Abstract
Adolescents and young adults (AYA) with rheumatologic diseases are at high risk for poor outcomes and gaps in care when transitioning from pediatric to adult care. However, tools for evaluating transition readiness and assessing the impact of transition interventions are limited. We implemented a written transition policy at our pediatric rheumatology center and evaluated preparation for transition among AYA 16 and older before and after distribution. 31 of 77 patients completed the follow-up survey (response rate 40%). Patient report of transition counseling increased following written transition policy implementation, though these results were not statistically significant in our small cohort. Most follow-up respondents (n = 19, 61%) had not yet completed care transfer; 4 (13%) had arranged a visit with an adult rheumatologist and 8 (26%) had fully transitioned to adult care. Those who successfully completed care transfer were older, had completed higher levels of education, and had significantly higher baseline transition preparation scores compared to those with no transfer arranged or planned visit only. Our single-center pilot study demonstrated that longitudinal assessment of transition preparation is feasible and that scores are significantly associated with care transfer outcomes. Tracking transition preparation over time may provide practices with information on areas of highest need for transition guidance and predict successful transfer among AYA with rheumatologic disease.
Keywords: Transition, Transfer of care, Adolescent, Patient-reported outcomes, Survey
Background
Adolescents and young adults (AYA) are at high risk for poor outcomes and gaps in care when transitioning from pediatric to adult care [1, 2]. The risks of this care transition period are well described in AYA with rheumatologic diseases, including increased disease flares, missed follow up visits, medication non-adherence, and even increased mortality [3–6]. There are increasing efforts to bring comprehensive transition care to AYA with rheumatologic diseases [7–11], though many pediatric rheumatology programs lack formalized transition pathways [12, 13]. Despite increased attention to high-quality transition care, measuring preparation for transition and evaluating transfer outcomes remain challenging. While several instruments have been developed to evaluate AYA preparation for and/or readiness for transition to adult care [14–17], these have not been previously correlated with transfer outcomes among youth with rheumatologic diseases. Additionally, owing to the difficulty of assessing effective transition, many interventions have been evaluated with measures of patient or provider satisfaction rather than objective measures of successful transfer [7, 8], especially in care settings where pediatric and adult specialists are not part of the same integrated healthcare organization.
We evaluated preparation for transition with a validated quality measure prior to implementing a written transition policy at our pediatric rheumatology center, as previously reported in this journal [18]. Following successful dissemination of the written transition policy, we repeated the survey to assess longitudinal changes in transition preparation after implementing the transition policy, and to evaluate the association of transition preparation scores with transfer outcomes.
Findings
Methods
We surveyed AYA 16 and older who had an ICD-9 or -10-confirmed rheumatologic diagnosis and had attended ≥3 rheumatology appointments with the ADolescent Assessment of Preparation for Transition (ADAPT) [14] through a REDCap [19, 20] form distributed via email prior to transition policy implementation. This instrument assesses transition preparation based on patient self-report of skills reviewed at the most recent visit (maximum 12 months prior) in three domains: (1) self-management, (2) medications and (3) transfer planning. We created a total composite score comprised of the proportion of affirmative answers to summarize overall preparation and to assess longitudinal change in preparation [18].
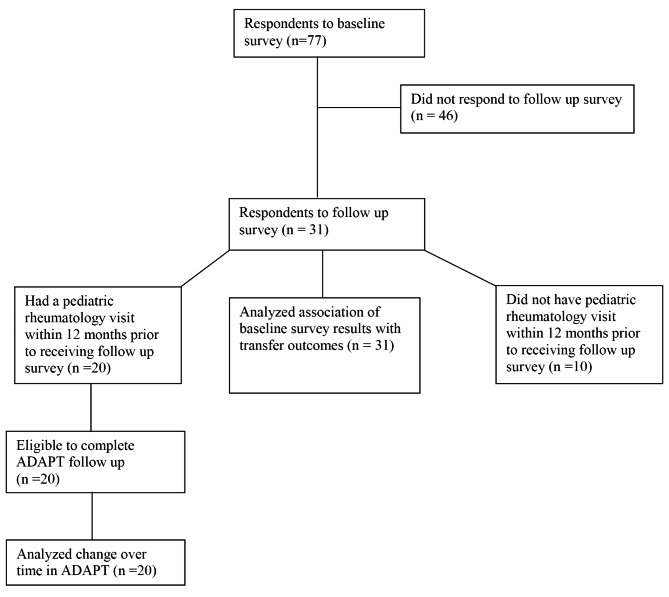
Due to reduction of in-person visits amid the COVID-19 pandemic, in-person distribution of the transition policy at each outpatient visit for all patients 14 and older began approximately 1 year after the initial survey. Patients and parents were asked to sign and return the written policy to confirm dissemination to the intended population. The policy was also made available on our clinic website for patients attending virtual visits. Respondents were invited via email to complete a REDCap follow-up survey including the ADAPT instrument and assessment of care transfer outcomes one year after transition policy implementation, and two years after the baseline survey. Those with a pediatric rheumatology visit within the last 12 months were eligible to complete the ADAPT instrument. Care transfer outcomes, specifically scheduling and attending a visit with an adult rheumatologist, were collected for all respondents regardless of timing of last pediatric rheumatology visit. A flow diagram of participants included in each analysis is presented in Fig. 1. The association between baseline transition preparation scores and transfer outcomes was evaluated using one-way ANOVA. Change in transition preparation over time was assessed with generalized estimating equations (identity or logit link, depending on the outcome) and robust standard errors to account for within patient correlation of repeated measures. This study was approved by the Boston Children’s Hospital Institutional Review Board, protocol number #P00031635.
Fig. 1.
Flow Diagram of Survey Participants
Results
Seventy-seven patients participated in our baseline assessment of transition preparation and were eligible for the follow-up survey, of whom 31 responded (40%). Of these, 20 had attended a pediatric rheumatology visit within the last 12 months and therefore were eligible to complete the follow-up ADAPT instrument. Each group of respondents had similar demographic and disease characteristics (Table 1), though owing to the older ages at follow up, respondents reported higher levels of formal education and longer length of time seeing their doctors (p < 0.001) compared to baseline. Respondents to the follow-up survey were more likely to be female compared to baseline respondents (p = 0.045).
Table 1.
Survey Participant Characteristics by Survey Response
| Respondents to Baseline Survey (n = 77) |
Respondents to Follow-Up Survey (n = 31) |
Respondents to Follow-Up Survey with Visit in Last Year (n = 20) |
||
|---|---|---|---|---|
| n (%) or Median [IQR] | ||||
| Race | ||||
| White | 66 (86) | 25 (81) | 17 (85) | |
| Black or African American | 8 (10) | 2 (6) | 0 (0) | |
| Asian | 1 (1) | 1 (3) | 1 (5) | |
| Ethnicity | ||||
| Not Hispanic, Latino, or Spanish Origin | 72 (94) | 29 (94) | 19 (95) | |
| Puerto Rican | 3 (4) | 2 (6) | 1 (5) | |
| Other Hispanic, Latino, or Spanish Origin | 2 (3) | 0 (0) | 0 (0) | |
| Female | 64 (83) | 29 (94) | 18 (90) | |
| Age (years) | 19 [17–20] | 20 [20–22] | 20 [20–22] | |
| Education | ||||
| 9th grade | 2 (3) | 0 (0) | 0 (0) | |
| 10th grade | 9 (12) | 0 (0) | 0 (0) | |
| 11th grade | 13 (17) | 0 (0) | 0 (0) | |
| 12th grade, high school graduate, or GED | 13 (17) | 6 (19) | 5 (25) | |
| Some college | 33 (43) | 14 (45) | 10 (50) | |
| College graduate | 7 (9) | 11 (35) | 5 (25) | |
| Primary Rheumatologic Diagnosis* | ||||
| Juvenile Idiopathic Arthritis | 52 (68) | 22 (71) | 15 (75) | |
| Uveitis (idiopathic) | 2 (3) | 1 (3) | 0 (0) | |
| Chronic Recurrent Multifocal Osteomyelitis | 3 (4) | 0 (0) | 0 (0) | |
| Systemic Lupus Erythematosus | 8 (10) | 3 (10) | 1 (5) | |
| Mixed Connective Tissue Disease | 4 (5) | 2 (6) | 1 (5) | |
| Sjögren’s | 3 (4) | 1 (3) | 1 (5) | |
| Juvenile dermatomyositis | 3 (4) | 2 (6) | 2 (10) | |
| Other vasculitis | 4 (5) | 0 (0) | 0 (0) | |
| Length of time seeing doctor | ||||
| At least 6 months but less than 1 year | 2 (3) | 0 (0) | 0 (0) | |
| At least 1 year but less than 3 years | 20 (26) | 2 (6) | 2 (10) | |
| At least 3 years but less than 5 years | 19 (25) | 11 (35) | 5 (25) | |
| 5 years or more | 36 (47) | 18 (58) | 13 (65) | |
| Frequency of visits in past year | ||||
| None | 0 (0) | 11 (35) | 0 (0) | |
| 1 time | 17 (22) | 7 (23) | 7 (35) | |
| 2 times | 24 (31) | 6 (19) | 6 (30) | |
| 3 times | 17 (22) | 4 (13) | 4 (20) | |
| 4 times | 13 (17) | 3 (10) | 3 (15) | |
| 5 or more times | 6 (8) | 0 (0) | 0 (0) | |
| Health status | ||||
| Excellent | 10 (13) | 3 (10) | 1 (5) | |
| Very good | 18 (23) | 8 (26) | 7 (35) | |
| Good | 32 (42) | 16 (52) | 11 (55) | |
| Fair | 15 (19) | 4 (13) | 1 (1) | |
| Poor | 2 (3) | 0 (0) | 0 (0) | |
*Some patients have more than 1 primary rheumatologic diagnosis.
Scores in the self-management and medication counseling domains and total composite scores at follow-up showed small numerical increases compared to the baseline, though this did not reach statistical significance in our small cohort (Table 2). In contrast, the median transfer planning score did not differ over time, with few respondents answering affirmatively to questions about discussing a specific transfer plan and receiving this plan in writing.
Table 2.
Change Over Time in Selected ADAPT Transition Preparation Measures
| Baseline Survey N = 77 |
Two Year Follow-Up N = 20 |
p-value | |
|---|---|---|---|
| Survey Question |
Yes n (%) |
Yes n (%) |
|
| In the last 12 months, did you talk with this provider without your parent or guardian in the room? | 46 (59.7%) | 12 (60.0%) | 0.50 |
| In the last 12 months, did you and this provider talk about you being more in charge of your health? | 53 (68.8%) | 14 (70.0%) | 0.91 |
| In the last 12 months, did you and this provider talk about remembering to take your medicines? | 37 (75.5%) | 8 (80.0%) | 0.49 |
| In the last 12 months, did you and this provider talk about whether you may need to change to a new provider who treats mostly adults? | 31 (40.8%) | 8 (44.4%) | 0.68 |
| In the last 12 months, did this provider ask if you had any questions or concerns about changing to a new provider who treats mostly adults? | 22 (71.0%) | 6 (75.0%) | 0.82 |
| In the last 12 months, did you and this provider talk about a specific plan for changing to a new provider who treats mostly adults? | 14 (45.2%) | 5 (62.5%) | 0.22 |
| Composite Transition Preparation Scores | Median [IQR] | Median [IQR] | |
| Self-management (highest score possible 4) | 2 [1–3] | 2.5 [1–3] | 0.36 |
| Medication counseling (highest score possible 3) | 2 [2,3] | 2.5 [2,3] | 0.58 |
| Transfer planning (highest score possible 4) | 0 [0–2] | 0 [0–3] | 0.31 |
| Total transition composite score (% of items answered yes) | 0.45 [0.27–0.55] | 0.52 [0.32–0.64] | 0.26 |
At the time of follow-up survey, most respondents (n = 19, 61%) had not yet completed care transfer to adult rheumatology (Table 3). Four (13%) had arranged a visit with an adult rheumatologist and 8 (26%) had fully transitioned to adult care. Those who had successfully completed rheumatology care transfer were older and had completed higher levels of education compared to those with no transfer arranged or planned visit only. Respondents with higher baseline transition preparation scores were significantly more likely to have completed care transfer to an adult rheumatologist.
Table 3.
Patient Characteristics and ADAPT Scores by Transfer Outcome
| Completed Transfer | Visit Arranged | No Transfer Arranged | p-value | |
|---|---|---|---|---|
| n = 8 | n = 4 | n = 19 | ||
| Age | 22.5 [21–23] | 22 [21–22.5] | 20 [19–21] | 0.009 |
| Education Level | 0.007 | |||
| High School Graduate | 0 (0) | 0 (0) | 6 (32) | |
| Some College | 2 (25) | 1 (25) | 11 (58) | |
| College Graduate | 6 (75) | 3 (75) | 2 (11) | |
| Female | 8 (100) | 4 (100) | 17 (89) | 0.51 |
| Primary Rheumatologic Disease | 0.29 | |||
| Juvenile Idiopathic Arthritis | 4 (50) | 4 (100) | 14 (74) | |
| Idiopathic Uveitis | 0 (0) | 0 (0) | 1 (5) | |
| Systemic Lupus Erythematosus | 2 (25) | 0 (0) | 1 (5) | |
| Mixed Connective Tissue Disease | 2 (25) | 0 (0) | 0 (0) | |
| Sjögren’s | 0 (0) | 0 (0) | 1 (5) | |
| Juvenile dermatomyositis | 0 (0) | 0 (0) | 2 (11) | |
| Composite scores: Baseline | n = 8 | n = 4 | n = 19 | |
| Total transition composite score (% yes) | 0.68 [0.48–0.88] | 0.52 [0.44–0.64] | 0.45 [0.27–0.55] | 0.01 |
| Self-management (highest possible 4) | 3 [2-3.5] | 2.5 [1-2] | 3 [1-3] | 0.36 |
| Transfer planning (highest possible 4) | 3 [0.5–3.5] | 1.5 [0.5-3] | 0 [0–1] | 0.005 |
| n = 4 | n = 2 | n = 14 | ||
| Medication counseling (highest possible 3) | 2.5 [1.5-3] | 3 [3] | 2 [2,3] | 0.29 |
| Composite scores: Follow Up* | n = 1 | n = 2 | n = 17 | |
| Total transition composite score | 0.64 | 0.56 [0.12-1.00] | 0.50 [0.36–0.64] | 0.80 |
| Self-management | 3 | 2.5 [1–4] | 2 [1–3] | 0.82 |
| Transfer planning | 3 | 2 [0–4] | 0 [0–2] | 0.37 |
| n = 1 | n = 1 | n = 8 | ||
| Medication counseling | 1 | 3 | 2.5 [2, 3] | 0.20 |
*Only patients with last rheumatology visit within 12 months were eligible to complete follow-up ADAPT (n = 20). Medication and transfer composites applicable only to those patients screening in based on earlier questions
Conclusion
In this single center pilot study, we demonstrated the feasibility of tracking patient preparation for transition longitudinally to evaluate change over time and assess response to a transition intervention, which was the distribution of a clinic transition policy in this report. We did not find significant improvements in preparation scores between the pre-policy and post-policy periods, which may be due to the limited impact of the transition policy intervention, or to underpowering given the low numbers of eligible respondents in the follow-up survey.
We found that baseline transition preparation scores were associated with patient-reported transfer outcomes, including attendance at a visit with an adult rheumatologist. By demonstrating the association of transition preparation scores with transfer outcomes in youth with rheumatologic diseases, our findings may identify at-risk AYA in need of additional support during the transition period, and to predict patients who may be ready for successful transfer. Tracking transition preparation longitudinally may provide practices with information on areas of highest need for transition counseling. For example, in our cohort we saw lowest scores in the transfer planning domain over both time points, which highlights the need to incorporate more focused discussions on these topics into clinical care.
Our study had several limitations, including small sample size, and delays in policy implementation due to COVID-19 which lengthened the time interval between the baseline and follow-up surveys, and may have impacted our response rate. COVID-related delays in care may also have impacted the frequency of visits during the follow-up period, decreasing exposure to the written transition policy and limiting opportunities to discuss the policy with the care team, as described by other centers attempting transition policy implementation during the pandemic [21]. Additionally, as a single-center study, our results may not be generalizable to all care settings. Our center is a quaternary care children’s hospital without an institution-wide age of transition and with several highly specialized programs where patients may be followed into adulthood. Age to initiate discussions about transition and transfer have traditionally been left to individual providers’ discretion, which may account for relatively low levels of transition counseling and higher age of transfer among our cohort.
Despite these limitations, our pilot study demonstrated that longitudinal assessment of transition preparation is feasible and predicts successful transfer outcomes. Further research is needed in larger cohorts to validate the association between transition preparation scores and transfer outcomes. Finally, higher transition preparation scores may be a function of both the actual transition counseling received, and patient resources, including self-management skills [22, 23]. Such self-management skills have also been shown to be correlated with socioeconomic status [24], which may itself impact successful transfer [4–6]. Therefore, identifying elements of transition preparation that are most readily modifiable via transition counseling and other clinical team supports may help to design more effective interventions for AYA with rheumatologic diseases who are at risk of poor transfer outcomes.
Acknowledgements
Not applicable.
Abbreviations
- ADAPT
ADolescent Assessment of Preparation for Transition.
- AYA
adolescents and young adults.
Authors’ contributions
JER conceptualized and designed the study, adapted the survey instrument, oversaw distribution of the survey and tracking of transition policy delivery, created tables and figures, and drafted the manuscript. OH contributed to the design of the study, critically revised and led patient and parent review of the transition policy, and reviewed the manuscript. CP assisted in design of analysis plan, carried out the analyses, created tables, and reviewed and revised the manuscript. MA, BE, MH and SS assisted with disseminating and tracking receipt of the transition policy in rheumatology clinic, and reviewed and revised the manuscript. JD assisted with survey distribution, REDCap management, IRB approval, and reviewed the manuscript. MBS conceptualized and designed the study, supervised revision and implementation of the transition policy, and reviewed and revised the manuscript. All authors read and approved the final manuscript.
Funding
Dr. Roberts was supported by NIH grant 5T32AI007512, a Lupus Foundation of America Gary S. Gilkeson Career Development Award, and a Fred Lovejoy House-staff Research and Education Fund grant. This work was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541). The NIH, Fred Lovejoy Fund, the Lupus Foundation of America, and the Harvard Catalyst had no role in the design and conduct of the study.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request and pending approval of data sharing by the Boston Children’s Hospital IRB.
Declarations
Ethics approval and consent to participate
This study was approved by the Boston Children’s Hospital Institutional Review Board (IRB-P00031635). All eligible patients received an email describing the study and were informed that completing the survey constituted consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians; Transitions Clinical Report Authoring Group. Pediatrics 2011 Jul;128(1):182–200. doi:10.1542/peds.2011-0969. [DOI] [PubMed]
- 2.McManus MA, Pollack LR, Cooley WC, McAllister JW, Lotstein D, Strickland B, Mann MY. Current status of transition preparation among youth with special needs in the United States. Pediatrics. 2013;131;6:1090–7. doi: 10.1542/peds.2012-3050. [DOI] [PubMed] [Google Scholar]
- 3.Hersh A, von Scheven E, Yelin E. Adult outcomes of childhood-onset rheumatic diseases. Nat Rev Rheumatol. 2011;7(5):290–5. doi: 10.1038/nrrheum.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Son MB, Sergeyenko Y, Guan H, Costenbader KH. Disease activity and transition outcomes in a childhood-onset systemic lupus erythematosus cohort. Lupus. 2016 Nov;25;13:1431–1439. doi: 10.1177/0961203316640913. [DOI] [PMC free article] [PubMed]
- 5.Bitencourt N, Makris UE, Solow EB, Wright T, Reisch EJ, Bermas BL. Predictors of Adverse outcomes in patients with systemic lupus erythematosus transitioning to adult care. Semin Arthritis Rheum. 2021;51(2):353–9. doi: 10.1016/j.semarthrit.2021.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Bitencourt N, Bermas BL, Makris UE, Wright T, Reisch J, Solow EB. Time to First Completed Visit and Health Care Utilization Among Young Adults Transferring From Pediatric to Adult Rheumatologic Care in a Safety-Net Hospital. Arthritis Care Res (Hoboken) 2021;73(12):1730–8. doi: 10.1002/acr.24409. [DOI] [PubMed] [Google Scholar]
- 7.Stringer E, Scott R, Mosher D, MacNeill I, Huber AM, Ramsey S, Lang B. Evaluation of a Rheumatology Transition Clinic. Pediatr Rheumatol Online J. 2015 Jun 11;13:22. doi: 10.1186/s12969-015-0016-x. [DOI] [PMC free article] [PubMed]
- 8.McDonagh JE, Southwood TR, Shaw KL, British Society of Paediatric and Adolescent Rheumatology The impact of a coordinated transitional care programme on adolescents with juvenile idiopathic arthritis. Rheumatol (Oxford) 2007;46(1):161–8. doi: 10.1093/rheumatology/kel198. [DOI] [PubMed] [Google Scholar]
- 9.Jensen PT, Karnes J, Jones K, Lehman A, Rennebohm R, Higgins GC, Spencer CH, Ardoin SP. Quantitative evaluation of a pediatric rheumatology transition program. Pediatr Rheumatol Online J. 2015 May 24;13:17. doi: 10.1186/s12969-015-0013-0. [DOI] [PMC free article] [PubMed]
- 10.Walter M, Kamphuis S, van Pelt P, de Vroed A, Hazes JMW. Successful implementation of a clinical transition pathway for adolescents with juvenile-onset rheumatic and musculoskeletal diseases. Pediatr Rheumatol Online J. 2018 Aug 3;16(1):50. doi: 10.1186/s12969-018-0268-3. [DOI] [PMC free article] [PubMed]
- 11.Overbury RS, Huynh K, Bohnsack J, Frech T, Hersh A. A novel transition clinic structure for adolescent and young adult patients with childhood onset rheumatic disease improves transition outcomes. Pediatr Rheumatol Online J. 2021 Dec 1;19(1):164. doi: 10.1186/s12969-021-00651-w. PMID: 34852832; PMCID: PMC8638174. [DOI] [PMC free article] [PubMed]
- 12.Chira P, Ronis T, Ardoin S, White P. Transitioning youth with rheumatic conditions: perspectives of pediatric rheumatology providers in the United States and Canada. J Rheumatol. 2014 Apr;41;4:768 – 79. doi: 10.3899/jrheum.130615. Epub 2014 Mar 1. [DOI] [PubMed]
- 13.Clemente D, Leon L, Foster H, Carmona L, Minden K. Transitional care for rheumatic conditions in Europe: current clinical practice and available resources. Pediatr Rheumatol Online J. 2017 Jun 9;15;1:49. doi: 10.1186/s12969-017-0179-8. [DOI] [PMC free article] [PubMed]
- 14.Sawicki GS, Garvey KC, Toomey SL, et al. Development and Validation of the Adolescent Assessment of Preparation for Transition: A Novel Patient Experience Measure. J Adolesc Health. 2015;57:282–7. doi: 10.1016/j.jadohealth.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sawicki GS, Whitworth R, Gunn L, Butterfield R, Lukens-Bull K, Wood D. Receipt of health care transition counseling in the national survey of adult transition and health. Pediatrics. 2011;128(3):e521-9. doi: 10.1542/peds.2010-3017. [DOI] [PubMed] [Google Scholar]
- 16.Ferris ME, Harward DH, Bickford K, Layton JB, Ferris MT, Hogan SL, Gipson DS, McCoy LP, Hooper SR. A clinical tool to measure the components of health-care transition from pediatric care to adult care: the UNC TR(x)ANSITION scale. Ren Fail. 2012;34(6):744–53. doi: 10.3109/0886022X.2012.678171. [DOI] [PubMed] [Google Scholar]
- 17.Wood DL, Sawicki GS, Miller MD, Smotherman C, Lukens-Bull K, Livingood WC, Ferris M, Kraemer DF. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014 Jul-Aug;14(4):415 – 22. doi: 10.1016/j.acap.2014.03.008. PMID: 24976354. [DOI] [PubMed]
- 18.Roberts JE, Halyabar O, Petty CR, Son MB. Assessing preparation for care transition among adolescents with rheumatologic disease: a single-center assessment with patient survey. Pediatr Rheumatol Online J. 2021 May 1;19(1):61. doi: 10.1186/s12969-021-00544-y. PMID: 33933123; PMCID: PMC8088202. [DOI] [PMC free article] [PubMed]
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42;2:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed]
- 20.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN, REDCap Consortium The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chang JC, Sears C, Bitencourt N, Peterson R, Alperin R, Goh YI, Overbury RS, Sadun R, Smitherman E, White PH, Lawson EF, Carandang K. CARRA Transition Workgroup. Implementation of rheumatology health care transition processes and adaptations to systems under stress: a mixed methods study. Arthritis Care Res (Hoboken). 2021 Nov 21. doi: 10.1002/acr.24822. Epub ahead of print. PMID: 34806346. [DOI] [PubMed]
- 22.Lawson EF, Hersh AO, Applebaum MA, Yelin EH, Okumura MJ, von Scheven E. Self-management skills in adolescents with chronic rheumatic disease: A cross-sectional survey. Pediatr Rheumatol Online J. 2011 Dec 6;9(1):35. doi: 10.1186/1546-0096-9-35. [DOI] [PMC free article] [PubMed]
- 23.Bingham CA, Scalzi L, Groh B, Boehmer S, Banks S. An assessment of variables affecting transition readiness in pediatric rheumatology patients. Pediatr Rheumatol Online J. 2015 Oct 13;13(1):42. doi: 10.1186/s12969-015-0040-x. [DOI] [PMC free article] [PubMed]
- 24.Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? Proc Natl Acad Sci U S A. 2002 Aug 6;99(16):10929-34. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request and pending approval of data sharing by the Boston Children’s Hospital IRB.