ABSTRACT
Hereditary hyperferritinemia-cataract syndrome is a rare autosomal dominant disease caused by a genetic mutation in the iron responsive element in the 5’ untranslated region of the ferritin light chain gene. Hereditary hyperferritinemia-cataract syndrome is characterized by elevated serum ferritin levels and bilateral cataract development early in life and may be misdiagnosed as hemochromatosis. This case report describes a Brazilian family with a clinical diagnosis of hereditary hyperferritinemia-cataract syndrome, which was submitted to ferritin light chain gene sequencing. The genetic mutation c.-164C>G was identified in the 5’ untranslated region. In conclusion, genetic testing can be used for accurate diagnosis of hereditary hyperferritinemia-cataract syndrome to avoid misdiagnosis of hemochromatosis, other diseases associated with iron overload or ophthalmic diseases.
Keywords: Ferritins, Cataract, Hyperferritinemia, Mutation, Iron overload, Iron metabolism disorders
INTRODUCTION
Hereditary hyperferritinemia-cataract syndrome (HHCS) is a rare autosomal dominant disease(1) characterized by elevated serum ferritin levels and bilateral cataract development early in life.(2,3) Hereditary hyperferritinemia-cataract syndrome is caused by a genetic alteration in the iron-responsive element in the 5’ untranslated region (UTR) of the ferritin light chain (FTL) gene.(4) The FTL gene is located in chromosome 19q13, contains four exons and encodes the light subunit of the ferritin protein. The 5’UTR region of the FTL and iron-regulating proteins are involved in the regulation of intracellular iron concentration.(5-10) Rather than a single mutational origin, several mutations of the FTL gene can trigger HHCS.
At least 25 different genetic alterations, including the whole iron responsive element structure, have been reported in families with HHCS. Sporadic cases due to de novo mutations have also been described.(11,12) Some of these genetic alterations interfere with the loop that interacts directly with iron regulatory proteins, while others affect the stems or the bulge of the iron-responsive element structure and modify its conformation.(13,14)
Specific genetic mutations in the iron-responsive element prevent it from binding to iron regulatory proteins, leading to continuous FTL gene synthesis and elevation of ferritin levels, with no impact on transferrin saturation (TS). This case report describes a Brazilian family with a clinical diagnosis of HHCS. Exon sequencing of the FTL gene was performed and revealed the presence of the genetic mutation c.-164C>G in the 5’UTR region.(14)
Study protocol
Four primer pairs were designed to explore the 4 exons (including an important 5’UTR region) of the FTL gene, extending to 20bps of intronic regions. Polymerase chain reaction (PCR) was carried out and the product purified with Exo SAP-IT (GE Healthcare, NJ, USA). Next, a reaction was prepared for Sanger sequencing using Applied Biosystems 3130/3130xl Genetic Analyzers. After sequencing, the electropherogram was analyzed using the Geneious software (Biomatters).(15)
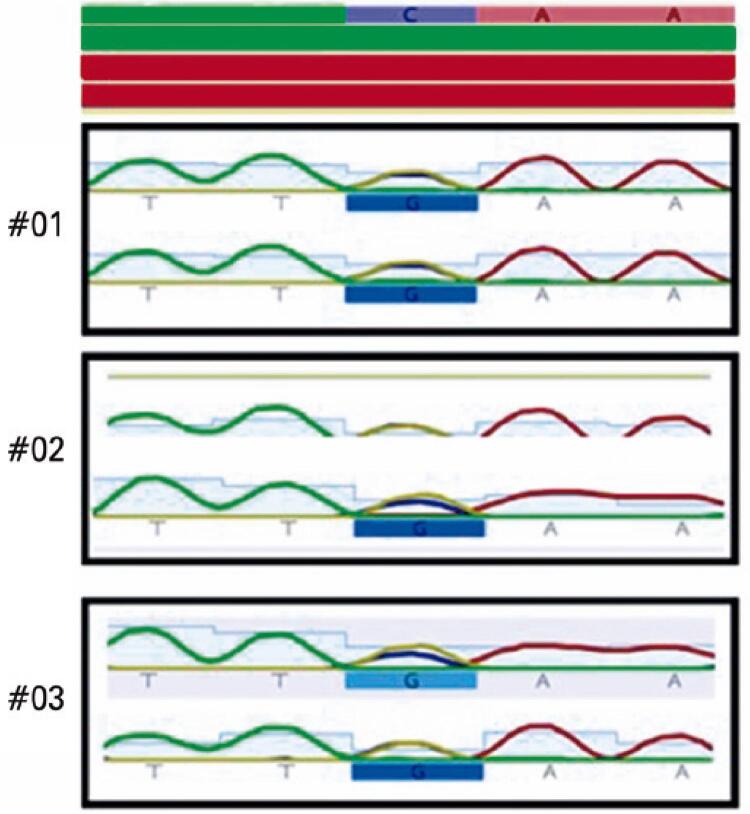
Sequencing of the 5’UTR region of the FTL gene revealed the pathogenic c.-164C>G mutation (Figure 1), first described in 2006, in all three family members.(16)
Figure 1. Ferritin light chain gene sequencing results. Patients #01, #02, #03: heterozygous genotype for the c.-164C>G pathogenic mutation.
The Ethics Committee of Escola Paulista de Medicina (EPM), Universidade Federal de São Paulo approved the study protocol (CAAE: 01507518.5.0000.5505; # 3.439.573). The participants signed a consent form prior to entering the study.
CASE REPORT
A 45-year-old Brazilian female patient living in São Paulo, Brazil, was referred to our service in 2016. Her first laboratory tests revealed iron levels of 100mcg/dL and serum ferritin (SF) levels of 1,487ng/mL and plasma TS of 28%. No signs of hepatic iron overload were seen on magnetic resonance imaging and her liver iron concentration was 1.1mg/g. Echocardiogram and abdominal ultrasound findings were unremarkable. She was HBsAg- and anti-HCV-negative. Genetic analysis failed to detect the pathogenic mutations p.Cys282Tyr and p.His63Asp in the HFE. Tests were repeated in 2020, with the following results: iron level of 80mcg/dL, SF level of 1,434ng/mL and TS of 33%. The second magnetic resonance imaging report described absence of hepatic iron overload, liver iron concentration of 1.0mg/g and mild hepatic steatosis. The reason she had sought treatment was a personal and family history of decreased visual acuity and glare. She had been diagnosed with bilateral cataract at the age of 25 years. Progressive glare prompted bilateral cataract surgery when she was in her fifties. In patients with HHCS, cataracts may develop early in infancy(17) and have been described as several dust-like lens opacities.(18)
The mother of the index case is 72 years old. In 2016, she had the following laboratory test results: SF of 1,703ng/mL and TS of 46%. She was also HBsAg- and anti-HCV-negative. Tests were repeated in 2020 and revealed iron level of 105μg/dL, SF level of 2,145ng/mL and TS of 34%. There was no evidence of iron overload on magnetic resonance imaging and her hepatic iron concentration was 1.3mg/g. No pathogenic mutations (p.Cys282Tyr and p.His63Asp) were found in the HFE gene.
In 2016, the son of the index case (an 11-year-old boy) had the following laboratory test results: iron level of 105μg/dL, SF level of 1,260ng/mL and TS of 28%. In 2020, his tests revealed iron level of 176μg/dL, SF level of 1,308ng/mL and TS of 46%. Magnetic resonance imaging showed no evidence of iron overload, and his hepatic iron concentration was 0.8mg/g. No pathogenic mutations (p.Cys282Tyr and p.His63Asp) were found in the HFE gene.
The proband and both family members were submitted to ophthalmic examination. Specific clinical and ophthalmological examinations revealed they all had cataracts.
DISCUSSION
The prevalence of HHCS in Brazil is unknown. However, in Australia the estimated prevalence is around 1/200,000. The clinical manifestations of HHCS are congenital cataract and persistent hyperferritinemia unrelated to iron overload. Congenital cataract is associated with several diseases. Hence, investigation of FTL gene mutations is seldom included in the diagnostic workup. Most patients affected by this syndrome are evaluated due to hyperferritinemia. HFE gene mutations associated with hemochromatosis are common in the Brazilian population,(19) and are the primary diagnostic hypothesis in these patients, leading to unnecessary diagnostic procedures and therapeutic phlebotomies.(20)
The frequency and in silico prediction of the pathogenic mutation in the population and the classification according to American College of Medical Genetics and Genomics (ACMG) criteria are shown in table 1. The mutation detected was assigned the “disease causing” status according to mutation Taster and was classified as “pathogenic” in ClinVar. As to others in silico predictors, no results were found. The mutation was also classified as “pathogenic” according to the ACMG.
Table 1. General patient information, clinical data, and classification of alterations according to American College of Medical Genetics and Genomics criteria.
| ID | Sex/Age | TS (%) / and SF (μg/L) 2016 | TS (%) / and SF (μg/L) 2020 | Liver iron concentration (mg/g) 2020 | FTL variants | ACMG criteria | ACMG |
|---|---|---|---|---|---|---|---|
| #01 | Female/41 | 28/1,487 | 33/1,434 | 1.0 | c-164 C>A | PS, PM, PP | Pathogenic |
| #02 | Female/67 | 46/1,703 | 34/2,145 | 1.3 | c-164 C>A | PS, PM, PP | Pathogenic |
| #03 | Male/11 | 28/1,260 | 46/1,308 | 0.8 | c-164 C>A | PS, PM, PP | Pathogenic |
ID: identification; TS: transferrin saturation; SF: serum ferritin; PS: pathogenic strong; PM: pathogenicity moderate; PP: pathogenicity supplementary; FTL: ferritin light chain; ACMG: American College of Medical Genetics and Genomics.
The genetic mutation c.-164C>G detected in the family described had been previously reported by another Brazilian group. That group described a case of a male Caucasian patient aged 7 years presenting with elevated serum ferritin and hemoglobin levels. The patient was tested for the pathogenic hemochromatosis mutation and for hepatitis, with negative results. The pathogenic mutation was also found in his mother.(20)
After analysis of the index case, the remaining cases (both index case relatives) could be screened. Laboratory tests revealed increased ferritin synthesis regardless of iron levels. The diagnosis was based on findings of clinical and specific examinations for cataract detection. The FTL gene was also sequenced and revealed the presence of the pathogenic genetic mutation in all three patients. This family is being followed by a medical team and is frequently examined, apart from having received medical guidance.
Patients with HHCS may be misdiagnosed with hemochromatosis, liver dysfunction or inflammation. Some patients may be submitted to invasive and unnecessary diagnostic procedures, such as liver biopsy, and may be inappropriately treated with phlebotomies, which may cause severe iron deficiency anemia. Hence the importance of accurate clinical and genetic diagnosis. Accurate diagnosis also contributes to earlier prescription of appropriate treatment.(21)
CONCLUSION
Genetic testing can be used for accurate diagnosis of hereditary hyperferritinemia-cataract syndrome to prevent misdiagnosis of hemochromatosis, other diseases associated with iron overload or ophthalmic diseases.
ACKNOWLEDGMENT
Coordenação de Aperfeiçoamento do Ensino Superior Pessoal 001. Fundação de Amparo à Pesquisa do Estado de São Paulo # 2019/08338-7.
REFERENCES
- 1.Craig JE, Clark JB, McLeod JL, Kirkland MA, Grant G, Elder JE, et al. Hereditary hyperferritinemia-cataract syndrome: prevalence, lens morphology, spectrum of mutations, and clinical presentations. Arch Ophthalmol. 2003;121(12):1753–1761. doi: 10.1001/archopht.121.12.1753. [DOI] [PubMed] [Google Scholar]
- 2.Girelli D, Corrocher R, Bisceglia L, Olivieri O, De Franceschi L, Zelante L, et al. Molecular basis for the recently described hereditary hyperferritinemia-cataract syndrome: a mutation in the iron-responsive element of ferritin L-subunit gene (the” Verona mutation”) Blood. 1995;86(11):4050–4053. [PubMed] [Google Scholar]
- 3.Bonneau D, Winter-Fuseau I, Loiseau MN, Amati P, Berthier M, Oriot D, et al. Bilateral cataract and high serum ferritin: a new dominant genetic disorder? J Med Genet. 1995;32(10):778–779. doi: 10.1136/jmg.32.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Girelli D, Bozzini C, Zecchina G, Tinazzi E, Bosio S, Piperno A, et al. Clinical, biochemical and molecular findings in a series of families with hereditary hyperferritinaemia-cataract syndrome. Br J Haematol. 2001;115(2):334–340. doi: 10.1046/j.1365-2141.2001.03116.x. [DOI] [PubMed] [Google Scholar]
- 5.Millonig G, Muckenthaler MU, Mueller S. Hyperferritinaemia-cataract syndrome: worldwide mutations and phenotype of an increasingly diagnosed genetic disorder. Human genomics. 2010;4(4):250–262. doi: 10.1186/1479-7364-4-4-250. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cremonesi L, Paroni R, Foglieni B, Galbiati S, Fermo I, Soriani N, et al. Scanning mutations of the 5′UTR regulatory sequence of l‐ferritin by denaturing high‐performance liquid chromatography: identification of new mutations. Br J Haematol. 2003;121(1):173–179. doi: 10.1046/j.1365-2141.2003.04253.x. [DOI] [PubMed] [Google Scholar]
- 7.Petroni RC, Rosa SE, Carvalho FP, Santana RA, Hyppolito JE, Nascimento CM, et al. Ferritin light chain gene mutations in two Brazilian families with hereditary hyperferritinemia-cataract syndrome. einstein (São Paulo) 2017;15(4):492–495. doi: 10.1590/S1679-45082017RC4006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Altés A, Pérez-Lucena MJ, Bruguera M, Comisión de Hiperferritinemia del Grupo Ibérico de Ferropatología Systematic approach to the diagnosis of hyperferritinemia. Med Clin. 2014;142(9):412–417. doi: 10.1016/j.medcli.2013.06.010. Spanish. Review. [DOI] [PubMed] [Google Scholar]
- 9.Baraibar MA, Barbeito AG, Muhoberac BB, Vidal R. A mutant light-chain ferritin that causes neurodegeneration has enhanced propensity toward oxidative damage. Free Radic Biol Med. 2012;52(9):1692–1697. doi: 10.1016/j.freeradbiomed.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barton JC, Beutler E, Gelbart T. Coinheritance of alleles associated with hemochromatosis and hereditary hyperferritinemia-cataract syndrome. Blood. 1998;92(11):4480. [PubMed] [Google Scholar]
- 11.Arosio C, Fossati L, Viganò M, Trombini P, Cazzaniga G, Piperno A. Hereditary hyperferritinemia cataract syndrome: a de novo mutation in the iron responsive element of the L-ferritin gene. Haematologica. 1999;84(6):560–561. [PubMed] [Google Scholar]
- 12.McLeod JL, Craig J, Gumley S, Roberts S, Kirkland MA. Mutation spectrum in Australian pedigrees with hereditary hyperferritinaemia-cataract syndrome reveals novel and de novo mutations. Br J Haematol. 2022;118(4):1179–1182. doi: 10.1046/j.1365-2141.2002.03690.x. [DOI] [PubMed] [Google Scholar]
- 13.Allerson CR, Cazzola M, Rouault TA. Clinical severity and thermodynamic effects of iron-responsive element mutations in hereditary hyperferritinemia-cataract syndrome. J Biol Chem. 1999;274(37):26439–26447. doi: 10.1074/jbc.274.37.26439. [DOI] [PubMed] [Google Scholar]
- 14.Jaffrey SR, Haile DJ, Klausner RD, Harford JB. The interaction between the iron-responsive element binding protein and its cognate RNA is highly dependent upon both RNA sequence and structure. Nucleic Acids Res. 1993;21(19):4627–4631. doi: 10.1093/nar/21.19.4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alvarenga AM, da Silva NK, Fonseca PF, Oliveira TG, da Silva Monteiro JB, Cançado RD, et al. Novel mutations in the bone morphogenetic protein 6 gene in patients with iron overload and non-homozygous genotype for the HFE p.Cys282Tyr mutation. Blood Cells Mol Dis. 2020;84:102444. doi: 10.1016/j.bcmd.2020.102444. [DOI] [PubMed] [Google Scholar]
- 16.Papanikolaou G, Chandrinou H, Bouzas E, Contopoulos-Ioannidis D, Kalotychou V, Prentzas K, et al. Hereditary hyperferritinemia cataract syndrome in three unrelated families of western Greek origin caused by the C39> G mutation of L-ferritin IRE. Blood Cells Mol Dis. 2006;36(1):33–40. doi: 10.1016/j.bcmd.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Girelli D, Corrocher R, Bisceglia L, Olivieri O, Zelante L, Panozzo G, et al. Hereditary hyperferritinemia-cataract syndrome caused by a 29-base pair deletion in the iron responsive element of ferritin L-subunit gene. Blood. 1997;90(5):2084–2088. [PubMed] [Google Scholar]
- 18.Cazzola M, Bergamaschi G, Tonon L, Arbustini E, Grasso M, Vercesi E, et al. Hereditary hyperferritinemia-cataract syndrome: relationship between phenotypes and specific mutations in the iron-responsive element of ferritin light-chain mRNA. Blood. 1997;90(2):814–821. [PubMed] [Google Scholar]
- 19.Ferreira AC, Oliveira VC, Caxito FA, Gomes KB, Castro AM, Pardini VC. Prevalence of C282Y and H63D mutations in the HFE gene of Brazilian individuals with clinical suspicion of hereditary hemochromatosis. Rev Bras Hematol Hemoter. 2008;30(5):379–383. [Google Scholar]
- 20.Herkenhoff ME, Pitlovanciv AK, Remualdo VR. Prevalence of C282Y and H63D mutations in the HFEgene in patients from São Paulo and Southern Brazil. J Bras Patol Med Lab. 2016;52(1):21–24. [Google Scholar]
- 21.Assis RA, Kay FU, Conti FM, Campregher PV, Szarf G, Diniz MS, et al. The role of magnetic resonance imaging‐T2* in the evaluation of iron overload early in hereditary hemochromatosis. A cross‐sectional study with 159 patients. Am J Hematol. 2015;90(12):E220–E221. doi: 10.1002/ajh.24189. [DOI] [PubMed] [Google Scholar]