Abstract
Aim and Objectives:
The aim of our study was to evaluate salivary estradiol and salivary calcium in postmenopausal women with varying degrees of oral dryness. The primary objective was to establish the interrelationship between salivary parameters and oral health status among menopausal women and compare the same with premenopausal women and normal controls.
Materials and Methods:
The study included 60 women Group I consisted of healthy menstruating women between 25 and 34 years of age. In Group II premenopausal women between 35 and 45 years of age were present and Group III consisted of menopausal women between 45 and 60 years of age. Unstimulated saliva was collected from the participants and estradiol analysis was done using ELISA method and calcium analysis was done using Arsenazo III reaction using colorimetric method. The oral health status in these patients was determined by using xerostomia score, Russell's periodontal score, and oral hygiene index. The values obtained were subjected to statistical analysis and the results were derived.
Results:
On oral examination, most of them had poor oral hygiene, periodontal disease, and moderate to severe levels of xerostomia. Salivary estradiol levels were low and salivary calcium levels were high among postmenopausal women and as salivary estradiol levels decreased there was an increase in xerostomia scores and salivary calcium. And also as salivary calcium levels increased the periodontal disease scores increased. All parameters were within normal limits among healthy menstruating women.
Conclusion:
Saliva can be a preferred medium and an emerging alternative for serum to estimate estradiol and calcium levels. As a dentist, we have to educate them about the oral changes they will experience during menopause and emphasize its strong association between low estradiol levels. Oral hygiene instructions should be given for the maintenance of healthy periodontium. Menopausal women who experience severe postmenopausal symptoms can be identified and the dentist and gynecologist can work hand in hand to treat the symptoms of these women.
KEYWORDS: Menopause, oral hygiene, periodontitis, salivary calcium, salivary estradiol, xerostomia
INTRODUCTION
The World Health Organisation (WHO) defined menopause as “The permanent cessation of menstruation due to loss of ovarian follicular activity.” A female is considered to have attained menopause when there is amenorrhea with no pathology for 12 months.[1] The average age for menopause in Indian women is 46.2 ± 4.9 years.[2] Estrogen (ER) exists in 3 physiological forms as ER (E1), Estradiol (E2 or 17 β-Estradiol), and Estriol (E3).[3] Estradiol (E2) is considered the most potent form of ER. It is secreted by theca cells of ovaries and also by fat cells, particularly visceral fat.[4] In postmenopausal period, there will be a decline in endogenous estradiol levels making it less available to bind with the ER receptors distributed all over the body. This scenario leads to diverse systemic and oral manifestations. The systemic manifestations exhibited by women are urogenital atrophy, osteoporosis, and vasomotor symptoms. Oral manifestations experienced by postmenopausal women are burning mouth syndrome, xerostomia, osteoporosis of jawbones, periodontitis, and less commonly mucosal disorders such as lichen planus, pemphigus vulgaris, benign mucosal pemphigoid, and Sjogren's syndrome.[1] Saliva is an ultrafiltrate of plasma, many studies have put forward that unstimulated saliva provides an undiluted form of biomarkers for appropriate analysis. The measurement of salivary estradiol may reflect the ovarian functionality level in women.[5] The measurement of the whole calcium (Ca2+) concentration in saliva may also serve as a prescreening tool and adjuvant for the prediction of osteoporosis.[6] The oral hygiene index, periodontal index, and xerostomia score of menopausal women were recorded to assess their oral health status. Thus, this study is aimed towards estimation of salivary estradiol and salivary calcium levels and correlating it with oral hygiene index, periodontal index, and xerostomia score among postmenopausal women, perimenopausal women, and healthy menstruating women.
MATERIALS AND METHODS
A proper clinical history was obtained from all subjects. The ethical committee of Ragas Dental College and Hospital approved the study protocol. All the patients were explained about the study and written consent was obtained.
The study consisted of three groups. In Group I, 20 female subjects between the age group of 25 and 34 years of age were selected based on the following criteria like, they should have good oral hygiene and should have a regular menstrual cycle. They should not have any systemic illness or any deleterious habits or take any xerogenic medication and should not be under contraceptive pills. In Group II, 20 female subjects between the age group of 35 and 45 years of age were selected based on the following criteria like, they should have good or fair oral hygiene and should have a regular menstrual cycle. They should not take any xerogenic medication and should not have any systemic illness or any deleterious habits and should not be under contraceptive pills. Group III is formed by 20 female subjects between 46 and 60 years of age who have not had a menstrual cycle for more than a year (<12 months). These subjects should not be under any xerogenic medical agents. They should be devoid of any systemic illness and deleterious habits.
The oral hygiene statuses of the subjects were analyzed using oral hygiene index proposed by John. C. Greene and Jack R. Vermillion (1964). The periodontal status was assessed by using Russell's periodontal index proposed by Russell A. L.(1956). They were evaluated for the presence of xerostomia using xerostomia XI inventory questionnaire (Thomas et al.). The unstimulated whole saliva (mixed saliva) which is a mixture of oral fluids and includes secretion from major and minor salivary glands is collected from the selected participants by draining method. In this method, the patient is asked to sit quietly with the head bent down. They should be trained to pool the saliva on the floor of the mouth without applying any stimulus. They were asked to open the mouth and allow the saliva to slowly drip from the lower lip into the sterile container. The ideal time for collection is between 9 am and 12 pm., and at least 2 h after the last intake of food or drink. The values obtained were recorded and subjected to statistical analysis.
RESULTS
The results of the study were as follows, the mean salivary estradiol level in healthy menstruating women (Group I) is 5.61. In premenopausal women (Group II) it is 7. 86 and in postmenopausal women (Group III) the mean salivary estradiol levels are 3.22 (P = 0.01) [Table 1]. The mean calcium level in healthy menstruating women (Group I) is 4.39. In premenopausal women (Group II) is 3.55 and in postmenopausal women (Group III) the mean salivary calcium levels are 5.9 (P- = 0.03) [Table 2].
Table 1.
Mean salivary estradiol levels among the groups
| n | Mean±SD | P | |
|---|---|---|---|
| Group I | 20 | 5.61±5.02 | 0.01 |
| Group II | 20 | 7.86±5.60 | |
| Group III | 20 | 3.22±2.87 |
SD: Standard deviation
Table 2.
Mean salivary calcium levels among the groups
| n | Mean±SD | P | |
|---|---|---|---|
| Group I | 20 | 4.39±2.75 | 0.03 |
| Group II | 20 | 3.55±2.29 | |
| Group III | 20 | 5.91±3.47 |
SD: Standard deviation
The mean xerostomia score in normal controls (Group I) is 11.0. In premenopausal women (Group II) is 13.80 and in postmenopausal women (Group III) the mean xerostomia score was 35.80 (P = 0.00). The mean Russell's periodontal score in normal controls (Group I) is 0.21. In premenopausal women (Group II) is 0.68 and in postmenopausal women (Group III) the mean Russell's periodontal score is 3.60 (P = 0.00). The mean OHI-S score in normal controls (Group I) is 1.08. In premenopausal women (Group II) is 1.35 and in postmenopausal women (Group III) the mean OHI-S score is 4.11 (P = 0.00).
Pearson's correlation between salivary estradiol levels and xerostomia score reveals a strong negative correlation [Figure 1]. Pearson's correlation between salivary calcium levels and periodontal score reveals a strong positive correlation [Figure 2]. Pearson's correlation between salivary calcium levels and salivary estradiol reveals a weak negative correlation [Figure 3].
Figure 1.
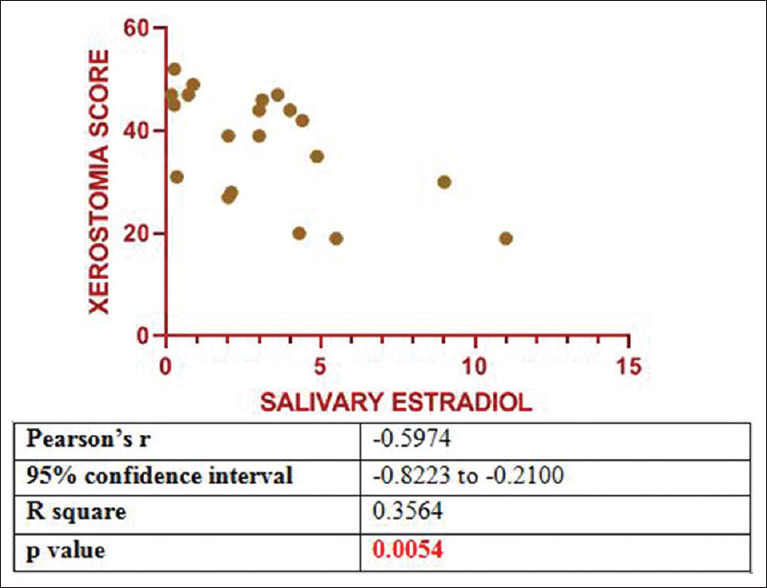
Correlation between salivary estradiol and xerostomia scores
Figure 2.
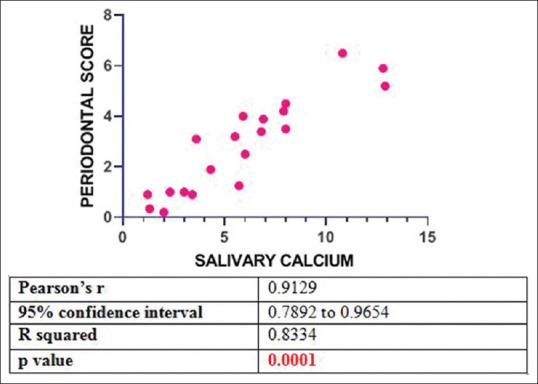
Correlation between salivary calcium and periodontal scores
Figure 3.
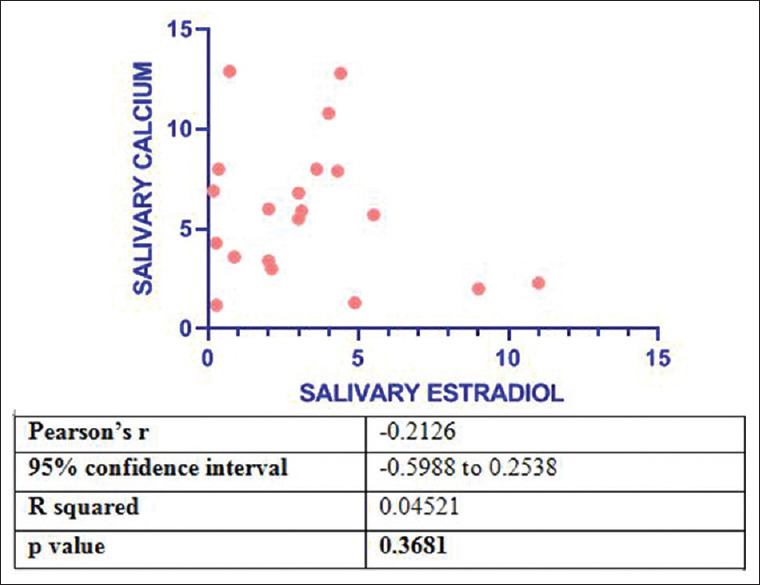
Correlation between salivary estradiol and salivary calcium
DISCUSSION
Menopause is a permanent cessation of menstruation due to loss of ovarian follicular activity. It occurs between the fourth and fifth decade of life.[1] The WHO has classified midlife of women into three categories, Menopause as the year of the final physiological menstrual period retrospectively designated as 1 year without flow (unrelated to pregnancy or therapy) in women aged ≥40 years. In premenopausal (35–39 years), there is decreased fertility and fecundity which appear as the foremost manifestations of ovarian follicle depletion and dysfunction, despite the absence of menstrual changes. Perimenopause stage is years immediately before menopause and the 1st year after menopause.[7]
According to staging of reproductive aging in women (staging of reproductive aging in women (STRAW) + 10) criteria, the midlife of women is classified into three phases as reproductive, menopausal transition, and menopausal phase. During menopause there is a decline in estradiol levels, progesterone is not produced after menopause and the follicular stimulating hormone (FSH) levels stabilize. Anti-mullerian hormone, Inhibin-B are other hormones which are low in this phase. The antral follicular count is also low in menopausal phase.[8] Saliva is considered an ultrafiltrate of plasma and is used as a medium to measure endocrine hormones. Estradiol is strongly bound to steroid hormone-binding globulin and weakly to albumin in blood. Only 1% estradiol exists as free form or biologically active form in blood. This hormone is transferred from bloodstream into the salivary gland by the process of passive diffusion through lipophilic layer of cells and glandular epithelial cells. This mechanism allows only biologically active forms of estradiol to be secreted in saliva. Hence, it can be used as an indicator to measure biologically active estradiol levels.[5]
In our study, we had three groups, Group I was formed by normal menstruating women, Group II was formed by premenopausal women, and Group III was formed by postmenopausal women. This grouping was done based on criteria for the classification of midlife of women by the World Health Organization and stages of reproductive aging in women criteria.
In our study, the age of the subjects in Group I was between 25 and 35 years, in Group II it is 36–45 years, and in Group III it is 46–60 years. However, subjects who fall under perimenopausal category were excluded since there will be fluctuating hormone levels during this phase. The WHO suggested >40 years as menopausal age but in our study menopausal women (Group III) between 45 and 60 years were included because the average age of menopausae in Indian women is 46.2 ± 4.9 years.[8]
Välimaa et al., put forth that ER β receptors are present in the acinar and ductal cells of the salivary glands. During menopause, low circulating estradiol levels are present so a sufficient level of hormones was not available to bind with the receptors. This leads to alteration in quantity as well as quality of salivary secretion. This is suggested as a probable cause for xerostomia which is a common oral symptom in postmenopausal women.[9] Agha-Hosseini et al. conducted a study to evaluate the relationship between unstimulated and stimulated salivary estradiol level and xerostomia among postmenopausal women he used xerostomia XI inventory questionnaire to evaluate the oral dryness in postmenopausal women.[10] Singh et al. also assessed oral dryness in postmenopausal women using xerostomia XI inventory questionnaire.[11] Hence, in our study also, we have used xerostomia XI inventory questionnaire by Thomson et al., to evaluate xerostomia among the groups since it helps in the quantification of symptoms of xerostomia.[12] We also assessed the relation between xerostomia and salivary estradiol among postmenopausal women.
The xerostomia score was measured among the subjects of 3 Groups using xerostomia XI inventory questionnaire. Xerostomia was absent in the control group, premenopausal women exhibited mild levels of xerostomia and postmenopausal women presented with higher xerostomia scores indicating severe levels of oral dryness. One-way ANOVA test and post hoc turkey test for multiple comparison was performed. The results were significant with a P = 0.001. Pearson's correlation test between salivary estradiol levels and xerostomia score among postmenopausal women revealed that as the salivary estradiol levels decrease the xerostomia scores increased among the postmenopausal women.
Gill et al., in their study, evaluated unstimulated salivary flow rate with oral symptoms in premenopausal women and postmenopausal women and appreciated that xerostomia was significantly higher in postmenopausal women.[13] Parakh et al., in their study evaluated the effect of menopause on saliva and dental health and found that xerostomia levels were higher in postmenopausal women.[14] The results of this study were in accordance with the results of our study.
Minicucci et al., in their study assessed salivary flow rate and xerostomia using xerostomia XI inventory questionnaire in postmenopausal women. It was found that the salivary flow rate was less in postmenopausal women and they did not show any clinical symptoms of xerostomia. The results of the above study were contradictory to our study because in their study group out of 30 postmenopausal women 16 postmenopausal women were under hormone replacement therapy but in our study, we have excluded postmenopausal women under hormone replacement therapy and 85% of postmenopausal women had severe levels of xerostomia.[15]
In our study, salivary estradiol levels were within normal limits in healthy menstruating women. In case of premenopausal women, it was normal in 90% of the patients while there was a decline in 10% of the cases. The estradiol levels were low in 95% of the postmenopausal women. One-way ANOVA test and post hoc turkey test for multiple comparisons were performed. The results were significant with a P = 0.01. Pearson's correlation also revealed that as the salivary estradiol level decreased the xerostomia levels increased.
Tivis et al., in their study, measured salivary estradiol levels and serum estradiol levels among postmenopausal women who are not under any ER substitutes. He put forth that there were low circulating levels of estradiol in both serum and saliva. The results of his study were in accordance with our study in which low salivary estradiol was appreciated in 95% of the postmenopausal women.[16]
Agha-Hosseini et al. in their study, obtained stimulated salivary estradiol from postmenopausal women. He proposed that stimulated salivary estradiol levels were low in postmenopausal women and also as stimulated salivary estradiol levels decreased there was an increase in xerostomia levels.[10] He also conducted another study by measuring unstimulated salivary estradiol levels and compared it with xerostomia status using xerostomia XI inventory questionnaire in postmenopausal women. It was found that as unstimulated salivary estradiol levels decreased there was an increase in xerostomia scores.[17] The results of both these studies were in line with our results.
Saliva in addition to ER and progesterone also contains calcium, phosphate, IgA, and mucin. In postmenopausal women, salivary estradiol levels decline and osteoclasts trigger the mobilization of calcium from bones to the serum resulting in rise of serum calcium levels.[18] This calcium diffuses into the salivary gland through its vasculature and is secreted in saliva.[19] In premenopausal women, there is either increase or decrease in estradiol levels depending on the infradian rhythm of the individual as they approach menopause.[20] When the estradiol level rises the osteblastic action is triggered and mobilization of calcium from serum to bone which causes the serum calcium level to fall. In healthy controls, both the estradiol and calcium levels are in normal range. The variation in serum level is depicted in saliva. In serum, parathyroid hormone and calcitonin maintain the calcium levels so a major discrepancy is not appreciated in serum levels of calcium.[18] In saliva, there are no such factors so salivary calcium serves as a prescreening tool and adjuvant for the determination of osteoporosis and evaluate the risk of periodontitis.
Singh et al., in their study, had proposed, there exists a significant correlation between serum estrogen levels and salivary calcium concentration.[11] Rane et al., in their study, stated that increased salivary calcium levels are associated with the risk of the development of periodontal disease. This is because salivary calcium is essential for the calcification of dental plaque to form supragingival and subgingival calculus. Since periodontitis and osteoporosis are important presentation of menopause we consider using salivary calcium as an indicator which would serve as an alternative to evaluate these conditions.[20]
In our study, salivary calcium levels were normal in all healthy menstruating women. In premenopausal women, 10% of them had normal levels while 90% had low circulating calcium levels. In postmenopausal women, 45% had higher calcium levels 25% had normal calcium levels and 35% had low levels of salivary calcium. One-way ANOVA test and post hoc turkey test for multiple comparisons were performed. The results were significant with a P = 0.01. Pearson's correlation test was done and it was found that as the salivary estradiol level decreased there was an increase in salivary calcium levels in postmenopausal women. It was observed that an increase in salivary calcium level was related to the increased occurrence of periodontal disease among postmenopausal women.
Singh et al. estimated salivary calcium in postmenopausal women. There was a significant difference among salivary calcium in postmenopausal women who had xerostomia and who did not have xerostomia. It was found salivary calcium levels were high in postmenopausal women with oral dryness.[21] The results were similar to our study in which 40% of the postmenopausal women showed high calcium levels while 90% premenopausal women and all the healthy menstruating women had normal salivary calcium levels.
Agha-Hosseini et al.in their study estimated salivary calcium in postmenopausal women with or without xerostomia. The results showed that salivary calcium was high in postmenopausal women with xerostomia when compare to postmenopausal women without oral dryness. The result of their study was similar to the results of our study in which 40% of the postmenopausal women had higher salivary calcium levels.[18]
Minicucci et al., in their study, had stated that during menopause, there is a significant decrease in salivary flow rate. This reduction in salivary volume is responsible for the development of xerostomia symptoms among postmenopausal women. It caused poor flushing of debris by saliva thereby gave rise to poor oral hygiene status and it also lead to loss of antibacterial properties of saliva which increased the risk of development of dental caries, periodontal disease in postmenopausal women. Hence, in our study, we have evaluated oral hygiene status using OHI-S scores and periodontal status using Russell's periodontal index scores among the groups.[15]
Deepa and Jain assessed periodontal health status among postmenopausal women and reported destructive periodontitis was common in postmenopausal women. Poor oral hygiene increased the risk of the development of periodontitis. The results matched with our study in which 85% of the postmenopausal women had established destructive periodontitis and 15% had terminal periodontal disease. Ninety-five percent of the patients had poor oral hygiene.[22]
Rukmini et al., in their study, evaluated the effect of menopause on saliva and dental health. The periodontal index scores as well as oral hygiene scores were higher in postmenopausal women. The results were similar to our study in which normal periodontium was observed in healthy menstruating women. In Group II, 35% had gingivitis, 10% had beginning destructive periodontal disease, and 5% had established periodontal disease. In postmenopausal group, 10% had beginning periodontal disease, 70% had established periodontal disease and 15% had terminal disease. One-way ANOVA test and post hoc turkey test for multiple comparisons were performed. The results were significant with a P = 0.01. With regard to the oral hygiene status, in our study, 95% of postmenopausal women had poor oral hygiene status.[23]
Obaidi and Qasim, in their study, estimated salivary estradiol levels and oral hygiene status among postmenopausal women and found that the salivary estradiol levels were low and oral hygiene index scores were high indicating poor oral hygiene.[24] The results of this study were in accordance with the results of our study where the oral hygiene status was appreciated among normal controls. It was good in 70%, fair in 25%, and poor in 5% of the subjects. In premenopausal women, the oral hygiene status was good in 60%, fair in 30%, and poor in 10% of the subjects. In postmenopausal women, oral hygiene was good in 5% and poor in 95% of the subjects. One-way ANOVA test and post hoc turkey test for multiple comparisons were performed. The results were significant with a P = 0.01.
CONCLUSION
This study put forth that saliva can be used as an emerging alternative to serum for estimation of estradiol and calcium levels. It threw light on the fact that decline in estradiol level is responsible for various systemic and oral manifestations during menopause. During the study, it was observed that most of the menopausal women were unaware that the oral changes occurring in them were due to the withdrawal of estradiol. It was necessary to create awareness among women across ages about the hormonal changes and their oral manifestations during various stages of their life. As a dentist, we should educate them about the oral manifestations of menopause and emphasize its strong association with low estradiol levels. Oral hygiene instructions should be given for the maintenance of healthy periodontium. Menopausal women experiencing severe postmenopausal symptoms can be identified. The dentist and gynecologist can work hand in hand to improve the overall health.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shigli KA, Giri PA. Oral manifestations of menopause. J Basic Clin Reprod Sci. 2015;4:4–8. [Google Scholar]
- 2.Ahuja M. Age of menopause and determinants of menopause age: A PAN India survey by IMS. J Midlife Health. 2016;7:126–31. doi: 10.4103/0976-7800.191012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guyton and Hall, Textbook of Medical Physiology. 13th. Philedelphia: Copyright © 2011, 2006, 2000, 1996, 1991, 1986, 1981, 1976, 1966, 1961, 1956 by Saunders, an imprint of Elsevier Inc. [Google Scholar]
- 4.Kozloski MJ, Schumm LP, McClintock MK. The utility and dynamics of salivary sex hormone measurements in the National Social Life, Health, and Aging Project, Wave 2. J Gerontol B Psychol Sci Soc Sci. 2014;69(Suppl 2):S215–28. doi: 10.1093/geronb/gbu123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leimola-Virtanen R, Salo T, Toikkanen S, Pulkkinen J, Syrjänen S. Expression of estrogen receptor (ER) in oral mucosa and salivary glands. Maturitas. 2000;36:131–7. doi: 10.1016/s0378-5122(00)00138-9. [DOI] [PubMed] [Google Scholar]
- 6.Saha MK, Agrawal P, Saha SG, Vishwanathan V, Pathak V, Saiprasad SV, et al. Evaluation of correlation between salivary calcium, alkaline phosphatase and osteoporosis - A prospective, comparative and observational study. J Clin Diagn Res. 2017;11:C63–6. doi: 10.7860/JCDR/2017/24960.9583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grover CM, More VP, Singh N, Grover S. Crosstalk between hormones and oral health in the mid-life of women: A comprehensive review. J Int Soc Prev Community Dent. 2014;4:S5–10. doi: 10.4103/2231-0762.144559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop+10: Addressing the unfinished agenda of staging reproductive aging. Menopause. 2012;19:387–95. doi: 10.1097/gme.0b013e31824d8f40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Välimaa H, Savolainen S, Soukka T, Silvoniemi P, Mäkelä S, Kujari H, et al. Estrogen receptor-beta is the predominant estrogen receptor subtype in human oral epithelium and salivary glands. J Endocrinol. 2004;180:55–62. doi: 10.1677/joe.0.1800055. [DOI] [PubMed] [Google Scholar]
- 10.Agha-Hosseini F, Mirzaii-Dizgah I, Mansourian A, Khayamzadeh M. Relationship of stimulated saliva 17beta-estradiol and oral dryness feeling in menopause. Maturitas. 2009;62:197–9. doi: 10.1016/j.maturitas.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Singh R, Pallagatti S, Sheikh S, Singh B, Arora G, Aggarwal A. Correlation of serum oestrogen with salivary calcium in post-menopausal women with and without oral dryness feeling. Gerodontology. 2012;29:125–9. doi: 10.1111/j.1741-2358.2011.00580.x. [DOI] [PubMed] [Google Scholar]
- 12.Thomson WM, Chalmers JM, Spencer AJ, Williams SM. The xerostomia inventory: A multi-item approach to measuring dry mouth. Community Dent Health. 1999;16:12–7. [PubMed] [Google Scholar]
- 13.Gill N, Ruparelia P, Verma O, Ruparelia K. Comparative evaluation of unstimulated whole salivary flow rate and oral symptoms in healthy premenopausal and postmenopausal women - An observational study. J Indian Acad Oral Med Radiol. 2019;31:234–8. [Google Scholar]
- 14.Parakh D, Garla BK, Dagli R, Solanki J, Thareja P, Vyas D. Evaluation of the effect of menopause on saliva and dental health. Int J Oral Health Dent. 2016;2:71–6. [Google Scholar]
- 15.Minicucci EM, Pires RB, Vieira RA, Miot HA, Sposto MR. Assessing the impact of menopause on salivary flow and xerostomia. Aust Dent J. 2013;58:230–4. doi: 10.1111/adj.12057. [DOI] [PubMed] [Google Scholar]
- 16.Tivis LJ, Richardson MD, Peddi E, Arjmandi B. Saliva versus serum estradiol: Implications for research studies using postmenopausal women. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:727–32. doi: 10.1016/j.pnpbp.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 17.Agha-Hosseini F, Mirzaii-Dizgah I. Unstimulated saliva 17β-estradiol and xerostomia in menopause. Gynecol Endocrinol. 2012;28:199–202. doi: 10.3109/09513590.2011.593668. [DOI] [PubMed] [Google Scholar]
- 18.Agha-Hosseini F, Mirzaii-Dizgah I, Moosavi MS. Relationship of serum and saliva calcium, phosphorus and alkaline phosphatase with dry mouth feeling in menopause. Gerodontology. 2012;29:e1092–7. doi: 10.1111/j.1741-2358.2012.00619.x. [DOI] [PubMed] [Google Scholar]
- 19.Mittal S, Bansal V, Garg S, Atreja G, Bansal S. The diagnostic role of Saliva - A review. J Clin Exp Dent. 2011;3:e314–20. [Google Scholar]
- 20.Rane MV, Suragimath G, Varma S, Zope SA, Ashwinirani S R. Estimation and comparison of salivary calcium levels in healthy controls and patients with generalized gingivitis and chronic periodontitis. J Oral Res Rev. 2017;9:12–5. [Google Scholar]
- 21.Singh B, Sheikh S, Pallagatti S, Kaur K, Sohi R. Evaluation of salivary calcium and salivary parathyroid levels in postmenopausal women with and without oral dryness. Contemp Clin Dent. 2013;4:488–92. doi: 10.4103/0976-237X.123051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deepa D, Jain G. Assessment of periodontal health status in postmenopausal women visiting dental hospital from in and around Meerut city: Cross-sectional observational study. J Midlife Health. 2016;7:175–9. doi: 10.4103/0976-7800.195696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rukmini JN, Sachan R, Sibi N, Meghana A, Malar CI. Effect of Menopause on Saliva and Dental Health. J Int Soc Prev Community Dent. 2018;8:529–33. doi: 10.4103/jispcd.JISPCD_68_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Obaidi N, Qasim A. Oral hygiene status in relation to salivary estradiol hormone level among pre-menopausal and post-menopausal Iraqi women. J Baghdad Coll Dent. 2019;31:70–4. [Google Scholar]


