Abstract
The school of social vulnerability in disaster sciences offers an alternative perspective on the current COVID-19 (coronavirus) pandemic crisis. Social vulnerability in general can be understood as a risk of exposure to hazard impacts, where vulnerability is embedded in the normal functioning of the society. The COVID-19 pandemic has exposed systemic (political and health care systems), demographic (aging, race) and,based on the results of our approach, spatial (spatial isolation and connectivity) yvulnerabilities as well. In this paper, we develop a risk prediction model based on two composite indicators of social vulnerability. These indicators reflect the two main contrasting risks associated with COVID-19, demographic vulnerability and, as consequences of the lockdowns, economic vulnerability. We conceptualise social vulnerability in the context of the extremely uneven spatial population distribution in Australia. Our approach helps extend understanding about the role of spatiality in the current pandemic disaster.
Keywords: Social vulnerability, Disaster risk, COVID-19 pandemic, Australia, Sparsely populated area
Graphical abstract
1. Introduction
The school of social vulnerability in disaster science offers valuable perspectives on the current COVID-19 (coronavirus) pandemic [1]. Social vulnerability in general can be understood as a form of risk exposure to a disaster, where vulnerability is embedded in the normal functioning of the society. To date, social vulnerability in relation to the global COVID-19 pandemic has been interpreted in terms of its systemic (policy, political and health care systems [[2], [3], [4]]), demographic [[5], [6], [7]], inequality [[8], [9], [10]] and spatial dimensions [[11], [12], [13]].
A social vulnerability lens on the COVID-19 pandemic would postulate that, while its origins were the sudden and unanticipated transmission of the virus from animals to humans, and its subsequent spread, its impacts have propagated through populations according to the highest relative levels of social vulnerability. While both hazard and vulnerability related to risk exposure in disaster (see Cardona [14], the main objective of this research is to develop and analyse social vulnerability composite indices for Australia to investigate the varying spatial risk from COVID-19 based on socio-cultural population determinants such as race, ethnicity, age and gender. It is our view that social vulnerability has not only a demographic-health component arising from the respiratory illness itself, but also a socio-economic dimension from the effects of lockdown efforts in disrupting normal economic activity and challenging the physical and mental wellbeing of those affected.
In Australia population distributions are highly uneven and characterised by significant urbanisation which is in contrast to the sparsely populated or ‘Outback’ areas of the nation. Demographic compositions are also highly diverse according to age, gender, race and other important variables [15,16]. While, relative to other areas, sparsely populated areas in Australia tend to have less per capita COVID-19 case numbers [17] they are also characterised by a significant proportion of vulnerable populations [18,19]. We argue, that the lower per capita case numbers could be explained by the spatial variation of social vulnerability, which is more complex in its composition than simply the difference in population densities. For these reasons we analyse social vulnerability using a human geographical approach, linking it to the spatial diversity of the population within Australia with a particular emphasis on its sparsely populated ‘edges’ to understand how spatial diversity in population compositions affect levels of social vulnerabilities.
In the first section of this paper we review the literature on social vulnerability and disasters. We then look at how social vulnerabilities expose risks in the current pandemic before developing a model for analysing the complex nature of these vulnerabilities, particularly in relation to their spatial diversity within Australia. Finally we discuss the results in relation to spatial analysis methods and disaster mitigation policies.
2. The effects of a disaster: when, where, and who is impacted?
In the initial global media coverage of the emergence of the COVID-19 pandemic, there was a great deal of discussion regarding the hazard event, with a focus on the role played by wet markets in Asia, particularly those in Wuhan, China [[20], [21], [22]]. Indeed, Parrish et al. [23]; Chan et al. [24] and Geoghegan et al. [25] argue that the risk of virus transmission by anthroponosis is globally increasing through the effects of habitat destruction, climate change, and the increase of populations living in hazard-prone areas, particularly the crowded megacities within developing nations [[26], [27], [28]].
Beyond the mitigation of impacts of the hazard event, in this case the transmission and the subsequent spread of the coronavirus [29], there exists an additional factor determining risk exposure; namely social vulnerability, and its variations according to demographic and social composition of the populations at different locations. Furthermore, instead of viewing disasters as ‘non-routine events’ (see Drabek [30] creating non-routine social problems, Blaikie et al. [31] and Wisner et al. [32] argue that disasters are embedded in the ‘normal’ functioning of society and are rooted in social inequalities. For these reasons, they emphasise the role which social, political and economic structures play in different levels of vulnerability. Their work has helped shift the understanding of disasters as extreme and unusual events to an expression of the vulnerability of human-social systems which themselves vary across space. As Cutter [33] has stated, disasters are not events but a reflection of society's vulnerability to environmental threats and extreme shocks. Oliver-Smith [34] similarly argued that “… social systems generate the conditions that place people […] at different levels of risk from the same hazard and subject to different forms of suffering from the same event” (p. 120).
Social vulnerability perspectives in the analysis of disasters emphasises that the scale and timing of impacts are inherently a function of social circumstances, which in turn determine who (individuals, social groups, communities etc.) is at risk and who is impacted [31,32]. Thus, the hazard event is a trigger which exposes pre-existing vulnerabilities generated by power-law relationships as well as underlying social and economic inequalities [32,35].
This paper is therefore premised on the view that the course of the current COVID-19 pandemic is strongly influenced by spatially-determined vulnerabilities which are a result of diversity in the demographic and geographic composition of Australia's population. In this respect, the COVID-19 pandemic has exacerbated pre-existing social inequalities [36]), exposed systemic (political and health care systems), population (aging) and spatial (spatial isolation and connectivity) vulnerabilities which have strongly influenced varying mortality rates between and within individual nations [37]. From this perspective, clinical and biomedical efforts to prevent, monitor and understand the transmission and mortality effects of the coronavirus can be seen as secondary responses to the primary effect of systemic social and economic vulnerabilities [38]). For example, health systems which, in the lead-up to 2020 had relatively less funding on which they could modernised or improve have been exposed for their lack of ability to cope with the challenges posed by the coronavirus [35,36]. In Australia, this is thought to be the critical reason the jurisdiction of Victoria had a significant ‘second wave’ with more deaths than the rest of the nation combined [39]. Countries which have sustained investment into advancing health care systems, such as Germany and Taiwan, however, have sufficient capacity to deal with caseloads [3,4]. In contrast, in the USA, which does not have a universal healthcare program and detrimentally suffered from mixed messages on population movements and containment measures between federal and state levels [40], the virus has disproportionally impacted on the poorer African American community living in congested metropolitan areas [[41], [42], [43], [44]].
Likewise, morbidity and mortality rates are disproportionately higher for older people for reasons that are more than just biological [45]. Gray and his co-authors [46] and Patel et al. [5] highlighted that engrained social inequalities mean some sub-sections of populations are more vulnerable to COVID-19. According to Fernandez et al. [47]; population ageing in developed countries is establishing age-related vulnerability enclaves which are particularly at risk in the current disaster. Additionally, some elderly have an elevated chance of exposure to the virus as residents in crowded and underfunded aged care facilities [6,7]. The pandemic has, therefore, exposed a long-term underlying neglect of the social and physical wellbeing of the aged in some countries, including Australia [7,48].
Along with characteristic demographic variables such as age, race and sex composition, dynamic demographic factors, in particular migration, also contribute to vulnerability. For instance, people such as refugees, internally displaced, tourists, and migrant workers may be particularly vulnerable to disasters [26,49]. During the current pandemic, there has been a resurgence in coronavirus cases among migrant workers [50,51], particularly in Singapore where they are accommodated in crowded dormitories [52] and among displaced people [53] such as the Rohingya refugees in Bangladesh [[54], [55], [56]]. Non-citizen populations may also be exposed to negative impacts on mental wellbeing or welfare. In Australia, for example, international students were not eligible for welfare assistance programmes provided to the general population by the Australian Government and were asked to leave by the Australian Prime Minister [57]. This mostly affected urban dwellers, particularly higher education sector students.
Spatially, sparsely populated and remote areas in developed nations have long exhibited lower health outcomes than for city-based residents [19]. In Australia, many remote regions are also characterised by highly mobile populations, including mobile Indigenous residents [58,59], which makes them vulnerable to viruses which are spread by human contact [2]). For Indigenous people, the risk of devastating impacts from the pandemic are evident from disproportionate rates of chronic health conditions including kidney infections and heart conditions [18]. Recognising this, in March 2020 the Prime Minister of Australia enacted the Biosecurity Act to effectively ban movements in to and out of 76 remote Indigenous communities in the jurisdiction of the Northern Territory, where around 80% of the population outside the main cities and towns are Indigenous [60]). Economically, many businesses in sparsely populated areas have been significantly impacted because they are more reliant on mobile populations including tourists and seasonal workers.
The examples provided thus far highlight that, from the social vulnerability point of view, case fatality rates from COVID-19 (the ratio of deaths to the number of confirmed cases), while important and the focus of most media attention on the pandemic, do not reveal the underlying social and spatial determinants of vulnerabilities in sub-populations [13]. Consequently, epistemological and ontological debates concerning high variations in COVID-19 mortality rates across countries cannot be resolved without understanding social vulnerability [37] since mortality rates are primarily determined by the age distribution and social status of the population [35]. These phenomena related to population composition, distribution and mobility highlight the importance of the intersection of demography and geography in the analysis of COVID-19 vulnerability. The geographical diversity of populations in Australia makes it challenging to encompass this vulnerability within a universal model.
Current literature on the COVID-19 pandemic has explored social vulnerability in what can be summarised as two main ways (see Table 1 ). The first is post-event analysis of actual case numbers and deaths as dependent variables and their correlations with vulnerabilities as independent variables. The second approach are prediction models which attempt to estimate future risk exposures as determined by risk factors (vulnerabilities). During the first wave of the pandemic the number of coronavirus cases in Australia was small compared to other nations [17] as a result of its distance from the global pandemic epicentres as well as the early adoption of a suppression strategy through both the closure of its international and internal borders and travel restrictions. The small number of cases of community transmission has meant that the data on per capita infection rates within small-area units are too ‘noisy’ to apply a post-event analysis of social vulnerability using methods such as multivariate regression. Consequently, in this paper, we have developed a spatially focused social vulnerability model to predict risk exposures by creating two composite indicators of social vulnerability to COVID-19 using Australian data. In the following section we outline the methods and data applied to developing this model.
Table 1.
Methods for spatial analyses of COVID-19 related social vulnerability.
| Author(s) | Aim | Methods | Results | |
|---|---|---|---|---|
| Index for identification of vulnerable areas and groups (risk prediction) | Acharya, Porwal [61] | Identification of vulnerable regions in India | Creating composite index by percentile ranking | There are some unclear connections between predicted vulnerabilities and actual spread |
| Amram et al. [62] | Small area vulnerability index (Washington state, USA) | Multilevel modelling of socio-demographic, occupation and health data and the COVID-19 cases | Postcode-level estimation of COVID-19 vulnerability | |
| Bamweyana et al. [63] | Vulnerability index for parishes in Kampala (Uganda) | Composite index using socio-economic indicators and pre-existing health conditions, densities and transport hubs | Composite vulnerability indicator based on adaptive capacity, exposure and susceptibility | |
| Santos et al. [64] | Vulnerability in Rio de Janeiro, Brazil | Weighted composite indicator of vulnerability based on census data | Identification of vulnerable city neighbourhoods | |
| Cuadros et al. [11] | Spatiotemporal transmission dynamics | Mathematical spatial simulation of virus spread estimating case numbers | Spatially uneven disease diffusion when urbanised, connected areas are compared with rural areas | |
| Savini et al. [65] | Modelling COVID-19 susceptibility in Italy | Municipality level modelling of contact rates by using census and commuting network data | Geographically detailed scenarios for risk prediction | |
| Esteve et al. [66] | Vulnerability based on age and household structure | Country level global simulation based on census microdata | Estimation of possible infection rates | |
| Fortaleza et al. [67] | Spatial and demographic factors of vulnerability in Sao Paulo State, Brazil | Typology of the municipalities based on socio-demographic data than modelling the spread of the virus | Reinforce of hypothesis on spatial hierarchic spread of the virus | |
| Lakhani [68] | Identifying vulnerable areas in Melbourne | Hotspot analysis of aging population, disability and low access areas to health services | Identifying priority areas for health service development | |
| Mishra et al. [69] | Identifying social factors jeopardising lockdown measures | Aggregation of weighted scores of selected variables for sub-city-level areas of Mumbai, Delhi, Kolkata and Chennai in India | Identifying vulnerable sub-city areas where social factors jeopardising lockdown measures | |
| Interdependence between vulnerability (vulnerable groups) and COVID-19 cases | Kim, Bostwick [43] | Vulnerability and racial inequality in Chicago | Hotspot analysis of COVID-19 deaths, social vulnerability index, health risks and percentage of African Americans based on community areas | Significant overlap between African American population and COVID-19 death rate |
| Bertocchi, Dimico [42] | Relationship between COVID-19 mortality and race (Cook County, Illinois, USA) | Correlation between COVID-19 mortality and the four sub-indices of vulnerability (socioeconomic status, household composition, minority status, housing) | Higher mortality among African Americans through lower socioeconomic status and household composition) | |
| Harris [13] | Correlates of COVID-19 deaths in London | Regression between COVID-19 mortality and socio-economic predictor variables considering neighbourhood connectivity | Mortality is influenced by age, wealth and ethnicity | |
| Hamidi et al. [12] | Connection between development density and COVID-19 infection rate | Regression modelling (Multilevel linear modelling) of density and infection rate and mortality rate | High density areas have significantly higher infection and mortality rates | |
| Khazanchi et al. [70] | County-level analysis of COVID-19 cases and death rates in the USA | Regression analysis of positive COVID-19 test and COVID-19 death per capita | Minority and socioeconomic status were associated with differential risk, while household composition and disability was not | |
| Maiti et al. [71] | Casual association between explanatory variables and COVID-19 transmission in the USA | Global and local, geographically weighted spatial regression model at county level | COVID-19 cases connected to ethnicity, crime and income factors while COVID-19 deaths are connected to deaths, migration and income factors. These connections highly vary across space and time. | |
| Chen, Krieger [72] | Provide estimate on unequal social and economic burden of COVID-19 | Rate differences in COVID-19 deaths, cases and positive tests at county and zip-code area levels. | Social inequalities strongly influence COVID-19 outcomes. |
Data source: Authors' collection.
3. Data and methods
Our approach was to collect a set of indicators (see Table 2 ) to describe social vulnerabilities based on existing scientific reports (Table 1) and data available from the Australian Bureau of Statistics (ABS) and then reduce this set to a small number of factors as the basis for a COVID-19 risk prediction model. Even though there are a large number of variables, some are correlated, and it is therefore possible to significantly reduce the dimensions while retaining a large amount of variation of the initial data set. To do this we used principal component analysis (PCA) which is a multi-variable method of dimension reduction to perform a linear decomposition of the initial variables into a set of components ranked by their ability to explain the covariance within the variable dataset. The resulting components represent composite and uncorrelated dimensions of vulnerability.
Table 2.
The pool of available indicators related to social vulnerabilities in Australia.
| Code of the indicator | Description |
|---|---|
| IND_SH | Share of Indigenous and Torres Strait Islander people from total population, 2016 (%) |
| NCIT_SH | Share of non-citizen from total population, 2016 (%) |
| NOENGS | Share of population not speaking English at home from total population, 2016 (%) |
| OPO_SH | Share of people aged 65 or older from total population (%) |
| CHURN | Churn rate (total arrivals and departures per estimated resident population) 2018 (%) |
| AG_SH | Employment in agriculture and forestry, 2016 (%) |
| ED_SH | Employment in education and training, 2016 (%) |
| HEALTH_SH | Employment in health care and social assistance, 2016 (%) |
| MIN_CO_SH | Employment in mining and construction, 2016 (%) |
| SERV_SH | Employment in wholesale and retail trade, accommodation and food services, rental, hiring and real estate services, arts and recreation and other services, 2016 (%) |
| SMALL_BUS_SH | Share of non-employing businesses or businesses employing less than 5 employees from total number of businesses, 2018 (%) |
| PEREMP_SM_BUS | Number of non-employing businesses or businesses employing less than 5 employees per total number of employees (%) |
| PEREMP_SERV_BUS | Number of businesses in wholesale and retail trade, accommodation and food services, rental, hiring and real estate services, arts and recreation and other services per total number of employees, 2018 (%) |
| PEREMP_AGRI_BUS | Number of agriculture and forestry businesses per total number of employees (%) |
| PCAP_DWELL | Total dwelling units approvals per estimated resident population, 2018 |
| PERCAP_VEH | Registered passenger vehicles per estimated resident population, 2018 |
| PERCAP_INC | Total income per estimated resident population, 2018 |
| PEREMP_INCOM | Total employee income per number of employees, 2016 |
| POOR_S | Persons earning less than $500 per week, 2016 (%) |
| UNEMP_R | Unemployment rate, 2016 (%) |
| PARTICIP | Participation rate, 2016 (%) |
| DISAB | Persons who have need for assistance with core activities, 2016 (%) |
Data source: ABS Data by Region, 2013–2018.
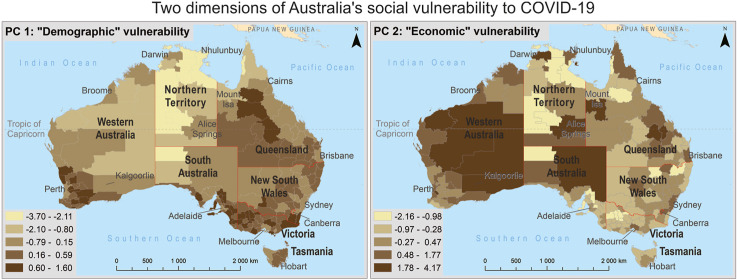
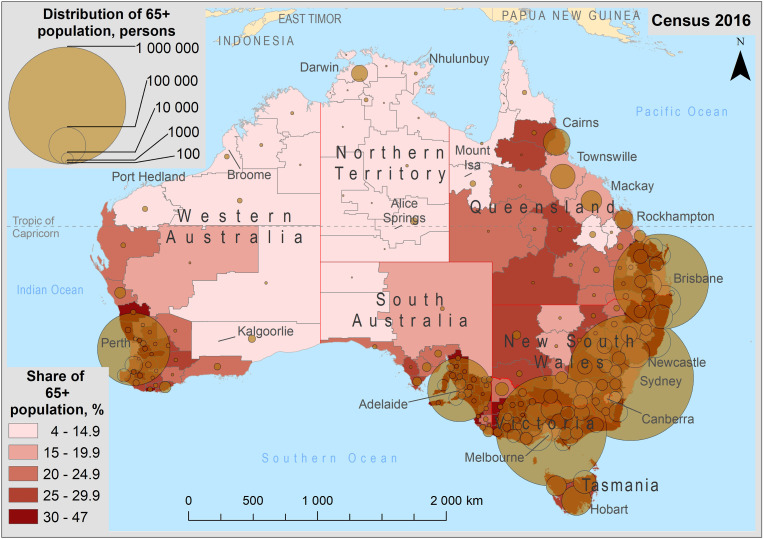
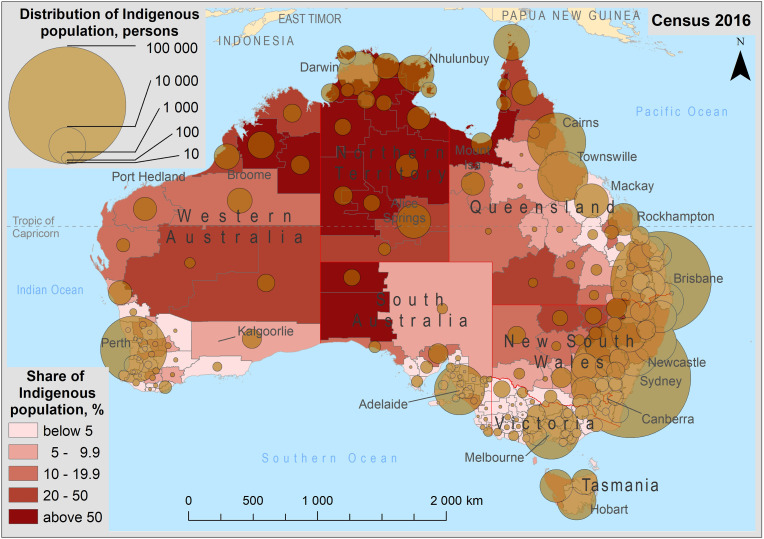
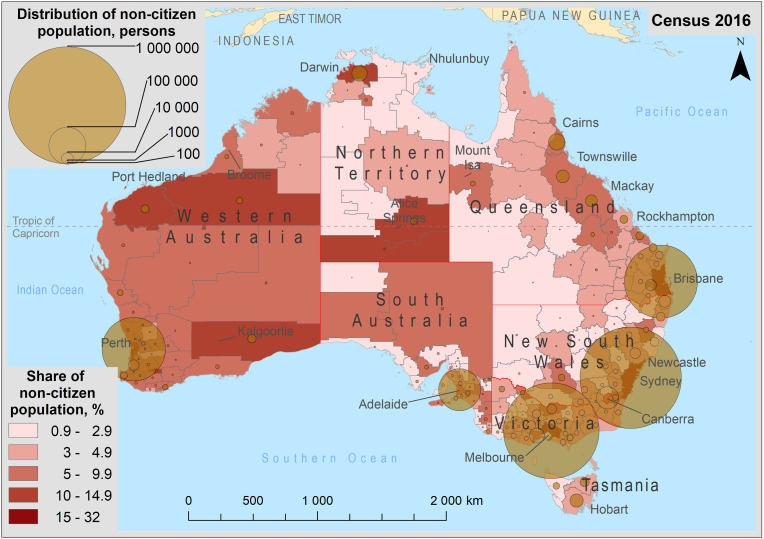
We used ABS estimated resident population data for 2018 and ABS census population data for 2016, both published as ‘Data by Region, 2013–2018’ by the ABS [73] for our small-area population compositions. To understand the spatial distribution of vulnerable populations, we first collected indicators related to probable vulnerable groups based on the availability of indicators and the existing literature we discussed in the previous section which highlights the most vulnerable groups in the population as being the elderly, Indigenous people, non-citizens and people on the move. The spatial distribution of each of these groups across Australia and the share of each of these groups as a proportion of the total estimated resident populations within each area determines the level of vulnerability of the population (see Fig. 1, Fig. 2, Fig. 3, Fig. 4 ).
Fig. 1.
Distribution and share of elderly people.
Fig. 2.
Distribution and share of Indigenous population.
Fig. 3.
Distribution and share of non-citizens. Note to Fig. 1, Fig. 2, Fig. 3: Share is the percentage of a subpopulation in the total of each subdivision, while distribution is the number of the subpopulation distributed across each subdivision.
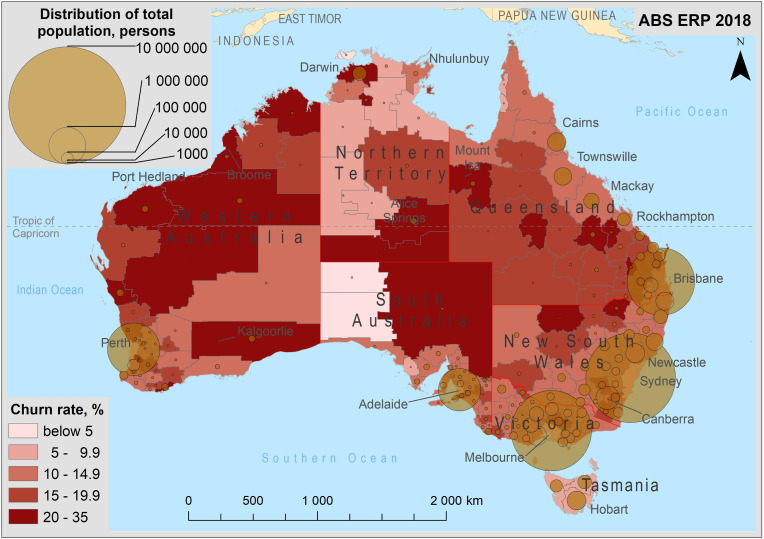
Fig. 4.
Population churn rate by region in Australia, 2018. Note: The churn rate is the sum of total in and out-migration as a proportion of the estimated resident population.
To contextualise the importance of the four sub-groups outlined above, in Fig. 1, we observe elderly people make up a higher proportion of residents in regional (relatively densely populated rural) Australia, outside greater capital city areas, even though their absolute numbers are the highest within capital (e.g. in Sydney) and other large cities (e.g. in Cairns). Meanwhile, Fig. 2 shows that the Indigenous population has the highest share in remote sparsely populated areas of Australia, particularly in Northern Australia (Kimberley in Western Australia, Northern Territory ex-Darwin, and Northern Queensland) and a low share but high number in Australia's largest cities. Fig. 3 shows that the absolute size of the non-citizen population is high in greater capital cities where its share is relatively high. On the other hand, the shares of non-citizen populations are the highest in those sparsely populated regions where the mining or tourism sectors are significant (e.g. the Pilbara and Alice Springs regions) while in other sparsely populated regions the shares of these people remain very low (e.g. Tanami Desert, East Arnhem, Queensland or New South Wales Outback). Both non-citizen and Indigenous populations have a lower level of English proficiency (in general) which increases their vulnerability. Fig. 4, meanwhile, shows the population churn rate as an indicator of population mobility. High churn rates are related to sparsely populated regions with remote mining towns and to Darwin with a significant fly-in-fly-out workforce.
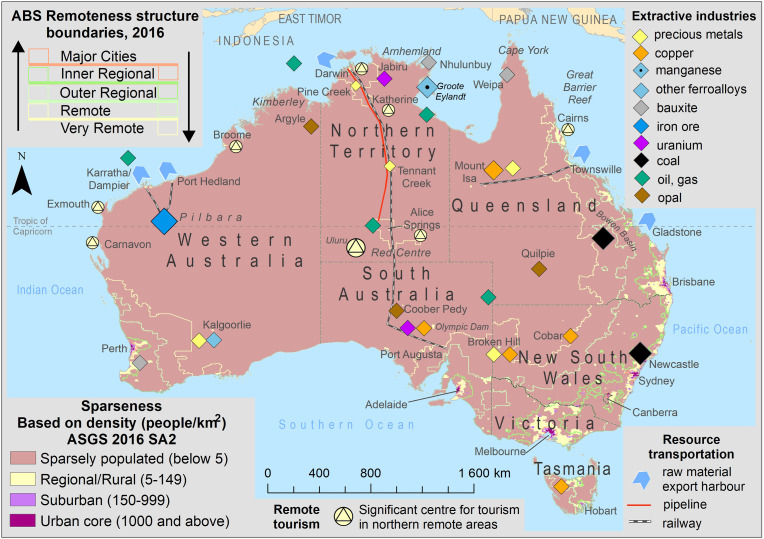
We also included economic variables in our approach to vulnerability since the economic consequences of lockdown efforts impacted employees and businesses differentially across sectors. Economic vulnerability to the COVID-19 pandemic is represented by indicators of those industries particularly impacted when lockdown efforts are imposed [[74], [75], [76], [77], [78]]. These included non-essential small business services (pubs, coffee shops, restaurants, gyms etc.), businesses with a highly mobile fly-in-fly-out labour force (mining, construction) or a seasonal migrant worker labour force (agriculture). Economic and demographic dimensions are often overlapped by mobility-related variables. For instance, as a result of the international travel ban, the education and horticulture sectors have been particularly hard hit due to the loss of overseas students, working holiday makers and seasonal migrant workers from Pacific islands nations (see also [79,80]. Small businesses and service businesses make up a relatively high proportion in regional areas close to large cities where there is a relatively high proportion of older residents [81,82]. Farming related businesses tend to be in outer regional areas, especially those related to cattle and sheep grazing [83]. Mining and construction sectors employing mobile fly-in-fly-out populations [16], are concentrated in sparsely populated areas where large mine sites are located (Fig. 5 ).
Fig. 5.
Remoteness and sparseness in Australia. Note: Remoteness Structure is based on ABS [103].
Based on the assumption that a lower socio-economic status leads to a higher vulnerability to any kind of hazard, we have included the variables of unemployment and labour force participation rates, the share of people earning less than $500AUD per week, per capita passenger vehicles and average incomes (see Table 2). While a high unemployment is clearly related to those sparsely populated remote areas with high proportions of Indigenous people [84], the share of people earning less than 500AUD is also high in inner regional areas with significant elderly populations.
It should be added that the ABS also provides small area estimates of populations at risk to the COVID-19 pandemic disaster based on the National Health Survey 2017–18. These estimates include people with chronic conditions such as cardiovascular diseases, diabetes and asthma [85,86]. However, this data is not published for most very remote areas for reasons of confidentiality related to these areas’ small population numbers. For this reason, we used data on the share of people living with disabilities taken from the 2016 census.
Data on estimated resident population is published for both ABS (Australian Statistical Geography Standard - ASGS) and non-ABS (Local Government Areas) regions. The former allows exploration of vulnerabilities at different spatial levels. The ASGS has four Statistical Area (SA) levels; SA1 is the smallest but most detailed geographical unit. However, the ABS only provides estimated resident population data at the higher SA levels of SA2, SA3 and SA4. When working with the ASGS geography we faced some challenges. For example, the ASGS statistical area levels are designed to reflect units of equal demographic or economic weight (e.g. communities or labour markets) rather than equal spatial weight, and as a result within a given level there can be a large variation in areal size. The high variation of areal sizes is closely related to the modifiable areal unit problem [87] which Openshaw [88,89] highlights the results of a spatial analysis can be different based on the scale and pattern (zonation) of the spatial units used. To overcome this limitation and to have a greater emphasis on the regional variation of COVID-19 vulnerabilities, we created our own geography based on ASGS at the SA2 level, where those SA2 units located in metropolitan areas have been aggregated into larger units. This resulted in 191 units out of the original 2239 ASGS 2016 SA2 units, with a reduced variation in area size and population density, and a slightly increased relative variation in population size (Table 3 ). As a by-product of this aggregation our geography is easier to interpret visually because its units are more equally weighted by areal size.
Table 3.
Comparison between the original ASGS and our adjusted geographic framework.
| Geography | n = | Average |
Relative range (%) |
Relative variance (%) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Area size (km2) | Population size (persons) | Population density (persons/km2) | Area | Popula-tion | Population density | Area | Popula-tion | Population density | ||
| Adjusted geographical framework | 191 | 39141 | 124742 | 3.19 | 13 | 47 | 1053 | 195 | 486 | 854 |
| ASGS SA2 | 2239 | 3386 | 10791 | 3.19 | 148 | 4 | 5730 | 732 | 64 | 2549 |
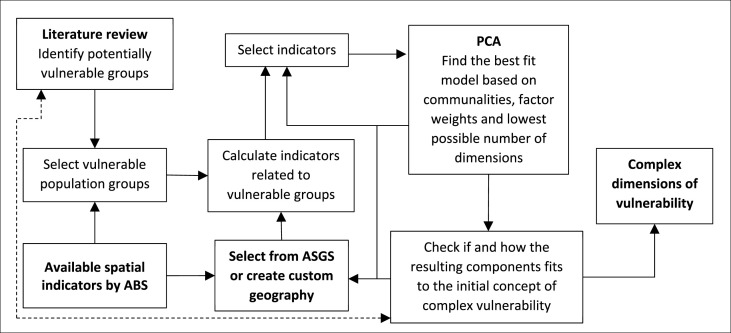
Finally in relation to geography, we extracted composite components of vulnerability according to both the ASGS SA2 and our adjusted geographies by using PCA (see a simplified workflow in Fig. 6 ). Comparing our results for the two different geographies helped us to understand the size effect due to the modifiable areal unit problem, and to validate our adjusted geography. During the selection of variables from the initial dataset (Table 2) we aimed to exclude those indicators having low communalities (not contributing to either components) or high factor weights on more than one component. This was undertaken to extract the best-fit model with the lowest possible number of composite dimensions which still have an explanatory strength (sums of squares) more than 1.
Fig. 6.
The workflow of our empirical survey.
4. Results
Principal component analysis (PCA) based on the adjusted SA2 geography allows us to factor the selected 12 standardised measures of vulnerability given in Table 4 into two dominant composite indicators which together explained 72.2% of the variation of the initial data set, the first encompassing 47.3% and the second 24.9%. The first component is weighted more on the share of Indigenous population, share of aged population, indicators related to service businesses, and the unemployment rate. The second dimension is weighted more on average income, mining and construction sectors, and the mobility related indicators. Based on these factor loadings we called the first dimension ‘demographic vulnerability’ and the second dimension ‘economic vulnerability’.
Table 4.
The extracted principal components by the adjusted geography.
| PC 1 | PC 2 | Communalities | |
|---|---|---|---|
| Zscore(IND_SH) | 0.941 | 0.125 | 0.901 |
| Zscore(NOENGS) | 0.919 | 0.088 | 0.852 |
| Zscore(OPO_SH) | −0.823 | 0.449 | 0.879 |
| Zscore(ED_SH) | 0.766 | 0.339 | 0.702 |
| Zscore(PEREMP_SM_BUS) | −0.755 | 0.269 | 0.642 |
| Zscore(PEREMP_SERV_BUS) | −0.728 | 0.310 | 0.626 |
| Zscore(PERCAP_VEH) | −0.906 | 0.010 | 0.821 |
| Zscore(POOR_S) | 0.089 | 0.853 | 0.736 |
| Zscore(UNEMP_R) | 0.849 | 0.329 | 0.829 |
| Zscore(NCIT_SH) | −0.139 | −0.722 | 0.541 |
| Zscore(PEREMP_INCOM) | 0.028 | −0.752 | 0.566 |
| Zscore(MIN_CO_SH) | 0.112 | −0.749 | 0.574 |
| Sums of squares: | 5.7 | 3.0 | 8.7 |
| % of Variance explained | 47.3 | 24.9 | 72.2 |
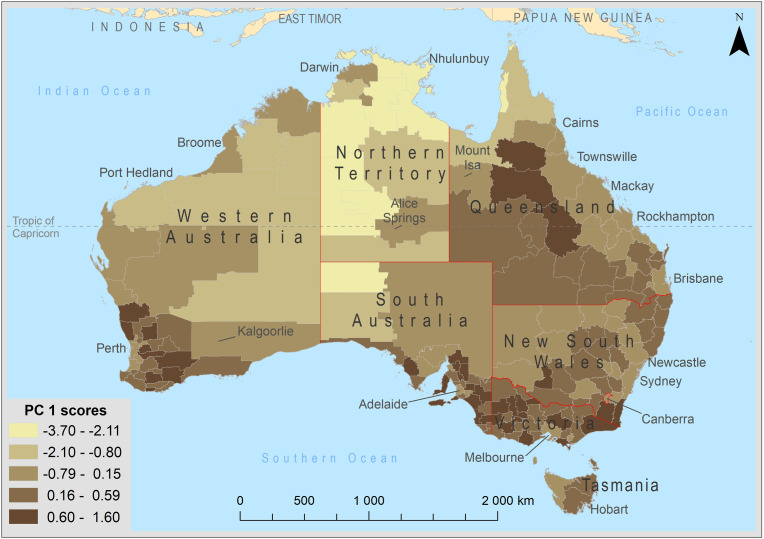
High (positive) scores of demographic vulnerability can be found mostly in regional Australia with its higher share of old people, higher importance of small and service-related businesses which is also connected to the older population in regional areas. Negative scores are mostly found in remote, Indigenous Australia, where along with the high share of Indigenous people who have (in general) a significantly higher unemployment rate than for the rest of the population, particularly in remote areas [84] (Fig. 7 ). It is important to clarify, that both negative and positive ‘extremes’ of that dimension represent a higher vulnerability, characterised either by high share of Indigenous or elderly population, and that the opposite signs simply indicate that where one is present the other tends to be absent.
Fig. 7.
Scores of the 1st principal component (demographic vulnerability).
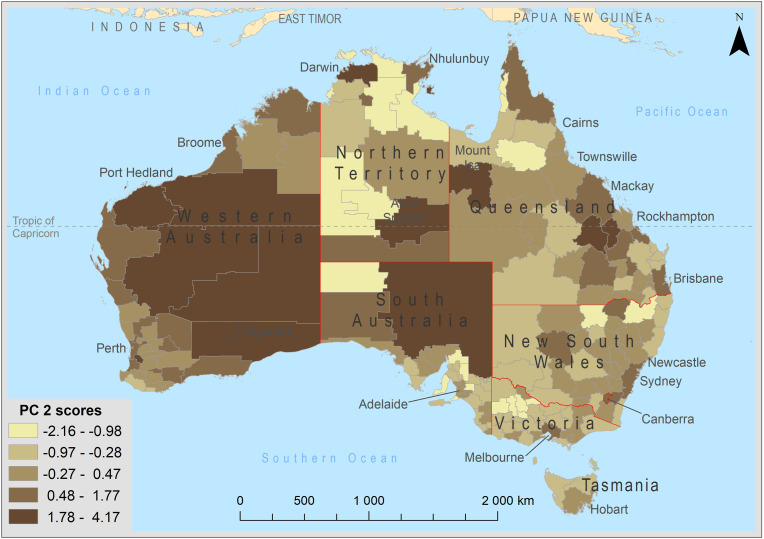
High (positive) scores of the economic vulnerability dimension correspond to greater capital city areas as well as mining areas in remote Australia (Fig. 8 ). These areas are characterised by high employee incomes, high shares of mining and construction workers and a high migration turnover, which together imply a high risk exposure to the negative economic impacts of lockdowns on businesses.
Fig. 8.
Scores of the 2nd principal component (economic vulnerability).
A PCA based on the original ASGS SA2 geography and the selected 10 standardised variables yielded three components which together explained the 79.9% of the variation of the initial variables, the first explaining only 36.9% (Table 5 ). The first component in this model we called the ‘household economic dimension’ because of the high factor loadings on those indicators related to economic performance and disability. The second component we called the ‘minority dimension’ because it had greater weights on overseas and Indigenous populations and high overseas migration turnover. These are all related to a higher share of non-English speaking populations. The third component we called the ‘business economic’ dimension because it is almost exclusively related to small and service-related businesses.
Table 5.
The extracted principal components by the original ASGS SA2 geography.
| PC 1 | PC 2 | PC 3 | Communalities | |
|---|---|---|---|---|
| Zscore(NCIT_SH) | 0.431 | 0.849 | 0.009 | 0.907 |
| Zscore(NOENGS) | 0.177 | 0.825 | 0.004 | 0.712 |
| Zscore(O_CHURN) | 0.476 | 0.763 | 0.010 | 0.809 |
| Zscore(PEREMP_SM_BUS) | 0.028 | −0.023 | 0.997 | 0.995 |
| Zscore(PEREMP_SERV_BUS) | 0.029 | −0.015 | 0.997 | 0.995 |
| Zscore(PERCAP_INC) | 0.806 | −0.210 | 0.131 | 0.711 |
| Zscore(PEREMP_INCOM) | 0.835 | −0.226 | −0.017 | 0.749 |
| Zscore(POOR_S) | −0.818 | 0.382 | 0.048 | 0.817 |
| Zscore(PARTICIP) | 0.791 | −0.207 | −0.108 | 0.680 |
| Zscore(DISAB) | −0.779 | 0.051 | 0.043 | 0.611 |
| Sums of squares: | 3.7 | 2.3 | 2.0 | 8.0 |
| % of Variance explained | 36.9 | 22.7 | 20.2 | 79.9 |
The first dimension of this model has its highest values in the CBDs of greater capital cities while certain suburbs have very low factor values. This spatial variation is repeated in regional and remote Australia where high scores in mining areas are contrasted with the low scores of predominantly farming and Indigenous areas. The second dimension has its highest scores where there is a higher share of non-citizens in metropolitan suburbs. High scores are also found in sparse, remote units where the Indigenous population makes up a higher proportion. Hence two different phenomena are combined in that single component: foreigners in urban areas, and Indigenous Australians in remote areas. The third dimension reflects small and service businesses which have low score values in residential suburbs and in remote sparsely populated areas.
On comparing the two models from the two different geographies, we see that the model based on the ASGS SA2 geography reflects intra-urban issues related to the location of wealth (economic participation, incomes and efficiency), segregation (overseas and Indigenous) and service sector concentration. These ‘urban’ dimensions are repeated in remote sparsely populated areas where high income inequalities (see Taylor et al. [90]) and spatial segregation (Indigenous vs. mining communities, spatial diversity, see Carson et al. [15,84]) are also present. On the other hand, when these results are compared to the adjusted geography we notice that the demographic-aging dimension contrasting regional and remote sparsely populated Australia in the model based on the adjusted geography is absent.
Furthermore, the three dimensions obtained from the analysis using the ASGS SA2 geography encompass phenomena that are predictably linked together, and do not reflect correlations with a complex ‘background’ vulnerability. In contrast, the first component in the model based on the adjusted geography incorporates aging, Indigenous people, services and unemployment into a single composite measure of vulnerability explaining 47.3% of the total variance. Additionally, while the first two components in the model based on the ASGS SA2 geography explain only 59.7% of the total variation, the two dimensional model based on the adjusted geography explains 72.2%. Hence the adjustment of SA2 spatial units allows us to better characterise Australia's COVID-19 vulnerability by removing the confounding effect of intra-urban spatial variations. These are the reasons why we decided to use the two-dimensional model based on the adjusted geography.
5. Discussion and conclusions
The two composite measures of demographic and economic vulnerability in our model reflect the two main contrasting risks from the COVID-19 pandemic disaster. The first dimension, demographic vulnerability, is related to the individual's socio-demographic status and highlights those jurisdictions which would be highly exposed to risk in the event of an uncontrolled spread of the virus. Demographic vulnerability, particularly the ethnic composition of the population, has been identified by the literature as the most important risk factor for COVID-19. Empirical studies by Kim, Bostwick [43]; Bertocci, Dimico Bertocci, Dimico [42] and Maiti et al. [71] revealed a strong interrelation between ethnicity and COVID-19 cases. It should be emphasised however that, according to Maiti et al. [71] while COVID-19 cases are related to both ethnicity and income factors, COVID-19 caused deaths are empirically connected only to income factors, hence socio-economic status and ethnicity are connected only in relation to the likelihood of contracting the virus. According to our risk prediction model, Indigenous Australians are particularly vulnerable in remote regions where the low socio-economic status is strongly related to ethnicity because Indigenous Australians make up the majority of unemployed there. Hence, Indigenous Australians are most at risk as a result of both their minority and income status.
It is important to add, however, that these demographic vulnerabilities were, thankfully, not clearly evident in Australia to date because of the very low level of community transmissions. Transmission in Australia has been almost exclusively within the geographic bounds of the greater capital cities which have hosted returning Australian residents from overseas in hotel quarantine. Several clusters in Melbourne, Sydney and Brisbane have emerged from the virus being ‘transported’ out from hotel quarantine positive cases by security guards, health worker and others. Fortunately, in regional and remote Australia the numbers have been just a handful of people who had contact with people in city-originating clusters. This pattern is demonstrated by Hamidi et al. [12] and Mishra et al. [69] who highlighted that the COVID-19 pandemic is strongly connected to densely populated urban core areas where the risk of community transmission is higher due to the physical proximity of residents. They also suggest that the current COVID-19 pandemic is challenging the concept of compact urban development as a sustainable model when future pandemics seem likely. In contrast, Cuadros et [11] emphasised that critical health care infrastructure unlike in large metropolises, may lack the necessary capacity in rural and remote areas despite the lower case numbers as a result of sparsity, and hence put the residents there in a more vulnerable situation.
In contrast to demographic vulnerability, the second dimension, economic vulnerability, is related to the impacts of lockdowns and border closures on businesses and their employees. Until recently this dimension has not been widely studied empirically. Nevertheless, Kikuchi et al. [91] examined declining household expenditures in Japan at the initial stage of the pandemic, which, as a result of lockdowns, will likely be the most serious consequence of the pandemic in Australia as well. To mitigate this impact the Australian Government implemented the Job Keeper program [92] and tax relief policies in order to maintain household expenditures and reduce business failures. Despite this, measures to prevent the spread of and totally eliminate the virus have hit metropolitan cores particularly hard and put at risk mining sites and the tourism sector in sparsely populated areas.
Our two dimensions are at the core of most policy debates around the pandemic as well: whether to accept a level of virus spread in order to save the economy and possibly achieve some kind of herd immunity this way (or since early 2021, through vaccination), or whether to totally eliminate the virus first in order to ease pressure on the health care system, save lives and ultimately re-open the economy. For example, Western Australia, a state particularly exposed to risk in the economic dimension (Fig. 8) followed the second approach by enacting and maintaining very strict border controls; a move which not only prevented transmission but also delivered a political whitewash for the standing government in the 2021 Western Australian state elections [93]. Of course, the policies which seek to balance both risks could expose both of these dimensions of vulnerability to some extent with consequences that will vary in time and place.
As a federation of states and territories, Australia is characterised by different levels of policy making and responsibilities (commonwealth vs. states and territories) which creates different outcomes, similar to the effects of scale in policy response emphasised by Delaney [40] in the context of the federalist USA and the more centralised Ireland. Both the WHO and the Australian federal government have often emphasised the lack of universal policies among nations, states and territories, but our work suggests such a universal recipe might never work. Australia in particular is an example of where states and territories have taken different approaches to overcoming the obstacles posed by the pandemic. We should probably expect further regional variations in lockdown policies, maintained or re-imposed border restrictions, and migration bubbles until a global heard immunity is achieved through vaccination in the coming years.
Along with the spatial variation of mitigation policy measures during the COVID-19 pandemic, geography has exerted a significant impact on societies through a ‘territorial trap’ [94] (p. 154) in the form of border closures, travel bans and zoning of regions and hot spot areas [106] where “time has been annihilated by space” [95] (p. 191). This is challenging the pre-pandemic view of an increasingly hyper connected global society [96,97]. According to Fortaleza et al. [67] large metropolises are playing a significant role through their global connectedness and the virus spreading from these centres down the settlement hierarchy and into the adjacent rural peripheries through commuting networks. Harris [13] also emphasised the role of neighbourhood connectivity at the intra-urban level. Adding to this, the variation in outcomes by scale shows that social vulnerabilities are also influenced by the geography along with health and social status. Thus, the spread of the virus is potentially influenced not only by spatially varying mitigation policies, population densities and connectivity, but also by spatial variations in social vulnerability.
Spatial variations of social vulnerability are also consistent with the view of Wisner and his co-authors [32] (p. 92) who argued that geographical space itself can be considered as one of the resources that are allocated by social processes, such that, under the routine operation of these processes people become more or less vulnerable to hazard impacts. For example, better access to jobs forces people to live in cities where they are more exposed to hazard risks because of the higher population densities. Through this view space is not only a container where actions unfold but it is itself a dynamic variable determining vulnerability outcomes.
In summary, the spatial variation of vulnerabilities which is evident from our modelling highlights that this pandemic should not only be presented as a crisis for the health and economies of nations. Our study for Australia shows certain sub-populations are highly vulnerable relative to others and that the scale of vulnerability is variable by geography. To truly minimize health and other effects from this and future pandemics, policy attention should be re-focused towards addressing underlying inequalities evident in almost all nations, including a rich and prosperous Australian society. While the speed and magnitude of the pandemic's spread globally was rapid, leading to policy-on-the-run, planning for future pandemics must recognise the potential role and impacts of vulnerabilities. Even at the time of writing, relatively low literacy levels and a mistrust of western medical systems is impacting on the voracity of vaccination uptakes in some areas of Australia, such as in the Torres Strait Islands which is exposed to potential transmissions from Papua New Guinea's extremely vulnerable population located just 100 km from the northern most Island of the Torres Strait [98]). Vulnerability, as represented in the data analysed in this study, is therefore the true ‘carrier’ of the virus which has impacted on so many of the world's poor and marginalised communities. For now Australia can consider itself fortunate, in part through good management and containment initiatives, that its most marginalised communities, Indigenous Australian's in remote areas, were not exposed in situ.
Lastly we would like to emphasise some limitations in and opportunities to extend our study. First, in the adjusted geography we lost some precision in spatial information because we used a higher spatial aggregation, but this adjustment helped us to focus on spatial-regional diversity instead of intra-urban diversity. Second, the PCA method itself may be strongly influenced by the researchers’ decisions about which indicators to include initially and which ones to exclude when searching for the best fit model [99,100]. On the other hand, the selection of the initial data set was guided by a review of the existing literature on social vulnerability and our understanding of those variables best able to represent COVID-19 related vulnerabilities. We also considered using geographically weighted PCA (GWPCA) [101,102] to better understand the spatially varying nature of social vulnerability which Maiti et al. [71] utilised explaining casual associations between explanatory variables and COVID-19 cases and deaths, but considered this as an extension of, rather than an integral part within our study. Lastly, validation of the two dimensional risk prediction model is also an important consideration, but the lack of large scale community transmission in Australia, and the corresponding lack of data against which validation methods might be applied, prevent this. There is an opportunity, therefore, to utilise international comparisons to extend this study and address this and other limitations.
Funding
This work was partly supported by the Australian Government Research Training Program Scholarship.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.McEntire D.A. Bissel, R, 2013. Preparadness and Response for Catastrophic Disasters. CRC Press, Taylor&Francis Group; Boca Raton, London, New York: 2013. Understanding catastrophes. A discussion of casuation, impacts, policy approaches, and organizational structures. [Google Scholar]
- 2.Fearnley C.J., Dixon D. Editorial: early warning systems for pandemics: lessons learned from natural hazards. International Journal of Disaster Risk Reduction. 2020;49:101674. doi: 10.1016/j.ijdrr.2020.101674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karagiannidis C., Mostert C., Hentschker C., Vashaar T., Malzahn J., Schillinger G., Klauber J., Janssens U., Marx G., Weber Carstens S., Kluge S., Pfeifer M., Grabenhenrich L., Welte T., Busse R. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: and observational study. Lancet Respiratory Medicine. 2020;8:853–862. doi: 10.1016/S2213-2600(20)30316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in taiwan. Big data analytics, new technology, and proactive testing. J. Am. Med. Assoc. 2020;323(14):1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 5.Patel J.A., Nielsen F.H.B., Badiani A.A. Poverty, inequality and COVID-19: the forgotten vulnerable. Publ. Health. 2020;183:110–111. doi: 10.1016/j.puhe.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fishman D.N., Bogoch I., Lapointe-Shaw L., McCready J., Tuite A.R. Failing our most vulnerable: COVID-19 and long-term care facilities in ontario. 2020. https://www.medrxiv.org/content/10.1101/2020.04.14.20065557v1 [DOI] [PMC free article] [PubMed]
- 7.Han D.S., Mosqueda L. Elder abuse in the Covid-19 era. J. Am. Geriatr. Soc. 2020;68(7):1386–1387. doi: 10.1111/jgs.16496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alcántara-Ayala I., Burton I., Lavell A., Mansilla E., Maskrey A., Oliver-Smith A., Ramírez-Gómez F. Editorial: root causes and policy dilemmas of the COVID-19 pandemic global disaster. International Journal of Disaster Risk Reduction. 2021;52:101892. doi: 10.1016/j.ijdrr.2020.101892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomas D.S.K., Jang S., Scandlyn K. The CHASMS conceptual model of cascading disasters and social vulnerability: the COVID-19 case example. International Journal of Disaster Risk Reduction. 2020;51:101828. doi: 10.1016/j.ijdrr.2020.101828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Platt L., Warwick R. Are some ethnic groups more vulnerable to COVID-19 than others? The Institute for Fiscal Studies. 2020. https://www.ifs.org.uk/inequality/chapter/are-some-ethnic-groups-more-vulnerable-to-covid-19-than-others/ [DOI] [PMC free article] [PubMed]
- 11.Cuadros D.F., Xiao Y., Mukandavire Z., Correa-Agudelo E., Hernández A., Kim H., MacKinnin N.J. Spatiotemporal transmission dynamics of the COVID-19 pandemic and its impact on critical healthcare capacity. Health Place. 2020;64:102404. doi: 10.1016/j.healthplace.2020.102404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamidi S., Ewing R., Sabouri S. Longitudinal analyses of the relationship between development density and the COVID-19 morbidity and mortality rates: early evidence from 1,165 metropolitan counties in the United States. Health Place. 2020;64:102378. doi: 10.1016/j.healthplace.2020.102378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris R. Exploring the neighbourhood-level correlates of Covid-19 deaths in London using a difference across spatial boundaries method. Health Place. 2020;66:102446. doi: 10.1016/j.healthplace.2020.102446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cardona O.D. In: Mapping Vulnerability: Disasters, Development and People. Bankoff G., Frerks G., Hilhorst D., editors. Sterling & VA: Earthscan; London: 2004. The need for rethinking the concepts of vulnerability and risk from a holistic perspective: a necessary review and criticism for effective risk management; pp. 37–51. [Google Scholar]
- 15.Carson D., Rasmussen R., Ensign P.C., Taylor A., Huskey L., editors. Demography at the Edge: Remote Human Populations in Developed Nations. Ashgate Publishing; Farnham, England: 2011. [Google Scholar]
- 16.Taylor A. In: Settlements at the Edge: Remote Human Settlements in Developed Nations. Taylor A., Carson D.B., Ensign P.C., Husky L., Rasmussen R.O., Saxinger G., editors. Edward Elgar; Gloucester, UK: 2016. Introduction: settlements at the edge; pp. 3–24. [Google Scholar]
- 17.Health. 2020. https://www.health.gov.au/resources/total-covid-19-cases-and-deaths-by-states-and-territories [Google Scholar]
- 18.AIHW . Australian Institute of Health and Welfare; 2014. Australia's Health 2014.https://www.aihw.gov.au/getmedia/3fae0eb7-b2be-4ffc-9903-a414388af557/7_7-indigenous-health-remoteness.pdf.aspx [Google Scholar]
- 19.AIHW . Australian Institute of Health and Welfare; 2020. Australia's Health 2020 in Brief.https://www.aihw.gov.au/getmedia/2aa9f51b-dbd6-4d56-8dd4-06a10ba7cae8/aihw-aus-232.pdf.aspx?inline=true [Google Scholar]
- 20.Liu Y.C., Kuo R.L., Shih S.R. COVID-19: the first documented coronavirus pandemic in history. Biomed. J. 2020;43:328–333. doi: 10.1016/j.bj.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Y.C., Chen C.S., Chan Y.J. The outbreak of COVID-19: an overview. J. Chin. Med. Assoc. 2020;83:217–220. doi: 10.1097/JCMA.0000000000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burki T. The origin of SARS-CoV-2. Lancet. 2020;20(August):1018–1019. doi: 10.1016/S1473-3099(20)30641-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parrish C.R., Holmes E.C., Morens D.M., Park E.C., Burke D.S., Calisher C.H., Laughlin C.A., Saif L.J., Daszak P. Cross-species virus transmission and the emergence of new epidemic diseases. Microbiol. Mol. Biol. Rev. 2008;72(3):457–470. doi: 10.1128/MMBR.00004-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chan J.W.C., To K.K.W., Chen H., Yuen K.Y. Cross-species transmission and emergence of novel viruses from birds. Current Opinion in Virology. 2015;10:63–69. doi: 10.1016/j.coviro.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Geoghegan J.L., Duchêne S., Holmes E.C. Comparative analysis estimates the relative frequencies of co-divergence and crossspecies transmission within viral families. PLoS Pathog. 2017;13(2) doi: 10.1371/journal.ppat.1006215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Donner W., Rodríguez H. Population composition, migration and inequality: the influence of demographic changes on disaster risk and vulnerability. Soc. Forces. 2008;87(2):1089–1114. [Google Scholar]
- 27.Hugo G. Future demographic change and its interactions with migration and climate change. Global Environ. Change. 2011;21:21–33. [Google Scholar]
- 28.Csomós G., Farkas J.Z., Kovács Z. Access to urban green spaces and environmental inequality in post-socialist cities. Hungarian Geographical Bulletin. 2020;69(2):191–207. [Google Scholar]
- 29.Maxmen A. WHO report into COVID pandemic origins zeroes in on animal markets, not labs. Nature. 2021 doi: 10.1038/d41586-021-00865-8. https://www.nature.com/articles/d41586-021-00865-8 [DOI] [PubMed] [Google Scholar]
- 30.Drabek T.E. Disasters as nonroutine social problems. Int. J. Mass Emergencies Disasters. 1989;7(3):253–264. [Google Scholar]
- 31.Blaikie P.T., Cannon T., Davis I., Wisner B. Routledge; London, UK: 1994. At Risk: Natural Hazards, People, Vulnerability, and Disasters. [Google Scholar]
- 32.Wisner B., Blaikie P., Cannon T., Davis I. Routlege; London-New York: 2004. At Risk. Natural Hazards, People's Vulnerability and Disasters. [Google Scholar]
- 33.Cutter S.L. In: What Is a Disaster? New Answers to Old Questions. Perry R.W., Quarantelli E.L., editors. International Committee on Disasters; 2005. Are we asking the right question? pp. 39–48. [Google Scholar]
- 34.Oliver-Smith A. In: Anthropology and Climate Change: from Encounters to Actions. Crate S.A., Nuttal M., editors. Left Coast Press Walnut Creek; CA: 2009. Climate change and population displacement: disasters and diasporas in the twenty-first century. [Google Scholar]
- 35.Lancet Redefining vulnerability in the era of COVID-19. Lancet. 2020;395(4):1089. doi: 10.1016/S0140-6736(20)30757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Standring A., Davies J. From crisis to catastrophe: the death and viral legacies of austere neoliberalism in Europe? Dialogues in Human Geography. 2020;10(2):146–149. [Google Scholar]
- 37.Brown P. Studying COVID-19 in light of critical approaches to risk and uncertainty: research pathways, conceptual tools, and some magic from Mary Douglas. Health. Risk & Society. 2020;22(1):1–14. [Google Scholar]
- 38.Smidt J.A., Judd J. COVID-19: vulnerability and the power of privilege in a pandemic. Health Promot. J. Aust. 2020;31:158–160. doi: 10.1002/hpja.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silva D.S. COVID-19 in the public housing towers of Melbourne: upholding social justice when invoking precaution. Aust. N. Z. J. Publ. Health. 2020;44(5):430. doi: 10.1111/1753-6405.13041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Delaney A. The politics of scale in the coordinated management and emergency response to the COVID-19 pandemic. Dialogues in Human Geography. 2020;10(2):141–145. [Google Scholar]
- 41.Gaynor T.S., Wilson M.E. Social vulnerability and equity: the disproportionate impact of COVID-19. Publ. Adm. Rev. 2020;80(5):832–838. doi: 10.1111/puar.13264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bertocchi G., Dimico A. 2020. Race and the COVID-19 Pandemic. VoxEU & CEPR Coverage of the Covid-19 Global Pandemic.https://voxeu.org/article/race-and-covid-19-pandemic [Google Scholar]
- 43.Kim S.J., Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ. Behav. 2020;47(4):509–513. doi: 10.1177/1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Poteat T., Millett G.A., Nelson L.E., Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann. Epidemiol. 2020;47:1–3. doi: 10.1016/j.annepidem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee Y.J. The impact of the COVID-19 pandemic on vulnerable older adults in the United States. J. Gerontol. Soc. Work. 2020;63(6–7):559–564. doi: 10.1080/01634372.2020.1777240. [DOI] [PubMed] [Google Scholar]
- 46.Gray D.M., Anyane-Yeboa A., Balzora S., Issaka R.B., May F.P. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nat. Rev. Gastroenterol. Hepatol. 2020;17:520–522. doi: 10.1038/s41575-020-0330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fernandez L.S., Byard D., Lin C.C., Benson S., Barbera J.A. Frail elderly as disaster victims: emergency management strategies. Prehospital Disaster Med. 2002;17(2):67–74. doi: 10.1017/s1049023x00000200. [DOI] [PubMed] [Google Scholar]
- 48.Hugo G. Contextualising the ‘crisis in aged care’ in Australia: a demographic perspective. Aust. J. Soc. Issues. 2007;42(2):169–182. [Google Scholar]
- 49.Robinson C. In: Demographic Methods in Emergency Assessment A Guide for Practitioners. Center for International Emergency, Disaster and Refugee Studies (CIEDRS) and the Hopkins Population Center. Robinson C., Hill K., editors. Johns Hopkins University Bloomberg School of Public Health; Baltimore, Maryland: 2003. Overview of disaster. [Google Scholar]
- 50.Gelatt J. Migration Policy Institute; 2020. Immigrant Workers. Vital to the U.S. COVID-19 Response, Disproportionately Vulnerable.https://www.migrationpolicy.org/research/immigrant-workers-us-covid-19-response [Google Scholar]
- 51.Haley E., Hennebry J.L., Caxaj S., Martell E., George G., McLaughlin J. Migrant farmworkers face heightened vulnerabilities during COVID-19. Journal of Agriculture, Food Systems, and Community Development. 2020;9(3):35–39. [Google Scholar]
- 52.Kaur-Gill S. The COVID-19 pandemic and outbreak inequality: mainstream reporting of Singapore's migrant workers in the margins. Frontiers in Communication. 2020;5:65. [Google Scholar]
- 53.Nott D. The COVID-19 response for vulnerable people in places affected by conflict and humanitarian crises. Lancet. 2020;395:1532–1533. doi: 10.1016/S0140-6736(20)31036-9. 10236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zaman S., Sammonds P., Ahmed B., Rahman T. Disaster risk reduction in conflict contexts: lessons learned from the lived experiences of Rohingya refugees in Cox's Bazar, Bangladesh. International Journal of Disaster Risk Reduction. 2020;50:101694. doi: 10.1016/j.ijdrr.2020.101694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Truelove S., Abrahim O., Altare C., Lauer S.A., Granzt K.H., Azman A.S., Spiegel P. The potential impact of COVID-19 in refugee camps in Bangladesh and beyond: a modelling study. PLoS Med. 2020;17(6) doi: 10.1371/journal.pmed.1003144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mainul Islam M., Yunus Y. Rohingya refugees at high risk of COVID-19 in Bangladesh. The Lancet Global Health. 2020;8:e994. doi: 10.1016/S2214-109X(20)30282-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Home Affairs. 2020. https://covid19.homeaffairs.gov.au/leaving-australia#toc-1 [Google Scholar]
- 58.Taylor A., Carson D. Indigenous mobility and the Northern Territory emergency response. People Place. 2009;17(1):29–38. [Google Scholar]
- 59.Taylor A. More than mobile: migration and mobility Impacts from the ‘technologies of change’ for Aboriginal communities in the remote Northern Territory of Australia. Mobilities. 2012;7(2):269–294. [Google Scholar]
- 60.Australian Broadcasting Commission . 2020. Coronavirus Travel Restrictions Set to Apply to 76 Remote Indigenous Communities in NT.https://www.abc.net.au/news/2020-03-20/nt-travel-restrictions-for-remote-communities-coronavirus/12076564 [Google Scholar]
- 61.Acharya R., Porwal A. A vulnerability index for the management of and response to the COVID-19 epidemic in India: an ecological study. Lancet Global Health. 2020;8:e1142–e1151. doi: 10.1016/S2214-109X(20)30300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Amram O., Amiri S., Lutz R.B., Rajan B., Monsivais P. Washington State, USA. Health and Place. vol. 64. 2020. Development of a vulnerability index for diagnosis with the novel coronavirus, COVID-19; p. 102377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bamweyana I., Okello D.A., Ssengendo R., Mazimwe A., Ojirot P., Mubiru F., Ndungo L., Kiyingi C.N., Ndyabakira A., Bamweyana S., Zabali F. Socio-economic vulnerability to COVID-19: the spatial case of greater kampala metropolitan area (GKMA) J. Geogr. Inf. Syst. 2020;12:302–318. [Google Scholar]
- 64.Santos J.P.C., Siqueria A.S.P., Praca H.L.F., Albuquerque H.G. Vulnerability to severe forms of COVID-19: an intra-municipal analysis in the city of Rio de Janeiro, Brazil. Reports in Public Health. 2020;36(5) doi: 10.1590/0102-311x00075720. [DOI] [PubMed] [Google Scholar]
- 65.Savini L., Candeloro L., Calistri P., Conte A. 2020. A Municipality-Based Approach Using Commuting Census Data to Characterise the Vulnerability to Influenza-like Epidemic: the COVID-19 Application in Italy. Preprint.https://www.medrxiv.org/content/10.1101/2020.05.12.20100040v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Esteve A., Permanyer I., Boertien D., Vaupel J.W. National age and co-residence patterns shape covid-19 vulnerability. 2020. https://www.medrxiv.org/content/10.1101/2020.05.13.20100289v1 [DOI] [PMC free article] [PubMed]
- 67.Fortaleza C.M.C.B., Guimaraes R.B., de Almeida G.B., Pronunciate M., Ferreire C.P. Taking the inner route: spatial and demographic factors affecting vulnerability to COVID-19 among 604 cities from inner São Paulo State, Brazil. Epidemiol. Infect. 2020;148(e118):1–5. doi: 10.1017/S095026882000134X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lakhani A. Which Melbourne metropolitan areas are vulnerable to COVID-19 based on age, disability, and access to health services? Using spatial analysis to identify service gaps and inform delivery. J. Pain Symptom Manag. 2020;60(1):e41–e44. doi: 10.1016/j.jpainsymman.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mishra S.V., Gayen A., Haque S.M. COVID-19 and urban vulnerability in India. Habitat Int. 2020;103:102230. doi: 10.1016/j.habitatint.2020.102230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Khazanchi R., Beiter E.R., Gondi S., Beckman A.L., Bilinski A., Ganguli I. County-level association of social vulnerability with COVID-19 cases and deaths in the USA. J. Gen. Intern. Med. 2020;35(9):2784–2787. doi: 10.1007/s11606-020-05882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Maiti A., Zhang Q., Sannigrahi S., Pramanik S., Chakraborti S., Cerda A., Pilla F. Exploring spatiotemporal effects of the driving factors on COVID-19 incidences in the contiguous United States. Sustainable Cities and Society. 2021;68:102784. doi: 10.1016/j.scs.2021.102784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen J.T., Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses. J. Publ. Health Manag. Pract. 2021;27(1):43–56. doi: 10.1097/PHH.0000000000001263. [DOI] [PubMed] [Google Scholar]
- 73.ABS Data by region, 2013-18. 2019. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/1410.02013-18?OpenDocument
- 74.Blundell R., Dias M.C., Joyce R., Xu X. COVID-19 and inequalities. Fisc. Stud. 2020;41(2):291–319. doi: 10.1111/1475-5890.12232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Blustein D.L., Duffy R., Ferreire J.A., Cohen-Scali V., Cinamon R.G., Allan B.A. Unemployment in the time of COVID-19: a research agenda. J. Vocat. Behav. 2020;119:103436. doi: 10.1016/j.jvb.2020.103436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mogaji E. Financial vulnerability during a pandemic: insights for coronavirus disease (COVID-19) Research Agenda Working Papers. 2020;5:57–63. [Google Scholar]
- 77.Nunes J. The COVID-19 pandemic: securitization, neoliberal crisis, and global vulnerabilization. Reports in Public Health. 2020;36(4) doi: 10.1590/0102-311x00063120. [DOI] [PubMed] [Google Scholar]
- 78.Winter J. The evolutionary and disruptive potential of Industry 4.0. Hungarian Geographical Bulletin. 2020;69(2):83–97. [Google Scholar]
- 79.Taylor A., Bell L., Gerritsen R. Benefits of skilled migration programs for regional Australia: perspectives from the Northern Territory. J. Econ. Soc. Pol. 2014;16(1):1–23. [Google Scholar]
- 80.Carson D.A., Cleary J., de la Barre S., Eimermann M., Marjavaara R. In: Settlements at the Edge: Remote Human Settlements in Developed Nations. Taylor A., Carson D.B., Ensign P.C., Husky L., Rasmussen R.O., Saxinger G., editors. Edward Elgar; Gloucester, UK: 2016. New mobilities – new economies? Temporary populations and local innovation capacity in sparsely populated areas; pp. 178–206. [Google Scholar]
- 81.Hugo G. Immigrant settlement outside of Australia's capital cities. Popul. Space Place. 2008;14(6):553–571. [Google Scholar]
- 82.Wilson T., Temple J. To what extent is Australia's population ageing? The application of traditional and alternative ageing measures. Australian Population Studies. 2020;4(1):57–69. [Google Scholar]
- 83.Holmes J. Diversity and change in Australia's rangelands: a post-productivist transition with a difference? Trans. Inst. Br. Geogr. 2002;27(3):362–384. [Google Scholar]
- 84.Carson D., Koster R. Addressing the problem of Indigenous disadvantage in remote areas of developed nations: a plea for more comparative research. Journal of Rural and Community Development. 2012;7(1):110–125. [Google Scholar]
- 85.ABS National health survey: first results. 2018. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0012017-18?OpenDocument
- 86.ABS . 2020. At Risk Populations: Health Conditions Distribution.https://covid19-esriau.hub.arcgis.com/app/df0735224318415f96007b0c2b41f69a [Google Scholar]
- 87.Gehlke C.E., Biehl K. Certain effects of grouping upon the size of the correlation coefficient in census tract material. Journal of the American Statistical Association Supplement. 1934;29:169–170. [Google Scholar]
- 88.Openshaw S. A geographical solution to scale and aggregation problems in region-building, partitioning and spatial modelling. Institute of British Geographers. Transactions, NewSeries. 1977;2:459–472. [Google Scholar]
- 89.Openshaw S. Geo Books; 1984. The Modifiable Areal Unit Problem; p. 41. [Google Scholar]
- 90.Taylor A., Larson S., Stoeckl N., Carson D. The haves and have nots in Australia's tropical north – new perspectives on a persisting problem. Geogr. Res. 2011;49(1):13–22. [Google Scholar]
- 91.Kikuchi S., Kitao S., Mikoshiba M. The University of Tokyo; 2020. Heterogeneous Vulnerability to the COVID-19 Crisis and Implications for Inequality in Japan. Crepe Discussion Paper 71. Centre for Research and Education for Policy Evaluation. [Google Scholar]
- 92.Treasury The JobKeeper payment: three-month review. The treasury of Australian government. 2020. https://treasury.gov.au/publication/jobkeeper-review
- 93.Australian Broadcasting Commission . 2021. WA Premier Stamps Authority on Labor with Ministry Purge after Colossal Election Win.https://www.abc.net.au/news/2021-03-16/wa-premier-stamps-authority-on-labor-with-cabinet-purge-analysis/13250984 [Google Scholar]
- 94.Tedeschi M. The body and the law across borders during the COVID-19 pandemic. Dialogues in Human Geography. 2020;10(2):178–181. [Google Scholar]
- 95.Ward C. The annihilation of time by space in the COVID-19 pandemic downturn. Dialogues in Human Geography. 2020;20(2):191–194. [Google Scholar]
- 96.Castells M. Basil Black; Oxford: 1989. The Informational City: Information Technology, Economic Restructuring, and the Urban-Regional Process. [Google Scholar]
- 97.Bauman Z. Space and time reunited. Time Soc. 2000;9(2–3):171–185. [Google Scholar]
- 98.Australian Broadcasting Commission Torres Strait communities fear worst-case scenario if virus spreads from PNG. 2021. https://www.abc.net.au/news/2021-03-17/torres-strait-risk-of-covid-coronavirus-virus-spread/13255208
- 99.Widaman K.F. Common factor analysis versus principal component analysis: differential bias in representing model parameters? Multivariate Behav. Res. 2010;28(3):263–311. doi: 10.1207/s15327906mbr2803_1. [DOI] [PubMed] [Google Scholar]
- 100.Czirfusz M. Factor analysis: a pseudo-solution. Space and Society. 2010;24:37–49. [Google Scholar]
- 101.Charlton M., Brunsdon C., Demšar U., Harris P., Fotheringham A.S. 2010. Principal Components Analysis: from Global to Local. 13th AGILE International Conference on Geographic Information Science. (Guimarães, Portugal) [Google Scholar]
- 102.Harris P., Brunsdon C., Charlton M. Geographically weighted principal components analysis. Int. J. Geogr. Inf. Sci. 2011;25(10):1717–1736. [Google Scholar]
- 103.ABS The Australian statistical geography standard (ASGS) remoteness structure. 2016. https://www.abs.gov.au/websitedbs/d3310114.nsf/home/remoteness+structure Accessed on-line on the.
- 106.Wang F., Sainan Z., Liu Y. Territorial traps in controlling the COVID-19 pandemic. Dialogues in Human Geography. 2020;10(2):154–157. [Google Scholar]