Abstract
Microscopic colitis (MC) is a chronic inflammatory bowel disease that is characterized by nonbloody watery diarrhea. The epidemiology in Japan differs from that in Europe and the United States, but little information is available from epidemiological surveys of MC in Japan. This study aimed to provide a new hypothesis regarding the factors associated with MC by using the Japanese Adverse Drug Event Report (JADER) database. “Colitis microscopic” (preferred term code: 10056979) cases entered into the JADER database between 2004 and 2021 were analyzed. Of the 246,997 cases in the JADER database, 161 cases were observed to be associated with MC. A Weibull analysis revealed that the median onset duration of MC (interquartile range) was 72.5 (36.0‒125.5) days in lansoprazole users and 116.0 (60.3‒1089.0) days in aspirin users. A multiple logistic regression analysis revealed that MC was significantly associated with the female sex, as well as ages ≥ 60 years and drugs including lansoprazole, aspirin, and nicorandil. A subset analysis revealed that MC was positively associated with obesity in female cases. Our study cannot demonstrate a causal inference between MC and each drug; however, the findings suggest that MC was associated with nicorandil as well as with lansoprazole and aspirin.
Subject terms: Diseases, Gastroenterology, Medical research, Risk factors
Introduction
Microscopic colitis (MC) is a chronic inflammatory bowel disease that is characterized by nonbloody watery diarrhea, with few or no endoscopic abnormalities1. There are two main subtypes of this disorder, including lymphocytic colitis (LC) and collagenous colitis (CC). The incidences of LC and CC have been reported to be 1.1‒5.2 and 3.1‒5.5 cases per 100,000 population in Europe and North America, respectively2,3. Clinical symptoms of LC and CC include chronic and persistent diarrhea, abdominal pain, weight loss and flatulence3,4, which can reduce the quality of life of patients5.
The reported incidence of MC is lower in Japan than in Europe and the United States, and CC is more common than LC in Japan6. In Europe and the United States, MC is typically associated with autoimmune disorders such as thyroiditis, celiac disease, and rheumatoid arthritis7. In contrast, of the Japanese patients who develop CC, the most common underlying diseases are hypertension and reflux esophagitis, with autoimmune disorders being rare8. As the situation of MC varies between Japan and other countries, further research is needed to identify the situation with regard to MC in Japan.
The underlying mechanisms of MC remain unclear, but an association has been suggested with abnormal reactions to luminal antigen, autoimmunity, bile acid malabsorption, infection, certain drugs and abnormal collagen metabolism9. The risk of MC has been found to be higher in females aged > 50 years, with a reported ratio of 4.4–7.9 in CC and 1.8–5.0 in LC compared with males3,10–13. Additionally, smoking and specific drugs have been reported to be risk factors for MC14, with drugs including proton pump inhibitors (PPIs), selective serotonin reuptake inhibitors (SSRIs), nonsteroid anti-inflammatory drugs (NSAIDs), antidepressants (such as carbamazepine and duloxetine), and β-blockers15–17. It is recommended to choose a first-line therapy for MC that avoids such risk factors. If there is no improvement in symptoms, loperamide, mesalazine, salazosulfapyridine, or oral steroids can be considered as treatments18,19. As the proportion of drug-induced cases of CC is considered to be higher in Japan than in Europe and the United States6, it is important to avoid risk factors for MC treatments; however, data regarding causative drugs are controversial20.
The spontaneous reporting system (SRS) is a valuable tool for evaluating drug-related adverse events21. In Japan, the Pharmaceuticals and Medical Devices Agency (PMDA) manages a SRS known as the Japanese Adverse Drug Event Report (JADER) database. Although the JADER database has several biases (such as a notoriety bias and competition bias) that may affect study outcomes22,23, it contains data regarding severe and rare adverse events, including drug-induced MC. Few reports have comprehensively evaluated the patient backgrounds of MC, causative drugs, or onset durations. Therefore, the purpose of this study was to provide a new hypothesis regarding the factors associated with the onset of MC by using the JADER database.
Materials and methods
Data source and data selection
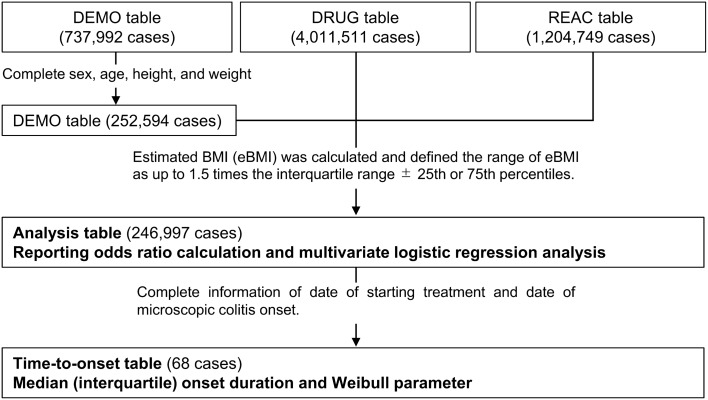
The SRS adverse event data recorded in the JADER database between April 2004 and August 2021 were downloaded from the PMDA website (http://www.pmda.go.jp/). The database consists of four tables: patient background information (DEMO), drug information (DRUG), adverse reactions (REAC), and medical history (HIST). All of the tables (except for the HIST table) were connected by an ID number. A flowchart of the data selection from the JADER database is shown in Fig. 1. Patients with missing or unclear data on sex, age, height, or weight were excluded from all of the reports. Height and weight data are entered into the JADER database in the form of 10-cm-denominated ranges (height) and 10-kg-denominated ranges (weight). We used the intermediate values in these classifications of height and weight as the continuous variables. For example, for a patient with height and weight in the 160‒169 cm and 50‒59 kg ranges, respectively, the intermediate values of height and weight would be 165 cm and 55 kg, respectively. To evaluate body type, we calculated estimated BMI (eBMI) by using the following formula24, which is shown here for the example patient above:
Figure 1.
Flowchart of dataset construction from the Japanese Adverse Drug Event Report database.
We excluded outliers of eBMI by using the boxplot method25 and we defined the range of eBMI as up to 1.5 times the interquartile range ± 25th or 75th percentiles. eBMI was classified as follows: underweight, eBMI < 18.5 kg/m2; normal, 18.5 ≤ eBMI < 25.0 kg/m2; and obese, eBMI ≥ 25.0 kg/m2. After applying the exclusion criteria, 246,997 patients were included in the table, which was renamed as the “Analysis table”. The following age classifications were then applied to the table: < 10, 10‒19, 20‒29, 30‒39, 40‒49, 50‒59, 60‒69, 70‒79, 80‒89, 90‒99 and 100‒109 years. The World Health Organization (WHO) defines “elderly” as those individuals who are greater than 65-years old. Accordingly, we stratified the analysis table into two groups: 0‒59-years-old and ≥ 60-years-old. The data were further limited to those cases with complete information regarding the date of the start of drug administration and the date of onset of adverse events, and this table was named the “Time-to-onset table” (68 cases). Time-to-onset was defined as the period from the start of drug administration to the onset of MC. In this study, time to onset was defined as the shortest duration to onset. The drugs that were included in the analysis of time-to-onset were lansoprazole and aspirin, which were reported in > 10 cases and identified the in multivariate logistic regression analysis.
Definitions of adverse events and drugs of interest
The definition of adverse events that was used in this study was that of the Medical Dictionary for Regulatory Activities/Japanese (MedDRA/J) version 24.0 (https://www.jmo.gr.jp/jmo/servlet/mdrLoginTop). We identified cases of MC based on the preferred term (PT) “Colitis microscopic” (PT code: 10056979) of the MedDRA/J. In the JADER database, a clinical outcome profile was entered into “Uncertain”, “Recovered”, “Improved”, “Unimproved”, “With sequelae”, and “Death”, and this outcome of MC was investigated. In patients with MC, drugs that were administered in at least five cases were considered drugs of interest, and these drugs are listed in Table 1. Among the drugs of interest, the most common therapeutic categories were defined as PPIs, NSAIDs, angiotensin converting enzyme inhibitors (ACE-Is)/angiotensin II receptor blockers (ARBs), statins, β-blockers, bisphosphonates, and calcium channel blockers.
Table 1.
Groupings of the analyzed drugs according to frequency of use.
| n | Drug |
|---|---|
| > 100 | Lansoprazole |
| 20‒100 | Aspirin, amlodipine, furosemide |
| 10‒19 | Loxoprofen, nicorandil, allopurinol, magnesium oxide, candesartan, rosuvastatin, carvedilol, etizolam, olmesartan, alendronic acid, rebamipide, bisoprolol, clopidogrel, ferrous citrate, mecobalamin, diclofenac, valsartan, atorvastatin, brotizolam, teprenone, prednisolone |
| 5‒9 | Ursodeoxycholic acid, alfacalcidol, rabeprazole, pravastatin, nifedipine, cilostazol, warfarin, zolpidem, enalapril, mosapride, esomeprazole, celecoxib, losartan, diltiazem, benidipine, febuxostat, spironolactone, flunitrazepam, loperamide, vonoprazan, risedronic acid, isosorbide nitrate, apixaban, triazolam, albumin tannate, tocopherol nicotinate, famotidine |
Statistical analysis
The median and interquartile range (IQR) days to onset and Weibull shape parameters26 were used to clarify the time-to-onset profile for MC. The Weibull distribution includes a scale parameter (α) and a shape parameter (β). The shape parameter indicates the failure rate distribution over time and is categorized as follows: early-failure type involves the upper limit of the 95% confidence interval (95% CI) of β less than 1, and incidence may decrease over time; random-failure type involves 95% CI of β and includes 1, with the incidence possibly being constant over time; and the wear-out-failure type involves the lower limit of 95% CI of β greater than 1, and the incidence may increase over time.
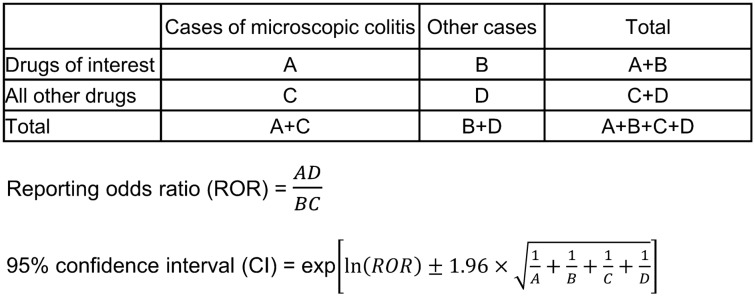
A two-by-two contingency table was compiled based on the presence or absence of MC and the drug of interest. The reporting odds ratio (ROR) and 95% CI were calculated to evaluate the safety of each drug based on a previous study27 (Fig. 2). A signal was considered to be positive when the lower limit of the 95% CI was greater than 1. We also performed a multiple logistic regression analysis to consider the confounding factors based on the methods that were used in previous studies28,29. Sex, age and eBMI are hypothesized to be confounding factors, and these factors were forced entry as the explanatory variables. To evaluate the effectiveness of all of the drugs of interest listed in Table 1 (except for albumin tannate, prednisolone, and loperamide), a forward and backward stepwise selection with a significance level of 0.05 was performed in all of the cases29,30. Albumin tannate, prednisolone, and loperamide were excluded from the stepwise selection because these drugs are used to treat MC. The objective variable was set to MC, and the explanatory variables were set to sex, age, eBMI and drugs which were selected using by the stepwise method. Additionally, a subset analysis was performed to evaluate the effect of sex. The explanatory variables for female and male patients were set to age, eBMI, lansoprazole, and aspirin, as these variables are reported to be associated with MC. The final multiple logistic regression model was as follows:
Figure 2.
Two-by-two contingency table for calculating the reporting odds ratio and 95% confidence interval of microscopic colitis.
S: sex (female vs. male), A: age (≥ 60 years vs. < 60 years), E: eBMI (obese or underweight vs. normal), L: lansoprazole, AS: aspirin, MO: magnesium oxide, N: nicorandil, D: diclofenac, R: rabeprazole, F: flunitrazepam, and V: vonoprazan.
Multicollinearity diagnosis was performed by variance inflation factors (VIF). All VIF values of the variables in the final multiple logistic regression model were less than 2 (Supplementary Table S1). In this study, all of the statistical analyses were performed by using JMP Pro, version 15.0.0 (SAS Institute Inc., Cary, NC, USA). A p value less than 0.05 was considered to be statistically significant.
Ethics approval statement
No ethical approval was required for this study.
Results
There were 737,992 cases in the DEMO table, 4,011,511 cases in the DRUG table, and 1,204,749 cases in the REAC table of the JADER dataset. After excluding the missing data, 246,997 cases were analyzed, and 161 cases of MC were identified (47 males and 114 females; 13 individuals in those aged 0–59 years and 148 individuals in those aged ≥ 60 years). The mean ± standard deviation (minimum to maximum) of eBMI was 21.5 ± 3.9 (14.6–31.2) kg/m2 in MC cases and 21.8 ± 3.9 (11.3–31.2) kg/m2 in non-MC cases. When regarding the clinical outcome profile, the numbers of uncertain, recovered, improved and unimproved cases were 8, 77, 74 and 2 cases, respectively. Moreover, there were no cases with sequelae or death. Table 1 groups the analyzed drugs according to frequency of use. The top four reported drugs for MC (in descending order) were lansoprazole (n = 128 cases), aspirin (n = 46 cases), amlodipine (n = 28 cases), and furosemide (n = 21 cases). The number of cases and crude RORs of MC are summarized in Supplementary Tables S2 and S3 online.
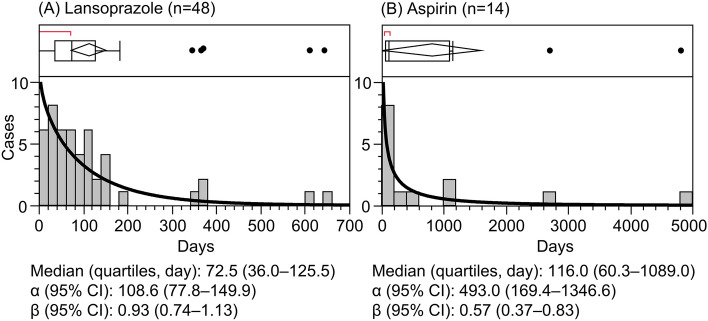
Figure 3 shows the median onset durations (IQRs) and Weibull parameters for lansoprazole and aspirin. Lansoprazole was used in 48 cases and aspirin in 14 cases. In the lansoprazole cases, the median onset duration (IQR) and the β parameter were 72.5 (36.0‒125.5) days and 0.93 (0.74‒1.13), respectively; in addition, the onset of MC was considered to be of the random-failure type. In the aspirin cases, the median onset duration (IQR) and the β parameter were 116.0 (60.3‒1089.0) days and 0.57 (0.37‒0.83), respectively, and the onset of MC was considered to be the early-failure type. Furthermore, the median onset duration of lansoprazole was shorter than that of aspirin.
Figure 3.
Histograms and Weibull shape parameters of microscopic colitis for (A) lansoprazole and (B) aspirin.
Tables 2 and 3 show the results of the multiple logistic regression analysis of MC by using the variables of individual drugs and patient background. The multiple logistic regression analysis revealed that MC was significantly associated with female sex [adjusted ROR (aROR): 3.26, 95% CI: 2.31‒4.60], age ≥ 60 years (aROR: 3.94, 95% CI: 2.22‒6.98), and lansoprazole (aROR: 35.55, 95% CI: 23.92‒52.84), aspirin (aROR: 1.66, 95% CI: 1.14‒2.41), magnesium oxide (aROR: 0.38, 95% CI: 0.22‒0.64), nicorandil (aROR: 2.11, 95% CI: 1.19‒3.74), diclofenac (aROR: 2.21, 95% CI: 1.18‒4.11), rabeprazole (aROR: 2.26, 95% CI: 1.09‒4.65), flunitrazepam (aROR: 2.32, 95% CI: 1.01‒5.31) and vonoprazan (aROR: 3.41, 95% CI: 1.38‒8.44). In females, MC was significantly associated with age ≥ 60 years (aROR: 4.45, 95% CI: 2.16‒9.19), obesity (aROR: 1.58, 95% CI: 1.03‒2.43), lansoprazole (aROR: 45.33, 95% CI: 27.22‒75.48), and aspirin (aROR: 1.59, 95% CI: 1.02‒2.46). In males, MC was significantly associated with lansoprazole (aROR: 15.32, 95% CI: 8.12‒28.91) and aspirin (aROR: 2.80, 95% CI: 1.52‒5.14).
Table 2.
Multiple logistic regression analysis of microscopic colitis using variables of drug and patient background in all cases.
| All cases | ||||
|---|---|---|---|---|
| Cases n = 161 | Non-cases n = 246,836 | aROR (95% CI) | p value | |
| Sex (female) | 114 | 114,463 | 3.26 (2.31‒4.60) | < 0.001*** |
| Age ≥ 60 years | 148 | 164,117 | 3.94 (2.22‒6.98) | < 0.001*** |
| eBMI | ||||
| Obese | 36 | 44,574 | 1.21 (0.82‒1.78) | 0.334 |
| Underweight | 28 | 40,153 | 1.17 (0.77‒1.79) | 0.467 |
| Normal | 97 | 162,109 | Ref | ‒ |
| Lansoprazole | 128 | 22,387 | 35.55 (23.92‒52.84) | < 0.001*** |
| Aspirin | 46 | 20,578 | 1.66 (1.14‒2.41) | 0.008** |
| Magnesium oxide | 15 | 25,972 | 0.38 (0.22‒0.64) | < 0.001*** |
| Nicorandil | 15 | 4219 | 2.11 (1.19‒3.74) | 0.011* |
| Diclofenac | 11 | 5544 | 2.21 (1.18‒4.11) | 0.013* |
| Rabeprazole | 8 | 10,399 | 2.26 (1.09‒4.65) | 0.028* |
| Flunitrazepam | 6 | 4224 | 2.32 (1.01‒5.31) | 0.046* |
| Vonoprazan | 5 | 3978 | 3.41 (1.38‒8.44) | 0.008** |
The adjusted reporting odds ratio (aROR) and 95% confidence intervals (95% CI) of microscopic colitis were calculated for sex, age, eBMI and each drug.
eBMI estimated body mass index.
***p < 0.001, **p < 0.01, *p < 0.05, p: statistical significance obtained in multiple logistic regression analysis.
Table 3.
Multiple logistic regression analysis of microscopic colitis using variables of drug and patient background for each sex.
| Cases | Non-cases | aROR (95% CI) | p value | |
|---|---|---|---|---|
| Females | n = 114 | n = 114,463 | ||
| Age ≥ 60 years | 106 | 71,545 | 4.45 (2.16‒9.19) | < 0.001*** |
| eBMI | ||||
| Obese | 32 | 23,121 | 1.58 (1.03‒2.43) | 0.038* |
| Underweight | 22 | 18,034 | 1.40 (0.86‒2.29) | 0.181 |
| Normal | 60 | 73,308 | Ref. | – |
| Lansoprazole | 96 | 9888 | 45.33 (27.22‒75.48) | < 0.001*** |
| Aspirin | 27 | 7,370 | 1.59 (1.02‒2.46) | 0.040* |
| Males | n = 47 | n = 132,373 | ||
| Age ≥ 60 years | 42 | 92,572 | 2.34 (0.92‒5.98) | 0.075 |
| eBMI | ||||
| Obese | 4 | 21,453 | 0.47 (0.17‒1.31) | 0.147 |
| Underweight | 6 | 22,119 | 0.74 (0.31‒1.75) | 0.489 |
| Normal | 37 | 88,801 | Ref. | ‒ |
| Lansoprazole | 32 | 12,499 | 15.32 (8.12‒28.91) | < 0.001*** |
| Aspirin | 19 | 13,208 | 2.80 (1.52‒5.14) | < 0.001*** |
The adjusted reporting odds ratio (aROR) and 95% confidence intervals (95% CI) of microscopic colitis were calculated for sex, age, eBMI, lansoprazole and aspirin.
eBMI estimated body mass index.
***p < 0.001, *p < 0.05, p: statistical significance obtained in multiple logistic regression analysis.
Discussion
In the present study, we analyzed the time to onset of MC and evaluated the association between MC and each drug and patient background. Our results suggest that the onset duration of MC was 1‒5 months in lansoprazole users and 2‒33 months in aspirin users. Furthermore, our results suggest that MC was associated with nicorandil, as well as with lansoprazole and aspirin. Although the severity of MC was mild in many cases, even mild MC may decrease the patient’s quality of life. It is important to discontinue the causative drugs for the improvement of symptoms.
A previous study reported that the mean duration of drug exposure before the start of diarrhea in MC patients was very long (15‒60 months) and that of lansoprazole was 4 months31. Another study found that the proportion of long-term users of NSAIDs (> 6 months) was higher in the MC group than in patients with irritable bowel syndrome (IBS) or colonic diverticular disease: in addition the mean ± standard deviation duration of onset of MC was 5.5 ± 4.4 years and ranged from 0.5‒15 years32. In addition, the duration of exposure to NSAIDs or PPIs for 4–12 months increased the risk of MC33. The median onset duration for lansoprazole and aspirin was shorter in the present study than in previous studies31–33; additionally, in the present study, the duration of lansoprazole tended to be shorter than that of aspirin. These results suggest that the long-term use of lansoprazole and aspirin may induce the onset of MC; therefore, it is important to identify the starting date of each drug.
A multiple logistic regression analysis in all of the cases revealed that MC was significantly associated with female sex and age ≥ 60 years. The subset analysis revealed that MC was significantly associated with age and obesity in females. The risk of MC has been observed to be higher in females aged > 50 years3,10–13, and our results are consistent with these previous studies. Previous studies have reported that obesity was associated with a lower risk of MC34,35; however, the present results suggest that obesity was positively associated with MC in females. Regarding underlying diseases, in Japan, CC is most commonly associated with hypertension and reflux esophagitis, whereas an association with autoimmune disorders has been reported in Europe and the United States7,8. In addition, the proportion of drug-induced MC was reported to be higher in Japan than in Europe and the United States6. Obesity is a risk factor for lifestyle diseases (such as hypertension), and the treatment of lifestyle diseases commonly requires patients to take many drugs, which may have correspondingly induced the onset of MC in Japanese patients. However, there is a lack of data regarding the association between MC and BMI in Japanese patients, and further research is necessary.
In addition to the association of MC with the female sex and older age, as mentioned above, associations with lansoprazole, aspirin, diclofenac and rabeprazole have also been reported. Lucendo et al. assessed the levels of probability at which different drugs can trigger MC20 based on the study of Beaugerie and Pardi15. In agreement with the present results, they observed the highest likelihood for aspirin, NSAIDs, and lansoprazole20. The PPIs evaluated by Lucendo et al. also included omeprazole and esomeprazole20. Previous studies have postulated several underlying mechanisms of PPI-induced MC, including their effects on tight junction functionality resulting in increased intestinal permeability17, alterations of intestinal microbiota36, and colonic dysbiosis37 related to acid suppression. These effects were also observed in users of other PPIs. In Japanese patients with MC, a higher proportion used lansoprazole than other PPIs6,38. However, a drug-class effect cannot be excluded and rabeprazole and vonoprazan (which is a potassium-competitive acid blocker) can also induce MC. Similarly, NSAIDs can cause MC, and this mechanism has been suggested to impair prostaglandin synthesis, thus resulting in increased intestinal permeability33. Increasing intestinal permeability induced by concomitant PPI and NSAID uses may be the underlying mechanism of MC.
The multiple logistic regression analysis revealed that nicorandil and flunitrazepam were also associated with MC. Nicorandil, which is a potassium channel opener and nitric oxide (NO) donor39, is commonly used for the treatment of angina pectoris. Although nicorandil can induce headaches with mild to moderate severity, it was generally well tolerated in clinical trials40. However, nicorandil may also cause gastrointestinal ulcers, fistulation41, and oral ulceration42. The release of inflammatory NO in the intestinal mucosa has been postulated as the mechanism of fistulation43. The abnormal metabolism of NO is considered to be one of the mechanisms of diarrhea in MC44; therefore, nicorandil may cause MC. In addition, β-blockers and calcium channel blockers are also used for the treatment of angina pectoris, and a disproportionate occurrence of MC was observed in our study in users of these drugs (Supplementary Tables S2). Thus, we cannot exclude the hypothesis that the condition of angina pectoris can cause MC. MC was also associated with flunitrazepam, although we were unable to determine a plausible biological mechanism. Moreover, magnesium oxide was observed to be negatively associated with MC. This scenario is due to magnesium oxide being commonly used as an osmotic purgative and is rarely used in MC patients presenting with diarrhea symptoms. The association between MC and magnesium oxide remains unclear, and further research is needed.
Our study had several limitations. First, the outcomes of the study using the JADER database may be affected by the lack of a denominator, over- or underreporting, and various biases, such as a competition bias and notoriety bias. The onset duration of MC may be shorter than the actual duration because reporters generally recognize recently started drugs in the adverse drug events report. Additionally, we could not investigate the association between MC and a dose-related effect of drugs because there is considerable missing information about drug dosages in the JADER database. A previous study reported that the risk of developing MC did not differ by a daily dose of NSAIDs, PPIs, SSRIs, and statins20. However, the dose-related effects of other drugs are possibly associated with the onset of MC, and further research is needed. Second, the clinical symptoms of MC are similar to those of IBS45, and patients with MC could have been misdiagnosed as having IBS. In addition, we could not classify CC and LC because adverse events were reported by using PT. These limitations could have affected the results of our study. Third, the stepwise method has been used to detect the previously unknown adverse drug events in previous studies46–49, but this method should be considered the limitation that the real explanatory variables that have causal effects on the objective variable may not be coincidentally statistical significance, while nuisance variables may be coincidentally significant50. Furthermore, a study using the JADER database cannot evaluate a true risk and provides a hypothesis as a starting point for exploratory analyses51. Our findings should be interpreted with caution due to the in silico approach that was used; thus, the results cannot provide causal inference between MC and each drug. A prospective clinical trial is needed to further evaluate these results. Nevertheless, this is the first study in Japan to evaluate the time-to-onset profile of MC and the pharmacoepidemiology of MC by using the JADER database.
Conclusions
In the present study, we analyzed the time-to-onset profile of MC and evaluated the association between MC and each drug and patient background by using the JADER database. Our results suggest that the onset duration of MC was 1‒5 months in lansoprazole users and 2‒33 months in aspirin users. A multiple logistic regression analysis revealed that MC was significantly associated with the female sex, age ≥ 60 years, and drugs including lansoprazole, aspirin, magnesium oxide, nicorandil, diclofenac, rabeprazole, flunitrazepam and vonoprazan. A subset analysis revealed that MC was positively associated with obesity in females. Our study used an in silico approach and cannot provide causal inference between MC and each drug; however, MC was associated with nicorandil as well as with lansoprazole and aspirin. These findings need to be evaluated in cohort studies and long-term clinical investigations.
Supplementary Information
Acknowledgements
The authors would like to thank FORTE Science Communications (www.forte-science.co.jp) and American Journal Experts (http://www.aje.com/) for English language review.
Author contributions
K.Y., M.J., Y.O. and K.H. contributed to the concept and designed the study. K.Y. analyzed the data and wrote the manuscript. K.H., S.Y., S.T., M.J., Y.O. and A.H. interpreted the data and helped to write the manuscript. F.O., T.N., S.T. and N.K. supervised the findings of the study and reviewed the manuscript. All authors have read and approved the final version of the manuscript.
Funding
This work was supported by JSPS KAKENHI (Grant Nos. JP19K16461 and JP22K10568).
Data availability
The datasets generated during and/or analyzed during the current study are available in the JADER database, https://www.pmda.go.jp/safety/info-services/drugs/adr-info/suspected-adr/0004.html.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-22257-2.
References
- 1.Münch A, et al. Microscopic colitis: Current status, present and future challenges: Statements of the European microscopic colitis group. J. Crohns Colitis. 2012;6:932–945. doi: 10.1016/j.crohns.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 2.Pardi DS, et al. The epidemiology of microscopic colitis: A population based study in Olmsted County, Minnesota. Gut. 2007;56:504–508. doi: 10.1136/gut.2006.105890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams JJ, Beck PL, Andrews CN, Hogan DB, Storr MA. Microscopic colitis-a common cause of diarrhoea in older adults. Age Ageing. 2010;39:162–168. doi: 10.1093/ageing/afp243. [DOI] [PubMed] [Google Scholar]
- 4.Bohr J, Tysk C, Eriksson S, Abrahamsson H, Järnerot G. Collagenous colitis: A retrospective study of clinical presentation and treatment in 163 patients. Gut. 1996;39:846–851. doi: 10.1136/gut.39.6.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hjortswang H, et al. Health-related quality of life is impaired in active collagenous colitis. Dig. Liver Dis. 2011;43:102–109. doi: 10.1016/j.dld.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Shimizu S. Present status and endoscopic diagnosis of drug-associated collagenous colitis. Gastroenterol. Endosc. 2018;60:2357–2368. doi: 10.11280/gee.60.2357. [DOI] [Google Scholar]
- 7.Brown WR, Tayal S. Microscopic colitis. A review. J. Dig. Dis. 2013;14:277–281. doi: 10.1111/1751-2980.12046. [DOI] [PubMed] [Google Scholar]
- 8.Yamazaki K, et al. Diagnosis and clinical features of drug-induced collagenous colitis. Stomach Intest. 2016;51:450–462. [Google Scholar]
- 9.Pardi DS. Microscopic Colitis: An update. Inflamm. Bowel Dis. 2004;10:860–870. doi: 10.1097/00054725-200411000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Williams JJ, et al. Microscopic colitis–defining incidence rates and risk factors: A population-based study. Clin. Gastroenterol. Hepatol. 2008;6:35–40. doi: 10.1016/j.cgh.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 11.Olesen M, Eriksson S, Bohr J, Järnerot G, Tysk C. Microscopic colitis: A common diarrhoeal disease. An epidemiological study in Örebro, Sweden, 1993–1998. Gut. 2004;53:346–350. doi: 10.1136/gut.2003.014431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bergman D, et al. A nationwide cohort study of the incidence of microscopic colitis in Sweden. Aliment. Pharmacol. Ther. 2019;49:1395–1400. doi: 10.1111/apt.15246. [DOI] [PubMed] [Google Scholar]
- 13.Weimers P, et al. Incidence and prevalence of microscopic colitis between 2001 and 2016: A Danish nationwide cohort study. J. Crohns Colitis. 2020;14:1717–1723. doi: 10.1093/ecco-jcc/jjaa108. [DOI] [PubMed] [Google Scholar]
- 14.Vigren L, et al. Is smoking a risk factor for collagenous colitis? Scand. J. Gastroenterol. 2011;46:1334–1339. doi: 10.3109/00365521.2011.610005. [DOI] [PubMed] [Google Scholar]
- 15.Beaugerie L, Pardi DS. Drug-induced microscopic colitis—Proposal for a scoring system and review of the literature. Aliment. Pharmacol. Ther. 2005;22:277–284. doi: 10.1111/j.1365-2036.2005.02561.x. [DOI] [PubMed] [Google Scholar]
- 16.Fernández-Bañares F, et al. Drug consumption and the risk of microscopic colitis. Am. J. Gastroenterol. 2007;102:324–330. doi: 10.1111/j.1572-0241.2006.00902.x. [DOI] [PubMed] [Google Scholar]
- 17.Keszthelyi D, et al. Proton pump inhibitor use is associated with an increased risk for microscopic colitis: A case-control study. Aliment. Pharmacol. Ther. 2010;32:1124–1128. doi: 10.1111/j.1365-2036.2010.04453.x. [DOI] [PubMed] [Google Scholar]
- 18.Tysk C, Bohr J, Nyhlin N, Wickbom A, Eriksson S. Diagnosis and management of microscopic colitis. World J. Gastroenterol. 2008;14:7280. doi: 10.3748/wjg.14.7280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miehlke S, et al. Microscopic colitis: Pathophysiology and clinical management. Lancet Gastroenterol. Hepatol. 2019;4:305–314. doi: 10.1016/S2468-1253(19)30048-2. [DOI] [PubMed] [Google Scholar]
- 20.Lucendo AJ. Drug exposure and the risk of microscopic colitis: A critical update. Drugs R&D. 2017;17:79–89. doi: 10.1007/s40268-016-0171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bate A, Evans SJW. Quantitative signal detection using spontaneous ADR reporting. Pharmacoepidemiol. Drug Saf. 2009;18:427–436. doi: 10.1002/pds.1742. [DOI] [PubMed] [Google Scholar]
- 22.de Boissieu P, et al. Notoriety bias in a database of spontaneous reports: The example of osteonecrosis of the jaw under bisphosphonate therapy in the French national pharmacovigilance database. Pharmacoepidemiol. Drug Saf. 2014;23:989–992. doi: 10.1002/pds.3622. [DOI] [PubMed] [Google Scholar]
- 23.Pariente A, et al. Effect of competition bias in safety signal generation. Drug Saf. 2012;35:855–864. doi: 10.1007/BF03261981. [DOI] [PubMed] [Google Scholar]
- 24.Yamashiro K, et al. Adverse event profiles of hypomagnesemia caused by proton pump inhibitors using the Japanese Adverse Drug Event Report (JADER) database. Pharmazie. 2022;77:243–247. doi: 10.1691/ph.2022.2416. [DOI] [PubMed] [Google Scholar]
- 25.Schwertman NC, Owens MA, Adnan R. A simple more general boxplot method for identifying outliers. Comput. Stat. Data Anal. 2004;47:165–174. doi: 10.1016/j.csda.2003.10.012. [DOI] [Google Scholar]
- 26.Abe J, et al. Analysis of Stevens–Johnson syndrome and toxic epidermal necrolysis using the Japanese Adverse Drug Event Report database. J. Pharm. Health Care Sci. 2016;2:1–10. doi: 10.1186/s40780-016-0048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Puijenbroek EP, et al. A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol. Drug Saf. 2002;11:3–10. doi: 10.1002/pds.668. [DOI] [PubMed] [Google Scholar]
- 28.Hosoya R, Uesawa Y, Ishii-Nozawa R, Kagaya H. Analysis of factors associated with hiccups based on the Japanese Adverse Drug Event Report database. PLoS ONE. 2017;12:e0172057. doi: 10.1371/journal.pone.0172057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shimada K, et al. Adverse reaction profiles of hemorrhagic adverse reactions caused by direct oral anticoagulants analyzed using the Food and Drug Administration Adverse Event Reporting System (FAERS) database and the Japanese Adverse Drug Event Report (JADER) database. Int. J. Med. Sci. 2019;16:1295–1303. doi: 10.7150/ijms.34629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takeyama M, et al. Influence of Japanese regulatory action on denosumab-related hypocalcemia using Japanese Adverse Drug Event Report database. Biol. Pharm. Bull. 2017;40:1447–1453. doi: 10.1248/bpb.b17-00266. [DOI] [PubMed] [Google Scholar]
- 31.Fernández-Bañares F, et al. Epidemiological risk factors in microscopic colitis: A prospective case-control study. Inflamm. Bowel Dis. 2013;19:411–417. doi: 10.1002/ibd.23009. [DOI] [PubMed] [Google Scholar]
- 32.Riddell RH, Tanaka M, Mazzoleni G. Non-steroidal anti-inflammatory drugs as a possible cause of collagenous colitis: A case-control study. Gut. 1992;33:683. doi: 10.1136/gut.33.5.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verhaegh BPM, et al. High risk of drug-induced microscopic colitis with concomitant use of NSAIDs and proton pump inhibitors. Aliment. Pharmacol. Ther. 2016;43:1004–1013. doi: 10.1111/apt.13583. [DOI] [PubMed] [Google Scholar]
- 34.Sandler RS, et al. Obesity is associated with decreased risk of microscopic colitis in women. World J. Gastroenterol. 2022;28:230–241. doi: 10.3748/wjg.v28.i2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu P-H, et al. Obesity and weight gain since early adulthood are associated with a lower risk of microscopic colitis. Clin. Gastroenterol. Hepatol. 2019;17:2523–2532. doi: 10.1016/j.cgh.2018.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vesper B, et al. The effect of proton pump inhibitors on the human microbiota. Curr. Drug Metab. 2009;10:84–89. doi: 10.2174/138920009787048392. [DOI] [PubMed] [Google Scholar]
- 37.Imhann F, et al. Proton pump inhibitors affect the gut microbiome. Gut. 2016;65:740. doi: 10.1136/gutjnl-2015-310376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Umeno J, et al. Linear mucosal defect may be characteristic of lansoprazole-associated collagenous colitis. Gastrointest. Endosc. 2008;67:1185–1191. doi: 10.1016/j.gie.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 39.Afzal MZ, et al. Nicorandil, a nitric oxide donor and ATP-sensitive potassium channel opener, protects against dystrophin-deficient cardiomyopathy. J. Cardiovasc. Pharmacol. Ther. 2016;21:549–562. doi: 10.1177/1074248416636477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simpson D, Wellington K. Nicorandil. Drugs. 2004;64:1941–1955. doi: 10.2165/00003495-200464170-00012. [DOI] [PubMed] [Google Scholar]
- 41.Noyes JD, Mordi IR, Zeb Q, Lang CC. Nicorandil-induced colovesical fistula in a patient with diverticular disease. Clin. Case Rep. 2021;9:1737–1741. doi: 10.1002/ccr3.3888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scully C, et al. Nicorandil can induce severe oral ulceration. Oral surg. oral med. oral pathol. oral radiol. Endod. 2001;91:189–193. doi: 10.1067/moe.2001.110306. [DOI] [PubMed] [Google Scholar]
- 43.McDaid J, et al. Diverticular fistulation is associated with nicorandil usage. Ann. R. Coll. Surg. Engl. 2010;92:463–465. doi: 10.1308/003588410x12699663904673a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Perner A, et al. Expression of nitric oxide synthases and effects of L-arginine and L-NMMA on nitric oxide production and fluid transport in collagenous colitis. Gut. 2001;49:387–394. doi: 10.1136/gut.49.3.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Madisch A, Miehlke S, Bartosch F, Bethke B, Stolte M. Microscopic colitis: Clinical presentation, treatment and outcome of 494 patients. Z. Gastroenterol. 2014;52:1062–1065. doi: 10.1055/s-0034-1366281. [DOI] [PubMed] [Google Scholar]
- 46.Field TS, et al. Risk factors for adverse drug events among older adults in the ambulatory setting. J. Am. Geriatr. Soc. 2004;52:1349–1354. doi: 10.1111/j.1532-5415.2004.52367.x. [DOI] [PubMed] [Google Scholar]
- 47.Inaba I, et al. Risk evaluation for acute kidney injury induced by the concomitant use of valacyclovir, analgesics and renin-angiotensin system inhibitors: The detection of signals of drug-drug interactions. Front. Pharmacol. 2019;10:874. doi: 10.3389/fphar.2019.00874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakao S, et al. Evaluation of anti-infective-related Clostridium difficile-associated colitis using the Japanese Adverse Drug Event Report database. Int. J. Med. Sci. 2020;17:921–930. doi: 10.7150/ijms.43789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tanaka M, et al. Analysis of drug-induced hearing loss by using a spontaneous reporting system database. PLoS ONE. 2019;14:e0217951. doi: 10.1371/journal.pone.0217951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smith G. Step away from stepwise. J. Big Data. 2018;5:32. doi: 10.1186/s40537-018-0143-6. [DOI] [Google Scholar]
- 51.Satake R, et al. Analysis of drug-induced gastrointestinal obstruction and perforation using the Japanese Adverse Drug Event Report database. Front. Pharmacol. 2021;12:692292. doi: 10.3389/fphar.2021.692292. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available in the JADER database, https://www.pmda.go.jp/safety/info-services/drugs/adr-info/suspected-adr/0004.html.