Abstract
Objective
Additive manufacturing has played an increasingly important role in the field of health care. One of the most recent applications has been the development of 3D printed anatomical models specifically to improve student education. The purpose of this review was to assess the potential for 3D printed models to improve understanding of complex anatomy in undergraduate and medical/professional students.
Methods
A systematic review was performed to investigate the different implementations of 3D printed anatomical models in educational curricula. In addition, a meta-analysis was conducted to assess the differences in comprehension between students who received 3D printed models as part of their instruction and those taught with traditional methods.
Results
Of the 10 groups included in the meta-analysis, students whose educational experience included a 3D printed model scored roughly 11% better on objective assessments compared to students who did not use such models (Hedge’s g = 0.742, p < 0.001).
Conclusion
Based on these findings, the use of 3D printed anatomical models as a method of education is likely to improve students’ understanding of complex anatomical structures.
Keywords: 3D printing, Anatomic model, Student, Education
Introduction
Within health care, 3D printers have been used to develop advanced prosthetic devices [1], implants for surgical intervention [2], guides for surgical planning [3, 4], and models for educational purposes [5]. The development of patient-specific 3D printed models has been used to plan complex surgeries and, in some cases, change the outcome of the entire operations [3]. Currently, 3D representations of unique surgical cases can be constructed using certain software but must be projected on a 2D screen, thus removing any perception of depth. Using 3D printing, it is possible to achieve a better understanding of the anatomical region of interest that includes both depth perception and tactile feedback that are currently lacking in virtual projections [6].
When describing the potential benefits that 3D printed anatomical models can have within the medical field, many authors have previously outlined the potential for student education [7, 8]. For example, experienced surgeons will likely not find as much value in using a 3D printed model for a simple operation but may find the model useful in complex surgeries that have other complications [9]. Novice surgeons, however, are more likely to find the models useful for any operation, based on their overall lack of experience [10]. The value of educational models ranges from teaching novice surgeons how to handle complex surgeries to teaching undergraduate students pursuing health care professions about simple anatomy. Utilization of 3D printing services in anatomical education could potentially be used to bridge the large gap in experience by improving spatial comprehension of unique pathologies and other complex anatomy topics in a format that is widely accessible to most audiences. While cadaver models and virtual reality environments have also previously been used for these purposes, the cost of maintaining a cadaver lab is not realistic for all institutions and virtual reality environments lack important tactile information [11]. In recent years, the average cost of 3D printing services has substantially decreased and become much more available, thus making their application to most classrooms much more realistic.
While there are numerous articles that look at the educational value of 3D printed anatomical models, the methods used to examine these effects are scattered through different types of quizzes, surveys, and examinations. There are a number of questions about the use of 3D printed models for educational purposes that remain to be answered before they become a regular implementation within a classroom setting.
The purpose of this systematic review with meta-analysis was to investigate if 3D printed anatomical models have had a significant impact on improving comprehension of various anatomy topics through objective measurements such as quizzes or in class assignments. We hypothesized that students who used a 3D printed model as a part of their education would perform better than those who did not on short-term assessments.
Methods
A comprehensive literature search was performed of published articles. The search terms study inclusion, and database search were performed by D.S. and M.T. according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Search Details
A literature search was performed through three electronic databases: Cochrane, Web of Science, and PubMed (Medline). The search was designed to target studies that used 3D printed models as a part of students’ education. The included search terms were as follows: (1) 3D OR 3-dimensional OR three-dimensional print, (2) anatomic model, (3) student, and (4) learn OR education. Only full-text articles that were accessible in English were included as a part of the systematic review and meta-analysis. The search included articles from inception to May 4th, 2021, and papers published after this date were not included.
Inclusion Criteria
For the purpose of this systematic review with meta-analysis, only full-text articles that were published in a peer-reviewed journal were included. Study designs included cohort studies and randomized control trials. In addition, the method of model development had to utilize 3D printing specifically.
Exclusion Criteria
Articles that stated the model being developed was for a specific surgical intervention were excluded from this review. Articles that lacked a method of assessment (i.e., quiz or lab practical) were excluded entirely, and articles that did not include a control group (a group that did not receive a model) were excluded from the quantitative analysis. Lastly, articles that solely described the method of making anatomical models were also excluded.
Data Extraction
For the qualitative analysis, extracted information included the study design, student education level, region of interest for model development, and major findings from the study. For articles included in the quantitative analysis, reported mean and standard deviation values on student performance were extracted and converted to a percent value based on the total potential score.
Bias Assessment
Articles were assessed for the impact on improving education on the target student population. The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) risk of bias assessment was used to evaluate the included full texts by two of the coauthors separately (D.S. and M.T.).
Statistical Analysis
A Hedge’s g random effect model was used to calculate the pooled effect size of the studies included in the quantitative analysis. Analysis was performed on the differences in performance scores between experimental group and the control group (those who used a 3D printed model versus those who did not). Percentage of answers correct in the assessment was compared across studies. Scores that were not presented as percentages were converted based on total potential score. When possible (n ≥ 3), sub-group analyses were conducted among the types of students assessed (e.g., medical students and residents). In addition, heterogeneity of the data was also calculated using I2 and Q-statistics. A fail-safe N was also calculated to check for the potential bias of unreported studies. A p-value of 0.05 was considered statistically significant.
Results
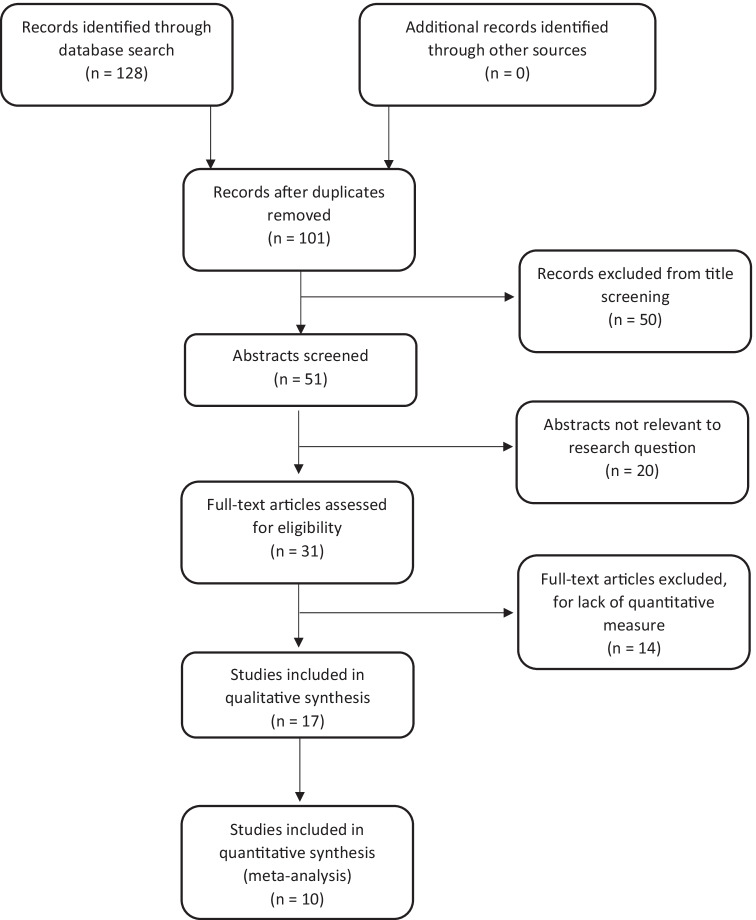
The workflow outlined in Fig. 1 initially identified 128 articles. After duplicates were removed, this number was reduced to 101. After titles and abstracts were reviewed, the number of included articles was reduced to 31. After full-text review, another 14 articles were excluded from the review based on the inclusion/exclusion criteria, leaving a total of 17 articles for the qualitative review [5, 7, 8, 12–25]. All the studies reported significant positive findings (the 3D printed model being found useful for teaching purposes), with the major outcomes being outlined in Table 1. Among the most common usages were applications to the head and skull [14, 15, 18, 19, 21, 22], heart [13, 17, 23, 24], and lower limb orthopedics [5, 16, 20, 25]. There were no major disputes across assessors in the STROBE scoring. The average STROBE score was 15.94 ± 2.14 with scores ranging between 12 and 20, indicating a moderate level of study quality. Of these 17, 7 were removed for having insufficient data (comparisons of assessment to a control group with mean scores reported) [7, 8, 13, 21–24]. While 12 randomized control trials were identified for the meta-analysis, 2 of the articles were excluded for not reporting mean and standard deviation values [7, 22]. The final list of studies that were included in the meta-analysis included 10 original research articles [5, 12, 14–20, 25].
Fig. 1.
Search workflow demonstrating the number of articles that were available from the initial database search to final inclusion in the qualitative and quantitative reviews
Table 1.
Study breakdown for all studies included in the systematic review reporting their study design, population, objectives for model development, and outcomes. Studies that were included in the meta-analysis are denoted by *
| Reference | Study design | Education level | Objective | Major findings | STROBE score |
|---|---|---|---|---|---|
| *AlAli et al. [19] | Randomized control trials (n = 67) | Medical students | Models of child cleft lip and palate were developed for hands on seminars | Models improved percentage of knowledge gained (p = 0.038) and self-reported learning experience (p = 0.005) and visualization (p = 0.001) | 14 |
| *Awan et al. [20] | Randomized control trial (n = 22) | Radiology residents | Model colored into different segments to show different acetabular fracture patterns | Radiology students who received the model performed better on a post-test than those who did not (p = 0.02) | 15 |
| Backhouse et al. [21] |
Cohort study (n = 69) |
First-year ocular anatomy students | Investigate students’ perceptions of the impact the 3D printed orbit had on their learning, predicting that students would find the 3D printed orbit an engaging and valuable resource | Ability to physically manipulate the model and accessibility significantly helped learning (p < 0.001). 94% of participants agreed that the 3D printed orbit helped understand the spatial relationship between the orbital bones | 17 |
| *Cai et al. [5] | Randomized control trial (n = 35) | First-year medical students | Observe differences between didactic learning and simulation model learning of the knee joint between sexes | Students who used the knee simulator model performed better than the didactic learning group on the 11-question quiz (p < 0.01) | 14 |
| Chen et al. [22] | Randomized control trial (n = 79) | Third-year medical students | Compare the learning efficiency of 3D printed skulls with that of cadaveric skulls and atlas | The 3D printed group was better than the other two groups in total score (p = 0.044) and scores of lab test (p = 0.049) | 17 |
| Costello et al. [23] | Cohort study (n = 29) | 16 medical students, 13 premedical students | Ventricular septal defect 3D printed models for educational curriculum for premedical and medical students | All students reported significant improvement in the areas of knowledge acquisition (p < 0.0001), knowledge reporting (p < 0.0001), and structural conceptualization (p < 0.0001) of VSDs following completion of the seminar | 18 |
| Garas et al. [24] |
Cohort study (n = 23) |
11 first-year undergraduate students, 13 third-year students | External heart, shoulder, and thigh models compared to plastinated cadaveric models | Students got significantly more answers correct with the model (p < 0.0001) | 17 |
| *Hojo et al. [25] | Randomized control trial (n = 102) | 34 medical students, 34 residents, 34 surgeons | Model used to explain lateral pelvic lymph node dissection | Students using the 3D printed models had performed better than controls on a number of short and long tests (p ≤ 0.05) | 17 |
| Kong et al. [7] | Randomized control trial (n = 92) | First-year medical students | Model based on cadaveric information of liver without hepatic disease to show different segments | Models were reported more useful that the traditional anatomic atlas (p < 0.05) | 13 |
| *Lane et al. [18] | Randomized control trial (n = 44) | Second-year medical students | Models developed to replicate craniosynostosis for repair through plastic surgery | The results of some individual scores were significant; however, there was no significant difference between the experimental and the control group (p = 0.38) | 16 |
| *Li et al. [12] | Randomized control trial (n = 120) | First- and second-year medical students | Students were randomized into three teaching module groups [two-dimensional computed tomography images (CT), 3D, or 3D printed] and asked to answer 10 key anatomical and 4 evaluative questions | The use of a 3D printed model improved scores compared to 2D images (p < 0.0001), but not more than 3D imaging groups (p = 0.0508). Students in the 3D printed model group were also able to complete the evaluations significantly faster (p < 0.0001 vs. CT, p = 0.0006 vs. 3D image) | 17 |
| Mogali et al. [8] | Cohort study (n = 15) | Second-year MBBS students | A multi-colored model was developed of the upper limb and compared to plastinated models | 73% of the students felt that the 3D printed model improved their understanding (4 ± 0.93 out of 5) | 16 |
| Smerling et al. [13] | Cohort study (n = 45) | First-year medical students | Explore the impact on medical student learning of incorporation of 3D printed models for a wide array of congenital heart disease lesions during a teaching workshop | Strong positive correlation was found between mean increase in perceived knowledge and complexity of CHD (p = 0.03) 74.2% of students rated 3D printed models were helpful in their understanding of PS (mean ± SD 3.8 ± 1.0 out of 5) | 13 |
| *Tanner et al. [14] | Randomized control trial (n = 123) | Undergraduate, graduate, medical, dental, and PA students | Skull model displaying specific regions of interest | Students with the 3D printed model performed better than with the traditional model (p = 0.001) and reported it as more useful (p < 0.05) | 20 |
| *White et al. [17] | Randomized control trial (n = 60) | Pediatric residents and pediatric/emergency medicine residents | Differences in education of heart models displaying ventricular septal defects and Tetralogy of Fallot | The group that didn’t receive a 3D printed model performed better on the ventricular septal defect examination (p = 0.012), while the group that did receive a 3D printed models performed better on the Tetralogy of Fallot (p = 0.037) | 17 |
| *Wu et al. [16] | Randomized control trial (n = 90) | Medical students | Use of 3D printed models versus radiographic images as a technique for the education of medical students about bone spatial anatomy and fractures | Test-taking times for the pelvis and the spine for the traditional radiographic image group were significantly longer than the test-taking times for the 3D printed model group (p < 0.001 and p = 0.002, respectively) | 12 |
| *Yi et al. [15] | Randomized control trial (n = 60) | Second-year medical students | Evaluate the educational effect of 3D printed models (3DPMs), 3D images (3DIs), and 2-dimensional images (2DI) for the ventricular system | Students in the 3DPM and 3DI groups performed significantly better than those in the 2DI group in terms of the practice test score (3DPM group vs. 2DI group, p < 0.001; 3DPM group vs. 2DI group, p < 0.009) and total score (3DPM group vs. 2DI group, p < 0.001; 3DI group vs. 2DI group, p < 0.025) | 18 |
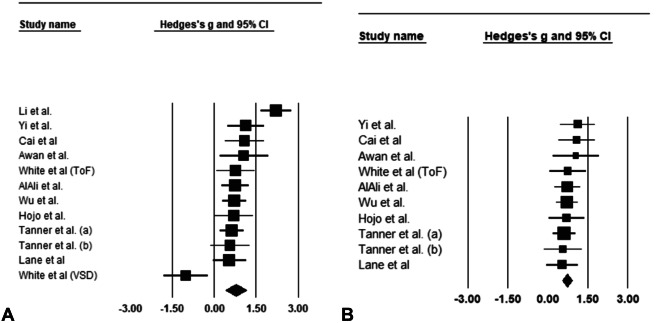
Of the 10 articles included in the meta-analysis [5, 12, 14–20, 25], two of the articles included two groups of interest [14, 17], meaning 12 total groups were compared for the analysis. For the 12 groups (n = 12) included in the quantitative analysis, performance assessments after instruction using the 3D printed model were compared to traditional teaching methods that lack these supplementations. These assessments were converted to percentages for similar comparisons. Most of the assessments used their own measurement techniques in the form of quizzes or rated performance assessments. The average score for students who used the model across the included studies was 73.41 ± 14.01, and 62.63 ± 14.13 for those who did not. A large, significant mean effect was found (g = 0.771, p < 0.001) in post-assessment performance when comparing the 3D printed model groups performance scores to the 2D image traditional learning groups (Table 2). The number of questions used in the assessments ranged from 7 to 15 questions unique to the region represented by the model. A large I2 value was calculated from this analysis, indicating a high probability of heterogeneity within the data (I2 = 77.567). When including all the studies in the quantitative analysis, we found the results to be heterogeneous (Q = 49.034, I2 = 77.567, p < 0.001).
Table 2.
Summary statistics for pooled effect size. Analysis 1 includes all applicable studies, analysis 2 excludes Li et al. and the ventricular septal defect group by White et al. [12, 17], analysis 3 included the studies focused on medical students, and analysis 4 included the studies focused on residents
| Analysis | n | Mean ∆ (95% CI) | p | Q | I2 | Fail-safe N |
|---|---|---|---|---|---|---|
| Analysis 1 | 12 | 0.771 (0.405, 1.137) | < 0.001 | 49.034 | 77.567 | 233 |
| Analysis 2 | 10 | 0.742 (0.560, 0.924) | < 0.001 | 3.827 | < 0.001 | 157 |
| Analysis 3 | 6 | 1.056 (0.562, 1.550) | < 0.001 | 23.808 | 78.999 | 123 |
| Analysis 4 | 3 | 0.263 (− 0.968, 1.493) | 0.676 | 15.055 | 86.715 | 0 |
Further investigation found two outliers within the dataset. In the study by Li et al., the experimental group who received the 3D printed models did significantly better than the control groups who did not receive the models [12]. Additionally, one of the groups in the study by White et al. actually found that the control group performed better than the experimental group that received the 3D printed models [17]. In the study by Li et al. the experimental group who received the models scored an average of 71.75 ± 14.35 which was similar to the total average; however, there was a large difference in the control group who only scored a 41.15 ± 13.30, which was well below the average of the pooled control group mean [12]. This difference led to a much greater effect size in the study by Li et al. and contributed to the greater heterogeneity within the data [12]. In the case for the ventricular septal defects group comparison in the study by White et al., the control group actually performed better than the experimental group that received the model [17]. The experimental group scored an average of 72.43 ± 16.29, while the control group scored an average of 85.71 ± 6.14 [17].
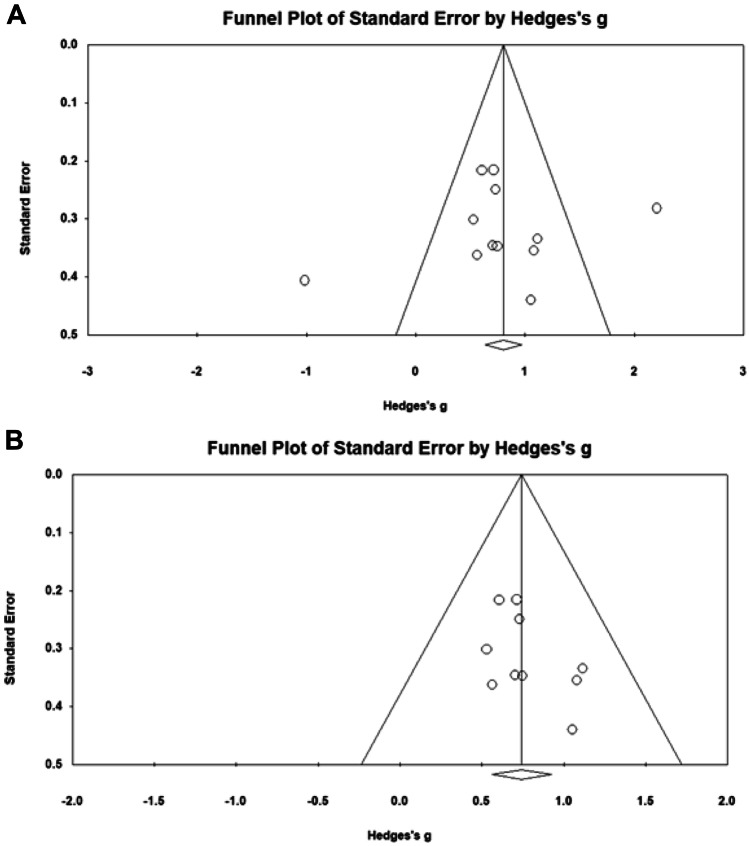
A second analysis was performed with the exclusion of the aforementioned studies by Li et al. and the ventricular septal defect study group in the article by White et al. (n = 10), and the average score for the model group was 73.68 ± 13.80, while the group that did not use a 3D printed model had an average of 62.47 ± 15.03 [12, 17]. These results were found to be much more homogenous (Q = 3.827, I2 < 0.001, p = 0.922), in addition to producing a significant mean effect size (g = 0.742, p < 0.001) when comparing the experimental group to the control group (Fig. 2). For this second analysis, there was a much smaller I2 value, indicating more homogeneity within the data (Fig. 3).
Fig. 2.
Forrest plot of the Hedge’s g values by the author of each study. A Analysis of all studies included in the review. B Exclusion of the study by Li et al. and the ventricular septal defect group by White et al. [12, 17]
Fig. 3.
Funnel plot of the Hedge’s g values for each of the studies by standard error. A Analysis of all studies included in the review. B Exclusion of the study by Li et al. and the ventricular septal defect group by White et al. [12, 17]
Of the 12 included comparisons, six were exclusive to medical students [5, 12, 15, 16, 18, 19], three contained residents [17, 20], two had a mixture of undergraduate, graduate, and medical students [14], while one had a mix of medical students and residents [25]. Therefore, sub-group analyses were conducted for the medical students and the resident comparisons. In the medical student population, the groups that received a 3D printed model performed significantly better than those who did not (p < 0.001); however, there was no significant difference between the model and no-model groups in the residency population (p = 0.676) (Table 2).
Discussion
The results from this systematic review show that the incorporation of a 3D printed anatomic model to supplement student education can be utilized for several different applications. Furthermore, the meta-analysis performed shows that when compared to traditional teaching methods, the incorporation of a 3D printed model significantly improves complex anatomy comprehension. The students who received the models consistently performed better than those who were taught with more traditional methods (i.e., CT scans or textbook images), showing a benefit to having a tangible model that can be manipulated rather than static 2D images. Comprehension of basic anatomy skills will directly impact patient quality of care, and as medicine continues to advance, the need to have a deep understanding of basic anatomy to treat unique pathologies will only increase. Improvements in anatomical understanding can play a large role in preparing for complex surgeries, especially for students with less overall experience than more senior surgeons.
3D printing for medical purposes is still a fairly new technology, with many recent innovations occurring within the last 10 years as printers have become more available. Therefore, the quality of papers included in the systematic review is only of a moderate quality. The results of the STROBE risk of bias assessment ranged from 12 to 20, with a mean value of 15.94 ± 2.14. Several of the studies did not address the potential lack of bias, as well as report all of their results. As more institutions begin to adapt this method of educating students, we are likely to see higher quality research emerge with similar assessments.
One major discrepancy among the articles was the methods used for assessment, which ranged from a full lab practical to small question surveys. It has previously been reported that major discrepancies currently exist between educational tools due to the difference in their desired outcomes [26]. In this study, there were a number of simple question surveys which were asked by a majority of the studies, then there were longer and more specific exams asked by Wu et al., and lastly, there were studies like Hojo et al. that were more interactive assessments and required students to correctly identify labels placed on the models [16, 25]. While the methods of assessment may have been different, the results were very similar. The group that used the 3D printed model as a part of their assessment consistently outperformed the group using only 2D CT images and textbook instructions.
Level of education is another important aspect to consider. Of the included studies, 12 included medical students [5, 7, 12–16, 18, 19, 22, 23, 25], 3 included residency students [17, 20, 25], and 3 included undergraduate students [14, 16, 24]. However, even at these different levels, there still seemed to be an improvement with the group that used the 3D printed models. The results of the sub-analyses found that there was a significant improvement in the medical student population (p < 0.001); however, no improvement was found within the residency population (p = 0.676). Sub-analysis could not be performed for the undergraduate population due to an insufficient sample size (n < 3).
The application of this technology can easily be seen when investigating the various model applications. As stated previously, the most common uses were the head and skull [14, 15, 18, 19, 21, 22], heart [13, 17, 23, 24], and lower limb orthopedics [5, 16, 20, 25]. These regions are notorious for being extremely complex and can significantly impact a patient’s quality of life. The results from other regions such as the liver [7] and arm [8] show that while these regions will still see benefit from 3D model implementation, the need for models in these regions is not as demanding.
The focus of this review was to investigate the impact anatomical models have on improving education specifically for human anatomy. We did find, however, similar results for animal models during the abstract review process [27, 28]. One previous study by Preece et al. found similar results to this study with the application of an equine hoof model, where students performed better with the utilization of a 3D model compared to without (p < 0.001) [27]. Another equine study conducted by Johnson et al. did not find significant differences between the group that used a 3D printed animal model and those who did not use a model when helping teach veterinary anatomy (p = 0.5732), but students who received a model reported more enjoyment during learning [28]. While animal models are outside the scope of this study, there is likely a benefit to animal anatomy education from the incorporation of 3D printed models.
There were several limitations to this study. The limited number of randomized control trials used for the meta-analysis left the final sample size relatively small since the cohort studies did not include a control group. This was especially an issue when attempting to perform sub-analyses groups such as undergraduate groups, where there were not a sufficient number of examples to produce meaningful results. While ten studies do shed some light on the subject, it may not be enough from which to draw large conclusions. Additionally, it is unknown the level of expertise of the people developing the 3D models. As previously explained by Tetsworth et al., there is a large discrepancy and steep learning curve associated with 3D model development that affects the accuracy of the final product [9]. Indeed, the models included in this study were likely sufficient at displaying the necessary information since there were significant findings in nearly all their applications.
Additionally, only the randomized control trials were used for the meta-analysis to make accurate comparisons, which limited the number of included studies. The article by Chen et al. only reported median values and inter-quartile ranges [22]. While the reported values were likely similar to the mean values, it was excluded from the final analysis. The study by Kong et al. only reported p-values, and was also not included in the final analysis [7].
Conclusion
The results from this systematic review with meta-analysis suggest that using 3D printed anatomical models to help teach both undergraduate and graduate students various anatomy topics will likely improve their short-term comprehension. However, there is currently a lack of literature showing the longevity of these results or the direct impact they have on patient care, with these two measurements requiring a more longitudinal approach. Due to how recent the implementation of 3D printing is within the medical field, it could be that these studies are currently underway or have not yet been performed by current research groups. Ideally, studies that observe these applications will be published to support the use of 3D printed models for student education.
Author Contribution
All authors contributed substantially to this study. Conception, literature review, analysis, and composition were performed by DS. MT assisted with the literature search and review. AR assisted with the data-analysis and meta-analysis interpretation. JZ assisted with revisions and supervision. All authors reviewed and approved the final document before submission.
Funding
This research was partially funded by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number R01NS114282 and the Biomechanical Rehabilitation and Manufacturing Initiative (BRMI).
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zuniga J, Katsavelis D, Peck J, Stollberg J, Petrykowski M, Carson A, et al. Cyborg beast: a low-cost 3D-printed prosthetic hand for children with upper-limb differences. BMC Res Notes. 2015;8. [DOI] [PMC free article] [PubMed]
- 2.Cui J, Chen L, Guan X, Ye L, Wang H, Liu L. Surgical planning, three-dimensional model surgery and preshaped implants in treatment of bilateral craniomaxillofacial post-traumatic deformities. J Oral Maxillofac Surg [Internet]. American Association of Oral and Maxillofacial Surgeons; 2014;72:1138.e1–1138.e14. Available from: 10.1016/j.joms.2014.02.023 [DOI] [PubMed]
- 3.Igami T, Nakamura Y, Hirose T, Ebata T, Yokoyama Y, Sugawara G, et al. Application of a three-dimensional print of a liver in hepatectomy for small tumors invisible by intraoperative ultrasonography: preliminary experience. World J Surg. 2014;38:3163–3166. doi: 10.1007/s00268-014-2740-7. [DOI] [PubMed] [Google Scholar]
- 4.Salazar D, Huff TJ, Cramer J, Wong L, Linke G, Zuniga J. Use of a three-dimensional printed anatomical model for tumor management in a pediatric patient. SAGE Open Med Case Reports. 2020;8:2050313X2092760. [DOI] [PMC free article] [PubMed]
- 5.Cai B, Rajendran K, Bay BH, Lee J, Yen C-C. The effects of a functional three-dimensional (3D) printed knee joint simulator in improving anatomical spatial knowledge. Anat Sci Educ [Internet]. 2019;12:610‐618. Available from: https://www.cochranelibrary.com/central/doi/. 10.1002/central/CN-02005754/full [DOI] [PubMed]
- 6.Ploch CC, Mansi CSSA, Jayamohan J, Kuhl E. Using 3D printing to create personalized brain models for neurosurgical training and preoperative planning. World Neurosurg. Elsevier Inc; 2016;90:668–74. [DOI] [PubMed]
- 7.Kong X, Nie L, Zhang H, Wang Z, Ye Q, Tang L, et al. Do 3D printing models improve anatomical teaching about hepatic segments to medical students? A randomized controlled study. World J Surg Springer International Publishing. 2016;40:1969–1976. doi: 10.1007/s00268-016-3541-y. [DOI] [PubMed] [Google Scholar]
- 8.Mogali SR, Yeong WY, Tan HKJ, Tan GJS, Abrahams PH, Zary N, et al. Evaluation by medical students of the educational value of multi-material and multi-colored three-dimensional printed models of the upper limb for anatomical education. Anat Sci Educ. 2018;11:54–64. doi: 10.1002/ase.1703. [DOI] [PubMed] [Google Scholar]
- 9.Tetsworth KD, Mettyas T. Overview of emerging technology in orthopedic surgery. Tech Orthop [Internet]. 2016;31:143–52. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00013611-201609000-00002
- 10.Waran V, Narayanan V, Karuppiah R, Pancharatnam D, Chandran H, Raman R, et al. Injecting realism in surgical training—initial simulation experience with custom 3D models. J Surg Educ [Internet]. Elsevier; 2014;71:193–7. Available from: 10.1016/j.jsurg.2013.08.010 [DOI] [PubMed]
- 11.Gasco J, Holbrook TJ, Patel A, Smith A, Paulson D, Muns A, et al. Neurosurgery simulation in residency training: feasibility, cost, and educational benefit. Neurosurgery. 2013;73:39–45. doi: 10.1227/NEU.0000000000000102. [DOI] [PubMed] [Google Scholar]
- 12.Li Z, Li Z, Xu R, Li M, Li J, Liu Y, et al. Three-dimensional printing models improve understanding of spinal fracture—a randomized controlled study in China. Sci Rep [Internet]. 2015;5:11570. Available from: https://www.cochranelibrary.com/central/doi. 10.1002/central/CN-01180013/full [DOI] [PMC free article] [PubMed]
- 13.Smerling J, Marboe CC, Lefkowitch JH, Pavlicova M, Bacha E, Einstein AJ, et al. Utility of 3D printed cardiac models for medical student education in congenital heart disease: across a spectrum of disease severity. Pediatr Cardiol [Internet]. Springer US; 2019;40:1258–65. Available from: 10.1007/s00246-019-02146-8 [DOI] [PubMed]
- 14.Tanner JA, Jethwa B, Jackson J, Bartanuszova M, King TS, Bhattacharya A, et al. A three-dimensional print model of the pterygopalatine fossa significantly enhances the learning experience. Anat Sci Educ. 2020;13:1–13. doi: 10.1002/ase.1942. [DOI] [PubMed] [Google Scholar]
- 15.Yi X, Ding C, Xu H, Huang T, Kang D, Wang D. Three-dimensional printed models in anatomy education of the ventricular system: a randomized controlled study. World Neurosurg [Internet]. 2019;125:e891‐e901. Available from: https://www.cochranelibrary.com/central/doi/. 10.1002/central/CN-02012582/full [DOI] [PubMed]
- 16.Wu A-M, Wang K, Wang J-S, Chen C-H, Yang X-D, Ni W-F, et al. The addition of 3D printed models to enhance the teaching and learning of bone spatial anatomy and fractures for undergraduate students: a randomized controlled study. Ann Transl Med AME Publishing Company. 2018;6:403–403. doi: 10.21037/atm.2018.09.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.White SC, Sedler J, Jones TW, Seckeler M. Utility of three-dimensional models in resident education on simple and complex intracardiac congenital heart defects. Congenit Heart Dis. 2018;13:1045–1049. doi: 10.1111/chd.12673. [DOI] [PubMed] [Google Scholar]
- 18.Lane JC, Black JS. Modeling medical education: the impact of three-dimensional printed models on medical student education in plastic surgery. J Craniofac Surg. 2020;31:1018–1021. doi: 10.1097/SCS.0000000000006567. [DOI] [PubMed] [Google Scholar]
- 19.AlAli AB, Griffin MF, Calonge WM, Butler PE. Evaluating the use of cleft lip and palate 3D-printed models as a teaching aid. J Surg Educ [Internet]. 2018;75:200‐208. Available from: https://www.cochranelibrary.com/central/doi/. 10.1002/central/CN-01665715/full [DOI] [PubMed]
- 20.Awan OA, Sheth M, Sullivan I, Hussain J, Jonnalagadda P, Ling S, et al. Efficacy of 3D printed models on resident learning and understanding of common acetabular fracturers. Acad Radiol [Internet]. Elsevier Inc.; 2019;26:130–5. Available from: 10.1016/j.acra.2018.06.012 [DOI] [PubMed]
- 21.Backhouse S, Taylor D, Armitage JA. Is this mine to keep? Three-dimensional printing enables active, personalized learning in anatomy. Anat Sci Educ. 2019;12:518–528. doi: 10.1002/ase.1840. [DOI] [PubMed] [Google Scholar]
- 22.Chen S, Pan Z, Wu Y, Gu Z, Li M, Liang Z, et al. The role of three-dimensional printed models of skull in anatomy education: a randomized controlled trail. Sci Rep [Internet]. 2017;7:575. Available from: https://www.cochranelibrary.com/central/doi/. 10.1002/central/CN-01628053/full [DOI] [PMC free article] [PubMed]
- 23.Costello JP, Olivieri LJ, Krieger A, Thabit O, Marshall MB, Yoo SJ, et al. Utilizing three-dimensional printing technology to assess the feasibility of high-fidelity synthetic ventricular septal defect models for simulation in medical education. World J Pediatr Congenit Hear Surg. 2014;5:421–426. doi: 10.1177/2150135114528721. [DOI] [PubMed] [Google Scholar]
- 24.Garas M, Vaccarezza M, Newland G, McVay-Doornbusch K, Hasani J. 3D-printed specimens as a valuable tool in anatomy education: a pilot study. Ann Anat [Internet]. Elsevier GmbH.; 2018;219:57–64. Available from: 10.1016/j.aanat.2018.05.006 [DOI] [PubMed]
- 25.Hojo D, Murono K, Nozawa H, Kawai K, Hata K, Tanaka T, et al. A three-dimensional printed pelvic model is useful for education about lateral lymph node dissection: a randomized controlled trial. Dis Colon Rectum [Internet]. 2019;62:e64‐e65. Available from: https://www.cochranelibrary.com/central/doi/ . 10.1002/central/CN-01957598/full
- 26.Cook DA, Ellaway RH. Evaluating technology-enhanced learning: a comprehensive framework. Med Teach. 2015;37:961–970. doi: 10.3109/0142159X.2015.1009024. [DOI] [PubMed] [Google Scholar]
- 27.Preece D, Williams SB, Lam R, Weller R. “Let’s get physical”: advantages of a physical model over 3D computer models and textbooks in learning imaging anatomy. 2013;224:216–24. [DOI] [PubMed]
- 28.Johnson KL, Hespel AM, Price JM, de Swarte M. Use of color-coded, three-dimensional-printed equine carpus models is preferred by students but does not result in statistically different academic performance. Vet Radiol Ultrasound. 2021;62:76–83. doi: 10.1111/vru.12929. [DOI] [PubMed] [Google Scholar]