Highlights
-
•
Mucinous tumors of the ovary are epithelial tumors. They are classified into benign, borderline and malignant tumors.
-
•
Vaginal pelvic ultrasound is the imaging test of first choice.
-
•
Conservative treatment, detorsion of the adnexa without adnexectomy, is recommended in non-menopausal women.
-
•
The knowledge of clinical and histological characters will allow a better diagnostic andtherapeutic approach.
Keywords: cystadenoma of the ovary, 15 years, Mucinous
Abstract
Introduction
Mucinous tumors of the ovary are epithelial tumors. They are classified into benign, borderline and malignant tumors.
Case report
In this observation, we report a case of Mucinous tumors of the ovary diagnosed in a 15-year-old female patient.
Discussion
Serous cystadenoma of the ovary is a benign epithelial tumor representing 20 to 25 % of benign ovarian tumors. Average age of 50 years with extremes of 13 to 79 years, vaginal pelvic ultrasound is the imaging test of first choice, Conservative treatment, detorsion of the adnexa without adnexectomy, is recommended in non-menopausal women.
Conclusion
The knowledge of clinical and histological characters will allow a better diagnostic and therapeutic approach.
1. Introduction
Mucinous tumors of the ovary are epithelial tumors, characterized by a proliferation of mucosecretory cells reminiscent of endocervical or intestinal epithelium. They are classified as benign, borderline and malignant tumors.
Serous cystadenoma of the ovary is a benign epithelial tumor representing 20 to 25 % of benign tumors of the ovary. It develops in the coelomic epithelium (the epithelium covering the ovary) and represents 50 % of all epithelial tumors. It preferably appears before the age of 40, but indeed, they can be observed at any age [1]. All our work was reported according to the SCARE criteria and guidelines [8].
2. Case report
Patient aged 15 years, without any particular pathological history, nulli gesture nulliparous, admitted to the maternity ward at hospital El Harouchi for pelvic pain of acute onset, dating back to a day before her admission without other associated signs. The clinical examination revealed a hemodynamically and respiratorily stable patient with a hypogastric renal mass that was painful to palpation and reached the umbilicus, measuring approximately 11 cm, without any inflammatory signs. The rest of the somatic examination was unremarkable.
Exploratory laparotomy Fig. 1 revealed a 20 cm latero-uterine mass twisted into 2 turns of a coil, benign in appearance, with no abnormalities noted in the uterus, appendix and left ovary. Detorsion of the right adnexa with cystectomy was carried out, with accidental rupture of the cyst at the end of the operation, bringing back mucinous contents. A pelvic ultrasound with an abdominal-pelvic CT scan Fig. 2, Fig. 3 came back in favor of a 10 cm thin-walled multilocular cystic abdominal mass without pelvic effusion or adenopathy.
Fig. 1.
Intraoperative image of the ovarian cyst.
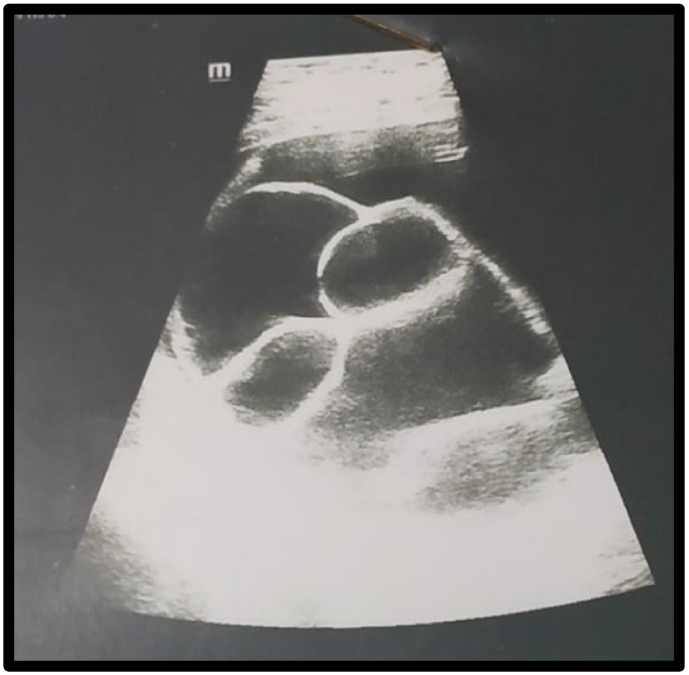
Fig. 2.
Pelvic ultrasound, showing a multilocular mass.
Fig. 3.
Pelvic CT scan.
Anatomopathological study revealed a mucinous cystadenoma of the right ovary with haemorrhagic infarction, compatible with a cyst torsion, with no sign of malignancy.
3. Discussion
Mucinous cystadenoma is a benign epithelial tumor of the ovary corresponding to class B1 of the FIGO histological classification [2]. It represents 15 % of all ovarian tumors, coming second after serous cysts. It is usually found in women during the genital activity period, rarely before puberty and after the menopause. In a study of 15 cases, Chaitin [3] found an average age of 50 years with extremes of 13 to 79 years.no particular risk factors were found, as in our patient's case.
Vaginal pelvic ultrasonography is the first-line imaging examination for a presumed benign urovarian tumor (PBOT) in adult women. In case of a pure liquid unilocular mass smaller than 7 cm, ultrasound is sufficient to characterize the mass. MRI is recommended as a second line of investigation for indeterminate masses or masses larger than 7 cm [4]. Ovarian serous cysts are classically unilocular, but sometimes multilocular, measuring on average 10 cm in diameter; in some cases they can reach 30 to 50 cm in size, with a volume varying from a few cubic centimetres to several dozen liters. It is bilateral in 12 to 20 % of cases.
MRI is recommended as a second-line procedure to explore indeterminate masses or masses larger than 7 cm.
The determination of tumor markers (CEA, CA 125 and CA 19-9) preoperatively does not distinguish malignant from benign tumors [5], [6], [7]. However, it will be useful to follow their evolution postoperatively in the context of surveillance of a malignant cyst. At the end of this workup, the presumptive diagnosis of benign mucinous cystadenoma can generally be made in adult women with no history of cancer.
In adult women with no history of cancer, abstention is possible in the case of asymptomatic pure unilocular cysts of less than 10 cm. In case of symptoms, laparoscopy is the reference approach for surgical treatment of BPT. Conservative surgical treatment (cystectomy) should be preferred to adnexectomy in non-menopausal women without a history of or risk factor for cancer. In case of suspected adnexal torsion, laparoscopic surgical exploration is recommended. Conservative treatment, detorsion of the adnexa without adnexectomy, is recommended in non-menopausal women, whatever the presumed duration of the torsion and the macroscopic appearance of the ovary. During pregnancy, expectation is recommended for asymptomatic unilocular fluid masses less than 6 cm [4].
4. Conclusion
Ovarian cystadenoma represents a distinct histological entity, which differs from other malignant epithelial tumors by its clinical and histological characteristics.
Knowledge of these differences will allow a better diagnostic and therapeutic approach.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
I declare on my honor that the ethical approval has been exempted by my establishment.
Sources of funding
None.
Author contribution
Zineb Sami: Corresponding author writing the paper
Watik Fedoua: writing the paper
Harrad Mouna: writing the paper
Said Hasna: writing the paper
Jalal Mohammed: correction of the paper
Lamrissi Amine: correction of the paper
Bouhya Said: correction of the paper
Guarantor
Dr. Watik Fedoua.
Registration of research studies
None.
Declaration of competing interest
The authors declare having no conflicts of interest for this article.
References
- 1.Borghèse B., Marzouk P., Santulli P., de Ziegler D., Chapron C. Traitementschirurgicaux des kystes de l’ovaire présumésbénins. J. Obstet. Gynecol Biol. Reprod. 2013 doi: 10.1016/j.jgyn.2013.09.033. Sous presse. [DOI] [PubMed] [Google Scholar]
- 2.Hein D.J., Kellerman R.D., Abbott G. Ovarian mucinous cystadenoma: evaluating the pelvic mass. Am. Fam. Physician. 1993;48(5):818–824. [PubMed] [Google Scholar]
- 3.- D.R. Jones A. Vasilakis L. Pillai G Timberlake ., A Giant, benign, mucinous cystadenoma of the ovary: case study andliterature review. [PubMed]
- 4.CNGOF . 2013. 37ES JOURNÉES NATIONALES Paris. [Google Scholar]
- 5.Buamah P.K., Skillen A.W. Serum CA 125 concentrations in patients with benign ovarian tumors. J. Surg. Oncol. 1994;56(2):71–74. doi: 10.1002/jso.2930560204. [DOI] [PubMed] [Google Scholar]
- 6.Takemori M., Nishimura R., Sugimura K., Obayashi C., Yasuda D. Ovarian strumal carcinoïd with markedly high serum levels of tumor. Gynecol. Oncol. 1995;58(2):266–269. doi: 10.1006/gyno.1995.1224. [DOI] [PubMed] [Google Scholar]
- 7.Ye C., Ito K., Komatsu Y., Takagi H. Extremely high levels of Ca 19–9 and Ca 125 antigen in benignmucinousovariancystadenoma. Gynecol. Oncol. 1994;52(2):267–271. doi: 10.1006/gyno.1994.1044. [DOI] [PubMed] [Google Scholar]
- 8.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating Consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]