Abstract
Introduction
Diabetic macular edema (DME) is one of the major sight-threatening complications of diabetic retinopathy, which is associated with retinal inflammation. However, it is still unknown whether DME is associated with systemic inflammation. The study aimed to investigate the association between systemic inflammatory and optical coherence tomography (OCT) biomarkers in patients with treatment-naïve center-involving diabetic macular edema (DME) and to further explore the role of systemic inflammation in DME.
Methods
Medical records including clinical characteristics and ophthalmic examinations were collected from patients with treatment-naïve center-involving DME. Systemic inflammation markers including systemic immune-inflammatory index (SII), neutrophil–lymphocyte ratio (NLR), and platelet–lymphocyte ratio (PLR) were calculated. OCT biomarkers, including intraretinal cyst (IRC) size, disorganization of retinal inner layers (DRIL), external limiting membrane (ELM)/ellipsoid zone (EZ) integrity, retinal hyperreflective foci (HRF), subretinal fluid (SRF) and vitreomacular (VM) status were evaluated manually. Correlation analysis and multivariable linear regression models were used to investigate the relationship between systemic inflammatory markers and OCT biomarkers.
Results
A total of 82 patients with treatment-naïve center-involving DME were included. The number of HRF on OCT was correlated with SII, NLR, and PLR and positively associated with SII (p < 0.001) in both univariate and multivariate linear regression analyses. The differences remained largely the same during subgroup analysis controlling DM duration, SRF, and ELM/EZ integrity. No significant association was observed between other OCT biomarkers and blood inflammatory markers.
Conclusion
Retinal HRF in diabetic macular edema is associated with blood inflammatory markers, which supports the theory of HRF’s inflammatory nature and emphasizes the important role of inflammation in DME. SII may be a potential marker for DME treatment decisions.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40123-022-00576-x.
Keywords: Biomarker, Diabetic macular edema, Inflammation, Optical coherence tomography
Key Summary Points
| This cross-sectional study aimed to comprehensively investigate the association between optical coherence tomography (OCT) biomarkers and systemic inflammation in patients with diabetic macular edema (DME), which is short of research and well worth attention. |
| This study found that hyperreflective foci (HRF) are positively associated with systemic immune-inflammatory index (SII) in multivariable regression models, while other OCT biomarkers are not significantly related to systemic inflammation in the current study. |
| Systemic inflammatory markers might be helpful for DME classification and treatment decision. |
Introduction
Diabetes macular edema (DME) is the most common sight-threatening complication of diabetic retinopathy (DR) [1], estimated to affect nearly 5–10% of patients with diabetes mellitus (DM) [2, 3]. The pathophysiology of DME involves alteration of the blood-retinal barrier [4], which is the result of retinal inflammation with vascular endothelial growth factor (VEGF) as a prominent pro-inflammatory agent [5, 6]. Thus, intravitreal injection of anti-VEGF agents is currently considered to be the optimal treatment for center-involving DME (CI-DME) [2, 7–10]. This treatment is relatively expensive. However, around 40% of patients with DME showed dissatisfactory response to anti-VEGF therapy, due to currently unknown reasons, and other treatment including intravitreal corticosteroids would be considered [11, 12]. Investigating possible markers related to treatment efficacy, either imaging or laboratory, is meaningful for further understanding, prognosis prediction, and personalized treatment of DME.
Spectral-domain optical coherence tomography (SD-OCT) is an easily obtained non-invasive imaging modality that provides in-depth cross-sectional information about the retina, which is widely adopted for DME diagnosis and evaluation [7, 13]. An increasing number of studies have attempted to use SD-OCT-based imaging biomarkers for evaluation and treatment-prediction of DME, including intraretinal cyst (IRC) [14], disorganization of retinal inner layers (DRIL) [15, 16], external limiting membrane (ELM)/ellipsoid zone (EZ) integrity [17], retinal hyperreflective foci (HRF) [18, 19], subretinal fluid (SRF) [20], and vitreomacular (VM) status [21]. The aforementioned imaging biomarkers were shown to be correlated with visual acuity at baseline or after anti-VEGF treatment to different extents. These OCT biomarkers are of vastly different pathophysiological origin and may represent different aspects of DME, either retinal inflammation or structural damage [22]. Understanding the biological nature of imaging markers is potentially helpful for shifting treatment and personalized medicine toward DME.
Laboratory findings of DME mainly focused on intraocular inflammatory cytokines. Several cytokines are associated with DME presence, OCT biomarkers, severity, and edema resolution [23–27]. However, extraction of aqueous humor is invasive and cannot be routinely conducted in clinical work. Nowadays, some easily obtained novel blood inflammatory markers, including systemic immune-inflammatory index (SII), neutrophil–lymphocyte ratio (NLR), and platelet–lymphocyte ratio (PLR), have been correlated with multiple inflammation-related diseases such as stroke [28], cardiovascular diseases [29], and cancer [30]. Recently, Elbeyli et al. reported that an elevated SII value is strongly associated with the presence of DME [31]. Özata Gündoğdu et al. found that NLR and SII levels were significantly higher in DME with SRF [32]. These studies shed light on the association between systemic inflammation markers and DME. However, in the previous studies, only SRF was studied. Few studies paid attention to other OCT biomarkers.
Given the current opinion of the great importance of inflammation in DME pathogenesis, we believe that studying the association of systemic inflammation and DME OCT biomarkers will be beneficial for DME management in three aspects. First, it advances the understanding of the biological meaning and pathogenesis mechanism behind these imaging biomarkers. Second, it is useful to establish the association between systemic inflammation and DME, which is currently less studied. Third, compared to aqueous humor cytokines, these easily performed blood-derived markers are potential surrogate predictive factors of anti-VEGF treatment.
Methods
This is an observational study conducted at the Eye Center of Second Affiliated Hospital of Zhejiang University from December 2021 to April 2022. The study was performed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of The Second Affiliated Hospital of Zhejiang University School of Medicine.
Study Participants and Data Collection
Inclusion criteria include (1) patients who were 18 years or older; (2) diagnosed with diabetes mellitus, either type 1 or 2 [33]; (3) diagnosed with center-involving DME defined by retinal thickening involving the 1-mm-diameter central subfield zone of macula on SD-OCT images [7]; (4) no previous treatment including intravitreal anti-VEGF injection, intravitreal or peribulbar corticosteroids, focal/grid macular photocoagulation, panretinal photocoagulation, or vitreoretinal surgery; (5) no cataract surgery in the past 6 months.
Exclusion criteria include (1) diagnosed with other vitreoretinal diseases other than DME; (2) OCT images with poor quality that are unable to read; (3) suffered from infectious illness or fever in the past 2 weeks; (4) once diagnosed with other diseases which might affect the blood test results, such as kidney or liver diseases, autoimmune disorders, hematological diseases, and malignant tumor; (5) use of immunosuppressive drugs in the past 6 months.
Clinical characteristics including gender, age, DM duration, blood test results, treatment history and comorbidities which might affect our results were collected from the electronic medical record system. Ophthalmological examinations include slit-lamp examination, visual acuity, OCT, OCTA, and fluorescence fundus angiography if necessary. Best-corrected visual acuity (BCVA) was transformed into logarithm of the minimum angle of resolution (logMAR) scale. DR severity was assessed using ultrawide-field fundus photographs, and graded into mild NPDR, moderate NPDR, severe NPDR, and PDR [34]. For patients in whom both eyes were affected by DME, only the worse eye was taken into consideration.
Evaluation of OCT Biomarkers
SD-OCT (Spectralis, Heidelberg, Germany) was performed. All OCT images were labeled by two blinded ophthalmologists. OCT biomarkers analyzed in this paper include intraretinal cyst (IRCs), disorganization of retinal inner layers (DRIL), external limiting membrane (ELM)/ellipsoid zone (EZ) integrity, retinal hyperreflective foci (HRF), subretinal fluid (SRF), and vitreomacular (VM) status. Examples of the annotation are provided in Fig. 1.
Fig. 1.
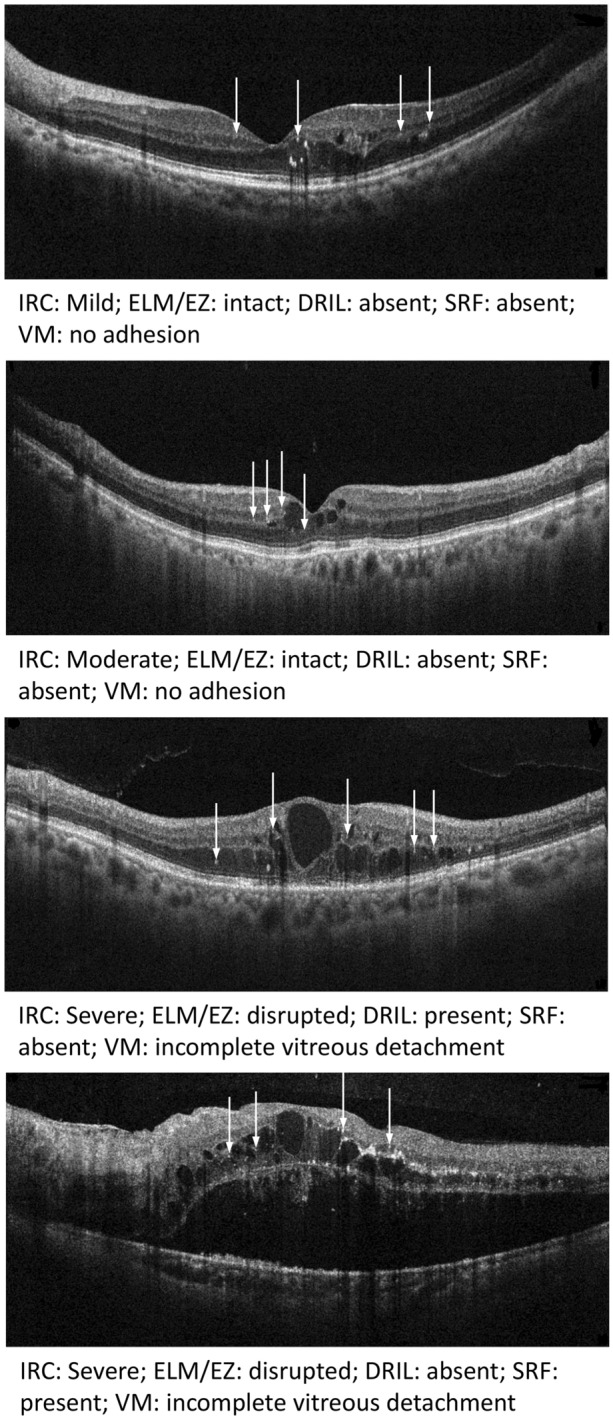
Examples of OCT imaging biomarkers labeling. White arrows represent HRF. DRIL disorganization of retinal inner layers, ELM external limiting membrane, EZ ellipsoid zone, HRF hyperreflective foci, IRC intraretinal cyst
IRCs were oval-shaped, hyporeflective regions within the neurosensory layer. As shown in Fig. 1, IRC size was graded qualitatively as no cyst, mild, moderate, or severe, according to previous research [35, 36].
DRIL was defined as the inability to distinguish between ganglion cell–inner plexiform layer complex, the inner nuclear layer, and the outer plexiform layer in the central fovea. It was graded as absence or presence of DRIL [15].
ELM/EZ integrity was graded on the basis of the visibility and continuity of the first and second hyperreflective layers of the four outermost layers. The integrity was categorized as intact for discernible and continuous, disrupted for partially visible, and absent for totally lost [17, 36].
HRFs were defined as round-shaped, hyperreflective dots in the retina. In order to distinguish between HRF, hard exudates, or microaneurysms, three criteria were adopted: (1) reflectivity similar to the retinal nerve fiber layer; (2) diameter less than 30 μm; (3) no back-shadowing. The number of HRFs was counted manually [18, 19, 35, 36].
SRF was defined as the subfoveal hyporeflective area due to neurosensory detachment [20]. It was categorized as absent or present.
VM status was graded on the basis of the International Vitreomacular Traction Study Group classification [37]. To make the classification of VM status, we more simply classified it as no adhesion, incomplete vitreous detachment (IVD), complete vitreous detachment (CVD), vitreomacular traction (VT), and epiretinal membrane (ERM) according to previous related research [35, 36].
The annotation process was conducted by Jingxin Zhou and Siyuan Song. They both labeled all images according to pre-designed annotation principles as mentioned above. For each disagreement considering any OCT characteristics, they would discuss and make the final decision. The intraclass correlation (ICC) of HRF annotations between these two authors was 0.8583 (p < 0.001), which means the annotation of HRF was highly concordant.
Calculation of Blood Inflammatory Markers
Blood count and biochemical measurements were conducted after an 8-h overnight fast, followed by a forearm venous puncture for blood sample extraction. Full blood count was measured on a Sysmex XE-2100 analyzer (Sysmex Corp. Kobe, Japan) using standard procedures.
Systemic immune-inflammatory index (SII) was calculated as platelet count × neutrophil count/lymphocyte count [38]. Neutrophil–lymphocyte ratio (NLR) was computed as neutrophil count/lymphocyte count [39]. Platelet–lymphocyte ratio (PLR) was calculated as platelet count/lymphocyte count [40].
Statistical Analysis
Continuous variables are described using mean ± standard deviation (SD), and categorical variables are presented as numbers and percentages. All continuous variables were tested for normal distribution using the Kolmogorov–Smirnov test. Patient characteristics were compared among different levels of imaging biomarkers using Student’s t test, Mann–Whitney–Wilcoxon test, one-way analysis of variance, or Kruskal–Wallis test according to grouping and normality. Bonferroni method was adopted for multiple comparison in all related situations. For further analysis, logarithmic transformation was adopted for non-normally distributed variables. Spearman correlation and its significance were used to investigate the correlation between patient characteristics, blood inflammatory markers, and imaging biomarkers. Univariable and multivariable linear regression models were adopted to further investigate their relationship. Variables with p value of 0.1 or smaller in univariable analysis would be included in multivariable analysis. The multivariable regression was conducted in a forward stepwise manner. Linear regression models were adopted for BCVA and HRF number as dependent variables, and logistic regression models were used when SRF was treated as the dependent variable. Subgroup analyses were performed on the basis of SRF presence and ELM/EZ integrity, considering their potential influence on HRF.
The statistical analyses were conducted using IBM SPSS Statistics (version 25.0, IBM, New York, USA). Visualization of the correlation matrix was realized with “corrplot” package (version 0.92) using R (version 4.1.1, R Foundation for Statistical Computing, Vienna, Austria). All statistical tests were two-tailed with a p value of 0.05 or smaller as significant.
Results
Patient Characteristics
A total of 121 patients with complete clinical documents and ophthalmic examinations were originally reviewed, among whom 17 had previous treatment including surgery, laser or intravitreal anti-VEGF injection, 10 had vitreous hemorrhage, 5 had renal dysfunction due to various reasons, 4 had non-center-involving DME, and 3 had OCT images with insufficient quality to assess. Finally, 82 treatment-naïve center-involving DME eyes from 82 patients were included in our work.
The study population is summarized in Table 1. The mean age of study population was 61.71 ± 10.64 years, with 51 (62.2%) male and 31 (37.8%) female patients. The mean duration of DM was 11.29 ± 4.42 years. The mean BCVA (logMAR, Snellen) was 0.29 ± 0.23 (20/40). The means and standard deviations of SII, NLR, and PLR were 552.97 ± 261.71, 2.75 ± 1.12, and 128.29 ± 45.92, respectively. OCT biomarkers are also summarized in Table 1.
Table 1.
Demographic and clinical characteristics of the study population
| Age (mean ± SD, years) | 61.71 ± 10.64 |
| Gender (n, %) | |
| Male | 51 (62.2) |
| Female | 31 (37.8) |
| Duration of DM (mean ± SD, years) | 11.29 ± 4.42 |
| DR severity level (n, %) | |
| Mild NPDR | 12 (14.6) |
| Moderate NPDR | 22 (26.8) |
| Severe NPDR | 24 (29.3) |
| PDR | 24 (29.3) |
| BCVA (mean ± SD, Snellen) | 0.29 ± 0.23 (20/40) |
| OCT features | |
| Cyst Size (n, %) | |
| Mild | 17 (20.7) |
| Moderate | 37 (45.1) |
| Severe | 28 (34.1) |
| ELM/EZ integrity (n, %) | |
| Intact | 33 (40.2) |
| Disrupted | 42 (51.2) |
| Absent | 7 (8.5) |
| DRIL (n, %) | |
| Absent | 70 (85.4) |
| Present | 12 (14.6) |
| Hyperreflective foci (mean ± SD) | 34.52 ± 21.41 |
| Subretinal fluid (n, %) | |
| Absent | 51 (62.2) |
| Present | 31 (37.8) |
| Vitreomacular condition (n, %) | |
| No adhesion | 32 (39) |
| Incomplete vitreous detachment | 23 (28) |
| Complete vitreous detachment | 5 (6.1) |
| Vitreomacular traction | 5 (6.1) |
| Epiretinal membrane | 17 (20.7) |
| Systemic inflammation markers (mean ± SD) | |
| SII | 552.97 ± 261.71 |
| NLR | 2.75 ± 1.12 |
| PLR | 128.29 ± 45.92 |
BCVA best-corrected visual acuity, DM diabetes mellitus, DRIL disorganization of retinal inner layers, ELM external limiting membrane, EZ ellipsoid zone, logMAR logarithm of the minimum angle of resolution, NLR neutrophil–lymphocyte ratio, NPDR non-proliferative diabetic retinopathy, OCT optical coherence tomography, PLR platelet–lymphocyte ratio, PDR proliferative diabetic retinopathy, SD standard deviation, SII systemic immune-inflammatory index
Comparison of Clinical Characteristics Between Patients with Different OCT Biomarkers
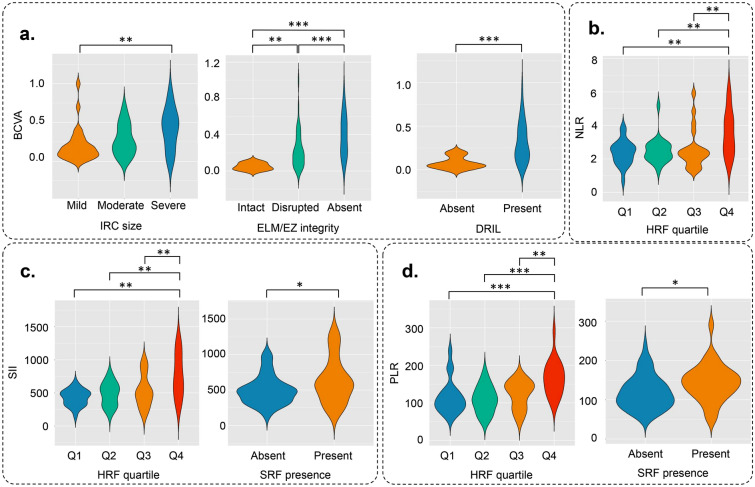
Clinical characteristics analyzed here include age, DM duration, DR severity, BCVA, and systemic inflammation markers. Statistically significant comparison results of clinical characteristics between patients with different OCT biomarkers are summarized in Fig. 2. Detailed results are presented in Supplementary material Tables S1–S6.
Fig. 2.
Comparison of clinical characteristics between patients with different OCT biomarkers. a With severer IRCs, ELM/EZ integrity disruption, and DRIL presence, patients tend to have lower BCVA. b Patients with more HRF were found to have higher NLR. c Patients with more HRF and SRF presence were found to have higher SII. d Patients with more HRF and SRF presence were found to have higher PLR. (*P < 0.05, **P < 0.01, ***P < 0.001.) BCVA best-corrected visual acuity, DRIL disorganization of retinal inner layers, ELM external limiting membrane, EZ ellipsoid zone, HRF hyperreflective foci, IRC intraretinal cyst, NLR neutrophil–lymphocyte ratio, PLR platelet–lymphocyte ratio, SII systemic immune-inflammatory index, SRF subretinal fluid
With severer IRCs, ELM/EZ integrity disruption, and DRIL presence, patients tend to have lower BCVA (IRC 0.20 ± 0.22 vs 0.28 ± 0.20 vs 0.42 ± 0.27, p = 0.008); ELM/EZ 0.05 ± 0.04 vs 0.33 ± 0.21 vs 0.20 ± 0.23, p < 0.001; DRIL 0.08 ± 0.07 vs 0.32 ± 0.23, p < 0.001).
HRF numbers were categorized into four different groups based on the quartiles. Patients with more HRF were found to have higher systemic inflammation markers (SII 430.57 ± 120.82 vs 482.78 ± 175.16 vs 533.18 ± 247.38 vs 769.85 ± 330.94, p = 0.001; NLR 2.38 ± 0.75 vs 2.50 ± 0.78 vs 2.56 ± 1.17 vs 3.57 ± 1.33, p = 0.003; PLR 115.95 ± 45.69 vs 109.64 ± 35.77 vs 122.94 ± 36.05 vs 165.84 ± 46.10, p < 0.001). Patients with SRF were found to have higher SII and PLR (SII 501.73 ± 205.54 vs 637.27 ± 320.49, p = 0.022; PLR 118.86 ± 42.37 vs 143.80 ± 47.96, p = 0.021).
No significant difference was found between IRC, ELM/EZ integrity, DRIL, and systemic inflammation markers, and there was no significant difference between HRF, SRF, and BCVA.
Correlation Among Clinical Characteristics and OCT Biomarkers
Spearman correlation was adopted to investigate the correlation between clinical characteristics and OCT biomarkers in patients with DME. Variables included in the correlation analysis were BCVA, OCT biomarkers, and systemic inflammation markers. The correlation matrix is shown in Fig. 3, with only significant correlations presented.
Fig. 3.
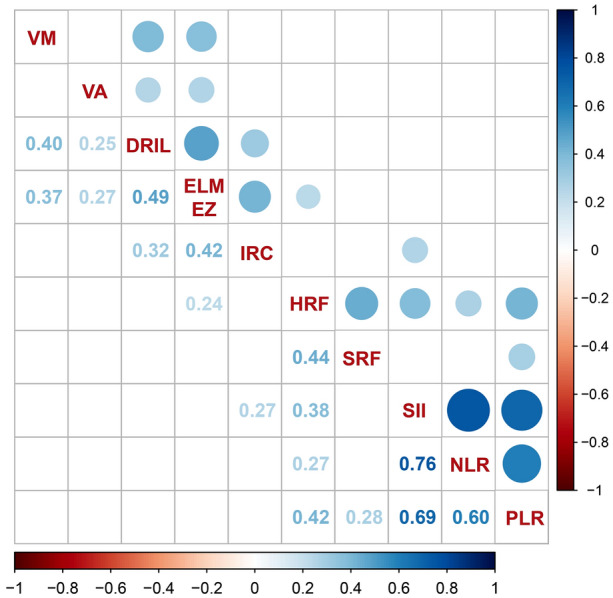
Correlation among clinical characteristics and OCT biomarkers. Color, size, and transparency of the dots in the upper half reflect the correlation tendency, degree, and significance. Only significant correlations are shown. VA visual acuity, DRIL disorganization of retinal inner layers, ELM external limiting membrane, EZ ellipsoid zone, HRF hyperreflective foci, IRC intraretinal cyst, NLR neutrophil–lymphocyte ratio, PLR platelet–lymphocyte ratio, SII systemic immune-inflammatory index, SRF subretinal fluid, VM vitreomacular status
DRIL presence and ELM/EZ integrity were significantly correlated with BCVAs (DRIL r = 0.25, p < 0.01; ELM/EZ r = 0.27, p < 0.01). HRF number was significantly correlated with SII, NLR, PLR, ELM/EZ integrity, and SRF presence (SII r = 0.38, p < 0.01; NLR r = 0.27, p = 0.01; PLR r = 0.42, p < 0.01; ELM/EZ r = 0.24, p = 0.03; SRF r = 0.44, p < 0.01).
Association of Blood Inflammatory Markers and HRF Number
To control the possible confounding effects of studied factors, regression models were adopted. Table 2 shows the association of systemic inflammatory markers and HRF number with linear regression models. In univariable regression, DM duration (p = 0.012), DR severity (p < 0.001), ELM/EZ integrity (p = 0.014), SRF (p < 0.001), SII (p < 0.001), NLR (p < 0.001), and PLR (p < 0.001) were significantly associated with HRF number. Variables with p value of 0.1 or smaller in univariable analysis were included in multivariable analysis, including DM duration, DM severity, BCVA, ELM/EZ status, SRF, SII, NLR, and PLR. In multivariable regression, only DM severity (p = 0.001), ELM/EZ integrity (p = 0.015), SRF (p = 0.007), and SII (p < 0.001) were significantly associated with HRF number.
Table 2.
Association of blood inflammatory markers and HRF number
| Hyperreflective foci | ||||
|---|---|---|---|---|
| Univariable | Multivariable | |||
| β coefficient | p value | β coefficient | p value | |
| Age | 0.057 | 0.611 | – | – |
| DM duration | 0.277 | 0.012* | 0.070 | 0.441 |
| DR severity | 0.530 | < 0.001** | 0.379 | 0.001** |
| BCVA | 0.189 | 0.089 | 0.062 | 0.558 |
| IRC | 0.065 | 0.564 | – | – |
| ELM/EZ | 0.271 | 0.014* | 0.202 | 0.015* |
| DRIL | − 0.022 | 0.848 | – | – |
| HRF | – | – | – | – |
| SRF | 0.413 | < 0.001*** | 0.235 | 0.007** |
| VM | 0.101 | 0.367 | – | – |
| SII | 0.471 | < 0.001*** | 0.334 | < 0.001*** |
| NLR | 0.424 | < 0.001*** | 0.151 | 0.267 |
| PLR | 0.428 | < 0.001*** | 0.019 | 0.861 |
BCVA best-corrected visual acuity, DM diabetes mellitus, DRIL disorganization of retinal inner layers, ELM external limiting membrane, EZ ellipsoid zone, HRF hyperreflective foci, IRC intraretinal cyst, NLR neutrophil–lymphocyte ratio, PLR platelet–lymphocyte ratio, SII systemic immune-inflammatory index, SRF subretinal fluid, VM vitreomacular status
*P < 0.05, **P < 0.01, ***P < 0.001
Subgroup Analysis
Subgroup analyses were conducted considering potential effects of DM duration, ELM/EZ integrity, and SRF on the association between HRF and systemic inflammation markers. Detailed results of subgroup analysis are listed in Supplementary material Tables S7–S9. Multivariable regression revealed that SII remained significantly associated with increased HRF number in patients with (p = 0.001) or without (p = 0.007) SRF, shorter DM duration (p = 0.002), and intact ELM/EZ (p = 0.007).
Discussion
In this study, HRF on OCT images was closely related to systemic inflammation in patients with DME, but ELM/EZ integrity and DRIL were related to visual function. In the multivariable analysis, HRF was also associated with other imaging biomarkers, including ELM/EZ integrity and SRF. These results suggest that (1) some OCT biomarkers, especially HRF, are a reflection of retinal inflammation status which can be affected by systemic inflammation; (2) DME is influenced by systemic inflammation, more than just regional inflammation within the retina; (3) these blood-derived inflammation parameters may be potential markers for shifting treatment and personalized medicine in DME and need further investigation.
Previously, attempts have been made to investigate the association between OCT biomarkers of patients with DME and blood test results, considering the role of inflammation in DME pathogenesis. Dimitriou et al. analyzed full blood count, biochemical parameters, and SD-OCT imaging biomarkers in patients with DME and found that presence of hyperreflective foci on SD-OCT was associated with significantly higher white blood cell count [41]. Their discovery also supported the inflammatory nature of HRF. Unfortunately, novel systemic inflammatory markers were not studied in that work. Elbeyli et al. [31] demonstrated that elevated SII is strongly associated with the occurrence of DME using data from patients with non-proliferative diabetic retinopathy, which agrees with our conclusion that DME is associated with systemic inflammation. Özata Gündoğdu et al. [32] found that SII levels were significantly higher in DME with SRF, which is consistent with our results, as is shown in Fig. 1, and no other OCT biomarkers were studied in their work. However, in Elbeyli et al.’s study [31], there was no significant difference in systemic inflammatory markers between patients with DME with or without SRF. According to previous research, it is suggested that SRF presence is associated with elevated pro-inflammatory cytokines in aqueous humor [42] and intravitreal corticosteroid injection is an effective treatment for subretinal fluid resolution [43]. Therefore, we tend to believe that there may be a relationship between SRF and systemic inflammation. We think the current disagreement between comparison results and correlation results was due to different statistical methods. However, more research needs to be done to clarify the association.
As promising systemic inflammation markers, SII, NLR, and PLR have been studied in a variety of chronic diseases. SII is thought to be a predictive and prognostic marker for multiple cancers [30, 38, 44, 45], autoimmune diseases [46, 47], cardiovascular disorders [28, 48, 49], and metabolic diseases [50]. There is no consensus on the normal value of SII, and in related research, most researchers utilized receiver operating characteristic curve (ROC) analysis to find various cutoff points for specific diseases, most of which are around 600 × 109/L. NLR is now widely used in all medical disciplines and is considered to be able to reflect body’s reaction to various external or internal stimuli, and the normal value of NLR was considered to be 1.0–2.0 [51]. Similarly, PLR also showed potential value in multiple diseases [52, 53] and the normal value of PLR was 70–200 [51]. These indices are calculated from common blood cell count, and the mechanisms behind them are thought to be results of cell functions, including those of neutrophils, lymphocytes, and platelets. White blood cells and their subtypes have long been seen as inflammatory markers in either infectious or non-infectious diseases. It is reported that in patients with DM and DR, systemic neutrophil count is elevated, indicating that neutrophil-mediated inflammation may play an important role in the pathogenesis of DM and DR [54]. Currently, platelets are increasingly thought to be related to inflammation. Platelet adhesion, aggregation, and secretion all participated in inflammatory reactions [55, 56]. In our study, these indices were associated with DME imaging features, which further supports the inflammatory origin of DME and reveals the relationship between different DME imaging features. The inflammatory reaction behind DME pathogenesis may be mediated by multiple blood cells including neutrophils, lymphocytes, and platelets.
As a major OCT feature discussed in the current paper, retinal HRF can be seen in multiple retinal diseases, and serves as a promising but controversial OCT biomarker in DME treatment [57]. Theories have been expounded upon the pathophysiology of HRF, including lipoprotein extravasation [18], inflammation-induced microglial cell activation [19], migrating retinal pigment epithelium (RPE) cells [58], and degenerated photoreceptor cells [59], etc. It is accepted that HRF is related to retinal inflammation in DME [57], and HRF is a potential biomarker for DME treatment management. Compared to anti-VEGF, corticosteroid treatment caused more HRF reduction in DME eyes [60]. Choroidal HRF is associated with better outcome of corticosteroid treatment [61], and it has been hypothesized that patients with DME and inflammatory OCT markers may gain more from corticosteroids [62].
The exact imaging definition of HRF is still controversial. In some publications, retinal nerve fibre layer reflectivity was used as the reference of HRF [19, 35, 36], as is in ours, while some used the RPE band reflectivity [63, 64]. In the current study, through multivariable regression and subgroup analysis, we advanced the understanding of HRF by illustrating the association between HRF and systemic inflammation reflected by SII, NLR, and PLR. Our study supported the inflammatory origin of HRF, and further expanded this correlation from retinal inflammation to systemic inflammation. Through such research, we believe at least two questions have been put forward: first, what is the exact relationship between systemic inflammation and DME, and how does it affect the disease; second, will these easily obtained blood-driven biomarkers be used for clinical instruction? Further research is needed to clarify these questions.
In our study, VM status is not related to systemic inflammation indices. However, it is thought that vitreoretinal interface abnormalities (VRIA) in general are substantially associated with inflammatory reactions and simultaneously with poorer response to anti-VEGF in patients with DME [65, 66]. We think the reasons can be discussed in three aspects. First, from a pathogenesis perspective, although high pro-inflammatory mediators around the vitreoretinal interface play an important role in VRIA formation [6], there are still chances that specific circumstances around the local retina are more important than systemic inflammation status. Second, from a visual outcome perspective, VRIA is related to poorer anti-VEGF response, but we think it is different from the way HRF works. In patients suffering from VRIA, such as VMT or ERM, their retinal structures have been destroyed to various extents. Local tissue injury is an unignorable factor affecting final visual outcome. However, patients with DME and high HRF may represent those patients’ whose macular edema is more related to inflammation, which may react better to corticoids [60]. Third, the lack of significant association between VRIA and inflammatory markers may be because of the relatively small sample size of our work.
The interplays between OCT biomarkers were interesting. In the current study, HRF is associated with broken ELM/EZ and SRF. ELM/EZ visibility reflects the photoreceptor integrity [35]. We tend to believe that the influence is mutual between ELM/EZ integrity and HRF. On the one hand, it is hypothesized that broken ELM/EZ may allow the HRF to migrate between retina and choroid and this kind of migration might affect the number of HRF [63]. On the other hand, lipoprotein extravasation may cause photoreceptor damage [67]. As is discussed before, SRF is closely related to inflammation [42, 43], and we believe the significant association of SRF and HRF is due to their common inflammatory nature.
The strength of the current paper lies in the systematical evaluation of novel systemic inflammatory makers and multiple OCT-based biomarkers, which has not been reported before according to our knowledge. There are also some limitations in the current study. First, this is a single-center study from an Asian population, which means the conclusions may not extend to other races and need to be validated. Second, although inclusion and exclusion criteria were discussed and made a priori, considering the complexity of potential factors associated with blood test, there might still be some unknown factors affecting the final results. Third, the sample size is relatively small and the findings still need to be validated in studies with a larger population. Fourth, the manual evaluation of HRF is subjective. Fifth, in the final study population, seven patients suffered from bilateral DME, and we chose the worse eye to represent the subject in the analysis, which might have introduced selection bias.
Conclusions
Retinal HRF in DME is associated with systemic inflammatory markers, which supports the theory of HRF’s inflammatory nature and emphasizes the important role of systemic inflammation in DME. More research needs to be done to evaluate these markers’ potential meaning in DME management. SII may be a potential marker for DME treatment decisions.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Funding
This study was supported by National key research and development program of China (2019YFC0118400), Key research and development program of Zhejiang Province (2019C03020), Clinical Medical Research Center for Eye Diseases of Zhejiang Province (2021E50007) and Natural Science Foundation of Zhejiang Province (grant number LQ21H120002). The journal’s Rapid Service fee was supported by the authors and their affiliations.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization: Jingxin Zhou, Kai Jin and Juan Ye. Methodology: All authors. Formal analysis and investigation: Jingxin Zhou, Siyuan Song and Yi Zhang. Writing—original draft preparation: Jingxin Zhou. Writing—review and editing: Yi Zhang, Kai Jin and Juan Ye. Funding acquisition: Kai Jin and Juan Ye. Resources: Yi Zhang and Juan Ye. Supervision: Yi Zhang, Kai Jin and Juan Ye.
Disclosures
Jingxin Zhou, Siyuan Song, Yi Zhang, Kai Jin and Juan Ye declare that they have no conflicts of interest and no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Compliance with Ethics Guidelines
The study was performed in accordance with the Declaration of Helsinki of 1964 and its later amendments and was approved by the Ethics Committee of The Second Affiliated Hospital of Zhejiang University School of Medicine.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Contributor Information
Kai Jin, Email: jinkai@zju.edu.cn.
Juan Ye, Email: yejuan@zju.edu.cn.
References
- 1.Zhang X, Saaddine JB, Chou CF, et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA. 2010;304(6):649–656. doi: 10.1001/jama.2010.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan GS, Cheung N, Simó R, Cheung GC, Wong TY. Diabetic macular oedema. Lancet Diabetes Endocrinol. 2017;5(2):143–155. doi: 10.1016/S2213-8587(16)30052-3. [DOI] [PubMed] [Google Scholar]
- 3.Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–564. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Das A, McGuire PG, Rangasamy S. Diabetic macular edema: pathophysiology and novel therapeutic targets. Ophthalmology. 2015;122(7):1375–1394. doi: 10.1016/j.ophtha.2015.03.024. [DOI] [PubMed] [Google Scholar]
- 5.Romero-Aroca P, Baget-Bernaldiz M, Pareja-Rios A, Lopez-Galvez M, Navarro-Gil R, Verges R. Diabetic macular edema pathophysiology: vasogenic versus inflammatory. J Diabetes Res. 2016;2016:2156273. doi: 10.1155/2016/2156273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forrester JV, Kuffova L, Delibegovic M. The role of inflammation in diabetic retinopathy. Front Immunol. 2020;11:583687. doi: 10.3389/fimmu.2020.583687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong TY, Sun J, Kawasaki R, et al. Guidelines on diabetic eye care: the International Council of Ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125(10):1608–1622. doi: 10.1016/j.ophtha.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Brown DM, Schmidt-Erfurth U, Do DV, et al. Intravitreal aflibercept for diabetic macular edema: 100-week results from the VISTA and VIVID studies. Ophthalmology. 2015;122(10):2044–2052. doi: 10.1016/j.ophtha.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 9.Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123(6):1351–1359. doi: 10.1016/j.ophtha.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nguyen QD, Brown DM, Marcus DM, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789–801. doi: 10.1016/j.ophtha.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The Restore Study. Ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–25. [DOI] [PubMed]
- 12.Gonzalez VH, Campbell J, Holekamp NM, et al. Early and long-term responses to anti-vascular endothelial growth factor therapy in diabetic macular edema: analysis of protocol I data. Am J Ophthalmol. 2016;172:72–79. doi: 10.1016/j.ajo.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Phadikar P, Saxena S, Ruia S, Lai TY, Meyer CH, Eliott D. The potential of spectral domain optical coherence tomography imaging based retinal biomarkers. Int J Retina Vitreous. 2017;3:1. doi: 10.1186/s40942-016-0054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsuboi K, You QS, Guo Y, et al. Association between fluid volume in inner nuclear layer and visual acuity in diabetic macular edema. Am J Ophthalmol. 2022;237:164–172. doi: 10.1016/j.ajo.2021.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun JK, Lin MM, Lammer J, et al. Disorganization of the retinal inner layers as a predictor of visual acuity in eyes with center-involved diabetic macular edema. JAMA Ophthalmol. 2014;132(11):1309–1316. doi: 10.1001/jamaophthalmol.2014.2350. [DOI] [PubMed] [Google Scholar]
- 16.Babiuch AS, Han M, Conti FF, Wai K, Silva FQ, Singh RP. Association of disorganization of retinal inner layers with visual acuity response to anti-vascular endothelial growth factor therapy for macular edema secondary to retinal vein occlusion. JAMA Ophthalmol. 2019;137(1):38–46. doi: 10.1001/jamaophthalmol.2018.4484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saxena S, Meyer CH, Akduman L. External limiting membrane and ellipsoid zone structural integrity in diabetic macular edema. Eur J Ophthalmol. 2022;32(1):15–16. doi: 10.1177/11206721211026106. [DOI] [PubMed] [Google Scholar]
- 18.Bolz M, Schmidt-Erfurth U, Deak G, Mylonas G, Kriechbaum K, Scholda C. Optical coherence tomographic hyperreflective foci: a morphologic sign of lipid extravasation in diabetic macular edema. Ophthalmology. 2009;116(5):914–920. doi: 10.1016/j.ophtha.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 19.Vujosevic S, Bini S, Torresin T, et al. Hyperreflective retinal spots in normal and diabetic eyes: B-scan and en face spectral domain optical coherence tomography evaluation. Retina. 2017;37(6):1092–1103. doi: 10.1097/IAE.0000000000001304. [DOI] [PubMed] [Google Scholar]
- 20.Gerendas BS, Prager S, Deak G, et al. Predictive imaging biomarkers relevant for functional and anatomical outcomes during ranibizumab therapy of diabetic macular oedema. Br J Ophthalmol. 2018;102(2):195–203. doi: 10.1136/bjophthalmol-2017-310483. [DOI] [PubMed] [Google Scholar]
- 21.Yoon D, Rusu I, Barbazetto I. Reduced effect of anti-vascular endothelial growth factor agents on diabetics with vitreomacular interface abnormalities. Int Ophthalmol. 2014;34(4):817–823. doi: 10.1007/s10792-013-9884-6. [DOI] [PubMed] [Google Scholar]
- 22.Chung YR, Kim YH, Ha SJ, et al. Role of inflammation in classification of diabetic macular edema by optical coherence tomography. J Diabetes Res. 2019;2019:8164250. doi: 10.1155/2019/8164250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Funatsu H, Noma H, Mimura T, Eguchi S, Hori S. Association of vitreous inflammatory factors with diabetic macular edema. Ophthalmology. 2009;116(1):73–79. doi: 10.1016/j.ophtha.2008.09.037. [DOI] [PubMed] [Google Scholar]
- 24.Jonas JB, Jonas RA, Neumaier M, Findeisen P. Cytokine concentration in aqueous humor of eyes with diabetic macular edema. Retina. 2012;32(10):2150–2157. doi: 10.1097/IAE.0b013e3182576d07. [DOI] [PubMed] [Google Scholar]
- 25.Hillier RJ, Ojaimi E, Wong DT, et al. Aqueous humor cytokine levels as biomarkers of disease severity in diabetic macular edema. Retina. 2017;37(4):761–769. doi: 10.1097/IAE.0000000000001210. [DOI] [PubMed] [Google Scholar]
- 26.Cacciamani A, Esposito G, Scarinci F, et al. Inflammatory mediators in the vitreal reflux of patients with diabetic macular edema. Graefes Arch Clin Exp Ophthalmol. 2019;257(1):187–97. [DOI] [PubMed]
- 27.Udaondo P, Hernández C, Briansó-Llort L, García-Delpech S, Simó-Servat O, Simó R. Usefulness of liquid biopsy biomarkers from aqueous humor in predicting Anti-VEGF response in diabetic macular edema: results of a pilot study. J Clin Med. 2019;8(11):1841. [DOI] [PMC free article] [PubMed]
- 28.Chu YW, Chen PY, Lin SK. Correlation between immune-inflammatory markers and clinical features in patients with acute ischemic stroke. Acta Neurol Taiwan. 2020;29(4):103–113. [PubMed] [Google Scholar]
- 29.Bhat T, Teli S, Rijal J, et al. Neutrophil to lymphocyte ratio and cardiovascular diseases: a review. Expert Rev Cardiovasc Ther. 2013;11(1):55–59. doi: 10.1586/erc.12.159. [DOI] [PubMed] [Google Scholar]
- 30.Hirahara T, Arigami T, Yanagita S, et al. Combined neutrophil-lymphocyte ratio and platelet-lymphocyte ratio predicts chemotherapy response and prognosis in patients with advanced gastric cancer. BMC Cancer. 2019;19(1):672. doi: 10.1186/s12885-019-5903-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elbeyli A, Kurtul BE, Ozcan SC, Ozarslan Ozcan D. The diagnostic value of systemic immune-inflammation index in diabetic macular oedema. Clin Exp Optom. 2021:1–5. 10.1080/08164622.2021.1994337. [DOI] [PubMed]
- 32.Özata Gündoğdu K, Doğan E, Çelik E, Alagöz G. Serum inflammatory marker levels in serous macular detachment secondary to diabetic macular edema. Eur J Ophthalmol. 2022:11206721221083465. [DOI] [PubMed]
- 33.Classification and Diagnosis of Diabetes Standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17–S38. doi: 10.2337/dc22-S002. [DOI] [PubMed] [Google Scholar]
- 34.Wilkinson CP, Ferris FL, 3rd, Klein RE, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110(9):1677–1682. doi: 10.1016/S0161-6420(03)00475-5. [DOI] [PubMed] [Google Scholar]
- 35.Szeto SK, Hui VWK, Tang FY, et al. OCT-based biomarkers for predicting treatment response in eyes with centre-involved diabetic macular oedema treated with anti-VEGF injections: a real-life retina clinic-based study. Br J Ophthalmol. 2021. 10.1136/bjophthalmol-2021-319587. [DOI] [PubMed]
- 36.Panozzo G, Cicinelli MV, Augustin AJ, et al. An optical coherence tomography-based grading of diabetic maculopathy proposed by an international expert panel: the European School for Advanced Studies in Ophthalmology classification. Eur J Ophthalmol. 2020;30(1):8–18. doi: 10.1177/1120672119880394. [DOI] [PubMed] [Google Scholar]
- 37.Duker JS, Kaiser PK, Binder S, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120(12):2611–2619. doi: 10.1016/j.ophtha.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 38.Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–6222. doi: 10.1158/1078-0432.CCR-14-0442. [DOI] [PubMed] [Google Scholar]
- 39.Buonacera A, Stancanelli B, Colaci M, Malatino L. Neutrophil to lymphocyte ratio: an emerging marker of the relationships between the immune system and diseases. Int J Mol Sci. 2022;23(7):3636. [DOI] [PMC free article] [PubMed]
- 40.Kumarasamy C, Tiwary V, Sunil K, et al. Prognostic utility of platelet-lymphocyte ratio, neutrophil-lymphocyte ratio and monocyte-lymphocyte ratio in head and neck cancers: a detailed PRISMA compliant systematic review and meta-analysis. Cancers. 2021;13(16):4166. [DOI] [PMC free article] [PubMed]
- 41.Dimitriou E, Sergentanis TN, Lambadiari V, Theodossiadis G, Theodossiadis P, Chatziralli I. Correlation between imaging morphological findings and laboratory biomarkers in patients with diabetic macular edema. J Diabetes Res. 2021;2021:6426003. doi: 10.1155/2021/6426003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yenihayat F, Özkan B, Kasap M, et al. Vitreous IL-8 and VEGF levels in diabetic macular edema with or without subretinal fluid. Int Ophthalmol. 2019;39(4):821–828. doi: 10.1007/s10792-018-0874-6. [DOI] [PubMed] [Google Scholar]
- 43.Ozdemir H, Karacorlu M, Karacorlu SA. Regression of serous macular detachment after intravitreal triamcinolone acetonide in patients with diabetic macular edema. Am J Ophthalmol. 2005;140(2):251–255. doi: 10.1016/j.ajo.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 44.Xie Q-K, Chen P, Hu W-M, et al. The systemic immune-inflammation index is an independent predictor of survival for metastatic colorectal cancer and its association with the lymphocytic response to the tumor. J Transl Med. 2018;16(1):273. doi: 10.1186/s12967-018-1638-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li QX, Shi DJ, Zhang LX, et al. Association of body mass and systemic immune-inflammation indices with endocrine therapy resistance in luminal breast cancers. J Int Med Res. 2019;47(5):1936–1947. doi: 10.1177/0300060519831570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dincer Rota D, Tanacan E. The utility of systemic-immune inflammation index for predicting the disease activation in patients with psoriasis. Int J Clin Pract. 2021;75(6):e14101. doi: 10.1111/ijcp.14101. [DOI] [PubMed] [Google Scholar]
- 47.Kelesoglu Dincer AB, Sezer S. Systemic immune inflammation index as a reliable disease activity marker in psoriatic arthritis. J Coll Physicians Surg Pak. 2022;32(6):773–778. doi: 10.29271/jcpsp.2022.06.773. [DOI] [PubMed] [Google Scholar]
- 48.Bağcı A, Aksoy F. Systemic immune-inflammation index predicts new-onset atrial fibrillation after ST elevation myocardial infarction. Biomark Med. 2021;15(10):731–739. doi: 10.2217/bmm-2020-0838. [DOI] [PubMed] [Google Scholar]
- 49.Erdoğan M, Erdöl MA, Öztürk S, Durmaz T. Systemic immune-inflammation index is a novel marker to predict functionally significant coronary artery stenosis. Biomark Med. 2020;14(16):1553–1561. doi: 10.2217/bmm-2020-0274. [DOI] [PubMed] [Google Scholar]
- 50.Wang J, Zhou D, Dai Z, Li X. Association between systemic immune-inflammation index and diabetic depression. Clin Interv Aging. 2021;16:97–105. doi: 10.2147/CIA.S285000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zahorec R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy. 2021;122(7):474–488. doi: 10.4149/BLL_2021_078. [DOI] [PubMed] [Google Scholar]
- 52.Liu D, Czigany Z, Heij LR, et al. The value of platelet-to-lymphocyte ratio as a prognostic marker in cholangiocarcinoma: a systematic review and meta-analysis. Cancers. 2022;14(2):438. doi: 10.3390/cancers14020438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang G, Mivefroshan A, Yaghoobpoor S, et al. Prognostic value of platelet to lymphocyte ratio in sepsis: a systematic review and meta-analysis. Biomed Res Int. 2022;2022:9056363. doi: 10.1155/2022/9056363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Woo SJ, Ahn SJ, Ahn J, Park KH, Lee K. Elevated systemic neutrophil count in diabetic retinopathy and diabetes: a hospital-based cross-sectional study of 30,793 Korean subjects. Invest Ophthalmol Vis Sci. 2011;52(10):7697–7703. doi: 10.1167/iovs.11-7784. [DOI] [PubMed] [Google Scholar]
- 55.Smith TL, Weyrich AS. Platelets as central mediators of systemic inflammatory responses. Thromb Res. 2011;127(5):391–394. doi: 10.1016/j.thromres.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schwertz H, Rowley JW, Portier I, et al. Human platelets display dysregulated sepsis-associated autophagy, induced by altered LC3 protein-protein interaction of the Vici-protein EPG5. Autophagy. 2022;18(7):1534–1550. doi: 10.1080/15548627.2021.1990669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fragiotta S, Abdolrahimzadeh S, Dolz-Marco R, Sakurada Y, Gal-Or O, Scuderi G. Significance of hyperreflective foci as an optical coherence tomography biomarker in retinal diseases: characterization and clinical implications. J Ophthalmol. 2021;2021:6096017. doi: 10.1155/2021/6096017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Curcio CA, Zanzottera EC, Ach T, Balaratnasingam C, Freund KB. Activated retinal pigment epithelium, an optical coherence tomography biomarker for progression in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2017;58(6):Bio211–bio26. [DOI] [PMC free article] [PubMed]
- 59.Uji A, Murakami T, Nishijima K, et al. Association between hyperreflective foci in the outer retina, status of photoreceptor layer, and visual acuity in diabetic macular edema. Am J Ophthalmol. 2012;153(4):710–717.e1. 10.1016/j.ajo.2011.08.041. [DOI] [PubMed]
- 60.Vujosevic S, Toma C, Villani E, et al. Diabetic macular edema with neuroretinal detachment: OCT and OCT-angiography biomarkers of treatment response to anti-VEGF and steroids. Acta Diabetol. 2020;57(3):287–296. doi: 10.1007/s00592-019-01424-4. [DOI] [PubMed] [Google Scholar]
- 61.Arrigo A, Capone L, Lattanzio R, Aragona E, Zollet P, Bandello F. Optical coherence tomography biomarkers of inflammation in diabetic macular edema treated by fluocinolone acetonide intravitreal drug-delivery system implant. Ophthalmol Ther. 2020;9(4):971–980. doi: 10.1007/s40123-020-00297-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kodjikian L, Bellocq D, Bandello F, et al. First-line treatment algorithm and guidelines in center-involving diabetic macular edema. Eur J Ophthalmol. 2019;29(6):573–584. doi: 10.1177/1120672119857511. [DOI] [PubMed] [Google Scholar]
- 63.Roy R, Saurabh K, Shah D, Chowdhury M, Goel S. Choroidal hyperreflective foci: a novel spectral domain optical coherence tomography biomarker in eyes with diabetic macular edema. Asia-Pac J Ophthalmol. 2019;8(4):314–318. doi: 10.1097/APO.0000000000000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu S, Wang D, Chen F, Zhang X. Hyperreflective foci in OCT image as a biomarker of poor prognosis in diabetic macular edema patients treating with Conbercept in China. BMC Ophthalmol. 2019;19(1):157. doi: 10.1186/s12886-019-1168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wong Y, Steel DHW, Habib MS, Stubbing-Moore A, Bajwa D, Avery PJ. Vitreoretinal interface abnormalities in patients treatedwith ranibizumab for diabetic macular oedema. Graefes Arch Clin Exp Ophthalmol. 2017;255(4):733–42. [DOI] [PMC free article] [PubMed]
- 66.Kulikov AN, Sosnovskii SV, Berezin RD, Maltsev DS, Oskanov DH, Gribanov NA. Vitreoretinal interface abnormalities in diabetic macular edema and effectiveness of anti-VEGF therapy: an optical coherence tomography study. Clin Ophthalmol. 2017;11:1995–2002. doi: 10.2147/OPTH.S146019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Murakami T, Nishijima K, Akagi T, et al. Optical coherence tomographic reflectivity of photoreceptors beneath cystoid spaces in diabetic macular edema. Invest Ophthalmol Vis Sci. 2012;53(3):1506–1511. doi: 10.1167/iovs.11-9231. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.