Abstract
This systematic review aimed to synthesize the literature on how ultrasound is currently used in anatomy education within medical schools. A systematic search of Ovid MEDLINE, Scopus, and Educational Resources Information Centre was conducted. Thirty-four relevant unique articles were included from the 1,272 identified from the databases and analyzed via narrative synthesis. Thematic analysis generated two domain summaries: “Successful Aspects of Ultrasound Teaching” and “Barriers to Implementation,” each with additional subthemes, aimed to help educators inform best teaching practices from the current evidence base in this field.
Keywords: Medical education, Medical students, Point-of-care ultrasonography, Ultrasonography, Ultrasound, Anatomy education, Undergraduate medical education, Systematic review
Introduction
Understanding best practices for teaching is essential to meet the demands placed on anatomy education in the modern era. For example, in 2009, the General Medical Council of the United Kingdom (UK) published “Tomorrow’s Doctors” [1] which noted the need for medical schools to provide students with teaching focused on more holistic and clinical content [2]. This resulted in a notable decrease in anatomical teaching hours [3], despite the fact that many quote anatomy as being central to the practice of well-qualified professionals [4]. This is not a problem unique to the UK alone; the decrease in anatomical teaching can be observed globally [5–8].
Unsurprisingly, this has caused concern regarding the quality of students’ understanding of anatomy [9], leading to publications communicating the need for better understanding alternative pedagogic techniques for teaching anatomy that are both cost and time efficient, as well as being engaging and useful for the clinical student population [10]. One of the technologies suggested has been the use of ultrasound.
Ultrasound education has developed into a very popular topic of discussion within the health professions field. A search of “ultrasound education” in PUBMED reveals the number of associated publications has increased drastically over the past 20 years, from 615 in the year 2000 to 6838 in 2020. Part of this expansion has been the push to have more healthcare workers and trainees be able to perform point-of-care ultrasound (POCUS) at the patient’s bedside, reducing wait times and staffing of formal sonography in some cases [11]. This includes medical students, who are now more frequently given the opportunity to learn how to produce and interpret radiological images, including ultrasound, as a component of their education prior to specialist training [12].
As a result, there has been a large increase in publications investigating and evaluating this implementation of ultrasound training programs within medical school curricula [13, 14], including a number of systematic reviews [15, 16]. However, these articles have broader aims about ultrasound education, and do not make considerations for the nuances of undergraduate anatomy education. Additionally, the limited number of reviews on ultrasound education are quite broad, including studies with a range of curricula from different specialties, ranging from cardiology [17] to family medicine [18].
Most research into the use of ultrasound in anatomy education has been associated with single-site studies, utilizing relatively small sample populations to research student attitudes or improvement in attainment. While such varied perspectives offer insight, one could argue that ultrasound education may not be a “one size fits all” teaching methodology. This viewpoint was concluded by Lian et al. [19], who discovered that some teaching methods do not suit all ultrasound competencies. Collating and understanding best teaching practice from varied studies is of utmost importance, as using ultrasound as an anatomical educational tool may necessitate a unique financial and resource burden [20, 21], as well as time commitment within already crowded curricula [6–8]. Additionally, it is key to try to and elucidate how ultrasound anatomy teaching compares or complements other methods, such as didactic content, or cadaveric teaching.
Thus, this systematic review aimed to synthesize the available literature on how ultrasound is currently used in anatomy education within medical schools, and to present the outcomes of such use. The narrative synthesis aspect in the present work aimed to use these outcomes in order to discuss themes which could add a new perspective to ultrasound educational programs and provide best teaching practice recommendations to help guide future ultrasound teaching sessions within anatomy education.
Methods
Search Strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) framework [22]. This review involved a thorough and systematic search of English-language articles published up to April 16, 2021, with a focus on ultrasound in anatomical education.
An initial limited search of Ovid MEDLINE and EMBASE identified relevant keywords contained in the title, abstract, and headings. These keywords were then used in an extensive search of the literature using three databases: Ovid MEDLINE, Scopus, and Education Resources Information Centre (ERIC). The keywords were used across the databases relating to the target population, the intervention, the setting, and the outcome. The full search strategy for each literature database can be provided to interested readers by contacting the corresponding author.
Inclusion and Exclusion Criteria
Prior to article screening, comprehensive inclusion and exclusion criteria were drawn up following discussion and consensus from all members of the research group. All articles meeting the following criteria were eligible for inclusion in this review: all forms of research methodology, involved ultrasound in an educational capacity to teach anatomy, used a study population of medical students, and English language. There were no date or country of publication restrictions. Exclusion criteria for this review included use of a study population including others except medical students, no primary data reported, or the use of therapeutic ultrasound.
Screening of Abstracts and Full-Text Articles
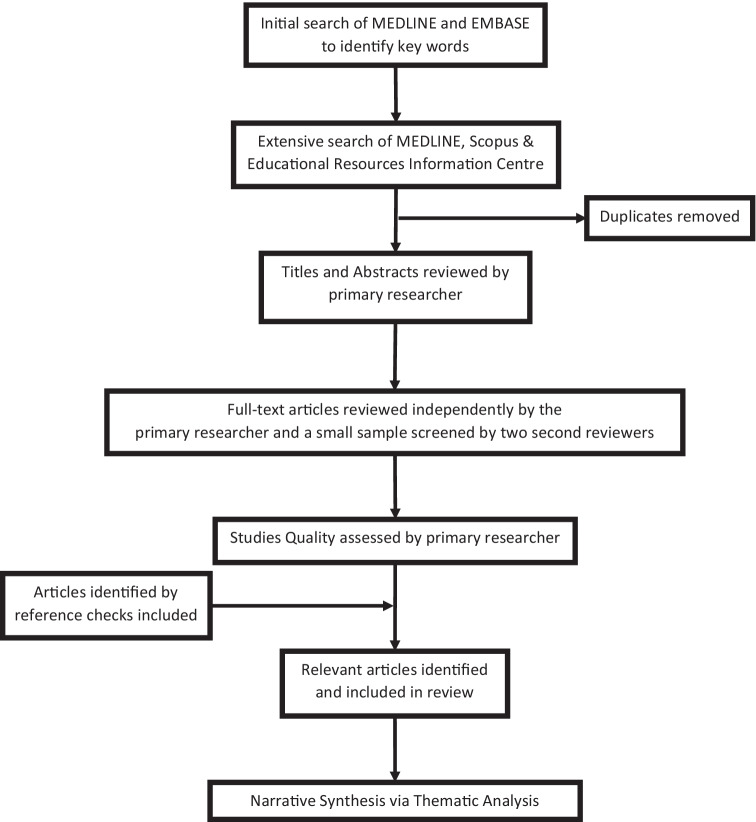
All titles and abstracts were reviewed by the primary investigator (EJGK) based on the inclusion and exclusion criteria listed above. Following this, the full text for all of the included studies was ordered and reviewed independently by the primary investigator. A small sample of studies (18%) were randomly selected and also independently analyzed by two second reviewers (MT and HNM). Reviews and outcomes for these subsets of articles were then discussed with the entire research team to ensure consensus and to ensure dependability of work. Additional articles were identified via citation chaining of included articles. The entire search process is summarized in Fig. 1.
Fig. 1.
Flow diagram for the selection of studies
Quality Assessment
The primary investigator evaluated the quality of included studies using the Medical Education Research Study Quality Index (MERSQI) [23]. The MERSQI is an instrument used to assess methodological quality in medical education research. It investigates several factors, for example, study design, sampling, and data analysis. It has been previously reported to be a reliable and useful tool [24]. Quality assessment was not done as a means of inclusion/exclusion, rather to provide additional data about included studies.
Analysis
This review utilized a narrative synthesis as the primary means of analysis. This method was selected due to the heterogeneity of included studies, as previously recommended by Davis et al. [15]. Narrative synthesis refers to an “approach to the systematic review and synthesis of findings from multiple studies that relies primarily on the use of words and text to summarize and explain the findings of the synthesis” [25]. While heterogeneous in nature, the included studies still offer important insights for teaching practice in ultrasound education, making narrative synthesis an appropriate analysis method to synthesize such points. Reflective thematic analysis was conducted for this narrative synthesis in the six-step approach as suggested by Braun and Clarke [26] with the exception of the use of domain summaries in the place of traditional themes. According to Braun and Clarke, while themes contain items of shared meanings, domain summaries are said to describe a range of similarities or differences in a shared topic [27]. The primary investigator (EJGK) became familiar with the data, generated initial codes, and identified domain summaries. The same two second reviewers (MT, HNM) were involved in coding and generating independent domain summaries for a small sample of included papers; each reviewed two studies. Following this, differences in coding and generated domain summaries were discussed among reviewers and the wider research team, to improve credibility of the work. The process of identifying domain summaries was inductive and completed during the full-text analysis.
Reflexivity
This research was conducted by a group of researchers with differing baseline paradigmatic views, including post-positivists [34]. Nevertheless, a narrative synthesis utilizing thematic analysis was selected as the most appropriate means of analysis, given the research aims and heterogeneity of included studies. It is also important to note here the interest in ultrasound education the authors share, especially at the undergraduate level of medical education. While the research team hold varying ultrasound experiences, no ultrasound curricula existed at the research team’s institution during the research period. As such, this might have resulted in more of an “outside” perspective on the analysis. Finally, the research team was diverse in educational background and professional level, offering heterogeneity in views when discussing analysis.
Results
Search Results
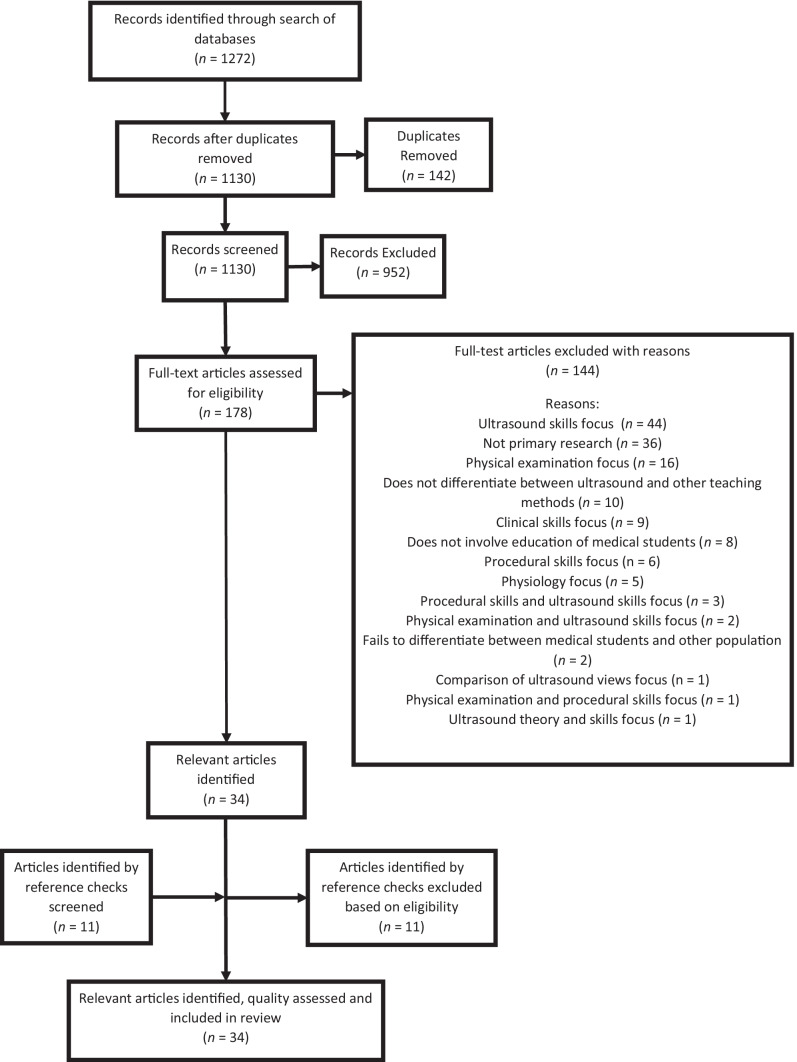
The search of the three databases yielded an initial number of 1,272 studies, which was reduced to 1,130 after duplicates were removed. 952 of these articles were excluded during title and abstract review for having no relevance to anatomical education and/or not including medical students as study cohorts. Following full-text screening, 34 relevant articles remained that met all the inclusion criteria. Citation chaining revealed 11 more potentially relevant articles based on their titles; however, these were later excluded during abstract and full-text screening. This whole process, including reasons for study exclusion, is summarized in Fig. 2.
Fig. 2.
Flow chart of the study selection process modelled from work by Liberati et al. [28] and Moher et al. [29]
Study Characteristics
The majority of the included studies were conducted in the USA (50%, [17 of 34]), followed by the UK (15%, [5 of 34]), Germany (12%, [4 of 34]), and Australia (9%, [3 of 34]). Norway [30], New Zealand [31], France [32], Poland [33], and Canada [34] were all the country of origin for one publication each. Notably, a higher proportion of the included studies were published in recent years, for example, only one was published in 2010 [35] compared to four in 2019 [36–39]. More detailed characteristics of the included studies can be provided to interested readers by contacting the corresponding author.
Ultrasound Educational Activities
There were several lesson structures used within the included studies, the most common being a didactic introduction, with demonstration by facilitators and then a hands-on practical, or laboratory (29%, [10 of 34]). This was closely followed by a similar method but excluding the demonstration component (26%, [9 of 34]).
Of the 22 studies that reported group sizes for the hands-on component of their ultrasound intervention, only one study reported students working individually [36]. The remainder varied to a large degree, from students working in pairs [33] to groups of up to 25 [40]. Notably, the two included studies that originally had the largest group sizes during the hands-on component of the ultrasound sessions both reduced the number of students allocated to each ultrasound machine during their data collection in response to student feedback [30, 40].
Half of the included studies investigated the use of ultrasound using first year medical student participants, while ten of the included studies investigated its use with second year medical students (29%). Three further papers investigated the use of ultrasound to teach anatomy using both first and second year medical students [40–42]. Investigating the use of ultrasound to teach anatomy within the traditional “clinical years” was less notable. Only four studies researched its use within the third [31, 43] or fourth years [33, 44] of the medical curriculum.
The data concerning the ultrasound session facilitators were also extracted from each of the included studies. Of those that reported the instructors used, the vast majority included the use of clinicians as instructors (78%, [21 of 27]), while anatomy faculty (33%, [9 of 27]), near-peer students (30%, [8 of 27]), and sonographers (15%, [4 of 27]) were used less often. The percentages here add up to greater than 100% to reflect the mixed use of instructors within some teaching sessions (48%, [13 of 27]).
All 34 studies described when their ultrasound interventions occurred in relation to the involved student participants’ standard anatomy teaching. Most conducted the ultrasound sessions “alongside” or integrated with the anatomy curriculum (53%, [18 of 34]), while slightly fewer set the intervention after the anatomy teaching sessions (29%, [10 of 34]). Even fewer studies involved students using ultrasound to learn the anatomy prior to the currently used anatomy teaching practices [38, 45, 46].
Study Outcomes
In the included studies, a range of outcomes were assessed. These ranged from solely objective measurements [4 of 34], solely subjective [15 of 34], or a combination of the two [15 of 34]. Objective measures were considered as those that assessed student knowledge improvement, whereas subjective were around student attitudes.
In those that included an objective measurement [19 of 34], the results ranged from positive (53%, [10 of 19]) to neutral (26%, [5 of 19]) and mixed (21%, [4 of 19]). None of the studies that assessed an objective outcome reported only negative results.
Subjective outcomes were assessed in 30 (88%) of the 34 studies. They predominantly focused on participants’ opinions on ultrasound, the ultrasound sessions, and the implementation of ultrasound into anatomy (93%, [28 of 30]). Overall, the results of subjective measures were either positive (60%, [18 of 30]) or mixed (40%, [12 of 30]). None of the included publications reported solely negative or neutral student perceptions.
The modes of assessment for both the objective and subjective measurements are detailed in the supplemental material that can be provided by contacting the corresponding author.
Qualitative Findings
Two domain summaries were generated via the narrative synthesis: “Successful Aspects of Ultrasound Teaching” and factors noted as “Barriers to Implementation” of ultrasound into the anatomy curriculum. The domain summary “Successful Aspects of Ultrasound Teaching” investigated the good teaching practices that tended to correlate to a positive outcome, for example, student satisfaction with the ultrasound session, whereas the domain summary, “Barriers to Implementation,” related to problems encountered or reported to be likely encountered by authors during the creation of their teaching sessions and future implementation into the anatomy curriculum. The extensive results of the thematic analysis, including a larger quantity of illustrative quotes, can be provided to interested readers by contacting the corresponding author. All key elements and subthemes are shown in Table 1, including some illustrative excerpts from included articles.
Table 1.
Table providing description and illustrative examples of the subthemes generated during thematic analysis
| Domain summary/theme | Subtheme description | Examples (quotes from included articles) |
|---|---|---|
| Successful aspects of ultrasound teaching | ||
| Stakeholder attitudes — student perception of ultrasound | Medical students’ viewpoints on ultrasound within the medical curriculum and what they particularly like and dislike about the educational resource | “…students of all groups often reported that the dynamic and real-time nature of the imaging provided them with a better understanding of how the anatomical structures “work” and allowing fostering of strong links to physiology…” [35] |
| Stakeholder attitudes — year of study | How year of study and potential prior anatomical experience affected student perception of ultrasound | “Students with high prior anatomy experience suggested ultrasound may be better taught on their clinical days rather than as a part of anatomy curriculum. This may be because these students were more comfortable with normal anatomy seen on ultrasound images and preferred to spend more time on pathology and linking patients’ clinical presentations to abnormal findings on the images.” [42] |
| Stakeholder attitudes — cognitive load | Findings associating increase in cognitive load with student viewpoints on using this technology as an imaging tool to further their anatomical understanding |
“[Comments from participant]: ‘Most difficult part of me is getting used to the orientation on the screen and correlating it with probe orientation.’” [34] “…the minimal introduction provided to the learners may be sufficient to mitigate significant harm induced by image interpretation during participation in ultrasound-facilitated sessions.” [34] |
| The structure and implementation of pedological approaches — group size | How group sizes within the educational activity affected study outcomes | “…students need to see the probe position on the volunteer and the resultant image in the same field of view, so that students can integrate information from all elements of the demonstration; in large groups, it is likely that only students close to the demonstration can see all elements of it, which may explain students’ desire for smaller groups.” [40] |
| The structure and implementation of pedological approaches — relation to normal anatomy | Findings on timing/placement of the ultrasound sessions within the medical curriculum and how this affected study outcomes | “Students favored having the sessions later-on in the teaching of the course, because they found the sessions more interesting after they already were exposed to the anatomical topics.” [47] |
| The structure and implementation of pedological approaches — educational activity | Details on the structure of the ultrasound sessions and whether the inclusion or exclusion of some activities affected study outcomes |
“The second-year students were very keen to have background information to guide them in the differentiation of tissue types so that they did not have to rely on their “imagination” to interpret the image.” [41] “Our experience revealed that teachers and students found more relevance in the practical phase of the session, which combined education and entertainment. This part appeared to best stimulate the interest of students and encourage their desire to deepen their knowledge of anatomy.” [32] |
| Impact of facilitators — type of teacher | Use of different types of facilitators within the ultrasound sessions and the effect on study outcomes |
“In this study, we utilized a physician to teach the relevant cardiac anatomy using a clinical imaging modality; this in itself may promote retention of cardiac anatomy as the students aim to become accepted as part of the clinical community.” [45] “…Minimally instructed student-teachers can be employed to teach anatomically skilled students, whereas medical experts should be used in earlier stages of anatomical education…One aspect might be the steep learning curve and the complexity of MSUS [musculoskeletal ultrasound].” [48] |
| Barriers to implementation | ||
| Lack of ultrasound equipment/cost | Prominent issues in ultrasound curriculum design; particularly, a lack of ultrasound resources |
“Tutors reported that access to more machines would enable further curriculum development (in teaching and assessment).” [40] “…the budget of many anatomy departments may not be large enough to support purchase of the machines.” [35] |
| Busy medical curriculum | Difficulties in implementing an ultrasound curriculum in an already arguably full medical curriculum | “…the addition of new instructional sessions may require that time is reallocated from other components of anatomy education” [49] |
| Teacher availability | Issues in recruiting and providing adequate training to ultrasound facilitators | “…the number of instructors required to establish an ultrasound curriculum will undoubtedly vary among medical schools – based on a number of factors, including class size, available machines, room availability, and others…” [21] |
Quality Assessment
All included studies were assessed for quality using the MERSQI. The mean score of this was 9.78 of a possible 18, a median of 9.5, with a range between 6 and 14.5. The most common study design was a single group post-intervention test (65%, [22 of 34]), followed by a randomized control trial design (18%, [6 of 34]). It is important to add that a majority of the included studies lacked a control group (71%, [24 of 34]). Sample sizes of the included studies were consistently over 100 medical students (71%, [24 of 34]). Evidence of validity of the evaluation instrument was seldom reported (32%, [11 of 34]), with content validity being most common (29%, [10 of 34]) and relationship to other variables being least common [50]. Unfortunately, a funnel plot could not be generated due to heterogenicity of the data.
Discussion
This systematic review identified 34 relevant studies that investigated the use of ultrasound to aid the acquisition of anatomical knowledge in a medical student population. Thirty of the studies assessed subjective outcomes, including student attitude to the introduction of ultrasound into the anatomy curriculum. The investigation of more objective outcomes, such as improvement in anatomical exam scores, was assessed in only 19 of the papers. Although the included studies were generally of “modest quality” by the standards of the MERSQI, the results of these papers were mostly positive and supported the introduction of ultrasound into the anatomy curriculum. Further, findings and conclusions prove insightful for the development and delivery of anatomy-related ultrasound sessions. The two domain summaries generated: “Successful Aspects of Ultrasound Teaching” and factors reported as “Barriers to Implementation” of ultrasound into the anatomy curriculum guide the discussion below.
Successful Aspects of Ultrasound Teaching
Stakeholder Attitudes
Most of the included studies reported that students had a positive perception of the use of ultrasound within anatomical education. For example, the Swamy and Searle [51] study had one student highlight how ultrasound sessions are “‘…useful as they will be will be applicable as our future as doctors’.” This is one criticism of traditional methods of teaching anatomy, such as prosections, where students are not able to recognize the clinical significance of learning anatomy during their preclinical years [4, 52, 53]. Clinical contextualization is important in medical education as it has been postulated that teaching with this focus can convey to students why learning anatomy is important to their future practice, thus facilitating long-term knowledge retention [54]. Students want a new teaching modality to be relevant not only to their future practice but also to their current studies. Both Sweetman et al. [41] and Moscova et al. [42] reported that while students in their preclinical years were happy with simply visualizing anatomical structures, those who had further progressed into the medical degree felt they wanted to see more pathological images and the clinical significance of these findings.
The Structure of the Pedological Approaches
It is interesting to note that some of the included studies omitted the use of a demonstration. In the studies that lacked a demonstration, it is reported that students felt they would have benefited from more teaching in the ultrasound technique and image interpretation [41, 55]. Where a demonstration was used, students highly valued it [32, 47, 50, 56, 57]. Although seemingly omitted due to time pressures, it has been previously published that medical students have the ability to adapt to new technology quickly [58–60]. Seemingly, only a short introduction to the ultrasound fundamentals and equipment would be necessary for students, especially considering that the focus of the teaching sessions in this review was to further anatomical knowledge, not teach students how to perform clinical assessment with ultrasound. These findings suggest that it may be beneficial to reduce didactic time in sessions, instead supplementing it with a scanning demonstration, to support student attention and feedback.
As reported by Hammoudi et al. [32], both teachers and students found the hands-on teaching format, where students were able to use the probes to produce ultrasound images, to not only be the most enjoyable part of the ultrasound session but also the most appropriate in terms of conveying clinical relevance and anatomical knowledge. The benefits of hands-on instruction were also demonstrated by Knudsen et al. [61] who reported that after 6 weeks, students who had hands-on training were able to answer questions relating to image interpretation much faster than those who did not have hands-on experience. This aligns with previous research suggesting hands-on education might train pattern recognition skills, help students retrieve prior knowledge, and improve students’ self-confidence with their answers more effectively than those with no hands-on education [62]. Indeed, there has been a push for educators to introduce more pattern recognition training into the medical curriculum [62–65]. Consequently, these results suggest that it would be advantageous to implement further hands-on teaching in ultrasound sessions to support student anatomical learning. However, it would be important to consider the balance of hands-on experience with anatomy focus on sessions.
Linked with this, students often felt that the group sizes were too large, particularly in hands-on aspects of the teaching sessions, to allow them to truly benefit from the implementation of ultrasound into the anatomy curriculum [30, 34, 40, 42]. Although group size has not been investigated further within the ultrasound teaching context, it has been for students on clinical rotations. A study by Ofei-dodoo et al. [66] discovered that students similarly preferred smaller group sizes. The students highlighted several advantages of having smaller group sizes, including more contact times with both patients and clinicians, and more participation confidence [66]. Some of these results are naturally transferable to the topic of this review, given the potential similarity in clinical skills and ultrasound sessions; however, further research into group sizes within the context of ultrasound and anatomy teaching would be required.
Implementing Ultrasound into the Anatomy Curriculum
Longitudinal integration of anatomy within the medical curriculum has been and continues to be widely supported by clinicians from all specialties [67, 68]. This point was also argued by several of the authors of included studies. They posit that ultrasound should be a longitudinal skill and therefore, introduced early and revisited across the years [21, 33, 37, 61, 69].
The most common placement of the ultrasound sessions was alongside relevant anatomy curriculum, with only three studies implementing ultrasound prior to anatomical teaching practices already within institutions’ curricula [38, 45, 46]. Results from the thematic analysis demonstrate that students felt they would have benefited further if interventions had occurred after prior anatomical teaching “…because they found the sessions more interesting after they already were exposed to the anatomical topics” [47]. Knobe et al. [70] further voice this notion, stating that the effectiveness of an ultrasound session is dependent on students having some prior anatomical knowledge. This aligns well with the educational theory, constructivism, whereby learners build new knowledge upon the foundation of previous learning [71, 72]. Therefore, this review supports the notion that ultrasound sessions should be implemented after standard anatomy teaching and act as a recap of anatomical knowledge.
The Impact of Facilitators
Although different types of facilitators had different strengths, they were generally enjoyed by the student participants from studies, including the use of near-peer students noted in numerous works [21, 44, 50, 55, 69, 73–75]. Most of the included studies were from the USA, where near-peer assisted learning is more prevalent [76]. This is thought to result from increased motivation and stress, knowing that a higher level of knowledge is needed to teach a topic to others [77]. Consequently, the findings of this review support that near-peer students, with appropriate prior training, can effectively teach ultrasound in an anatomical context. This is congruent with findings present in the wider literature on the effectiveness of near-peer tutors [78–83].
Extensive training of facilitators prior to the session was often required and reported in numerous included studies as a barrier to the implementation of ultrasound into anatomy curricula [40, 47, 55, 73, 75]. Although this supports the notion that those with appropriate training can use ultrasound to highlight anatomy, there are conflicting views in the ultrasound education community. Hoppmann et al. [84] and Rao et al. [85] conclude that an ultrasound curriculum should be delivered by those with extensive experience using ultrasonography in the clinical setting, which contradicts reliance on anatomists and near-peers. To ease this conflict, course designers could aim to have more engagement with the sonography workforce and seek advice from professional bodies. Additionally, clinical collaboration could be targeted as some specialties regularly use ultrasound in practice. This would ensure sufficient expertise is available to allow students to recognize the utility of ultrasound in visualizing anatomy.
Barriers to Ultrasound Implementation
The two most reported barriers to implementation of ultrasound into the medical curriculum were the cost and lack of ultrasound equipment in many medical schools, and a lack of space in the already congested medical curriculum.
Although reducing in cost and relatively inexpensive in comparison to other imaging modalities [86], ultrasound continues to be unavailable to many anatomy departments. One suggestion to limit the potential problem of cost and lack of ultrasound equipment could be for medical schools to work more in tandem with ultrasound manufacturers to guarantee the availability of required resources and equipment. In reality, this is already standard practice in a number of medical schools in the USA [39, 87, 88] and Australia [42]. Nonetheless, should resources and suitable facilitators continue to be lacking, the use of a demonstration by a clinician and anatomy faculty in a large lecture theater could be employed. Indeed, Stringer et al. [31] found this teaching method to be effective in stimulating student interest in anatomy and ultrasound. However, the authors noted that some students struggled with image orientation and acknowledged that hands-on experience may help to combat this [31]. Alternatively, Smith et al. [75], who were similarly concerned about the funding of their anatomy department and the implications of introducing ultrasound sessions, were able to contact and borrow the required machines and resources from local simulation and emergency departments. All of these could be a potential solution should educators be concerned about the heavy financial and resource requirement of implementing ultrasound into the anatomy curriculum.
The problem associated with a busy medical curriculum is perhaps more difficult to solve. Time allocated to anatomy education within the medical curriculum has gradually decreased over the years, with Turney [3] previously suggesting this had fallen below a safe level. By implementing ultrasound into the already full anatomy curriculum [6, 7], other learning opportunities will be lost, for example, allocation of student learning time with traditional learning resources such as prosections. Consequently, this could have the effect of proliferating the problem of medical student lack of anatomical knowledge. This is a perennial problem associated with implementing any new teaching method into the medical curriculum and will likely continue to be in the future.
Limitations and Contradiction with Other Literature
Firstly, in conducting a systematic review, there is always the possibility of missing other potentially germane articles. In an attempt to mitigate this problem, three different databases were searched and citation chaining was conducted.
Second, the included studies were conducted in several different countries with different entry requirements for the medical degree, which affects the potential prior knowledge and experiences of the student populations [89–91]. This does not discount the research but is an important consideration point. Educators should keep this in mind, and consider their personal curricular circumstances, in their own application of this review’s findings.
Finally, another potential limitation encountered was the heterogeneity of the data. The studies included in this systematic review used various methodological designs and assessed a wide range of outcomes, despite being focused on anatomy education. Consequently, a meta-analysis could not be conducted. As a result, this systematic review includes descriptive analysis of the quantitative data, and the use of thematic analysis for a narrative synthesis of findings. While narrative synthesis may be viewed as “less rigorous” from a strict post-positivist perspective, or inferior to meta-analysis, this form of analysis can provide equally valuable perspectives from this particularly heterogenous literature, particularly for research aims like those in the present work.
This is particularly notable when comparing the present review to other recent literature in this field. Interestingly, a recent similar systematic review, also surrounding ultrasound education, came to different conclusions in their interpretation of their included articles [16]. Feilchenfeld et al. contended the introduction of ultrasound into the medical curriculum, as they concluded that the resources required for ultrasound implementation were not justified when factored against objective measurements. They argue that because medical education research is conducted by enthusiastic researchers, they will have a bias towards the study intervention and lack the ability to report the consequences of implementing such interventions into the medical curriculum. As a result, negative implications are not recognized until after significant resources have been expended to produce a change in the curriculum [16].
However, this perspective does not consider the tenets of confirmability that shape qualitative inquiry, rather than notions of objectivity, and that may be beneficial to combat perceptions of “bias” within medical education. Typically, a reflexivity section is provided to allow the reader to question the positionality under which the researcher has interpreted the data [92]. Indeed, perhaps all research should aim to include such, although this was not noted in many of the included studies of this review. Nevertheless, a number of the included articles’ aims were to describe their curricula and report the resources necessary for their use, taking a pragmatic and transparent approach [21, 88].
The present review has a number of different methodological approaches compared to the review conducted by Feilchenfeld et al. [16], which only included 8 studies specifically related to anatomical education. Furthermore, Feilchenfeld et al. [16] consider a non-statistically significant difference in student anatomical knowledge improvement between ultrasound and the currently approved “gold standard” pedagological approach, with the latter being superior. However, such non-statistically different results suggest that ultrasound may be on par with the current gold standard teaching method.
Additionally, while Feilchenfeld et al. [16] are correct to note that the articles surrounding ultrasound education are highly heterogenous, such heterogeneity of the articles simply highlights that ultrasound is being utilized and studied in a diverse range of settings. There are undoubtedly limitations to the studies that exist in this field; however, the narrative synthesis methodology in the current study examines the included studies beyond simply their findings to be able to inform educational practice. Still, institutions can thus weigh the proposed advantages against barriers for themselves, while considering best practice suggestions synthesized from the review above.
Conclusion
To conclude, this systematic review identified 34 relevant studies that assessed outcomes related to the use of ultrasound within the medical curriculum to teach anatomy. Despite some variation in study design and quality, the results of these studies indicated that students enjoyed the use of ultrasound to aid the acquisition of anatomical knowledge. To the anatomy educator looking to either start an ultrasound program or improve their existing program, six key “take-aways” from this review are as follows:
Ultrasound should be taught alongside standard anatomy teaching, as a supplemental experience that is “introduced early, and revisited often.”
The learning objectives for ultrasound activities in preclinical years should appear clinically relevant to students but focused on immediate anatomy education — students need to visualize “normal” to be able to then understand “abnormal.”
Individuals conducting anatomy education (ultrasound) research need to demonstrate more transparent reflexivity, to better frame understanding of activity implementation.
Anatomy ultrasound curricula should prioritize hands-on activities, with reduction of didactic time, supplementing it with scanning demonstrations, when used.
With appropriate training, “near-peer” student instructors for anatomical ultrasound sessions can be very effective.
Cost, equipment access, and “space” in medical curricula are the biggest barriers to more widespread integration of ultrasound within anatomy education, but collaborations may help remedy this.
Furthermore, future studies in this field should focus less on student perception of ultrasound, which have been shown to be overwhelmingly positive, and conduct more rigorous investigation of whether the addition of ultrasound to standard teaching practices furthers student anatomical knowledge to a statistically significant degree, and the potential longitudinal effects. But for now, by considering these best practice points among others identified in this review, it is the hope that ultrasound education will continue to make great advances in its role within anatomy education.
Author Contribution
Edward J. G. Kenny (EJGK) and Angelique N. Dueñas (AND) contributed to the review design and conception. Material preparation and data collection was performed by EJGK. Data analysis was performed by EJGK, with assistance from Haran N. Makwana (HNM) and Maria Thankachan (MT). The first draft of the manuscript was written by EJGK, and all authors commented on previous versions of the manuscript, with more revisions from AND and Lauren Clunie (LC). All authors read and approved the final manuscript.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Declarations
Ethics Approval
NA.
Consent to Participate
NA.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.GMC. Tomorrow’s doctors: outcomes and standards for undergraduate medical education. 3rd ed. Gen. Med. Counc. London, UK: General Medical Council; 2009.
- 2.Smith CF, Finn GM, Stewart J, Atkinson MA, Davies DC, Dyball R, et al. The Anatomical Society core regional anatomy syllabus for undergraduate medicine. J Anat [Internet]. John Wiley & Sons, Ltd; 2016;228:15–23. Available from: 10.1111/joa.12405. [DOI] [PMC free article] [PubMed]
- 3.Turney BW. Anatomy in a modern medical curriculum. Ann R Coll Surg Engl [Internet]. The Royal College of Surgeons of England. 2007;89:104–7. Available from: https://pubmed.ncbi.nlm.nih.gov/17346399. [DOI] [PMC free article] [PubMed]
- 4.Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: a review for its modernization. Anat Sci Educ [Internet]. 2010;3:83–93. Available from: 10.1002/ase.139. [DOI] [PubMed]
- 5.Papa V, Vaccarezza M. Teaching anatomy in the XXI century: new aspects and pitfalls. Georgiades P, Pretterklieber M, Klüppel M, Akita M, editors. Sci World J [Internet]. Hindawi Publishing Corporation; 2013;2013:310348. Available from: 10.1155/2013/310348. [DOI] [PMC free article] [PubMed]
- 6.Drake RL, McBride JM, Pawlina W. An update on the status of anatomical sciences education in United States medical schools. Anat Sci Educ [Internet]. John Wiley & Sons, Ltd; 2014;7:321–5. Available from: 10.1002/ase.1468. [DOI] [PubMed]
- 7.McBride JM, Drake RL. National survey on anatomical sciences in medical education. Anat Sci Educ [Internet]. John Wiley & Sons, Ltd; 2018;11:7–14. Available from: 10.1002/ase.1760. [DOI] [PubMed]
- 8.Rockarts J, Brewer-Deluce D, Shali A, Mohialdin V, Wainman B. National survey on Canadian undergraduate medical programs: the decline of the anatomical sciences in Canadian medical education. Anat Sci Educ [Internet]. John Wiley & Sons, Ltd; 2020;13:381–9. Available from: 10.1002/ase.1960. [DOI] [PubMed]
- 9.Farey JE, Bui DT, Townsend D, Sureshkumar P, Carr S, Roberts C. Predictors of confidence in anatomy knowledge for work as a junior doctor: a national survey of Australian medical students. BMC Med Educ [Internet]. 2018;18:174. Available from: 10.1186/s12909-018-1280-5. [DOI] [PMC free article] [PubMed]
- 10.Singh K, Bharatha A, Sa B, Adams OP, Majumder MAA. Teaching anatomy using an active and engaging learning strategy. BMC Med Educ [Internet]. 2019;19:149. Available from: 10.1186/s12909-019-1590-2. [DOI] [PMC free article] [PubMed]
- 11.Wong F, Franco Z, Phelan MB, Lam C, David A. Development of a pilot family medicine hand-carried ultrasound course. Wis Med J. 2013;112:257–261. [PubMed] [Google Scholar]
- 12.Jacob J, Paul L, Hedges W, Hutchison P, Cameron E, Matthews D, et al. Undergraduate radiology teaching in a UK medical school: a systematic evaluation of current practice. Clin Radiol England. 2016;71:476–483. doi: 10.1016/j.crad.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 13.Bell FE, Wilson LB, Hoppmann RA. Using ultrasound to teach medical students cardiac physiology. Adv Physiol Educ American Physiological Society. 2015;39:392–396. doi: 10.1152/advan.00123.2015. [DOI] [PubMed] [Google Scholar]
- 14.So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: impact on learning anatomy and physical diagnosis. Anat Sci Educ [Internet]. John Wiley & Sons, Ltd; 2017;10:176–89. Available from: 10.1002/ase.1630. [DOI] [PubMed]
- 15.Davis J, Wessner CE, Potts J, Au AK, Pohl CA, Fields M. Ultrasonography in undergraduate medical education: a systematic review. J ultrasound Med England. 2018;37:2667–2679. doi: 10.1002/jum.14628. [DOI] [PubMed] [Google Scholar]
- 16.Feilchenfeld Z, Dornan T, Whitehead C, Kuper A. Ultrasound in undergraduate medical education: a systematic and critical review. Med Educ England. 2017;51:366–378. doi: 10.1111/medu.13211. [DOI] [PubMed] [Google Scholar]
- 17.DeCara JM, Kirkpatrick JN, Spencer KT, Ward RP, Kasza K, Furlong K, et al. Use of hand-carried ultrasound devices to augment the accuracy of medical student bedside cardiac diagnoses. J Am Soc Echocardiogr [Internet]. 2005;18:257–63. Available from: http://www.sciencedirect.com/science/article/pii/S0894731704010910. [DOI] [PubMed]
- 18.Steller J, Russell B, Lotfipour S, Maldonado G, Siepel T, Jakle H, et al. USEFUL: ultrasound exam for underlying lesions incorporated into physical exam. West J Emerg Med United States. 2014;15:260–266. doi: 10.5811/westjem.2013.8.19080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lian A, Rippey JCR, Carr PJ. Teaching medical students ultrasound-guided vascular access—which learning method is best? J Vasc Access [Internet]. SAGE Publications Ltd STM; 2017;18:255–8. Available from: 10.5301/jva.5000730. [DOI] [PubMed]
- 20.Mirabel M, Celermajer D, Beraud A-S, Jouven X, Marijon E, Hagege AA. Pocket-sized focused cardiac ultrasound: strengths and limitations. Arch Cardiovasc Dis Netherlands. 2015;108:197–205. doi: 10.1016/j.acvd.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 21.Siegel-Richman Y, Kendall J. Establishing an ultrasound curriculum in undergraduate medical education: how much time does it take? J ultrasound Med England. 2018;37:569–576. doi: 10.1002/jum.14371. [DOI] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ [Internet]. 2021;372:n71. Available from: http://www.bmj.com/content/372/bmj.n71.abstract. [DOI] [PMC free article] [PubMed]
- 23.Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. J Am Med Assoc [Internet]. 2007;298:1002–9. Available from: 10.1001/jama.298.9.1002. [DOI] [PubMed]
- 24.Cook DA, Reed DA. Appraising the quality of medical education research methods: the medical education research study quality instrument and the Newcastle–Ottawa scale-education. Acad Med [Internet]. 2015;90. Available from: https://journals.lww.com/academicmedicine/Fulltext/2015/08000/Appraising_the_Quality_of_Medical_Education.23.aspx. [DOI] [PubMed]
- 25.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme. London: Institute for Health Research; 2006. [Google Scholar]
- 26.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol [Internet]. Routledge; 2006;3:77–101. Available from: https://www.tandfonline.com/doi/abs/10.1191/1478088706qp063oa.
- 27.Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Heal [Internet]. Routledge; 2019;11:589–97. Available from: 10.1080/2159676X.2019.1628806.
- 28.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol [Internet]. 2009;62:e1–34. Available from: http://www.sciencedirect.com/science/article/pii/S0895435609001802. [DOI] [PubMed]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med [Internet]. 2009;151:264–9. Available from: https://www.acpjournals.org/doi/abs/10.7326/0003-4819-151-4-200908180-00135. [PMC free article] [PubMed]
- 30.Heilo A, Hansen AB, Holck P, Laerum F. Ultrasound, “electronic vivisection” in the teaching of human anatomy for medical students. Eur J Ultrasound. 1997;5:203–207. doi: 10.1016/S0929-8266(97)00015-3. [DOI] [Google Scholar]
- 31.Stringer MD, Duncan LJ, Samalia L. Using real-time ultrasound to teach living anatomy: an alternative model for large classes. N Z Med J [Internet]. New Zealand; 2012;125:37–45. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med9&NEWS=N&AN=22960714. [PubMed]
- 32.Hammoudi N, Arangalage D, Boubrit L, Renaud MCMC, Isnard R, Collet J-PJ-P, et al. Ultrasound-based teaching of cardiac anatomy and physiology to undergraduate medical students. Arch Cardiovasc Dis [Internet]. Netherlands; 2013;106:487–91. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med10&NEWS=N&AN=23911833. [DOI] [PubMed]
- 33.Torres A, Staskiewicz GJ, Lisiecka J, Pietrzyk L, Czekajlo M, Arancibia CU, et al. Bridging the gap between basic and clinical sciences: a description of a radiological anatomy course. Anat Sci Educ [Internet]. United States; 2016;9:295–303. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med13&NEWS=N&AN=26599321. [DOI] [PubMed]
- 34.Jamniczky HA, Cotton D, Paget M, Ramji Q, Lenz R, McLaughlin K, et al. Cognitive load imposed by ultrasound-facilitated teaching does not adversely affect gross anatomy learning outcomes. Anat Sci Educ [Internet]. United States; 2017;10:144–51. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med14&NEWS=N&AN=27533319. [DOI] [PubMed]
- 35.Ivanusic J, Cowie B, Barrington M. Undergraduate student perceptions of the use of ultrasonography in the study of “living anatomy”. Anat Sci Educ [Internet]. United States; 2010;3:318–22. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med8&NEWS=N&AN=20872744. [DOI] [PubMed]
- 36.Bell FE, Neuffer FH, Haddad R, Epps JC, Kozik ME, Warren BC. Active learning of the floor of mouth anatomy with ultrasound. Anat Sci Educ [Internet]. United States; 2019;12:310–6. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med16&NEWS=N&AN=30414266. [DOI] [PubMed]
- 37.Ireson M, Warring S, Medina-Inojosa JR, O’malley MT, Pawlina W, Lachman N, et al. First year medical students, personal handheld ultrasound devices, and introduction of insonation in medical education. Ann Glob Heal. 2019;85. [DOI] [PMC free article] [PubMed]
- 38.Kleiman AM, Potter JF, Bechtel AJ, Forkin KT, Dunn LK, Collins SR, et al. Generative retrieval results in positive academic emotions and long-term retention of cardiovascular anatomy using transthoracic echocardiography and long-term retention of cardiovascular anatomy. Adv Physiol Educ [Internet]. United States; 2019;43:47–54. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med16&NEWS=N&AN=30615478. [DOI] [PubMed]
- 39.Liu RB, Suwondo DN, Donroe JH, Encandela JA, Weisenthal KS, Moore CL. Point-of-care ultrasound: does it affect scores on standardized assessment tests used within the preclinical curriculum?. J Ultrasound Med [Internet]. England; 2019;38:433–40. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med16&NEWS=N&AN=30058124. [DOI] [PubMed]
- 40.Patten D. Using ultrasound to teach anatomy in the undergraduate medical curriculum: an evaluation of the experiences of tutors and medical students. Ultrasound. 2015;23:18–28. doi: 10.1177/1742271X14542173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sweetman GM, Crawford G, Hird K, Fear MW. The benefits and limitations of using ultrasonography to supplement anatomical understanding. Anat Sci Educ [Internet]. United States; 2013;6:141–8. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med10&NEWS=N&AN=23109325. [DOI] [PubMed]
- 42.Moscova M, Bryce DADA, Sindhusake D, Young N. Integration of medical imaging including ultrasound into a new clinical anatomy curriculum. Anat Sci Educ [Internet]. United States; 2015;8:205–20. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med12&NEWS=N&AN=25132661. [DOI] [PubMed]
- 43.Arya R, Morrison T, Zumwalt A, Shaffer K. Making education effective and fun: stations-based approach to teaching radiology and anatomy to third-year medical students. Acad Radiol [Internet]. United States; 2013;20:1311–8. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med10&NEWS=N&AN=24029065. [DOI] [PubMed]
- 44.Wilson SP, Mefford JM, Lahham S, Lotfipour S, Subeh M, Maldonado G, et al. Implementation of a 4-year point-of-care ultrasound curriculum in a liaison committee on medical education-accredited US medical school. J Ultrasound Med [Internet]. England; 2017;36:321–5. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med14&NEWS=N&AN=27943456. [DOI] [PubMed]
- 45.Griksaitis MJ, Sawdon MA, Finn GM. Ultrasound and cadaveric prosections as methods for teaching cardiac anatomy: a comparative study. Anat Sci Educ [Internet]. United States; 2011;5:20–6. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med9&NEWS=N&AN=22069248. [DOI] [PubMed]
- 46.Finn GM, Sawdon MA, Griksaitis MJ. The additive effect of teaching undergraduate cardiac anatomy using cadavers and ultrasound echocardiography. Eur J Anat. 2012;16:199–205. [Google Scholar]
- 47.Jurjus RA, Dimorier K, Brown K, Slaby F, Shokoohi H, Boniface K, et al. Can anatomists teach living anatomy using ultrasound as a teaching tool? Anat Sci Educ United States. 2014;7:340–349. doi: 10.1002/ase.1417. [DOI] [PubMed] [Google Scholar]
- 48.Knobe M, Carow JB, Ruesseler M, Leu BM, Simon M, Beckers SK, et al. Arthroscopy or ultrasound in undergraduate anatomy education: a randomized cross-over controlled trial. BMC Med Educ. 2012;12. [DOI] [PMC free article] [PubMed]
- 49.Smith JP, Kendall JL, Royer DF. Improved medical student perception of ultrasound using a paired anatomy teaching assistant and clinician teaching model. Anat Sci Educ [Internet]. United States; 2018;11:175–84. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med15&NEWS=N&AN=28817242. [DOI] [PubMed]
- 50.Gradl-Dietsch G, Korden T, Modabber A, Sönmez TT, Stromps J-P, Ganse B, et al. Multidimensional approach to teaching anatomy—do gender and learning style matter? Ann Anat. 2016;208:158–164. doi: 10.1016/j.aanat.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 51.Swamy M, Searle RF. Anatomy teaching with portable ultrasound to medical students. BMC Med Educ [Internet]. England; 2012;12:99. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med9&NEWS=N&AN=23088725. [DOI] [PMC free article] [PubMed]
- 52.McCrorie P. The place of the basic sciences in medical curricula. Med Educ. 2000;34:594–595. doi: 10.1046/j.1365-2923.2000.00737.x. [DOI] [PubMed] [Google Scholar]
- 53.McLachlan JC, Patten D. Anatomy teaching: ghosts of the past, present and future. Med Educ [Internet]. John Wiley & Sons, Ltd; 2006;40:243–53. Available from: 10.1111/j.1365-2929.2006.02401.x. [DOI] [PubMed]
- 54.Finn GM, Patten D, McLachlan J. The impact of wearing scrubs on contextual learning in undergraduate medical students. Med Teach. 2010;32:381–384. doi: 10.3109/01421590903437196. [DOI] [PubMed] [Google Scholar]
- 55.Knobe M, Carow JBJB, Ruesseler M, Leu BMBM, Simon M, Beckers SKSK, et al. Arthroscopy or ultrasound in undergraduate anatomy education: a randomized cross-over controlled trial. BMC Med Educ [Internet]. England; 2012;12:85. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med9&NEWS=N&AN=22958784. [DOI] [PMC free article] [PubMed]
- 56.Kondrashov P, Johnson JCJC, Boehm K, Rice D, Kondrashova T. Impact of the clinical ultrasound elective course on retention of anatomical knowledge by second-year medical students in preparation for board exams. Clin Anat [Internet]. United States; 2015;28:156–63. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med12&NEWS=N&AN=25534185. [DOI] [PubMed]
- 57.Allsop S, Gandhi S, Ridley N, Spear M. Implementing ultrasound sessions to highlight living anatomy for large medical student cohorts. Transl Res Anat. 2021;22:100088. doi: 10.1016/j.tria.2020.100088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Busari JO. The discourse of generational segmentation and the implications for postgraduate medical education. Perspect Med Educ [Internet]. Bohn Stafleu van Loghum; 2013;2:340–8. Available from: https://pubmed.ncbi.nlm.nih.gov/23670694. [DOI] [PMC free article] [PubMed]
- 59.Fakoya FA. Integrating ultrasound technology into teaching gross anatomy: point of order! Med Educ Online. 2013;18:20888. doi: 10.3402/meo.v18i0.20888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boysen PG, Daste L, Northern T. Multigenerational challenges and the future of graduate medical education. Ochsner J [Internet]. the Academic Division of Ochsner Clinic Foundation; 2016;16:101–7. Available from: https://pubmed.ncbi.nlm.nih.gov/27046415. [PMC free article] [PubMed]
- 61.Knudsen L, Nawrotzki R, Schmiedl A, Mühlfeld C, Kruschinski C, Ochs M, et al. Hands-on or no hands-on training in ultrasound imaging: a randomized trial to evaluate learning outcomes and speed of recall of topographic anatomy. Anat Sci Educ [Internet]. United States; 2018;11:575–91. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med15&NEWS=N&AN=29683560. [DOI] [PubMed]
- 62.Sibbald M, Sherbino J, Preyra I, Coffin-Simpson T, Norman G, Monteiro S. Eyeballing: the use of visual appearance to diagnose ‘sick.’ Med Educ [Internet]. John Wiley & Sons, Ltd; 2017;51:1138–45. Available from: 10.1111/medu.13396. [DOI] [PubMed]
- 63.Coderre S, Mandin H, Harasym PH, Fick GH. Diagnostic reasoning strategies and diagnostic success. Med Educ [Internet]. John Wiley & Sons, Ltd; 2003;37:695–703. Available from: 10.1046/j.1365-2923.2003.01577.x. [DOI] [PubMed]
- 64.Lambe KA, O’Reilly G, Kelly BD, Curristan S. Dual-process cognitive interventions to enhance diagnostic reasoning: a systematic review. BMJ Qual Saf [Internet]. 2016;25:808–20. Available from: http://qualitysafety.bmj.com/content/25/10/808.abstract. [DOI] [PubMed]
- 65.Koury HF, Leonard CJ, Carry PM, Lee LMJ. An expert derived feedforward histology module improves pattern recognition efficiency in novice students. Anat Sci Educ [Internet]. John Wiley & Sons, Ltd; 2019;12:645–54. Available from: 10.1002/ase.1854. [DOI] [PubMed]
- 66.Ofei-Dodoo S, Goerl K, Moser S. Exploring the impact of group size on medical students’ perception of learning and professional development during clinical rotations. Kansas J Med [Internet]. University of Kansas Medical Center; 2018;11:70–5. Available from: https://pubmed.ncbi.nlm.nih.gov/30206466. [PMC free article] [PubMed]
- 67.Waterston SW, Stewart IJ. Survey of clinicians’ attitudes to the anatomical teaching and knowledge of medical students. Clin Anat. 2005;18:380–384. doi: 10.1002/ca.20101. [DOI] [PubMed] [Google Scholar]
- 68.Zumwalt AC, Lufler RS, Monteiro J, Shaffer K, Luefler RS, Monteiro J, et al. Building the body: active learning laboratories that emphasize practical aspects of anatomy and integration with radiology. Anat Sci Educ. 2010;3:134–140. doi: 10.1002/ase.153. [DOI] [PubMed] [Google Scholar]
- 69.Dreher SM, Dephilip R, Bahner D. Ultrasound exposure during gross anatomy. J Emerg Med [Internet]. United States; 2014;46:231–40. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med11&NEWS=N&AN=24113480. [DOI] [PubMed]
- 70.Knobe M, Sellei R, Maus U, Mooij S, Gradl-Dietsch G, Sopka S, et al. Undergraduate curricular training in musculoskeletal ultrasound: the impact of preexisting anatomic knowledge. Z Orthop Unfall. 2010;148:685–690. doi: 10.1055/s-0030-1250378. [DOI] [PubMed] [Google Scholar]
- 71.Peters M. Does constructivist epistemology have a place in nurse education? J Nurs Educ. 2000;39:166–172. doi: 10.3928/0148-4834-20000401-07. [DOI] [PubMed] [Google Scholar]
- 72.Dahmen U, Schulze C, Schindler C, Wick K, Schwartze D, Veit A, et al. Recommendations to enhance constructivist-based learning in interprofessional education using video-based self-assessment. GMS J Med Educ [Internet]. German Medical Science GMS Publishing House; 2016;33:Doc33–Doc33. Available from: https://pubmed.ncbi.nlm.nih.gov/27280144. [DOI] [PMC free article] [PubMed]
- 73.Naeger DM, Conrad M, Nguyen J, Kohi MP, Webb EM. Students teaching students: evaluation of a “near-peer” teaching experience. Acad Radiol [Internet]. United States; 2013;20:1177–82. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med10&NEWS=N&AN=23810649. [DOI] [PubMed]
- 74.Carter JL, Hocum G, Pellicer R, Patel A, Benninger B. Integration of 3D/4D ultrasound in teaching medical anatomy. Med Sci Educ. 2016;26:343–348. doi: 10.1007/s40670-016-0271-6. [DOI] [Google Scholar]
- 75.Smith JP, Kendall JL, Royer DF. Improved medical student perception of ultrasound using a paired anatomy teaching assistant and clinician teaching model. Anat Sci Educ [Internet]. United States; 2017;11:175–84. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med15&NEWS=N&AN=28817242. [DOI] [PubMed]
- 76.Andrew Jay E, Starkman SJ, Pawlina W, Lachman N. Developing medical students as teachers: an anatomy-based student-as-teacher program with emphasis on core teaching competencies. Anat Sci Educ [Internet]. John Wiley & Sons, Ltd; 2013;6:385–92. Available from: 10.1002/ase.1364. [DOI] [PubMed]
- 77.Gregory A, Walker I, McLaughlin K, Peets A. Both preparing to teach and teaching positively impact learning outcomes for peer teachers. Med Teach. 2011;33:e417–e422. doi: 10.3109/0142159X.2011.586747. [DOI] [PubMed] [Google Scholar]
- 78.Sobral DT. Cross-year peer tutoring experience in a medical school: conditions and outcomes for student tutors. Med Educ [Internet]. John Wiley & Sons, Ltd; 2002;36:1064–70. Available from: 10.1046/j.1365-2923.2002.01308.x. [DOI] [PubMed]
- 79.Colaco SM, Chou CL, Hauer KE. Near-peer teaching in a formative clinical skills examination. Med Educ [Internet]. John Wiley & Sons, Ltd; 2006;40:1129–30. Available from: 10.1111/j.1365-2929.2006.02593.x. [DOI] [PubMed]
- 80.Peets AD, Coderre S, Wright B, Jenkins D, Burak K, Leskosky S, et al. Involvement in teaching improves learning in medical students: a randomized cross-over study. BMC Med Educ [Internet]. BioMed Central; 2009;9:55. Available from: https://pubmed.ncbi.nlm.nih.gov/19706190. [DOI] [PMC free article] [PubMed]
- 81.Yu T-C, Wilson NC, Singh PP, Lemanu DP, Hawken SJ, Hill AG. Medical students-as-teachers: a systematic review of peer-assisted teaching during medical school. Adv Med Educ Pract [Internet]. Dove Medical Press; 2011;2:157–72. Available from: https://pubmed.ncbi.nlm.nih.gov/23745087. [DOI] [PMC free article] [PubMed]
- 82.Jackson TA, Evans DJR. Can medical students teach? A near-peer-led teaching program for year 1 students. Adv Physiol Educ [Internet]. American Physiological Society; 2012;36:192–6. Available from: 10.1152/advan.00035.2012. [DOI] [PubMed]
- 83.Nelson AJ, Nelson S V, Linn AMJ, Raw LE, Kildea HB, Tonkin AL. Tomorrow’s educators … today? Implementing near-peer teaching for medical students. Med Teach [Internet]. Taylor & Francis; 2013;35:156–9. Available from: 10.3109/0142159X.2012.737961. [DOI] [PubMed]
- 84.Hoppmann RA, Rao V V, Poston MB, Howe DB, Hunt PS, Fowler SD, et al. An integrated ultrasound curriculum (iUSC) for medical students: 4-year experience. Crit Ultrasound J [Internet]. 2011/02/01. Springer Milan; 2011;3:1–12. Available from: https://pubmed.ncbi.nlm.nih.gov/21516137. [DOI] [PMC free article] [PubMed]
- 85.Rao S, Van Holsbeeck L, Musial JLJL, Parker A, Bouffard JAA, Bridge P, et al. A pilot study of comprehensive ultrasound education at the Wayne State University School of Medicine: a pioneer year review. J Ultrasound Med [Internet]. England; 2008;27:745–9. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med7&NEWS=N&AN=18424650. [DOI] [PubMed]
- 86.Brown B, Adhikari S, Marx J, Lander L, Todd GLGL. Introduction of ultrasound into gross anatomy curriculum: perceptions of medical students. J Emerg Med [Internet]. United States; 2012;43:1098–102. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med9&NEWS=N&AN=22459597. [DOI] [PubMed]
- 87.Wittich CM, Montgomery SC, Neben MA, Palmer BA, Callahan MJ, Seward JB, et al. Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device. J Am Med Assoc. 2002;288:1062–1063. doi: 10.1001/jama.288.9.1062. [DOI] [PubMed] [Google Scholar]
- 88.Rempell JS, Saldana F, DiSalvo D, Kumar N, Stone MBMB, Chan W, et al. Pilot point-of-care ultrasound curriculum at Harvard Medical School: early experience. West J Emerg Med [Internet]. United States; 2016;17:734–40. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med13&NEWS=N&AN=27833681. [DOI] [PMC free article] [PubMed]
- 89.George C. Should all medical students be graduates first? NO. Br Med J [Internet]. 2007;335:1073. Available from: http://www.bmj.com/content/335/7629/1073.abstract. [DOI] [PMC free article] [PubMed]
- 90.Peile E. Should all medical students be graduates first? Yes. Br Med J [Internet]. BMJ Publishing Group Ltd.; 2007;335:1072. Available from: https://pubmed.ncbi.nlm.nih.gov/18033927. [DOI] [PMC free article] [PubMed]
- 91.DeZee KJ, Artino AR, Elnicki DM, Hemmer PA, Durning SJ. Medical education in the United States of America. Med Teach [Internet]. Taylor & Francis; 2012;34:521–5. Available from: 10.3109/0142159X.2012.668248. [DOI] [PubMed]
- 92.Walters P. Qualitative archiving: engaging with epistemological misgivings. Aust J Soc Issues. Wiley Online Library; 2009;44:309–20.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.