Abstract
Many epidemiological studies have shown an increased risk of venous thromboembolism (VTE) in patients with rheumatoid arthritis (RA). RA and VTE share some background factors, such as increasing age, smoking, and obesity. At the same time, other VTE factors, such as knee replacement and oral contraceptive pills, occur commonly in RA patients. In addition, the chronic inflammatory state of RA might hypothetically lead to endothelial injury and a hypercoagulable state. Two critical pathophysiological pathways lead to VTE. Recently, concerns increased about the increased risk of VTE in patients using Janus Kinase inhibitors. This review aims at reviewing the risk of VTE in RA and the role of traditional risk factors and disease-related inflammation and develops a conceptual framework that describes the interaction between these factors.
Keywords: rheumatoid arthritis, venous thromboembolism, Janus Kinase inhibitors
Introduction
Venous thromboembolic (VTE) disease is a major health problem affecting 100 /100,000 persons, which is associated with significant disability and mortality.1 Extensive epidemiological studies have indicated that patients with rheumatoid arthritis (RA) are at a higher risk of developing VTE than age- and sex-matched controls, even after adjusting for clinical risk factors and acute-phase reactants.2,3 Both diseases have common background demographics such as increased age,4,5 obesity,6,7 smoking,8,9 and certain comorbidities. In addition, the development of a VTE event in an RA patient might be triggered by immobility due to fracture occurrence, hospitalization, and joint replacement.10 These factors might partially explain the increased risk, but RA inflammatory milieu might play a role in causing endothelial injury and increasing hypercoagulability.
Additionally, female RA patients commonly use oral contraceptive pills during premenopausal periods due to the teratogenicity of many treatment options. The management of RA has evolved significantly in the last three decades. This was mainly due to the approval of highly effective therapies and the developing of a “Treat To Target” strategy.11 Conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs) and biological (bDMARDs) have played a major role in controlling inflammation, reducing disability, and developing morbidity and mortality.12
Recently, the introduction of Janus kinase inhibitors (JAKi) to treat RA and the observation of increased risk of VTE in the associated clinical trial program have drawn the attention of the rheumatology community to the risk of VTE in RA patients.13
VTE prevention should be aimed at high-risk patients through medical treatment, mechanical methods, and early mobilization.14–16 Heparin, warfarin, and direct oral anticoagulants are the main therapeutic classes.17,18
RA and the Virchow’s Triad
Virchow’s triad, comprising venous stasis, endothelial injury, and a hypercoagulable state, was first described in 1856.19 In this condition, an imbalance between procoagulants and anticoagulants leads to a hypercoagulable state. Venous thrombi comprise two layers: an inner rich platelet layer surrounded by a dense red cell fibrin clot. Clots are usually formed in areas with altered blood flow, such as pockets adjacent to venous valves in the legs.20 Here we dissect how RA affects each component of Virchow’s triad.
Endothelial Injury
Endothelial injury in RA patients primarily occurs secondary to inflammation. It has been linked to the positivity of antiphospholipid antibodies, human leucocyte antigen (HLA) status such as HLA-DRB1*04:01,21 and some unusual genotypes of tumor necrosis factor inhibitors (TNF) or plasminogen activator inhibitor-1 (PAI-1).22
In the early stages of RA, a pro-inflammatory state plays a major role in endothelial dysfunction by activating endothelial cells, leading to altered endothelial permeability and increased leukocyte and platelet adhesion, resulting in increased monocyte–endothelial interaction.23 During inflammation, monocytes express intercellular adhesion molecules, which are induced by pro-inflammatory cytokines such as IL-1β, TNF-α, and C-reactive protein (CRP).23
The activation of coagulation factors of endothelial origins, such as the von Willebrand factor and PAI-1, may play a significant role in RA and thrombosis.24
Hypercoagulability
In RA patients, inflammation regulates thrombotic responses by three important components: upregulating procoagulants (homocysteine and P-selectin), downregulating anticoagulants (thrombomodulin and protein C and S), and suppressing fibrinolysis.25
Upregulating Procoagulants
Fibrinogen, D-dimer, cytokines (such as IL-6, IL-8, and TNF), and CRP, considered inflammatory markers, are associated with an increased risk of thrombosis and may play significant roles in VTE.26 Homocysteine has been increasingly observed in RA and may increase the risk of venous thrombosis.27 A high homocysteine level is considered to have a modest association with atherothrombosis or venous thrombosis.28 P-selectin, a member of adhesion receptors that normally generates procoagulant particles and activates platelets, has been an important predictor of VTE development.29,30 Furthermore, it was found to be an important biomarker in leucocyte-endothelial interaction and RA-related thrombocytosis.31,32
Downregulating Anticoagulants
Natural anticoagulant mechanisms reduce the thrombotic response but may be depressed by inflammatory mediators. Thrombomodulin is a transmembrane glycoprotein synthesized by vascular endothelial cells and is distributed on the surface of the vein, artery, and capillary endothelial cells. Its gene polymorphism has been associated with an increased risk of VTE.33 Prothrombotic activities are believed to exert a toxic effect on the endothelium and lead to decreased thrombomodulin expression.34 Therefore, the protein C pathway is considered a major target. TNF-α specifically downregulates Thrombomodulin and the endothelial cell protein C receptor; while both are needed for optimal protein C activation, they are downregulated by inflammatory mediators. In addition, the protein S glycoprotein is an essential natural anticoagulant for activating the activation protein C pathway, and tissue pathway factor inhibitor can be downregulated in a chronic inflammatory state, resulting in the impaired anticoagulant function of activated protein C.35,36
Suppressing Fibrinolysis
The thrombin activatable fibrinolysis inhibitor (TAFI) is a proenzyme that activates the fibrinolytic system once activated by factors such as thrombin/plasmin and thrombomodulin.37 TAFI has been found to be elevated in RA patients compared to controls,38 especially patients with active inflammation.39 Therefore, higher activated TAFI may cause a transient hypercoagulable state that leads to VTE.40
Antiphospholipid Antibodies
The expression of antiphospholipid antibodies is considered a risk factor for VTE, arterial thrombosis, and pregnancy-related complications in patients with rheumatic diseases, especially those with background lupus or primary antiphospholipid syndrome (APS).41 In the case of RA, the literature is scarce, and no solid conclusion has been drawn due to the high variability in the observed results. In a review published in 2006 by Olech and Merrill, the median prevalence of aPL antibodies in RA patients was 22% in samples not exceeding 200 patients, with a few studies showing some relation.42–44 However, the functionality of these antibodies is questionable. However, their persistence is unknown, as aPL antibodies can result from infection or are induced by drugs such as TNF inhibitors (TNFi).45
Smoking
Smoking is an important environmental risk factor for both RA and VTE.46,47 Smoking primarily causes a hypercoagulable state through different mechanisms. An increase in procoagulant factors (II, V, VIII, X, and XIII), homocysteine, and tissue factor levels is unbalanced by a decrease in anti-thrombin III and tissue factor pathway inhibitor levels. Epidemiologically, Cigarette smoking (CS), intensity, and duration are directly related to the risk of RA development, even after CS cessation. Di Giuseppe et al found in a meta-analysis including three prospective and seven case-control studies that the risk of developing RA increased by 26% in CS users who smoked 1–10 pack-years and by 94% in those with more than 20 pack-years. A meta-analysis also showed that rheumatoid factor (RF)-positive smokers had a higher risk of RA than RF-negative smokers.47 On the other hand, Hedström et al conducted a case–control study in a Swedish population with 3655 cases and 5883 controls and showed a dose-dependent increase in RA risk regardless of whether the anti-citrullinated peptide antibodies (ACPA) were positive or negative. When comparing the duration and intensity of CS, duration was found to have a stronger influence on the association between CS and RA.
Two closely published systematic reviews showed an increased risk of VTE in current and former smokers. Cheng et al found a relative risk (RR) of 1.23 (95% CI 1.14–1.33) for current and 1.10 (95% CI 1.03–1.17) for former smokers.46 Similarly, Zhang et al described an RR of (1.24; 95% CI:1.14–1.35) for current and (1.05; 95% CI:1.01–1.10) for former smokers.9
Hyper-Viscosity and Venous Stasis
The exact mechanisms underlying increased plasma viscosity and subsequent VTE development in RA remain unknown. Two possible factors might explain this phenomenon:
Intrinsic Factors
Acute-phase reactants are elevated in many autoimmune diseases, including RA, contributing to increased plasma viscosity and risk of thrombosis. This includes CRP, erythrocyte sedimentation rate (ESR), coagulation factor VIII, fibrinogen, and von Willebrand factor.48
Immobility
RA causes joint destruction that leads to disability and immobility.49 Also, RA is the second cause of joint replacement after osteoarthritis,50 a high-risk surgery for VTE development. Finally, RA patients are at increased risk of infection,51 osteoporotic fractures,52 cardiovascular,53 and pulmonary diseases,54 all leading to hospitalization and immobility.
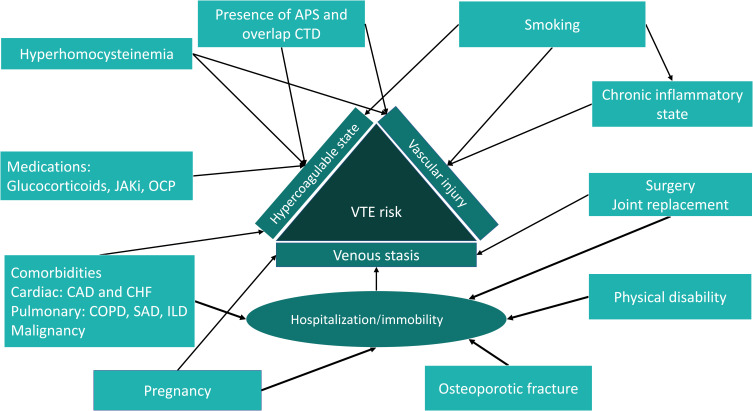
Figure 1 shows the interaction between intrinsic and extrinsic risk factors for VTE in patients with RA.
Figure 1.
Conceptualization framework describing the interaction between intrinsic and extrinsic venous thromboembolism risk factors in rheumatoid arthritis patients.
Abbreviations: APS, antiphospholipid syndrome; CTD, connective tissue disease; JAKi, Janus kinase inhibitor; OCP, oral contraceptive pills; VTE, venous thromboembolism; CAD, coronary artery disease; CHF, congestive heart failure; COPD, chronic obstructive lung disease; SAD, small airway disease; ILD, interstitial lung disease.
Risk of VTE in RA Patients
It has been proposed that patients with RA have an increased risk of VTE. Lee and Pope reported a cumulative incidence rate of 2.18% (95% CI:1.82% to 2.54%) and an odds ratio of 2.23 (95% CI: 2.02 to 2.47) compared to age-sex-matched populations of.55 A recent meta-analysis of nine studies by Ungprastert et al showed a pooled risk ratio of VTE of 1.96 (95% CI 1.81–2.11) in patients with RA.2 In another systematic review, Hu et al demonstrated similar results, with a doubled OR of VTE (2.23, 95% CI:1.79 to 2.77, p<0.001) compared to control3 (Table 1). Although recent hospitalization is an established risk factor for VTE,1,56,57 patients with RA have an increased risk of VTE, irrespective of hospitalization. This risk was well observed in a UK cohort showing a VTE relative risk of 2.16 in outpatient settings.58 Furthermore, the risk of VTE was increased in RA patients independent of other traditional risk factors, such as chronic comorbidities, recent fractures, and use of oral contraceptive pills.59,60 In addition, the occurrence of the first VTE was associated with a threefold increased risk of cardiovascular disease in patients.61 RA disease activity is associated with an increased risk of VTE.61,62 In a recent Swedish cohort, the risk of VTE increased twofold in patients with evidence of disease activity compared to patients in remission.62 Although it has been proposed that longer disease duration increases the risk of VTE,59,63 many studies have shown that the relative risk is higher in the first year and remains relatively stable in subsequent years.56,58,60,64,65 Several studies have observed an association between increased body mass index and risk of VTE.56,61,63,66,67 In a recent Italian cohort, obesity was associated with a hazard ratio (HR) of 1.37 for developing VTE.63 In another study by Ozen et al, obesity was found to be associated with an increased risk of VTE (HR 1.46 (95% CI), (1.13–1.87))61 (Table 2).
Table 1.
Summary of Systematic Reviews Examining Venous Thromboembolism Risk in Rheumatoid Arthritis Patients
| First Author | Year | Number of Studies | Inclusion Criteria | Main Outcomes |
|---|---|---|---|---|
| HU et al3 | 2021 | 12 | Studies evaluating the incidence of VTE, DVT, and PE in RA patients | OR of DVT in RA patients relative to controls: (2.25, 95% CI: 1.70 to 2.98, p<0.001) OR of PE in RA patients relative to controls (2.15, 95% CI: 1.39 to 3.49, p=0.001). OR of VTE in RA patients relative to controls (2.23, 95% CI: 1.79 to 2.77, p<0.001) |
| Lee and Pope.55 | 2014 | 10 | Studies evaluating the incidence of VTE, DVT, and PE in RA patients | OR of DVT in RA patients relative to controls: 2.23 (95% CI: 2.02 to 2.47) Cumulative incidence of VTE is 2.18% (95% CI:1.82% to 2.54%) |
| Ungprasert et al2 | 2014 | 9 | Observational studies (case-control, cross-sectional, cohort) evaluating the association between RA and VTE, DVT or PE | Pooled risk ratio for VTE 1.96 (95% CI 1.81–2.11) Pooled risk ratio for DVT= 2.08 (95% CI 1.75–2.47) Pooled risk ratio for PE= 2.17 (95% CI 2.05–2.31) |
Abbreviations: RA, rheumatoid arthritis; VTE, venous thromboembolism; DVT, deep venous thrombosis; PE, pulmonary embolism; CI, confidence interval; OR, odds ratio.
Table 2.
Summary of Major Epidemiological Studies Evaluating Venous Thromboembolism in Rheumatoid Arthritis Patients
| First Author | Year | Country | Study Design | Sample Size | Main Outcomes |
|---|---|---|---|---|---|
| Matta et al87 | 2009 | United States | Cohort | 895,873,000 | Incident of DVT 0.9 in RA vs 0.4 in non-RA, RR 2.25. Incident of PE 1.6 in RA vs 0.9 in non-RA, RR 1.90. Incident of VTE 2.3 in RA vs 1.1 in non-RA, RR 1.99. |
| Davies et al74 | 2011 | United Kingdom | Cohort | 15,554 | IR was 3.7/1000 person-year in RA with TNFi vs 3.7/1000 person-year in RA with csDMARD. Adjusted HR of VTE with TNFi group= 0.8. |
| Kang et al88 | 2012 | Taiwan | Case control | 25,965 | OR of RA in cases of VTE= 1.92 (95% CI, 1.46–2.53; P < 0.001). |
| Holmqvist et al64 | 2012 | Sweden | Prospective cohort study | 215,175 | Prevalent cohort: IR of VTE was 5.9/1000 person-year in RA vs 2.8/1000 person-year in non-RA, HR= 2. Incident cohort: IR of VTE was 4.5/1000 person-year in RA vs 1.6/1000 person-year in non-RA, HR= 1.6. |
| Choi et al58 | 2012 | United Kingdom | Cohort | 105,365 | IR of DVT 2.1/1000 patient-year in RA vs 1.0/1000 patient-year in non-RA. IR of PE 1.5/1000 patient-year in RA vs 0.7/1000 patient-year in non-RA. IR for VTE 3.3/1000 patient-year in RA vs 1.5/1000 patient-year in non-RA. RR of VTE in RA after adjustment for multivariant 2.14. |
| Bacani et al56 | 2012 | United States | Cohort | 928 | Cumulative incidence: DVT 3.1±10 in RA vs 1.7±0.9 in non-RA (P value= 0.034)PE 4.8±1.5 in RA vs 1.6±0.7 in non-RA (P value=0.050). VTE 6.7±1.7 in RA vs 2.8±1.1 in non-RA (P value=0.005). Rate of VTE = 7.4/1000 patient-year. HR of VTE= 3.6 (95% confidence interval [95% CI] 1.5–8.6) in RA group. |
| Chung et al59 | 2013 | Taiwan | Cohort | 146,190 | IR of DVT 1.7/1000 person-years in RA vs 0.322/1000 person-years in non-RA, HR = 3.36. IR of PE 0.36/1000 person-years in RA vs 0.175/1000 in non-RA, HR= 2.07. |
| Kim et al67 | 2013 | United States | Retrospective cohort | 110,715 | IR of DVT 4.5/1000 person-year in RA vs 2.1/1000 person-year in non-RA, Risk ratio= 2.2. IR of PE 2.6/1000 person-year in RA vs 0.9/1000 person-year in non-RA, Risk ratio= 2.7. IR of VTE 6.1/1000 person-year in RA vs 2.5/1000 person-year in non-RA, Risk ratio= 2.4. |
| Yusuf et al89 | 2015 | United States | Cohort | 296,352 | IR of VTE was 4.90/1000 person-year in RA vs 1.91/1000 person-year in controls. IR of VTE was 19.74/1000 person-year in autoimmune hemolytic anemia. IR of VTE was 7.72/1000 person-year in immune thrombocytopenic purpura. IR of VTE was 9.89/1000 person-year in lupus patients. |
| Ogdie et al90 | 2018 | United States | Retrospective Cohort | 1,483,705 | IR of DVT was 3.7 and 3.4/10,000 person-year in RA with DMARDs vs no DMARDs, respectively, and 2.1/10,000 person-year in non-RA. IR of PE was 1.3 and 0.9/10,000 person-year in RA with DMARDs vs no DMARDs, respectively, and 0.5/10,000 person-year in non-RA. IR of VTE was 4.7 and 4.2/10,000 person-year in RA with DMARDs vs no DMARDs, respectively, and 2.5/10,000 person-year in non-RA. HR of VTE in RA = 1.29 in no DMARD group vs 1.35 in DMARD group. |
| Mansour et al91 | 2019 | Israel | Cohort | 69,755 | IR of VTE was 6.92% in RA vs 3.18% in non-RA. OR of VTE in RA = 2.27. |
| Galloway et al66 | 2020 | United Kingdom | Cohort | 266,890 | HR of VTE was 1.54 in RA. HR of PE was 1.57 in RA. HR of DVT was 1.64 in RA vs HR= 1 in control. HR of VTE was 1.27,1.73, 1.20 in UC, CD, PsA respectively. HR of PE was 1.23, 1.69,1.34 in UC, CD, PsA respectively. HR of DVT was 1.33,1.96,1.34 in UC, CD, PsA respectively. vs HR =1 in control. |
| Molander et al62 | 2020 | Sweden | Cohort | 262,159 | IR of DVT 0.45/1000 person-year in RA vs 0.22/1000 person-year in non-RA. IR of PE 0.26/1000 person-year in RA vs 0.14/1000 person-year in non-RA. IR of VTE 0.71/1000 person-year in RA vs 0.36 in non-RA. Adjusted RR for VTE in RA = 1.88. Within RA cohort: IR of VTE was 0.52, 0.63, 0.80,1.08 in remission, low, intermediate, and high disease activity, respectively. Adjusted RR of VTE was 1.12,1.48, and 2.03 in low, intermediate, and high disease activity, respectively. |
| Chen et al72 | 2021 | Taiwan | Cohort | 28,873 | IR of VTE in RA with csDMARD was 12.61/10,000 person-year vs 14.33 was 12.61/10,000 person-year in RA with bDMARDs. HR of VTE in bDMARDs was= 1.11 (not statically significant). |
| Dore et al92 | 2021 | United States | Retrospective cohort | VTE incident in csDMARD naive = 0.8 (0.7 for DVT, 0.3 for PE) VTE incident in csDMARD switchers= 0.7 (0.6 for DVT, 0.3 for PE) VTE incident in bDMARD switchers= 0.9 (0.7 for DVT, 0.3 for PE). | |
| Conforti et al63 | 2021 | Italy | Retrospective Cohort | IR of VTE was 7.8 per 1000 person-year in the RA cohort. IR of VTE was 1 per 1000 person-year in the general population from previous data. HR for predictive factors: Age = 1.07 (P value= 0.015) BMI = 1.37 (P value= 0.025) Disease duration= 1.13 (P value= 0.006). |
|
| Ozen et al61 | 2021 | United States | Cohort | Number of VTE events = 539 HR of BMI >30 and VTE= 1.47 HR of steroid use and VTE= 1.99 HR of age >65 and VTE= 2.32 HR of RDCI and VTE= 1.20 HR of recent fracture and VTE= 1.62 HR of hospitalization and VTE= 1.09 HR of recent surgery and VTE= 1.18. HR of moderate/sever disease activity and VTE = 1.31 |
|
| Li et al60 | 2021 | Canada | Cohort | 117,220 | IR of DVT 2.82 per 1000 person-year in RA vs.1.94/1000 person-year in non-RA. IR of PE 1.43/1000 person-year in RA vs 1.03/1000 person-year in non-RA. IR of VTE 3.79/1000 person-year in RA vs 2.70/1000 person-year in non-RA. Fully adjusted HR of VTE = 1.28. |
Abbreviations: RA, rheumatoid arthritis; VTE, venous thromboembolism; DVT, deep venous thrombosis; PE, pulmonary embolism; CI, confidence interval; OR, odds ratio; RR, relative risk; HR, hazard ratio; IR, incidence rate; DMARDs, disease-modifying anti-rheumatic drugs; csDMARDs, conventional synthetic DMARDs; bDMARDs, biological DMARDs; TNFi, tumor necrosis factor inhibitors; UC, ulcerative colitis; CD, Crohn’s disease; PsA, psoriatic arthritis; BMI, body mass index; RDCI, rheumatic disease comorbidity index.
RA Treatment and the Risk of VTE
Glucocorticoids (GCs) play an essential role in the management of RA. Efforts have been made to limit their use as bridging therapy or during flares;68 their chronic use is still significant but decreases over time.69 GC use increases VTE risk 2-3-fold in different patient populations.70 GCs further increase endothelial injury by decreasing nitric oxide levels and increasing adhesion molecule expression. Finally, GCs cause hypercoagulability by increasing factors II and VIII and the von Willebrand factor, critical procoagulant factors.71
bDMARDs have not been linked to an increased risk of VTE in RA.56,72–75 In a large Chinese cohort studying the risk of VTE with bDMARDs compared to csDMARDs, there was no statistically significant association between biologic use and VTE (HR, 1.11 (95% CI 0.79–1.55); (p > 0.05).72 In another cohort study on the risk of VTE and TNFi use, there was no significant association between TNFi and VTE (HR of TNFi group was 0.8).74 The significant effect of JAKi on different cytokine pathways may hypothetically reduce the risk of thrombosis. However, the outcome could not be predicted as some cytokines have a pleiotropic effect, and some have both pro- and anti-inflammatory effects.76 The increased risk was particularly observed in the group treated with tofacitinib 10 mg twice daily in an extensive analysis that included clinical trial programs and the (Consortium of Rheumatology Researchers of North America) CORRONA registry.77 The Oral Surveillance Study confirmed these findings, a randomized, open-label, non-inferiority, post-authorization, safety end-point trial that compared the long-term safety of tofacitinib 5 mg and 10 mg twice daily compared to TNFi in an enriched population of patients with increased risk for major adverse cardiovascular events and cancer (age ≥50 years and at least one cardiovascular risk factor). VTE had a numerically higher Hazard ratio for the 5 mg dosing group (HR 1.66 (0.76–3.63)) and a statistically significant Hazard ratio for the 10 mg dosing (HR 3.52 (1.74–7.12)).78 These findings prompted the Food Drug Administration and the European Medicine Agency to select patients for the entire JAKi class cautiously. In contrast, multiple systematic reviews showed no increased risk of VTE in different JAKi, and variable patient populations compared to controls, even when assessing different dosing arms (Table 3).79–85 These conflicting findings could be explained by the dilutional effect of low-risk patients in clinical trial programs who are classically young with high disease activity and lack significant comorbidities. In this subset of patients, the anti-cytokine effect of JAKi leads to a reduction in VTE following the control of RA-related inflammation. In patients with multiple risk factors, the impact on the JAK/STAT pathway and the inhibitory effect on some cytokines may be responsible for potentiating the risk of VTE. Therefore, it is important to stratify patients’ risk prior to JAKi initiation.86
Table 3.
Systematic Reviews Assessing Venous Thromboembolism Risk in Patients Treated with Janus Kinase Inhibitors
| First Author | Year | Number of Studies | Inclusion Criteria | Main Outcomes |
|---|---|---|---|---|
| Alves et al79 | 2022 | 42 | RA RCTs of baricitinib, filgotinib, peficitinib, tofacitinib, and upadacitinib. | No differences were observed between different JAKis regarding the risk of VTE compared with placebo |
| Bilal et al80 | 2021 | 29 | RCTs of JAK inhibitors, regardless of clinical condition, that reported adverse event data for the treatment and control groups | No association between the use of JAK inhibitors and the risk of VTE (odds ratio, 0.91; 95% CI, 0.57 to 1.47), even when cancer studies were excluded and analysis was stratified according to underlying disease. |
| Giménez et al81 | 2020 | 59 | RCTs and non-RCTs and controlled cohort studies (prospective or retrospective) comparing oral baricitinib or tofacitinib at any dose with another active drug or placebo in which patients received at least one dose of oral baricitinib or tofacitinib for any indication. | Overall, an odds ratio (OR) for VTE events of 0.29 (95% CI 0.10–0.84) for tofacitinib. -The ORs for VTE events for baricitinib was 3.39 (95% CI 0.82–14.04) overall. -The indirect meta-analysis comparing tofacitinib with baricitinib showed an OR for VTE events of 0.086 (95% CI 0.02–0.51) for tofacitinib and a superior safety profile for VTE events. -In the meta-regression analysis, the effect was 0.02 (95% CI −0.04 to 0.08) for tofacitinib and 0.01 (95% CI −1.29 to 1.26 for baricitinib. -Plotting data for tofacitinib showed that VTE risk increased with high doses. -The effect, however, was less than 1 for the 10- and 20-mg doses, indicating a protective effect. This effect was not observed for baricitinib. |
| Yates et al82 | 2020 | 42 | RCTs of JAKi therapy with a placebo comparator arm | IRR of VTE, PE and DVT in patients receiving JAKi were 0.68 (95% CI 0.36 to 1.29), 0.44 (95% CI 0.28 to 0.70) and 0.59 (95% CI 0.31 to 1.15), respectively. |
| Wang et al83 | 2020 | 20 | RTCs of tofacitinib or baricitinib, or upadacitinib in RA patients | VTE data were unavailable for tofacitinib or baricitinib, but there was no increase in risk with upadacitinib (15 mg daily: RR, 2.34; 95% CI, 0.34 to 15.92). |
| Xie et al84 | 2019 | 29 | RCTs in adult patients with immune-mediated inflammatory disorders using tofacitinib | There was a decreased rate of VTEs (OR 0.03, 95% CI 0.00–0.21) in patients initiating tofacitinib. Tofacitinib 10 twice daily was associated with an increase in VTEs risk (OR = 1.47, 95% CI 0.25–8.50) compared with the 5 mg regimen. |
| Xie et al | 2019 | 25 for placebo comparison 18 for dose dependence |
RTCs of tofacitinib or baricitinib, or upadacitinib in RA patients | There was no increased risk of VTEs in users of the 3 JAKi (OR 1.16 (0.48 to 2.81), p = 0.74). There was no dose dependent increase of VTE in any JAKi |
Abbreviations: RCT, randomized controlled trial; RA, rheumatoid arthritis; JAKi, Janus kinase inhibitor; VTE, venous thromboembolism; DVT, deep venous thrombosis; PE, pulmonary embolism; CI, confidence interval; OR, odds ratio; RR, relative risk; HR, hazard ratio; IR, incident rate.
Conclusion
The increased risk of VTE in RA patients can be explained by a complex interaction between intrinsic and extrinsic factors. Therefore, Modification of risk factors, adequate disease control, and appropriate risk stratification is recommended for VTE prevention.
Disclosure
Mohammed A. Omair received speaker honoraria from Abbvie, Actelion, Amgen, Bristol Myers Squibb, Glaxo-Smith-Kline, Hekma, Janssen, Lilly, New Bridge, Novartis, Pfizer, and Roche. The other authors have no conflicts of interest to declare.
References
- 1.White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I4–8. doi: 10.1161/01.CIR.0000078468.11849.66 [DOI] [PubMed] [Google Scholar]
- 2.Ungprasert P, Srivali N, Spanuchart I, Thongprayoon C, Knight EL. Risk of venous thromboembolism in patients with rheumatoid arthritis: a systematic review and meta-analysis. Clin Rheumatol. 2014;33(3):297–304. doi: 10.1007/s10067-014-2492-7 [DOI] [PubMed] [Google Scholar]
- 3.Hu LJ, Ji B, Fan HX. Venous thromboembolism risk in rheumatoid arthritis patients: a systematic review and updated meta-analysis. Eur Rev Med Pharmacol Sci. 2021;25(22):7005–7013. doi: 10.26355/eurrev_202111_27249 [DOI] [PubMed] [Google Scholar]
- 4.Xu B, Lin J. Characteristics and risk factors of rheumatoid arthritis in the United States: an NHANES analysis. PeerJ. 2017;5:e4035. doi: 10.7717/peerj.4035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stein PD, Hull RD, Kayali F, Ghali WA, Alshab AK, Olson RE. Venous thromboembolism according to age: the impact of an aging population. Arch Intern Med. 2004;164(20):2260–2265. doi: 10.1001/archinte.164.20.2260 [DOI] [PubMed] [Google Scholar]
- 6.Lu B, Hiraki LT, Sparks JA, et al. Being overweight or obese and risk of developing rheumatoid arthritis among women: a prospective cohort study. Ann Rheum Dis. 2014;73(11):1914–1922. doi: 10.1136/annrheumdis-2014-205459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahmani J, Haghighian Roudsari A, Bawadi H, et al. Relationship between body mass index, risk of venous thromboembolism and pulmonary embolism: a systematic review and dose-response meta-analysis of cohort studies among four million participants. Thromb Res. 2020;192:64–72. doi: 10.1016/j.thromres.2020.05.014 [DOI] [PubMed] [Google Scholar]
- 8.Sugiyama D, Nishimura K, Tamaki K, et al. Impact of smoking as a risk factor for developing rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. 2010;69(1):70–81. doi: 10.1136/ard.2008.096487 [DOI] [PubMed] [Google Scholar]
- 9.Zhang G, Xu X, Su W, Xu Q. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health. 2014;45(3):736–745. [PubMed] [Google Scholar]
- 10.Anderson FA, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I9–16. doi: 10.1161/01.CIR.0000078469.07362.E6 [DOI] [PubMed] [Google Scholar]
- 11.Smolen JS. Treat-to-target: rationale and strategies. Clin Exp Rheumatol. 2012;30(4 Suppl 73):S2–6. [PubMed] [Google Scholar]
- 12.Curtis JR, Singh JA. Use of biologics in rheumatoid arthritis: current and emerging paradigms of care. Clin Ther. 2011;33(6):679–707. doi: 10.1016/j.clinthera.2011.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kragstrup TW, Glintborg B, Svensson AL, et al. Waiting for JAK inhibitor safety data. RMD Open. 2022;8(1):e002236. doi: 10.1136/rmdopen-2022-002236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roderick P, Ferris G, Wilson K, et al. Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis. Health Technol Assess. 2005;9(49):iii–iv, ix–x, 1–78. doi: 10.3310/hta9490 [DOI] [PubMed] [Google Scholar]
- 15.Greenall R, Davis RE. Intermittent pneumatic compression for venous thromboembolism prevention: a systematic review on factors affecting adherence. BMJ Open. 2020;10(9):e037036. doi: 10.1136/bmjopen-2020-037036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lau BD, Murphy P, Nastasi AJ, et al. Effectiveness of ambulation to prevent venous thromboembolism in patients admitted to hospital: a systematic review. CMAJ Open. 2020;8(4):E832–e843. doi: 10.9778/cmajo.20200003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hong J, Ahn SY, Lee YJ, et al. Updated recommendations for the treatment of venous thromboembolism. Blood Res. 2021;56(1):6–16. doi: 10.5045/br.2021.2020083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Konstantinides SV, The MG. 2019 ESC Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism. Eur Heart J. 2019;40(42):3453–3455. doi: 10.1093/eurheartj/ehz726 [DOI] [PubMed] [Google Scholar]
- 19.Ackerknecht EH, Virchow R. Doctor, Statesman, Anthro-Pologist. University of Wisconsin, Madison; 1953. [Google Scholar]
- 20.Mammen EF. Pathogenesis of venous thrombosis. Chest. 1992;102(6 Suppl):640s–644s. doi: 10.1378/chest.102.6_Supplement.640S [DOI] [PubMed] [Google Scholar]
- 21.van Drongelen V, Holoshitz J. Human Leukocyte Antigen-Disease Associations in Rheumatoid Arthritis. Rheum Dis Clin North Am. 2017;43(3):363–376. doi: 10.1016/j.rdc.2017.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin YJ, Anzaghe M, Schulke S. Update on the pathomechanism, diagnosis, and treatment options for rheumatoid arthritis. Cells. 2020;9(4). doi: 10.3390/cells9040880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mameli A, Barcellona D, Marongiu F. Rheumatoid arthritis and thrombosis. Clin Exp Rheumatol. 2009;27(5):846–855. [PubMed] [Google Scholar]
- 24.Wallberg-Jonsson S, Cvetkovic JT, Sundqvist KG, Lefvert AK, Rantapaa-Dahlqvist S. Activation of the immune system and inflammatory activity in relation to markers of atherothrombotic disease and atherosclerosis in rheumatoid arthritis. J Rheumatol. 2002;29(5):875–882. [PubMed] [Google Scholar]
- 25.Fox EA, Kahn SR. The relationship between inflammation and venous thrombosis. A systematic review of clinical studies. Thromb Haemost. 2005;94(2):362–365. doi: 10.1160/TH05-04-0266 [DOI] [PubMed] [Google Scholar]
- 26.Zacharski LR, Brown FE, Memoli VA, et al. Pathways of coagulation activation in situ in rheumatoid synovial tissue. Clin Immunol Immunopathol. 1992;63(2):155–162. doi: 10.1016/0090-1229(92)90008-C [DOI] [PubMed] [Google Scholar]
- 27.Yxfeldt A, Wallberg-Jonsson S, Hultdin J, Rantapaa-Dahlqvist S. Homocysteine in patients with rheumatoid arthritis in relation to inflammation and B-vitamin treatment. Scand J Rheumatol. 2003;32(4):205–210. doi: 10.1080/03009740310003686 [DOI] [PubMed] [Google Scholar]
- 28.Welch GN, Loscalzo J. Homocysteine and atherothrombosis. N Engl J Med. 1998;338(15):1042–1050. doi: 10.1056/NEJM199804093381507 [DOI] [PubMed] [Google Scholar]
- 29.Ardoin SP, Shanahan JC, Pisetsky DS. The role of microparticles in inflammation and thrombosis. Scand J Immunol. 2007;66(2–3):159–165. doi: 10.1111/j.1365-3083.2007.01984.x [DOI] [PubMed] [Google Scholar]
- 30.Antonopoulos CN, Sfyroeras GS, Kakisis JD, Moulakakis KG, Liapis CD. The role of soluble P selectin in the diagnosis of venous thromboembolism. Thromb Res. 2014;133(1):17–24. doi: 10.1016/j.thromres.2013.08.014 [DOI] [PubMed] [Google Scholar]
- 31.Schmitt-Sody M, Metz P, Gottschalk O, et al. Platelet P-selectin is significantly involved in leukocyte-endothelial cell interaction in murine antigen-induced arthritis. Platelets. 2007;18(5):365–372. doi: 10.1080/09537100701191315 [DOI] [PubMed] [Google Scholar]
- 32.Ertenli I, Kiraz S, Arici M, et al. P-selectin as a circulating molecular marker in rheumatoid arthritis with thrombocytosis. J Rheumatol. 1998;25(6):1054–1058. [PubMed] [Google Scholar]
- 33.Xu J, Jin J, Tan S. Association of thrombomodulin gene polymorphisms with susceptibility to atherosclerotic diseases: a meta-analysis. Ann Hum Genet. 2016;80(3):172–181. doi: 10.1111/ahg.12148 [DOI] [PubMed] [Google Scholar]
- 34.Weiler H, Isermann BH. Thrombomodulin. J Thromb Haemost. 2003;1(7):1515–1524. doi: 10.1046/j.1538-7836.2003.00306.x [DOI] [PubMed] [Google Scholar]
- 35.Esmon CT. The impact of the inflammatory response on coagulation. Thromb Res. 2004;114(5–6):321–327. doi: 10.1016/j.thromres.2004.06.028 [DOI] [PubMed] [Google Scholar]
- 36.Hoppe B, Dorner T. Coagulation and the fibrin network in rheumatic disease: a role beyond haemostasis. Nat Rev Rheumatol. 2012;8(12):738–746. doi: 10.1038/nrrheum.2012.184 [DOI] [PubMed] [Google Scholar]
- 37.Sillen M, Declerck PJ. Thrombin Activatable Fibrinolysis Inhibitor (TAFI): an Updated Narrative Review. Int J Mol Sci. 2021;22(7):3670. doi: 10.3390/ijms22073670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.So AK, Varisco PA, Kemkes-Matthes B, et al. Arthritis is linked to local and systemic activation of coagulation and fibrinolysis pathways. J Thromb Haemost. 2003;1(12):2510–2515. doi: 10.1111/j.1538-7836.2003.00462.x [DOI] [PubMed] [Google Scholar]
- 39.Peters MJ, Nurmohamed MT, van Eijk IC, Verkleij CJ, Marx PF. Thrombin-activatable fibrinolysis inhibitor and its relation with inflammation in rheumatoid arthritis. Ann Rheum Dis. 2009;68(7):1232–1233. doi: 10.1136/ard.2008.097485 [DOI] [PubMed] [Google Scholar]
- 40.Esmon CT. The interactions between inflammation and coagulation. Br J Haematol. 2005;131(4):417–430. doi: 10.1111/j.1365-2141.2005.05753.x [DOI] [PubMed] [Google Scholar]
- 41.Giannakopoulos B, Passam F, Rahgozar S, Krilis SA. Current concepts on the pathogenesis of the antiphospholipid syndrome. Blood. 2007;109(2):422–430. doi: 10.1182/blood-2006-04-001206 [DOI] [PubMed] [Google Scholar]
- 42.Jurado M, Páramo JA, Gutierrez-Pimentel M, Rocha E. Fibrinolytic potential and antiphospholipid antibodies in systemic lupus erythematosus and other connective tissue disorders. Thromb Haemost. 1992;68(5):516–520. doi: 10.1055/s-0038-1646310 [DOI] [PubMed] [Google Scholar]
- 43.Fort JG, Cowchock FS, Abruzzo JL, Smith JB. Anticardiolipin antibodies in patients with rheumatic diseases. Arthritis Rheum. 1987;30(7):752–760. doi: 10.1002/art.1780300705 [DOI] [PubMed] [Google Scholar]
- 44.Seriolo B, Accardo S, Garnero A, Fasciolo D, Cutolo M. Anticardiolipin antibodies, free protein S levels and thrombosis: a survey in a selected population of rheumatoid arthritis patients. Rheumatology. 1999;38(7):675–678. doi: 10.1093/rheumatology/38.7.675 [DOI] [PubMed] [Google Scholar]
- 45.Gladd DA, Olech E. Antiphospholipid antibodies in rheumatoid arthritis: identifying the dominoes. Curr Rheumatol Rep. 2009;11(1):43–51. doi: 10.1007/s11926-009-0007-3 [DOI] [PubMed] [Google Scholar]
- 46.Cheng YJ, Liu ZH, Yao FJ, et al. Current and former smoking and risk for venous thromboembolism: a systematic review and meta-analysis. PLoS Med. 2013;10(9):e1001515. doi: 10.1371/journal.pmed.1001515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Di Giuseppe D, Discacciati A, Orsini N, Wolk A. Cigarette smoking and risk of rheumatoid arthritis: a dose-response meta-analysis. Arthritis Res Ther. 2014;16(2):R61. doi: 10.1186/ar4498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smith BD, La Celle PL. Blood viscosity and thrombosis: clinical considerations. Prog Hemost Thromb. 1982;6:179–201. [PubMed] [Google Scholar]
- 49.Bombardier C, Barbieri M, Parthan A, et al. The relationship between joint damage and functional disability in rheumatoid arthritis: a systematic review. Ann Rheum Dis. 2012;71(6):836–844. doi: 10.1136/annrheumdis-2011-200343 [DOI] [PubMed] [Google Scholar]
- 50.Ravi B, Escott B, Shah PS, et al. A systematic review and meta-analysis comparing complications following total joint arthroplasty for rheumatoid arthritis versus for osteoarthritis. Arthritis Rheum. 2012;64(12):3839–3849. doi: 10.1002/art.37690 [DOI] [PubMed] [Google Scholar]
- 51.Singh JA, Cameron C, Noorbaloochi S, et al. Risk of serious infection in biological treatment of patients with rheumatoid arthritis: a systematic review and meta-analysis. Lancet. 2015;386(9990):258–265. doi: 10.1016/S0140-6736(14)61704-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gupta A, Pipe SG, Towheed T, Anastassiades T. Is rheumatoid arthritis a risk factor for fractures: a systematic review of observational studies. Curr Rheumatol Rev. 2020;16(1):29–37. doi: 10.2174/1573397115666190723160312 [DOI] [PubMed] [Google Scholar]
- 53.Restivo V, Candiloro S, Daidone M, et al. Systematic review and meta-analysis of cardiovascular risk in rheumatological disease: symptomatic and non-symptomatic events in rheumatoid arthritis and systemic lupus erythematosus. Autoimmun Rev. 2022;21(1):102925. [DOI] [PubMed] [Google Scholar]
- 54.Ungprasert P, Srivali N, Cheungpasitporn W, Davis Iii JM. Risk of incident chronic obstructive pulmonary disease in patients with rheumatoid arthritis: a systematic review and meta-analysis. Joint Bone Spine. 2016;83(3):290–294. doi: 10.1016/j.jbspin.2015.05.016 [DOI] [PubMed] [Google Scholar]
- 55.Lee JJ, Pope JE. A meta-analysis of the risk of venous thromboembolism in inflammatory rheumatic diseases. Arthritis Res Ther. 2014;16(5):435. doi: 10.1186/s13075-014-0435-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bacani AK, Gabriel SE, Crowson CS, Heit JA, Matteson EL. Noncardiac vascular disease in rheumatoid arthritis: increase in venous thromboembolic events? Arthritis Rheum. 2012;64(1):53–61. doi: 10.1002/art.33322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ramagopalan SV, Wotton CJ, Handel AE, Yeates D, Goldacre MJ. Risk of venous thromboembolism in people admitted to hospital with selected immune-mediated diseases: record-linkage study. BMC Med. 2011;9:1. doi: 10.1186/1741-7015-9-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Choi HK, Rho YH, Zhu Y, Cea-Soriano L, Avina-Zubieta JA, Zhang Y. The risk of pulmonary embolism and deep vein thrombosis in rheumatoid arthritis: a UK population-based outpatient cohort study. Ann Rheum Dis. 2013;72(7):1182–1187. doi: 10.1136/annrheumdis-2012-201669 [DOI] [PubMed] [Google Scholar]
- 59.Chung WS, Peng CL, Lin CL, et al. Rheumatoid arthritis increases the risk of deep vein thrombosis and pulmonary thromboembolism: a nationwide cohort study. Ann Rheum Dis. 2014;73(10):1774–1780. doi: 10.1136/annrheumdis-2013-203380 [DOI] [PubMed] [Google Scholar]
- 60.Li L, Lu N, Avina-Galindo AM, et al. The risk and trend of pulmonary embolism and deep vein thrombosis in rheumatoid arthritis: a general population-based study. Rheumatology. 2021;60(1):188–195. doi: 10.1093/rheumatology/keaa262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ozen G, Pedro S, Schumacher R, Simon T, Michaud K. Risk factors for venous thromboembolism and atherosclerotic cardiovascular disease: do they differ in patients with rheumatoid arthritis? RMD Open. 2021;7(2):e001618. doi: 10.1136/rmdopen-2021-001618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Molander V, Bower H, Frisell T, Askling J. Risk of venous thromboembolism in rheumatoid arthritis, and its association with disease activity: a nationwide cohort study from Sweden. Ann Rheum Dis. 2021;80(2):169–175. doi: 10.1136/annrheumdis-2020-218419 [DOI] [PubMed] [Google Scholar]
- 63.Conforti A, Berardicurti O, Pavlych V, Di Cola I, Cipriani P, Ruscitti P. Incidence of venous thromboembolism in rheumatoid arthritis, results from a ”real-life” cohort and an appraisal of available literature. Medicine. 2021;100(33):e26953. doi: 10.1097/MD.0000000000026953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Holmqvist ME, Neovius M, Eriksson J, et al. Risk of venous thromboembolism in patients with rheumatoid arthritis and association with disease duration and hospitalization. JAMA. 2012;308(13):1350–1356. doi: 10.1001/2012.jama.11741 [DOI] [PubMed] [Google Scholar]
- 65.Yusuf HR, Hooper WC, Beckman MG, Zhang QC, Tsai J, Ortel TL. Risk of venous thromboembolism among hospitalizations of adults with selected autoimmune diseases. J Thromb Thrombolysis. 2014;38(3):306–313. doi: 10.1007/s11239-014-1050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Galloway J, Barrett K, Irving P, et al. Risk of venous thromboembolism in immune-mediated inflammatory diseases: a UK matched cohort study. RMD Open. 2020;6(3):e001392. doi: 10.1136/rmdopen-2020-001392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim SC, Schneeweiss S, Liu J, Solomon DH. Risk of venous thromboembolism in patients with rheumatoid arthritis. Arthritis Care Res. 2013;65(10):1600–1607. doi: 10.1002/acr.22039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sadra V, Khabbazi A, Kolahi S, Hajialiloo M, Ghojazadeh M. Randomized double-blind study of the effect of dexamethasone and methylprednisolone pulse in the control of rheumatoid arthritis flare-up: a preliminary study. Int J Rheum Dis. 2014;17(4):389–393. doi: 10.1111/1756-185X.12278 [DOI] [PubMed] [Google Scholar]
- 69.Hua C, Buttgereit F, Combe B. Glucocorticoids in rheumatoid arthritis: current status and future studies. RMD Open. 2020;6(1):e000536. doi: 10.1136/rmdopen-2017-000536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Johannesdottir SA, Horváth-Puhó E, Dekkers OM, et al. Use of glucocorticoids and risk of venous thromboembolism: a nationwide population-based case-control study. JAMA Intern Med. 2013;173(9):743–752. doi: 10.1001/jamainternmed.2013.122 [DOI] [PubMed] [Google Scholar]
- 71.Coelho MC, Santos CV, Vieira Neto L, Gadelha MR. Adverse effects of glucocorticoids: coagulopathy. Eur J Endocrinol. 2015;173(4):M11–21. doi: 10.1530/EJE-15-0198 [DOI] [PubMed] [Google Scholar]
- 72.Chen CP, Kung PT, Chou WY, Tsai WC. Effect of introducing biologics to patients with rheumatoid arthritis on the risk of venous thromboembolism: a nationwide cohort study. Sci Rep. 2021;11(1):17009. doi: 10.1038/s41598-021-96508-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sepriano A, Kerschbaumer A, Smolen JS, et al. Safety of synthetic and biological DMARDs: a systematic literature review informing the 2019 update of the EULAR recommendations for the management of rheumatoid arthritis. Ann Rheum Dis. 2020;79(6):760–770. doi: 10.1136/annrheumdis-2019-216653 [DOI] [PubMed] [Google Scholar]
- 74.Davies R, Galloway JB, Watson KD, Lunt M, Symmons DP, Hyrich KL. Venous thrombotic events are not increased in patients with rheumatoid arthritis treated with anti-TNF therapy: results from the British Society for Rheumatology Biologics Register. Ann Rheum Dis. 2011;70(10):1831–1834. doi: 10.1136/ard.2011.153536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ketfi C, Boutigny A, Mohamedi N, et al. Risk of venous thromboembolism in rheumatoid arthritis. Joint Bone Spine. 2021;88(3):105122. doi: 10.1016/j.jbspin.2020.105122 [DOI] [PubMed] [Google Scholar]
- 76.Kotyla PJ, Engelmann M, Giemza-Stokłosa J, Wnuk B, Islam MA. Thromboembolic Adverse Drug Reactions in Janus Kinase (JAK) Inhibitors: does the Inhibitor Specificity Play a Role? Int J Mol Sci. 2021;22(5):2449. doi: 10.3390/ijms22052449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mease P, Charles-Schoeman C, Cohen S, et al. Incidence of venous and arterial thromboembolic events reported in the tofacitinib rheumatoid arthritis, psoriasis and psoriatic arthritis development programmes and from real-world data. Ann Rheum Dis. 2020;79(11):1400–1413. doi: 10.1136/annrheumdis-2019-216761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ytterberg SR, Bhatt DL, Mikuls TR, et al. Cardiovascular and Cancer Risk with Tofacitinib in Rheumatoid Arthritis. N Engl J Med. 2022;386(4):316–326. doi: 10.1056/NEJMoa2109927 [DOI] [PubMed] [Google Scholar]
- 79.Alves C, Penedones A, Mendes D, Marques FB. Risk of Cardiovascular and Venous Thromboembolic Events Associated With Janus Kinase Inhibitors in Rheumatoid Arthritis: a Systematic Review and Network Meta-analysis. J Clin Rheumatol. 2022;28(2):69–76. doi: 10.1097/RHU.0000000000001804 [DOI] [PubMed] [Google Scholar]
- 80.Bilal J, Riaz IB, Naqvi SAA, et al. Janus Kinase Inhibitors and Risk of Venous Thromboembolism: a Systematic Review and Meta-analysis. Mayo Clin Proc. 2021;96(7):1861–1873. doi: 10.1016/j.mayocp.2020.12.035 [DOI] [PubMed] [Google Scholar]
- 81.Giménez Poderós T, Gallardo Borge S, Vazquez-Ferreiro P. Risk of Venous Thromboembolism Associated With Tofacitinib and Baricitinib: a Systematic Review and Indirect Meta-Analysis. Pharmacotherapy. 2020;40(12):1248–1264. doi: 10.1002/phar.2472 [DOI] [PubMed] [Google Scholar]
- 82.Yates M, Mootoo A, Adas M, et al. Venous thromboembolism risk with jak inhibitors: a meta-analysis. Arthritis Rheumatol. 2021;73(5):779–788. doi: 10.1002/art.41580 [DOI] [PubMed] [Google Scholar]
- 83.Wang F, Sun L, Wang S, et al. Efficacy and safety of tofacitinib, baricitinib, and upadacitinib for rheumatoid arthritis: a systematic review and meta-analysis. Mayo Clin Proc. 2020;95(7):1404–1419. doi: 10.1016/j.mayocp.2020.01.039 [DOI] [PubMed] [Google Scholar]
- 84.Xie W, Xiao S, Huang Y, Sun X, Zhang Z. Effect of tofacitinib on cardiovascular events and all-cause mortality in patients with immune-mediated inflammatory diseases: a systematic review and meta-analysis of randomized controlled trials. Ther Adv Musculoskelet Dis. 2019;11:1759720x19895492. doi: 10.1177/1759720X19895492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xie W, Huang Y, Xiao S, Sun X, Fan Y, Zhang Z. Impact of Janus kinase inhibitors on risk of cardiovascular events in patients with rheumatoid arthritis: systematic review and meta-analysis of randomised controlled trials. Ann Rheum Dis. 2019;78(8):1048–1054. doi: 10.1136/annrheumdis-2018-214846 [DOI] [PubMed] [Google Scholar]
- 86.Mori S, Ogata F, Tsunoda R. Risk of venous thromboembolism associated with Janus kinase inhibitors for rheumatoid arthritis: case presentation and literature review. Clin Rheumatol. 2021;40(11):4457–4471. doi: 10.1007/s10067-021-05911-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Matta F, Singala R, Yaekoub AY, Najjar R, Stein PD. Risk of venous thromboembolism with rheumatoid arthritis. Thromb Haemost. 2009;101(1):134–138. doi: 10.1160/TH08-08-0551 [DOI] [PubMed] [Google Scholar]
- 88.Kang JH, Keller JJ, Lin YK, Lin HC. A population-based case-control study on the association between rheumatoid arthritis and deep vein thrombosis. J Vasc Surg. 2012;56(6):1642–1648. doi: 10.1016/j.jvs.2012.05.087 [DOI] [PubMed] [Google Scholar]
- 89.Yusuf HR, Hooper WC, Grosse SD, Parker CS, Boulet SL, Ortel TL. Risk of venous thromboembolism occurrence among adults with selected autoimmune diseases: a study among a U.S. cohort of commercial insurance enrollees. Thromb Res. 2015;135(1):50–57. doi: 10.1016/j.thromres.2014.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ogdie A, Kay McGill N, Shin DB, et al. Risk of venous thromboembolism in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a general population-based cohort study. Eur Heart J. 2018;39(39):3608–3614. doi: 10.1093/eurheartj/ehx145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mansour R, Azrielant S, Watad A, et al. Venous thromboembolism events among RA patients. Mediterr J Rheumatol. 2019;30(1):38–43. doi: 10.31138/mjr.30.1.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dore RK, Antonova JN, Burudpakdee C, et al. Prevalence, and Associated Costs of Anemia, Malignancy, Venous Thromboembolism, Major Adverse Cardiovascular Events, and Infections in Rheumatoid Arthritis Patients by Treatment History in the United States. ACR Open Rheumatol. 2022;4(6):473–482. doi: 10.1002/acr2.11376 [DOI] [PMC free article] [PubMed] [Google Scholar]