Abstract
Team-sports staff often administer non-exhaustive exercise assessments with a view to evaluating physiological state, to inform decision making on athlete management (e.g., future training or recovery). Submaximal fitness tests have become prominent in team-sports settings for observing responses to a standardized physical stimulus, likely because of their time-efficient nature, relative ease of administration, and physiological rationale. It is evident, however, that many variations of submaximal fitness test characteristics, response measures, and monitoring purposes exist. The aim of this scoping review is to provide a theoretical framework of submaximal fitness tests and a detailed summary of their use as proxy indicators of training effects in team sports. Using a review of the literature stemming from a systematic search strategy, we identified five distinct submaximal fitness test protocols characterized in their combinations of exercise regimen (continuous or intermittent) and the progression of exercise intensity (fixed, incremental, or variable). Heart rate-derived indices were the most studied outcome measures in submaximal fitness tests and included exercise (exercise heart rate) and recovery (heart rate recovery and vagal-related heart rate variability) responses. Despite the disparity between studies, these measures appear more relevant to detect positive chronic endurance-oriented training effects, whereas their role in detecting negative transient effects associated with variations in autonomic nervous system function is not yet clear. Subjective outcome measures such as ratings of perceived exertion were less common in team sports, but their potential utility when collected alongside objective measures (e.g., exercise heart rate) has been advocated. Mechanical outcome measures either included global positioning system-derived locomotor outputs such as distance covered, primarily during standardized training drills (e.g., small-sided games) to monitor exercise performance, or responses derived from inertial measurement units to make inferences about lower limb neuromuscular function. Whilst there is an emerging interest regarding the utility of these mechanical measures, their measurement properties and underpinning mechanisms are yet to be fully established. Here, we provide a deeper synthesis of the available literature, culminating with evidence-based practical recommendations and directions for future research.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40279-022-01712-0.
Key Points
| Submaximal fitness tests provide a practical tool for team-sport practitioners to evaluate an athlete’s physiological state in a short duration and non-exhaustive manner, whereby testing can be integrated within the training session. |
| We propose a theoretical framework for submaximal fitness tests in team sports, encompassing an operational definition, five test protocol categories according to their exercise regimen and intensity parameters, and an evidence-based synthesis of protocols and outcome measures derived from three main response types: cardiorespiratory/metabolic, subjective, and mechanical. |
| Heart rate indices are most prevalent in the literature (57% of all outcome measures) and appear sensitive to detect positive endurance-oriented training effects. However, their utility in inferring negative transient effects associated with variations in autonomic nervous system function is questionable in team sports. |
| At present, limited evidence exists regarding the utility of ratings of perceived exertion to monitor training effects within submaximal fitness tests in team sports. |
| Collecting outcome measures derived from inertial measurement units during submaximal fitness tests may be a promising approach to monitor transient changes in lower limb neuromuscular function. Further work to establish the underlying theoretical framework and measurement properties is warranted. |
Background
Monitoring the training process and its outcomes within team-based sports requires a systematic approach that: (1) is grounded on a rigorous conceptual framework; (2) can be implemented pragmatically on a frequent basis; (3) uses proxy outcome measures possessing sufficient measurement properties; and (4) is sensitive to identify acute (e.g., post-match) and chronic (e.g., post-training program) training effects [1–4]. Such an approach can be used to inform decision making around athlete and training management, including future programming, adjustments to training delivery, or the implementation of recovery interventions [1].
Assessing aerobic-oriented training effects has traditionally been made via distinct maximal-effort exhaustive tests. For example, improvements denoted in maximal intermittent field tests (e.g., 30–15 Intermittent Fitness Test) can infer improved aerobic capacity (amongst other systems), whereas decreased values may be interpreted as a negative response or de-training [5, 6]. However, given the nature of the in-season phase common to professional teams, which frequently experiences fixture congested periods, it is considered less feasible to expose athletes to serial exhaustive assessments [7, 8]. With regard to neuromuscular function, a variety of test protocols are administered to quantify chronic training effects on athletic qualities such as strength and power, but more frequently as indicators of acute and transient responses (e.g., post-match recovery kinetics) [7, 9]. Similarly, the practicability of such assessments in the team-sports environment is challenged by different factors such as the number of athletes, the time available for discreet testing protocols, and the numerous contextual and individual elements that may undermine inferences derived from the data (e.g., motivation, physical qualities, season stage) [1, 7, 8].
Submaximal fitness tests (SMFT) have been proposed to deliver a feasible alternative to evaluate an athlete’s physiological state, presumably because of their time-efficient nature, low physical/physiological burden, and relative ease of administration [10]. In essence, SMFT provide a pragmatic and systematic approach of observing response(s) to a standardized physical stimulus [11, 12]. Such assessments have been investigated since the late 1940s [13] and were mainly adopted among clinicians diagnosing health conditions or physical fitness in non-athletic populations, whereby exposure to maximal or exhaustive activities was thought to be ill-advisable because of the health risk it posed to patients [13, 14]. Over the years, a number of walking [15–19], cycling [14, 20–22], and running [23–25] SMFT have been administered among clinical and healthy populations. These tests involve single or multiple continuous steady-state protocols, with some prescribing an absolute standardized intensity, while others include relative intensity ranges, or self-paced protocols (refer to File 1 in the Electronic Supplementary Material [ESM]).
Elite Sports
The implementation of SMFT in elite sports has been traditionally used for quantifying relevant physiological transitions between exercise intensity domains (e.g., anaerobic threshold [i.e., the threshold indicates an equal rate of lactate production and disposal] and the onset of blood lactate accumulation [4-mmol·L−1 lactate threshold]) [26, 27], often administered to inform training prescription or determine exercise economy. However, these tests generally necessitate a laboratory environment, are resource intensive and obtrusive, and therefore considered less feasible in the day-to-day field context, particularly with large cohorts of athletes [7].
Individual endurance sport practitioners were the first to develop and implement SMFT as part of their training monitoring processes [28, 29]. Throughout the years, a broad range of cycling and running SMFT have been adopted across a variety of endurance sport athletes such as cyclists [28–32], runners [33–35], and triathletes [29, 36, 37]. Extensively used SMFT in endurance sports include exercise tasks prescribed by fixed internal intensities (% of an individual heart rate [HR] maximum) [32, 34], while the outcome measures are considered both external (e.g., speed [34], cadence, power [32] collected throughout the test) and internal responses (HR recovery [HRR] [38, 39], ratings of perceived exertion [RPE] [32] collected immediately post-exercise). Alternatively, researchers have adopted tests using standardized external intensities (usually via absolute running speed values) [33, 37]. Initially, the primary purpose of these SMFT was to predict performance (e.g., time trial) or physiological capacities (i.e., maximal oxygen uptake) [32]; however, more recently, they have been used to identify impaired performance (e.g., functional overreaching) [40, 41].
Because of the simplicity of implementing SMFT, their non-exhaustive nature, and their potential to provide information regarding both positive and negative training effects, SMFT have become common in team sports. Indeed, the adoption of SMFT in team-sports research [8, 10, 42] and practice [43, 44] has increased substantially over the last decade. However, given the broad range of SMFT adopted, including various protocols (continuous vs intermittent) [45, 46], activity modes (running vs cycling) [47, 48], intensities (fixed vs incremental, absolute vs individualized) [12, 48], outcome measures (cardiorespiratory/metabolic, subjective, or mechanical) [12, 49, 50], and purposes (monitoring positive vs negative effects) [47, 51], a synthesis appears warranted. Accordingly, the aims of this scoping review were to (1) develop an operational definition of SMFT and protocol taxonomy, (2) identify previously used SMFT in the team-sports research and discuss their conceptual and methodical aspects, (3) provide an audit of outcome measures, collection methods, and analytical processes, as well as evaluate the theoretical rationale underpinning their inclusion, (4) provide a narrative synthesis of the available research on SMFT as indicators of training effects in team sports, and (5) conclude with practical recommendations and future directions.
Methods
Systematic searches of the electronic databases MEDLINE, Scopus, and Web of Science were used to identify relevant studies. From 2170 records identified in the original searches, we accepted 87 team-sport studies meeting our inclusion criteria. A detailed description of the searching strategy, screening process, and the inclusion–exclusion criteria are provided in File 2 in the ESM.
Results
Submaximal Fitness Test Definition
A table presenting the characteristics of the included studies is provided in File 3 in the ESM. Based on the available literature, we defined SMFT as a short exercise bout, undertaken at a standardized intensity that is intended to be non-exhausting, and performed with the purpose of inferring an athlete’s physiological state through the monitoring of relevant outcome measures. In this regard:
Exercise is typically a cyclic activity involving large muscle groups. In team-sports settings, this is often administered as running activities, however, cycling has also been featured.
Standardized intensity refers to a threshold(s) that is standardized based on an internal response or external intensity parameter, and can be either fixed for all athletes (i.e., absolute) or individualized to a capacity anchor (relative; e.g., fraction of HR maximum or maximal aerobic speed).
Non-exhausting generally excludes frequent or prolonged ‘all-out’ maximal intensities, intensities that would cause voluntary cessation, or intensities that elicit an excessive training stimulus beyond that originally intended. From a practical standpoint, in team sports, the test should not have negative carry-over effects for the subsequent training session (for instance, if administered during the warm-up), or elsewhere it is implemented as an integrated standardized training component within the session plan (see for example, Sect. 3.2; intermittent-variable category).
-
Physiological state can be defined as a particular condition or function of an individual’s physiological system, or a combination of systems—primarily, cardiovascular, respiratory, nervous, and muscular—at a specific point in time. In the context of SMFT, it may be used to infer an athlete’s current (physical) performance capacity or training effects (i.e., training responses).
Training effects [4] indicate the direction (i.e., positive, negative) and the time course of the effect. Considering the challenges of dichotomizing time course criteria, we opted to use commonly referenced durations [4, 42] that align with the context and design of the included studies in our review, classified as acute (i.e., immediate [49] and up to a 1-week duration [47, 52]), short term (typically 1–3 weeks; e.g., congested or intensified periods [53, 54], training camps [54, 55], exposure to extreme environments [56, 57], season break [58]), and chronic (usually established over several weeks or months of training; e.g., pre-season [51, 59], training intervention [60, 61]). The first two are commonly referred as transient effects, while the latter typically indicates more ‘persistent’ or ‘enduring’ changes [4].
Outcome measures include cardiorespiratory/metabolic, subjective, mechanical, or a combination, and are used as proxy (surrogate) measures that reflect (either directly or indirectly) the physiological systems they intend to assess. These are collected continuously within exercise and then aggregated into a summary metric (e.g., mean HR, accumulated ground impacts estimated via accelerometery-derived data), or measured immediately post-exercise (e.g., HRR, blood lactate, RPE).
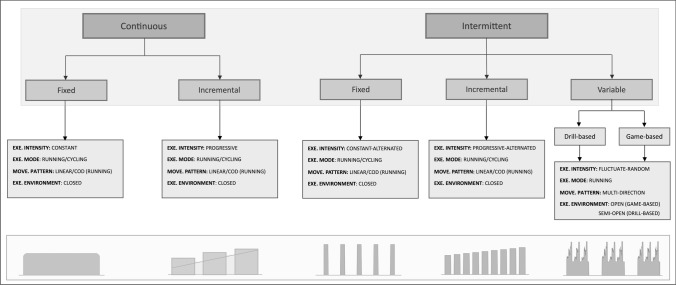
Protocol Taxonomy
Information on SMFT protocols was extracted and categorized in reference to two main levels of classification: (1) exercise regimen (continuous or intermittent) and (2) manipulation of exercise intensity (fixed, incremental, or variable). Regarding exercise regimen characteristics, continuous activity represents a constant load exercise bout (typically for at least several minutes), without frequent alterations in velocity or rest periods [14, 62]. Alternatively, intermittent is defined as an activity that is interrupted and restarts after a particular time span, characterized by alternated loads and rest intervals [63, 64]. Considering all possible combinations of these categories, we subsequently identified five distinct SMFT categories from the available literature (Fig. 1), with each category further sub-divided based on the activity mode (running or cycling), movement pattern (linear, change of direction, or multi-directional), and exercise environment (closed, semi-open, or open):
Continuous-fixed category represents a fixed-intensity exercise bout that remains constant for the entire SMFT and intends to elicit a steady state (e.g., 4 min running at 12 km·h−1) [65, 66].
Continuous-incremental category is characterized by a progressive increase in intensity within (single) or between (multiple) exercise bout(s), whereas each bout lasts for several minutes (e.g., 4 min running with progressive increases in speed, 3 sets × 3-min bouts at 10, 11, and 12 km·h−1, interceded by 1-min rest periods) [11, 67].
Intermittent-fixed category involves reoccurring activities performed at a constant intensity and rest intervals (e.g., four running bouts × 50–60 m at 18–22.5 km·h−1, separated by 30 s of recovery) [49, 68].
Intermittent-incremental category predominantly involves fixed rest periods, while intensity is increased between exercise bouts (e.g., 30-s shuttle runs at 10–14 km·h−1, alternated by a 15-s rest period and with a-0.5 km·h−1 increment after each bout) [59, 69].
Intermittent-variable category represents specific and non-specific standardized drills, and therefore locomotive demands fluctuate during the exercise (i.e., multi-directional movements). This category can be further categorized into drill-based and game-based exercises. Drill-based exercises refer to exercises that do not include competition features (e.g., passing drills) [70], whereas game-based exercises are characterized with competition features (small-sided games [SSG]) [71, 72].
Fig. 1.
Submaximal fitness tests (SMFT) protocol taxonomy. Each protocol category consists of two levels: (1) exercise (EXE) intensity intermittency (continuous or intermittent) and (2) manipulation of exercise intensity (fixed, incremental, or variable), together yielding five distinct SMFT protocol categories (shaded areas). Intermittent-variable can be further categorized into drill-based and game-based formats. Each category can be further manipulated based on the movement (MOVE) pattern (linear, change of direction [CoD], and multi-direction), activity mode (running or cycling), and exercise environment (closed, semi-open, or open)
Application of the Taxonomy to the SMFT Team-Sports Literature
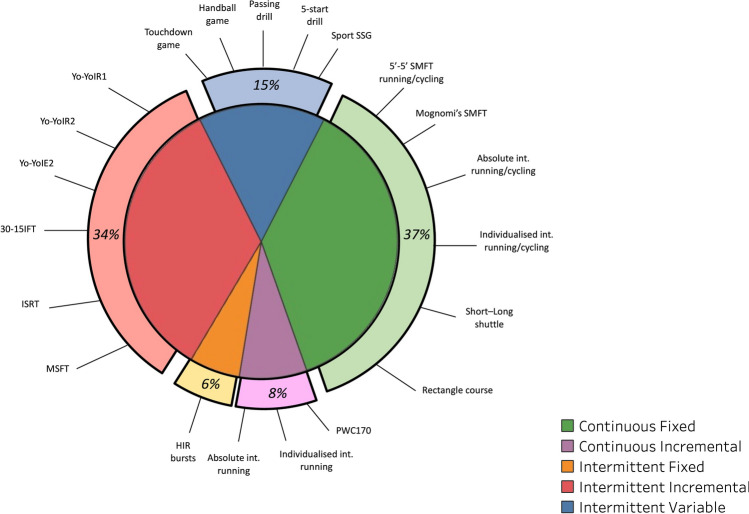
From the 87 included team-sport studies, we identified 100 independently described SMFT. As illustrated in Fig. 2, the majority of studies in the literature adopted continuous-fixed SMFT (37%), followed by intermittent-incremental (34%), intermittent-variable (15%), continuous-incremental (8%), and intermittent-fixed (6%). Table 1 provides a summary of these SMFT as described in these studies. Continuous-fixed protocols were administered in both running and cycling exercise modes and include linear and change of direction (running protocols) movement patterns performed at absolute or relative standardized intensities. Continuous-incremental protocols comprised incremental exercises that were terminated when a specific internal (e.g., HR) or external (e.g., speed) intensity was achieved. Intermittent-fixed SMFT solely involved short-duration (8–12 s), high-intensity standardized bursts (~ 50–60 m). Intermittent-incremental SMFT incorporated shorter versions of the most common intermittent shuttle fitness tests, such as the Yo-Yo Intermittent Recovery Tests (Yo-YoIR1&2) [46] and 30–15 Intermittent Fitness Test [5]. Finally, intermittent-variable SMFT were mostly administered as game-based practices, including non-specific (handball, touchdown games) and specific (SSG of the sport) exercises, while drill-based practices included a variety of passing exercises (Table 1).
Fig. 2.
Frequency of submaximal fitness test (SMFT) categories and their highlighted individual tests as identified in the team-sports literature. A detailed description of these tests is highlighted in Table 1. 30-15IFT 30–15 Intermittent Fitness Test, HIR high-intensity runs, Int. intensity, ISRT interval shuttle run test, MSFT multi-stage fitness test, PCW physical capacity work, Yo-YoIE2 yo-yo intermittent endurance level 2, Yo-YoIR1 yo-yo intermittent recovery test level 1, Yo-YoIR2 yo-yo intermittent recovery test level 2
Table 1.
SMFT described in the team-sports literature
| SMFT | No. of studies | Test description | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Category | Activity mode | Move. Patt | Protocol | Dimensions | Stand. volume | Stand. intensity | Exe. configuration | ||
| Continuous- fixed | Running | Linear | 5’-5’ | 1 | Treadmill | 5 minW/5 minR | 833/917 m | 10/11 km·h−1 | |
| Mognomi’s test | 4 | Track/treadmill | 6 min | 1350 m | 13.5 km·h−1 | ||||
| 5’-5’ | 2 | Track | 5 minW/5 minR | 750 m | 9 km·h−1 | ||||
| Individualized run | 1 | NS | 6 min | 1150–1200 m | 60%VIFT | ||||
| Individualized run | 1 | Treadmill | 10 min | NS | 90% VAT | ||||
| Individualized run | 1 | NS | 10 min | NS | 75% HR[RESERVE] | ||||
| Cycling | 5’-5’ | 4 | Bicycle | 5 minW/5 minR | 130 watts/85 rpm | ||||
| Individualized cycling | 1 | Bicycle | 4 min | 75%VO2 max/70 rpm | |||||
| Running | CoD | 5’-5’ rectangle | 2 | 20 × 20 m | 5 minW/5 minR | 750 m | 9 km·h−1 | ≈37 turns 90° | |
| Rectangle course | 3 | 100 × 50 m | 4 min | 800 m | 12 km·h−1 | ≈10 turns 90° | |||
| Short shuttle | 5 | 20 m | 3–5 min | 750–1000 m | ~ 9–12 km·h−1 | ≈38–50 shuttles 180° | |||
| 5’-5’ | 3 | 40 m | 5 minW/5 minR | 833–1083 m | ~ 10–13 km·h−1 | ≈21–27 shuttles 180° | |||
| Medium shuttle | 2 | 40 m | 5 min | 833–1000 m | ~ 10–12 km·h−1 | ≈21–25 shuttles 180° | |||
| Long shuttle | 3 | 80/100 m | 5/4 min | 1000/800 m | ~ 12 km·h−1 | 12.5/8 shuttles 180° | |||
| Long shuttle 5’-5’ | 2 | ≈80 m | 5 minW/5 minR | 750–1000 m | ~ 9–12 km·h−1 | ≈9–12.5 shuttles 180° | |||
| Individualized shuttle | 1 | 57–68 m | 4 min | ≈680–820 m | 75%MAS/ ~ 60%VIFT | 12 shuttles 180° | |||
| Continuous- incremental | Running | Linear | Individualized run | 1 | Treadmill | NS | NS | S 8 km·h−1; F THR | ↑ 1 km·h−1 every 1 min |
| Absolute run | 1 | Treadmill | 5 min | 1000 m | S 8; F 12 km·h−1 | ↑ 0.8 km·h−1 every 1 min | |||
| Absolute run | 1 | Treadmill | 3 min × 3 sets | 1700 m | 9, 11, 14 km·h−1 | 3-min continuous bouts | |||
| Absolute run | 2 | Treadmill | 12 min | 750–900 m | S 6/8; F 12 km·h−1 | ↑ 2 km·h−1 every 3 min | |||
| Cycling | PCW170 | 1 | Bicycle | 3 min × 3 sets | F at 170 beats/min−1 | 120–170 beats/min−1 stages | |||
| Running | CoD | Short shuttle | 1 | 20 m | 5 min | 900 m | ~ 8, 10, 12 km·h−1 | 1 min 8, 1 min 10, 3 min 12 km·h−1 | |
| Short shuttle sets | 1 | 20 m | 4 min × 3 sets | 2000 m | ~ 9, 10, 11 km·h−1 | ≈100 shuttles 180° | |||
| Medium shuttle sets | 1 | 50 m | 2 min × 4 sets | ≈1600 m | ~ 9.3, 11.1, 12.8, 14.6 km·h−1 | ≈32 shuttles 180° | |||
| Intermittent-fixed | Running | Linear | High-intensity run | 3 | 50-m bursts | 8 s | 50 m | ~ 18 km·h−1 | 3–4 reps |
| High-intensity run | 3 | ~ 60-m bursts | 12 s | ≈60 m | 18–24 km·h−1 | 4 reps | |||
| Intermittent-incremental | Running | CoD | 30-15IFT | 1 | 40-m shuttle |
≈8:25 min/ individualized |
≈960 m/ individualized |
F 13 km·h−1/ 25–75%VIFT |
≈24/individualized shuttles 180° |
| Yo-YoIR1 | 19 | 20-m shuttle | 2–6:51 min | 240–800 m | S ~ 10; F ~ 13.5/14.5 km·h−1 | 11–40 shuttles 180° | |||
| Yo-YoIR2 | 3 | 20-m shuttle | 2–8 min | 240–1040 m | S ~ 13; F ~ 16.5–18 km·h−1 | ≈12–52 shuttles 180° | |||
| Mod. Yo-YoIR2 | 1 | 18-m shuttle | 2–4 min | ≈470 m | S ~ 11.7; F ~ 14.9–15.8 km·h−1 | ||||
| Yo-YoIE2 | 2 | 20-m shuttle | 2–6 min | 280–920 m | S ~ 11.5; F ~ 13.5–14.5 km·h−1 | 14–46 shuttles 180° | |||
| ISRT | 1 | 20-m shuttle | 2–9 min | ≈260–1225 m | S ~ 10; F ~ 11–14 km·h−1 | ≈13–61 shuttles 180° | |||
| Individualized ISRT | 3 | 20-m shuttle | 9–12 min | 1225–1700 m |
70% max of the test S ~ 10; F ~ 14–15 km·h−1 |
≈61–85 shuttles 180° | |||
| MSFT | 1 | 20-m shuttle | ≈5:30 min | ≈800 m | S ~ 8.5; F ~ 10.5 km·h−1 | ≈40 shuttles 180° | |||
| Skating | 30-15IFT ice | 1 | 40-m shuttle | ≈3/6 min | ≈390/870 m | S ~ 10.8; F ~ 12.7/15.2 km·h−1 | ≈10/22 shuttles 180° | ||
| Yo-YoIR1 ice | 2 | 20-m shuttle | 6 min | ≈700 m | S ~ 10; F ~ 14.5 km·h−1 | ≈35 shuttles 180° | |||
| Intermittent-variable GB | Running | MD | 9v8 handball | 1 | 141 m2/player | 8 min | Similar game style | ||
| 4v4 touchdown | 1 | 150 m2/player | 4 min of 1 set | Score into the zone area | |||||
| 4v4 SSG | 1 | 80 m2/player | 4 min × 3 sets | ||||||
| 4v4 SSG | 1 | 120 m2/player | 1.5 min × 6 sets | With GK | |||||
| 4v4 SSG | 1 | 2 min × 4 sets | |||||||
| 5v5–10v10 SSG | 1 | 117 ± 65 m2/player | NS | Possession/with GK | |||||
| 3v3–6v6 SSG | 3 | 67.5–90 m2/player | 3 min × 2 sets | With/without GK, limit/free touch | |||||
| 5v5 + 5 SSG | 1 | 135 m2/player | 3 min × 4 sets | With GK, free play | |||||
| 5v5 SSG | 2 | 62.5/105 m2/player | 3 min × 3–4 sets | Without GK, free play | |||||
| Intermittent-variable DB | Running | MD | 5-star drills | 2 | 15–25 m runs | 4–5 min × 3 sets | Kicking, handballing, and marking | ||
| Passing drill | 1 | ~ 2/3 pitch | 6 min × 2 sets | Short and long distances | |||||
30-15IFT 30–15 Intermittent Fitness Test, CoD change of direction, DB drill-based, F finish, GB game-based, GK goalkeeper, HR[RESERVE] HR reserve, ind. individualized, ISRT interval shuttle run test, m meters, MAS maximal aerobic speed, max maximum, MD multi-direction, min minute, Mod. modified, Mov. Patt. movement pattern, MSFT multi-stage fitness test, NS not specified, PCW170 physical work test, R recovery, reps repetitions, rpm rate per minute, S start, sec second, SMFT submaximal fitness tests, SSG small-sided games, THR target HR = [(HR maximum – resting HR) * 80–85% intensity] + resting HR, VAT velocity at anaerobic threshold, VIFT final velocity achieved in 30-15IFT, W work, Yo-YoIE2 Yo-Yo intermittent endurance level 2, Yo-YoIR1 Yo-Yo intermittent recovery test level 1, Yo-YoIR2 Yo-Yo intermittent recovery test level 2, ≈ approximately, ~ mean, ↑ increase, ° CoD angle
SSG area per player was computed including GK
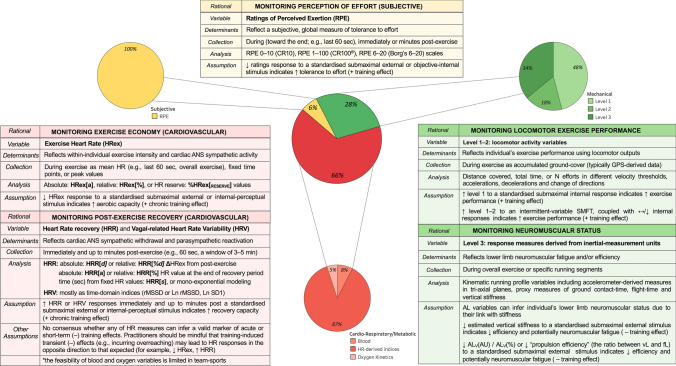
Outcome Measures
We identified 202 total outcome measures used in previous team-sports research. As shown in Fig. 3, cardiorespiratory/metabolic were the most used outcome measures (66%), followed by mechanical (28%) and subjective (6%). The following sections present the outcome measures corresponding to each response type, discuss their putative underlying mechanisms, and synthesize the current available evidence examining their changes within the SMFT framework.
Fig. 3.
Frequency of submaximal fitness test (SMFT) outcome measures as identified in the team-sports literature. Heart rate (HR)-derived indices are the most common cardiorespiratory/metabolic outcome measures and include variables representing exercise intensity (HRex) and recovery (HRR and HRV). Level 1–2 mechanical outcome measures represent locomotor activity variables collected during SMFT that are standardized by an internal stimulus or intermittent-variable exercise such as small-sided games (SSG). Level 3 mechanical outcome measures are response measures derived from inertial measurement units (micro-electrical mechanical systems [MEMS]) for monitoring neuromuscular status. Subjective outcome measures represent tolerance to effort and have been monitored solely via ratings of perceived exertion (RPE). AL accelerometry-load, ALV (AU) the vertical vector magnitude component of tri-axial AL, ALV (%) percentage contribution of the vertical vector magnitude component to tri-axial AL, ANS autonomic nervous system, CT contact time, Force-load (fL) sum of estimated ground-reaction forces during all foot impacts, GPS global positioning system, Ln rMSSD natural log of rMSSD, Ln SD1 log-transformed standard deviation of successive R spikes measured from Poincaré plots, rMSSD root mean square of the sum of all differences between successive normal heartbeats, Velocity-load (vL) sum of distance covered weighted by the speed of displacement (in SMFT refers to the actual mean velocity), + positive, − negative
Cardiorespiratory/Metabolic Outcome Measures
In team-sports settings, which can include a large number of individuals who may possess different aerobic capacities [8, 12], it is difficult to implement SMFT that are standardized by internal intensity variables. Accordingly, the majority of the tests were applied by standardizing the external intensity and measuring the corresponding internal responses [10, 73]. A variety of cardiorespiratory/metabolic outcome measures have been used in the literature, with the most common being HR-derived indices (Fig. 3). These include variables collected during (exercise HR [HRex]), immediately after (HRR) the SMFT, and soon after (HR variability [HRV, vagal-related HRV]) the SMFT. Other measures include blood markers (e.g., blood lactate) [67, 74–80] and oxygen consumption-related parameters (e.g., oxygen uptake) [75, 76, 81, 82]. As blood and oxygen uptake outcome measures are time consuming, expensive, and obtrusive, their viability to provide standardized and repeatable response measures is considered limited, particularly in team sports [11, 83]. Accordingly, we focused on HR-derived indices.
Exercise HR
Exercise HR is collected during the SMFT and is analyzed in absolute (beats per minute; HRex[a]) [47, 59, 66, 69, 74–76, 81, 82, 84–103, 104], relative to maximal HR (HRex[%]) [6, 11, 12, 45, 46, 48, 51, 54, 56, 57, 59–61, 66, 67, 70, 79, 83, 84, 89, 91, 105–119, 120], or HR reserve (HRex[reserve]) [53] values. A variety of methods are used to derive HRex, with the majority calculating the mean HR during the last 10–60 s of the test [11, 12, 45, 47, 48, 51, 53–61, 66, 69, 71, 74, 75, 82, 83, 85–87, 89, 92, 93, 96, 97, 103, 105–108, 111, 113–115, 117, 119–121]. Other approaches calculate the mean HR during the overall test (particularly during intermittent-variable protocols such as SSG) [70, 71, 79, 94, 98, 101, 104, 116], specific fixed timepoints [6, 46, 59, 60, 84, 91, 95, 99, 105, 109, 110, 112, 122], or peak values observed [61, 90].
HR Recovery
Heart rate recovery can be defined as the rate at which HR declines after exercise cessation [10, 39] and may be collected with athletes lying supine [123], sitting upright [12, 45], standing [89, 121], or walking [95]. Similarly, HRR can be assessed as the absolute (HRR[d]) [45, 47, 48, 53, 54, 57, 59, 61, 66, 88, 100, 103, 107, 114, 119, 121, 123, 124] or relative (HRR[%d]) [12, 47, 53, 60, 66, 102, 104, 107, 113, 114, 121] difference between HRex and HR value observed between 10 and 180 s post-test. Alternative approaches include the actual HR value observed at the end of the designated recovery period in absolute (HRR[a]) [66, 74, 89, 95, 99, 121, 125] or relative (HRR[%]) [66, 89, 109, 110, 113] values, or the overall mean HR during a variety of fixed time intervals [90, 97, 107]. Other approaches calculate time-based variables such as the time required to decrease from between fixed HR values (HRR[s]; e.g., time between 80 and 70% HR maximum) [79], or the time constant of HRR derived from mono-exponential modeling [61, 126].
HR Variability
Vagal-related HRV is defined as the variability in the time intervals (usually in milliseconds) between adjacent heartbeats and reflects the regulation of cardiac autonomic nervous system (ANS) balance [10, 127]. Heart rate variability indices are commonly collected in a seated or supine position and resting state in a laboratory or quiet room [10, 42]; however, as the aim in SMFT is to monitor the response during and after a given submaximal workload, only HRV parameters observed immediately or soon after the test are relevant for SMFT in team sports. These measures are usually analyzed within a window of 3–5 min post-test cessation, and predominantly calculated as time domain-related variables such as the square root of the mean of the sum of the squares of all differences between successive normal heartbeats (rMSSD) [61, 107] or its natural log (Ln rMSSD) [45, 47, 53, 59, 100, 106, 114], natural log of standard deviation of successive ‘R spikes’ (the peak of the QRS complex, reflective of ventricular depolarization, recorded from an electrocardiogram wave) measured from Poincaré plots (Ln SD1) [57, 106], and the standard deviation of mean interval differences between normal heartbeats (SDNN) [61, 107].
Putative Mechanisms
Heart rate-derived indices are commonly used to inform chronic aerobic-oriented training effects, attributed to the linear relationship between HRex and oxygen uptake during an intended steady-state activity [10, 42]. A reduction in HRex to a standardized submaximal stimulus may represent improved exercise economy, which may translate to the development of aerobic fitness [51, 120], whereas an increment of HRex is considered to reflect a negative response (de-training of the cardiorespiratory system) [87], likely due to central adaptations (i.e., left-ventricular function) [128]. In addition, an increment of HRR or vagal-related HRV measures is considered a positive effect [59, 60, 107], reflecting the reactivation of the parasympathetic system and hemodynamic adjustments post-exercise [10]. That said, in addition to being more time consuming, these measures may be influenced by preceding exercise, with higher intensities eliciting increased blood acidosis that simulate the metaboreflex, and therefore may reduce HR decay post-exercise and alter HRR and vagal-related HRV results [10, 53].
The use of HR-derived indices to infer negative transient training effects is inconclusive in the SMFT research. The theoretical basis for their inclusion is due to the potential influence of various training-induced physiological processes that originate in central (i.e., ‘central command’) and peripheral (e.g., afferent feedback from skeletal muscles) body regions to alter cardiac ANS function (i.e., the balance between the sympathetic and parasympathetic systems), and subsequently HR activity [10, 38, 42]. It has been hypothesized that training-induced fatigue or an incomplete recovery might result in a greater muscle activation at a given intensity [129], promoting increased oxygen demands [129] and yielding accelerated cardiac sympathetic activity that consequently increase HRex, and reduce HRR and HRV [114, 129]. In contrast, previous research has proposed that increased training stress (leading at least to an overreaching state) may cause opposite responses — increased parasympathetic activity or blood plasma volume, consequently lowering HRex and increasing HRR and HRV [37, 38, 130].
Inferring Physiological State
Generally, across a standard micro-cycle, HR measures tend to stay relatively stable [45, 47]. For example, studies among youth and senior athletes have observed no changes in the day-to-day variability of SMFT HRex [45, 47, 75] and HRR [45, 47] derived from multiple SMFT administered throughout the week, despite substantial variations in training loads. Whilst vagal-related HRV indices are considered to provide a better insight into the cardiac ANS [10, 53], daily variations in training loads were associated with stable [45, 47] and lower [53] responses. The disparity across studies may be due to the differences in training loads and HRV variables [53], an athlete’s fitness levels [45], or simply reflective of measurement ‘noise’ (either measurement errors or biological variations) [10, 61, 107], thus challenging between-study comparisons.
The current research suggests that the use of HR-derived indices appears more relevant after acute (3–7 days) and short-term (~ 2 weeks) altered training stress, albeit it may cause misleading interpretations. In team sports, 3–4 consecutive days of accumulated training loads have been associated with both increased [114] and decreased [54] SMFT HRex. Lower SMFT HRex values have been also observed after 2 weeks of intensified training [84], but also following a substantial decline in training loads due to season breaks [58]. Whilst the information in team-sports settings is limited, studies among various cohorts of individual endurance athletes (e.g., cyclists, triathletes) provide encouraging evidence that short-term intensified periods (1–3 weeks) of training-induced fatigue (incurring functional overreaching) lowered SMFT HRex [36, 38, 130] and increased SMFT HRR [36, 37, 39]. These responses likely reflect a complex interplay between acute cardiac ANS function (usually referred to as larger parasympathetic activity) and increased plasma volume [37, 54, 104], leading to an enhanced stroke volume for a similar cardiac output [10, 131]. In summary, the use of HR-derived indices (especially HRex and HRR) to infer transient training effects associated with cardiac ANS dysfunction is currently questionable (at least, not straightforward), with no consensus around the underlying mechanisms and conflicting results in the literature.
Overall, SMFT HRex has small to very large inverse relationships with performance indicators (i.e., maximal oxygen uptake, intermittent endurance capacity) when measured concurrently (lower HRex is associated with higher test results) [46, 48, 105], suggesting its validity as an indicator of an individual’s current endurance capacity. Indeed, it has been highlighted that a chronic exposure to internal (e.g., HR-based training impulse, session RPE) [86, 90] and external (e.g., total distance covered, force load) [71, 120] loads is associated with reduced SMFT HRex. However, the studies examining training effects within athletes have reported contrasting findings. For example, studies in soccer players [46, 91] have observed moderate to very large relationships between SMFT HRex and intermittent endurance performance at different timepoints across the season, albeit with no interaction between the magnitude of these effects. Likewise, improved [91] or maintained [87] intermittent running ability did not necessarily coincide with reduced or stable SMFT HRex, respectively. In contrast, studies conducted on a variety of team sports and age groups have observed significant relationships between changes in similar markers from pre-season to in-season [51, 59], and across a full season [107]. Improved SMFT HRex were also largely correlated with the changes in running speed at 4 mmol·L−1 blood lactate [11, 83] or a reduced oxygen uptake at fixed submaximal intensities (i.e., exercise economy) [81].
Research observations are more consistent where SMFT HRex has been administered to evaluate the adaptation time course to changes in extreme environments (heat and altitude) during training camps or competitions [55–57, 93, 104, 106, 132]. Collectively, HRex displayed substantial deteriorations upon arrival and up to days of exposure [56, 57, 93, 104], and generally return to baseline values within 6–10 [55, 106] or 14 days [56], with quicker adaptations among highly trained individuals or across repeated exposures within individuals [133, 134]. Taken together, whilst it appears that SMFT HRex has the potential to serve as a valid and sensitive marker of positive training-induced effects, it remains questionable whether it can be used as a surrogate measure of within-athlete changes in maximal aerobic capacity. There is, however, considerable evidence suggesting its use during exposure to changes in environments for monitoring the athlete’s acclimatization.
The magnitude of correlations between cardiac parasympathetic-related variables (HRR and vagal-related HRV) and performance indicators is less clear and ranged from no correlation to a very large relationship [48, 66, 100]. The disparity could be the consequence of varied protocol intensities [10, 35, 42, 45], collection time (e.g., 60 s and 180 s post-exercise) [48], analysis approaches [66], and fitness criterion measures [45, 79]. Importantly, inferences regarding their long-term validity as proxy measures of chronic training effects can be somewhat impacted by SMFT intensity (i.e., HRex) [10]. The rate of the sympathetic withdrawal and parasympathetic reactivation post-exercise is altered when the recovery period starts from different intensities. As an example, different absolute HRR values (HRR[d]) may be expected 60 s post-SMFT if the exercise intensity varies (e.g., 90% vs 75% HR maximum). Hence, in theory, a significant reduction in HRex might influence the concurrent interpretation of post-exercise outcomes. Although this issue has been addressed by analyzing HRR in relative values (HRR[%d]) [60, 114], the time necessary to decrease from two fixed HR values (HRR[s]) [79], or employing individualized intensity protocols [12], these are not yet fully understood. In support of this, regardless of the HRR analysis used, authors examining training-induced changes in both HRex and HRR did not always find congruent trends [60, 61, 102]. Other studies observed a lack of association between changes in HRR and endurance performance, despite significant relationships with HRex [59, 107]. However, increased SMFT vagal-related HRV has been shown to be more appropriate, with studies reporting its validity for monitoring endurance-oriented training effects [59, 61, 107].
Considerations
Of critical importance when using HR-derived indices as proxies of training effects is the range of confounding factors, such as environmental (e.g., temperature), habitual (e.g., sleep, diet), circadian (time during the day), and psychological (e.g., emotions, stress). These could all contribute to the error of measurement of SMFT HR measures — HRex (coefficient of variation (CV): 1.0–3.5%) [12, 45, 48], HRR (CV: 2.8–13.8%) [45, 48, 66], and vagal-related HRV (CV: 6.6–19.0%) [45, 61, 106] — and should be considered (or standardized where pragmatic) when interpreting changes in HR-derived indices responses to SMFT [10, 42].
Further research is warranted to explore the use of all HR-derived measures to infer acute and short-term effects, in particular, verifying the interaction between temporary changes in cardiac ANS function and plasma volume responses. In this respect, it should be highlighted that HR responses may still be less appropriate to denote peripheral neuromuscular fatigue, which are considered more important to monitor delayed recovery and injury risk mitigation in team sports [49, 135]. In the longer term, HRex is probably the easiest to collect and most reliable HR measure, and its utility in observing positive changes in aerobic capacity has stronger empirical support. Accordingly, the utility of adding post-exercise (HRR, vagal-related HRV) SMFT HR responses to infer chronic effects may be redundant. In order to enhance interpretations, future research should first determine meaningful changes in SMFT HRex (i.e., smallest worthwhile change) in reference to variations in physiological states.
Finally, when monitoring the responses to intermittent-variable SMFT (e.g., SSG), an athlete’s HRex may be influenced by their locomotor activity. These are likely to differ between tests and should be accounted for when interpreting data. Therefore, we recommend quantifying intermittent-variable SMFT locomotor activity for consideration. Given the reasonable association between internal and external measures during field-based sessions [136], it is also possible to standardize HRex to a given (fixed) external intensity parameter. Whilst some have attempted to achieve this by dividing the former by the latter, creating a ratio [137], there are complex statistical properties and assumptions associated with such indexes, presenting as a major validity concern [138]. To appropriately examine HRex while holding external intensity parameters constant, we recommend linear regression techniques, which do not violate statistical assumptions and achieve the desired outcome ratios [139].
Subjective Outcome Measures
Subjective measures are recognized by their ability to serve as gestalt measures that can be used across different exercise typologies, given their feasibility and low cost [140]. These are commonly applied to quantify an athlete’s perception of intensity and training effects. The former is derived solely from RPE, while the latter are commonly referred to as athlete-reported outcome measures [141] of latent response constructs such as readiness, wellness, and stress. [4, 142]. Accordingly, RPE are the only subjective outcome measures that can be applied to SMFT, a notion supported by their exclusivity (albeit the limited number of studies) in the team-sport SMFT literature (Fig. 3). Among the available studies, different scales such as the Category-Ratio 10 (CR10 deciMax) [50, 56, 57, 67, 70, 98, 108], 100 (CR100® centiMax) [91], and 6–20 (Borg’s 6–20) [75, 76] have been adopted, using a variety of collection protocols (during the last 180 s, immediately, and up to 5 minutes post-exercise).
Putative Mechanisms
Perception of effort is defined as the ‘conscious sensation of how hard or strenuous a physical task is’ [142], and mainly depends on how easy or hard it is to breathe and drive the working muscles during exercise [143]. As part of SMFT, the athlete provides a retrospective appraisal of perceived effort to a standardized stimulus that can be prescribed by either an objective internal [32] or external [91] means. Because RPE is strongly associated with cardiorespiratory, metabolic, and neuromuscular measures of exercise intensity [144, 145], and influenced by the mental state [142], changes in RPE may reflect positive [32, 91] or negative [37, 41] alterations in the psycho-physiological state. However, given their gestalt nature, it is perhaps difficult to align RPE as a proxy to a single physiological system during SMFT. For example, RPE has been empirically associated with HRex during a continuous exercise [144] and might therefore be used as a cardiorespiratory proxy measure. However, spinal or supraspinal motoneuron inhibition, which is a neuromuscular phenomenon, can increase central motor command and subsequently RPE [146]. This is not to say that RPE cannot be used to infer a physiological state during SMFT, but rather the mechanisms may be less precise. In addition, given that RPE has also been used to regulate exercise intensity [147], RPE can be used as an anchoring intensity variable (i.e., running or cycling at fixed RPE), whereby external outcomes such as velocity or power output are used as response measures [148]. However, to our knowledge, there is no published team-sports research evaluating the theoretical basis of such SMFT and their actual utility.
Inferring Physiological State
Whilst some evidence supports the use of SMFT RPE [58, 91, 98], it is difficult to support or refute their utility to determine training effects, given the limited data available in team sports. In endurance athletes, RPE have been shown to detect negative transient effects associated with functional overreaching and disturbances in endurance performance [30, 37, 41], while their sensitivity to chronic positive effects is less certain [34, 40]. In the team-sports context, one study [91] showed that reduced SMFT RPE (albeit maintained HRex[a]) was accompanied with enhanced intermittent running performance (Yo-YoIR1) and soccer match high-intensity running [91]. Another study [50] in professional soccer players did not observe any significant relationships between RPE collected immediately after an individualized SMFT and athlete-reported outcome measures across 6 in-season standard weeks. Despite the conflicting results, researchers have suggested the potential usefulness of SMFT RPE when measured concomitantly with other objective outcome measures (e.g., HRex) as part of a multivariate monitoring approach [37, 42, 130].
Considerations
It is noteworthy to highlight some of the challenges associated with collecting and interpreting RPE in team sports, where interpretation is challenged by the presence of the coach and peers biasing ratings, the application of unvalidated collection tools, lack of or inappropriate athlete familiarization/education, and their gestalt nature [142, 146, 149]. Moreover, RPE may be confounded by other sensations associated with exercise, such as mood, discomfort, pain, and enjoyment [142]. In view of these challenges, researchers may consider other perceptual measures such as ratings of fatigue [150], or techniques such as numerically blinded [149] and differential [151] RPE, alongside the implementation of rigorous familiarization processes to facilitate authentic and sensitive perceptual ratings associated with SMFT.
With this in mind, a benefit of SMFT in team sports is to provide an assessment that can be seamlessly integrated into the training session such as the warm-up or standardized drills. The need to collect RPE from all athletes individually (~ 20–40) under controlled conditions is likely to be disruptive and impractical, which is perhaps why there are few studies using this practice. It is probably reasonable to assume that unless SMFT are completed as a discreet activity, with smaller groups, or RPE collection procedures are made more accessible (e.g., mobile devices, human resources), these outcome measures may be less pragmatic or sustainable in team sports.
Mechanical Outcome Measures
Within the current monitoring schemes in sport, there is a broad classification of external load parameters. These indices represent kinematic outputs [152] performed by an athlete throughout an exercise bout/session [153] and have been classified into three distinct levels, which we will use here to audit their implementation in the context of SMFT [8, 154].
Level 1–2 Measures
Level 1 variables are typically the locomotor performance outputs including distance covered, time spent, or the count of efforts in different velocity zones, whilst Level 2 variables reflect changes in velocity such as accelerations and decelerations (i.e., change of directions) [8]. Such kinematic parameters are routinely collected using global positioning systems (GPS) or other tracking technologies (i.e., semi-automated pixel tracking, local positioning systems). In the team-sports SMFT framework, the use of level 1–2 mechanical outcome measures can occur in two scenarios: (1) monitoring the speed achieved to a submaximal exercise that is standardized by internal intensity responses [50, 155] and (2) monitoring the changes in these variables during intermittent-variable standardized drills [54, 58, 70–72, 79, 93, 98, 106, 116, 132, 156], as they are standardized by a variety of other parameters such as duration, sets, recovery, and unique constraints (e.g., number of players, rules modifications). Whilst the former is considered less practical in team sports for many pragmatic reasons, the latter are implemented as a part of the training plan, encompassing sport-specific actions and are perhaps the most feasible to apply routinely [8, 131]. Conceptually, higher values (e.g., accumulated distance covered), coupled with stable or lowered internal responses are indicative of positive effects (i.e., improved exercise performance) [8, 58, 98]. In fact, studies examining level 1–2 variables during drill (passing) and game (SSG) exercises have highlighted their pragmatic advantages to deliver information related to an athlete’s performance [58, 71, 72, 98]. However, it should be noted that intermittent-variable SMFT are influenced by a variety of individual and contextual factors such as technical level, motivation, and tactics [8, 72], and have a higher degree of variation (test–retest reliability) compared with other SMFT modalities [70, 72, 156, 157], and therefore, should not necessarily be interpreted in the aforementioned simplistic manner [8].
Level 3 Measures
Level 3 external load variables are derived from inertial-measurement units such as tri-axial accelerometers, magnetometers, and gyroscopes [8] (collectively referred to as micro-electrical mechanical systems [MEMS] [158, 159]). Unlike level 1–2 variables, these outcome measures can be used for the majority of SMFT applied in the team-sport context and have been proposed to provide an insight into an athlete’s neuromuscular system, given their potential link with lower limb vertical stiffness [135, 154, 160–163]. Vertical stiffness is considered to affect several athletic parameters, including elastic energy storage and utilization (i.e., stretch shortening cycle) [164] and has traditionally been measured through a variety of jump assessments (counter-movement, hopping, and drop jumps) using variables such as jump height, contact time, and flight time [52, 165, 166]. However, because of the limited viability of these assessments in field conditions and their lack of specificity (jumping activities may be less sensitive to detect changes in running strategies) [52, 161], researchers and practitioners have started to collect proxy variables required to estimate vertical stiffness derived from MEMS during SMFT [49, 52, 55, 65, 68, 72, 167–169].
To date, studies have adopted accelerometer-derived vector magnitudes (collectively termed in this review as accelerometery load [AL]) [49, 52, 72] and individual vector components (vertical AL [ALV], antero-posterior AL [ALAP], and medio-lateral AL [ALML]) using MEMS-embedded accelerometers [49, 52, 68, 167, 168], predominantly collected during intermittent-fixed protocols comprising high-intensity running bursts [49, 52, 55, 68, 168]. Generally, reduced AL in the vertical plane (ALV [arbitrary units; AU]), or the percentage contribution of the ALV to the overall tri-axial vector magnitude (ALV [%]) during SMFT have been postulated as an indicator of reduced leg vertical stiffness and subsequently inferred a degree of lower limb neuromuscular fatigue [167, 170]. Theoretically, reduced vertical stiffness may lead to reduced efficiency for the same speed through altered kinetic and kinematic parameters, such as reduced vertical ground-reaction forces and increased ground-contact time [161, 170], which likely lead to decreased stride length [52, 72] and elevated energy cost [162, 170].
Inferring Physiological State
Studies investigating acute effects on mechanical outcome measures during SMFT are scarce, and those available are quite disparate in terms of protocols, variables, and their analytical processes [49, 52, 65]. Nonetheless, there is an emerging agreement from these studies that suggest AL measures can provide sensitive indicators of an athlete’s neuromuscular fatigue and efficiency. In a group of professional soccer players who performed an intermittent-fixed SMFT (4 × ~ 60-m runs, alternated by an ~ 30 s recovery) before and immediately after a training session, Buchheit et al. [49] found that various AL variables respond differently to different training modes (strength, speed, endurance-oriented conditioned sessions). Estimated vertical stiffness slightly increased after all training modes, whereas propulsion efficiency (the ratio between velocity loads and force load; refer to Fig. 3 for variables) was session dependent (largely increased after strength, small and moderate decreases after endurance and speed, respectively), suggesting its sensitivity to detect changes in running strategies (hypothetically, horizontal force application capability) [8, 49]. A study [52] using a similar SMFT protocol and outcome measures among university rugby union players reported large relationships between the vector magnitude and vertical accelerometer components derived from the constant phase of the run, versus leg stiffness measured more directly via submaximal hopping test performed on a force platform [52]. Whilst only trivial effects were observed in leg stiffness over the week, the changes in SMFT AL data were large [52].
Similar trends were also found in a study investigating the alterations in triaxial AL data collected before, 48 h, and 96 h after an Australian football match [68]. A main finding reported in this latter study was that ALV (AU) and ALML (AU) derived from the constant phase of the SMFT were still impaired 96 h post-match among players who were classified as ‘fatigued’ (> 8% reduced counter-movement jump at a 48 h post-match) [68]. Finally, a within-individual longitudinal study among soccer players [72] showed reductions in AL m·min−1 and AL slow·min−1 collected during a standardized SSG (5v5 + 5) 1 day before a match were concomitant with a reduction in neuromuscular function (flight-time:contact-time ratio measured from counter-movement jump) and an altered match running profile—increased ALML (%) and decreased ALV (%) contribution to AL—indicative of potential neuromuscular fatigue [72, 167]. Collectively, it appears that specific mechanical level 3 metrics may be useful for identifying acute variations in performance (neuromuscular fatigue and efficiency) associated with changes in lower limb function.
Inferring longer term training effects from mechanical variables ascertained during SMFT has received limited attention, and insights have been drawn exclusively from tracking locomotor outputs during intermittent-variable SMFT in the form of SSG. For example, moderate to very large positive relationships have been reported between higher level 1–2 outputs during SSG and intermittent running capacity [98]. In addition, during intensified training camps (1–2 weeks), within-individual increases in running parameters (e.g., total and high-speed running distance) measured during intermittent-variable SMFT were also concordant with improved intermittent running capacity [54, 106, 132]. Of note, the utility of all mechanical outcome measures (levels 1, 2, and 3) derived during SMFT in detecting chronic training effects in neuromuscular function such as improved running efficiency (enhanced muscle–tendon unit recoil) is unknown.
Considerations
Most studies adopting mechanical outcome measures to denote acute neuromuscular effects have administered SMFT characterized by intermittent high-intensity bursts. These outcome measures are often sampled from the constant running velocity phases of the SMFT and using the vertical accelerometer component [52, 68, 167], perhaps owing to an enhanced association with vertical stiffness [52, 68]. Typically, such techniques have demonstrated an inferior degree of reliability (CV: 6.7–17.5%, standardized TE: small to moderate [49, 52, 68]) versus maximal and non-running-based assessments of neuromuscular function (jump and force indices; CV: 2.9–6.1%, standardized TE: small [49, 65, 171]). One study [65] using a continuous-fixed SMFT and lower running intensity (mean velocity of 12 km·h−1 compared to 18–22.5 km·h−1) reported lower measurement noise (CV: 2.1–8.0%, standardized TE rated as small). Additionally, the changes found in ALV (%) [decreased] and ALML (AU) [increased] 24 h after a strenuous soccer training session were greater than smallest worthwhile change (signal-to-noise ratio > ± 1) [167]. Although these findings indicate enhanced reliability and sensitivity for SMFT involving lower running speeds in a more continuous manner, this is based on only one study and the utility of different SMFT protocols has not yet been compared in the available literature, and barriers to implementation should also be considered. Similarly, the questionable reliability of locomotor outputs recorded during intermittent-variable SMFT in the form of SSG (total distance CV: 2.3–11.7%, high-speed thresholds CV: 8.1–83.0% [70, 72, 94, 98, 156, 157], small to moderate in magnitude [70, 156, 157], perhaps limits their utility to denote moderate-to-large effects only (i.e., larger CV may decrease the signal-to-noise ratio).
Although studies have suggested that changes in AL variables may reflect effects on lower limb stiffness [162, 172, 173], few have directly assessed stiffness [52, 174]. Moreover, these studies have typically used MEMS mounted between the scapulae, which may be influenced by upper-body kinematics during running or dampening of ground-contact vibrations [172, 175]. Whilst unit placement may have limited the impact under standardized conditions, intermittent-variable SMFT may be more susceptible to positioning noise as changes in orientation of the MEMS devices are not considered in the quantification of accelerometer metrics. In addition to positioning, users should be cautious of other extraneous factors such as movement artifacts within the device harness, running surface (e.g., ground stiffness), and footwear [158].
Future work should address the overall convergent validity of MEMS-derived data to obtain an accurate estimation of running strategy characteristics such as vertical stiffness. It is also necessary to investigate the theoretical framework for the sensitivity of these measures and their potential mechanisms (i.e., with respect to human tissue and gait mechanics). Furthermore, more research is required to examine whether protocol characteristics (e.g., exercise regimen, running intensity) and unit placement (e.g., center of mass, foot-mounted MEMS unit) can enhance measurement properties, and therefore facilitate inferences regarding lower limb stiffness and ultimately neuromuscular fatigue or efficiency.
Summary and Conclusions
Our review provides an overview of the literature regarding SMFT in team sports, including the development of the SMFT definition, protocol categorization, and a systematic audit of protocols and outcome measures. We also provide a narrative synthesis of the applications of SMFT within the training continuum of sport teams and future research directions (outlined in Table 2). In summary, SMFT have the potential to serve as time-efficient, non-exhaustive, and feasible standardized tests that can be administered to a group of athletes simultaneously as a part of the warm-up and using specific drill(s) during the training session. Multivariate outcome measures such cardiorespiratory/metabolic (e.g., HR-derived indices), subjective (e.g., RPE), and mechanical (GPS and MEMS-derived data) can be collected simultaneously, and in theory, provide a multifactorial evaluation for athlete monitoring in team sports. Collectively, the literature suggests that several outcome measures collected during and immediately post-SMFT can inform on an athlete’s physiological state. Heart rate-derived indices seem more appropriate to denote positive chronic training effects on endurance performance, whereas their role in detecting negative transient effects associated with variations in ANS function is questionable. Despite the lack of knowledge about the underlying mechanisms and the inconsistent findings between studies, their sensitivity appears to improve after days or over short periods that are characterized by substantial alterations in training stress, seemingly caused by an interaction between cardiac ANS status and plasma volume responses. Subjective outcome measures are less common in team-based sports and only global RPE have been adopted thus far. Although their validity and practicability have yet to be established, researchers have proposed their utility when measured concomitantly with other objective measures (e.g., HRex) as part of a multivariate monitoring system. Mechanical outcome measures are relatively novel and have been mostly investigated using intermittent-variable and intermittent-fixed protocols, whereby the former primarily involves GPS-derived kinematic variables (levels 1–2) to monitor exercise performance, while the latter includes response measures derived from inertial measurement units (level 3) to monitor lower limb neuromuscular function. Whilst monitoring locomotor outputs during standardized training drills is more feasible and has shown to provide valuable data on an athlete’s performance, practitioners should consider the large influence of various individual and contextual factors (e.g., technical/tactical level, motivation) that may undermine their interpretations. Accelerometery load parameters can provide sensitive indicators of acute changes in lower limb function and therefore neuromuscular fatigue and efficiency, albeit the overall validity of these outcome measures and the physiological mechanisms underpinning their changes have not yet been fully evaluated. Moreover, there is an absence of information on the use of all mechanical metrics (levels 1–3) to monitor chronic training effects. Finally, future research should also examine the methodical elements (e.g., protocol characteristics, collection, and analytical processes) related to SMFT to derive the most appropriate protocol to capture reliable, valid, and sensitive outcome measures that provide useful inferences regarding an athlete’s physiological state.
Table 2.
Practical applications and future directions
| SMFT protocol | |||
| • | In team sports, which comprise a large number of individuals, it is more practical to prescribe external (duration and velocity) rather internal intensity (e.g., fixed HR response) parameters | ||
| • | Whilst (theoretically) individualized prescription of SMFT intensities accounts for the potential variation of physiological capacities within team-sports squads, this may be less feasible given the inherent requirement for periodic fitness assessments during seasonal stages | ||
| • | When HR-derived indices are monitored, notably HRex, we recommend the use of continuous (fixed, incremental) SMFT protocols, with a minimum dose of 3–4 min to attain more stable HR during data collection | ||
| • | Most studies administer intermittent-fixed, high-intensity SMFT to denote transient effects in lower limb function. This could be because researchers consider that higher velocities are required to examine neuromuscular status. Whilst no studies have explicitly examined this query, we encourage team-sport researchers to test the utility of continuous lower intensity SMFT | ||
| • | In the absence of strong evidence of regarding the optimal SMFT exercise intensity, we recommend the prescription of fixed intensities that serve the training purposes (e.g., integrated into the warm-up), without negatively impacting the subsequent session, and can be easily repeated over time (i.e., individual and resource constraints) | ||
| • | Because of the notable influence of individual and contextual factors, practitioners should consider administering intermittent-variable protocols (e.g., SSG) in combination with more generic SMFT, rather than isolation. For example, continuous SMFT during the warm-up and SSG within the main parts of the session. This may provide insight into general vs sport-specific training effects | ||
| • | When monitoring the internal response to intermittent-variable SMFT (e.g., SSG HRex), we recommend quantifying and, if possible, controlling for external intensity parameters. The latter should be sought through linear regression techniques, with ratios (e.g., internal:external) being avoided | ||
| HR-derived indices | |||
| • | HRex is the most viable SMFT outcome measure to evaluate an athlete’s physiological state, principally to monitor chronic aerobic-oriented training effects | ||
| • | Considering that similar changes in HR-derived indices can infer positive and negative training effects, researchers and practitioners are advised to include more than a single-outcome measure (e.g., HRex and RPE) and interpret the trends observed in relation to training aims and context | ||
| • | We recommend caution to practitioners when interpreting changes in cardiac parasympathetic outcome measures (e.g., HRR), given their direct link with exercise intensity (i.e., changes in HRex may influence HRR) | ||
| Subjective | |||
| • | RPE may provide a useful adjunct to objective SMFT outcome measures such as HRex or accelerometry-load measures for monitoring physiological state, but data must be collected in an appropriate and standardized manner (i.e., appropriate anchoring and education, correct scales, in isolation) to mitigate the influence of conscious bias and habitual ratings | ||
| • | The practicality of collecting SMFT RPE in the originally intended manner from groups of team-sport athletes (~ 20–40) is logistically challenging. However, this may be feasible if SMFT is performed as a discreet session that is not integrated within training, when working with individuals (e.g., small group training, or the rehabilitation return-to-play phase), or if data collection procedures are made more accessible (e.g., mobile applications, human resources) | ||
| • | Differential RPE (respiratory, muscular) may provide a more sensitive appraisal of perceived exertion in response to change in physiological state, but the utility of these measures requires further investigation | ||
| Mechanical | |||
| • | Monitoring locomotor outputs such as distance covered and high-intensity efforts during SSG displays a larger magnitude of measurement error and therefore may compromise their sensitivity. We suggest future work scrutinizing whether modifications in game constraints can reduce physical performance variability, or alternatively explore the utility of drill-based exercises such as passing drills | ||
| • | MEMS devices used within SMFT may be a promising tool to monitor lower limb neuromuscular status (fatigue and efficiency). However, before confident inferences can be made, further research is necessary to address their validity as markers of changes in running mechanics. The technology and the associated analytical techniques used, as well as other aspects such as the SMFT properties, outcome measures collected, and unit placement should be also considered | ||
HR heart rate, HRex heart rate exercise, HRR heart rate recovery, MEMS micro-electrical mechanical systems, RPE ratings of perceived exertion, SMFT submaximal fitness tests, SSG small-sided games
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the authors who provided additional data for the studies included in our review. We also thank the reviewers for their constructive comments and contributions.
Declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. No sources of funding were used to assist in the preparation of this article.
Conflict of interest
The authors have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Supplementary materials for this paper are also available on the Open Science Framework at https://osf.io/f9xwj/.
Code availability
Not applicable.
Authors’ contributions
TS conceived the idea for the article, performed the literature search and data analysis, and wrote the first draft of the manuscript and all subsequent versions. RL and SJM provided significant writing content and revisions to the manuscript. RL, SJM, MB, TJC, and SB contributed substantially to the conceptual direction and content and provided edits and feedback to the manuscript. All authors read and approved the final manuscript. TS coordinated the submission and revision process.
References
- 1.Impellizzeri FM, Menaspà P, Coutts AJ, et al. Training load and its role in injury prevention, part I: back to the future. J Athl Train. 2020;55:885–892. doi: 10.4085/1062-6050-500-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalkhoven JT, Watsford ML, Impellizzeri FM. A conceptual model and detailed framework for stress-related, strain-related, and overuse athletic injury. J Sci Med Sport. 2020;23:726–734. doi: 10.1016/j.jsams.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Vanrenterghem J, Nedergaard NJ, Robinson MA, et al. Training load monitoring in team sports: a novel framework separating physiological and biomechanical load-adaptation pathways. Sports Med. 2017;47:2135–2142. doi: 10.1007/s40279-017-0714-2. [DOI] [PubMed] [Google Scholar]
- 4.Jeffries AC, Marcora SM, Coutts AJ, et al. Development of a revised conceptual framework of physical training for use in research and practice. Sports Med. 2022;52(4):709–724. doi: 10.1007/s40279-021-01551-5. [DOI] [PubMed] [Google Scholar]
- 5.Buchheit M, Rabbani A. The 30–15 intermittent fitness test versus the Yo-Yo intermittent recovery test level 1: relationship and sensitivity to training. Int J Sports Physiol Perform. 2014;9:522–524. doi: 10.1123/ijspp.2012-0335. [DOI] [PubMed] [Google Scholar]
- 6.Bradley PS, Bendiksen M, Dellal A, et al. The application of the Yo-Yo Intermittent Endurance Level 2 Test to elite female soccer populations: Yo-Yo IE2 testing in female soccer players. Scand J Med Sci Sports. 2014;24:43–54. doi: 10.1111/j.1600-0838.2012.01483.x. [DOI] [PubMed] [Google Scholar]
- 7.Carling C, Lacome M, McCall A, et al. Monitoring of post-match fatigue in professional soccer: welcome to the real world. Sports Med. 2018;48:2695–2702. doi: 10.1007/s40279-018-0935-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lacome M, Simpson BM, Buchheit M. Monitoring training status with player-tracking technology: still on the road to Rome. Aspetar Sports Med J. 2018;7:54–63. [Google Scholar]
- 9.Norris D, Joyce D, Siegler J, et al. Considerations in interpreting neuromuscular state in elite level Australian Rules football players. J Sci Med Sport. 2021;24:702–708. doi: 10.1016/j.jsams.2021.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Buchheit M. Monitoring training status with HR measures: do all roads lead to Rome? Front Physiol. 2014;5:73. doi: 10.3389/fphys.2014.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buchheit M, Simpson BM, Lacome M. Monitoring cardiorespiratory fitness in professional soccer players: is it worth the prick? Int J Sports Physiol Perform. 2020;15:1437–1441. doi: 10.1123/ijspp.2019-0911. [DOI] [PubMed] [Google Scholar]
- 12.Scott TJ, McLaren SJ, Caia J, et al. The reliability and usefulness of an individualised submaximal shuttle run test in elite rugby league players. Sci Med Football. 2018;2:184–190. doi: 10.1080/24733938.2018.1448937. [DOI] [Google Scholar]
- 13.Bruce RA, Pearson R. Variability of respiratory and circulatory performance during standardized exercise. J Clin Invest. 1949;28:1431–1438. doi: 10.1172/jci102208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Åstrand P-O, Ryhming I. A nomogram for calculation of aerobic capacity (physical fitness) from pulse rate during submaximal work. J Appl Physiol. 1954;7:218–221. doi: 10.1152/jappl.1954.7.2.218. [DOI] [PubMed] [Google Scholar]
- 15.Bassey EJ, Fentem PH, MacDonald IC, et al. Self-paced walking as a method for exercise testing in elderly and young men. Clin Sci Mol Med. 1976;51:609–612. doi: 10.1042/cs0510609. [DOI] [PubMed] [Google Scholar]
- 16.Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 17.McGavin CR, Gupta SP, McHardy GJ. Twelve-minute walking test for assessing disability in chronic bronchitis. Br Med J. 1976;1:822–823. doi: 10.1136/bmj.1.6013.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kline GM, Porcari JP, Hintermeister R, et al. Estimation of VO2max from a one-mile track walk, gender, age, and body weight. Med Sci Sports Exerc. 1987;19:253–259. doi: 10.1249/00005768-198706000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Ebbeling CB, Ward A, Puleo EM, et al. Development of a single-stage submaximal treadmill walking test. Med Sci Sports Exerc. 1991;23:966–973. doi: 10.1249/00005768-199108000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Broman S, Wigertz O. Transient dynamics of ventilation and heart rate with step changes in work load from different load levels. Acta Physiol Scand. 1971;81:54–74. doi: 10.1111/j.1748-1716.1971.tb04877.x. [DOI] [PubMed] [Google Scholar]
- 21.Haber P, Schlick W, Schmid P, et al. Estimation of the performance spectrum of healthy adolescents by using the PWC 170 (Physical Work Capacity) Acta Med Austriaca. 1976;3:164–166. [PubMed] [Google Scholar]
- 22.Franks BD. YMCA youth fitness test manual. 6th ed. Champaign (IL): YMCA of the USA; 1989.
- 23.Singh SJ, Morgan MD, Scott S, et al. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax. 1992;47:1019–1024. doi: 10.1136/thx.47.12.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bruce RA. Exercise testing of patients with coronary heart disease: principles and normal standards for evaluation. Ann Clin Res. 1971;3:323–332. [PubMed] [Google Scholar]
- 25.Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85:546–562. doi: 10.1016/0002-8703(73)90502-4. [DOI] [PubMed] [Google Scholar]
- 26.Ghosh AK. Anaerobic threshold: its concept and role in endurance sport. Malays J Med Sci. 2004;11:24–36. [PMC free article] [PubMed] [Google Scholar]
- 27.Wasserman K. The anaerobic threshold: definition, physiological significance and identification. Adv Cardiol. 1986;35:1–23. [PubMed] [Google Scholar]
- 28.Barbeau P, Serresse O, Boulay MR. Using maximal and submaximal aerobic variables to monitor elite cyclists during a season. Med Sci Sports Exerc. 1993;25:1062–1069. doi: 10.1249/00005768-199309000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Urhausen A, Gabriel H, Weiler B, et al. Ergometric and psychological findings during overtraining: a long-term follow-up study in endurance athletes. Intl J Sports Med. 1998;19:114–120. doi: 10.1055/s-2007-971892. [DOI] [PubMed] [Google Scholar]
- 30.Halson SL, Bridge MW, Meeusen R, et al. Time course of performance changes and fatigue markers during intensified training in trained cyclists. J Appl Physiol. 2002;93:947–956. doi: 10.1152/japplphysiol.01164.2001. [DOI] [PubMed] [Google Scholar]
- 31.Jeukendrup A, Hesselink M, Snyder A, et al. Physiological changes in male competitive cyclists after two weeks of intensified training. Int J Sports Med. 1992;13:534–541. doi: 10.1055/s-2007-1021312. [DOI] [PubMed] [Google Scholar]
- 32.Lamberts RP, Swart J, Noakes TD, et al. A novel submaximal cycle test to monitor fatigue and predict cycling performance. Br J Sports Med. 2011;45:797–804. doi: 10.1136/bjsm.2009.061325. [DOI] [PubMed] [Google Scholar]
- 33.Wallace LK, Slattery KM, Coutts AJ. A comparison of methods for quantifying training load: relationships between modelled and actual training responses. Eur J Appl Physiol. 2014;114:11–20. doi: 10.1007/s00421-013-2745-1. [DOI] [PubMed] [Google Scholar]
- 34.Vesterinen V, Nummela A, Äyrämö S, et al. Monitoring training adaptation with a submaximal running test under field conditions. Int J Sports Physiol Perform. 2016;11:393–399. doi: 10.1123/ijspp.2015-0366. [DOI] [PubMed] [Google Scholar]
- 35.Vesterinen V, Nummela A, Laine T, et al. A submaximal running test with postexercise cardiac autonomic and neuromuscular function in monitoring endurance training adaptation. J Strength Cond Res. 2017;31:233–243. doi: 10.1519/JSC.0000000000001458. [DOI] [PubMed] [Google Scholar]
- 36.Aubry A, Hausswirth C, Louis J, et al. The development of functional overreaching is associated with a faster heart rate recovery in endurance athletes. PLoS ONE. 2015;10:e0139754. doi: 10.1371/journal.pone.0139754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Le Meur Y, Buchheit M, Aubry A, et al. Assessing overreaching with heart-rate recovery: what is the minimal exercise intensity required? Int J Sports Physiol Perform. 2017;12:569–573. doi: 10.1123/ijspp.2015-0675. [DOI] [PubMed] [Google Scholar]
- 38.Bosquet L, Merkari S, Arvisais D, et al. Is heart rate a convenient tool to monitor over-reaching? A systematic review of the literature. Br J Sports Med. 2008;42:709–714. doi: 10.1136/bjsm.2007.042200. [DOI] [PubMed] [Google Scholar]
- 39.Daanen HAM, Lamberts RP, Kallen VL, et al. A systematic review on heart-rate recovery to monitor changes in training status in athletes. Int J Sports Physiol Perform. 2012;7:251–260. doi: 10.1123/ijspp.7.3.251. [DOI] [PubMed] [Google Scholar]
- 40.Capostagno B, Lambert MI, Lamberts RP. Analysis of a submaximal cycle test to monitor adaptations to training: implications for optimizing training prescription. J Strength Cond Res. 2021;35:924–930. doi: 10.1519/jsc.0000000000003227. [DOI] [PubMed] [Google Scholar]
- 41.Decroix L, Lamberts RP, Meeusen R. Can the Lamberts and Lambert Submaximal Cycle Test reflect overreaching in professional cyclists? Int J Sports Physiol Perform. 2018;13:23–28. doi: 10.1123/ijspp.2016-0685. [DOI] [PubMed] [Google Scholar]
- 42.Schneider C, Hanakam F, Wiewelhove T, et al. Heart rate monitoring in team sports: a conceptual framework for contextualizing heart rate measures for training and recovery prescription. Front Physiol. 2018;9:639. doi: 10.3389/fphys.2018.00639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Akenhead R, Nassis GP. Training load and player monitoring in high-level football: current practice and perceptions. Int J Sports Physiol Perform. 2016;11:587–593. doi: 10.1123/ijspp.2015-0331. [DOI] [PubMed] [Google Scholar]
- 44.Taylor K-L, Chapman DW, Cronin JB, et al. Fatigue monitoring in high performance sport: a survey of current trends. J Aust Strength Cond. 2012;20:12–23. [Google Scholar]
- 45.Buchheit M, Mendez-Villanueva A, Quod MJ, et al. Determinants of the variability of heart rate measures during a competitive period in young soccer players. Eur J Appl Physiol. 2010;109:869–878. doi: 10.1007/s00421-010-1422-x. [DOI] [PubMed] [Google Scholar]
- 46.Mohr M, Krustrup P. Yo-Yo intermittent recovery test performances within an entire football league during a full season. J Sports Sci. 2014;32:315–327. doi: 10.1080/02640414.2013.824598. [DOI] [PubMed] [Google Scholar]
- 47.Thorpe RT, Strudwick AJ, Buchheit M, et al. Tracking morning fatigue status across in-season training weeks in elite soccer players. Int J Sports Physiol Perform. 2016;11:947–952. doi: 10.1123/ijspp.2015-0490. [DOI] [PubMed] [Google Scholar]
- 48.Veugelers KR, Naughton GA, Duncan CS, et al. Validity and reliability of a submaximal intermittent running test in elite Australian football players. J Strength Cond Res. 2016;30:3347–3353. doi: 10.1519/jsc.0000000000001441. [DOI] [PubMed] [Google Scholar]
- 49.Buchheit M, Lacome M, Cholley Y, et al. Neuromuscular responses to conditioned soccer sessions assessed via GPS-embedded accelerometers: insights into tactical periodization. Int J Sports Physiol Perform. 2018;13:577–583. doi: 10.1123/ijspp.2017-0045. [DOI] [PubMed] [Google Scholar]
- 50.Haddad M, Chaouachi A, Wong DP, et al. Influence of fatigue, stress, muscle soreness and sleep on perceived exertion during submaximal effort. Physiol Behav. 2013;119:185–189. doi: 10.1016/j.physbeh.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 51.Hulin BT, Gabbett TJ, Johnston RD, et al. Sub-maximal heart rate is associated with changes in high-intensity intermittent running ability in professional rugby league players. Sci Med Football. 2019;3:50–56. doi: 10.1080/24733938.2018.1475748. [DOI] [Google Scholar]
- 52.Leduc C, Tee J, Lacome M, et al. Convergent validity, reliability, and sensitivity of a running test to monitor neuromuscular fatigue. Int J Sports Physiol Perform. 2020;15:1067–1073. doi: 10.1123/ijspp.2019-0319. [DOI] [PubMed] [Google Scholar]
- 53.Thorpe RT, Strudwick AJ, Buchheit M, et al. Monitoring fatigue during the in-season competitive phase in elite soccer players. Int J Sports Physiol Perform. 2015;10:958–964. doi: 10.1123/ijspp.2015-0004. [DOI] [PubMed] [Google Scholar]
- 54.Malone S, Hughes B, Roe M, et al. Monitoring player fitness, fatigue status and running performance during an in-season training camp in elite Gaelic football. Sci Med Football. 2017;1:229–236. doi: 10.1080/24733938.2017.1361040. [DOI] [Google Scholar]
- 55.Buchheit M, Cholley Y, Lambert P. Psychometric and physiological responses to a preseason competitive camp in the heat with a 6-hour time difference in elite soccer players. Int J Sports Physiol Perform. 2016;11:176–181. doi: 10.1123/ijspp.2015-0135. [DOI] [PubMed] [Google Scholar]
- 56.Buchheit M, Simpson BM, Garvican-Lewis LA, et al. Wellness, fatigue and physical performance acclimatisation to a 2-week soccer camp at 3600 m (ISA3600) Br J Sports Med. 2013;47:i100–i106. doi: 10.1136/bjsports-2013-092749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Buchheit M, Voss SC, Nybo L, et al. Physiological and performance adaptations to an in-season soccer camp in the heat: associations with heart rate and heart rate variability: monitoring responses to training in the heat. Scand J Med Sci Sports. 2011;21:e477–e485. doi: 10.1111/j.1600-0838.2011.01378.x. [DOI] [PubMed] [Google Scholar]
- 58.Buchheit M, Morgan W, Wallace J, et al. Physiological, psychometric, and performance effects of the Christmas break in Australian football. Int J Sports Physiol Perform. 2015;10:120–123. doi: 10.1123/ijspp.2014-0082. [DOI] [PubMed] [Google Scholar]
- 59.de Freitas VH, Pereira LA, de Souza EA, et al. Sensitivity of the Yo-Yo Intermittent Recovery Test and cardiac autonomic responses to training in Futsal players. Int J Sports Physiol Perform. 2015;10:553–558. doi: 10.1123/ijspp.2014-0365. [DOI] [PubMed] [Google Scholar]
- 60.Aoki MS, Ronda LT, Marcelino PR, et al. Monitoring training loads in professional basketball players engaged in a periodized training program. J Strength Cond Res. 2017;31:348–358. doi: 10.1519/jsc.0000000000001507. [DOI] [PubMed] [Google Scholar]
- 61.Buchheit M, Millet GP, Parisy A, et al. Supramaximal training and postexercise parasympathetic reactivation in adolescents. Med Sci Sports Exerc. 2008;40:362–371. doi: 10.1249/mss.0b013e31815aa2ee. [DOI] [PubMed] [Google Scholar]
- 62.DiffSense. Continuous vs intermittent: what is the difference? 2021. Available from: https://diffsense.com/diff/continuous/intermittent. [Accessed 15 Jan 2021].
- 63.Christensen EH, Rune H, Bengt S. Intermittent and continuous running (a further contribution to the physiology of intermittent work.). Acta Physiol Scand. 1960;50:269–86. 10.1111/j.1748-1716.1960.tb00181.x. [DOI] [PubMed]
- 64.Encyclopedia.com. Exercise, intermittent. 2021. Available from: https://www.encyclopedia.com/sports/sports-fitness-recreation-and-leisure-magazines/exercise-intermittent. [Accessed 15 Jan 2021].
- 65.Fitzpatrick JF, Hicks KM, Russell M, et al. The reliability of potential fatigue-monitoring measures in elite youth soccer players. Strength Cond Res. 2021;35:3448–3452. doi: 10.1519/JSC.0000000000003317. [DOI] [PubMed] [Google Scholar]
- 66.Rabbani A, Kargarfard M, Twist C. Reliability and validity of a submaximal warm-up test for monitoring training status in professional soccer players. J Strength Cond Res. 2018;32:326–333. doi: 10.1519/jsc.0000000000002335. [DOI] [PubMed] [Google Scholar]
- 67.Castagna C, Manzi V, Impellizzeri F, et al. Validity of an on-court lactate threshold test in young basketball players. J Strength Cond Res. 2010;24:2434–2439. doi: 10.1519/JSC.0b013e3181e2e1bf. [DOI] [PubMed] [Google Scholar]
- 68.Garrett J, Graham SR, Eston RG, et al. A novel method of assessment for monitoring neuromuscular fatigue in Australian Rules football players. Int J Sports Physiol Perform. 2019;14:598–605. doi: 10.1123/ijspp.2018-0253. [DOI] [PubMed] [Google Scholar]
- 69.Buchheit M, Lefebvre B, Laursen PB, et al. Reliability, usefulness, and validity of the 30–15 Intermittent Ice Test in young elite ice hockey players. J Strength Cond Res. 2011;25:1457–1464. doi: 10.1519/jsc.0b013e3181d686b7. [DOI] [PubMed] [Google Scholar]
- 70.Iacono AD, Beato M, Unnithan V. Comparative effects of game profile-based training and small-sided games on physical performance of elite young soccer players. J Strength Cond Res. 2019;9. 10.1519/jsc.0000000000003225. [DOI] [PubMed]
- 71.Lacome M, Simpson B, Broad N, et al. Monitoring players’ readiness using predicted heart-rate responses to soccer drills. Int J Sports Physiol Perform. 2018;13:1273–1280. doi: 10.1123/ijspp.2018-0026. [DOI] [PubMed] [Google Scholar]
- 72.Rowell AE, Aughey RJ, Clubb J, et al. A standardized small sided game can be used to monitor neuromuscular fatigue in professional A-League football players. Front Physiol. 2018;9:1011. doi: 10.3389/fphys.2018.01011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Scott TJ. Testing, prescribing and monitoring training in team sports: the efficiency and versatility of the 30–15 Intermittent Fitness Test. Sport Perform Sci Rep. 2018;5.
- 74.Delisle-Houde P, Reid RER, Insogna JA, et al. Seasonal changes in physiological responses and body composition during a competitive season in male and female elite collegiate ice hockey players. J Strength Cond Res. 2019;33:2162–2169. doi: 10.1519/jsc.0000000000002338. [DOI] [PubMed] [Google Scholar]
- 75.Dillern T. Markers of the aerobic energy-delivery system as measures of post-match fatigue and recovery in soccer; a repeated measures design. Asian J Sports Med. 2017;8. 10.5812/asjsm.14425.
- 76.Dobbin N, Moss SL, Highton J, et al. An examination of a modified Yo-Yo test to measure intermittent running performance in rugby players. Eur J Sport Sci. 2018;18:1068–1076. doi: 10.1080/17461391.2018.1475509. [DOI] [PubMed] [Google Scholar]
- 77.Ferioli D, Bosio A, La Torre A, et al. Different training loads partially influence physiological responses to the preparation period in basketball. J Strength Cond Res. 2018;32:790–797. doi: 10.1519/jsc.0000000000001823. [DOI] [PubMed] [Google Scholar]
- 78.Iaia FM, Fiorenza M, Larghi L, et al. Short- or long-rest intervals during repeated-sprint training in soccer? PLoS ONE. 2017;12:e0171462. doi: 10.1371/journal.pone.0171462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Reinhardt L, Schulze S, Kurz E, et al. An investigation into the relationship between heart rate recovery in small-sided games and endurance performance in male, semi-professional soccer players. Sports Med Open. 2020;6:43. doi: 10.1186/s40798-020-00273-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rampinini E, Donghi F, Martin M, et al. Impact of COVID-19 lockdown on Serie A soccer players’ physical qualities. Int J Sports Med. 2021;2:917–923. doi: 10.1055/a-1345-9262. [DOI] [PubMed] [Google Scholar]
- 81.Owen AL, Wong DP, Paul D, et al. Effects of a periodized small-sided game training intervention on physical performance in elite professional soccer. J Strength Cond Res. 2012;26:2748–2754. doi: 10.1519/jsc.0b013e318242d2d1. [DOI] [PubMed] [Google Scholar]
- 82.Signorelli GR, Perim RR, Santos TM, et al. A pre-season comparison of aerobic fitness and flexibility of younger and older professional soccer players. Int J Sports Med. 2012;33:867–872. doi: 10.1055/s-0032-1311597. [DOI] [PubMed] [Google Scholar]
- 83.Altmann S, Neumann R, Härtel S, et al. Using submaximal exercise heart rate for monitoring cardiorespiratory fitness changes in professional soccer players: a replication study. Int J Sports Physiol Perform. 2021;16:1096–1102. doi: 10.1123/ijspp.2020-0554. [DOI] [PubMed] [Google Scholar]
- 84.Bradley PS, Mohr M, Bendiksen M, et al. Sub-maximal and maximal Yo–Yo intermittent endurance test level 2: heart rate response, reproducibility and application to elite soccer. Eur J Appl Physiol. 2011;111:969–978. doi: 10.1007/s00421-010-1721-2. [DOI] [PubMed] [Google Scholar]
- 85.Brink MS, Visscher C, Coutts AJ, et al. Changes in perceived stress and recovery in overreached young elite soccer players: stress and recovery in overreaching. Scand J Med Sci Sports. 2012;22:285–292. doi: 10.1111/j.1600-0838.2010.01237.x. [DOI] [PubMed] [Google Scholar]
- 86.Brink MS, Nederhof E, Visscher C, et al. Monitoring load, recovery, and performance in young elite soccer players. J Strength Cond Res. 2010;24:597–603. doi: 10.1519/jsc.0b013e3181c4d38b. [DOI] [PubMed] [Google Scholar]
- 87.Brink MS, Visscher C, Schmikli SL, et al. Is an elevated submaximal heart rate associated with psychomotor slowness in young elite soccer players? Eur J Sport Sci. 2013;13:207–214. doi: 10.1080/17461391.2011.630101. [DOI] [Google Scholar]
- 88.Dobbin N, Highton J, Moss SL, et al. The effects of in-season, low-volume sprint interval training with and without sport-specific actions on the physical characteristics of Elite Academy rugby league players. Int J Sports Physiol Perform. 2020;15:705–713. doi: 10.1123/ijspp.2019-0165. [DOI] [PubMed] [Google Scholar]
- 89.Doncaster G, Scott M, Iga J, et al. Reliability of heart rate responses both during and following a 6 min Yo-Yo IR1 test in highly trained youth soccer players. Sci Med Football. 2019;3:14–20. doi: 10.1080/24733938.2018.1476775. [DOI] [Google Scholar]
- 90.Dubois R, Lyons M, Paillard T, et al. Influence of weekly workload on physical, biochemical and psychological characteristics in professional rugby union players over a competitive season. J Strength Cond Res. 2020;34:527–545. doi: 10.1519/jsc.0000000000002741. [DOI] [PubMed] [Google Scholar]
- 91.Fanchini M, Schena F, Castagna C, et al. External responsiveness of the Yo-Yo IR Test Level 1 in high-level male soccer players. Int J Sports Med. 2015;36:735–741. doi: 10.1055/s-0035-1547223. [DOI] [PubMed] [Google Scholar]
- 92.Fanchini M, Castagna C, Coutts AJ, et al. Are the Yo-Yo intermittent recovery test levels 1 and 2 both useful? Reliability, responsiveness and interchangeability in young soccer players. J Sports Sci. 2014;32:1950–1957. doi: 10.1080/02640414.2014.969295. [DOI] [PubMed] [Google Scholar]
- 93.Garvican LA, Hammond K, Varley MC, et al. Lower running performance and exacerbated fatigue in soccer played at 1600 m. Int J Sports Physiol Perform. 2014;9:397–404. doi: 10.1123/ijspp.2012-0375. [DOI] [PubMed] [Google Scholar]
- 94.Hulka K, Weisser R, Belka J, et al. Stability of internal response and external load during 4-a-side football game in an indoor environment. Acta Gymnica. 2015;45:21–25. doi: 10.5507/ag.2015.003. [DOI] [Google Scholar]
- 95.Hulse M, Morris J, Hawkins R, et al. A field-test battery for elite, young soccer players. Int J Sports Med. 2012;34:302–311. doi: 10.1055/s-0032-1312603. [DOI] [PubMed] [Google Scholar]
- 96.Ingebrigtsen J, Bendiksen M, Randers MB, et al. Yo-Yo IR2 testing of elite and sub-elite soccer players: performance, heart rate response and correlations to other interval tests. J Sports Sci. 2012;30:1337–1345. doi: 10.1080/02640414.2012.711484. [DOI] [PubMed] [Google Scholar]
- 97.Natera AOW, Jennings J, Oakley AJ, et al. Influence of environmental conditions on performance and heart rate responses to the 30–15 Incremental Fitness Test in rugby union athletes. J Strength Cond Res. 2019;33:486–491. doi: 10.1519/jsc.0000000000001865. [DOI] [PubMed] [Google Scholar]
- 98.Owen AL, Newton M, Shovlin A, et al. The use of small-sided games as an aerobic fitness assessment supplement within elite level professional soccer. J Hum Kinet. 2020;71:243–253. doi: 10.2478/hukin-2019-0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Owen C, Jones P, Comfort P. The reliability of the submaximal version of the Yo-Yo intermittent recovery test in elite youth soccer. J Train. 2017;6:31–34. doi: 10.17338/trainology.6.1_31. [DOI] [Google Scholar]
- 100.Pereira LA, Abad CCC, Leiva DF, et al. Relationship between resting heart rate variability and intermittent endurance performance in novice soccer players. Res Q Exerc Sport. 2019;90:355–361. doi: 10.1080/02701367.2019.1601666. [DOI] [PubMed] [Google Scholar]
- 101.Younesi S, Rabbani A, Manuel Clemente F, et al. Session-to-session variations of internal load during different small-sided games: a study in professional soccer players. Res Sports Med. 2021;29:462–474. doi: 10.1080/15438627.2021.1888103. [DOI] [PubMed] [Google Scholar]
- 102.Cornforth DJ, Robinson DJ, Spence I, et al. Heart rate recovery in decision support for high performance athlete training schedules. IJIKM. 2014;9:193–207. doi: 10.28945/2085. [DOI] [Google Scholar]
- 103.Moreira A, Machado DG da S, Moscaleski L, et al. Effect of tDCS on well-being and autonomic function in professional male players after official soccer matches. Physiol Behav. 2021;233:113351. 10.1016/j.physbeh.2021.113351. [DOI] [PubMed]
- 104.Meylan CMP, Bowman K, Stellingwerff T, et al. The efficacy of heat acclimatization pre-World Cup in female soccer players. Front Sports Act Living. 2021;3:614370. doi: 10.3389/fspor.2021.614370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Araújo M, Baumgart C, Freiwald J, et al. Contrasts in intermittent endurance performance and heart rate response between female and male soccer players of different playing levels. Biol Sport. 2019;36:323–331. doi: 10.5114/biolsport.2019.88755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Buchheit M, Racinais S, Bilsborough JC, et al. Monitoring fitness, fatigue and running performance during a pre-season training camp in elite football players. J Sci Med Sport. 2013;16:550–555. doi: 10.1016/j.jsams.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 107.Buchheit M, Simpson MB, Al Haddad H, et al. Monitoring changes in physical performance with heart rate measures in young soccer players. Eur J Appl Physiol. 2012;112:711–723. doi: 10.1007/s00421-011-2014-0. [DOI] [PubMed] [Google Scholar]
- 108.Buchheit M, Simpson BM, Schmidt WF, et al. Predicting sickness during a 2-week soccer camp at 3600 m (ISA3600) Br J Sports Med. 2013;47:i124–i127. doi: 10.1136/bjsports-2013-092757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Deprez D, Fransen J, Lenoir M, et al. The Yo-Yo intermittent recovery test level 1 is reliable in young high-level soccer players. Biol Sport. 2015;32:65–70. doi: 10.5604/20831862.1127284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Deprez D, Coutts AJ, Lenoir M, et al. Reliability and validity of the Yo-Yo intermittent recovery test level 1 in young soccer players. J Sports Sci. 2014;32:903–910. doi: 10.1080/02640414.2013.876088. [DOI] [PubMed] [Google Scholar]
- 111.Francini L, Rampinini E, Bosio A, et al. Association between match activity, endurance levels and maturity in youth football players. Int J Sports Med. 2019;40:576–584. doi: 10.1055/a-0938-5431. [DOI] [PubMed] [Google Scholar]
- 112.Lignell E, Fransson D, Krustrup P, et al. Analysis of high-intensity skating in top-class ice hockey match-play in relation to training status and muscle damage. J Strength Cond Res. 2018;32:1303–1310. doi: 10.1519/jsc.0000000000001999. [DOI] [PubMed] [Google Scholar]
- 113.Rabbani A, Kargarfard M, Twist C. Fitness monitoring in elite soccer players: group vs. individual analyses. J Strength Cond Res. 2020;34:3250–7. 10.1519/jsc.0000000000002700. [DOI] [PubMed]
- 114.Thorpe RT, Strudwick AJ, Buchheit M, et al. The influence of changes in acute training load on daily sensitivity of morning-measured fatigue variables in elite soccer players. Int J Sports Physiol Perform. 2017;12:S2–107-S2–113. 10.1123/ijspp.2016-0433. [DOI] [PubMed]
- 115.Vigh-Larsen JF, Beck JH, Daasbjerg A, et al. Fitness characteristics of elite and subelite male ice hockey players: a cross-sectional study. J Strength Cond Res. 2019;33:2352–2360. doi: 10.1519/jsc.0000000000003285. [DOI] [PubMed] [Google Scholar]
- 116.Younesi S, Rabbani A, Clemente FM, et al. Relationships between aerobic performance, hemoglobin levels, and training load during small-sided games: a study in professional soccer players. Front Physiol. 2021;12:649870. doi: 10.3389/fphys.2021.649870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Nakamura FY, Pereira LA, Moraes JE, et al. Physical and physiological differences of backs and forwards from the Brazilian national rugby union team. J Sports Med Phys Fitness. 2017;57:1549–1556. doi: 10.23736/s0022-4707.16.06751-7. [DOI] [PubMed] [Google Scholar]
- 118.Hulin BT, Gabbett TJ, Pickworth NJ, et al. Relationships among PlayerLoad, high-intensity intermittent running ability, and injury risk in professional rugby league players. Int J Sports Physiol Perform. 2020;15:423–429. doi: 10.1123/ijspp.2019-0139. [DOI] [PubMed] [Google Scholar]
- 119.Ryan S, Pacecca E, Tebble J, et al. Measurement characteristics of athlete monitoring tools in professional Australian football. Int J Sports Physiol Perform. 2019;1–7. 10.1123/ijspp.2019-0060. [DOI] [PubMed]
- 120.Rago V, Krustrup P, Martín-Acero R, et al. Training load and submaximal heart rate testing throughout a competitive period in a top-level male football team. J Sports Sci. 2020;38:1408–1415. doi: 10.1080/02640414.2019.1618534. [DOI] [PubMed] [Google Scholar]
- 121.Fox R, Patterson SD, Waldron M. The relationship between heart rate recovery and temporary fatigue of kinematic and energetic indices among soccer players. Sci Med Football. 2017;1:132–138. doi: 10.1080/24733938.2017.1329590. [DOI] [Google Scholar]
- 122.Ingebrigtsen J, Brochmann M, Castagna C, et al. Relationships between field performance tests in high-level soccer players. J Strength Cond Res. 2014;28:942–949. doi: 10.1519/jsc.0b013e3182a1f861. [DOI] [PubMed] [Google Scholar]
- 123.Harry K, Booysen MJ. Faster heart rate recovery correlates with high-intensity match activity in female field hockey players: training implications. J Strength Cond Res. 2020;34:1150–1157. doi: 10.1519/jsc.0000000000003073. [DOI] [PubMed] [Google Scholar]
- 124.Starling LT, Nellemann S, Parkes A, et al. The sensitivity of the Fatigue and Fitness Test for Teams (FFITT) to measure the demands of a rugby match. Eur J Sport Sci. 2021;21:803–810. doi: 10.1080/17461391.2020.1780327. [DOI] [PubMed] [Google Scholar]
- 125.Prajapat A, Ahmad I, Khan Z, et al. Cardiac autonomic profile of soccer, field hockey and basketball players: a comparative study. Asian J Sports Med. 2018;9. 10.5812/asjsm.62492.
- 126.Vachon A, Berryman N, Mujika I, et al. Tapering and repeated high-intensity effort ability in young elite rugby union players: influence of pretaper fatigue level. Int J Sports Physiol Perform. 2021;16:993–1000. doi: 10.1123/ijspp.2020-0639. [DOI] [PubMed] [Google Scholar]
- 127.Ernst G. Heart-rate variability: more than heart beats? Front Public Health. 2017;5:240. doi: 10.3389/fpubh.2017.00240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Stone NM, Kilding AE. Aerobic conditioning for team sport athletes. Sports Med. 2009;39:615–642. doi: 10.2165/00007256-200939080-00002. [DOI] [PubMed] [Google Scholar]
- 129.Kuipers H, Keizer HA. Overtraining in elite athletes: review and directions for the future. Sports Med. 1988;6:79–92. doi: 10.2165/00007256-198806020-00003. [DOI] [PubMed] [Google Scholar]
- 130.ten Haaf T, Foster C, Meeusen R, et al. Submaximal heart rate seems inadequate to prescribe and monitor intensified training. Eur J Sport Sci. 2019;19:1082–1091. doi: 10.1080/17461391.2019.1571112. [DOI] [PubMed] [Google Scholar]
- 131.Laursen P, Buchheit M, editors. Science and application of high-intensity interval training. Champaign, IL, USA: Human Kinetics; 2019.
- 132.Racinais S, Buchheit M, Bilsborough J, et al. Physiological and performance responses to a training camp in the heat in professional Australian football players. Int J Sports Physiol Perform. 2014;9:598–603. doi: 10.1123/ijspp.2013-0284. [DOI] [PubMed] [Google Scholar]
- 133.Pryor JL, Johnson EC, Roberts WO, et al. Application of evidence-based recommendations for heat acclimation: individual and team sport perspectives. Temperature. 2019;6:37–49. doi: 10.1080/23328940.2018.1516537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Racinais S, Alonso JM, Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Br J Sports Med. 2015;49:1164–1173. doi: 10.1111/sms.12467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Garrett JM, Gunn R, Eston RG, et al. The effects of fatigue on the running profile of elite team sport athletes: a systematic review and meta-analysis. J Sports Med Phys Fitness. 2019;59:1328. doi: 10.23736/s0022-4707.19.09356-3. [DOI] [PubMed] [Google Scholar]
- 136.McLaren SJ, Macpherson TW, Coutts AJ, et al. The relationships between internal and external measures of training load and intensity in team sports: a meta-analysis. Sports Med. 2018;48:641–658. doi: 10.1007/s40279-017-0830-z. [DOI] [PubMed] [Google Scholar]
- 137.Akubat I, Barrett S, Abt G. Integrating the internal and external training loads in soccer. Int J Sports Physiol Perform. 2014;9:457–462. doi: 10.1123/ijspp.2012-0347. [DOI] [PubMed] [Google Scholar]
- 138.Atkinson G, Batterham AM. The use of ratios and percentage changes in sports medicine: time for a rethink? Int J Sports Med. 2012;33:505–506. doi: 10.1055/s-0032-1316355. [DOI] [PubMed] [Google Scholar]
- 139.Wiseman RM. On the use and misuse of ratios in strategic management research. In: Bergh DD, editor. Research methodology in strategy and management. Bing: Emerald Group Publishing Limited; 2009. pp. 75–110. [Google Scholar]
- 140.Coyne JOC, Gregory Haff G, Coutts AJ, et al. The current state of subjective training load monitoring: a practical perspective and call to action. Sports Med Open. 2018;4:58. doi: 10.1186/s40798-018-0172-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Jeffries AC, Wallace L, Coutts AJ, et al. Athlete-reported outcome measures for monitoring training responses: a systematic review of risk of bias and measurement property quality according to the COSMIN guidelines. Int J Sports Physiol Perform. 2020;15:1203–1215. doi: 10.1123/ijspp.2020-0386. [DOI] [PubMed] [Google Scholar]
- 142.McLaren S, Coutts A, Impellizzeri FM. Perception of effort and subjective monitoring. In: French D, Ronda LT, (editors) NSCA’s essentials of sport science. Champaign, IL, USA: Human Kinetics, Inc.; 2022: p. 231–54.
- 143.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. doi: 10.1249/00005768-198205000-00012. [DOI] [PubMed] [Google Scholar]
- 144.Chen MJ, Fan X, Moe ST. Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: a meta-analysis. J Sports Sci. 2002;20:873–899. doi: 10.1080/026404102320761787. [DOI] [PubMed] [Google Scholar]
- 145.Lea JWD, O’Driscoll JM, Coleman DA, et al. Validity and reliability of the ‘Isometric Exercise Scale’ (IES) for measuring ratings of perceived exertion during continuous isometric exercise. Sci Rep. 2021;11:5334. doi: 10.1038/s41598-021-84803-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pageaux B. Perception of effort in exercise science: definition, measurement and perspectives. Eur J Sport Sci. 2016;16:885–894. doi: 10.1080/17461391.2016.1188992. [DOI] [PubMed] [Google Scholar]
- 147.Halperin I, Emanuel A. Rating of perceived effort: methodological concerns and future directions. Sports Med. 2020;50:679–687. doi: 10.1007/s40279-019-01229-z. [DOI] [PubMed] [Google Scholar]
- 148.Sangan HF, Hopker JG, Davison G, et al. The self-paced submaximal run test: associations with the graded exercise test and reliability. Int J Sports Physiol Perform. 2021;16:1865–1873. doi: 10.1123/ijspp.2020-0904. [DOI] [PubMed] [Google Scholar]
- 149.Lovell R, Halley S, Siegler J, et al. Use of numerically blinded ratings of perceived exertion in soccer: assessing concurrent and construct validity. Int J Sports Physiol Perform. 2020;15:1430–1436. doi: 10.1123/ijspp.2019-0740. [DOI] [PubMed] [Google Scholar]
- 150.Micklewright D, St Clair Gibson A, Gladwell V, et al. Development and validity of the Rating-of-Fatigue Scale. Sports Med. 2017;47:2375–93. 10.1007/s40279-017-0711-5. [DOI] [PMC free article] [PubMed]
- 151.McLaren SJ, Taylor JM, Macpherson TW, et al. Systematic reductions in differential ratings of perceived exertion across a 2-week repeated-sprint-training intervention that improved soccer players’ high-speed-running abilities. Int J Sports Physiol Perform. 2020;15:1414–1421. doi: 10.1123/ijspp.2019-0568. [DOI] [PubMed] [Google Scholar]
- 152.Winter EM, Abt G, Brookes FBC, et al. Misuse of “power” and other mechanical terms in sport and exercise science research. J Strength Cond Res. 2016;30:292–300. doi: 10.1519/jsc.0000000000001101. [DOI] [PubMed] [Google Scholar]
- 153.Bourdon PC, Cardinale M, Murray A, et al. Monitoring athlete training loads: consensus statement. Int J Sports Physiol Perform. 2017;12:S2–161-S2–170. 10.1123/ijspp.2017-0208. [DOI] [PubMed]
- 154.Buchheit M, Simpson BM. Player-tracking technology: half-full or half-empty glass? Int J Sports Physiol Perform. 2017;12:S2–35-S2–41. 10.1123/ijspp.2016-0499. [DOI] [PubMed]
- 155.Nikolaidis PT, Busko K, Afonso J, et al. The effect of maturity on heart rate responses during training and testing in postpubescent female volleyball players. Hum Physiol. 2015;41:636–643. doi: 10.7868/s0131164615060053. [DOI] [PubMed] [Google Scholar]
- 156.Younesi S, Rabbani A, Clemente F, et al. Session-to-session variations in external load measures during small-sided games in professional soccer players. Biol Sport. 2021;38:185–193. doi: 10.5114/biolsport.2020.98449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Clemente FM, Rabbani A, Kargarfard M, et al. Session-to-session variations of external load measures of youth soccer players in medium-sided games. Int J Environ Res Public Health. 2019;16:3612. doi: 10.3390/ijerph16193612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Malone JJ, Lovell R, Varley MC, et al. Unpacking the black box: applications and considerations for using GPS devices in sport. Int J Sports Physiol Perform. 2017;12:S2–18-S2–26. 10.1123/ijspp.2016-0236. [DOI] [PubMed]
- 159.Verheul J, Nedergaard NJ, Vanrenterghem J, et al. Measuring biomechanical loads in team sports: from lab to field. Sci Med Football. 2020;4:246–252. doi: 10.1080/24733938.2019.1709654. [DOI] [Google Scholar]
- 160.Barrett S, Midgley AW, Towlson C, et al. Within-match PlayerLoad™ patterns during a simulated soccer match: potential implications for unit positioning and fatigue management. Int J Sports Physiol Perform. 2016;11:135–140. doi: 10.1123/ijspp.2014-0582. [DOI] [PubMed] [Google Scholar]
- 161.Buchheit M, Gray A, Morin J-B. Assessing stride variables and vertical stiffness with GPS-embedded accelerometers: preliminary insights for the monitoring of neuromuscular fatigue on the field. J Sports Sci Med. 2015;14:698–701. [PMC free article] [PubMed] [Google Scholar]
- 162.Cormack SJ, Mooney MG, Morgan W, et al. Influence of neuromuscular fatigue on accelerometer load in elite Australian football players. Int J Sports Physiol Perform. 2013;8:373–378. doi: 10.1123/ijspp.8.4.373. [DOI] [PubMed] [Google Scholar]
- 163.Hobara H, Inoue K, Gomi K, et al. Continuous change in spring-mass characteristics during a 400m sprint. J Sci Med Sport. 2010;13:256–261. doi: 10.1016/j.jsams.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 164.Brughelli M, Cronin J. A review of research on the mechanical stiffness in running and jumping: methodology and implications: mechanical stiffness. Scand J Med Sci Sports. 2008;18:417–426. doi: 10.1111/j.1600-0838.2008.00769.x. [DOI] [PubMed] [Google Scholar]
- 165.Rowell AE, Aughey RJ, Hopkins WG, et al. Identification of sensitive measures of recovery after external load from football match play. Int J Sports Physiol Perform. 2017;12:969–976. doi: 10.1123/ijspp.2016-0522. [DOI] [PubMed] [Google Scholar]
- 166.Silva JR, Ascensão A, Marques F, et al. Neuromuscular function, hormonal and redox status and muscle damage of professional soccer players after a high-level competitive match. Eur J Appl Physiol. 2013;113:2193–2201. doi: 10.1007/s00421-013-2633-8. [DOI] [PubMed] [Google Scholar]
- 167.Fitzpatrick JF, Akenhead R, Russell M, et al. Sensitivity and reproducibility of a fatigue response in elite youth football players. Sci Med Football. 2019;3:214–220. doi: 10.1080/24733938.2019.1571685. [DOI] [Google Scholar]
- 168.Garrett JM, Graham SR, Eston RG, et al. Comparison of a countermovement jump test and submaximal run test to quantify the sensitivity for detecting practically important changes within high-performance Australian Rules football. Int J Sports Physiol Perform. 2020;15:68–72. doi: 10.1123/ijspp.2019-0150. [DOI] [PubMed] [Google Scholar]
- 169.Garrett J, Akyildiz Z, Leduc C, et al. Peak running speed can be used to monitor neuromuscular fatigue from a standardized running test in team sport athletes. Res Sports Med. 2021;1–12. 10.1080/15438627.2021.1966012. [DOI] [PubMed]
- 170.Huygaerts S, Cos F, Cohen DD, et al. Mechanisms of hamstring strain injury: interactions between fatigue, muscle activation and function. Sports (Basel) 2020;8:65. doi: 10.3390/sports8050065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Cormack SJ, Newton RU, McGuigan MR, et al. Reliability of measures obtained during single and repeated countermovement jumps. Int J Sports Physiol Perform. 2008;3:131–144. doi: 10.1123/ijspp.3.2.131. [DOI] [PubMed] [Google Scholar]
- 172.Barrett S, Midgley A, Reeves M, et al. The within-match patterns of locomotor efficiency during professional soccer match play: implications for injury risk? J Sci Med Sport. 2016;19:810–815. doi: 10.1016/j.jsams.2015.12.514. [DOI] [PubMed] [Google Scholar]
- 173.Kelly SJ, Murphy AJ, Watsford ML, et al. Reliability and validity of sports accelerometers during static and dynamic testing. Int J Sports Physiol Perform. 2015;10:106–111. doi: 10.1123/ijspp.2013-0408. [DOI] [PubMed] [Google Scholar]
- 174.Eggers TM, Massard TI, Clothier PJ, et al. Measuring vertical stiffness in sport with accelerometers: exercise caution! J Strength Cond Res. 2018;32:1919–1922. doi: 10.1519/jsc.0000000000002318. [DOI] [PubMed] [Google Scholar]
- 175.Barrett S, Midgley A, Lovell R. PlayerLoad™: reliability, convergent validity, and influence of unit position during treadmill running. Int J Sports Physiol Perform. 2014;9:945–952. doi: 10.1123/ijspp.2013-0418. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.