Abstract
Objective.
We aimed to characterize the relationship between cardiorespiratory fitness and quality of life in a sample of healthy midlife women aged 40-65 years.
Methods.
Cardiorespiratory fitness was measured with a VO2max test. Quality of life was assessed with the menopause-specific Utian Quality of Life scale (UQOL). The UQOL measures overall quality of life, which comprises health, emotional, occupational, and sexual domains. Simple and multiple linear regression models were built to analyze relationships between cardiorespiratory fitness and overall quality of life as well as the separate UQOL domains.
Results.
Forty-nine women with an average age of 52.5 years were included in the analysis. In simple linear models, cardiorespiratory fitness was related to overall (R2=0.34, p<0.001), health (R2=0.55, p<0.001), emotional (R2=0.08, p=0.05), and occupational (R2=0.09, p=0.03) quality of life. In multiple regression models, cardiorespiratory fitness was associated with overall (p<0.01) and health (p<0.001) quality of life, after controlling for physical activity, age, body mass index, and time sedentary.
Conclusions.
Higher cardiorespiratory fitness is associated with better quality of life during midlife, particularly in the health domain. Increasing cardiorespiratory fitness may be a useful means to promote quality of life in this population.
Keywords: menopause, cardiorespiratory fitness, quality of life
Introduction
Midlife is a time when women face psychological and physical challenges to their health and well-being. Midlife may offer a critical window of opportunity to enhance health, reduce disease risk, and improve quality of life among women. Quality of life (QOL), is conceptualized as “a state of complete physical, mental, and social well-being.”1 In midlife, the transition to menopause is a period of major change that may significantly impact QOL2 and can include changes in health, physical, and psychosocial outcomes. Health changes with menopause include an increase in risk factors for cardiovascular disease, such as alterations in body composition3, plasma lipids4,5, and blood pressure.6 Menopause is associated with sleep disturbances, anxiety, and depression.7,8 Vasomotor symptoms of menopause, such as hot flashes and night sweats, have been suggested to have a significant and deleterious effect on QOL.2,9 Further, menopause is associated with declines in physical function.10,11 Psychosocial factors, such as relationship status, degree of life stress12, financial well-being, and employment status2, are also related to QOL in midlife women. Given these multi-faceted changes, it is critical to understand which factors may have the greatest impact on QOL in midlife women. This knowledge can be used to develop evidence-based solutions and recommendations to improve women’s QOL during challenges to well-being.
While physical activity (PA) is movement that increases energy expenditure beyond what is required at rest, cardiorespiratory fitness (CRF) is a measure of the maximum capacity of the body to utilize oxygen and is related to an individual’s capacity to perform work. Greater CRF is a strong, independent risk factor for cardiovascular disease, all-cause mortality13,14, and future disability15. In patients with one or more risk factors for CVD, the risk for developing the disease is significantly reduced in those with moderate to high levels of CRF.16,17 Further, higher CRF is associated with significantly greater reductions in CVD risk than greater PA .18 These data make CRF an important target for improving overall health and QOL.
Cardiorespiratory fitness has been associated with QOL domains in older men and women19 and in early postmenopausal women20; however, the influence of CRF on QOL in midlife women remains unclear. Studies have shown positive correlations between both self-report21 and objective measures22 of habitual physical activity on QOL and a positive effect of increasing physical activity on QOL23 in women; however, these studies did not assess specific relationships between QOL and CRF. Therefore, it is important to understand the link between CRF and QOL in midlife women. A better understanding of these associations can help guide prescription of therapies targeted to improve QOL among midlife women. The purpose of this study was to investigate the relationship between objectively-measured CRF and QOL in midlife women. We hypothesized that CRF would be positively related to QOL.
Methods
This research was approved by the University of Massachusetts Amherst Institutional Review Board. Participants provided informed consent prior to completing study protocols. Vascular outcomes from these participants have been published elsewhere.24-26
Study Population
This cohort included healthy midlife women aged 40-65 years. The original study aimed to evaluate differences in vascular function in women at different menopausal stages and with differing CRF before and after an acute bout of exercise. An a priori sample size estimation for our original aims was calculated with a power of 0.80 and an alpha of 0.05. Fifty-one women participated in the study. In this analysis, two women were excluded because of missing QOL data, one for missing occupational QOL and one for missing sexual QOL, leaving a total of 49 women for this analysis. Women were categorized as premenopausal, perimenopausal, and postmenopausal according to their self-reported menstrual cycle as per standards set by STRAW+10.27 Premenopausal women had regular menstrual cycles and were not taking oral contraceptives for at least 6 months prior to enrollment in the study. Perimenopausal women had menstrual cycles of variable length, at least 7 days different between consecutive cycles, or had up to 11 months of amenorrhea. Postmenopausal women had undergone natural menopause and were at least 5 years from their final menstrual period. Perimenopausal and postmenopausal women were not using hormone therapy for at least 6 months prior to enrollment. Women were included if they had blood pressure <140/<90 mmHg, fasting plasma glucose <126 mg/dL, LDL-C≤159mg/dl, HDL-C >40mg/dl, triglycerides <150mg/dl and had no history of cardiac events or cardiovascular disease. Participants were excluded if they were current smokers, used medications or dietary supplements known to impact cardiovascular function (e.g. blood pressure or lipid-lowering medications), or had a history of long-term menstrual irregularities prior to menopause.
Quality of Life
Quality of Life (QOL) was measured using the Utian QOL instrument (UQOL), a questionnaire that assesses QOL specific to the menopausal transition.28 The Utian questionnaire measures perceptions of well-being rather than physiological symptoms.28 The questionnaire comprises four QOL domains: health, occupational, emotional, and sexual. There are 23 statements to which participants must respond, such as: “I feel physically well,” “My mood is generally depressed,” and “I am able to control things in my life that are important to me”.28 To calculate scores for each domain and overall QOL, we followed the UQOL scoring system. Specifically, questions were scored on a scale of 1-5, from “Not true of me” as 1, “Moderately true of me” as 3, and “Very true of me,” as 5, with no specific labels for values 2 and 4.28 Points for statements within each QOL domain were summed with the range of scores for each domain as follows: Health (7-35), Emotional (6-30), Occupational (7-35), and Sexual (3-15). The scores for each domain were then summed to produce an overall QOL score (23-115). Higher scores indicate better QOL for each domain and the overall score. The UQOL is a reliable measure with good internal consistency.28
Cardiorespiratory fitness
Cardiorespiratory fitness was measured using a graded exercise treadmill test (Parvo Medics TrueOne 2400, Parvo, UT). Participants walked or ran on a treadmill at a self-selected speed starting at a 0% incline. During the test, the incline was increased by 2% every 2 minutes until the participant reached volitional fatigue. If necessary, speed was increased during the test. Heart rate and rhythm were monitored via 12-lead ECG. Standard criteria were used to determine VO2max.29 Because not all participants reached the criteria for a maximal test, data are reported as VO2peak.
Physical Activity
Self-reported physical activity (PA) was measured via the International Physical Activity Questionnaire Short-Form (IPAQ) which measures walking, moderate activity, vigorous activity, and sitting over the past week. The IPAQ has good reliability, with a test-retest correlation of roughly ρ=0.76.30 MET-minutes per week were calculated as per the IPAQ scoring guidelines.31 MET-minutes per week were calculated for each category of PA, and total MET-minutes were calculated from the sum of the PA categories. Due to the original study design, which focused on vascular outcomes, women were recruited who either met the “low” (less than 150 minutes per week of moderate intensity activity or less than 75 minutes per week of vigorous intensity activity accumulated in 10-minute bouts) or the “high” (at least 300 minutes per week of moderate intensity activity or 150 min/week of vigorous intensity activity accumulated in 10-minute bouts) criteria. Participants had a similar level of activity over the past 2 years. Time sedentary was measured as average hours per day sitting, which included time spent sitting at a desk, visiting with friends, reading or traveling on a bus, or sitting or lying down to watch television.31
Body Composition
Total body fat percentage was measured with Dual-energy X-ray Absorptiometry (DEXA) technology. Body mass index (BMI) was determined using height and weight measures taken in the laboratory and calculated as the participant’s weight in kilograms divided by height in meters squared.
Data Analysis
All analyses utilized RStudio software version 3.6.2. Descriptive statistics were performed to characterize the study population (e.g., age, body composition, PA, CRF, and QOL scores). We used simple linear regression to analyze bivariate relationships between QOL domains and overall score and CRF in separate models. Bivariate relationships between QOL domains and covariates were also examined. Pearson correlation coefficients and corresponding p-values are reported in Figure 1. Covariates PA (MET-minutes per week), time sedentary (hours per day), age, and BMI were added to multiple regression models as continuous variables. Covariates were chosen based on established correlations with QOL.21-23,32-35
Figure 1.
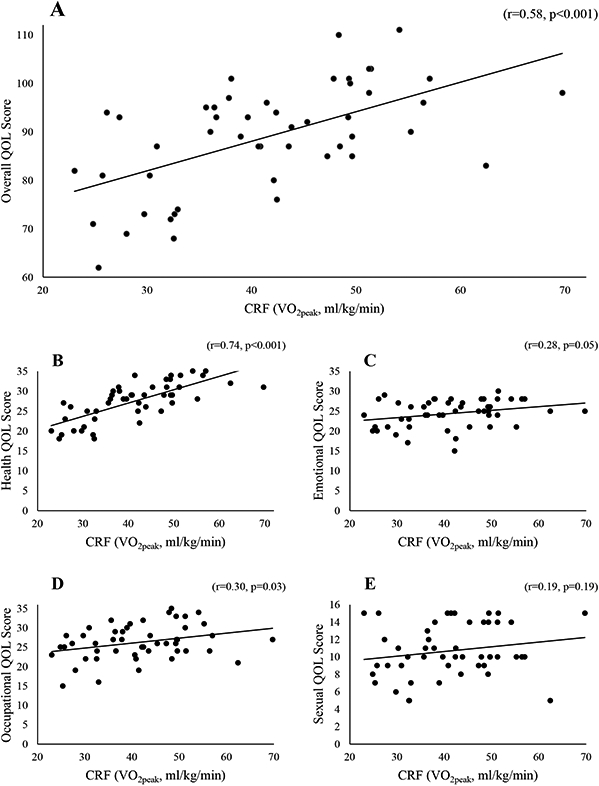
Pearson correlation coefficients (r) and corresponding p-values between A. cardiorespiratory fitness (CRF) and overall quality of life (QOL). B. CRF and health QOL. C. CRF and emotional QOL. D. CRF and occupational QOL. E. CRF and sexual QOL. QOL, quality of life; CRF, cardiorespiratory fitness (reported as VO2peak values).
Multiple regression models for each QOL domain and overall QOL score were constructed using reverse stepwise methods. All independent variables were added to the models initially, and then variables with the largest p-values were removed one at a time until only a single independent variable remained (see Supplemental Tables 1-5, which show all regression models). Age was kept in the model regardless of significance. Final models were chosen from this process of removing one variable at a time by p-value magnitude; the model with the highest adjusted R2 value, out of all stepwise models for a single dependent variable (overall QOL or one of the QOL domains), was selected as the “final model” for that dependent variable. For cases in which multiple models shared the same adjusted R2, the model with the fewest independent variables was chosen. All regression models were checked for conditions of residual normality, linearity, heteroscedasticity, and independence.
Results
Participant Characteristics
Forty-nine participants were included in this analysis. By study design, women were healthy and had few risk factors for cardiovascular disease. The average BMI was within the normal range, along with blood pressure, cholesterol, and fasting plasma glucose. Participants had an average age in their early fifties and were unevenly distributed across menopausal stages with more participants in perimenopause and postmenopause than premenopause (Table 1).
TABLE 1.
Participant characteristics
| Characteristic | Mean ± SDa |
|---|---|
| Age (years) | 52.5 ± 7.2 |
| Number of Participants | 49 |
| Premenopausal (n,%) | 11 (22.5) |
| Perimenopausal (n, %) | 18 (36.7) |
| Postmenopausal (n, %) | 20 (40.8) |
| BMI (kg/m2) | 23.5 ± 3.5 |
| Total Body Fat (%) | 31.8 ± 9.5 |
| Blood Pressure (Systolic/Diastolic) (mmHg) | 106.8/61.2 ± 12.6/7.9 |
| Low-Density Lipoprotein Cholesterol (mg/dL) | 103.3 ± 24.6 |
| High-Density Lipoprotein Cholesterol (mg/dL) | 80.9 ± 18.1 |
| Triglycerides (mg/dL) | 44.0 ± 16.1 |
| Fasting Plasma Glucose (mg/dL) | 95.2 ± 6.7 |
| VO2peak (ml/kg/min) | 41.4 ± 10.6 |
| PA (MET-min/week) | 2705.0 ± 2364.8 |
| Time Sedentary (hours/day) | 7.2 ± 3.4 |
| Overall QOL Score (range, 48-100) | 88.9 ± 11.2 |
| Health QOL Score (range, 11-31) | 27.5 ± 4.8 |
| Emotional QOL Score (range, 12-28) | 24.4 ± 3.4 |
| Occupational QOL Score (range, 13-35) | 26.3 ± 4.5 |
| Sexual QOL Score (range, 0-15) | 10.7 ± 3.0 |
Unless otherwise noted
In bivariate analyses, there were significant correlations between CRF and overall QOL (r=0.58, p<0.001), health QOL (r=0.74, p<0.001), emotional QOL (r=0.28, p=0.05), and occupational QOL (r=0.30, p=0.03) (Figure 1). CRF was significantly related to overall QOL (R2=0.34, p<0.001), health QOL (R2=0.55, p<0.001), emotional QOL (R2=0.08, p=0.05), and occupational QOL (R2=0.09, p=0.03) (Table 2). For health and overall QOL, there was a moderate-to-strong, positive, linear relationship between CRF and QOL. For emotional and occupational QOL, there was a small-to-moderate positive relationship between CRF and QOL. Sexual QOL was not significantly related to CRF (R2=0.04, p=0.19). In bivariate models, CRF explained a larger proportion of the variance in health, emotional, and overall QOL than any other independent variable, including PA, and BMI.
TABLE 2.
Bivariate and multiple linear regression models of cardiorespiratory fitness and overall and domains of quality of life
| Overall QOL | ||||
|---|---|---|---|---|
| Model | Variables | P Value | R2a | Adjusted R2 |
| Model 1 (p<0.001)a | CRF | <0.001a | 0.34 | 0.32 |
| Model 2 (p<0.001)a | CRF | 0.01c | 0.42 | 0.39 |
| PA | 0.02c | |||
| Age | 0.74 | |||
| Health QOL | ||||
| Model 1 (p<0.001)a | CRF | <0.001a | 0.55 | 0.54 |
| Model 2 (p<0.001)a | CRF | <0.001a | 0.59 | 0.56 |
| PA | 0.14 | |||
| Age | 0.40 | |||
| Emotional QOL | ||||
| Model 1 (p=0.05)c | CRF | 0.05c | 0.08 | 0.06 |
| Model 2 (p=0.15) | CRF | 0.12 | 0.11 | 0.05 |
| Time Sed | 0.24 | |||
| Age | 1.00 | |||
| Occupational QOL | ||||
| Model 1 (p=0.03)c | CRF | 0.03c | 0.09 | 0.07 |
| Model 2 (p=0.01)b | PA | <0.001a | 0.22 | 0.17 |
| Time Sed | 0.14 | |||
| Age | 0.30 | |||
| Sexual QOL | ||||
| Model 1 (p=0.19) | CRF | 0.19 | 0.04 | 0.02 |
| Model 2 (p=0.04)c | PA | 0.04c | 0.13 | 0.09 |
| Age | 0.19 |
R2 represents the proportion of variance in the dependent variable predicted by the model.
Final multiple regression models predicted a significant proportion of the variance in overall, health, occupational, and sexual QOL (Table 2). Cardiorespiratory fitness was a significant predictor of overall and health QOL when controlling for PA, age, BMI, and time sedentary (see Supplemental Tables 1 and 2, which show all regression models). Cardiorespiratory fitness, PA, and age explained 42% of the variance in overall QOL and 59% of the variance in health QOL (Table 2). CRF alone explained 34% of the variance in overall QOL, with an 8% increase in variance explained when adding PA and age to the model. CRF alone explained 55% of the variance in health QOL, with only a 4% increase in variance explained when adding PA and age to the model.
Physical activity, and not CRF, significantly predicted occupational and sexual QOL in multiple regression models: PA, time sedentary, and age predicted 22% of the variance in occupational QOL, while PA and age predicted 13% of the variance in sexual QOL (Table 2). While CRF alone predicted a significant proportion of the variance in emotional QOL, after controlling for additional covariates, these associations were no longer significant (Table 2).
Discussion
The purpose of this study was to investigate the relationship between objectively-measured CRF and QOL in healthy midlife women. Using the UQOL questionnaire, our analysis showed, in accordance with our hypothesis, that CRF was a significant predictor of overall QOL, which includes health, emotional, occupational, and sexual QOL domains. We also found that CRF predicted a large proportion of the variance in health QOL, and that the relationship between CRF and health QOL was significant after controlling for covariates. Additionally, we report that CRF was moderately related to emotional QOL in unadjusted models, although the relationship did not remain significant when adjusting for age and sedentary time. Finally, PA was moderately related to occupational and sexual QOL. These results reflect the importance of CRF for midlife women and indicate that CRF may be a useful interventional target for improving QOL in this population.
Quality of life is a subjective multidimensional construct that includes physical, mental and social domains1 and is not simply the absence of symptoms or disease. The vast majority of studies that have measured QOL in women around menopause have used assessments that measure symptoms.36 However, in an analysis of a large, diverse group of midlife women from the Study of Women’s Health Across the Nation (SWAN), Avis, et al.10 demonstrated that vasomotor symptoms were not associated with QOL in midlife women. While the transition to menopause is a major event for women, and is associated with symptoms and increased disease risk, studies have shown that other factors, such as perceived daily stress, are influential to well-being during midlife.12,37 The UQOL questionnaire is a tool that was created for and validated in perimenopausal and postmenopausal women and assesses the perception of well-being, distinct from menopausal symptoms.28 The UQOL assesses subjective feelings of emotional, physical, occupational, and sexual wellness, including feelings of content and control. The UQOL is considered an assessment of both general and menopause-specific QOL. To our knowledge, no other studies have evaluated the role of CRF using the UQOL in this population.
Midlife women experience reductions in physical function, and the transition to menopause appears to be a critical period in the development of physical limitations.38-40 In a 2-year longitudinal study of women aged 45-50 years, in those transitioning to perimenopause, the greatest declines in health were in physical functioning and role limitation (e.g. trouble completing “work or other daily activities”)41 due to physical changes.11 In data from SWAN, Avis, et al.42 reported a reduction in the physical component score of the Short-Form Health Survey-36 (SF-36) health-related QOL over 11 years of follow up. Midlife, and, specifically, the menopause transition, is an important time to focus on reducing the development of physical limitations. Considering our findings in this context, higher CRF may allow women around menopause to independently perform daily activities with a high level of physical function, leading to a higher subjective rating of health and overall QOL. Conversely, it may also suggest that women with low QOL may benefit from an intervention that focuses on improving CRF.
Few studies have specifically investigated the relationship between CRF and QOL in midlife women across menopausal stages. In early postmenopausal women with an average age of 55.6±5SD years, there was a correlation between higher overall QOL score on the SF-36 and CRF assessed with the 6-min walk test. In this analysis, the 6-min walk test was also significantly related to “emotional role,” “bodily pain,” and “vitality” SF-36 subscores.20 On the other hand, a study of postmenopausal Taiwanese women aged 50-89 years reported a positive relationship between SF-36 scores and metrics of back strength but not the step test for cardiorespiratory endurance.43 Exercise intervention trials that include women at different menopausal stages and have assessed changes in CRF have shown concomitant improvements in CRF and QOL measures.23,32,44 These studies did not specifically evaluate the relationships between change in CRF and QOL. The studies were focused on symptoms,23,44 used a combination of physical and psychosocial interventions,44 used interventions to change multiple aspects of physical fitness, such as CRF, muscular fitness, and flexibility,32,44 or only focused on postmenopausal women.32,44 The data presented herein extend our knowledge from these prior studies by incorporating an objective, high quality measure of CRF, a measure of QOL distinct from a symptom inventory, and a sample of women across different menopausal stages. Our data indicate that CRF explained a larger proportion of the variance in health, emotional, and overall QOL than physical activity and BMI. This supports the importance of CRF for QOL relative to other factors that may be influenced by exercise in midlife women.12,19,45
Psychological well-being involves both feeling good and functioning optimally in the world.46,47 Data from SWAN and others have generally found that perimenopausal, and, often, postmenopausal women have a heightened chance of experiencing an episode of major depression or depressive symptoms.7 In midlife women, higher CRF may be associated with better mental health, which could contribute to the higher measures of QOL found in the present study. In the one study published to date that specifically evaluated CRF and QOL in women, researchers measured the relationship between various components of physical fitness (e.g. strength, flexibility, balance) with health-related QOL via the SF-36 in early postmenopausal women. They found that CRF (assessed via the 6-min walk test) was positively and independently related to the mental component of the SF-36, but not the physical component.20 In perimenopausal women, higher self-reported fitness, measured by the International Fitness Scale (IFIS), was associated with better mental health outcomes including lower anxiety and depression, and improved affect.48 Our data show that CRF significantly predicted overall and emotional QOL, although the relationship between CRF and emotional QOL disappears when controlling for age and sedentary time. Together these data suggest that higher CRF may have a unique influence on QOL via mental well-being for women around the menopausal transition, but more study is needed to clarify this relationship.
We found that PA, but not CRF, was significantly related to occupational and sexual QOL and helped to explain the variance in overall QOL. Studies have addressed the benefits of PA on QOL in women around the menopausal transition.21-23 Through a mediation analysis, Elavsky49 showed that greater PA was related to self-worth and positive affect, which were related to UQOL outcomes. The benefits of PA on QOL may be both direct and indirect. Recent data from the FLAMENCO project showed that while a greater amount of light PA was related to the emotional role dimension on the SF-36, moderate and vigorous PA were associated with physical function and vitality and physical function and bodily pain, respectively.22 These data are in alignment with our finding that higher CRF was strongly associated with health QOL, while PA alone was more strongly related to occupational QOL. Higher intensities of PA, which may be necessary to improve CRF, appear to be important for improving the self-report of physical health in women around menopause.
Clinical Implications
This study is of clinical importance because the results suggest that quality of life, a critical health outcome, may be improved by increasing CRF in midlife women. Our results indicate that healthcare practitioners would benefit from targeting CRF as an important health indicator beyond its prognostic ability to predict disease risk. CRF can be measured by a variety of simple tests, such as the 6-minute walk test, which does not require expensive equipment or a great investment of time. Similarly, our data support the measurement of QOL for midlife women. Exercise training programs aimed at improving CRF may be prescribed to midlife women who have low QOL. These interventions include activities outlined in the American College of Sports Medicine (ACSM) Guidelines as moderate intensity aerobic exercise done at least 5 days/week or vigorous intensity aerobic exercise done at least 3 days/week, or a weekly combination of 3-5 days/week of moderate and vigorous intensity exercise.29 Specific prescriptions would depend on initial CRF level. Future study is needed to clarify exact exercise interventions that can maximize QOL in this population. Finally, targeting patients with low CRF may improve not only QOL but also reduce healthcare costs. A recent analysis showed that individuals with the lowest CRF had $14,662 higher health costs per year compared with individuals with the highest CRF.50
Strengths and Limitations
The study has a number of strengths. To our knowledge, this is the first study to evaluate the association between objectively-measured CRF and QOL in women at multiple stages of the menopausal transition. Additionally, we used a well-validated QOL assessment, the UQOL Scale, specifically designed for women going through menopause that measures QOL beyond menopausal symptoms. To date, studies evaluating exercise training, PA, and physical fitness have largely focused on symptoms. Finally, we had a sample with a large range of habitual PA and CRF, including both participants who were very low and those who were very high on these measures.
This study is not without limitations. Differences in QOL have been shown between ethnic groups.51 Our sample was from a healthy population of mostly white women. Therefore, future analyses should evaluate whether the relationship between CRF and QOL are consistent in a more ethnically diverse population. The sample size for this analysis was powered on the original study aims and participants were selected to have few disease risk factors, which allowed us to evaluate the independent relationship between CRF and QOL while limiting potential confounding variables. However, we were unable to pull apart the influences of body fat percentage and CRF on QOL due to their high collinearity. On average, our participants had a significantly higher QOL in every domain of the UQOL than the population norms of the scale, except for occupational QOL, therefore, results may not be translatable to individuals who score lower on the UQOL.28 Due to the cross-sectional design of this study, we were unable to establish a causal relationship between CRF and QOL. It is possible that low QOL may have a negative impact on physical activity and CRF. Finally, this study focused on objectively measured CRF, therefore, we are limited in our ability to speak to the relationship between QOL and other facets of fitness. Future studies should investigate the relationship between objectively-measured CRF and QOL in a larger, more nationally representative sample and elucidate whether the relationship between CRF and QOL differs in premenopausal, perimenopausal, and postmenopausal women.
Conclusions
In conclusion, we found that CRF is significantly related to QOL in a population of healthy midlife women. The relationship between CRF and health QOL in particular was strong. We hypothesize that high CRF contributes significantly to perceptions of well-being and one’s capacity to complete daily tasks and engage in leisure activities20, thereby influencing overall QOL. Therefore, including bouts of higher intensity PA may be worth considering in crafting exercise prescriptions for menopausal women in order to improve QOL
Supplementary Material
Acknowledgments:
The authors would like to thank the participants and study personnel for their contributions to this project. We would like to thank Jennifer Smetzer for her statistical assistance.
Sources of funding:
Smith College Student Research in Departments (STRIDE) Fellowship (Flesaker), American College of Sports Medicine Foundation Doctoral Student Research Grant (Serviente), National Institute on Aging Grant T32-AG049676 (Pennsylvania State University).
Footnotes
Financial Disclosures/Conflicts of Interest: None reported.
References
- 1.World Health Organization. Constitution of the World Health Organization. Am J Public Health Nations Health. 1946;36(11):1315–1323. doi: 10.2105/ajph.36.11.1315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Szadowska-Szlachetka ZC, Stasiak E, Leziak A, et al. Intensity of menopausal symptoms and quality of life in climacteric women. Prz Menopauzalny. 2019;18(4):217–221. doi: 10.5114/pm.2019.93113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ambikairajah A, Walsh E, Tabatabaei-Jafari H, Cherbuin N. Fat mass changes during menopause: a metaanalysis. American Journal of Obstetrics and Gynecology. 2019;221(5):393–409.e50. doi: 10.1016/j.ajog.2019.04.023 [DOI] [PubMed] [Google Scholar]
- 4.Wang Q, Ferreira DLS, Nelson SM, Sattar N, Ala-Korpela M, Lawlor DA. Metabolic characterization of menopause: cross-sectional and longitudinal evidence. BMC Med. 2018;16(1):17. doi: 10.1186/s12916-018-1008-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthews KA, Crawford SL, Chae CU, et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol. 2009;54(25):2366–2373. doi: 10.1016/j.jacc.2009.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Son MK, Lim N-K, Lim J-Y, et al. Difference in blood pressure between early and late menopausal transition was significant in healthy Korean women. BMC Womens Health. 2015;15:64. doi: 10.1186/s12905-015-0219-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bromberger JT, Kravitz HM. Mood and menopause: findings from the Study of Women’s Health Across the Nation (SWAN) over 10 years. Obstet Gynecol Clin North Am. 2011;38(3):609–625. doi: 10.1016/j.ogc.2011.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hildreth KL, Ozemek C, Kohrt WM, Blatchford PJ, Moreau KL. Vascular dysfunction across the stages of the menopausal transition is associated with menopausal symptoms and quality of life. Menopause. 2018;25(9):1011–1019. doi: 10.1097/GME.0000000000001112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams RE, Levine KB, Kalilani L, Lewis J, Clark RV. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas. 2009;62(2):153–159. doi: 10.1016/j.maturitas.2008.12.006 [DOI] [PubMed] [Google Scholar]
- 10.Avis NE, Colvin A, Bromberger JT, et al. Change in health-related quality of life over the menopausal transition in a multiethnic cohort of middle-aged women: Study of Women’s Health Across the Nation. Menopause. 2009;16(5):860–869. doi: 10.1097/gme.0b013e3181a3cdaf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishra GD. Physical and mental health: Changes during menopause transition. Quality of Life Research. 2003;12(4):405–412. doi: 10.1023/A:1023421128141 [DOI] [PubMed] [Google Scholar]
- 12.Avis NE, Assmann SF, Kravitz HM, Ganz PA, Ory M. Quality of life in diverse groups of midlife women: assessing the influence of menopause, health status and psychosocial and demographic factors. Qual Life Res. 2004;13(5):933–946. doi: 10.1023/B:QURE.0000025582.91310.9f [DOI] [PubMed] [Google Scholar]
- 13.Ozemek C, Laddu DR, Lavie CJ, et al. An Update on the Role of Cardiorespiratory Fitness, Structured Exercise and Lifestyle Physical Activity in Preventing Cardiovascular Disease and Health Risk. Progress in Cardiovascular Diseases. 2018;61(5-6):484–490. doi: 10.1016/j.pcad.2018.11.005 [DOI] [PubMed] [Google Scholar]
- 14.Lee D-C, Sui X, Ortega FB, et al. Comparisons of leisure-time physical activity and cardiorespiratory fitness as predictors of all-cause mortality in men and women. Br J Sports Med. 2011;45(6):504–510. doi: 10.1136/bjsm.2009.066209 [DOI] [PubMed] [Google Scholar]
- 15.Cochrane T, Munro J, Davey R, Nicholl J. Exercise, Physical Function and Health Perceptions of Older People. Physiotherapy. 1998;84(12):598–602. doi: 10.1016/S0031-9406(05)66153-6 [DOI] [Google Scholar]
- 16.Farrell SW, Finley CE, Barlow CE, et al. Moderate to High Levels of Cardiorespiratory Fitness Attenuate the Effects of Triglyceride to High-Density Lipoprotein Cholesterol Ratio on Coronary Heart Disease Mortality in Men. Mayo Clin Proc. 2017;92(12):1763–1771. doi: 10.1016/j.mayocp.2017.08.015 [DOI] [PubMed] [Google Scholar]
- 17.Lavie CJ, Schutter AD, Archer E, McAuley PA, Blair SN. Obesity and prognosis in chronic diseases--impact of cardiorespiratory fitness in the obesity paradox. Curr Sports Med Rep. 2014;13(4):240–245. doi: 10.1249/JSR.0000000000000067 [DOI] [PubMed] [Google Scholar]
- 18.Williams PT. Physical fitness and activity as separate heart disease risk factors: a metaanalysis. Med Sci Sports Exerc. 2001;33(5):754–761. doi: 10.1097/00005768-200105000-00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wanderley FAC, Silva G, Marques E, Oliveira J, Mota J, Carvalho J. Associations between objectively assessed physical activity levels and fitness and self-reported health-related quality of life in community-dwelling older adults. Qual Life Res. 2011;20(9):1371–1378. doi: 10.1007/s11136-011-9875-x [DOI] [PubMed] [Google Scholar]
- 20.Moratalla-Cecilia N, Soriano-Maldonado A, Ruiz-Cabello P, et al. Association of physical fitness with health-related quality of life in early postmenopause. Qual Life Res. 2016;25(10):2675–2681. doi: 10.1007/s11136-016-1294-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daley A, Macarthur C, Stokes-Lampard H, McManus R, Wilson S, Mutrie N. Exercise participation, body mass index, and health-related quality of life in women of menopausal age. Br J Gen Pract. 2007;57(535):130–135. [PMC free article] [PubMed] [Google Scholar]
- 22.Marín-Jiménez N, Ruiz-Montero PJ, De la Flor-Alemany M, Aranda P, Aparicio VA. Association of objectively measured sedentary behavior and physical activity levels with health-related quality of life in middle-aged women: The FLAMENCO project. Menopause. Published online February 17, 2020. doi: 10.1097/GME.0000000000001494 [DOI] [PubMed] [Google Scholar]
- 23.Elavsky S, McAuley E. Physical activity and mental health outcomes during menopause: a randomized controlled trial. Ann Behav Med. 2007;33(2):132–142. doi: 10.1007/bf02879894 [DOI] [PubMed] [Google Scholar]
- 24.Serviente C, Witkowski S. Follicle-stimulating hormone, but not cardiorespiratory fitness, is associated with flow-mediated dilation with advancing menopausal stage. Menopause. 2019;26(5):531–539. doi: 10.1097/GME.0000000000001267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Serviente C, Burnside A, Witkowski S. Moderate-intensity exercise reduces activated and apoptotic endothelial microparticles in healthy midlife women. J Appl Physiol. 2019;126(1):102–110. doi: 10.1152/japplphysiol.00420.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Serviente C, Troy LM, de Jonge M, Shill DD, Jenkins NT, Witkowski S. Endothelial and inflammatory responses to acute exercise in perimenopausal and late postmenopausal women. Am J Physiol Regul Integr Comp Physiol. 2016;311(5):R841–R850. doi: 10.1152/ajpregu.00189.2016 [DOI] [PubMed] [Google Scholar]
- 27.Harlow SD, Gass M, Hall JE, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012;97(4):1159–1168. doi: 10.1210/jc.2011-3362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Utian WH, Janata JW, Kingsberg SA, Schluchter M, Hamilton JC. The Utian Quality of Life (UQOL) Scale: development and validation of an instrument to quantify quality of life through and beyond menopause. Menopause. 2018;25(11):1224–1231. doi: 10.1097/GME.0000000000001223 [DOI] [PubMed] [Google Scholar]
- 29.American College of Sports Medicine, Riebe D, Ehrman JK, Liguori G, Magal M, eds. ACSM’s Guidelines for Exercise Testing and Prescription. Tenth edition. Wolters Kluwer; 2018. [Google Scholar]
- 30.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. doi: 10.1186/1479-5868-8-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). Short and Long Forms. Published November 2005. Accessed June 25, 2020. https://www.ipaq.ki.se/ [Google Scholar]
- 32.Teoman N, Ozcan A, Acar B. The effect of exercise on physical fitness and quality of life in postmenopausal women. Maturitas. 2004;47(1):71–77. doi: 10.1016/s0378-5122(03)00241-x [DOI] [PubMed] [Google Scholar]
- 33.Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obesity Reviews. 2001;2(3):173–182. doi: 10.1046/j.1467-789x.2001.00032.x [DOI] [PubMed] [Google Scholar]
- 34.Han TS, Tijhuis MA, Lean ME, Seidell JC. Quality of life in relation to overweight and body fat distribution. Am J Public Health. 1998;88(12):1814–1820. doi: 10.2105/ajph.88.12.1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mikkola TM, Kautiainen H, von Bonsdorff MB, et al. Body composition and changes in health-related quality of life in older age: a 10-year follow-up of the Helsinki Birth Cohort Study. Qual Life Res. Published online March 2, 2020. doi: 10.1007/s11136-020-02453-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matthews KA, Bromberger JT. Does the menopausal transition affect health-related quality of life? Am J Med. 2005;118 Suppl 12B:25–36. doi: 10.1016/j.amjmed.2005.09.032 [DOI] [PubMed] [Google Scholar]
- 37.Dennerstein L, Lehert P, Guthrie J. The effects of the menopausal transition and biopsychosocial factors on well-being. Arch Womens Ment Health. 2002;5(1):15–22. doi: 10.1007/s007370200018 [DOI] [PubMed] [Google Scholar]
- 38.El Khoudary SR, Greendale G, Crawford SL, et al. The menopause transition and women’s health at midlife: a progress report from the Study of Women’s Health Across the Nation (SWAN). Menopause. 2019;Publish Ahead of Print. doi: 10.1097/GME.0000000000001424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.El Khoudary SR, McClure CK, VoPham T, et al. Longitudinal Assessment of the Menopausal Transition, Endogenous Sex Hormones, and Perception of Physical Functioning: The Study of Women’s Health Across the Nation. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2014;69(8):1011–1017. doi: 10.1093/gerona/glt285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sowers M, Pope S, Welch G, Sternfeld B, Albrecht G. The association of menopause and physical functioning in women at midlife. J Am Geriatr Soc. 2001;49(11):1485–1492. doi: 10.1046/j.1532-5415.2001.4911241.x [DOI] [PubMed] [Google Scholar]
- 41.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 42.Avis NE, Colvin A, Bromberger JT, Hess R. Midlife Predictors of Health-Related Quality of Life in Older Women. J Gerontol A Biol Sci Med Sci. 2018;73(11):1574–1580. doi: 10.1093/gerona/gly062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hsu W-H, Chen C, Kuo LT, Fan C-H, Lee MS, Hsu RW-W. The relationship between health-related fitness and quality of life in postmenopausal women from Southern Taiwan. Clin Interv Aging. 2014;9:1573–1579. doi: 10.2147/CIA.S66310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Godoy-Izquierdo D, de Guevara NML, Toral MV, de T Galván C, Ballesteros AS, García JFG. Improvements in health-related quality of life, cardio-metabolic health, and fitness in postmenopausal women after a supervised, multicomponent, adapted exercise program in a suited health promotion intervention: a multigroup study. Menopause. 2017;24(8):938–946. doi: 10.1097/GME.0000000000000844 [DOI] [PubMed] [Google Scholar]
- 45.Grindler NM, Santoro NF. Menopause and exercise. Menopause. 2015;22(12):1351–1358. doi: 10.1097/GME.0000000000000536 [DOI] [PubMed] [Google Scholar]
- 46.Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Well-Being. Simon and Schuster; 2012. [Google Scholar]
- 47.Brown L, Bryant C, Judd FK. Positive well-being during the menopausal transition: a systematic review. Climacteric. 2015;18(4):456–469. doi: 10.3109/13697137.2014.989827 [DOI] [PubMed] [Google Scholar]
- 48.Aparicio VA, Marín-Jiménez N, Coll-Risco I, et al. Doctor, ask your perimenopausal patient about her physical fitness; association of self-reported physical fitness with cardiometabolic and mental health in perimenopausal women: the FLAMENCO project. Menopause. 2019;26(10):1146–1153. doi: 10.1097/GME.0000000000001384 [DOI] [PubMed] [Google Scholar]
- 49.Elavsky S Physical activity, menopause, and quality of life: the role of affect and self-worth across time. Menopause. 2009;16(2):265–271. doi: 10.1097/gme.0b013e31818c0284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Myers J, Doom R, King R, et al. Association Between Cardiorespiratory Fitness and Health Care Costs: The Veterans Exercise Testing Study. Mayo Clin Proc. 2018;93(1):48–55. doi: 10.1016/j.mayocp.2017.09.019 [DOI] [PubMed] [Google Scholar]
- 51.Avis NE, Ory M, Matthews KA, Schocken M, Bromberger J, Colvin A. Health-related quality of life in a multiethnic sample of middle-aged women: Study of Women’s Health Across the Nation (SWAN). Med Care. 2003;41(11):1262–1276. doi: 10.1097/01.MLR.0000093479.39115.AF [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


