Abstract
Introduction:
To examine the effects of coronavirus disease 2019 (COVID-19) on patients in an academic psychiatric ambulatory clinic, data from a measurement-based care (MBC) system were analyzed to evaluate impacts on psychiatric functioning in patients using telemedicine. Psychiatric functioning was evaluated for psychological distress (brief adjustment scale [BASE]-6), depression (patient health questionnaire [PHQ]-9), and anxiety (generalized anxiety disorder [GAD]-7), including initial alcohol (U.S. alcohol use disorders identification test) and substance use (drug abuse screening test-10) screening.
Methods:
This observational study included MBC data collected from November 2019 to March 2021. Patient-Reported Outcome Measures (PROMs) were examined to determine changes in symptomatology over the course of treatment, as well as symptom changes resulting from the pandemic. Patients were included in analyses if they completed at least one PROM in the MBC system.
Results:
A total of 2,145 patients actively participated in the MBC system completing at least one PROM, with engagement ranging from 35.07% to 83.50% depending on demographic factors, where completion rates were significantly different for age, payor status, and diagnostic group. Average baseline scores for new patients varied for the GAD-7, PHQ-9, and BASE-6. Within-person improvements in mental health before and after the pandemic were statistically significant for anxiety, depression, and psychological adjustment.
Discussion:
MBC is a helpful tool in determining treatment progress for patients engaging in telemedicine. This study showed that patients who engaged in psychiatric services incorporating PROMs had improvements in mental health during the COVID-19 pandemic. Additional research is needed exploring whether PROMs might serve as a protective or facilitative factor for those with mental illness during a crisis when in-person visits are not possible.
Keywords: COVID, telepsychiatry, behavioral health, telemedicine, e-Health
Introduction
The World Health Organization declared the novel coronavirus disease 2019 (COVID-19) a pandemic on March 11, 2020.1 Since the initial identification of COVID-19 in December 2019,2 studies have shown pronounced effects on psychiatric health functioning, including depression, anxiety, substance use, and post-traumatic stress disorder.3–10
Specific COVID-19 factors impacting mental illness include uncertainty, fears of infection, having adequate basic supplies, unemployment, and inadequate personal protective equipment.11,12 Quarantine, lockdown, and shelter in place status create additional psychiatric distress due to changing guidelines and messaging from authorities, loss of personal freedoms, home confinement, boredom, and financial loss.13 This constellation of factors along with avoidance of health settings and shared transportation creates significant barriers to mental health interventions during a pandemic.11,12
We know that individuals with a history of psychiatric illness are at higher risk for worsening psychiatric symptoms during a pandemic14,15 and that having mental illness increases one's risk of contracting COVID-19 through lack of preventive health care, limited health care access, higher prevalence of comorbid medical illness, and homelessness.16–18 Taken together, social changes due to the COVID-19 pandemic and its psychiatric consequences are significant, highlighting the need for identification of preventive or prophylactic actions that mitigate negative effects.19 As the pandemic continues, data on mental health outcomes of individuals receiving psychiatric care before and during COVID-19 are still emerging. The identification and evaluation of the effects of mental illness intervention on psychiatric sequelae in community samples may prove instructive.20
The COVID-19 pandemic has provided an unprecedented challenge to health service providers.21 The rapid transition to telemedicine resulting from the pandemic required significant changes to traditional therapeutic processes.22–24 Of particular concern is the clinician's ability to reliably assess patients' symptomatology to aid in clinical decision-making in the context of telemedicine.25 It has also changed the definition of telemedicine since many places adopted a hybrid of services. Our group allowed for phone, video, and in-person visits, although the latter were the least common. We opted to define the delivery method of a case as telemedicine when a patient was seen by phone or video more than 70% of the time.
The psychiatry clinic also engages patients in Measurement-Based Care (MBC), an evidence-based tool that uses systematic ongoing collaborative evaluation of patient symptoms to inform clinical decision-making.26 It is poised to address some of the challenges of telemedicine and improve patient and clinician communication in this platform.27 One essential component of MBC is the regular use of Patient-Reported Outcome Measures (PROMs). MBC has demonstrated ability to assess psychiatric symptoms, psychological functioning, and clinical changes, resulting in improved patient outcomes.28,29 Remote MBC can enhance care within telemedicine.30,31
Consequently, one of MBC's most relevant applications is during a crisis when in-person interventions are not possible.32 When MBC is integrated into a system before a crisis onset (e.g., COVID-19 pandemic), it provides a cost-effective capacity to evaluate real-time changes in mental illness. This project seizes on the confluence of utilizing MBC in conjunction with in-person psychiatric care 4 months before and with predominantly telemedicine 12 months after the declaration of COVID-19 as an international pandemic.1,31,32
The present study aimed to document the mental illness status of patients receiving outpatient psychiatric tele-care with MBC within a regional health care system (∼20-county region) and to examine its association with the COVID-19 environment, through the following: (1) examining differences in PROM completion rates across demographic factors; (2) evaluating new patient baseline psychological distress before and during COVID-19; and (3) evaluating within group differences for psychiatric symptomatology before and during COVID-19. It was hypothesized that patient exposure to pandemic-related stressors, along with loss of employment, finances, and social functioning, as well as patients receiving care through telemedicine rather than in person, would be associated with higher levels of psychiatric symptomatology, psychological distress, and decreased well-being.
Methods
STUDY POPULATION AND DESIGN
Participants were identified from the Department of Psychiatry and Behavioral Medicine's (PBM) outpatient clinic in a United States regional hospital. Inclusion criteria comprised patients ≥18 years of age who completed at least one PROM between November 1, 2019 and March 18, 2021 resulting in 2,145 eligible patients.
Telemedicine was defined as care conducted more than 70% of the time through phone or video. Before the pandemic, between November 2019 and February 2020, patients in the PBM clinic received services by phone or video 3–5% of the time. From April 2020 to March 2021, 71–95% of patients received services through telephone or video, depending on the month, spotlighting the swift change to telemedicine as the primary service modality. This study was granted exemption from Institutional Review Board (IRB) review under DHHS regulatory category 4(iii): Secondary Research Without Consent, according to the Carilion Clinic Institutional Review Board.
PROCEDURE
As part of our standard care, adult patients seen in PBM are encouraged to complete PROMs. Patients are given the opportunity to complete a standardized set of PROMs immediately before the initial clinician appointment. Participants are then encouraged to complete specific PROMs monthly. Measurement data were collected through a secure cloud-based program with results immediately available for review.
MEASURES
Patient demographics
Age, ethnicity, race, payor status, rurality location based on rural-urban commuting area code, and diagnosis were obtained from individual patients' Electronic Medical Records and deidentified datasets exported into a cloud-based secure research environment for analysis.
The following standard administered MBC PROMs were used in this study.
Brief adjustment scale-6 (initial and monthly)
The brief adjustment scale-6 (BASE-6) is a 6-item self-report scale designed to address overall psychological functioning and adjustment.33 All items are rated from 1 (not at all) to 7 points (extremely), and total scores range from 6 to 42 points. Higher scores indicate lower general psychological adjustment with a clinical cutoff of 19 indicating clinically meaningful distress. The BASE-6 has demonstrated good to excellent internal consistency (Cronbach's α = 0.87–0.93) in both clinical and nonclinical samples, and test–retest reliability was 0.77 for nonclinical samples.33
Drug abuse screening test-10 (initial)
The drug abuse screening test (DAST)-10 is a 10-item self-report questionnaire that assesses potential involvement with drugs, excluding alcohol and tobacco, during the past 12 months.34 Subjects report problematic drug use with yes/no answers. Results provide a quantitative index of the extent of problems related to drug abuse.
Generalized anxiety disorder-7 (initial and monthly)
The generalized anxiety disorder (GAD)-7 is a 7-item self-report scale designed to measure the severity of GAD symptoms.35 Participants are asked to report their anxiety symptoms over the past two weeks, and items are rated on a 4-point Likert scale. Scores range from 0 to 21 points, with higher scores indicating greater levels of anxiety. GAD-7 also has excellent internal consistency (Cronbach's α = 0.92) and test–retest reliability (r = 0.83).35
Patient health questionnaire-9 (initial and monthly)
The patient health questionnaire (PHQ)-9 is a 9-item self-report measure of depression symptoms over the past 2 weeks, mapping onto the DSM-5 diagnostic criteria.36 Items are rated as 0 (not at all) to 3 (almost every day), and the total score ranges from 0 to 27 points. The higher scores represent greater severity of depressive symptoms. PHQ-9 demonstrates good internal consistency (Cronbach's α = 0.89) and test–retest reliability (r = 0.84).36
U.S. alcohol use disorders identification test (initial)
The U.S. alcohol use disorders identification test (USAUDIT) is a brief self-report screening measure to identify subjects using alcohol in a problematic way over the past 12 months.37 It measures three domains of alcohol use: (1) hazardous use, (2) dependence symptoms, and (3) harmful alcohol use. The total score ranges from 0 to 46 points, with higher scores suggesting a mild/moderate/severe level of alcohol use and dependence.36
STATISTICAL ANALYSIS
Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). Descriptive analyses were completed where numeric variables were investigated by measures of central tendency and variation, and categorical variables were investigated by frequencies and percentages. Analysis of variance (ANOVA) and t tests analyzed the mean difference in survey responses by the various demographic variables.
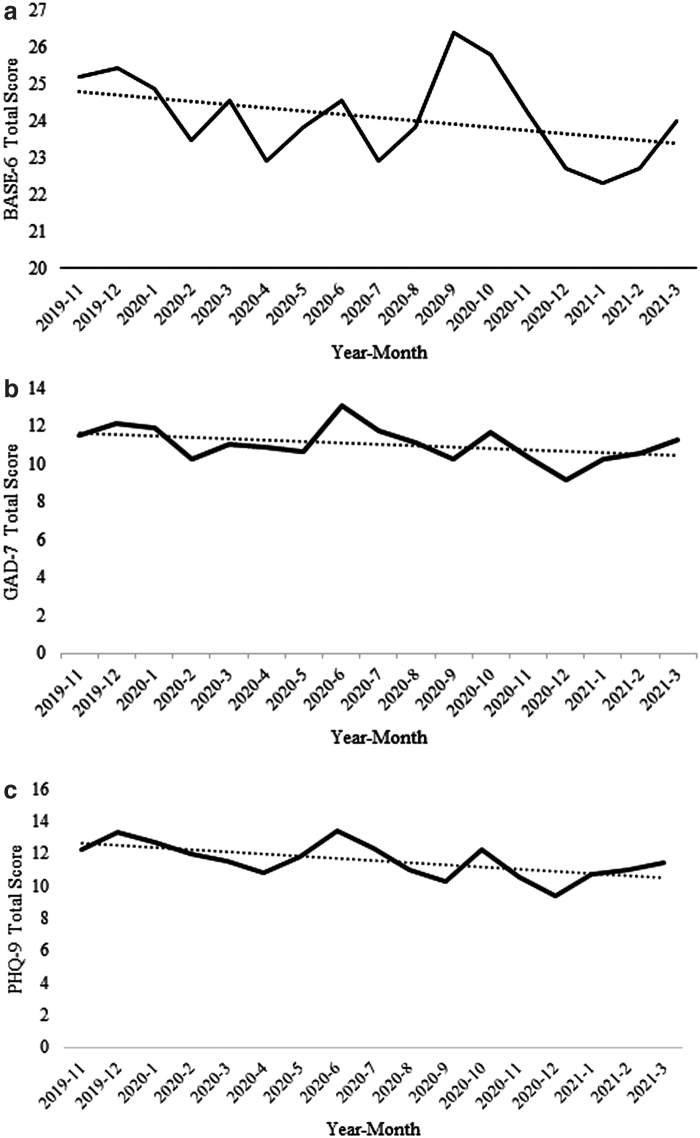
For aim 1, MBC completion percentage was representative of the number of completions compared to the number of months in treatment (Table 1). In addition, chi-square tests were performed to examine differences in completion rate across demographic factors (Table 1). Regarding aim 2, regression analyses were conducted for baseline PROMs for each new patient to determine if a significant time trend was apparent (Table 2 and Fig. 1a–c). Aim 3 used paired-sample t tests to examine PROM scores before and after COVID-19 onset in patients established in the clinic (Table 3). At least 176 pairs of data were collected for each main PROM, achieving at least 74% power to reject the null hypothesis when the population effect size is considered small.
Table 1.
Comparison of completion rates across demographics by (a) age, (b) gender, (c) race, (d) diagnostic category, (e) payor status, and (f) rurality
| (a) AGE | TOTAL N | N OF COMPLETED PROMS | TREATMENT MONTHS | COMPLETION RATE (%) | P |
|---|---|---|---|---|---|
| Unknown | 4 | 4 | 11 | 36.36 | <0.00 |
| 18–22 | 129 | 252 | 340 | 74.12 | |
| 23–27 | 232 | 456 | 698 | 65.33 | |
| 28–32 | 275 | 680 | 1041 | 65.32 | |
| 33–37 | 247 | 545 | 980 | 55.61 | |
| 38–42 | 243 | 593 | 1041 | 56.96 | |
| 43–47 | 210 | 565 | 834 | 67.75 | |
| 48–52 | 187 | 461 | 669 | 68.91 | |
| 53–57 | 168 | 434 | 676 | 64.20 | |
| 58–62 | 168 | 373 | 630 | 59.21 | |
| 63–67 | 117 | 290 | 418 | 69.38 | |
| 68–72 | 91 | 200 | 296 | 67.57 | |
| 73–77 | 48 | 108 | 182 | 59.34 | |
| 78–82 | 21 | 34 | 77 | 44.16 | |
| 83–87 | 5 | 6 | 15 | 40.00 | |
| Total | 2,145 | 5,001 | 7,908 | 63.24 | |
| (b) GENDER | N | COMPLETED PROMS | TREATMENT MONTHS | % | p |
| F | 1,485 | 3,510 | 5,612 | 62.54 | 0.11 |
| M | 659 | 1,489 | 2,292 | 64.97 | |
| U | 1 | 2 | 4 | 50.00 | |
| Total | 2,145 | 5,001 | 7,908 | 63.24 | |
| (c) RACE | N | COMPLETED PROMS | TREATMENT MONTHS | % | |
| Other | 209 | 442 | 687 | 64.34 | |
| White or Caucasian | 1,936 | 4,559 | 7,221 | 63.14 | |
| Total | 2,145 | 5,001 | 7,908 | 63.24 | |
| (d) DIAGNOSTIC CATEGORY | N | COMPLETED PROMS | TREATMENT MONTHS | % | p |
| Anxiety disorders | 150 | 341 | 458 | 74.45 | <0.00 |
| Bipolar disorders | 249 | 640 | 871 | 73.48 | |
| Depressive Disorders | 727 | 1,876 | 2,554 | 73.45 | |
| Generalized Anxiety Disorder | 197 | 496 | 594 | 83.50 | |
| Other | 719 | 1,426 | 2,798 | 50.96 | |
| SUD | 103 | 222 | 633 | 35.07 | |
| Total | 2,145 | 5,001 | 7,908 | 63.24 | |
| (e) PAYOR | N | COMPLETED PROMS | TREATMENT MONTHS | % | P |
| Commercial | 835 | 2,076 | 2,582 | 80.40 | <0.00 |
| Medicaid | 504 | 1,073 | 1,958 | 54.80 | |
| Medicare | 377 | 868 | 1,423 | 61.00 | |
| Other | 22 | 57 | 80 | 71.25 | |
| Self | 165 | 544 | 864 | 62.96 | |
| Unknown | 242 | 383 | 1,001 | 38.26 | |
| Total | 2,145 | 5,001 | 7,908 | 63.24 | |
| (f) RURALITY DESCRIPTION | N | COMPLETED PROMS | TREATMENT MONTHS | % | |
| Metropolitan area core: primary flow within an urbanized area | 1,483 | 3,410 | 5,377 | 63.42 | |
| Other | 662 | 1,591 | 2,531 | 62.86 | |
| Total | 2,145 | 5,001 | 7,908 | 63.24 |
Bold value signifies p < 0.00.
PROM, patient-reported outcome measure; SUD, substance use disorder.
Table 2.
Mean scores for new patient baseline psychological distress (BASE-6), depression (PHQ-9), and anxiety (GAD-7) are presented for each month from November 2019 to March 2021
| COHORT | MEAN (SD) |
MEDIAN |
|||
|---|---|---|---|---|---|
| BASE-6 | PHQ-9 | GAD-7 | DAST-10 | AUDIT | |
| November 2019 | 25.20 (10.81) | 12.28 (8.49) | 11.49 (6.30) | 0.5 | 1 |
| December 2019 | 25.42 (9.17) | 13.32 (7.06) | 12.09 (6.02) | 0 | 3 |
| January 2020 | 24.88 (9.09) | 12.72 (7.08) | 11.93 (5.73) | 0 | 3 |
| February 2020 | 23.46 (10.90) | 11.94 (7.09) | 10.26 (6.70) | 0 | 1 |
| March 2020 | 24.56 (10.01) | 11.53 (6.80) | 11.00 (5.95) | 0 | 1 |
| April 2020 | 22.91 (10.66) | 10.84 (7.24) | 10.85 (6.67) | 0 | 2 |
| May 2020 | 23.84 (10.33) | 11.84 (7.09) | 10.66 (6.40) | 0 | 2 |
| June 2020 | 24.56 (10.01) | 13.45 (6.58) | 13.04 (5.67) | 0 | 2 |
| July 2020 | 22.91 (10.66) | 12.38 (7.34) | 11.76 (6.39) | 0 | 2 |
| August 2020 | 23.84 (10.33) | 11.00 (7.06) | 11.12 (6.27) | 0 | 1 |
| September 2020 | 26.38 (9.79) | 10.27 (8.38) | 10.23 (6.74) | 0 | 1 |
| October 2020 | 25.80 (10.77) | 12.21 (7.30) | 11.64 (6.43) | 0 | 1 |
| November 2020 | 24.24 (9.93) | 10.56 (7.41) | 10.33 (6.49) | 0 | 1 |
| December 2020 | 22.71 (11.59) | 9.35 (8.28) | 9.17 (6.98) | 0 | 0 |
| January 2021 | 22.33 (10.93) | 10.75 (7.67) | 10.29 (6.49) | 0 | 1 |
| February 2021 | 22.72 (11.33) | 10.99 (7.53) | 10.57 (6.75) | 0 | 1.5 |
| March 2021 | 23.98 (10.62) | 11.46 (6.76) | 11.25 (6.16) | 0 | 1 |
| p-value | 0.14 | 0.01** | 0.09 | 0.10 | 0.03* |
p ≤ 0.05, **p ≤ 0.01.
AUDIT, alcohol use disorders identification test; BASE-6, brief adjustment scale-6; DAST-10, drug abuse screening test-10; GAD-7, generalized anxiety disorder-7; PHQ-9, patient health questionnaire-9; SD, standard deviation.
Note: Since drug use (DAST-10) and alcohol use (AUDIT) data were heavily skewed, the median total score is presented.
Fig. 1.
(a) Average monthly new patient baseline scores of the BASE-6. (b) Average monthly new patient baseline scores of the GAD-7.(c). Average monthly new patient baseline scores of the PHQ-9. BASE-6, brief adjustment scale-6; GAD-7, generalized anxiety disorder-7; PHQ-9, patient health questionnaire-9.
Table 3.
Comparison of scores for clinic patients with at least one PROM before and after pandemic declaration as measured by paired-sample t-test of survey responses for the BASE-6, GAD-7, and PHQ-9
| N | PRE | POST | PRE-POST | p | |
|---|---|---|---|---|---|
| BASE-6 | 196 | 23.91 | 21.01 | 2.9 | <0.00 |
| GAD-7 | 199 | 10.55 | 8.39 | 2.16 | <0.00 |
| PHQ-9 | 176 | 11.88 | 9.7 | 2.18 | 0.00 |
BASE-6 range 6–42, >19 = higher distress. GAD-7 range 0–21, clinically meaningful change = 6 with change from one severity level to another. PHQ-9 range 0–27, clinically meaningful change = 5.
Results
COMPLETION OF PROMs ACROSS DEMOGRAPHICS
PROM completion rates were examined across different demographic factors (aim 1; Table 1). Completion rates were calculated for different age bands, gender, diagnostic category, payor status, and rurality, where the percentage represented the number of completions compared to the number of months in treatment, as patients were encouraged to complete PROMs monthly.
The results of chi-square tests showed significant differences in completion rates among different age groups, diagnostic groups, and payor status, while there were no significant differences among gender groups. Differences by race were not calculated due to 90.26% of subjects being White/non-Hispanic. For different age groups, completion rates ranged from 40.00% (83- to 87-years-old) to 74.12% (18- to 22-years-old). White/non-Hispanic patients (63.14%) had similar completion rates to other racial groups (63.34%), as did female (62.54%) and male (64.97%), or metropolitan (63.42%) and other areas (62.86%).
Rates varied by payor status with the lowest completion among unknown (38.26%) and the highest completion in commercial patients (80.40%), followed by other (71.25%). Diagnostic groups varied in completion rates with the least completion from patients with substance use disorders (35.07%) compared to the highest completion rates in GAD patients (83.50%).
BASELINE PSYCHOLOGICAL DISTRESS
Baseline psychological symptoms (BASE-6, PHQ-9, GAD-7, DAST-10, and USAUDIT) were compared for new patients entering treatment each month from November 2019 to March 2021 (aim 2; Table 2 and Fig. 1a–c). Linear regression analyses were conducted to determine if month entering treatment was significant to the mean BASE-6, GAD-7, PHQ-9, DAST-10, and USAUDIT survey scores. Month entering care was not a significant predictor for mean BASE-6 (p = 0.14), GAD-7 (p = 0.09), and DAST-10 (p = 0.10) scores, but month entering care was significant to mean PHQ-9 (p = 0.01) and USAUDIT (p = 0.03) scores. Figure 1a–c shows average scores and trends of the BASE-6, GAD-7, and PHQ-9.
WITHIN-GROUP PROMs SPANNING THE ONSET OF COVID-19
Within-group differences were evaluated for psychological distress (BASE-6), depression (PHQ-9), and anxiety (GAD-7). Due to the high volume of missing data, only the first survey for the pre-COVID-19 period (November 2019 through February 2020) and the final survey of the examined post-COVID-19 period were considered. Patients who completed at least 1 survey before and after the pandemic onset for the BASE-6 (n = 196), PHQ-9 (n = 176), and GAD-7 (n = 199) were included. Paired samples t tests were conducted to determine changes related to COVID-19 (Table 3). The GAD-7 showed significant improvements from before (M = 10.55) and after March 2020 (M = 8.39; p < 0.00). Both the BASE-6 (p < 0.00) and PHQ-9 (p < 0.00) also showed significant positive change (Table 3).
WITHIN-GROUP DEMOGRAPHICS
Within-group demographic differences were evaluated using ANOVA and t tests to analyze the mean difference in survey responses by the following variables: age groups, male or female gender, race, payor, rurality, and diagnosis. Multiple variables were recorded for testing to combine less frequent subgroups, resulting in the following: age (in 5-year spans), race (white or other), gender (male or female), payor (commercial, Medicaid, Medicare, self, or other), rurality (primary flow in an urban area or other), and diagnosis (anxiety [excluding GAD], bipolar, depressive, substance, generalized anxiety, other disorders).
Regarding psychological distress, no significant differences were found for change in mean BASE-6 score by age (p = 0.56), race (p = 0.28), payor status (p = 0.39), rurality (p = 0.51), or diagnosis (p = 0.69). A significant difference was found for gender (p = 0.04). For anxiety, there were no significant differences in mean change on the GAD-7 for age (p = 0.70), gender (p = 0.14), race (p = 0.38), payor status (p = 0.21), rurality (p = 0.12), or diagnosis (p = 0.18). There were no significant changes in depression by mean change on the PHQ-9 by age (p = 0.96), gender (p = 0.69), race (p = 0.41), payor status (p = 0.07), or rurality (p = 0.56); however, there was a significant difference by diagnosis (p = 0.03) (Table 4).
Table 4.
Differences in PROM means by demographic variables (age, gender, race, payor status, rurality, and diagnostic group)
| N | BASE-6 | N | GAD-7 | N | PHQ-9 | |
|---|---|---|---|---|---|---|
| Age group (p) | 195 | 0.56 | 198 | 0.70 | 173 | 0.96 |
| 18–22 | 12 | −5.17 (7.81) | 12 | −5.17 (4.63) | 12 | −3.75 (10.34) |
| 23–27 | 12 | −5.92 (9.22) | 12 | −3.00 (6.54) | 10 | −2.20 (6.39) |
| 28–32 | 22 | 0.50 (9.64) | 22 | 0.09 (5.73) | 18 | 0.44 (10.17) |
| 33–37 | 23 | −4.09 (8.56) | 22 | −3.41 (6.01) | 22 | −2.27 (9.85) |
| 38–42 | 23 | −4.22 (11.31) | 25 | −1.88 (6.50) | 18 | 0 (12.27) |
| 43–47 | 20 | −1.85 (8.93) | 20 | −2.25 (4.94) | 14 | −1.57 (12.18) |
| 48–52 | 21 | −3.38 (7.94) | 21 | −1.67 (5.59) | 21 | −3.43 (9.74) |
| 53–57 | 16 | −1.75 (9.66) | 17 | −2.65 (7.20) | 17 | −2.24 (8.48) |
| 58–62 | 18 | −4.22 (7.93) | 18 | −1.44 (5.71) | 16 | −3.69 (8.40) |
| 63–67 | 15 | 0.67 (10.89) | 16 | −1.56 (7.35) | 14 | −1.79 (9.98) |
| 68–72 | 9 | −6.11 (13.50) | 9 | −3.33 (7.12) | 8 | −5.75 (6.32) |
| 73–77 | 4 | −1.25 (6.13) | 4 | −2.75 (4.99) | 3 | −1.67 (4.93) |
| Gender (p) | 0.04* | 0.14 | 0.69 | |||
| Female | 147 | −3.76 (9.55) | 150 | −2.55 (5.93) | 132 | −2.01 (9.62) |
| Male | 48 | −0.48 (8.79) | 48 | −1.08 (6.39) | 41 | −2.71 (9.79) |
| Race (p) | 0.28 | 0.38 | 0.41 | |||
| White or Caucasian | 180 | −3.16 (9.23) | 183 | −2.31 (5.86) | 158 | −2.36 (9.50) |
| Other | 15 | −0.40 (11.85) | 15 | −0.87 (8.29) | 15 | −0.20 (11.16) |
| Payor (p) | 0.39 | 0.21 | 0.07 | |||
| Commercial | 71 | −4.00 (9.48) | 71 | −2.82 (6.14) | 66 | −4.18 (9.89) |
| Medicaid | 38 | −3.87 (10.10) | 39 | −3.13 (6.44) | 33 | 0.82 (9.62) |
| Medicare | 40 | −2.40 (9.61) | 40 | −2.10 (5.98) | 37 | −1.43 (9.24) |
| Self | 43 | −0.70 (8.51) | 45 | −0.40 (5.66) | 34 | −1.29 (8.33) |
| Other | 3 | −6.00 (11.36) | 3 | −3.67 (0.58) | 3 | −10.00 (15.72) |
| Rurality (p-values) | 0.51 | 0.12 | 0.56 | |||
| Primary urban area | 157 | −2.73 (9.18) | 159 | −1.87 (5.87) | 134 | −2.40 (9.58) |
| Other | 38 | −3.87 (10.60) | 39 | −3.54 (6.69) | 39 | −1.38 (9.91) |
| Diagnostic group (p) | 0.69 | 0.18 | 0.03* | |||
| Anxiety disorders | 16 | −3.44 (10.35) | 16 | −2.13 (5.03) | 14 | −3.64 (7.92) |
| Bipolar disorder | 33 | −2.30 (8.66) | 33 | −2.73 (6.25) | 33 | 0.76 (9.21) |
| Depressive disorders | 75 | −3.33 (9.82) | 78 | −2.45 (5.74) | 68 | −3.88 (9.41) |
| Substance use disorder | 15 | 0.07 (6.82) | 14 | 0.93 (3.58) | 14 | 2.21 (10.38) |
| Generalized anxiety disorder | 15 | −5.67 (12.85) | 15 | −4.80 (8.13) | 12 | 1.75 (12.66) |
| Other | 41 | −2.68 (8.58) | 42 | −1.45 (6.44) | 32 | −4.31 (8.37) |
p ≤ 0.05.
Note: Mean survey differences were calculated by subtracting the pre-March survey score from the post-March survey score. Numbers are represented as mean (SD).
Discussion
Surveys suggest that people with a history of psychiatric illness are experiencing worsening depression and anxiety during the COVID-19 pandemic.3–10 Higher rates of depression and anxiety, as well as substance use, have been documented in those who contracted or were exposed to COVID-19, as well as in those impacted by the pandemic socially and economically. Parallel to these early clinical findings, measures required to prevent the spread of COVID-19 necessitated a shift in psychiatric care to virtual platforms, a sudden change for the vast majority of patients and clinicians.
Our clinic's use of PROMs allowed for symptom tracking before and during the COVID-19 pandemic and provided novel information about the symptoms of new and returning psychiatry patients during this time. Based on the early research findings noted above, we hypothesized that psychiatric symptomatology would increase both between and within subject groups during the COVID-19 pandemic compared to prepandemic times. In fact, this did not occur.
New patients entering the clinic had statistically lower scores on all scales from November 2019 to March of 2021 (Table 2 and Fig. 1). Statistically significant improvements were also observed in PHQ-9, GAD-7, and BASE-6 scores for patients followed longitudinally before and through the pandemic (Table 3).
Thus, despite uncertainty surrounding a novel coronavirus and its impact on communities, workforce, health care, finances, daily living, and a change to telemedicine, subjects improved. In particular, for returning patients, women showed improved functioning during the study period more than men, and there was a difference in PHQ-9 scores dependent on the diagnostic group. Differences in gender and diagnostic group completion could reflect greater willingness for certain groups to engage in PROMs, an area that deserves further study.
Differences in completion rates for new patients based on demographics and mental health diagnosis were significant for age, diagnosis, and payor status. Comparing initial symptom severity of depression, anxiety, and functional status from pre-COVID to COVID months, there was no evidence that patients new to the clinic were more severely ill following the state stay-at-home mandate or as the pandemic persisted; however, care became more challenging to access in the earliest stages which may have prevented those with severe psychopathology from accessing necessary care.
Alcohol and substance use severity pre- and post-COVID could not be assessed given overall low PROM completion, again suggesting that there may be additional barriers to MBC that could be investigated in this population. Since only 35% of patients in this category completed PROMs, we may not have captured data from patients who would endorse higher scores.
Previous studies suggested development or worsening of mental health issues during the pandemic, but our group did not replicate that finding. We suspect that, consistent with MBC efficacy studies, use of PROMs allowed for closer monitoring of symptoms in the context of telemedicine, as it has been shown to do for in-person visits. Therefore, it may have facilitated patient engagement and allowed more regular symptom assessment and treatment adjustments.
The study has several limitations. One is the absence of a patient comparison group who did not complete measures. It is possible that those who did not engage in MBC may have also experienced improvement in psychiatric symptoms. In addition, many patients only completed the PROMs, in part, and at different frequencies.
In some areas, insufficient data points exist to show any potential relationship between PROM completion frequency and outcomes. While we considered that COVID-19 stimulus checks may have mitigated the anticipated symptom decline in this population, measurement of this factor was not within the scope of this study. Finally, our psychiatric assessment was in a geographical area, predominantly White/non-Hispanic, not initially affected by high rates of infection. That said, patients were dealing with uncertainty and unprecedented isolation surrounding the pandemic and high rates of infection and hospitalization later in the pandemic, much like other areas of the United States.
Navigating the switch to telemedicine during the COVID-19 pandemic has been demanding. Through use of PROMs, this study reveals that patients with psychiatric illness in an ambulatory psychiatry clinic experienced improvement in their symptoms. As psychiatric practice pivots to greater use of telemedicine and is faced with managing the impact of COVID-19 on patients with psychiatric illness, it is important that we optimize patient care. While additional research is needed, this study suggests that MBC, utilizing PROMs in particular, can be used proactively in telemedicine to track symptoms and minimize psychiatric sequelae through a crisis, when psychiatric care remains paramount.
Disclosure Statement
The authors declare that this represents original work, that we have the rights to this work, and that this work is not being considered for publication elsewhere and has not been published elsewhere. In addition, we have obtained and can supply all necessary permissions for the reproduction of any copyright works that are not owned by us. The authors declare that there is no conflict of interest.
Funding Information
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
REFERENCES
- 1. World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19-11, March 2020. Available at https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 (last accessed December 5, 2020).
- 2. Lu H, Stratton CW, Tang Y. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol 2020;92:401–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ettman CK, Abdalla SM, Cohen GH, et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 2020;3:e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 2020;87:40–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord 2020;277:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liu CH, Zhang E, Wong GTF, et al. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry Res 2020;290:113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Klimkiewicz A, Jasionowska J, Schmalenberg A, et al. COVID-19 pandemic-related depression and insomnia among psychiatric patients and the general population. J Clin Med 2021;10:3425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berardelli I, Sarubbi S, Rogante E, et al. The impact of the COVID-19 pandemic on suicide ideation and suicide attempts in a sample of psychiatric inpatients. Psychiatry Res 2021;303:114072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tsai J, Elbogen EB, Huang M, et al. Psychological distress and alcohol use disorder during the COVID-19 era among middle- and low-income US adults. J Affect Disord 2021;288:41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nigatu YT, Elton-Marshall T, Wells S, et al. The association between COVID-19 diagnosis or having symptoms and anxiety among Canadians: A repeated cross-sectional study. Anxiety Stress Coping 2021;34:503–512. [DOI] [PubMed] [Google Scholar]
- 11. Serafini G, Parmigiani B, Amerio A, et al. The psychological impact of COVID-19 on the mental health in the general population. QJM Int J Med 2020;113:531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020;395:912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang Q, Xu R, Volkow ND. Increased risk of COVID-19 infection and mortality in people with mental disorders: Analysis from electronic health records in the United States. World Psychiatry 2021;20:124–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hao F, Tan W, Jiang L, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun 2020;87:100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Taquet M, Luciano S, Geddes JR, et al. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2020;8:130–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shinn AK, Viron M. Perspectives on the COVID-19 pandemic and individuals with serious mental illness. J Clin Psychiatry 2020;81:20com13412. [DOI] [PubMed] [Google Scholar]
- 18. Sáiz PA, de la Fuente-Tomas L, García-Alvarez L, et al. Prevalence of passive suicidal ideation in the early stage of the coronavirus disease 2019 (COVID-19) pandemic and lockdown in a large Spanish sample. J Clin Psychiatry 2020;81:20.|13421. [DOI] [PubMed] [Google Scholar]
- 19. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern Med 2020;180:817–818. [DOI] [PubMed] [Google Scholar]
- 20. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med 2020;383:510–512. [DOI] [PubMed] [Google Scholar]
- 21. Zhou X, Snoswell CL, Harding LE, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed J E Health 2020;26:377–379. [DOI] [PubMed] [Google Scholar]
- 22. Kalin ML, Garlow SJ, Thertus K, et al. Rapid implementation of telehealth in hospital psychiatry in response to COVID-19. Am J Psychiatry 2020;177:636–637. [DOI] [PubMed] [Google Scholar]
- 23. Puspitasari AJ, Heredia D Jr, Gentry M, et al. Rapid adoption and implementation of telehealth group psychotherapy during COVID 19: Practical strategies and recommendations. Cogn Behav Pract 2021;28:492–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chen JA, Chung W-J, Young SK, et al. COVID-19 and telepsychiatry: Early outpatient experiences and implications for the future. Gen Hosp Psychiatry 2020;66:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Torous J, Wykes T. Opportunities from the coronavirus disease 2019 pandemic for transforming psychiatric care with telehealth. JAMA Psychiatry 2020;77:1205–1206. [DOI] [PubMed] [Google Scholar]
- 26. Lewis CC, Boyd M, Puspitasari A, et al. Implementing measurement-based care in behavioral health: A review. JAMA Psychiatry 2019;76:324–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Douglas S, Jensen-Doss A, Ordorica C, et al. Strategies to enhance communication with telemental health measurement-based care (tMBC). Pract Innovations 2020;5:143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lambert MJ. Outcome in psychotherapy: The past and important advances. Psychotherapy 2013;50:42–51. [DOI] [PubMed] [Google Scholar]
- 29. Lambert MJ, Whipple JL, Kleinstäuber M. Collecting and delivering progress feedback: A meta-analysis of routine outcome monitoring. Psychotherapy 2018;55:520–537. [DOI] [PubMed] [Google Scholar]
- 30. Goldberg SB, Buck B, Raphaely S, et al. Measuring psychiatric symptoms remotely: A systematic review of remote measurement-based care. Curr Psychiatry Rep 2018;20:81. [DOI] [PubMed] [Google Scholar]
- 31. Miu AS, Vo HT, Palka JM, et al. Teletherapy with serious mental illness populations during COVID-19: Telehealth conversion and engagement. Counselling Psychol Q 2021;34:3–4:704–721. [Google Scholar]
- 32. Augusterfer EF, Mollica RF, Lavelle J. Leveraging technology in post-disaster settings: The role of digital health/telemental health. Curr Psychiatry Rep 2018;2:88. [DOI] [PubMed] [Google Scholar]
- 33. Cruz RA, Peterson AP, Fagan C, et al. Evaluation of the Brief Adjustment Scale-6 (BASE-6): A measure of general psychological adjustment for measurement-based care. Psychol Serv 2020;17:332–342. [DOI] [PubMed] [Google Scholar]
- 34. Bohn MJ, Babor T, Kranzler HR. Validity of the Drug Abuse Screening Test (DAST-10) in inpatient substance abusers. Probl Drug Depend 1991;119:233–235. [Google Scholar]
- 35. Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006;166:1092. [DOI] [PubMed] [Google Scholar]
- 36. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Barbor TF, Higgins-Biddle JC, Robaina K. USAUDIT, the alcohol use disorders identification test, adapted for use in the United States: A guide for primary care practitioners. 2017. Available at https://www.researchgate.net/publication/322721505 (last accessed December 5, 2020).