localisation | 22 months |
| Muscolo D et al. (2003)12 | 2 | The 2 cases are 2 years old | 1 male and 1 female | The femur | Between 6 months and one year |
| Key SJ et al. (2004)13 | 3 | 30 months old, 12 and 45 years old | 2 females and 1 male | Maxillofacial skeleton | 3 months, 18 months and 3 years |
| Rajendram R et al. (2005)14 | 1 | 17 years old | Male | Orbital localisation | 5 months |
| Satoh K et al. (2011)15 | 1 | 22 years old | Male | Orbital localisation | 7 months |
| Vargas A et al. (2016)16 | 1 | 16 years old | Male | The maxilla | 3 months |
| Ono K et al. (2021)17 | 1 | 4 years old | Male | Mandible | 18 months |
| Broaddus WC el al. (2021)18 | 1 | 40 years old | Male | The greater wing of the sphenoid extending into the right orbit | 10 months |
| Our case report (2021) | 1 | 18 years old | Male | Orbital localisation | 9 months |
The mechanism of spontaneous remission after biopsy is still unknown. However, some authors have found that certain stimulation associated with the biopsy itself or decompression of the lesion by the biopsy can influence the inflammatory process of the lesion and induce healing.22
For all the cases described in Table 1, the follow-up was scheduled for a period that varies between 1 year and 5 years. No clinical or radiological recurrence was detected and we do not have a clear idea of the pace of surveillance.
Therefore, an expectant attitude after a diagnosis is defined histologically by biopsy can be offered in the case of EG without severe pain, without unacceptable deformity, or risk of pathological fracture. This attitude is suggested above all in cases of orbital localization, since the majority of cases of spontaneous regression described in the literature are located in the orbit. However, long-term follow-up is essential since the rate of recurrence for treated EG in the jaw bones can reach 7.3%, and younger patients are more likely to develop new lesions.23
Conclusion
LCH is a heterogeneous disease, with unknown etiopathogenesis. Its clinical expression is variable and its course is unpredictable, ranging from spontaneous regression to rapid progression or recurrence with the risk of long-term irreversible disabilities. The mechanism of spontaneous remission after biopsy is unknown. An expectant attitude toward the possibility of spontaneous regression after only performing biopsy, can be proposed, especially in small lesions. However, long-term follow-up is essential given the risk of recurrence.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Data availability statement: The data that support the findings of this study are available from the corresponding author (ghorbelasma.med@gmail.com), upon reasonable request.
ORCID iD
Asma Gorbel https://orcid.org/0000-0002-2712-7250
References
- 1.Desbarats C, Adnot J, Bastien AV, et al. Histiocytose langerhansienne révélée par un désordre de l’appareil manducateur : rapport d’un cas et revue de la littérature des atteintes crâniofaciales. Rev Médecine Interne Janv 2020; 41(1): 50–53. [DOI] [PubMed] [Google Scholar]
- 2.Iurescia AC, Rendo J, Gimeno FL, et al. Manifestaciones oculares de la histiocitosis de células de Langerhans: Revisión de 40 casos. Oftalmol Clin Exp 2007; 1(12–5). [Google Scholar]
- 3.Durham BH. Molecular characterization of the histiocytoses: Neoplasia of dendritic cells and macrophages. Semin Cel Dev Biol. Févr 2019; 86: 62–76. [DOI] [PubMed] [Google Scholar]
- 4.Giovannetti F, Giona F, Ungari C, et al. Langerhans cell histiocytosis with orbital involvement: our experience. J Oral Maxillofac Surg 2009; 67(1): 212–216. [DOI] [PubMed] [Google Scholar]
- 5.Herwig MC, Wojno T, Zhang Q, et al. Langerhans Cell Histiocytosis of the Orbit: Five Clinicopathologic Cases and Review of the Literature. Surv Ophthalmol Juill 2013; 58(4): 330–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gulati N, Allen CE. Langerhans cell histiocytosis: Version 2021. Hematol Oncol Juin 2021; 39(Suppl 1): 15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiCaprio MR, Roberts TT. Diagnosis and management of langerhans cell histiocytosis. J Am Acad Orthop Surg 2014; 22(10): 643–652. [DOI] [PubMed] [Google Scholar]
- 8.El-Gayyar M, Sallam M, Khaled M, et al. Langerhans Cell Histiocytosis: Clinical, Histopathological and Radiological Case Series Study: An Institutional Experience, 2020. [Google Scholar]
- 9.Minkov M. Histiocytose à cellules de Langerhans : directives d’évaluation et de traitement de la société des histiocytes. Société des histiocytes, 2009. [Google Scholar]
- 10.Esmaili N, Harris GJ. Histiocytose à cellules de Langerhans de l’orbite: spectre de la maladie et risque de séquelles du système nerveux central dans les cas unifocaux. Ophthal Plast Reconstr Surg 2016; 32: 28–34. [DOI] [PubMed] [Google Scholar]
- 11.Lachkar R, Ibrahimy W, Benharbit M, et al. L’histiocytose Langerhansienne a localisation orbitaire. Bull Soc Ophtalmol Fr 2008; 309: 31. [PubMed] [Google Scholar]
- 12.Hasenyager Smith J, Fulton L, O’Brien JM. Spontaneous regression of orbital Langerhans cell granulomatosis in a three-year-old girl. Am J Ophthalmol Juill 1999; 128(1): 119–121. [DOI] [PubMed] [Google Scholar]
- 13.Namai T, Yusa H, Yoshida H. Spontaneous remission of a solitary eosinophilic granuloma of the mandible after biopsy: a case report. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg Déc 2001; 59(12): 1485–1487. [DOI] [PubMed] [Google Scholar]
- 14.Paula JS de, Chahud F, Cruz AAV e. Remissão espontânea de um granuloma eosinofílico orbitário após biópsia: relato de caso e revisão da literatura. Arq Bras Oftalmol Août 2003; 66(4): 523–526. [Google Scholar]
- 15.Muscolo DL, Slullitel G, Ranalletta M, et al. Spontaneous remission of massive solitary eosinophilic granuloma of the femur. J Pediatr Orthop Nov 2003; ■■■: 763–765. [DOI] [PubMed] [Google Scholar]
- 16.Key SJ, O’Brien CJ, Silvester KC, et al. Eosinophilic granuloma: resolution of maxillofacial bony lesions following minimal intervention Report of three cases and a review of the literature. J Cranio-maxillofac Surg Juin 2004; 32(3): 170–175. [DOI] [PubMed] [Google Scholar]
- 17.Rajendram R, Rose GE, Luthert PJ, et al. Biopsy-confirmed spontaneous resolution of orbital langerhans cell histiocytosis. Orbit Janv 2005; 24(1): 39–41. [DOI] [PubMed] [Google Scholar]
- 18.Satoh K, Tada M, Shimizu H, et al. Early adult-onset orbital apex Langerhans cell histiocytosis histologically confirmed during “truly spontaneous” regression. Acta Neurochir (Wien) Févr 2012; 154(2): 301–302. [DOI] [PubMed] [Google Scholar]
- 19.Vargas A, Ramírez H, Ramírez P, et al. Spontaneous remission of eosinophilic granuloma of the maxilla after incisional biopsy: a case report. Head Face Med Déc 2016; 12(1): 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ono K, Okui T, Kunisada Y, et al. A case of langerhans cell histiocytosis of the mandible that spontaneously regressed after biopsy in a child. https://onlinelibrary.wiley.com/doi/10.1002/ccr3.4321.6. [DOI] [PMC free article] [PubMed]
- 21.Broaddus WC, Somasundaram A, Carr MT, et al. Resolution and Re-ossification of Orbital Wall Langerhans Cell Histiocytosis Following Stereotactic Needle Biopsy. J Neurol Surg Rep 10 Mai 2022; ■■■. a-1847-8245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roychoudhury A, Shah N, Parkash H, et al. Eosinophilic granuloma of the jaws. Br J Oral Maxillofacial Surg 1998; 36(5): 380–383. [DOI] [PubMed] [Google Scholar]
- 23.Gnanasekhar JD, Ahmad MS, Reddy RR. Multifocal Langerhans cell histiocytosis of the jaws: a case report. Quintessence Int Berl Gerjuill 1985; 22(7): 559–564. [PubMed] [Google Scholar]