Abstract
Background
Vertebral fractures, frequently resulting from high-impact trauma to the spine, are an increasingly relevant public health concern. Little is known about the long-term economic and demographic trends affecting patients undergoing surgery for such fractures. This study examines national economic and demographic trends in vertebral fracture surgery in the United States to improve value-based care and health care utilization.
Methods
The National Inpatient Sample (NIS) was queried for patients who underwent surgical treatment of a vertebral fracture (ICD-9-CM-3.53) (excluding kyphoplasty and vertebroplasty) between 1993 and 2015. Demographic data included patient age, sex, income, insurance type, hospital size, and location. Economic data including aggregate charge, aggregate cost, hospital cost, and hospital charge were analyzed.
Results
The number of vertebral fracture surgeries, excluding kyphoplasty and vertebroplasty, increased 461% from 3,331 in 1993 to 18,675 in 2014, while inpatient mortality increased from 1.9% to 2.5%.
The mean age of patients undergoing vertebral fracture surgeries increased from 42 in 1993 to 53 in 2015. The aggregate cost of surgery increased from $189,164,625 in 2001 to $1,060,866,580 in 2014, a 461% increase.
Conclusions
The significant increase in vertebral fracture surgeries between 1993 and 2014 may reflect an increased rate of fractures, more surgeons electing to treat fractures surgically, or a combination of both. The increasing rate of vertebral fracture surgery, coupled with increasing hospital costs and mortality, signifies that the treatment of vertebral fractures remains a challenging issue in healthcare. Further research is necessary to determine the underlying cause of both the increase in surgeries and the increasing mortality rate.
Keywords: Vertebral fracture, National inpatient survey, HCUP, Demographics, Economics, Spine surgery
Background
Vertebral fractures most commonly occur in the thoracolumbar region of the spine (T11 to L2) [1]. This region is highly susceptible to injury because it acts as a fulcrum between the more rigid thoracic spine and the more flexible lumbar spine [2]. The most common types of fractures in these regions are chance fractures and thoracolumbar burst fractures. Vertebral fractures normally result from high-impact trauma to the spine [3]. However, in older patients or in those with comorbidities, they can result from low-impact trauma (such as a fall from a standing height) [4,5].
Most vertebral fractures can be managed non-operatively with bracing to immobilize the spinal column [6,7]. However, in cases where there are progressive neurological deficits, gross spinal instability, or intractable pain, surgical intervention is often required [6]. Surgical treatment normally involves decompression of the neural elements and internal fixation to stabilize the affected vertebrae [8].
Vertebral fractures represent a large public health concern given their underdiagnosis and proclivity for re-fracture. If left untreated, a patient's likelihood to develop another vertebral fracture increases five-fold [9]. In 2005, 26.1% of patients with a vertebral fracture experienced a re-fracture within a year. They incurred an extra $5,906 in medical expenses due to this re-fracture [9]. Burge et al projects vertebral fractures to increase in cost (52%) and incidence (53%) by 2025 [10]. There has been a significant investigation into the costs associated with vertebral fractures, however, there is little information about the changing economic and demographic identifiers associated with vertebral fracture surgery. Economic and demographic trends are vital factors to consider when formulating new healthcare policies or improving surgical decision-making.
The purpose of this study was to investigate economic and demographic trends pertaining to the surgical treatment of vertebral fractures between 1993 and 2015 using data from the National Inpatient Sample (NIS) database. We hypothesize that the number of vertebral fracture surgeries and their cost should have increased between 1997 and 2014 especially with the increased rate of fractures and with more spine surgeons electing to treat vertebral fractures surgically. To the authors’ knowledge, this is the largest study of its kind investigating demographic and economic trends in vertebral fracture surgery.
Methods
Data source
The National Inpatient Sample (NIS) was queried for all patients undergoing vertebral fracture surgeries between 1993 and 2015. The NIS database was developed through the Healthcare Cost and Utilization Project (HCUP) and is maintained by the Agency for Healthcare Research and Quality (AHRQ). The NIS comprises a weighted sample of discharges from US hospitals (excluding rehabilitation and long-term acute care hospitals) and represents 96% of the US population.
Patient selection and characteristics
The database was queried between 1993 and 2015 for patients who underwent vertebral fracture surgery using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM 3.53) [11]. Patients undergoing kyphoplasty or vertebroplasty were excluded. Due to the switch from ICD-9 to ICD-10 in 2015, only a few data were collected for that year, and therefore the year 2015 was excluded in some of the statistical comparisons.
Demographic data gathered included age, sex, income, insurance type, hospital size, mortality, length of stay (LOS), and hospital location. Patient age was classified as: <1, 1-17, 18-44, 45-64, 65-84, and 85+. Patients classified as the low-income group lived in a zip code with a mean income in the bottom quartile for that year. Insurance Payers included Medicare, Medicaid, Private Insurance, Uninsured, Other, and Missing. The other category included patients with Tricare/CHAMPUS, a health care program of the United States Department of Defense Military Health System; CHAMPVA, the Civilian Health and Medical Program of the Department of Veterans Affairs; Title V, a program that is available to low-income women, children and adolescents who are not eligible for Medicaid, CHIP, CHIP Perinatal or another source that covers the same service; workers compensation and other governmental programs excluding Medicare and Medicaid. The uninsured category included those classified as being no charge or self-pay. The hospital size was classified into three groups: small, medium, and large, based on bed count. The location of surgery was based on geographical regions of the United States: Northeast, South, Midwest, and West [11].
Economic data on vertebral fracture surgeries included hospital charges and costs, and aggregate hospital charges and costs. In terms of surgical treatment, kyphoplasty and vertebroplasty in addition to outpatient procedures were excluded. Hospital charge represents the mean amount that a US hospital charged for vertebral fracture surgery. Aggregate charge or the “National Bill” is defined as the sum of all hospital charges in the United States. Aggregate cost represents the cost of production for all specific procedures across the United States.
Results
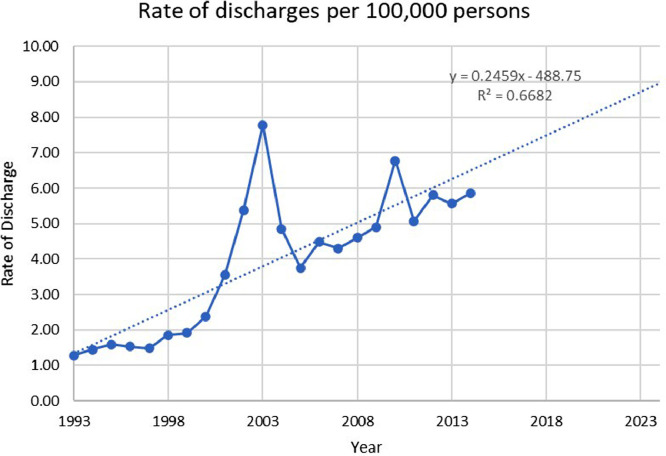
Tabulated from the database, an estimated 256,823 patients underwent vertebral fracture surgery between 1993 and 2014. In that period, the number of vertebral fracture surgeries rose 461% from 3,331 cases in 1993 to 18,675 cases in 2014. The largest increase was in 2003 when the total number of cases rose from 15,436 cases in 2002 to 22,586 cases in 2003, a 46% increase. The peak prevalence was observed in 2003 (Fig. 1). Between 1993 and 2015, the incidence per 100,000 increased 357% from 1.28 in 1993 to 5.86 in 2014 (Fig. 2).
Fig. 1.
Incidence of vertebral fracture repair surgery per 100,000 discharges in the US between 1993 and 2015.
Fig. 2.
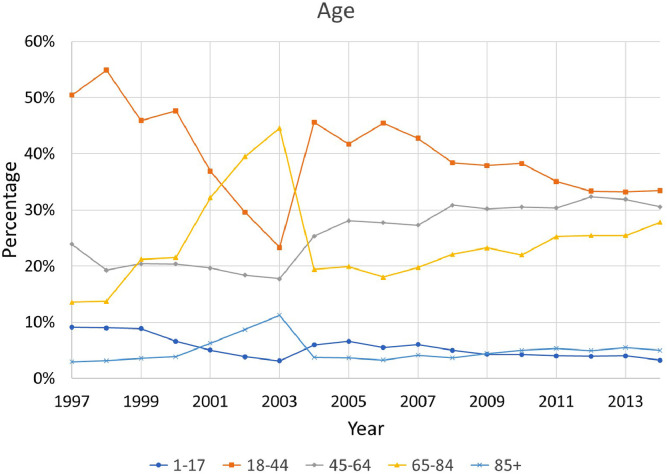
The percentage of patients in each age group was graphed. The percentage of patients in the 1–17 and 18–44 age groups decreased between 1997 and 2014 while the percentage of patients in the 45–64, 65–84, and 85+ age groups all increased between 2004 and 2014.
Most patients who underwent vertebral fracture surgeries between 1997 and 2014 were between the ages of 18 and 44 (40%). The percentage of patients who were between 18 and 44 decreased from 50% in 1997 to 33% in 2014. In 1997, 24% of patients receiving surgery were aged 45-64, this increased to 31% by 2014. In 1997, 14% of patients receiving surgery were aged 65-85, this increased to 28% in 2014. In 1997, 3% of patients receiving vertebral fracture surgery were 85+, this increased to 5% in 2014. In 1997, patients aged 1-17 composed 9% of those receiving surgery, this decreased to 3% in 2014 (Fig. 3). Between 1997 and 2015, the mean age of patients undergoing surgery increased by 11 years, from 42 in 1997 to 53 in 2015. The peak mean age was observed to be 67 in 2003.
Fig. 3.
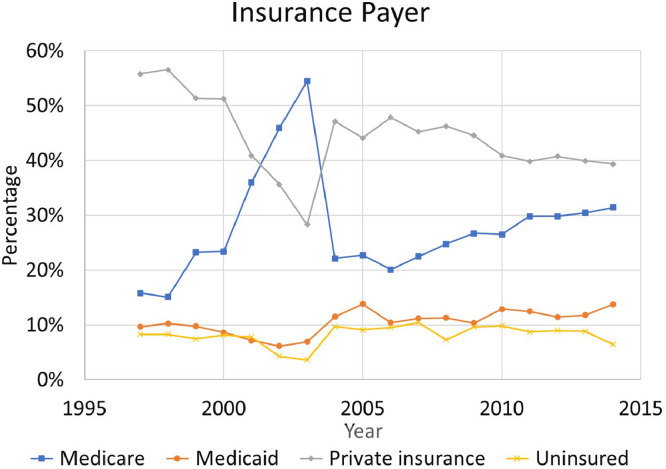
Percentage of patients’ Insurance payers for surgeries between 1997 and 2014. Medicare and Medicaid utilization increased between 1997 and 2014 while private insurance and uninsured patients decreased between 1997 and 2014.
Over the study period, 59% of vertebral fracture surgery patients were male and 41% were female. 76% of all patients were classified as “not low income”. There were 72% of all patients who had their surgery at a teaching hospital and 75% had it at a “large” hospital (75%). Geographically, the Southern region of the United States accounted for the largest fraction of vertebral fracture surgeries (41%). In 1997, 56% of patients were privately insured but this decreased to 39% by 2014. Medicare beneficiaries saw the biggest increase over the study period from 16% of patients in 1997 to 31% of patients in 2014. The prevalence of Medicaid patients increased from 10% to 14% in the same time period. The percentage of uninsured patients decreased from 8% in 1997 to 6% in 2014. Additionally, patients with an “other” payer type decreased from 11% in 1997 to 9% in 2014 (Fig. 4).
Fig. 4.
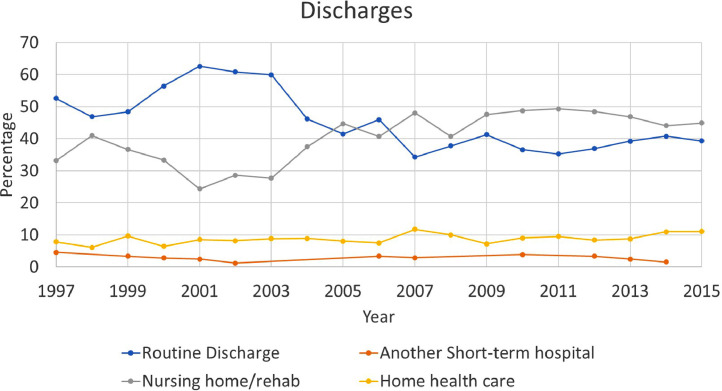
Percentages of different locations to which patients who received vertebral fracture repair were discharged between 1997 and 2015.
The rate of routine discharge decreased by 14% between 1997 and 2015. In 1997, the rate of routine discharge was 53% and this decreased to 39% in 2015. In 1997, 33% of patients were discharged to a nursing home or rehabilitation facility and this percentage increased to 45% in 2015. The percentage of patients discharged to home health care was 8% in 1997 and this increased to 11% in 2015. In 1997, 5% of patients were discharged to another short-term care hospital and this decreased to 2% in 2014.
The mean hospital charge for vertebral fracture surgery increased from $43,394 in 2001 to $175,141 in 2014, a 304% increase. In 2006, the mean hospital cost was $42,104 and this increased to $44,258 in 2014. The aggregate charge (“National Bill”) increased from $189,164,625 in 2001 to $1,060,866,580 in 2014, a 461% increase. In 2006, the aggregate cost was $146,014,536. This increased to $268,255,693 in 2014, an 84% increase. The mean length of stay decreased from 11.2 days in 1997 to 9.5 days in 2015 (figures are not adjusted for inflation). Overall, mortality increased from 1.85% in 2001 to 2.52% in 2015.
Discussion
Due to the increased risk for future vertebral fractures, back pain, loss of neurologic function, and progressive kyphosis, surgery has become an increasingly common intervention for the treatment of vertebral body fractures. To better understand the nature of vertebral fracture surgery, this study utilized the NIS database. To the authors’ knowledge, this is the largest study of its kind which investigates the economic and demographic trends and impact of vertebral fracture surgery.
Between 1993 and 2014 the number of patients surgically treated for a vertebral fracture rose by 461%. It is possible that the incidence is even higher given that prior works have estimated that two-thirds of vertebral fractures are undiagnosed due to radiological errors and dismissal of symptoms by patients [12]. The increase in surgical treatment may be explained by the increased use and recent improvements in radiological detection of vertebral fractures between 1993 and 2014 [13].
The fluctuations in the incidence of vertebral fracture surgeries may be explained by legislative actions that took place over the last decade. In 2000, Congress passed the Benefits Improvement and Protection Act (BIPA) which increased Medicare payments to health care providers [14]. Between 2000 and 2003, the number of patients covered by Medicare increased by 21%. Then, in 2003, Congress passed the Medicare Prescription Drug, Improvement, and Modernization Act (MMA), which further restructured the program [14]. Between 2003 and 2004, there was a 32% decrease in the percentage of patients covered by Medicare. Similarly, between 2000 and 2004, the percentage of patients aged 65-84 showed a similar trend in that the percentage of patients in this age group increased by 23% between 2000 and 2003, only to decrease by 26% in 2004.
Between 2001 and 2014, the mean hospital charge for vertebral fracture surgery increased by 304%. Related literature has identified a similar trend toward increasing costs, although no specific cause to explain this trend has been confirmed [12,15]. This trend is important to consider given that the number of vertebral fracture surgeries performed over this same period had increased by 85%. This increase in vertebral fracture surgery incidence and cost is reflected in the aggregate charge which increased 461% between 2001 and 2014. In 2025, the mean hospital charge is expected, using a logarithmic projection, to increase to $340,477 and the aggregate charge is expected, using a linear projection, to increase to $1,791,381,298. This signifies that vertebral fracture surgeries are going to become increasingly expensive and the most cost-effective approaches and selective indications should be investigated to provide equal and equitable care to all.
In the present study, there was a notable increase in the percentage of people aged 45-64 (7%), 65-85 (14%), and the mean age of patients (11 years) between 1997 and 2014. This may be representative of an increasingly aging population in the United States [10]. In addition, there are associated risk factors with increased age which can also explain this trend. These include osteoporosis, decreased BMI, lower levels of estrogen, vertebral deformity, and a high resting pulse, and have been associated with an increased risk of fracture in patients 65+ [16], [17], [18]. Bouxsein, et al, reported that in patients 65+, a vertebral fracture may result from normal daily activities, such as lifting a heavy object [5]. Center et al also found that even low-impact trauma, such as a fall from a standing height, is sufficient to cause a fracture in patients aged 60+ [4]. Further research is needed to investigate other causes which affect vertebral fracture incidence that is age dependent.
Between 2001 and 2015, mortality increased from 1.85% to 2.52% – a concerning trend. This may be the result of invasive procedures being performed on an aging population with more comorbidities [10,19]. Studies have found that mortality associated with the vertebral fracture surgery population is normally the result of cancer, cardiovascular disease, and pulmonary disease [20], [21], [22]. However, analysis of mortality and morbidity rates associated with different treatments using the Medicare database has found that patients who undergo surgical treatment for vertebral fractures experience lower mortality and morbidity rates than those who undergo conservative management [20]. Some have suggested that this decrease in mortality rate associated with treatment may be caused by increased pulmonary function following surgery [20,23]. Further research is needed to determine the exact cause for this increase in the observed mortality rate.
An estimated 50% of patients treated for a vertebral fracture will require some form of additional care associated with their surgery following discharge and 34.4% of patients will require multiple surgeries [24]. Thus, given the increase in vertebral fracture surgeries, it is important to consider therapeutic options which may help improve one's bone quality to decrease a patient's risk of developing a fracture. While many of these fractures can be treated non-operatively, poor bone quality can also be a contributing risk factor for surgical treatment. Studies investigating the use of calcitonin, vitamin D, and bisphosphonates in the treatment of osteoporosis in patients 60+ have found them all to be effective in lowering a patient's risk for developing a vertebral fracture [25], [26], [27]. All of these medications work to minimize bone density loss, and thus make the bones more resistant to fragility fractures [19,28]. Although these medications have proven effective in attenuating the progression of osteoporosis, only about 30% of patients who suffer a vertebral fracture report using one of these medications at the time of fracture [29]. Therefore, further effort should be devoted to proactively treating osteoporosis before it progresses enough to cause a vertebral fracture. This can in turn decrease complications, mortality, and healthcare expenditure costs.
This study is not without limitations. This study was designed to describe trends and compare them to the results of other investigations. Therefore, any hypothesis presented to explain these trends is purely speculative in nature. Additionally, the NIS database categorizes data using the ICD-9-CM, which has one code for all types of vertebral fracture surgeries. Center, et al, found that patients who have one vertebral fracture have an increased re-fracture risk, even after 15 years [4]. Therefore, since the ICD-9-CM code does not distinguish between initial fractures and subsequent fractures, vertebral re-fracture rates might confound the increase in vertebral fracture surgeries observed. Another complication of the granularity of the ICD-9-CM codes is that it is not possible to delineate between the different types of vertebral fractures which could have precipitated the need for surgery. This could be further complicated by inaccuracies in the ICD-9-CM billing record, errors in transferring hospital records to the NIS database, and a lack of data about revision surgeries. Lastly, data pertaining to pathological conditions which might put a patient at increased risk of developing a vertebral fracture like osteoporosis, cancer, and Paget's disease was not available and therefore was not analyzed.
Conclusion
Vertebral fractures represent a large concern to individuals over 50, given their increased risk of fracture. The purpose of this study was to describe demographic and economic trends in patients who undergo vertebral fracture surgery. Understanding these trends will aid healthcare professionals and health policymakers in making evidence-based decisions about the treatment of vertebral fractures. This study found that the number of vertebral fracture surgeries increased by 461% between 1993 and 2014, most surgeries were performed on males (59%), most patients were aged 18-44 (40%), and the majority of surgeries were performed at teaching hospitals (72%). Additionally, the percentage of patients covered by Medicare increased between 1993 (16%) and 2014 (31%) and the percentage of patients using private insurance decreased between 1993 (56%) and 2014 (39%). Between 2001 and 2014, the national bill for vertebral fracture surgery increased by 461%, and mortality increased by 0.67% between 2001 and 2015. Further research needs to be performed to understand the underlying causes of these trends.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: AMB: Nothing to disclose. KMT: Nothing to disclose. DAR: Nothing to disclose. NL: Nothing to disclose. KB: Nothing to disclose. SG: Nothing to disclose. JML: Nothing to disclose. AF: Nothing to disclose. CS: Nothing to disclose. AV: Nothing to disclose.
Summary Sentence: This retrospective cohort database study showed a significant increase in vertebral fracture surgeries between 1993 and 2014, which may reflect an increased rate of fractures, more surgeons electing to treat fractures surgically, or a combination of both.
References
- 1.Wasnich RD. Vertebral fracture epidemiology. Bone. 1996;18(3):S179–S183. doi: 10.1016/8756-3282(95)00499-8. [DOI] [PubMed] [Google Scholar]
- 2.Singer KP, Day RE, Breidahl PD. In vivo axial rotation at the thoracolumbar junction: an investigation using low dose CT in healthy male volunteers. Clin Biomech. 1989;4(3):145–150. doi: 10.1016/0268-0033(89)90017-X. [DOI] [PubMed] [Google Scholar]
- 3.Parizel PM, van der Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imaging strategies. Eur Spine J. 2010;19(Suppl 1):8–17. doi: 10.1007/s00586-009-1123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center JR, Bliuc D, Nguyen TV, Eisman JA. Risk of subsequent fracture after low-trauma fracture in men and women. JAMA. 2007;297(4):387–394. doi: 10.1001/jama.297.4.387. [DOI] [PubMed] [Google Scholar]
- 5.Bouxsein ML. In: Osteoporosis (Second Edition) Marcus R, Feldman D, Kelsey J, editors. Academic Press; San Diego: 2001. Chapter 19 - Biomechanics of age-related fractures; pp. 509–531. [Google Scholar]
- 6.James KS, Wenger KH, Schlegel JD, Dunn HK. Biomechanical evaluation of the stability of thoracolumbar burst fractures. Spine. 1994;19(15):1731–1740. doi: 10.1097/00007632-199408000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Mumford J, Weinstein JND, Spratt KF, Goel VK. Thoracolumbar burst fractures: the clinical efficacy and outcome of nonoperative management. Spine. 1993;18(8):955–970. [PubMed] [Google Scholar]
- 8.Shono Y, McAfee PC, Cunningham BWB. Experimental study of thoracolumbar burst fractures: a radiographic and biomechanical analysis of anterior and posterior instrumentation systems. Spine. 1994;19(15):1711–1722. doi: 10.1097/00007632-199408000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Lindsay R, Burge RT, Strauss DM. One year outcomes and costs following a vertebral fracture. Osteoporos Int. 2005;16(1):78–85. doi: 10.1007/s00198-004-1646-x. [DOI] [PubMed] [Google Scholar]
- 10.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22(3):465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 11.Gacutan K. 2015. Introduction to the HCUP National Inpatient Sample (NIS) 2015; p. 59. [Google Scholar]
- 12.Cooper C, Atkinson EJ, MichaelO'Fallon W, Melton JL. Incidence of clinically diagnosed vertebral fractures: A population-based study in rochester, minnesota, 1985-1989. J Bone Miner Res. 7(2):221-227. [DOI] [PubMed]
- 13.Kaup M, Wichmann JL, Scholtz J-E, et al. Dual-energy CT–based display of bone marrow edema in osteoporotic vertebral compression fractures: impact on diagnostic accuracy of radiologists with varying levels of experience in correlation to MR imaging. Radiology. 2016;280(2):510–519. doi: 10.1148/radiol.2016150472. [DOI] [PubMed] [Google Scholar]
- 14.Center for Medicare and Medicaid Services. Medicare-and-Medicaid-Milestones-1937-2015.pdf. https://www.cms.gov/About-CMS/Agency-Information/History/Downloads/Medicare-and-Medicaid-Milestones-1937-2015.pdf. Accessed July 18, 2018.
- 15.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet North Am Ed. 2002;359(9319):1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 16.Nevitt MC, Cummings SR, Stone KL, et al. Risk factors for a first-incident radiographic vertebral fracture in women ≥65 years of age: the study of osteoporotic fractures. J Bone Miner Res. 20(1):131-140. [DOI] [PubMed]
- 17.Melton LJ, Wenger DE, Atkinson EJ, et al. Influence of baseline deformity definition on subsequent vertebral fracture risk in postmenopausal women. Osteoporos Int. 2006;17(7):978–985. doi: 10.1007/s00198-006-0106-1. [DOI] [PubMed] [Google Scholar]
- 18.Roy DK, O'Neill TW, Finn JD, et al. Determinants of incident vertebral fracture in men and women: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 2003;14(1):19–26. doi: 10.1007/s00198-002-1317-8. [DOI] [PubMed] [Google Scholar]
- 19.Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and Vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med. 1997;337(10):670–676. doi: 10.1056/NEJM199709043371003. [DOI] [PubMed] [Google Scholar]
- 20.Edidin AA, Ong KL, Lau E, Kurtz SM. Morbidity and mortality after vertebral fractures: comparison of vertebral augmentation and nonoperative management in the medicare population. Spine. 2015;40(15):1228–1241. doi: 10.1097/BRS.0000000000000992. [DOI] [PubMed] [Google Scholar]
- 21.Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O. Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003;14(1):61–68. doi: 10.1007/s00198-002-1316-9. [DOI] [PubMed] [Google Scholar]
- 22.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet North Am Ed. 1999;353(9156):878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 23.Yang H-L, Zhao L, Liu J, et al. Changes of pulmonary function for patients with osteoporotic vertebral compression fractures after kyphoplasty. J Spinal Disord. 2007;20(3):221–225. doi: 10.1097/01.bsd.0000211273.74238.0e. [DOI] [PubMed] [Google Scholar]
- 24.Gehlbach SH, Burge RT, Puleo E. Hospital care of osteoporosis-related vertebral fractures. Osteoporos Int. 2003;14(1):53–60. doi: 10.1007/s00198-002-1313-z. [DOI] [PubMed] [Google Scholar]
- 25.Gehlbach SH, Fournier M, Bigelow C. Recognition of osteoporosis by primary care physicians. Am J Public Health. 2002;92(2):271–273. doi: 10.2105/ajph.92.2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE. Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int. 2004;15(10):767–778. doi: 10.1007/s00198-004-1675-5. [DOI] [PubMed] [Google Scholar]
- 27.Lufkin EG. Treatment of postmenopausal osteoporosis with transdermal estrogen. Ann Intern Med. 1992;117(1):1. doi: 10.7326/0003-4819-117-1-1. [DOI] [PubMed] [Google Scholar]
- 28.Felson DT, Zhang Y, Hannan MT, Kiel DP, Wilson P, Anderson JJ. The effect of postmenopausal estrogen therapy on bone density in elderly women. N Engl J Med. 1993;329(16):1141–1146. doi: 10.1056/NEJM199310143291601. [DOI] [PubMed] [Google Scholar]
- 29.Gehlbach SH, Bigelow C, Heimisdottir M, May S, Walker M, Kirkwood JR. Recognition of vertebral fracture in a clinical setting. Osteoporos Int. 2000;11(7):577–582. doi: 10.1007/s001980070078. [DOI] [PubMed] [Google Scholar]