Abstract
Introduction:
Cost studies of telehealth (TH) and virtual visits are few and report mixed results of the economic impact of virtual care and TH. Largely missing from the literature are studies that identify the cost of delivering TH versus in-person care. The objective was to demonstrate a modified time-driven activity-based costing (TDABC) approach to compare weighted labor cost of an in-person pediatric clinic sick visit before COVID-19 to the same virtual and in-person sick-visit during COVID-19.
Methods:
We examined visits before and during COVID-19 using: (1) recorded structured interviews with providers; (2) iterative workflow mapping; (3) electronic health records time stamps for validation; (4) standard cost weights for wages; and (5) clinic CPT billing code mix for complexity weighs. We examined the variability in estimated time using a decision tree model and Monte Carlo simulations.
Results:
Workflow charts were created for the clinic before COVID-19 and during COVID-19. Using TDABC and simulations for varying time, the weighted cost of clinic labor for sick visit before COVID-19 was $54.47 versus $51.55 during COVID-19.
Discussion:
The estimated mean labor cost for care during the pandemic has not changed from the pre-COVID period; however, this lack of a difference is largely because of the increased use of TH.
Conclusions
: Our TDABC approach is feasible to use under virtual working conditions; requires minimal provider time for execution; and generates detailed cost estimates that have “face validity” with providers and are relevant for economic evaluation.
Keywords: TDABC, costing, telehealth, telemedicine, COVID
Introduction
When the COVID-19 pandemic struck, telehealth (TH) and virtual visits became essential for both patients and providers. The urgent need to convert in-person care to TH meant few health systems had time to plan and be deliberate in their TH approach. TH programs already in place were scaled-up quickly and improvisations were common. We are now at a stage where we must make strategic decisions for a streamlined, sustainable TH approach and identify the best opportunities for improvement. The cost and value of TH services developed during the pandemic scale-up should inform our choices. Unfortunately, cost/economic studies of TH are few and report mixed results of the economic impact of virtual care and TH. Reports include large variations in prices,1 increased overall cost of care owing to “convenience” effect of virtual visits,2 and cost savings accrued from reduced travel time, improved triage, and access to timely care.3
These published studies report costs from the perspective of patients, payers, and populations. Largely missing from the literature are studies that identify the cost of delivering TH versus in-person care from a provider perspective. As health care costs increase at alarming rates, there is a need to have accurate information when making decisions based on the value (cost-effectiveness) of health interventions and health care processes. Decision makers must determine the most efficient allocation of limited resources while delivering the best quality of care. Cost analysis can be assessed using a top-down approach or a bottom-up approach.
Typically cost analysis was evaluated using a top-down approach to allocate indirect costs (e.g., physical facility, equipment, and utilities) based on a predetermined cost driver; this method may distribute costs across departments in a hierarchical system centered on revenue or through weighting procedures, such as, Medicare's Relative Value Units (RVUs) established by the intensity of the procedure. This top-down approach provides an average cost per patient that depends on the institution's historical production flows and skewed by factors aiming at maximizing reimbursement, thus, may not be representative of the true costs of care4,5 and are difficult to apply to virtual visits.
The true cost of a care process usually requires a micro-costing approach to measure. A bottom-up approach, micro-costing establishes patient-specific resource use directly attributed to actual diagnostics, devices, and drugs used in treatment and patient-specific treatment times to determine actual labor resources use.4,6 This more detailed level of costing provides the ability to identify subpopulations (e.g., race, comorbidity, and age group) most affected by costs.6 Time-driven activity-based costing (TDABC) is a less frequently used micro-costing methodology that identifies costs of production using service-specific activity and resource use evaluated with patient-specific treatment times.4,6,7
Literature suggests that TDABC is an effective method to find true costs that can be used to identify inefficiencies and cost drivers within processes. This precise method of costing was used to address a concern that health care administrators were emphasizing blood transfusions over other alternatives based on a misconception of actual cost, affecting quality of care.
The researchers determined the true costs of blood transfusions, using TDABC to include the costs of acquiring and administrating, were much costlier than the mean acquisition costs used by administrators to inform clinical process decisions.8 At a children's hospital, TDABC and process mapping identified an area to improve efficiency by the addition of a physician assistant that decreased patient waiting times and increased revenue; similar results were found when a psychiatrist in Norway used the process to analyze the efficiency of his clinic and discovered a need to modify the care process, resulting in better outcomes and improved capacity.9
A preoperative assessment center applied TDABC methods to evaluate the two-phase implementation of a process improvement initiative that ultimately reduced process time by 33% and cut cost of care by almost half, without negatively impacting outcomes.10 The TDABC method has been utilized to inform clinical process decisions and identify areas for process improvement, although, it is resource intensive to perform8 because it requires research staff to be present in the clinic to observe and record the care processes using a stopwatch to collect minute data on the process.
A solution to this barrier of traditional TDABC could be through the modification of the data collection using structured interviews and electronic health records (EHR), providing a more efficient approach to record times of the sequence of events through electronic time stamps to implement TDABC. EHR activity logs have been effectively utilized to evaluate quality and efficiency of workflow and process of care.11–13
The objective of this project was to demonstrate the use of a modified TDABC approach to compare the weighted labor costs of an in-person clinic sick visit before COVID-19 to the mix of in-person and TH clinic sick visit during the COVID-19 pandemic in a pediatric clinic.
Methods
We assessed cost of providing an in-person versus mix of TH and in-person sick visits at a pediatric clinic in a suburban area. The study met institutional definition of a quality improvement project and did not require IRB oversight. A mixed methods approach was used for data collection and analysis to perform a modified TDABC of a sick visit that could be assessed in a virtual environment.
A sick visit was defined as a low complexity clinic visit for established patients (Current Procedural Terminology [CPT] 99213), classified as a 15-min face-to-face visit. This low complexity clinic visit includes a limited examination of the affected body area or organ system and low-level medical decision making. Examples of this type would be a sick visit for an ear infection or strep throat. Visits were described for children between the ages of 5–9 years. The TDABC steps included the following: (1) recorded structured interviews with providers, (2) iterative workflow mapping, (3) EHR timestamps for time validation, (4) standard cost weights for wages, (5) clinic CPT billing code mix for complexity weights, and (6) simulations to assess effects of uncertainty on cost differences.
INTERVIEW DATA
Structured interviews were used to collect data to map the care process of a sick clinic visit for an established patient age of 5–9 years. An interview guide with five questions with probes was used (eAppendix A in Supplementary Data). Interviews were conducted by two interviewers familiar with the workflow and EHR system. Two providers were interviewed separately: a physician and a nurse practitioner (NP). Both interviewers were present for both sessions and the interviews were recorded.
The recorded interviews were processed with Rapid Qualitative Analysis,14 which uses repeated listening by each researcher to the recorded interviews to each develop their version of the workflow charts. The charts were then revised using joint iterative review of recordings for the researchers reach consensus on clinic flow graphics. The resulting flow charts were reviewed and edited as needed by the providers who then gave final approval of their position-relevant charts.
EHR DATA
Two independent sources of data from the clinic were used to extract time stamps of the process for clinic visits with CPT 99213. Mean (standard deviation [SD]) in minute values were used to validate the providers' minute estimates from the interviews in the clinic flow charts. One source of process validation data was extracted from the EPIC TH dashboard, used by practice managers and TH personnel to monitor the processes in the clinic. Data were extracted for all clinic pediatric patients with a low complexity clinic visit (CPT 99213) seen during September 2020. These data included the timestamps for check-in, treatment start time, provider treatment team composition (i.e., physician or NP), record access by each actor, and printing timestamp used by providers to present a visit summary and care plan for patients at the end of the visit.
A second source of data was extracted from the EPIC Clarity Warehouse, which included all CPT 99213 clinic visits in September 2019 and September 2020. These data included the clinic provider (i.e., MD or NP) and method of visit delivery (i.e., in-person or TH) and were used to validate provider mix (i.e., percentage of visits seen by physician and NP) and delivery method mix (i.e., percentage of visits seen in-person or by TH) to be used for estimating visit costs.
WORKFLOW MAPPING CONVENTIONS APPLIED
The clinic flow mapping process for patients utilizing the clinic for a sick visit, from signing-in at the beginning of the appointment to the conclusion of the clinic visit, began with the review of the recorded interviews. Identification of each step in the process was completed along with the determination of actors (e.g., physician, NP, nurse, and front desk personnel) and approximate time in minutes to complete each step. Three workflow charts were then developed for (1) in-person clinic visits before COVID-19, (2) TH clinic visits during COVID-19, and (3) in-person clinic visits during COVID-19. For each of the workflow charts, steps of the process (identified by a square) are organized by the order in which they are completed.
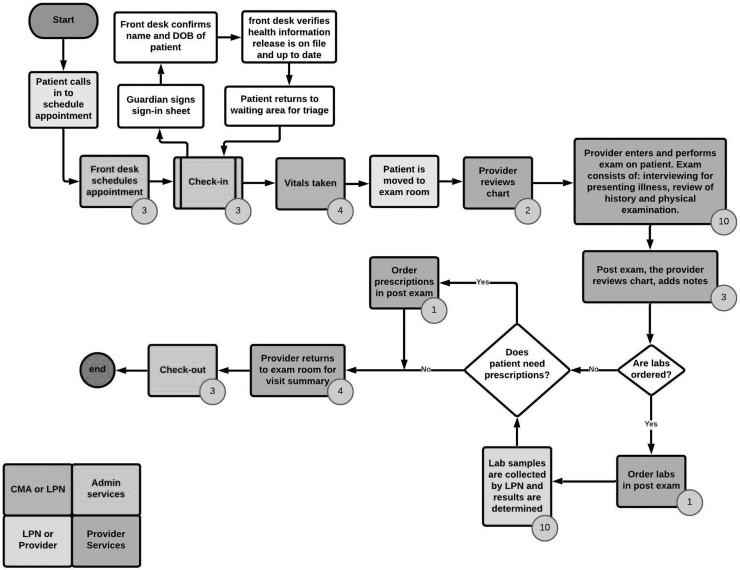
Potential additional or alternative steps were identified with decision nodes (diamond) in the flow chart. For each step of the process, the average time to complete is noted (contained within small circle in bottom right corner of squares), and actors involved (color-coded) were identified and listed. The three workflow charts were created from each interview, and then the interviews were reviewed again to make edits to the workflow charts. The two interviewers then met to review the workflow charts and both interviewers agreed on the construction of the charts (Fig. 1).
Fig. 1.
Workflow chart for in-person clinic visits before COVID.
The workflow chart was reviewed while listening to the recorded interviews and checked to be sure there were no missing connections and then returned to the interviewees for verification of accuracy. Once any suggested edits were completed, the interviewers reviewed the recorded interviews to ensure the accuracy of the workflow charts. This process was repeated as analysis of minutes and cost were conducted. The workflow charts generated by the physician and NP were combined to create a single clinic process workflow chart for each visit type before and during COVID-19.
To validate the workflow process and time estimates of the chart for TDABC, the electronic timestamps of patient EHR access by actors during the visit were used as a proxy to establish contact time of actors with the patient. This is the step that replaces in-clinic time estimation in traditional TDABC and makes this a modified TDABC approach.
WORKFLOW COST CALCULATION
Using TDABC costing methods, the labor cost of care was estimated for in-person clinic visits before COVID-19 and the TH and in-person clinic visits during COVID-19 (Fig. 1). Labor costs were calculated using median U.S. salaries for each individual using the U.S. Bureau of Labor Statistics salary data for 2019. Total loaded salary for each individual was calculated as median salary plus fringe benefits, equal to 35% of the median salary. A total of 2,080 annual hours worked were assumed for a full-time employee; a position-specific work capacity rate was applied: (1) nursing (e.g., Licensed Practical Nurse [LPN] and Certified Medical Assistant [CMA]) and administration staff at 80% (1,664 h) and (2) for provider (e.g., pediatrician and NP) at 72.3% (1,504 h).
The cost per minute for each individual was calculated as the total loaded salary divided by the number of minutes from capacity hours per year. For process steps that were either completed by two different actors or may potentially be completed by two different actors, as identified in the workflow chart, a 50/50 weight was given to each individual's salary to estimate the cost per minute for the time in the mixed process step.
The cost of each individual for the visit was determined by the total minutes utilized multiplied by the cost per minute for the individual. For in-person and TH sick visit, the labor costs across all individuals were summed to determine the total labor cost of the clinic visit. To account for potential technical difficulties in providers' time during TH visits, the estimated time for linkage and/or phone number issues in the workflow chart were included in the providers' time at a rate of 5%, as providers reported this issue only about once a month. Analysis of labor cost was conducted using Microsoft Excel.
SIMULATIONS
Monte Carlo simulations were developed using the minutes estimated from the workflow chart to mimic the expected variation of labor minutes by the providers and staff, thus the variation of total labor cost, in the clinic setting. The provider time was simulated using a Weibull distribution identified by Medicare specified range for the given visit type.15
All other staff time was modeled on a Beta PERT distribution defined by a “most likely” value (estimated time from the flow chart) and a minimum and maximum value (±10% of the estimated time). Median salary for individuals varied on a normal distribution with 10% of the median salary for the SD. The variation in minutes and cost per minute for actors provided a distribution of costs across 100,000 visits for in-person visits before COVID and TH and in-person visits during COVID. Simulations were conducted using Crystal Ball software.
FINAL COSTING AND DECISION TREE
EHR data extracted from EPIC were used to identify and categorize providers to determine a provider mix for the same week in September for 2019 and 2020. Providers for each of the clinic visits were categorized as physician or NP. Decision trees were estimate mean costs for mixtures of providers delivery method mix (in-person or TH visit).
COST COMPARISON
Mean and SDs of forecasted visit cost estimated by simulations were evaluated for differences between before COVID and during COVID. Minimally important difference (MID) measured by a well-defined anchor has been identified as a conservative effect size for low-cost studies.16 The MID was anchored based on the relationship of clinic reimbursement between the low complexity sick visit (CPT 99213), defined as a 15-min face-to-face clinic visit, and the moderate complexity sick visit (CPT 99214), defined as a 25-min face-to-face clinic visit. The median Medicare medical fee in 2017 was $125 and $184, for low and moderate complexity visits, respectively. The adjacent CPT visits provided a meaningful payment difference of $59.
Results
WORKFLOW CHART
Workflow charts capturing visit resource use estimates before COVID-19 were similar in process and time for each provider. The combined workflow used an average of estimated times for each step where times differed. In addition, the workflow charts for each provider of a TH visit during COVID-19 were almost identical. However, the workflow created for an in-person clinic visit during COVID-19 had variations in the process. The risk of a patient with a suspected COVID-19 infection for the in-person clinic sick visits during the COVID-19 phase had the greatest variation that depended on need for use of personal protective equipment (PPE). We chose to use the most conservative process for time estimates (i.e., assuming donning and doffing PPE for each encounter instead of remaining in the same PPE all day).
Before COVID-19, the estimated time a provider was involved in the clinic visit between treatment start time and visit summary printing was 19 min; however, the laboratory steps were excluded as it was billed separately and not included in the basic clinic costs. The average time for an LPN or CMA was 4 min and medical office assistant was 9 min, providing a total labor time of 32 min.
TH clinic visits during COVID-19 involved only providers after initial check-in by the administration staff (∼3 min). The estimated total labor minutes were 18, unless the provider encountered internet link issues with the patient that required them to verify information and assist patient with the connection. However, some TH visits were aborted. If it was determined during the TH visit that the patient needs to be seen in-person then the TH visit was canceled so that the patient does not get billed twice. However, labor costs were still accrued and allocated across all TH visits. The provider must conduct the TH assessment, schedule an in-person visit, and provide notes for the in-person clinic provider who will be seeing the patient. This unbilled visit takes an estimated 21 min of the provider's time (eFig. 1 in Supplementary Data).
The clinic process for an in-person visit during COVID-19 for a non-COVID risk patient was almost identical to the process before COVID-19. However, the in-person clinic visit with a COVID risk resulted in less overall labor time because of fewer actors being involved. These visits were completed by the provider alone to reduce staff COVID exposure. The estimated labor time for the process was 18–19 min, regardless of the method of delivery or the effect of the pandemic (eFig. 2 in Supplementary Data).
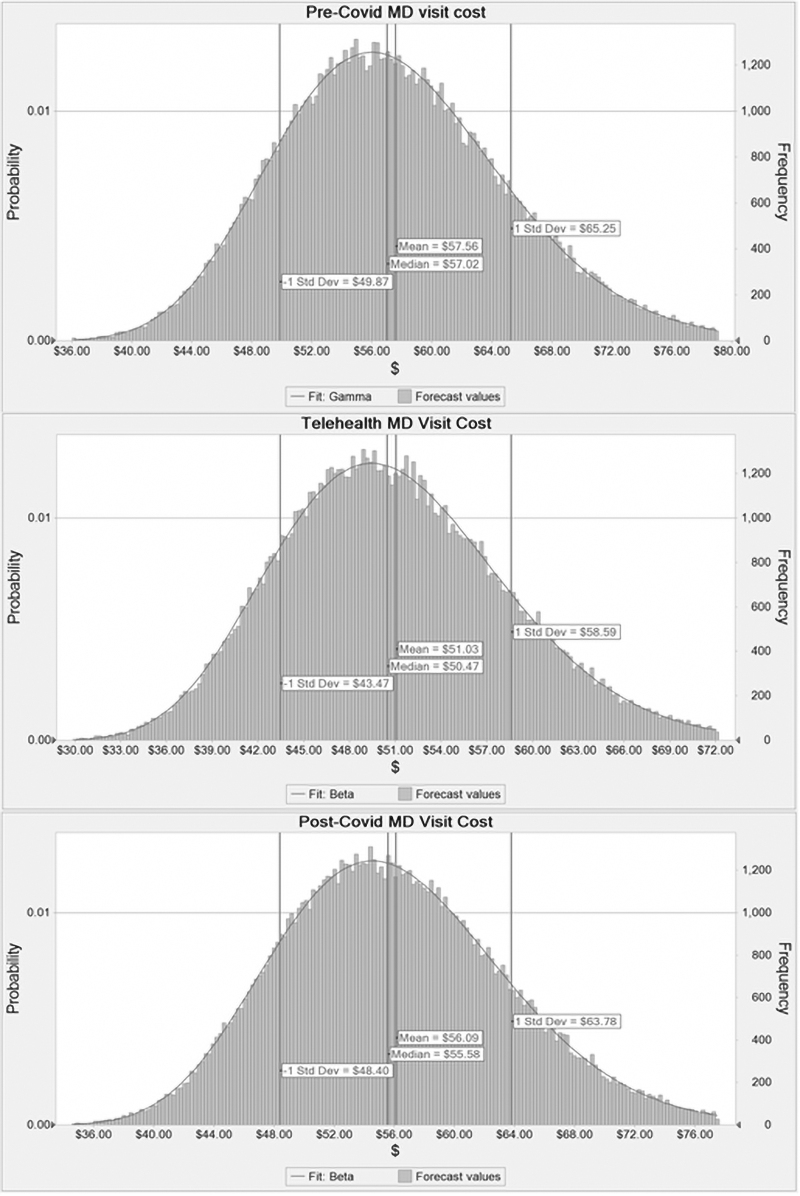
Fig. 2.
Distribution of Monte Carlo simulations for MD.
VISIT COST CALCULATION
Total loaded salary and cost per minute for each actor were calculated from median U.S. salaries (Table 1). Using TDABC methods, the labor cost for a sick clinic visit was calculated using established workflow charts (Table 2). The labor costs for in-person visits before and during the pandemic were similar; however, the process became more efficient during the pandemic and results in a slightly lower labor cost ($56.16 vs. $54.68 for a physician and $38.23 vs. $31.63 for NP, before COVID and during COVID pandemic, respectively). Although TH visits were mostly restricted to only provider time, the provider spent almost the same time on the visit but the elimination of additional actors resulted in lower labor costs ($49.61 and $31.63 for a physician and NP, respectively).
Table 1.
Median Salary Costs and Cost/Minute (USD) for Actors in Clinic Care Process
| ROLE | MEDIAN SALARY | FRINGE | LOADED SALARY | ANNUAL HOURS | COST/MIN |
|---|---|---|---|---|---|
| Pediatric physician | $175,300 | $61,355 | $236,655 | 1,504 | $2.62 |
| Pediatric nurse practitioner | $109,800 | $38,430 | $148,230 | 1,504 | $1.64 |
| CMA | $34,800 | $12,180 | $46,980 | 1,664 | $0.47 |
| LPN | $47,500 | $16,625 | $64,125 | 1,664 | $0.64 |
| Medical office assistant | $36,600 | $12,810 | $49,410 | 1,664 | $0.49 |
CMA, Certified Medical Assistant; LPN, Licensed Practical Nurse.
Table 2.
Labor Costs Estimated for Clinic Visits from Workflow Chart and Simulation of 100,000 Visits (USD)
| VISIT TYPE/PROVIDER | FLOW CHART |
MONTE CARLO SIMULATIONS |
||||
|---|---|---|---|---|---|---|
| TOTAL STAFF MINUTES | TOTAL PROVIDER MINUES | LABOR COST | MEAN | SD | FIT DISTRIBUTION | |
| Before COVID-19 | ||||||
| In-person with MD | 13 | 19 | $56.16 | $57.56 | $7.69 | Gamma |
| In-person with NP | 13 | 19 | $38.23 | $39.10 | $4.83 | Gamma |
| During COVID-19 | ||||||
| Telehealth with MD | 3 | 18.35a | $49.61 | $51.03 | $7.56 | Beta |
| Telehealth with NP | 3 | 18.35a | $31.63 | $32.49 | $4.72 | Beta |
| In-person with MD | 10 | 19 | $54.68 | $56.09 | $7.69 | Beta |
| In-person with NP | 10 | 19 | $36.75 | $37.60 | $4.82 | Gamma |
Link and telephone issues assessed at 5% of visits.
NP, nurse practitioner; SD, standard deviation.
SIMULATIONS
We used Monte Carlo simulations executed in Excel with a Crystal Ball extension specifying 100,000 estimates to examine the effect of potential variations in minute and costs on the estimates. Table 2 provides the mean and SD from the Monte Carlo simulations developed with the distribution the labor costs fit for each of the three workflows assessed under the MD and NP teams. For clinic visit costs before COVID, provider minutes varied by 14.7 min and higher with the distribution from the simulations of visit labor costs for MD ranging from $36 to $80 (Fig. 2). The clinic visit costs for TH during COVID had a lower cost range for MD visit costs than in-person visits (Fig. 2). For the estimated in-person clinic visit costs, the distribution for the MD in-person visit costs had a slightly narrower range during COVID than before COVID (Fig. 2).
FINAL COSTING AND DECISION TREE
The provider mix at the clinic was identified from EHR as 83.2% MD and 16.8% NP for visits (eFig. 3 in Supplementary Data). Using this provider mix with the estimated costs, the mean weighted clinic cost per visit was $54.47 ($47.26–$61.68 within 1 SD) before COVID (Table 3). During COVID, the delivery method mix identified from EHR of 28.3% TH and 71.7% in-person was added to the decision tree to provide an overall weighted labor cost across both provider mix and delivery mix per visit of $51.55 ($44.38–$58.73 within 1 SD). The difference in mean weighted visit costs were well below the MID of $59 that we had specified as important for this study.
Table 3.
Weighted Labor Costs Forecast by Monte Carlo Simulations (USD)
| 1 SD BELOW MEAN | MEAN | 1 SD ABOVE MEAN | |
|---|---|---|---|
| Before COVID-19 | 47.26 | 54.47 | 61.68 |
| During COVID-19 | 44.38 | 51.55 | 58.73 |
| Difference | 2.88 | 2.92 | 2.95 |
Discussion
This study has demonstrated that using our modification of TDABC the estimated mean labor cost for care during the pandemic has not changed from the pre-COVID period. This lack of a difference is largely owing to the increased use of TH, which reduced provider time by allowing them to perform several tasks simultaneously, such as chart review, during their virtual encounters instead of before entering the exam room. However, our results indicate that TH may actually be underutilized.
In addition, the mix of physician and NP providers should be examined to assure that the optimal mix is present for the clinic's patient severity mix. Our TDABC approach can provide the cost data needed to inform important discussions of (1) which TH programs to maintain; (2) how best to improve TH efficiency; and (3) which factors in a clinic's workflow can be changed to achieve the most efficient mix of TH and in-person visits.
Furthermore, we found that simulations were simple to execute in Excel and were valuable for illustrating the effect of uncertainty in estimates but that it is important to use the correct distributional assumptions for the simulations or the results may be misleading. We used the assumptions embedded in the CMS specifications of expected ranges of minutes for a CPT code. Our simulation results replicate what CMS specifies to be resource ranges that are acceptable for reimbursement of provider time. Thus, this approach to choosing distributions for simulations could be useful if applied to other visit types. Implementing the approach across multiple clinics can provide a better assessment of an estimated delivery method mix and provider mix that would optimize labor resources and reimbursement while providing quality care.
Use of TDABC in TH is not yet common, but it appears to have great potential. Cidav and colleagues used TDABC to cost an ostomy TH training process for use in cost-effectiveness analysis for a clinical trial.17 Zanotto et al. used TDABC for costing ophthalmology visits in primary care based on 2 weeks of visual observation of the care process, and reports that “the TDABC process deserves more prominence as it allows us to retrieve more accurate cost of technology.”18 However, neither of these studies used EHR time-stamp data to validate their process flow chart estimates.
LIMITATIONS
A limitation of our analysis was the inability to account for the number of TH visits that were aborted because the provider decided that the problem warranted an in-person visit. An increase in this rate would increase the weighted labor cost during COVID. To examine the effect of this factor we performed a sensitivity analysis. Assuming an 80/20 mix of TH and aborted TH to in-person in the decision tree, the mean weighted visit cost during COVID would be $54.47, the same mean weighted visit cost as observed before COVID. However, if we assume the addition of a 20% aborted TH visit to in-person visit to the decision tree resulted in the identified 28.3/71.7 delivery method mix seen, the true delivery method would actually have a rate of 35.5/64.5 with a mean weighted visit cost during COVID being $54.84.
Conclusions
As health care providers plan for sustained TH operations, our modified TDABC approach may be helpful. This approach is feasible to use under virtual working conditions, requires minimal provider time, can be implemented quickly, captures important variations in the process of care that affect costs, and generates detailed cost estimates that have “face validity” with providers and are relevant for process improvement and economic evaluation. It addresses the barrier to the practical use of TDABC by avoiding direct observation and replacing observed time with EHR time stamp analysis. This reduces resources required to complete the analysis and makes it implementable for processes that take place in our current “virtual” environment.
Although no cost difference was found in this study during the pandemic, on the other side of cost allocation that is beyond the scope of this research, is the ever-evolving TH reimbursement, which may also impact choice of TH or in-person visits.
Supplementary Material
Acknowledgments
The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services (HHS) or the U.S. Government.
Authors' Contributions
All authors made substantial contributions to the conception and design of the work. M.J.D., K.N.S., K.K., and J.T.M. contributed to the acquisition of data, M.J.D. and K.N.S. conducted all analysis, and all authors contributed to the interpretation of data. Drafting of the article was conducted by M.J.D. and K.N.S. with all authors revising the article critically for important intellectual content. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure Statement
Authors have no competing interests, personal financial interests, funding, employment, or other competing interests to disclose.
Funding Information
This publication was supported by the HRSA of the HHS as part of the National Telehealth Center of Excellence Award (U66 RH31458-01-00). Data analytic support for the study was provided through the CEDAR core funded by the MUSC Office of the Provost and by the South Carolina Clinical and Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, through NIH Grant No. UL1 RR029882 and UL1 TR001450.
Supplementary Material
REFERENCES
- 1. Nguyen A. How much does a telemedicine visit cost? A price comparison chart. March 26, 2020. Available at https://www.goodrx.com/blog/telemedicine-true-cost-and-telehealth-price-comparison-chart (last accessed February 25, 2021).
- 2. Jain T, Mehrotra A. A comparison of direct-to-consumer telemedicine visits with primary care visits. JAMA Net Open 2020;3:e2028392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hooshmand M, Foronda C. Comparison of telemedicine to traditional face-to-face care for children with special needs: A quasi experimental study. Telemed J E Health 2018;24:433–441. [DOI] [PubMed] [Google Scholar]
- 4. Carroll N, Lord J. The growing importance of cost accounting for hospitals. J Health Care Finance 2016;43:172–185. [PMC free article] [PubMed] [Google Scholar]
- 5. Zilberberg M, Shorr A. Understanding cost-effectiveness. Clin Microbiol Infect 2010;16:1707–1712. [DOI] [PubMed] [Google Scholar]
- 6. Tan S, Rutten F, van Ineveld B, Redekop W, Roijen L. Comparing methodologies for the cost estimation of hospital services. Eur J Health Econ 2009;10:39–45. [DOI] [PubMed] [Google Scholar]
- 7. Gammon E, Cotton A. The efficacy of activity-based accounting techniques for target case management in outpatient settings. J Health Care Finance 2016;43:2–12. [Google Scholar]
- 8. Shander A, Hofmann A, Ozawa S, Theusinger O, Gombotz H, Spahn D. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion 2010;50:753–765. [DOI] [PubMed] [Google Scholar]
- 9. Kaplan R, Witkowski M. Better accounting transforms health care delivery. Accounting Horizons 2014;28:365–383. [Google Scholar]
- 10. French K, Albright H, Frenzel J, Incalcaterra J, Rubio A, Jones J, Feeley T. Measuring the value of process improvement initiatives in a preoperative assessment center using time-driven activity-based costing. Healthcare 2013;1:136–142. [DOI] [PubMed] [Google Scholar]
- 11. Mans R, Schonenberg H, Leonardi G, Panzarasa S, Cavallini A, Quaglini S, van der Aalst W. Process mining techniques: An application to stroke care. Stud Health Technol Inform 2008;136:573–578. [PubMed] [Google Scholar]
- 12. Chen Y, Xie W, Gunter C, Liebovitz D, Mehrotra S, Zhang H, Malin B. Inferring clinical workflow efficiency via electronic medical record utilization. AMIA Annu Symp Proc 2015;2015:416–425. [PMC free article] [PubMed] [Google Scholar]
- 13. Wu D, Smart N, Ciemins E, Lanham H, Lindberg C, Zheng K. Using EHR audit trial logs to analyze clinical workflow: A case study from community-based ambulatory clinics. AMIA Annu Symp Proc 2018;2017:1820–1827. [PMC free article] [PubMed] [Google Scholar]
- 14. Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open 2018;8:e019993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Medicare and Medicaid Services, CMS.gov. November 23, 2020. Available at https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-federal-regulation-notices/cms-1734-f (last accessed December 3, 2021).
- 16. Dooley M, Simpson AN, Nietert PJ, Williams D Jr., Simpson KN. Minimally important difference in cost savings: Is it possible to identify an MID for cost savings? Health Serv Outcomes Res Methodol 2021. [Epub ahead of print]; DOI: 10.1007/s10742-020-00233-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cidav Z, Marcus S, Mandell D, et al. Programatic costs of the telehealth ostomy self-management training: An application of time-driven activity-based costing. Value Health 2021;24:1245–1253. [DOI] [PubMed] [Google Scholar]
- 18. Zanotto BS, Beck AP, Siqueira AC, et al. Economic evaluation of a telemedicine service to expand primary health care in Rio Grande do Sul: Teleoftalmo's microcosting analysis. Cien Saude Colet 2020;25:1349–1360. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.