Abstract
Nasolacrimal duct obstruction (NLDO) is a rare complication after radioiodine therapy and may cause false positive 131I uptake at the point of obstruction in 131I whole body scan. Here, we report a 59-year-old female patient with papillary thyroid cancer treated with total thyroidectomy followed by 131I therapy. 131I whole body scan revealed focal uptake in the head. Single photon emission computed tomography/computed tomography (CT) showed focal uptake at the right proximal nasolacrimal duct. The ophthalmologic examination and the diagnostic maxillofacial CT confirmed the diagnosis of NLDO.
Keywords: 131I, radioiodine therapy, nasolacrimal duct obstruction, thyroid cancer
Abstract
Nazolakrimal kanal tıkanıklığı (NLKT), radyoiyot tedavisi sonrası nadir görülen bir komplikasyondur ve 131I tüm vücut tarama sintigrafisinde tıkanma noktasında yanlış pozitif 131I tutulumuna neden olabilir. Burada, 59 yaşında papiller tiroid kanserli, total tiroidektomi ve ardından 131I tedavisi uygulanan bir kadın hasta sunuldu. 131I tüm vücut tarama sintigrafisinde kafada odaksal bir 131I tutulumu izlendi. Tek foton emisyon tomografisi/bilgisayarlı tomografi (BT) sağ nazolakrimal kanal proksimal kesiminde fokal 131I tutulumu gösterdi. Oftalmolojik muayene ve tanısal maksillofasiyal BT, NLKT tanısını doğruladı.
Figure 1.
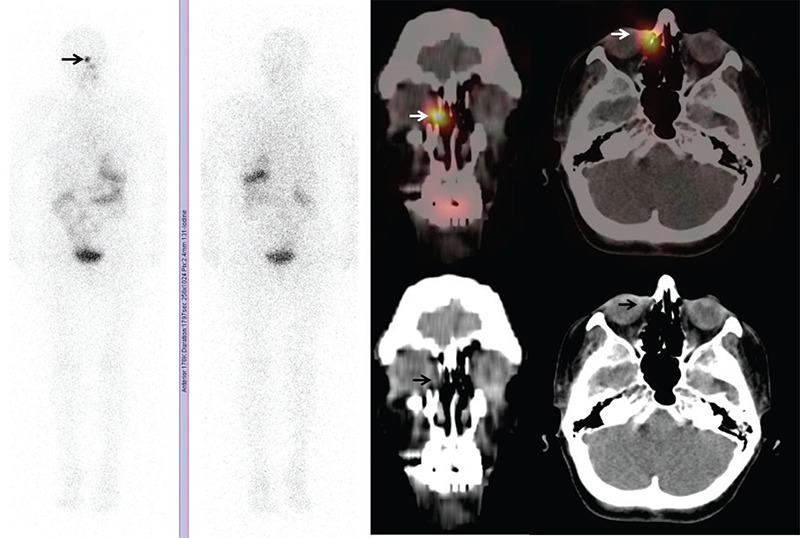
131I whole body scan was performed on a 59-year-old female patient with papillary thyroid cancer (T3N1bM0), who was treated 5 years ago with total thyroidectomy followed by a single dose 150 mCi 131I therapy. A planar 131I whole body scan with single photon emission computed tomography/computed tomography (SPECT/CT) and spot neck pinhole images were obtained at the 48th hour after 5 mCi 131I oral administration. At the time of imaging, stimulated thyroid-stimulating hormone level was 280 IU/mL, thyroglobulin (Tg) level was 0.20 ng/mL and anti-Tg antibody level was <0.9 IU/mL. The patient had no symptoms at the time of imaging. Planar 131I whole body scan showed no significant radioactivity uptake that may be compatible with residual thyroid tissue or recurrent thyroid cancer, on the other hand a suspicious focus of intense increased uptake was noted at the right paranasal region, which mimics a metastatic lesion (arrow in planar images). SPECT/CT images revealed 7x4 mm sized soft tissue density lesion-demonstrating 131I uptake, in the right infraorbital region next to the lateral wall of ethmoid sinus (arrows in fused SPECT/CT images) suggesting nasolacrimal duct obstruction (NLDO). Subsequently, an ophthalmologic examination and a diagnostic maxillofacial CT were performed to confirm the diagnosis. 131I has been used for many years as a valuable treatment in thyroid diseases such as hyperthyroidism and differentiated thyroid carcinomas (1,2,3). NLDO is an uncommon complication of 131I therapy, especially rarely occurs after a single dose of radioiodine treatment. Morgenstern et al. (4) reported that the cells of the lacrimal drainage system have the same Na/I symporters expressed by the cells of the thyroid gland and eventually the accumulation of 131I in these cells results in radiation induced damage. Fibrosis and obstruction of lacrimal drainage system will cause 131I uptake at the point of obstruction in whole body 131I scan and that may be misinterpreted as a metastasis (5,6). SPECT/CT can be useful to discriminate these false positive findings of planar 131I whole-body imaging, as in this study (7). Beside that early identification of these lesions may hasten the subsequent appropriate treatment of the patients and improve quality of life (8).
Footnotes
Ethics
Informed Consent: Informed consent form was obtained.
Peer-review: Externally peer-reviewed.
Authorship Contributions
Surgical and Medical Practices: N.F., K.Ö., S.Ö., O.B., T.Y.E., Concept: N.F., T.Y.E., Design: N.F., T.Y.E., Data Collection or Processing: N.F., K.Ö., Analysis or Interpretation: N.F., T.Y.E., Literature Search: N.F., T.Y.E., Writing: N.F., S.Ö.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Ali MJ. Iodine-131 Therapy and nasolacrimal duct obstructions: what we know and what we need to know. Ophthalmic Plast Reconstr Surg. 2016;32:243–248. doi: 10.1097/IOP.0000000000000647. [DOI] [PubMed] [Google Scholar]
- 2.Burns JA, Morgenstern KE, Cahill KV, Foster JA, Jhiang SM, Kloos RT. Nasolacrimal obstruction secondary to I(131) therapy. Ophthalmic Plast Reconstr Surg. 2004;20:126–129. doi: 10.1097/01.iop.0000117340.41849.81. [DOI] [PubMed] [Google Scholar]
- 3.Fard-Esfahani A, Mirshekarpour H, Fallahi B, Eftekhari M, Saghari M, Beiki D, Ansari-Gilani K, Takavar A. The effect of high-dose radioiodine treatment on lacrimal gland function in patients with differentiated thyroid carcinoma. Clin Nucl Med. 2007;32:696–699. doi: 10.1097/RLU.0b013e318124fdb6. [DOI] [PubMed] [Google Scholar]
- 4.Morgenstern KE, Vadysirisack DD, Zhang Z, Cahill KV, Foster JA, Burns JA, Kloos RT, Jhiang SM. Expression of sodium iodide symporter in the lacrimal drainage system: implication for the mechanism underlying nasolacrimal duct obstruction in I(131)-treated patients. Ophthalmic Plast Reconstr Surg. 2005;21:337–344. doi: 10.1097/01.iop.0000179369.75569.a8. [DOI] [PubMed] [Google Scholar]
- 5.Yuoness S, Rachinsky I, Driedger AA, Belhocine TZ. Differentiated thyroid cancer with epiphora: detection of nasolacrimal duct obstruction on I-131 SPECT/CT. Clin Nucl Med. 2011;36:1149–1152. doi: 10.1097/RLU.0b013e3182336016. [DOI] [PubMed] [Google Scholar]
- 6.Fard-Esfahani A, Farzanefar S, Fallahi B, Beiki D, Saghari M, Emami-Ardekani A, Majdi M, Eftekhari M. Nasolacrimal duct obstruction as a complication of iodine-131 therapy in patients with thyroid cancer. Nucl Med Commun. 2012;33:1077–1080. doi: 10.1097/MNM.0b013e3283570fb8. [DOI] [PubMed] [Google Scholar]
- 7.Brockmann H, Wilhelm K, Joe A, Palmedo H, Biersack HJ. Nasolacrimal drainage obstruction after radioiodine therapy: case report and a review of the literature. Clin Nucl Med. 2005;30:543–545. doi: 10.1097/01.rlu.0000170013.84378.2a. [DOI] [PubMed] [Google Scholar]
- 8.Ali MJ, Vyakaranam AR, Rao JE, Prasad G, Reddy PV. Iodine-131 therapy and lacrimal drainage system toxicity: nasal localization studies using whole body nuclear scintigraphy and SPECT-CT. Ophthalmic Plast Reconstr Surg. 2017;33:13–16. doi: 10.1097/IOP.0000000000000603. [DOI] [PubMed] [Google Scholar]


