Abstract
Objective
To investigate the use and trends of virtual care in ophthalmology and examine associated factors in a universal health care system during the COVID-19 pandemic in 2020.
Design
Cross-sectional study.
Participants
Ontarians eligible for the Ontario Health Insurance Plan.
Methods
We used physician billing data from 2017–2020 to describe the use of virtual versus in-person care. We used logistic regression to examine factors associated with virtual care use.
Results
The uptake of ophthalmic virtual visits increased immediately following the government's directive to ramp down clinic activities and institution of a new virtual fee code (17.6%), peaked 2 weeks later (55.8%), and decreased immediately after the directive was lifted (24.2%). In March–December 2020, virtual visits were higher in female (11.6%) versus male (10.3%) patients and in patients <20 years of age (16.4%) and 20–39 years of age (12.3%) versus those aged 40–64 years (10.8%) and 65+ years (10.6%). Patients residing in the poorest/poorer neighbourhoods (10.9%) had similar use as their counterparts (11.1%). Patients with an acute infectious disease (14.2%) or nonurgent diagnosis (16.2%) had the highest use. Those with retinal disease had the lowest use (4.2%). Female ophthalmologists (15.4%) provided virtual care more often than male ophthalmologists (9.9%). Ophthalmologists aged 60–69 years (13.1%) provided virtual care more often than any other age groups (<40 years: 11.3%; 40–49 years: 11.0%; 50–59 years: 10.0%; and 70+ years: 7.7%). Multiple logistic regression models revealed similar results.
Conclusion
Virtual care in ophthalmology increased significantly during the initial phase of the pandemic and decreased thereafter. There were significant variations in virtual care use by patient and ophthalmologist characteristics.
To limit the spread of the COVID-19 and maintain patient care, virtual visits were encouraged in many jurisdictions. Consequently, rapid adoption of digital tools and technologies for health care delivery has grown exponentially worldwide during the pandemic.1 , 2 Several terms such as telehealth and telemedicine were used in the literature to name medical services provided through digital tools and technologies. In this study, we used virtual care to refer to “any interaction between patients and/or members of their circle of care, occurring remotely, using any forms of communication or information technologies, with the aim of facilitating or maximizing the quality and effectiveness of patient care,” as defined in the Virtual Health Symposium.3
A recent U.S. study showed striking variation among medical specialties in the use of virtual care, with the lowest use in ophthalmology.4 In ophthalmology, information is limited regarding which patients and ophthalmologists adopted virtual care more often and if the initial surge in virtual care services was sustained during the pandemic period. In the United States, a report suggested that during the pandemic marginalized populations were less likely to receive ophthalmic virtual care.5 Socioeconomic disparities in eye care thus were widened during the pandemic.5 It is unknown whether this reported disparity holds true in Canada with a universal publicly funded health system.
Using population-based health administrative data, we describe the use and trends of virtual care in ophthalmology and examine factors associated with the use of ophthalmic virtual care in Ontario during the COVID-19 pandemic in 2020.
Materials and Methods
In Canada, medically necessary services are universally covered for all residents by publicly funded health insurance administered at the provincial level. In Ontario, the largest province in Canada by population (>14.7 million in 2020),6 ophthalmologists submit claims to the Ontario Health Insurance Plan (OHIP) for payment of insured services, including in-person and virtual visits.
Data sources
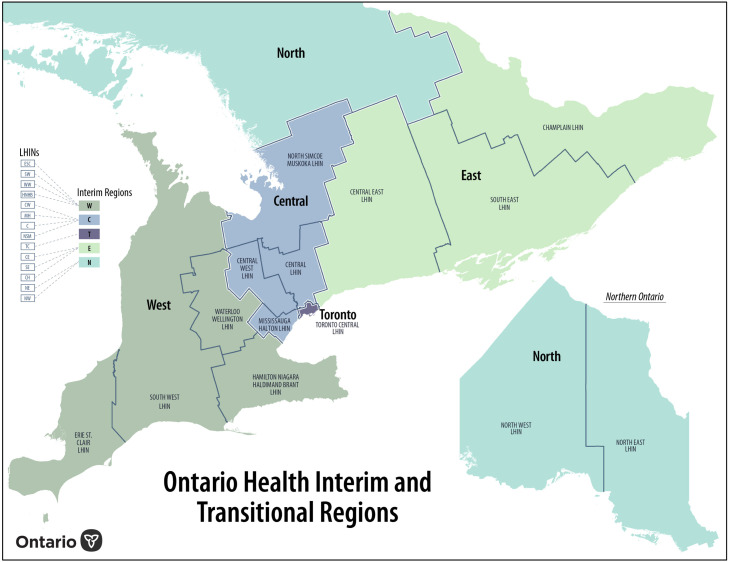
Study data were obtained from 3 population-based databases housed at ICES from 2017 to 2020: OHIP physician billing database, ICES Physician Database and Registered Persons Database.7 The OHIP database provided patient–physician encounter information (e.g., date of visit, diagnosis, fee/service code). The ICES Physician Database furnished physician-related information (e.g., physician sex, age, and specialty). The Registered Persons Database contained demographic information (e.g., age, sex, and neighbourhood income quintiles) for OHIP-insured Ontarians. There were 5 health regions (Toronto, Central, North, West, and East) in Ontario in 20208 (Fig. 1 ). Database linkages were done using encrypted unique health card numbers in a protected environment by ICES analysts. Aggregated data were provided for analyses. This study was approved by the Research Ethics Board at the University of Toronto.
Fig. 1.
Five health regions in Ontario in 2020.
Virtual visits and ophthalmologists
Prior to the COVID-19 pandemic, physician services provided electronically were coded with a “U” prefix,9 which had rules and restrictions regulating when they could be used.9 In response to the COVID-19 pandemic, on March 14, 2020, the Ontario Ministry of Health introduced new temporary billing codes for physician encounters with insured persons by telephone or video.10 Specifically, the fee code “K083” was used by ophthalmologists to claim services provided by telephone or video.10 The new “K” code had few restrictions on use. The payment claimed for virtual services is determined by the number of units. To determine the number of units, the in-person fee listed in the Schedule of Benefits for Physician Services for the service provided is rounded to the nearest $5 and then divided by 5.10 For example, a partial assessment (A234) with a listed fee of $28.95 in the Schedule of Benefits for Physician Services would be 6 units ($28.95 rounded to the nearest $5, i.e., $30, divided by 5 represents 6 units) for virtual services.10 , 11 Similarly, a specific assessment (A233) with a listed fee of $57.70 would be 12 units, and a consult (A235 or A253) with a fee of $82.20 would be 16 units.11 An ophthalmic virtual visit should never be billed for less than 6 units and is very unlikely to qualify for more than 16 units. Ophthalmologists were identified from specialty code.
Ophthalmology diagnostic groups
We grouped ophthalmic diseases into 8 categories: acute infectious disease (e.g., conjunctivitis), urgent eye condition (e.g., superficial injury of eye), cataract, glaucoma, diabetes, retinal disease, nonurgent eye conditions (e.g., amblyopia), and other unspecified eye conditions (i.e., diseases not included in any of the preceding groups). Details of the classification are presented in Appendix A (available online). Surgeries cannot be done virtually, so these services were excluded.
Statistical analysis
Descriptive data on the number and percentage of virtual encounters at the population level in Ontario were calculated yearly from 2017 to 2020. The percentage of virtual encounters was computed as the number of virtual visits (numerator) divided by the total number of virtual and in-person visits (denominator). To better understand the trend in use of virtual care during the 2020 pandemic period, we calculated the weekly use of virtual care, with week 1 defined as the week starting on March 16, 2020. We considered the use of virtual care from March 16, 2020, to December 31, 2020, as the study event, and patient characteristics (i.e., age, sex, neighbourhood income quintile, health region of residence) and ophthalmologist characteristics (i.e., age and sex) as the independent factors. These 6 variables were put into a logistic regression model to assess patients’ and ophthalmologists’ factors associated with virtual versus in-person visits and adjust for the confounding effects of covariates. Except for the independent variable in question (e.g., patient sex), all other 5 variables in the model served as covariates. These 6 variables were chosen because they were available in ICES databases, they were potential confounding factors and not in the causal pathway to virtual care, and their associated frequency data met ICES data-release rules.12, 13, 14 Results of these models are presented as adjusted odds ratios (aORs) with 95% CIs.
Results
The total number of ophthalmology assessments or consults (i.e., including in-person and virtual visits) was 2.51 million in 2017, 2.54 million in 2018, 2.53 million in 2019, and 2.02 million in 2020 (20% reduction compared with 2019). Considering virtual visits only, there were 1733 in 2017, 2007 in 2018, 2610 in 2019, and 167,633 in 2020. The percentage of virtual care use was 0.07% in 2017, 0.08% in 2018, 0.10% in 2019, and 8.31% in 2020.
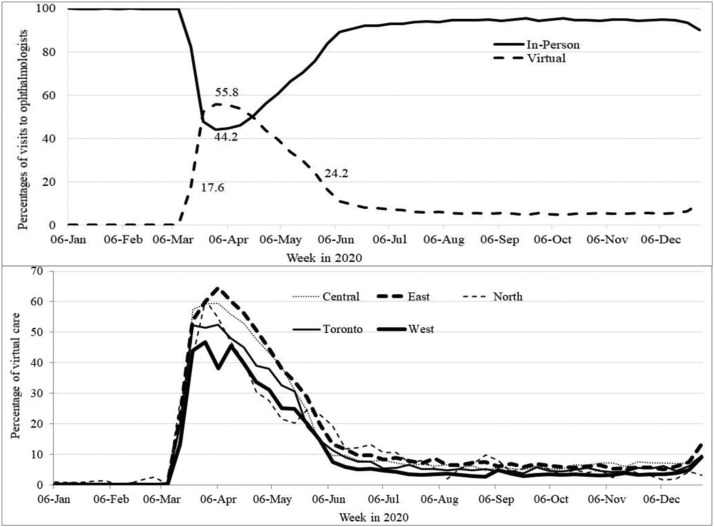
In 2020, the weekly uptake of virtual visits increased immediately during the week of the Ontario government's directive to ramp down clinic activities and institution of a new virtual fee code (17.6%, week of March 16, 2020),15 peaked 2 weeks later (55.8%, week of March 30, 2020), and decreased immediately after the directive was lifted (24.2%, week of May 25, 2020)16 (Fig. 2 A). The use of virtual care was further reduced to 8%–16% in June 2020 and to 5%–10% in July–December 2020. By health region, the level of virtual care use was lowest in the West region versus any other region during the entire study period (Fig. 2B).
Fig. 2.
Weekly use (%) of virtual and in-person visits to ophthalmologists in 2020 in Ontario (A) and weekly use of virtual visits to ophthalmologists by health regions in 2020 in Ontario (B).
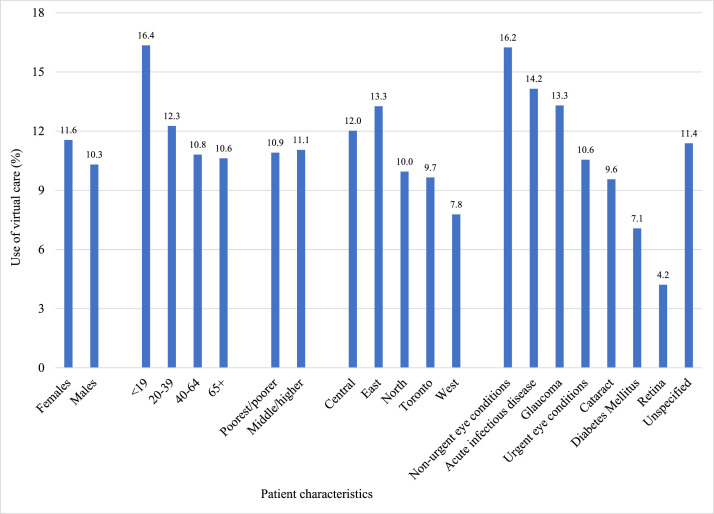
Figure 3 shows that during the 2020 pandemic period (March 16–December 31, 2020), higher uptake of virtual care was seen in female versus male patients and in patients <20 and 20–39 years of age versus those aged 40–64 and 65+ years. Patients residing in the poorest/poorer neighbourhoods used virtual care similarly to their counterparts (10.9% vs 11.1%). Patients with nonurgent eye diagnoses (16.2%), acute infectious disease (14.2%), or glaucoma (13.3%) had the highest use of virtual care. Those with a retinal disease diagnosis (4.2%) used virtual care the lowest.
Fig. 3.
Use (%) of virtual care during the pandemic period in 2020 (March 16–December 31) by patient characteristics in Ontario.
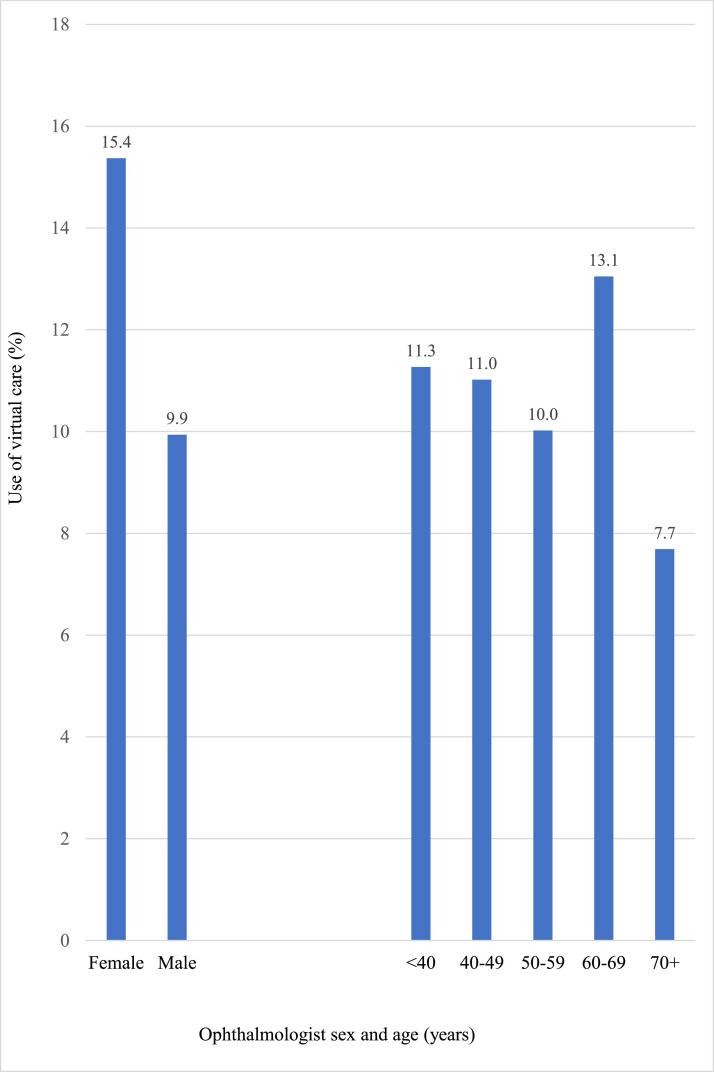
Figure 4 shows that female ophthalmologists were 1.6 times more likely to provide virtual care than male ophthalmologists, and ophthalmologists aged 60–69 years were more likely to provide virtual care than those in any other age group.
Fig. 4.
Use (%) of virtual care during the pandemic period in 2020 (March 16–December 31) by ophthalmologist characteristics in Ontario.
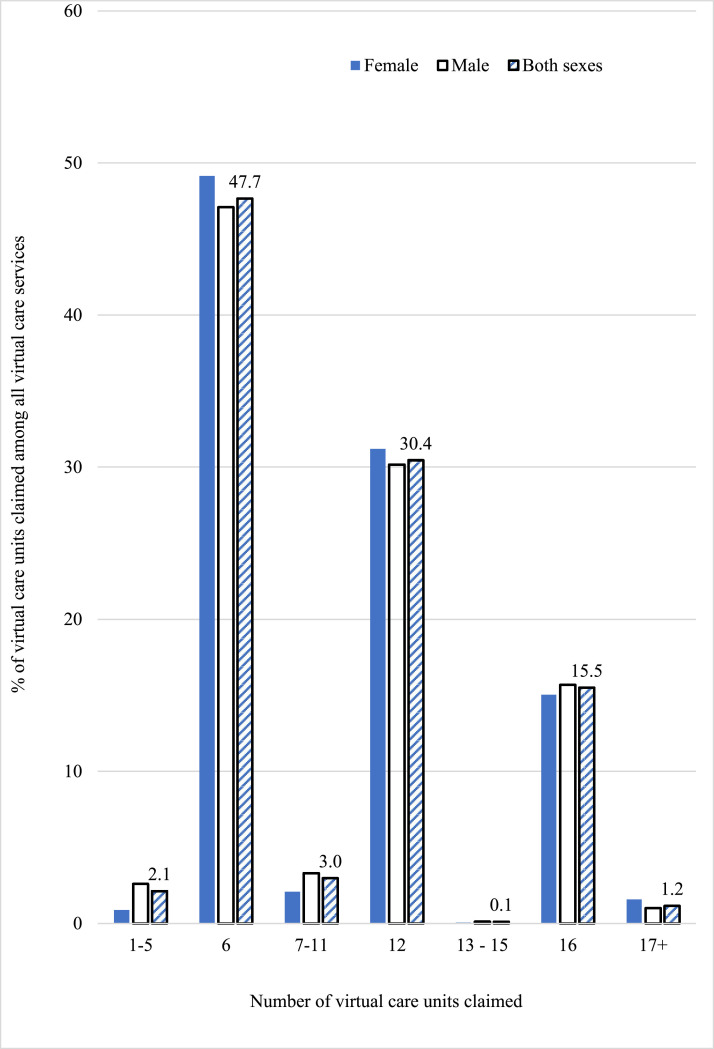
Figure 5 shows the percentage of virtual care units claimed among all virtual care services stratified by ophthalmologist sex. For both sexes, about half (48%) of virtual services were billed as 6 units (partial assessment); an additional 30% and 16% were billed as 12 units (specific assessment) and 16 units (consult), respectively. In addition, about 2% of virtual care services were billed for 1–5 units and 1% for 17+ units (with the maximum number of units for one visit being 80).
Fig. 5.
Percentage of virtual care units claimed among all virtual services stratified by ophthalmologist sex during the pandemic period in 2020 (March 16–December 31) in Ontario. The number of virtual care units is calculated by rounding the in-person billing fee listed in the Schedule of Benefits for Physician Services for the service provided to the nearest $5 and then divided by 5.10,11 See a calculation example under Materials and Methods, Virtual visits and ophthalmologists.
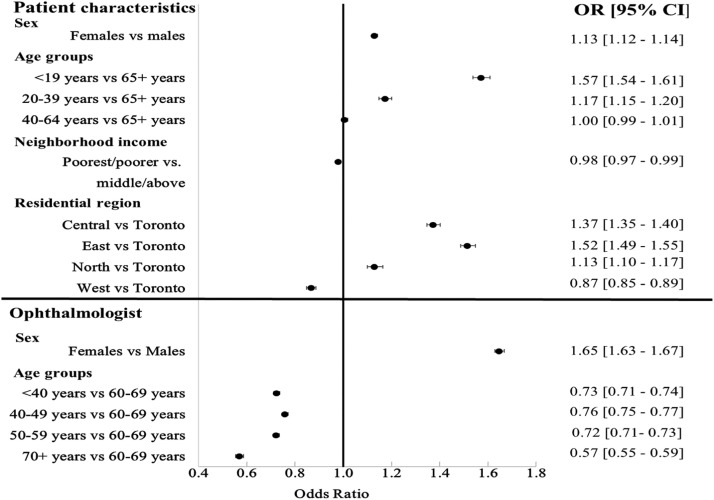
Results of logistic regression analyses are shown in Figure 6 . Significantly higher odds of virtual care use were found in female (aOR = 1.13) versus male patients, in patients <20 years of age (aOR = 1.57), and 20–39 years of age (aOR = 1.17) versus 65+ years of age; in patients residing in the Central (aOR = 1.37), East (aOR = 1.52), and North (aOR = 1.13) regions versus those in the Toronto region, and in female (aOR = 1.65) versus male ophthalmologists. Compared with ophthalmologists aged 60–69 years, those in other age groups were less likely to use virtual care.
Fig. 6.
Adjusted odds ratio (aOR) and 95% CI of virtual care utilization derived from logistic regression models during the pandemic period in 2020 (March 16–December 31) in Ontario. Variables included in the model were patient age group, sex, neighbourhood income area, residential health region, and ophthalmologist age group and sex.
Discussion
To mitigate the disruption of health care services from the COVID-19 pandemic and to protect both patients and health care providers, virtual care seems an ideal option. Using physician billing data from a single government payer, this study reports that the use of virtual care by ophthalmologists in Ontario had an 80-fold increase in the pandemic year 2020, from 0.07%–0.10% before COVID-19 to 8.31% in 2020. The increased use of virtual care in 2020 fluctuated closely with the government's directive on health care service delivery and institution of a new virtual care billing code. After the first wave of the pandemic, virtual care represented 5%–10% of visits, much higher than the prepandemic level (0.07%–0.10%). Users of ophthalmic virtual care were more likely to be female patients, patients younger than 40 years of age, patients with an acute infectious disease or nonurgent diagnosis, patients residing in a health region other than the West, female ophthalmologists, and ophthalmologists aged 60–69 years.
The increased use of virtual care during the pandemic may be attributed to multiple factors, including social distancing mandates, government's institution of a new virtual billing code, the availability and affordability of electronic devices such as widely available personal telephones and home computers, and patient convenience. Decreased use of ophthalmic virtual care following the lifting of the government's directive after the first pandemic wave suggests that ophthalmologic assessments require an examination of the visual system that in most cases cannot be done virtually. The need of specialized equipment and use of technology for the diagnosis and management of most ophthalmic conditions require an in-person assessment. Thus, if the option of in-person care is possible, both patients and ophthalmologists will choose in-person services. This explanation is consistent with the report that among various specialities, ophthalmology has the lowest number of telehealth users.4 , 17 The higher use of virtual care for patients with an acute eye infectious disease (e.g., conjunctivitis) and the lower use of virtual care for patients with retinal disease further support this explanation. Many acute eye infectious diseases are superficial and can be diagnosed without requiring specialized equipment or technology, whereas retinal disease usually requires an in-person examination in order to view the back of the eye, which cannot be done via virtual tools at the present time. Hopefully, more research efforts and technology development in the future will make virtual examinations of the visual system possible so that more ophthalmic patients can be benefit from virtual care.
In the United States, worsened disparity in access to virtual care during the pandemic was reported.5 , 18 This finding, however, was not evident in our study. Many factors, including the universal health care in Canada and the population-based nature of this study, may contribute to the different conclusions. However, in either privatized health care in the United States5 or universal health care in Canada, female eye patients used virtual care more often than male eye patients. Similarly, when looking at all patient visits, female ophthalmologists used virtual care more frequently than male ophthalmologists (15.4% vs 9.9%; Fig. 4). These findings are in agreement with a report that females have followed preventive practices of physical distancing, mask wearing, and maintaining hygiene to a greater degree than males.19 Young patients were more likely to use virtual care, which is expected because young people are reported to be more savvy with technology,20 a key requirement for virtual care. However, we found that young ophthalmologists used virtual care less often than ophthalmologists aged 60–69 years (Fig. 4). This unexpected result may demonstrate different concerns and priorities and adherence to preventive health practices by ophthalmologists of different ages. Further studies are needed to understand the reasons why young ophthalmologists used less virtual care.
Major limitations of this study include that billing codes do not distinguish between video- and telephone-based services. In the United States, 92% of the ophthalmic virtual services are video based.5 We do not know if this is true in Ontario. Second, information is not available regarding patient ethnicity, levels of education and income, and spoken language; these are factors frequently discussed in the U.S. studies. However, the available information on neighbourhood income level in this study may have taken into account the effects of education and income on the use of virtual care, which reveal a different conclusion from the U.S. reports.5 , 18 Third, studies are needed to understand outcomes of virtual versus in-person care and patients’ and physicians’ views and perceptions of the benefits and challenges of delivering care virtually. Fourth, the new virtual billing code introduced during the pandemic, which has fewer restrictions than the virtual billing codes pre-COVID-19, limits comparisons of virtual care use in 2020 versus 2017–2019. However, the new virtual billing code has been available since the onset of the pandemic, making comparisons of virtual care use during the pandemic period valid. Fifth, our analysis included data up to December 2020 only. Repeated shutdowns and reopenings in Ontario because of the different waves of COVID-19 call for an analysis with updated data to see how ophthalmic virtual care evolved in the various waves of COVID-19. Lastly, Ontario's quick response to institute a new virtual billing code to cope with the COVID-19 pandemic was associated with some misunderstanding in how the new billing code should be used by physicians. We found both over- (units 17+) and underclaims (units 1–5) in the number of units for a single virtual encounter. These incorrect billings are harmful to both ophthalmologists (underpayment for units 1–5) and government (potential overpayment for units 17+). We communicated this billing issue to the Ministry of Health, which resulted in a bulletin to Ontario physicians further clarifying how the new virtual code should be billed.21 These incorrect billings, however, do not affect our results on the use of virtual care because the number of units billed affects the financial payment but not the number of virtual encounters.
In conclusion, the COVID-19 pandemic has expanded the use of virtual care in 2020 and onward. In response to the government's directive and institution of a new virtual billing code, the use of virtual care in ophthalmology in Ontario increased significantly during the initial phase of the pandemic in 2020 and decreased immediately during the week the directive was lifted. This suggests that in-person care is preferred in ophthalmology. Both patients and ophthalmologists have subgroups associated with a higher level of virtual care use, reflecting different concerns and adherence to preventive health practices associated with the COVID-19 pandemic. Increased disparity in the use of virtual care observed in studies in the United States5 , 18 was not evident in this study based in Ontario.
Footnotes and Disclosure
The authors have no proprietary or commercial interest in any materials discussed in this article.
This work was supported by the Ontario Ministry of Health and Long-Term Care for the COVID-19 Challenge Questions Initiative and the Lindenfield Family Research Grant.
Acknowledgements
This study contracted Institute for Clinical Evaluative Sciences (ICES) Data & Analytic Services (DAS) and used deidentified data from the ICES Data Repository, which is managed by ICES with support from its funders and partners: Canada's Strategy for Patient-Oriented Research (SPOR), the Ontario SPOR Support Unit, the Canadian Institutes of Health Research, and the Government of Ontario. The opinions, results, and conclusions reported are those of the authors. No endorsement by ICES or any of its funders or partners is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of CIHI.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jcjo.2022.10.015.
Appendix. Supplementary materials
Online-only material: This article includes online-only material. Appendix A can be found on the CJO web site at http://pubs.nrc-cnrc.gc.ca/cjo/cjo.html. It is linked to this article in the online contents of the xxx 2022 issue.
References
- 1.Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193:E200–E210. doi: 10.1503/cmaj.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joshi AU, Lewiss RE. Telehealth in the time of COVID-19. Emerg Med J. 2020;37:637–638. doi: 10.1136/emermed-2020-209846. [DOI] [PubMed] [Google Scholar]
- 3.Women's College Hospital Institute for Health Systems Solutions and Virtual Care. Virtual Care: A Framework for a Patient-Centric System. Report, Women's College Hospital, Toronto, Canada, 2014.
- 4.Commonwealth Fund. The impact of the COVID-19 pandemic on outpatient care: visits return to prepandemic levels, but not for all providers and patients [Internet]. 2020. Available at:https://www.commonwealthfund.org/publications/2020/oct/impact-covid-19-pandemic-outpatient-care-visits-return-prepandemic-levels (accessed 3 Jan 2022).
- 5.Aziz K, Moon JY, Parikh R, et al. Association of patient characteristics with delivery of ophthalmic telemedicine during the COVID-19 pandemic. JAMA Ophthalmol. 2021;139:1174–1182. doi: 10.1001/jamaophthalmol.2021.3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Statistics Canada. Table 17-10-0005-01: Population estimates on July 1st, by age and sex [Internet]. 2020. Available at:https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501 (accessed 18 Nov 2021).
- 7.Institute for Clinical Evaluative Sciences. Data dictionary [Internet]. 2021. Avaialble at: https://datadictionary.ices.on.ca/Applications/DataDictionary/Default.aspx (accessed 18 Jan 2022).
- 8.Dapasoft. 14 LHINs reorganized into 5 transitional regions in Ontario [Internet]. 2020. Available at: https://www.dapasoft.com/14-lhins-reorganized-ontario/ (accessed 6 Aug 2021).
- 9.Minstry of Health and Long-Term Care in Ontario. Schedule of benefits [Internet]. 2021. Available at:https://www.health.gov.on.ca/en/pro/programs/ohip/sob/physserv/sob_master08052015.pdf (accessed 10 Dec 2021).
- 10.Ministry of Health and Long-Term Care in Ontario. Changes to the schedule of benefits for physician services (schedule) in response to COVID-19 influenza pandemic effective March 14, 2020 [Internet]. 2020. Available at:https://www.health.gov.on.ca/en/pro/programs/ohip/bulletins/4000/bul4745.pdf (accessed 19 Jan 2022).
- 11.Ministry of Health and Long-Term Care in Ontario. Schedule of benefits: physician services under the Health Insurance Act (July 2, 2021 (Effective October 1, 2021)). 2021. Available at: https://www.health.gov.on.ca/en/pro/programs/ohip/sob/physserv/sob_master.pdf (accessed 19 Jan 2022).
- 12.Sauer BC, Brookhart MA, Roy J, VanderWeele T. A review of covariate selection for non-experimental comparative effectiveness research. Pharmacoepidemiol Drug Saf. 2013;22:1139–1145. doi: 10.1002/pds.3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braga LHP, Farrokhyar F, Bhandari M. Practical tips for surgical research: confounding: what is it and how do we deal with it? Can J Surg. 2012;55:132–138. doi: 10.1503/cjs.036311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Szklo M, Nieto FJ. In: Epidemiology: Beyond the basics. 2nd ed. Szklo M, Nieto FJ, editors. Jones and Bartlett Publishers; Toronto: 2007. Identifying noncausal associations: confounding; pp. 151–179. [Google Scholar]
- 15.Ontario Ministry of Health Ramping down elective surgeries and other non-emergent activities [memorandum to Ontario Health and hospitals] Ministry of Health and Long-Term Care, Toronto [Internet] 2020 http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/memos/DM_OH_CMOH_memo_COVID19_elective_surgery_March_15_2020.pdf Mar 15. Available at. (accessed 6 Aug 2021) [Google Scholar]
- 16.Williams DC. COVID-19 directive #2 for health care providers (regulated health professionals or persons who operate a group practice of regulated health professionals), issued under Section 77.7 of the Health Protection and Promotion Act (HPPA), R.S.O. 1990, c. H.7. Ministry of Health and Long-Term Care, Toronto [Internet]. 2020. Available at:https://www.oha.com/Bulletins/CMOH%20Directive%202%20-%20Health%20Care%20Providers%20-%20April%2020%202021%20FINAL%20AODA.pdf (accessed 6 Aug 2021).
- 17.Aguwa UT, Aguwa CJ, Repka M, et al. Teleophthalmology in the era of COVID-19: characteristics of early adopters at a large academic institution. Telemed J E Health. 2021;27:739–746. doi: 10.1089/tmj.2020.0372. [DOI] [PubMed] [Google Scholar]
- 18.Zachrison KS, Yan Z, Sequist T, et al. Patient characteristics associated with the successful transition to virtual care: lessons learned from the first million patients. J Telemed Telecare. 2021 doi: 10.1177/1357633X211015547. 1357633X211015547. [DOI] [PubMed] [Google Scholar]
- 19.Okten IO, Gollwitzer A, Oettingen G. Gender differences in preventing the spread of coronavirus. Behav Sci Policy. 2020;6:109–122. [Google Scholar]
- 20.Shangraw RE, Whitten CW. Managing intergenerational differences in academic anesthesiology. Curr Opin Anaesthesiol. 2007;20:558–563. doi: 10.1097/ACO.0b013e3282f132e3. [DOI] [PubMed] [Google Scholar]
- 21.Ministry Health and Long-Term Care in Ontario. Keeping health care providers informed of payment, policy or program changes [Internet]. 2021. Available at:https://www.health.gov.on.ca/en/pro/programs/ohip/bulletins/4000/bul4764.aspx (accessed 24 Jan 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online-only material: This article includes online-only material. Appendix A can be found on the CJO web site at http://pubs.nrc-cnrc.gc.ca/cjo/cjo.html. It is linked to this article in the online contents of the xxx 2022 issue.