Abstract
Introduction
Plate osteosynthesis, external fixators and intramedullary nails are the commonly used devices for fixation of humerus shaft fractures. Humerus nails are gradually coming into popular use. Both antegrade and retrograde nails are used for this, however no evidence clearly states the benefits of one over the other. Thus, the purpose of this study was to evaluate the available evidence comparing the complications and outcomes of antegrade versus retrograde nails.
Patients and methods
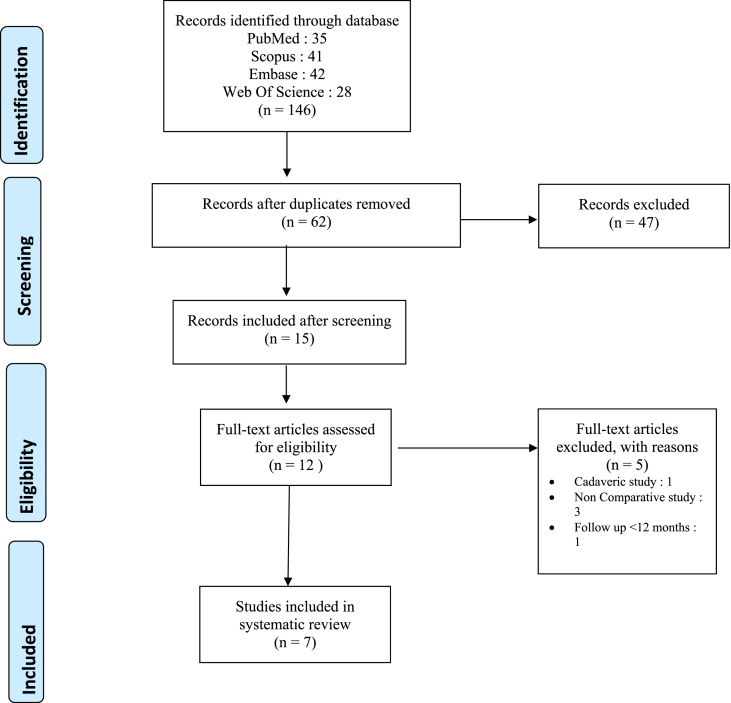
We followed the Preferred Reporting Items for Meta-analyses Statement (PRISMA) guidelines. All studies in any language comparing the use of antegrade and retrograde nailing for humerus fractures, with a minimum follow up of 12 months were included. The primary outcome measures were complications and time to union.
Results
Seven studies including 384 patients (200 antegrade, 184 retrograde) were analyzed. A significantly lower complication rate was observed with retrograde nails (OR 1.77, p = 0.04, 95% CI 1.02,3.06; p = 0.04). Antegrade nails were associated with shorter operative time (MD -13.69, p > 0.00001). There was no significant difference in time to union and intra-operative blood loss between the two techniques.
Conclusion
Retrograde nails have a significantly lower complication rate. However, the surgeon's experience with these devices and the location of the fracture are the primary considerations when choosing either implant
Loe
Level IV.
Keywords: Humerus nailing, Antegrade, Retrograde, Complications, Union
1. Introduction
Fractures of humerus account for 1–3% of all fractures encountered in an orthopaedic clinic.1 Shaft of humerus fractures have long been considered to heal very well with conservative management, with very few specific indications for surgical management. Conventionally, surgical intervention is usually recommended for open fractures, fractures with vascular injury, segmental fractures, pathological fractures, floating elbow, failure of conservative treatment and fracture patterns not amenable to closed reduction.2,3
The treatment philosophy of shaft of humerus fractures has undergone a gradual shift from non-operative to operative methods over the past few decades.4 Currently, various modalities of treatment ranging from closed reduction, casting, functional bracing to plate osteosynthesis and intramedullary nailing are available. Surgical treatment for shaft humerus fractures has slowly gained traction due to the advantage of early mobilization and return to activity. Plate osteosynthesis has been the workhorse for operative management of these fractures for long, allowing direct visualization of fracture site, sparing of adjacent joints and stable fixation. However, with improving implant design for intramedullary devices and the added benefits of load sharing, preservation of soft tissue, periosteal blood supply and avoiding exposure of the radial nerve, humerus nails have emerged as a good alternative to plating.
Humerus nails can be inserted in an antegrade or a retrograde manner. Antegrade nails are technically easier, but associated with the complications such as injury to the articular cartilage, rotator cuff impairment, shoulder stiffness and chronic pain.5 Retrograde nails were introduced to avoid the complications associated with antegrade nailing, are more technically demanding and carry the risk of causing elbow stiffness and fractures of the distal humerus.6 There is no clear evidence documenting the superiority of one technique over the other.7, 8, 9, 10 The use is most often governed by surgeon's preference and fracture location, with nailing from short to the long bone fragment being more biomechanically sound.11 The purpose of this systematic review and meta-analysis, thus, was to evaluate the available evidence comparing the complications and outcomes of antegrade versus retrograde nails (locked nails).
2. Methods
2.1. Protocol and registration
The PRISMA guidelines were followed for conducting this review (Table 1). The protocol for this study was registered in the PROSPERO database CRD42021282451.
Table 1.
PRISMA Flow Diagram for the study.
2.2. Inclusion and exclusion criteria
All prospective and retrospective studies in any language comparing the use of antegrade and retrograde nailing for humerus fractures were included. Cadaveric studies, conference abstracts, case reports and studies with incomplete data for statistical analysis were excluded from the review. Studies with a follow up of less than 12 months were also excluded.
2.3. Search methodology
Using a well-defined search strategy, a primary search was conducted on PubMed, Embase, Web of Science and Scopus. In addition, the bibliographies from the primary search were screened for any additional article.
2.4. Data collection and analysis
The studies were screened by two independent reviewers. The abstracts were read for titles that looked fit for inclusion and full texts were read. The articles relevant to the topic were subsequently identified and included in the review. Any selection conflict was resolved by mutual discussion. Data was collected and entered into pre-specified forms and included the name of author, year, type of study, implant used, age, mechanism of injury and classification. This data is summarised in Table 2.
Table 2.
Basic Characteristics of the study (RCT: Randomized Control Trial; UHN: Unreamed Humerus Nail; UOD: United Orthopaedic Device; MVN: Marchetti Vicenzi nail; RT: Russel Taylor nail; RTA: Road Traffic Accident).
| S. No. | Author | Type of study | Technique | Implant used | Number of patients | Gender (M/F) | Average age and SD in years | Mechanism of injury |
AO classification (A/B/C) | Average follow up | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RTA | Fall | Assault | Others | ||||||||||
| 1. | Sharma | Prospective/RCT | Antegrade | – | 24 | 24/19 | 42.4 ± 1.8 | 13 | 7 | 4 | – | 12/4/8 | 2 years |
| Retrograde | – | 19 | 44.1 ± 2.4 | 11 | 6 | 2 | – | 9/6/4 | 2 years | ||||
| 2. | Scheerlink | Prospective/Case Series | Antegrade | UHN | 17 | 10/7 | 47.8 ± 21/5 | 9 | 8 | – | – | 5/10/2 | 1.6 years |
| Retrograde | MVN | 19 | 9/10 | 54.2 ± 23 | 5 | 12 | 1 | 1 | 9/9/1 | 2.2 years | |||
| 3. | Cheng | Prospective/RCT | Antegrade | UOD | 44 | 26/18 | 43.2 ± 19.3 | 37 | 2 | 3 | 2 | 28/13/3 | 18.6 months |
| Retrograde | UOD | 45 | 28/17 | 48.3 ± 21.4 | 36 | 4 | 2 | 3 | 36/7/2 | 19.8 months | |||
| 4. | Blum | Prospective/Case Series | Antegrade | UHN | 27 | 46/38 | 55.9 ± 18.5 | 45/30/9 | 1 year | ||||
| Retrograde | UHN | 57 | |||||||||||
| 5. | Liu | Prospective/Case Series | Antegrade | – | 69 | 67/25 | 37 ± 13.5 | 33/50/9 | 1 year | ||||
| Retrograde | 23 | ||||||||||||
| 6. | Yin | Prospective/Case Series | Antegrade | RT | 10 | 9/1 | 35.2 ± 10.1 | 3 | 6 | – | 1 | 3/2/5 | 26 months |
| Retrograde | RT | 8 | 5/3 | 37.2 ± 12.9 | 3 | 5 | – | – | 5/3/0 | 26 months | |||
| 7. | Reyes | Retrospective/Case Series | Antegrade | UHN | 9 | 17/5 | 50.4 ± 11 | – | – | – | – | – | 35 months |
| Retrograde | UHN | 13 | 46.6 ± 10.5 | – | – | – | – | – | 40 months | ||||
2.5. Statistical analysis
The data was analyzed using the Review Manager Software (Rev-Man 5.4). For dichotomous data, odds ratio (OR) and 95% confidence intervals (CI) were calculated. For continuous data, mean difference (MD) and 95% CI were calculated. We assessed the heterogeneity using the I2 and >50% was considered as significantly heterogenous. If heterogeneity was not significant, a fixed effect model was used to asses overall estimate. Otherwise, a random effects model was used.
2.6. Risk of bias
The risk of bias was done using the Cochrane risk of bias tool for randomized studies while the MINORS tool was used for non-randomized studies. Publication bias was also assessed for the complication rate using the funnel plot.
3. Results
3.1. Study characteristics
7 studies were included in the review. A summary of the studies is presented in Table 2, Table 3. A total of 384 patients were included, with antegrade nailing in 200 patients and retrograde nailing in 184. The average follow-up ranged from 12 months to a maximum of 40 months.
Table 3.
Summary of reported studies.(E/G/F/P: Excellent/Good/Fair/Poor).
| S No | Name of Study | Technique | Surgical Time | Blood Loss | Time to Union | Length of Hospital Stay | Functional Scores |
|---|---|---|---|---|---|---|---|
| 1 | Sharma | Antegrade | 80 ± 8.4 | 43 ± 8.6 | 15 ± 2.4 | 5.2 ± 1.4 | Stewart Hundley criteria: E/G/F/P: 8/27/6/2 |
| Retrograde | 95 ± 5.3 | 41 ± 7.1 | 16 ± 4.1 | 6.1 ± 2.8 | |||
| 2 | Scheerlinck | Antegrade | 107.7 ± 44.8 | – | – | – | Median difference In constant score: 17 vs 8; statistically significant |
| Retrograde | 89.2 ± 30.1 | – | – | – | |||
| 3 | Cheng | Antegrade | 51.3 ± 13.3 | 60 ± 20 | 10.8 ± 3.5 | 5.1 ± 2.7 | Mayo score: 96.3 ± 4.4 vs 94.8 ± 5.3; Neer Shoulder score: 90.8 ± 6.5 vs 93.5 ± 4.6 |
| Retrograde | 64.8 ± 12.2 | 54 ± 23 | 12.1 ± 3.9 | 4.5 ± 2.2 | |||
| 4 | Blum | Antegrade | – | – | – | – | Poor shoulder function: 3.7% vs 1.8%; Poor elbow function: None vs 1.8% |
| Retrograde | – | – | – | – | |||
| 5 | Liu | Antegrade | 95 ± 42.5 | – | 14 ± 2.5 | – | Constant score: 94.5 ± 5.2 va 99.5 ± 0.4; Mayo score: 99.5 ± 0.3 vs 99.1 ± 0.4 |
| Retrograde | 100 ± 46.25 | – | 12 ± 2 | – | |||
| 6 | Yin | Antegrade | – | – | 7.42 ± 2 | – | Outcome: E/G/F: 5/2/1 vs 5/2 |
| Retrograde | – | – | – | ||||
| 7 | Reyes | Antegrade | 115 ± 15 | 155 ± 50 | 5.2 ± 4.1 | – | Outcome: E/G/F: 6/2/1 vs 8/3/2 |
| Retrograde | 128 ± 54.5 | 265 ± 125 | 3.6 ± 1.5 | – |
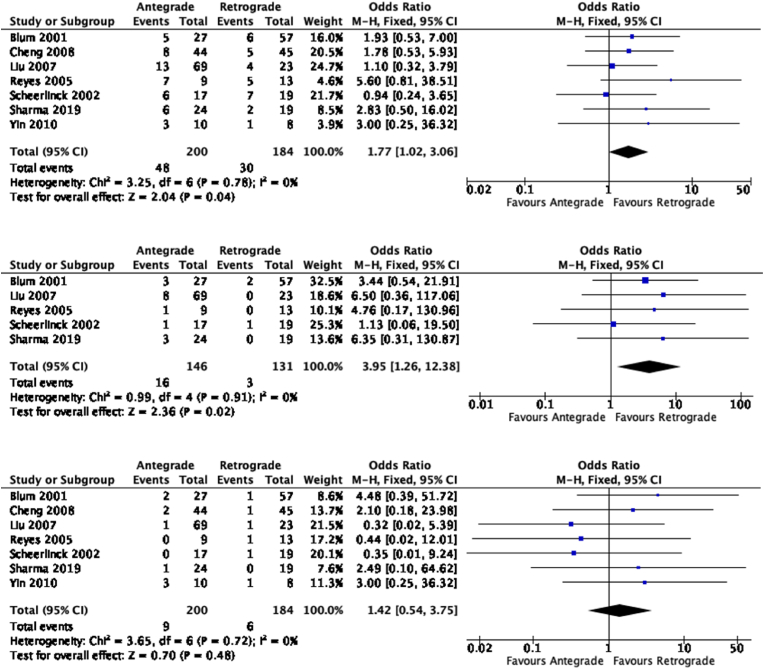
3.2. Complications
The complications reported in various studies are depicted in Table 4. There was a significant difference observed in the total complication rate when comparing the two techniques. The results showed an odds ratio of 1.77 favoring a lower complication rate in the retrograde group (95% CI 1.02,3.06; p = 0.04) (Fig. 1a).
Table 4.
Complications reported in various studies.
| S No | Name of Study | Technique | Infection | Radial nerve palsy | Non Union/Delayed Union | Screw loosening/breakage | Shoulder Stiffness | Iatrogenic fractures |
|---|---|---|---|---|---|---|---|---|
| 1 | Sharma | Antegrade | 1 | 1 | 1 | 0 | 3 | 0 |
| Retrograde | 1 | 0 | 0 | 0 | 0 | 1 | ||
| 2 | Scheerlinck | Antegrade | 0 | 0 | 1 | 1 | 1 | 3 |
| Retrograde | 0 | 1 | 2 | 0 | 1 | 3 | ||
| 3 | Cheng | Antegrade | 0 | 2 | 2 | 4 | 0 | 0 |
| Retrograde | 0 | 1 | 3 | 1 | 0 | 0 | ||
| 4 | Blum | Antegrade | 0 | 2 | 0 | 0 | 3 | 0 |
| Retrograde | 0 | 1 | 0 | 0 | 2 | 3 | ||
| 5 | Liu | Antegrade | 0 | 1 | 4 | 0 | 8 | 0 |
| Retrograde | 0 | 1 | 0 | 0 | 0 | 3 | ||
| 6 | Yin | Antegrade | 0 | 3 | 0 | 0 | 0 | 0 |
| Retrograde | 0 | 1 | 0 | 0 | 0 | 0 | ||
| 7 | Reyes | Antegrade | 0 | 0 | 3 | 0 | 1 | 3 |
| Retrograde | 0 | 1 | 3 | 0 | 0 | 1 |
Fig. 1.
a) Total Complication Rate b) Shoulder Stiffness c) Radial Nerve Palsy.
In terms of shoulder stiffness (reported in 5 studies), there was significant increase in stiffness associated with antegrade nailing, with an odds ratio of 3.95 (95% CI 1.26, 12.38); p = 0.02) (Fig. 1b).
There was however no significant difference observed in the incidence of radial nerve palsy between in the two groups (7 studies). The odds ratio of 1.42 however slightly favor the retrograde group (95% CI 0.54,3.75; p = 0.48) (Fig. 1c).
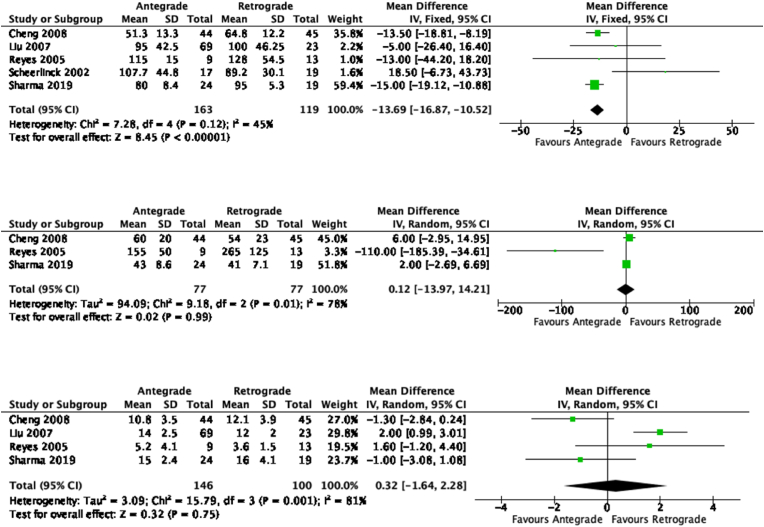
3.2.1. Time to union
This was reported in 4 studies; there was no significant difference observed between the two groups with a mean difference of 0.32 (95% CI -1.64,2.28, p = 0.75) (Fig. 2a).
Fig. 2.
a)Surgical Time b) Blood Loss c) Time to Union.
3.2.2. Perioperative events
The surgical time was documented in 5 studies, and was lesser with the antegrade technique; this was statistically significant with a mean difference of −13.69 (95% CI -16.87,-10.52, p < 0.00001). Only one study by Scheerlinck et al. showed lesser surgical duration with retrograde technique as compared to the antegrade technique (Fig. 2b).
Intra-operative blood loss was documented in 3 studies; no significant difference was found between the 2 groups with a mean difference of 0.12 (95% CI -13.97,14.21; p = 0.99) (Fig. 2c).
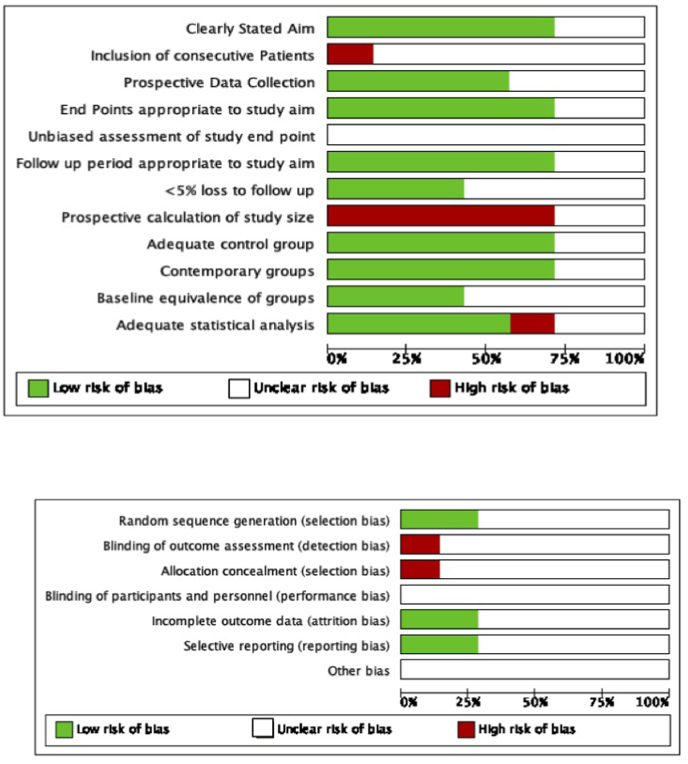
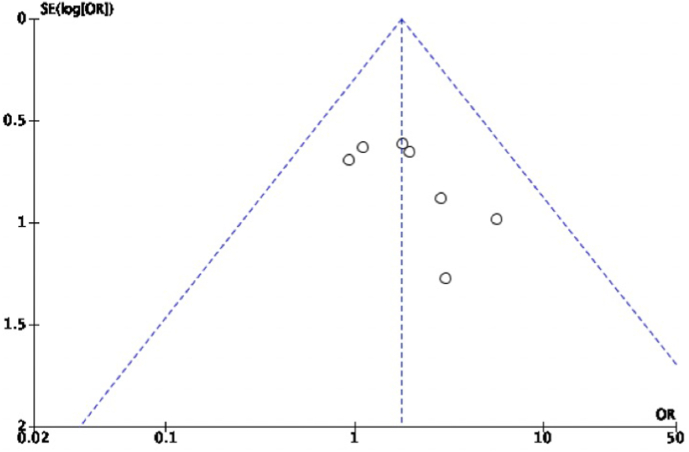
3.3. Risk of bias
The risk of bias for the included studies is depicted in Fig. 3a and b. There was a moderate risk of bias observed in the studies with scores ranging from 16/24 to 19/24. Publication bias was assessed for the complication rate and it was seen that studies with larger sample size were evaluated while those with smaller sample size were not present (Fig. 4).
Fig. 3.
Risk of bias graphs for a)Non Randomized studies b)Randomized studies.
Fig. 4.
Funnel Plot depicting publication bias for comlication rate.
4. Discussion
Intramedullary nailing allows for better preservation of biology and is a load sharing implant, resulting in lesser stress shielding. The introduction of locked intramedullary nailing has also improved rotational stability. Antegrade nailing has its inherent shortcomings like damage to articular cartilage and the rotator cuff, proximal nail migration causing impingement, and the antero-posterior distal locking increases the possibility of iatrogenic neurovascular injury. Retrograde nailing, though technically more challenging, was introduced to overcome these shortcomings. Retrograde nailing was also found to be associated with iatrogenic distal humerus fractures, possibly arising due to high nail resistance in distal humerus during entry and nonlinear entry. Elbow stiffness has also been reported after retrograde humeral nailing, due to violation of triceps.6
The implant choice currently depends on the surgeon's preference and the fracture morphology. Lin et al. in a biomechanical study concluded that nailing from shorter to longer segment creates a more stable construct.11 Plating is an equally efficient option and Beeres et al. in their review comparing nailing and plating observed that satisfactory results can be achieved with both treatment modalities. However, nailing was associated with a lower rate of infection, post-operative radial nerve palsy and a shorter operative time. Shoulder impingement was found to be the main disadvantage of nailing.
Conclusive evidence comparing the outcomes and complications of antegrade and retrograde nailing is not available, with various studies reporting discordant outcomes. The experience with locked intramedullary nailing is limited spanning over the past two decades. We included 7 studies in our meta-analysis (2 Level II and 5 Level IV studies).
Most of them compared intraoperative considerations like duration of surgery, blood loss; length of stay and outcomes like fracture union and functional scores. Complications like radial nerve palsy, iatrogenic fractures, implant loosening/breakage and joint stiffness/pain were also studied.
Amongst the operative considerations, we found a statistically significant difference only in the duration of surgery, with the surgical time being significantly lesser with antegrade nails. 5 studies documented the duration of surgery, with four reporting shorter surgical times with antegrade intramedullary nail.7,8,12 The only study reporting shorter durations with a retrograde nail, was using a Marchetti Vicenzi nail, which did not need distal locking,8 which explains the reduced time. Additionally, retrograde nails are more technically demanding; pre drilling and creation of an entry portal in the distal humerus, non-linear entry, high nail resistance during insertion and locking in the proximal muscular shoulder without a jig are all factors contributing to longer surgical duration. The experience with antegrade humerus nail is more extensive, as these implants have been in use for a longer time as compared to retrograde nails.
Our evaluation showed no statistically significant difference in the operative blood loss and the time to fracture union. Only 3 studies reported blood loss and 2 of them showed a slightly greater loss with antegrade nail, which can be due to breaching of the joint capsule and bulky rotator cuff. Fracture union technically does not depend on the approach, as the principle of secondary bone healing and preservation of biology is the same for both the devices.
We found significant heterogeneity in the reporting of functional outcomes, with all the studies reporting with different criteria. Scheerlink et al. and Liu et al. reported a statistically significant difference in Constant-Murley shoulder score post-operatively.8 Blum et al. reported double the number of patients having poor shoulder function in antegrade nailing group compared to retrograde nailing.9 Cheng et al. reported that time for shoulder functional recovery was longer in the antegrade group, however the final functional outcome was similar in both groups. This reinforces that antegrade nailing has a greater tendency to cause impairment of shoulder function due to cartilage and rotator cuff damage, which may lead to stiffness and pain. Retrograde nailing has the propensity to cause elbow stiffness, the occurrence of which did not reach statistical significance and the final elbow functional outcome was similar in both approaches.
The total complication rate was found to be significantly lower with retrograde nailing. No significant differences were found in the rates of infection. The incidence of radial nerve palsy was higher with antegrade nailing, though not statistically significant. Kolonja et al. in an anatomical study found the latero-medial distal lock of the antegrade nail crossed the radial nerve in 20% cases, whereas in retrograde nails, distal locking bolts were applied in antero-posterior direction, with no impairment of the radial nerve.13 Shoulder stiffness and pain were found to be significantly higher with antegrade nailing, which is in agreement with the existing evidence. This was one of the main factors contributing to the advent of retrograde nails.
Rate of fracture union and implant breakage did not vary significantly between both the groups. Iatrogenic fractures occurred more frequently with retrograde nails, which might have arisen out of improper technique or inadequate instrumentation, coupled with high nail resistance during entry due to thick distal humeral cortex. The introduction of specially designed devices to create entry and improvement in surgical technique may tackle this complication.14
There are a few limitations to our analysis, which calls for further research into this subject. Firstly, variable implants with different designs were used in the studies evaluated, which in turn led to heterogenous findings. This included the use of both rigid and flexible humerus nails. Additionally, there was no data available on whether the nails were locked in static or dynamic mode. Secondly, no uniform criteria were applied for assessment of functional outcomes. In our view, standardized scores, like Constant-Murley score for shoulder and Mayo elbow performance scale for elbow, should be used to reporting outcomes in future studies. Further randomized controlled trials, with large samples must be conducted to generate good quality evidence on the subject.
5. Conclusion
Humerus nails are excellent devices for stable internal fixation of humeral shaft fractures. Retrograde nails have a significantly lower complication rate and address all the concerns historically associated with antegrade nailing. Improved instrumentation and surgical training may increase the use of these devices and further decrease complications.
However, the surgeon's preference and the location of the fracture are the primary considerations when choosing either implant.
Ethical approval
N/A.
Source of funding
Nil.
Authors contribution
DN: Conceptualization, Methodology, review and editing of draft.
AG: Original draft writing.
KJ: Formal Analysis, original draft writing.
PB: Data curation.
SS: Methodology.
MD: Validation and Supervision.
Informed consent
N/A.
Declaration of competing interest
None.
Acknowledgement
None.
References
- 1.Kim S.H., Szabo R.M., Marder R.A. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res. 2012;64:407–414. doi: 10.1002/acr.21563. [DOI] [PubMed] [Google Scholar]
- 2.Spiguel A.R., Steffner R.J. Humeral shaft fractures. Curr Rev Musculoskelet Med. 2012;5:177–183. doi: 10.1007/s12178-012-9125-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker M., Palumbo B., Badman B., Brooks J., Gelderen J.V., Mighell M. Humeral shaft fractures: a review. J Shoulder Elbow Surg. 2011;20:833–844. doi: 10.1016/j.jse.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 4.Schoch B.S., Padegimas E.M., Maltenfort M., Krieg J., Namdari S. Humeral shaft fractures: national trends in management. J Orthop Traumatol. 2017;18:259–263. doi: 10.1007/s10195-017-0459-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ajmal M., O'Sullivan M., McCabe J., Curtin W. Antegrade locked intramedullary nailing in humeral shaft fractures. Injury. 2001;32:692–694. doi: 10.1016/s0020-1383(01)00076-6. [DOI] [PubMed] [Google Scholar]
- 6.Rommens P.M., Blum J., Runkel M. Retrograde nailing of humeral shaft fractures. Clin Orthop. 1998:26–39. [PubMed] [Google Scholar]
- 7.Cheng H.-R., Lin J. Prospective randomized comparative study of antegrade and retrograde locked nailing for middle humeral shaft fracture. J Trauma Acute Care Surg. 2008;65:94–102. doi: 10.1097/TA.0b013e31812eed7f. [DOI] [PubMed] [Google Scholar]
- 8.Scheerlinck T., Handelberg F. Functional outcome after intramedullary nailing of humeral shaft fractures: comparison between retrograde marchetti-vicenzi and unreamed AO antegrade nailing. J Trauma Acute Care Surg. 2002;52:60–71. doi: 10.1097/00005373-200201000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Blum J., Janzing H., Gahr R., Langendorff H.S., Rommens P.M. Clinical performance of a new medullary humeral nail: antegrade versus retrograde insertion. J Orthop Trauma. 2001;15:342–349. doi: 10.1097/00005131-200106000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Li W., Zhang B., Zhang L., Zheng S., mao Wang S. [Comparative study of antegrade and retrograde intramedullary nailing for the treatment of humeral shaft fractures] Zhongguo Gu Shang China J Orthop Traumatol. 2009;22:199–201. [PubMed] [Google Scholar]
- 11.Lin J., Inoue N., Valdevit A., Hang Y.S., Hou S.M., Chao E.Y. Biomechanical comparison of antegrade and retrograde nailing of humeral shaft fracture. Clin Orthop. 1998:203–213. [PubMed] [Google Scholar]
- 12.Reyes-Saravia G.A. Complications of surgical treatment of humeral shaft fractures managed with a UHN pin: comparison of antegrade versus retrograde insertion. Acta Ortop Mex. 2005;19(1):22–27. [Google Scholar]
- 13.Kolonja A., Vécsei N., Mousavi M., Marlovits S., Machold W., Vécsei V. A Clinical and Anatomical Study. Osteosynth Trauma Care. vol. 10. © Georg Thieme Verlag Stuttgart; New York: 2002. Radial nerve injury after anterograde and retrograde locked intramedullary nailing of humerus; pp. 197–199. [Google Scholar]
- 14.Biber R., Zirngibl B., Bail H.J., Stedtfeld H.-W. An innovative technique of rear entry creation for retrograde humeral nailing: how to avoid iatrogenic comminution. Injury. 2013;44:514–517. doi: 10.1016/j.injury.2012.12.019. [DOI] [PubMed] [Google Scholar]