Abstract
Background
Patellar resurfacing is optional during total knee replacement (TKR). Some surgeons always resurface the patella, some never resurface, and others selectively resurface. Which resurfacing strategy provides optimal outcomes is unclear. We assessed the effectiveness of patellar resurfacing, no resurfacing, and selective resurfacing in primary TKR.
Methods
A systematic review and meta-analysis was performed. MEDLINE, Embase, Web of Science, The Cochrane Library, and bibliographies were searched to November 2021 for randomised-control trials (RCTs) comparing outcomes for two or more resurfacing strategies (resurfacing, no resurfacing, or selective resurfacing) in primary TKR. Observational studies were included if limited or no RCTs existed for resurfacing comparisons. Outcomes assessed were patient reported outcome measures (PROMs), complications, and further surgery. Study-specific relative risks [RR] were aggregated using random-effects models. Quality of the evidence was assessed using GRADE.
Results
We identified 33 RCTs involving 5,540 TKRs (2,727 = resurfacing, 2,772 = no resurfacing, 41 = selective resurfacing). One trial reported on selective resurfacing. Patellar resurfacing reduced anterior knee pain compared with no resurfacing (RR = 0.65 (95% CI = 0.44–0.96)); there were no significant differences in PROMs. Resurfacing reduced the risk of revision surgery (RR = 0.63, CI = 0.42–0.94) and other complications (RR = 0.54, CI = 0.39–0.74) compared with no resurfacing. Quality of evidence ranged from high to very low. Limited observational evidence (5 studies, TKRs = 215,419) suggested selective resurfacing increased the revision risk (RR = 1.14, CI = 1.05–1.22) compared with resurfacing. Compared with no resurfacing, selective resurfacing had a higher risk of pain (RR = 1.25, CI = 1.04–1.50) and lower risk of revision (RR = 0.92, CI = 0.85–0.99).
Conclusions
Level 1 evidence supports TKR with patellar resurfacing over no resurfacing. Resurfacing has a reduced risk of anterior knee pain, revision surgery, and complications, despite PROMs being comparable. High-quality RCTs involving selective resurfacing, the most common strategy in the UK and other countries, are needed given the limited observational data suggests selective resurfacing may not be effective over other strategies.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-022-05877-7.
Keywords: Primary total knee replacement, Patellar resurfacing, Selective resurfacing, No resurfacing, Outcomes, Meta-analysis
Introduction
Total knee replacement (TKR) is clinically and cost-effective for treating patients with painful arthritis [1, 2]. In the UK over 100,000 primary TKRs are performed annually [3, 4], with numbers rising [5]. Despite good TKR implant longevity [1–3], up to 34% of patients experience persistent pain [6], which can leave patients dissatisfied, with reduced mobility, and needing long-term analgesia [7]. Priority setting partnerships with patients and healthcare workers highlight chronic pain after TKR as an important area for future research [8, 9]. The reasons why many patients have pain after TKR remain unclear [10, 11], however it may relate to interventions performed during surgery.
When performing TKR, surgeons can retain the native patella, or resurface the patella (patellar resurfacing) using a polyethylene implant. Patellar resurfacing may be performed for a variety of indications including patient age, weight, patellar anatomy, the condition of the patella articular cartilage, presence of inflammatory arthritis, radiographic findings, and preoperative anterior knee pain [12, 13]. The National Joint Registry (NJR) recorded patellar resurfacing in 38% of 1,100,000 primary TKRs [3]. However rates vary substantially worldwide (USA 82% vs. Sweden 2%) [14].
Some surgeons always resurface the patella whilst others never do. Proponents of patellar resurfacing claim that if not resurfaced, 25% of patients develop chronic anterior knee pain with poor outcomes and dissatisfaction [15]. This adversely affects patient reported outcome measures (PROMs) and can lead to further surgery (secondary patellar resurfacing) in 7% [15]. Two-thirds of patients experience poor satisfaction after secondary patellar resurfacing [16, 17]. Opponents of patellar resurfacing propose that resurfacing is an unnecessary additional procedure given similar PROMs between those resurfaced and not [1]. Resurfacing also extends surgical time and increases the risk of intraoperative complications (e.g. patella fracture, tendon injury) [15].
The National Institute for Health and Care Excellence (NICE) guidance currently recommends always performing patellar resurfacing rather than not resurfacing [18]. However a third option exists (selective patellar resurfacing), where the surgeon decides case-by-case whether or not to resurface the patella based on their experience and intraoperative findings. Selective resurfacing could be a more effective strategy than always resurfacing, as it potentially preserves benefits from both approaches. Selective resurfacing may improve outcomes by only resurfacing patients whom surgeons judge are at higher risk of future pain if they were not resurfaced. Conversely by not resurfacing patients where the surgeon thinks resurfacing is not needed, or where there may be a high risk of complications, there are potential cost-savings from decreased theatre time and implants.
Limited evidence exists for selective patellar resurfacing with only one RCT published [19]. NICE were therefore unable to make recommendations about selective resurfacing; however NICE have recently recommended future RCTs comparing selective resurfacing with always resurfacing to define the role of selective resurfacing in TKR [18]. This is concerning, as a recent survey of 309 UK surgeons demonstrated the most common practice is selective patellar resurfacing (39%), followed by always resurfacing (37%), and no resurfacing (24%) [12]. Furthermore most selective patellar resurfacing surgeons (71%) resurface in less than 50% of TKRs [12], which is contrary to NICE recommendations [18]. Many countries, including Australia and New Zealand, also employ selective resurfacing in up to two-thirds of cases, for which there may be little supportive evidence [14, 20, 21]. However since NICE issued their guidance, 5 more RCTs have been published, and NICE did not consider observational evidence for selective resurfacing which is important given only 1 RCT exists involving selective resurfacing.
We performed a systematic review to determine the clinical effectiveness and complication risks of patellar resurfacing, no resurfacing, and selective resurfacing in primary TKR patients.
Methods
Data sources and search strategy
This review was registered with the prospective register of systematic reviews, PROSPERO (CRD42020182670) and conducted using PRISMA and MOOSE guidelines [22, 23]. (Supplementary Materials 1–2) We performed electronic searches of MEDLINE, Embase, Web of Science and Cochrane Library databases from inception to 06 November 2021 to identify studies comparing at least two of the three possible patellar resurfacing options in primary TKR patients; resurfacing, no resurfacing, or selective resurfacing. The computer-based searches combined free and MeSH search terms and key words related to the population (e.g., “total knee replacement”), intervention (e.g., “resurfacing”) and outcomes (e.g., “revision rate”). There were no language restrictions. Full details of the search strategy are reported (Supplementary Material 3).
Titles and abstracts of retrieved studies were initially screened to assess their suitability for inclusion by two independent reviewers (MJG and MCB). Full text evaluations of potentially relevant articles meeting the selection criteria were performed by the same two independent reviewers. Any disagreements regarding eligibility of a study were discussed, and if needed consensus was reached with a third author (SKK). Reference lists of identified studies and relevant review articles were scanned manually and the “Cited Reference Search” function in Web of Science was used to check for additional eligible studies.
Study eligibility criteria
Studies were included in our analyses if they were RCTs that compared any two or more of the following patellar resurfacing strategies (patellar resurfacing, no resurfacing, or selective resurfacing) in adult patients (18 years and above) undergoing primary TKR with at least one outcome of interest reported. If limited or no RCTs were available for a comparison, we included observational studies (prospective or retrospective). This was decided a priori as it was suspected limited RCTs would be available for the selective resurfacing arm given the evidence supporting national recommendations [18].
Outcomes evaluated were postoperative PROMs (e.g. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Knee Society Score (KSS), range of movement (ROM), Knee Injury and Osteoarthritis Outcome Score (KOOS), Hospital for Special Surgery (HSS), Oxford Knee Score, Feller’s Patellar Score) and rates of postoperative complications, revision surgery and any reoperation. We excluded the following studies: (i) those restricted to selected patients such as those with prevalent conditions like diabetes or selected populations with no comparison or control groups; (ii) observational studies investigating patellar resurfacing vs. no resurfacing without a selective resurfacing arm; and (iii) studies of any surgery other than primary TKR (such as revision surgery or unicompartmental knee replacement). No limits were placed on study follow-up duration.
Data extraction, risk of bias and methodological quality assessment
One author (MCB) initially extracted data from eligible studies using a standardised predesigned data collection form. Two reviewers (MJG and SKK) independently checked these data with those in the original articles. We extracted data on study characteristics, sample size, preoperative and postoperative PROMs, and counts of outcomes of interest for the intervention and comparator(s) where relevant. When further information was required from a study, we attempted to contact the corresponding authors. When multiple publications involving the same cohort existed, we used the most complete study with the longest follow-up and/or analysis covering the largest number of participants. The Cochrane Collaboration’s risk of bias tool was used to assess the risk of bias of included RCTs [24]. This tool evaluates seven possible sources of bias, which are random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias. For each individual component, studies were classified into low, unclear and high risk of bias. The methodological quality of each observational study was assessed using the nine-star Newcastle–Ottawa Scale (NOS) [25], which uses three pre-defined domains including: (i) selection of participants; (ii) comparability; and (iii) ascertainment of outcomes of interest. To grade the quality of evidence across outcomes, we used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool, a widely adopted reproducible and transparent framework for grading certainty in evidence [26]. GRADE considers the following criteria: study limitations, inconsistency of effect, imprecision, indirectness, and publication bias, and has four levels of evidence: very low, low, moderate, and high.
Statistical analyses
Summary measures were presented as relative risks [RR] with 95% confidence intervals (CIs) for binary outcomes, and mean differences (95% CIs) for continuous outcomes. RRs were calculated from the extracted raw counts for the intervention and comparator. For continuous data, if the mean or standard deviation (SD) was not reported, we estimated the mean and variance from the reported median, range and sample size using methods proposed by Hozo and colleagues [27]. Given the heterogeneous follow-up periods reported by included studies, risk estimates for the longest follow-up of each study were used for the outcomes. The inverse variance weighted method was used to combine summary measures using random-effects models. Parallel analyses utilised fixed effects models. Statistical heterogeneity across studies was quantified using the Cochrane χ2 statistic and the I2statistic. Pre-specified study-level characteristics such as geographical location, study year, mean age at baseline, mean follow-up duration and sample size were explored as sources of heterogeneity, using stratified analysis and meta-regression [28]. STATA release MP 16 (StataCorp LP, College Station, TX, USA) was used for all statistical analyses.
Results
Study identification and selection
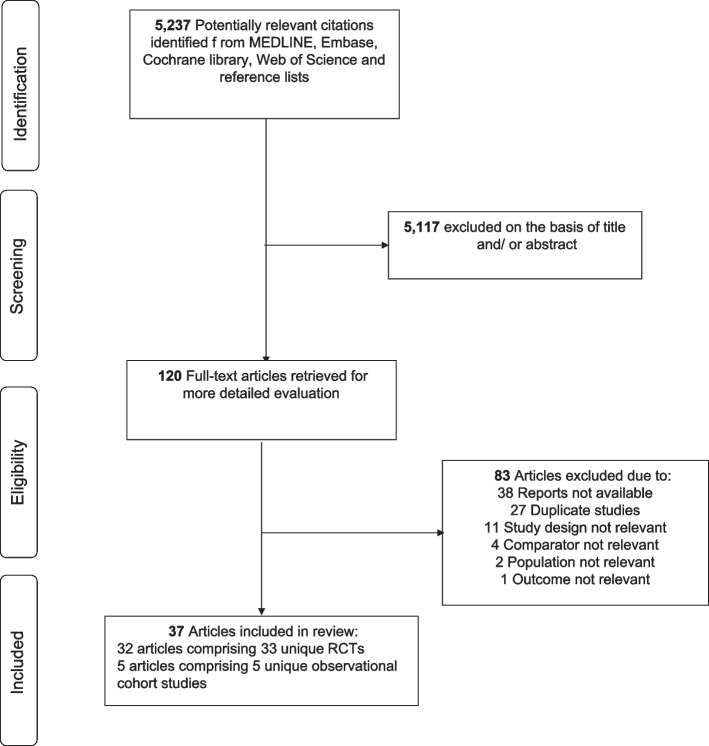
A total of 5,237 potential citations were identified from the initial search. Of these, 120 potential articles were selected for full text evaluation after screening the titles and abstracts. Following detailed evaluation of full texts, 83 citations were excluded. The remaining 37 articles comprising of 38 unique studies were eligible (Fig. 1; Supplementary Material 4). In total, there were 33 individual RCTs (based on 32 articles) that compared patellar resurfacing vs. no patellar resurfacing [1, 19, 29–58]. One trial had three arms (resurfacing vs. no resurfacing vs. selective resurfacing) [19]. We identified 5 unique observational studies that compared selective resurfacing with no resurfacing or patellar resurfacing [20, 21, 59–61].
Fig. 1.
PRISMA flow diagram. RCT, randomised controlled trials
Study characteristics, risk of bias and methodological quality
The included studies were published from 1995 to 2021, with baseline characteristics of the individual RCTs summarised in Table 1. The 33 RCTs involved 5,540 primary TKRs (2,727 = resurfacing, 2,772 = no resurfacing, 41 = selective resurfacing). Overall, 14 studies [1, 19, 29–39] were conducted in Europe (Finland, France, Germany, Italy, the Netherlands, Norway, Serbia, Sweden and United Kingdom), 10 in Asia (China, India, Iran, Japan, South Korea and Thailand) [40–49], 5 in North America (Canada and USA) [50–54] and 4 in Australasia (Australia) [55–58] The mean baseline age of participants in the included studies ranged from 56.1 to 74.1 years with a weighted mean of 69.4 years. The mean follow-up periods in the trials ranged from 0.5 to 10 years with a weighted mean of 6.3 years. Using the Cochrane Risk of Bias tool, 11 trials demonstrated a low risk of bias in all domains [30, 34, 39, 42, 48, 51–54, 57, 58]. Five trials demonstrated a high risk of bias in one or more domains [1, 31, 38, 40, 45]. Except for 6 trials [31, 32, 35, 41, 47, 50], all trials demonstrated a low risk of bias in random sequence generation (Supplementary Material 5). Baseline characteristics of the observational studies are summarised in Supplementary Material 6. The 5 observational studies [20, 21, 59–61] included 4 retrospective cohort designs [20, 21, 59, 61] and 1 prospective cohort design [60], comprising a total of 215,419 primary TKRs. Studies were conducted in Australia, New Zealand, Korea, United Kingdom and USA. The mean baseline age of participants ranged from 64.3 to 68.7 years with mean follow-up periods ranging from 4.5 to 10.0 years. The NOS score ranged from 7 to 9 (Supplementary Material 7).
Table 1.
Baseline characteristics of randomised controlled trials
| Author, year of publication | Location | Baseline year of study | Population | Mean/median age (years) | % Males | Mean follow-up duration (years) | Implant design | Interventions evaluated |
No. of participants/ joint replacements |
|---|---|---|---|---|---|---|---|---|---|
| Partio, 1995 [38] | Finland | 1991–1992 | Osteoarthritis/Rheumatoid arthritis | 67.5 | 22.0 | 3.0 | Johnson & Johnson Press-fit condylar implant | Resurfacing/ No resurfacing | 95 |
| Feller, 1996 [56] | Australia | 1990–1991 | Osteoarthritis (not otherwise specified) | 70.8 | 55.3 | 3.0 | Howmedica PCA Modular prosthesis | Resurfacing/ No resurfacing | 38 |
| Kajino, 1997 [45] | Japan | NR | Rheumatoid arthritis | 56.1 | 7.7 | 6.6 | Yoshino-Shoji total knee prosthesis; Biomet, Warsaw, Indiana | Resurfacing/ No resurfacing | 52 |
| Schroeder-Boersch, 1998 [35] | Germany | NR | Primary osteoarthritis | 72.6 | 30.0 | 2.0 | Howmedica Duracon | Resurfacing/ No resurfacing | 40 |
| Newman, 2000 [19] | United Kingdom | 1992–1997 | Primary osteoarthritis | 71.9 | 32.8 | 5.0 | Howmedica PCA Modular prosthesis | Resurfacing/ No resurfacing/ Selective resurfacing | 105 |
| Wood, 2002 [58] | Australia | 1992–1996 | Non-inflammatory arthritis | 73.7 | 52.7 | 4.0 | Zimmer Miller-Galante II | Resurfacing/ No resurfacing | 201 |
| Mayman, 2003 [50] | Canada | 1991 | Osteoarthritis | 70.0 | 42.0 | 10.0 | Anatomic Medullary Knee, DePuy, Warsaw, IN | Resurfacing/ No resurfacing | 100 |
| Waters, 2003 [37] | United Kingdom | 1992- | Osteoarthritis/inflammatory arthritis | 69.1 | 40.2 | 5.3 | Johnson & Johnson Press-fit condylar implant | Resurfacing/ No resurfacing | 390 |
| Burnett, 2004 [13, 51] | Canada | 1991- | Osteoarthritis (not otherwise specified) | 70 | 43.3 | 10.0 | DePuy Anatomic Medullary Knee | Resurfacing/ No resurfacing | 83 |
| Gildone, 2005 [32] | Italy | 2002–2004 | Primary osteoarthritis | 74.1 | 30.4 | 2.1 | Zimmer Nexgen | Resurfacing/ No resurfacing | 56 |
| Campbell, 2006 [55] | Australia | 1991–1993 | Primary osteoarthritis | 72.1 | 28.0 | 10.0 | Zimmer Miller-Galante II | Resurfacing/ No resurfacing | 100 |
| Myles, 2006 [34] | United Kingdom | NR | Non-inflammatory arthritis | 70 | 52.0 | 1.8 | DePuy LCS rotating platform | Resurfacing/ No resurfacing | 50 |
| Smith, 2008 [57] | Australia | 1998–2002 | Primary osteoarthritis | 71.5 | 50.4 | 4.0 | Smith & Nephew PROFIX | Resurfacing/ No resurfacing | 164 |
| Burnett, 2009 [52] | USA | 1992–1993 | Degenerative osteoarthrosis | 66.2 | 79.1 | 10.0 | Zimmer Miller-Galante II | Resurfacing/ No resurfacing | 86 |
| Beaupre, 2012 [53] | Canada | 1996–1999 | Non-inflammatory arthritis | 63.6 | 31.6 | 10.0 | Profix™ Total Knee System | Resurfacing/ No resurfacing | 38 |
| Liu, 2012 [46] | China | 2000–2002 | Osteoarthritis | 67.7 | 62.9 | 7.0 | Press Fit Condylar, DePuy, Warsaw, IN | Resurfacing/ No resurfacing | 144 |
| Ferguson, 2014 [33] (Fixed bearing) | United Kingdom | NR | Osteoarthritis (not otherwise specified) | 69.8 | 47.0 | 2.0 | PFC Sigma© Posterior Stabilised, DePuy, Warsaw, IN | Resurfacing/ No resurfacing | 176 |
| Ferguson, 2014 [33] (Mobile Bearing) | United Kingdom | NR | Osteoarthritis (not otherwise specified) | 70.2 | 47.0 | 2.0 | PFC Sigma© Posterior Stabilised, DePuy, Warsaw, IN | Resurfacing/ No resurfacing | 176 |
| Murray, 2014 [1] | United Kingdom | 1999–2003 | Osteoarthritis/Rheumatoid arthritis | 70 | 44.3 | 10.0 | NR | Resurfacing/ No resurfacing | 1715 |
| Roberts, 2015 [54] | USA | 1996–2001 | Primary osteoarthritis | 70.7 | 48.6 | 7.8 | DePuy Sigma CR | Resurfacing/ No resurfacing | 114 |
| Aunan, 2016 [30] | Norway | 2007–2011 | Primary osteoarthritis | 69.5 | 43.4 | 3.0 | Zimmer Nexgen | Resurfacing/ No resurfacing | 129 |
| Ali, 2016 [29] | Sweden | 2008–2009 | Primary osteoarthritis | 68.5 | 39.2 | 6.0 | Triathlon CR | Resurfacing/ No resurfacing | 74 |
| Vukadin, 2017 [36] | Serbia | NR | Osteoarthrosis/Valgus deformity | 67.4 | 45.0 | 2.0 | Zimmer Nexgen LPS-type | Resurfacing/ No resurfacing | 60 |
| Dong, 2018 [47] | China | 2013–2015 | Late-stage osteoarthritis | 67.7 | 43.0 | 3.0 | Posterior cruciate stabilizing total knee prostheses | Resurfacing/ No resurfacing | 106 |
| Jia, 2018 [43] | China | 2013–2015 | Bilateral knee osteoarthritis | 57.2 | 80.0 | 2.6 | NR | Resurfacing/ No resurfacing | 30 |
| Kaseb, 2018 [40] | Iran | 2012–2013 | Non-inflammatory arthritis | 64.8 | 16.0 | 0.5 | Profix™ Total Knee System | Resurfacing/ No resurfacing | 50 |
| Ha, 2019 [42] | China | 2011–2017 | Bilateral knee osteoarthritis | 65.2 | 63.3 | 5.5 | Stryker Scorpio NRG | Resurfacing/ No resurfacing | 120 |
| Chawla, 2019 [49] | India | 2011–2013 | Osteoarthritis (not specified) | NR | 20.0 | 5.0 | NR | Resurfacing/ No resurfacing | 100 |
| Kaseb, 2019 [41] | Iran | 2014–2017 | Primary osteoarthritis | 66.7 | 20.5 | 0.7 | Zimmer Nexgen | Resurfacing/ No resurfacing | 73 |
| Thiengwittayaporn, 2019 [48] | Thailand | NR | Osteoarthritis (not otherwise specified) | 68.2 | 17.5 | 1.3 | Smith & Nephew Legion PS Total Knee System | Resurfacing/ No resurfacing | 84 |
| Koh, 2019 [44] | Korea | 2012–2013 | Primary Osteoarthritis | 70.0 | NR | 5.0 | NR | Resurfacing/ No resurfacing | 98 |
| van Raaij, 2021 [39] | Netherlands | 2012–2015 | Tricompartmental osteoarthritis | 69.5 | 38.1 | 2.0 | AGC Total Knee System, Biomet, Warsaw, IN | Resurfacing/ No resurfacing | 40 |
| Deroche, 2022 [31] | France | 2017–2018 | Medial femorotibial osteoarthritis | 69.3 | 58.1 | 1.5 | Anatomic, AMPLITUDE®, Valence 26,000, FRANCE | Resurfacing/ No resurfacing | 250 |
NR Not reported
Patellar resurfacing vs. no resurfacing
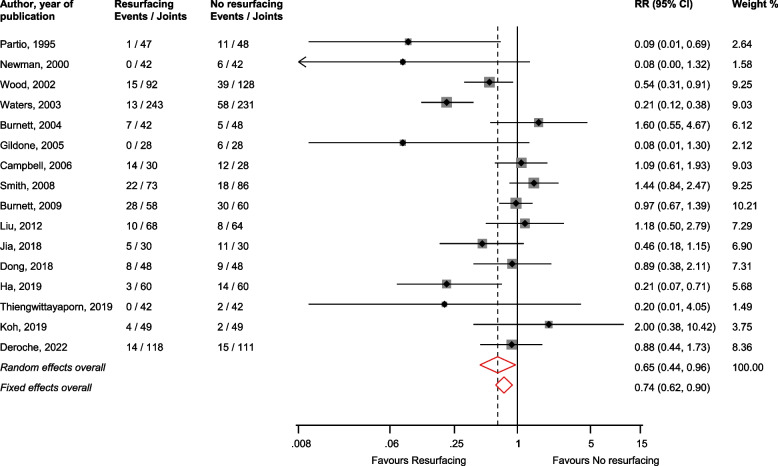
Anterior knee pain
In pooled analysis of 16 studies [19, 31, 32, 37, 38, 42–44, 46–48, 51, 52, 55, 57, 58], patellar resurfacing reduced the risk of anterior knee pain compared with no resurfacing: RR (CI) = 0.65 (0.44–0.96; I2 = 70%; CI = 50–82%; p for heterogeneity < 0.01) (Fig. 2). In subgroup analyses, none of the study-level characteristics explored explained the substantial heterogeneity between studies (Supplementary Material 8).
Fig. 2.
Risk of anterior knee pain comparing patellar resurfacing with no resurfacing. CI, confidence interval (bars); RR, relative risk
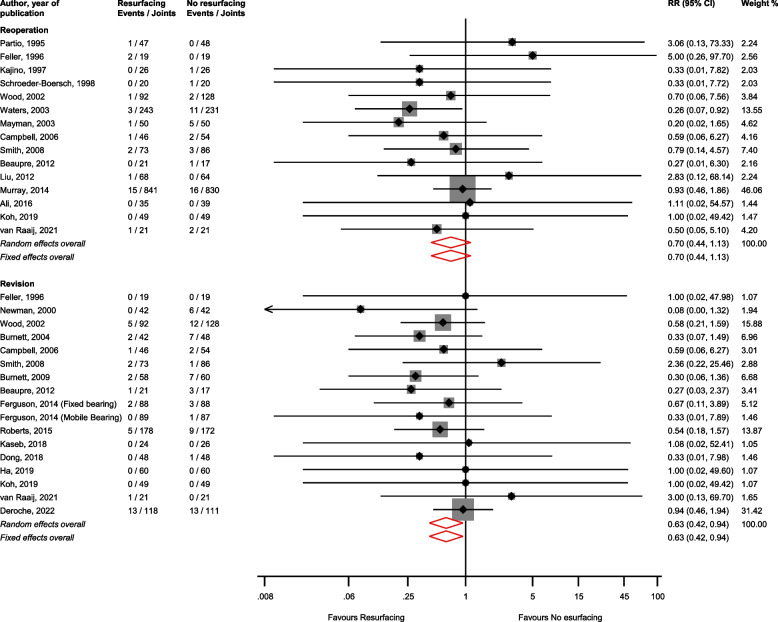
Reoperations and revisions
There was no significant difference in the risk of reoperation (15 studies) [1, 29, 35, 37–39, 44–46, 50, 53, 55–58] comparing patellar resurfacing vs. no resurfacing: RR (CIs) = 0.70 (0.44–1.13; I2 = 0%; CI = 0–54%; p for heterogeneity = 0.87); however patellar resurfacing reduced the risk of revision (17 studies) [19, 31, 33, 39, 40, 42, 44, 47, 51–58]: RR (CIs) = 0.63 (0.42–0.94; I2 = 0%; CI = 0–51%; p for heterogeneity = 0.95) (Fig. 3).
Fig. 3.
Risk of reoperation and revision comparing patellar resurfacing with no resurfacing. CI, confidence interval (bars); RR, relative risk
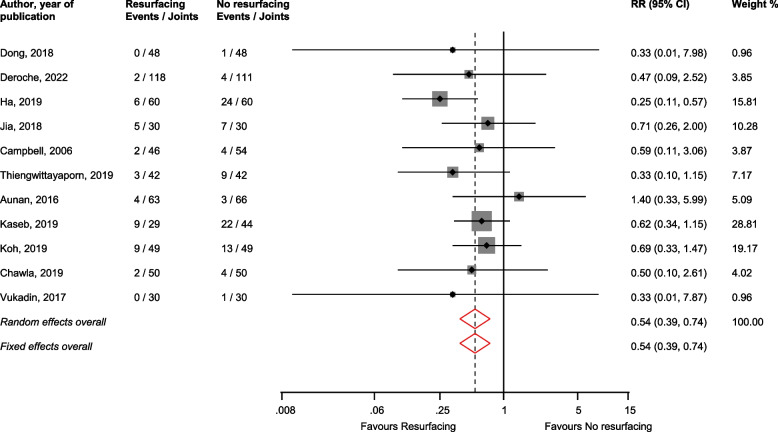
Other complications
In pooled analysis of 11 studies [30, 31, 36, 41–44, 47–49, 55], patellar resurfacing reduced the risk of other complications (e.g. patellar dislocation, crepitus, clunk syndrome) compared with no resurfacing: RR (CIs) = 0.54 (0.39–0.74; I2 = 0%; CI = 0–60%; p for heterogeneity = 0.75) (Fig. 4).
Fig. 4.
Risk of other complications comparing patellar resurfacing with no resurfacing. CI, confidence interval (bars); RR, relative risk
Function
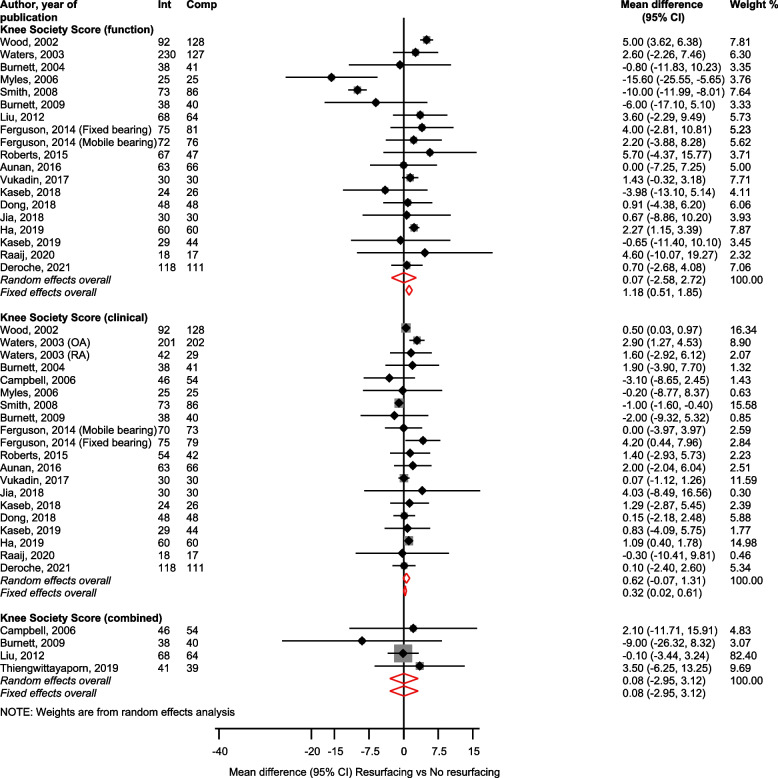
KSS
KSS Function (19 studies) [30, 31, 33, 34, 36, 37, 39–43, 46, 47, 51, 52, 54, 57, 58], Clinical (20 studies) [30, 31, 33, 34, 36, 37, 39–43, 47, 51, 52, 54, 55, 57, 58], and Combined (4 studies) [46, 48, 52, 55] scores showed no statistically significant differences for patellar resurfacing vs. no resurfacing; mean differences (CIs) of 0.07 (-2.58–2.72), 0.62 (-0.07–1.31) and 0.08 (-2.95–3.12), respectively (Fig. 5).
Fig. 5.
Patellar resurfacing versus no resurfacing and Knee Society Scores. CI, confidence interval (bars); Int, resurfacing; Comp, no resurfacing
KOOS
There were no statistically significant differences in KOOS subscales for symptoms (3 studies) [29, 30, 39], activities of daily living (ADL) (3 studies) [29, 30, 39], and Sport/recreation (3 studies) [29, 30, 39] between patellar resurfacing and no resurfacing: mean differences (CIs) of 1.72 (-1.84–5.27), 0.60 (-5.13–6.33) and 0.27 (-12.25–12.80) respectively (Supplementary Material 9). Results from a single report [41] showed no significant difference in KOOS combined score between the two intervention groups (Supplementary Material 9).
ROM
In pooled analysis of 7 studies [31, 33, 48, 51, 52, 54], there was no statistically significant difference in ROM comparing patellar resurfacing with no resurfacing: mean difference (CI) = -0.22 (-1.84–1.39) (Supplementary Material 10).
Other measures of function
There were no statistically significant differences between patellar resurfacing and no resurfacing for other measures of function such as patellar score (2 studies) [48, 56], Oxford Knee Score (6 studies) [1, 30, 33, 36, 48], and Feller’s Patellar Score (3 studies) [42, 44, 47]: mean differences (CIs) of 0.26 (-3.56–3.04), 1.09 (-0.30–2.48) and 0.66 (-1.13–2.45), respectively (Supplementary Material 11). Results from single reports [34, 39, 40, 56] showed no statistically significant differences in HSS Knee Score; WOMAC physical function, stiffness and combined scores; and Baldini score between the two intervention groups (Supplementary Material 11).
Pain
There were no statistically significant differences between patellar resurfacing and no resurfacing for measures of pain such as KSS pain score (2 studies) [46, 51], Visual Analogue Scale (VAS) pain (4 studies) [29, 30, 34, 36], and KOOS pain (3 studies) [29, 30, 39]: mean differences (CIs) of 1.03 (-1.14–3.21), -0.20 (-0.45–0.06) and 0.96 (-5.72–7.64), respectively (Supplementary Material 12). Results from single reports [34, 40, 57] showed no significant differences in WOMAC pain, Knee Pain Scale, VAS Pain Score and Anterior Knee Pain Score (Supplementary Material 12).
Health status, satisfaction and quality of life
Measures of health status and quality of life were mostly based on single reports [1, 29, 30, 33, 39, 40], which showed no statistically significant differences between patellar resurfacing and no resurfacing (Supplementary Material 13). In pooled analysis of 10 studies that reported the number of patients satisfied with their procedure [29, 37, 42, 44, 46, 47, 50–52, 57], there was no significant difference between patellar resurfacing and no resurfacing: RR (CIs) = 1.00 (0.94–1.08; I2 = 57%; CI = 14–79%; p for heterogeneity = 0.01) (Supplementary Material 14).
Publication bias
Funnel plots for risk of anterior knee pain, reoperation, revision, other complications and overall satisfaction comparing patellar resurfacing with no resurfacing which involved 10 or more studies were symmetrical on visual inspection, implying little evidence of small study effects or publication bias (Supplementary Material 15). These were consistent with Egger’s regression tests (p-values of 0.16, 0.94, 0.57, 0.81 and 0.24, respectively).
Selective resurfacing
Only one RCT evaluated outcomes of selective resurfacing, which was compared with patellar resurfacing and no resurfacing [19]. At five-year follow-up, the no resurfacing group required more reoperations (14%) than the patellar resurfacing (0%) and selective resurfacing (2%) groups. These findings were statistically significant. Using the mean Bristol Knee Score, there were little differences between the three groups.
In observational studies, there was no statistically significant difference in the risk of complications (2 studies) [20, 59] comparing selective resurfacing with no resurfacing: RR (CIs) = 1.06 (0.92–1.22). Selective resurfacing reduced the risk of revision (4 studies) [20, 21, 59, 61] and increased the risk of pain (2 studies) [20, 60] compared with no resurfacing: RRs (CIs) of 0.92 (0.85–0.99) and 1.25 (1.04–1.50), respectively (Supplementary Material 16).
In pooled analysis of two observational studies [20, 21], selective resurfacing was associated with an increased risk of revision compared with patellar resurfacing: RR (CIs) = 1.14 (1.05–1.22) (Supplementary Material 17). Results from one report [20] showed an increased risk of complications and pain with selective resurfacing over patellar resurfacing (Supplementary Material 17).
Measures of function and pain
Improved HSS Knee score (2 studies) [60, 61] and function score (2 studies) [60, 61] were seen with selective resurfacing compared with no resurfacing, with a decrease in the ROM (2 studies) [60, 61]: mean differences (CIs) of 3.47 (2.29–4.65), 1.99 (0.78–3.19) and -2.57 (-4.67,-0.47), respectively (Supplementary Material 18). Results from single reports [20, 60] showed no significant difference in pain score, but a significant improvement in the Oxford Knee Score comparing selective resurfacing vs. no resurfacing (Supplementary Material 18).
GRADE summary of findings
The GRADE working group recommends up to 7 patient-important outcomes to be listed in the “summary of findings” tables in systematic reviews. Given that all the outcomes assessed were important, we selected the outcomes based on their frequency of reporting. GRADE ratings for the outcomes of anterior knee pain, reoperation, revision, KSS Function, KSS Clinical, ROM and overall satisfaction comparing patellar resurfacing vs. no resurfacing are reported in Supplementary Material 19. GRADE quality of the evidence ranged from high to very low.
Discussion
Whether or not to perform patellar resurfacing during primary TKR is controversial, with advantages and disadvantages recognised for each approach [15]. Our systematic review has demonstrated that many trials exist comparing resurfacing with no resurfacing (33 RCTs involving 5,499 primary TKRs). These show that patellar resurfacing is associated with a reduced risk of anterior knee pain, revision surgery, and complications, although PROMs are similar between both strategies. The quality of the evidence ranged from high to very low. Level 1 evidence for selective resurfacing is lacking with only one small RCT available from over 20 years ago, but selective resurfacing is the most common strategy used by UK surgeons and in many other countries [12, 14, 20, 21]. Findings from the limited observational data were mostly inconsistent. Selective resurfacing decreased revision rates when compared with no resurfacing, although revision rates for selective resurfacing were increased when compared with patellar resurfacing. Selective resurfacing increased the risk of pain when compared with each of the other resurfacing strategies.
Although there is no clinical benefit in terms of PROMs between patellar resurfacing and no resurfacing, the higher risk of revision with no resurfacing is concerning, especially as outcomes after revision are much less favourable than primary TKR [62, 63]. Many revisions are performed for anterior knee pain, which is more prevalent in those TKRs not resurfaced initially [16, 17]. A recent NJR study of 842,072 primary TKRs highlighted the scale of the problem, with a significantly increased risk of all-cause revision at ten-years with no resurfacing compared with resurfacing; this equated to 2,842 excess revision procedures compared with if all TKRs underwent resurfacing initially [62]. The largest RCT identified (n= 1,715) recruited from 34 UK centres with 10 years follow-up and showed no significant differences in PROMs between groups [1]. However, patellar resurfacing was estimated to be very probably cost-effective. Always resurfacing resulted in more QALYs and was cheaper overall, as the incremental costs of resurfacing during the initial TKR admission were outweighed by the costs of complications and further surgery associated with needing to resurface some of the no resurfacing group in the future. Therefore NICE currently recommend patellar resurfacing over no resurfacing [18]. Previous trials and recommendations [1, 3, 18] are gradually changing clinical practice in the UK with 43% of TKRs undergoing patellar resurfacing in 2019 compared to 36% in 2011 [64].
A recent survey of UK knee surgeons identified selective patellar resurfacing as the most common strategy for primary TKR [12]. Deciding whether or not to resurface the patella is multifactorial, with surgeons stating the twelve commonest reasons for this being the condition of the patella articular cartilage (61%), presence of inflammatory arthritis (53%), native patella thickness (49%), preoperative anterior knee pain (47%), the risk of future secondary patellar resurfacing (43%), how the native patella moves/tracks during surgery (40%), the risk of postoperative anterior knee pain (38%), patient age (26%), the risk of patella fracture/extensor mechanism failure postoperatively (23%), level of TKR constraint used (22%), brand of TKR (20%), and the risk of needing revision secondary to patellar component loosening/failure (11%) [12]. In addition to the above indications, other studies have also cited indications for selective patellar resurfacing to include patient gender, weight and patella anatomy [13]. However our work demonstrated that little evidence is available to support selective patellar resurfacing. Only one small RCT from 20 years ago exists, which randomised 125 patients to resurfacing, no resurfacing or selective resurfacing [19]. The no resurfacing group required more reoperations at five-years compared with the other two groups [19]. NICE could not make any recommendations about selective resurfacing as there was only one RCT available [19]. However our updated review confirmed none of the five RCTs published since the NICE guidelines included a selective resurfacing arm. It was therefore important to consider the observational evidence available, given this is the only data that can help inform clinical decision-making, although it is recognised that such evidence is weaker compared to RCTs. The five observational studies we included suggested that currently selective resurfacing appears to have little clinical benefit over the other resurfacing strategies used. This is an important clinical concern as aside from the UK, selective patellar resurfacing is the most commonly used approach for primary TKR in many other countries worldwide including Australia, New Zealand and Denmark [14, 20, 21]. Therefore many TKR patients worldwide may be at unnecessary risk by receiving selective patellar resurfacing.
As life expectancy increases, the growing burden of osteoarthritis is expected to proportionally increase and there will continue to be increasing demand for primary TKR. This will be compounded by substantial delays in elective operating for the last two-years due to COVID-19. Many patients have suboptimal outcomes following TKR and their continued pain and need for further surgery may relate to the choices made about their patella during TKR surgery. Our findings confirm that there is plenty of level 1 evidence supporting patella resurfacing over no resurfacing. We suggest that no further trials are needed comparing these two treatment options. However, there is a lack of interventional evidence available for selective resurfacing. The current observational data shows selective resurfacing has an increased revision risk compared with resurfacing, and a higher risk of pain compared with no resurfacing. This is clinically concerning as presently there is a lack of evidence to suggest that selective resurfacing has clinical benefits over other strategies, and it is possible that selective resurfacing may actually lead to harm.
Strengths and limitations
Based on evidence from 33 RCTs and 5 observational cohort studies, our review represents an up-to-date comprehensive meta-analysis evaluating the effectiveness of all three resurfacing options in primary TKR. Detailed assessments of methodological quality of observational studies and the risk of bias of RCTs were conducted using robust validated tools. We also evaluated a comprehensive list of outcomes. Though the limitations were mostly inherent to the studies, they include: (i) a significant degree of heterogeneity among some pooled comparisons, (ii) risk estimates for the longest follow-up of each study were pooled because of the varied follow-up periods across studies; however, where there was relevant and adequate data available, we conducted subgroup analysis by the follow-up duration, and (iii) findings on selective resurfacing were largely based on observational cohorts which are methodological weaker (as there was only one small old RCT available which included patients having selective resurfacing), with those observational cohorts limited by residual confounding, regression dilution bias, reverse causation, and inability to establish causation.
Conclusions
Our systematic review has demonstrated level 1 evidence supports primary TKR with patellar resurfacing over no resurfacing, as resurfacing is associated with a reduced risk of anterior knee pain, revision surgery, and complications; however, PROMs are similar between resurfacing and no resurfacing groups. Although selective resurfacing is the most common strategy currently used by UK surgeons and in many other countries, there is very little published research evidence available to support this approach. We recommend large high-quality RCTs involving selective patellar resurfacing and always resurfacing to establish the role of selective resurfacing, as limited observational data suggests selective resurfacing may not have clinical benefits over other strategies.
Supplementary Information
Additional file 1: Supplementary Material 1: PRISMA checklist. Supplementary Material 2. MOOSE checklist. Supplementary Material 3. Literature search strategy. Supplementary Material 4. Reference list of studies. Supplementary Material 5. Risk of bias assessment for randomised controlled trials. Supplementary Material 6. Baseline characteristics of observational studies. Supplementary Material 7. NOS scores for observational studies. Supplementary Material 8. Risk of anterior knee pain comparing patellar resurfacing with no resurfacing, by study-level characteristics. Supplementary Material 9. Patellar resurfacing versus no resurfacing and KOOS scale. Supplementary Material 10. Patellar resurfacing versus no resurfacing and range of movement. Supplementary Material 11. Patellar resurfacing versus no resurfacing and other measures of function. Supplementary Material 12. Patellar resurfacing versus no resurfacing and measures of pain. Supplementary Material 13. Patellar resurfacing versus no resurfacing and measures of health status, satisfaction, and quality of life. Supplementary Material 14. Patellar resurfacing versus no resurfacing and overall satisfaction. Supplementary Material 15. Funnel plots for risk of anterior knee pain, reoperations and revisions. Supplementary Material 16. Risk of revision, complications and pain comparing selective resurfacing with no resurfacing in observational cohort studies. Supplementary Material 17. Risk of revision, complications and pain comparing selective resurfacing with resurfacing in observational cohort studies. Supplementary Material 18. Selective resurfacing versus non-resurfacing and measures of function and pain in observational cohort studies. Supplementary Material 19. GRADE summary of findings.
Acknowledgements
This study was supported by the NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health.
Abbreviations
- CI
Confidence intervals
- OKS
Oxford Knee Score
- PROMS
Patient reported outcome measures
- RCT
Randomised-control trial
- RR
Relative risk
- TKR
Total knee replacement
Authors’ contributions
SKK, AWB, MRW and GSM conceived and designed the study. MG, MB, and SKK acquired the data. MG, MB, SKK, and GSM analysed and interpreted the data. MG, MB, SKK, and GSM drafted the manuscript. All authors critically revised the manuscript for important intellectual content. GSM is the guarantor for the study. The author(s) read and approved the final manuscript.
Funding
No funding was received for this study. SKK, AWB, and MRW are supported by the NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available in a dedicated repository because the data extracted and analysed for this study is freely available by accessing the individual articles referenced in this publication. However the datasets may be available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not required as systematic review of published literature.
Consent for publication
Not applicable.
Competing interests
We declare no competing interests for any author.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murray DW, MacLennan GS, Breeman S, Dakin HA, Johnston L, Campbell MK, Gray AM, Fiddian N, Fitzpatrick R, Morris RW, Grant AM, group KAT A randomised controlled trial of the clinical effectiveness and cost-effectiveness of different knee prostheses: the knee arthroplasty trial (KAT) Health Technol Assess. 2014;18(19):1–235. doi: 10.3310/hta18190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393(10172):655–663. doi: 10.1016/S0140-6736(18)32531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Joint Registry (NJR) for England, Wales, Northern Ireland and the Isle of Man 17th Annual Report. 2020. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2017th%20Annual%20Report%202020.pdf.
- 4.The Scottish Arthroplasty Project Report 2019.https://www.arthro.scot.nhs.uk/Reports/Main.html.
- 5.Culliford D, Maskell J, Judge A, Cooper C, Prieto-Alhambra D, Arden NK, Group COS Future projections of total hip and knee arthroplasty in the UK: results from the UK clinical practice research datalink. Osteoarthritis Cartilage. 2015;23(4):594–600. doi: 10.1016/j.joca.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 6.Blom AW, Artz N, Beswick AD, Burston A, Dieppe P, Elvers KT, Gooberman-Hill R, Horwood J, Jepson P, Johnson E, Lenguerrand E, Marques E, Noble S, Pyke M, Sackley C, Sands G, Sayers A, Wells V, Wylde V. Improving patients' experience and outcome of total joint replacement: the RESTORE programme. Programme Grants for Applied Research. Southampton (UK). 2016. [PubMed]
- 7.Williams DP, Blakey CM, Hadfield SG, Murray DW, Price AJ, Field RE. Long-term trends in the Oxford knee score following total knee replacement. Bone Joint J. 2013;95-B(1):45–51. doi: 10.1302/0301-620X.95B1.28573. [DOI] [PubMed] [Google Scholar]
- 8.James Lind Alliance Priority Setting Partnerships . Hip & Knee Replacement for Osteoarthritis Top 10. 2014. [Google Scholar]
- 9.Mathews JA, Kalson NS, Tarrant PM, Toms AD. Revision knee replacement priority setting partnership steering group. top ten research priorities for problematic knee arthroplasty. Bone Joint J. 2020;102-B(9):1176–1182. doi: 10.1302/0301-620X.102B9.BJJ-2020-0203.R1. [DOI] [PubMed] [Google Scholar]
- 10.Scott CE, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010;92(9):1253–1258. doi: 10.1302/0301-620X.92B9.24394. [DOI] [PubMed] [Google Scholar]
- 11.Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ. Three groups of dissatisfied patients exist after total knee arthroplasty: early, persistent, and late. Bone Joint J. 2018;100-B(2):161–169. doi: 10.1302/0301-620X.100B2.BJJ-2017-1016.R1. [DOI] [PubMed] [Google Scholar]
- 12.Matharu GS, Blom AW, Venkatesh R, Metcalfe AJ, Whitehouse MR. Patellar resurfacing practices in primary total knee replacement: a survey of BASK members. Knee. 2020.10.1016/j.knee.2020.1011.1014.
- 13.Burnett RS, Bourne RB. Indications for patellar resurfacing in total knee arthroplasty. Instr Course Lect. 2004;53:167–186. [PubMed] [Google Scholar]
- 14.Fraser JF, Spangehl MJ. International rates of patellar resurfacing in primary total knee arthroplasty, 2004–2014. J Arthroplasty. 2017;32(1):83–86. doi: 10.1016/j.arth.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 15.Longo UG, Ciuffreda M, Mannering N, D'Andrea V, Cimmino M, Denaro V. Patellar resurfacing in total knee arthroplasty: systematic review and meta-analysis. J Arthroplasty. 2018;33(2):620–632. doi: 10.1016/j.arth.2017.08.041. [DOI] [PubMed] [Google Scholar]
- 16.Thomas C, Patel V, Mallick E, Esler C, Ashford RU. The outcome of secondary resurfacing of the patella following total knee arthroplasty: Results from the Trent and Wales arthroplasty register. Knee. 2018;25(1):146–152. doi: 10.1016/j.knee.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Clements WJ, Miller L, Whitehouse SL, Graves SE, Ryan P, Crawford RW. Early outcomes of patella resurfacing in total knee arthroplasty. Acta Orthop. 2010;81(1):108–113. doi: 10.3109/17453670903413145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Institute for Health and Care Excellence. Joint replacement (primary): hip, knee and shoulder. [L] Evidence review for patella resurfacing. NICE guideline NG157. Intervention evidence review underpinning recommendation 1.7.2 and the research recommendation in the NICE guideline. 2020. p. 134-135.https://www.nice.org.uk/guidance/ng157/evidence/l-patella-resurfacing-pdf-315756469335.
- 19.Newman JH, Ackroyd CE, Shah NA, Karachalios T. Should the patella be resurfaced during total knee replacement? Knee. 2000;7:17–23. [Google Scholar]
- 20.Maney AJ, Koh CK, Frampton CM, Young SW. Usually, selectively, or rarely resurfacing the patella during primary total knee arthroplasty: determining the best strategy. J Bone Joint Surg Am. 2019;101(5):412–420. doi: 10.2106/JBJS.18.00389. [DOI] [PubMed] [Google Scholar]
- 21.Vertullo CJ, Graves SE, Cuthbert AR, Lewis PL. The effect of surgeon preference for selective patellar resurfacing on revision risk in total knee replacement: an instrumental variable analysis of 136,116 procedures from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am. 2019;101(14):1261–1270. doi: 10.2106/JBJS.18.01350. [DOI] [PubMed] [Google Scholar]
- 22.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB, Group ftM-aOOSiE Meta-analysis of observational studies in epidemiology. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane. 2021. Available from www.training.cochrane.org/handbook.
- 25.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2011. [Google Scholar]
- 26.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schunemann HJ. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 27.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: a comparison of methods. Stat Med. 1999;18(20):2693–2708. doi: 10.1002/(sici)1097-0258(19991030)18:20<2693::aid-sim235>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 29.Ali A, Lindstrand A, Nilsdotter A, Sundberg M. Similar patient-reported outcomes and performance after total knee arthroplasty with or without patellar resurfacing. Acta Orthop. 2016;87(3):274–279. doi: 10.3109/17453674.2016.1170548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aunan E, Naess G, Clarke-Jenssen J, Sandvik L, Kibsgard TJ. Patellar resurfacing in total knee arthroplasty: functional outcome differs with different outcome scores: a randomized, double-blind study of 129 knees with 3 years of follow-up. Acta Orthop. 2016;87(2):158–164. doi: 10.3109/17453674.2015.1111075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deroche E, Batailler C, Swan J, Sappey-Marinier E, Neyret P, Servien E, Lustig S. No difference between resurfaced and non-resurfaced patellae with a modern prosthesis design: a prospective randomized study of 250 total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2022;30(3):1025–1038. doi: 10.1007/s00167-021-06521-y. [DOI] [PubMed] [Google Scholar]
- 32.Gildone A, Manfredini M, Biscione R, Faccini R. Patella resurfacing in posterior stabilised total knee arthroplasty: a follow-up study in 56 patients. Acta Orthop Belg. 2005;71(4):445–451. [PubMed] [Google Scholar]
- 33.Ferguson KB, Bailey O, Anthony I, James PJ, Stother IG, M JGB. A prospective randomised study comparing rotating platform and fixed bearing total knee arthroplasty in a cruciate substituting design--outcomes at two year follow-up. Knee. 2014;21(1):151–155. [DOI] [PubMed]
- 34.Myles CM, Rowe PJ, Nutton RW, Burnett R. The effect of patella resurfacing in total knee arthroplasty on functional range of movement measured by flexible electrogoniometry. Clin Biomech (Bristol, Avon) 2006;21(7):733–739. doi: 10.1016/j.clinbiomech.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 35.Schroeder-Boersch H, Scheller G, Fischer J, Jani L. Advantages of patellar resurfacing in total knee arthroplasty. Two-year results of a prospective randomized study. Arch Orthop Trauma Surg. 1998;117(1–2):73–78. doi: 10.1007/BF00703446. [DOI] [PubMed] [Google Scholar]
- 36.Vukadin OB, Blagojevic ZB, Bascarevic ZL, Slavkovic NS, Stevanovic V, Vukomanovic BD. The importance of patellar resurfacing in total knee arthroplasty for symptomatic valgus degenerative deformity. Acta Chir Orthop Traumatol Cech. 2017;84(1):30–34. [PubMed] [Google Scholar]
- 37.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;85(2):212–217. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Partio E. Comparison of patellar resurfacing and nonresurfacing in total knee arthroplasty : a prospective ramdamized study. J Orthop Rheumatol. 1995;8:69–74. [Google Scholar]
- 39.van Raaij TM, van dear Meij E, de Vries AJ, van Raay JJ. Patellar resurfacing does not improve clinical outcome in patients with symptomatic tricompartmental knee osteoarthritis. An RCT study of 40 patients receiving primary cruciate retaining total knee arthroplasty. J Knee Surg. 2021;34(14):1503–1509. doi: 10.1055/s-0040-1710369. [DOI] [PubMed] [Google Scholar]
- 40.Kaseb MH, Tahmasebi MN, Mortazavi SJ, Sobhan MR, Nabian MH. Comparison of clinical results between patellar resurfacing and non-resurfacing in total knee arthroplasty: a short term evaluation. Arch Bone Jt Surg. 2018;6(2):124–129. [PMC free article] [PubMed] [Google Scholar]
- 41.Kaseb MH, Mortazavi J, AyatiFiroozabadi M, Toofan H. Comparison between patellar resurfacing and retention in total knee arthroplasty regarding the postoperative satisfaction of patients and patellar crepitus. Arch Bone Jt Surg. 2019;7(5):441–444. [PMC free article] [PubMed] [Google Scholar]
- 42.Ha C, Wang B, Li W, Sun K, Wang D, Li Q. Resurfacing versus not-resurfacing the patella in one-stage bilateral total knee arthroplasty: a prospective randomized clinical trial. Int Orthop. 2019;43(11):2519–2527. doi: 10.1007/s00264-019-04361-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jia C, Ni M, Fu J, Li X, Li X, Chai W, Chen J. A comparative study on effectiveness of patellar resurfacing against non-resurfacing in total knee arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32(4):394–399. doi: 10.7507/1002-1892.201708128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koh IJ, Kim MS, Sohn S, Song KY, Choi NY, In Y. Patients undergoing total knee arthroplasty using a contemporary patella-friendly implant are unaware of any differences due to patellar resurfacing. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1156–1164. doi: 10.1007/s00167-018-5120-2. [DOI] [PubMed] [Google Scholar]
- 45.Kajino A, Yoshino S, Kameyama S, Kohda M, Nagashima S. Comparison of the results of bilateral total knee arthroplasty with and without patellar replacement for rheumatoid arthritis. A follow-up note. J Bone Joint Surg Am. 1997;79(4):570–574. [PubMed] [Google Scholar]
- 46.Liu ZT, Fu PL, Wu HS, Zhu Y. Patellar reshaping versus resurfacing in total knee arthroplasty - results of a randomized prospective trial at a minimum of 7 years' follow-up. Knee. 2012;19(3):198–202. doi: 10.1016/j.knee.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 47.Dong Y, Li T, Zheng Z, Xiang S, Weng X. Adding patella resurfacing after circumpatellar electrocautery did not improve the clinical outcome in bilateral total knee arthroplasty in Chinese population: a prospective randomized study. J Arthroplasty. 2018;33(4):1057–1061. doi: 10.1016/j.arth.2017.10.039. [DOI] [PubMed] [Google Scholar]
- 48.Thiengwittayaporn S, Srungboonmee K, Chiamtrakool B. Resurfacing in a posterior-stabilized total knee arthroplasty reduces patellar crepitus complication: a randomized, controlled trial. J Arthroplasty. 2019;34(9):1969–1974. doi: 10.1016/j.arth.2019.04.050. [DOI] [PubMed] [Google Scholar]
- 49.Chawla L, Bandekar SM, Dixit VP, Krishnamoorthi A, Mummigatti S. Functional outcome of patellar resurfacing vs non resurfacing in total knee arthoplasty in elderly: a prospective five year follow-up study. J Arthrosc Jt Surg. 2019;6(1):65–69. [Google Scholar]
- 50.Mayman D, Bourne RB, Rorabeck CH, Vaz M, Kramer J. Resurfacing versus not resurfacing the patella in total knee arthroplasty: 8- to 10-year results. J Arthroplasty. 2003;18(5):541–545. doi: 10.1016/s0883-5403(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 51.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years' followup. Clin Orthop Relat Res. 2004;428:12–25. [PubMed] [Google Scholar]
- 52.Burnett RS, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty. A concise follow-up of a randomized trial. J Bone Joint Surg Am. 2009;91(11):2562–2567. doi: 10.2106/JBJS.H.00109. [DOI] [PubMed] [Google Scholar]
- 53.Beaupre L, Secretan C, Johnston DW, Lavoie G. A randomized controlled trial comparing patellar retention versus patellar resurfacing in primary total knee arthroplasty: 5–10 year follow-up. BMC Res Notes. 2012;5:273. doi: 10.1186/1756-0500-5-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roberts DW, Hayes TD, Tate CT, Lesko JP. Selective patellar resurfacing in total knee arthroplasty: a prospective, randomized, double-blind study. J Arthroplasty. 2015;30(2):216–222. doi: 10.1016/j.arth.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 55.Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;88(6):734–739. doi: 10.1302/0301-620X.88B6.16822. [DOI] [PubMed] [Google Scholar]
- 56.Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;78(2):226–228. [PubMed] [Google Scholar]
- 57.Smith AJ, Wood DJ, Li MG. Total knee replacement with and without patellar resurfacing: a prospective, randomised trial using the profix total knee system. J Bone Joint Surg Br. 2008;90(1):43–49. doi: 10.1302/0301-620X.90B1.18986. [DOI] [PubMed] [Google Scholar]
- 58.Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002;84(2):187–193. doi: 10.2106/00004623-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 59.Maradit-Kremers H, Haque OJ, Kremers WK, Berry DJ, Lewallen DG, Trousdale RT, Sierra RJ. Is selectively not resurfacing the patella an acceptable practice in primary total knee arthroplasty? J Arthroplasty. 2017;32(4):1143–1147. doi: 10.1016/j.arth.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 60.Misra AN, Smith RB, Fiddian NJ. Five year results of selective patellar resurfacing in cruciate sparing total knee replacements. Knee. 2003;10(2):199–203. doi: 10.1016/s0968-0160(02)00097-2. [DOI] [PubMed] [Google Scholar]
- 61.Park SJ, Jung YB, Jeong HJ, Shin HK, Jung HJ, Lim JJ, Yoon JW, Kim E. Long-term results of primary total knee arthroplasty with and without patellar resurfacing. Acta Med Okayama. 2010;64(5):331–338. doi: 10.18926/AMO/40509. [DOI] [PubMed] [Google Scholar]
- 62.Hunt LP, Matharu GS, Blom AW, Howard PW, Wilkinson JM, Whitehouse MR. Patellar resurfacing during primary total knee replacement is associated with a lower risk of revision surgery. Bone Joint J. 2021;103-B(5):864–871. doi: 10.1302/0301-620X.103B5.BJJ-2020-0598.R2. [DOI] [PubMed] [Google Scholar]
- 63.Deere K, Whitehouse MR, Kunutsor SK, Sayers A, Price AJ, Mason J, Blom AW. How long do revised and multiply revised knee replacements last? A retrospective observational study of the National Joint Registry. Lancet Rheumatology. 2021;3(6):E438–E446. doi: 10.1016/S2665-9913(21)00079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.National Joint Registry. Knees - Primary Procedures - Surgical Technique.https://reports.njrcentre.org.uk/knees-primary-procedures-surgical-technique.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Material 1: PRISMA checklist. Supplementary Material 2. MOOSE checklist. Supplementary Material 3. Literature search strategy. Supplementary Material 4. Reference list of studies. Supplementary Material 5. Risk of bias assessment for randomised controlled trials. Supplementary Material 6. Baseline characteristics of observational studies. Supplementary Material 7. NOS scores for observational studies. Supplementary Material 8. Risk of anterior knee pain comparing patellar resurfacing with no resurfacing, by study-level characteristics. Supplementary Material 9. Patellar resurfacing versus no resurfacing and KOOS scale. Supplementary Material 10. Patellar resurfacing versus no resurfacing and range of movement. Supplementary Material 11. Patellar resurfacing versus no resurfacing and other measures of function. Supplementary Material 12. Patellar resurfacing versus no resurfacing and measures of pain. Supplementary Material 13. Patellar resurfacing versus no resurfacing and measures of health status, satisfaction, and quality of life. Supplementary Material 14. Patellar resurfacing versus no resurfacing and overall satisfaction. Supplementary Material 15. Funnel plots for risk of anterior knee pain, reoperations and revisions. Supplementary Material 16. Risk of revision, complications and pain comparing selective resurfacing with no resurfacing in observational cohort studies. Supplementary Material 17. Risk of revision, complications and pain comparing selective resurfacing with resurfacing in observational cohort studies. Supplementary Material 18. Selective resurfacing versus non-resurfacing and measures of function and pain in observational cohort studies. Supplementary Material 19. GRADE summary of findings.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available in a dedicated repository because the data extracted and analysed for this study is freely available by accessing the individual articles referenced in this publication. However the datasets may be available from the corresponding author on reasonable request.