SUMMARY
Older adults are at high risk for inappropriate medication use given their myriad medical conditions and medications. Screening efforts may seem overwhelming, but starting with a focused approach and leveraging a team-based strategy can help practicing clinicians gain initial momentum. Future research is needed to strengthen the evidence base for pharmacotherapy in older adults and to elucidate effective and scalable interventions to improve medication safety.
Keywords: Elderly, Geriatrics, Deprescribing, Inappropriate prescribing, Polypharmacy
INTRODUCTION
Medications are the most frequently used form of therapy for medical problems in older adults.1 Older adults often have multiple medical conditions that may require several medications to manage.2 Although pharmacotherapy can improve quality and quantity of life for older adults, there are also inherent risks. Of potential concern is that inappropriate medication use can lead to medication-related problems, such as adverse drug reactions, therapeutic failures, and adverse drug withdrawal events.3 These medication-related problems are associated with morbidity, mortality, and additional health care costs.
Medication appropriateness is a global concept composed of 3 specific domains: (1) overuse, (2) potentially inappropriate medication (PIM) use, and (3) underuse (Table 1). Overuse can be defined as the use of more medications than clinically needed. Examples of medication overuse include duplication of therapy (eg, use of 2 nonsteroidal anti-inflammatory drugs), use of medication with no medical indication (eg, proton pump inhibitor [PPI] without an indication), or use of a medication that is not effective. Overuse is frequently referred to as polypharmacy, although it is important to recognize that the target of screening is unnecessary polypharmacy.4 The Screening Tool of Older Person’s Prescriptions (STOPP) is explicit criteria organized by physiologic system along with explanations to help providers discontinue unnecessary medications (and those that are potentially inappropriate).5,6 PIM use is defined as medication use where the risk outweighs the benefit. Most commonly, PIM use is assessed with explicit criteria, such as the American Geriatrics Society Beers Criteria for Potentially Inappropriate Medication Use in Older Adults, which are guidelines to help clinicians to maximize benefit and minimize harm when prescribing medications to older adults.6,7 Underuse is the lack of medication therapy in those with a clinical indication based on guideline recommendations. It can be due to a host of reasons, including lack of sufficient evidence in older adults (because of their frequent exclusion from studies), inadequate insurance coverage, patient goals of care, and provider perception of the patient’s prognosis, to name a few. Underuse can be assessed with explicit criteria like the Screening Tool to Alert doctors to Right Treatment (START) criteria, which is a validated tool that helps identify prescribing omissions by physiologic system.6,8 Table 2 provides clinical examples of types of prescribing problems by care setting.
Table 1.
Three domains of medication appropriateness
| Domain | Definition | Example Measures |
|---|---|---|
| Overuse | Use of more medications than clinically necessary | Explicit: STOPP Implicit: MAI |
|
| ||
| PIM use | Use where the risk outweighs the benefit | Explicit: Beers Criteria/STOPP Implicit: MAI |
|
| ||
| Underuse | Absence of evidence-based medication use in those with a clinical indication | Explicit: START Implicit: AOU index |
Abbreviations: AOU, assessment of underutilization; MAI, medication appropriateness index.
Table 2.
Examples of medication inappropriateness across care settings in older adults
| Care Setting | Medication Inappropriateness Type | Clinical Hypothetical Example |
|---|---|---|
| Community | Overuse | 87 year-old woman living independently at home taking omeprazole and ranitidine for indigestion |
| PIM use | 76 year-old woman with a history of falls using acetaminophen/diphenhydramine for insomnia | |
| Underuse | 65 year-old man with clinical atherosclerotic cardiovascular disease not receiving a high-intensity statin | |
|
| ||
| Hospital | Overuse | 76 year-old man with no indication for stress ulcer prophylaxis and no history of GERD receiving esomeprazole |
| PIM use | 66 year-old woman with opioid use disorder started on scheduled long-acting oxycodone on admission for osteoarthritis pain | |
| Underuse | 68 year-old man with Parkinson disease whose levodopa was not continued while inpatient due to medication reconciliation error | |
|
| ||
| Nursing home | Overuse | 93 year-old woman with advanced cancer and poor prognosis receiving 16 scheduled medications, including a statin, bisphosphonate, calcium, and vitamin D |
| PIM use | 87 year-old woman with advanced dementia receiving risperidone for new-onset behavioral symptoms without aggression | |
| Underuse | 74 year-old woman with osteoporosis and a history of major osteoporotic fracture not receiving a bisphosphonate | |
Abbreviation: GERD, gastroesophageal reflux disease.
Screening for appropriate medication use in older adults thus ideally involves the use of patient-level information and an up-to-date evidence base. For patient-level information, the following information is needed: (1) an accurate medical problem list, and (2) a comprehensive and up-to-date medication list, including prescription, over-the-counter, and supplement use. In addition, an up-to-date evidence base is needed in order to inform the identification and resolution of medication-related problems. Importantly, patient preferences should always be solicited and incorporated into such screening and any subsequent decision-making regarding pharmacotherapy.
The objectives of this review are as follows:
To describe the impact of medication inappropriateness on health outcomes and the rationale for performing screening;
To examine practical ways in which screening for medication appropriateness can be done across care settings;
To highlight gaps in knowledge and future research needs to inform clinical practice; and
To summarize clinical strategies to screen for medication appropriateness.
IMPACT OF MEDICATION INAPPROPRIATENESS ON HEALTH OUTCOMES
Inappropriate medication use in older adults has been shown to increase the risk of morbidity, mortality, and health care costs. Specifically, overuse, the use of more medications than are medically necessary,9 has been shown to be associated with higher likelihood of unplanned hospitalization in older adults.10,11 PIM use has been found to be associated with confusion, falls, and mortality.7,12 Underuse has been found to be associated with unplanned hospitalization in older adults.13 Furthermore, it has been estimated that for every dollar spent purchasing medications, approximately $1.75 is spent treating drug-related problems.14,15 It is clear that medication-related problems are common and costly to older adults and the health care system.
RATIONALE FOR SCREENING FOR MEDICATION APPROPRIATENESS
The impact of overuse, PIM use, and underuse of medications on health outcomes is a strong part of the rationale for screening for medication appropriateness. Above and beyond that apparent clinical benefit, other potential benefits are likely to exist. We now function in an era of accountable care. In such an era, medication appropriateness screening is a potential high-impact opportunity to not only improve health but also reduce costs to the patient and health care system while improving patient satisfaction.
HOW TO SCREEN FOR MEDICATION APPROPRIATENESS
Overview
Screening for medication appropriateness may seem like a daunting task at first given that older adults often have multiple medical conditions and medications. This clinical complexity leads to many possible appropriate and inappropriate medication-condition and medication-medication combinations. Nonetheless, strategies for incorporating medication appropriateness screening into clinical practice can be efficient and feasible.
Targeted Reviews
One approach to screening is to select a specific therapeutic area or condition. This selection could be based on one or more criteria. Clinicians might select a condition for screening that is highly prevalent in the patient population they serve. For example, focusing on diabetes may narrow the scope of the medication appropriateness screening while addressing a condition of high relevance. Selecting a medication class to target for screening may also be a feasible first step. For instance, screening all patients on antipsychotics can allow for a targeted approach. Expertise of the clinicians in the primary care practice is another parameter for selecting a therapeutic area or condition for screening. If a practice has a pharmacist with prior training in infectious diseases, a focus on infectious illnesses might be a sensible way to initially implement screening. Furthermore, reimbursement is a prudent way to select a screening focus. Conditions included in Medicare’s Hospital Readmissions Reduction Program are a common focus for screening.16 Practices could therefore start by screening for medication appropriateness in patients with acute myocardial infarction, heart failure, and pneumonia. Finally, the preferences and care goals of patients may be an ideal starting place for the implementation of medication appropriateness screening. Patient visits could begin with a reappraisal of patients’ goals of care and preferences. Medications could then be discontinued or initiated through shared decision making to maximally align the care plan with the patients’ values. Two potential questions to ask patients are, “Do you think that you are currently taking too many medications?” and “Which of your medications do you feel is least beneficial to you?” Ultimately, deciding where to start will be determined based on resources, priorities, and quality measures.
Dashboards, Reports, and Electronic Medical Records
The use of dashboards and reports is another way to implement medication appropriateness screening. Dashboards have been successfully developed for patient management.17–20 Dashboards are often condition-specific applications that attempt to provide timely and clinically relevant information for clinician decision making. For example, dashboards might display the number of PIMs that a patient is on or display those patients who are on any PIMs. Peterson and colleagues21 conducted a pilot study of hospitalized adults aged 65 years and older in which they used a computerized PIMs dashboard to identify individuals with at least one administered PIM or a high calculated anticholinergic score. The dashboard was also able to show the 48-hour cumulative narcotic and benzodiazepine administration for each patient. Upon completion of the study, the investigators concluded that the dashboard provided an efficient mechanism for providers to perform medication appropriateness screening while older adults were hospitalized, and to subsequently deliver a point-of-care pharmacist intervention to improve medication use.21 Dashboards are a promising method for medication appropriateness screening, but more evidence is needed to support their full integration.
Computerized decision support programs are being developed to implement inappropriate medication use criteria into clinical practice.22,23 The inclusion of criteria into computerized decision support tools is relatively new. Although neither explicit criteria5,7 nor computerized decision support24 is new, combining these 2 approaches continues to increase in uptake over time.25 For example, the STOPP tool was successfully integrated into a computer-based tool to reduce PIM use in an example published in 2016.26 The investigators conducted an observational study of patients aged ≥65 years admitted to geriatric hospital units in Italy. They found that the computerized tool successfully enabled treating physicians to reduce PIM use. Other forthcoming studies have implemented the Beers Criteria medications as computerized decision support.4 Until more information is available about the incorporation of explicit criteria into computerized decision support tools, standalone online tools and other resources may be a viable solution to assist with medication appropriateness screening.
Online Resources to Screen for Medication Appropriateness
Practices should incorporate tools into their daily workflow that provide structure for the process of medication appropriateness screening. Several resources exist to assist with screening for medication appropriateness and reduction of inappropriate medications (Table 3). All of the available resources aim to systematize the process of screening for medication appropriateness or to easily integrate processes to deprescribe inappropriate medications for primary care clinicians.
Table 3.
Medication appropriateness resources
| Problem | Tool | Type | Source | Link | Description | Pros | Cons |
|---|---|---|---|---|---|---|---|
| PIM use | Deprescribing Guidelines | Web site with downloadable materials | Canadian Deprescribing Network | http://deprescribing.org | Algorithms, patient information brochures, and pamphlets to promote deprescribing of proton pump inhibitors, benzodiazepines and sedative-hypnotics, and glucose-lowering agents | • Free • Written at appropriate health literacy levels for patient use • Evaluated in at least one clinical trial43 |
• Focused on only a few select classes of drugs |
|
| |||||||
| Overuse | A Practical Guide to Stopping Medicines in Older People | Article | Best Practice Journal | http://www.bpac.org.nz/BPJ/2010/April/stopguide.aspx | Article focused on (1) a framework of the factors to consider when deprescribing, including patient wishes, indication and benefit, appropriateness, duration of use, medication adherence, and the prescribing cascade and (2) stepwise guidance for deprescribing | • Contains specific guidance on safe tapering methods for specific drug classes | • Conceptual, less practical in busy clinical situations |
|
| |||||||
| Overuse and PIM use | Deprescribing Resources | Web resource with downloadable materials | Deprescribing Clinical Reference Group, the Australian Government, and Primary Health Tasmania | http://www.primaryhealthtas.com.au/resources/deprescribing | Downloadable fact sheets for providers to guide deprescribing of several medication classes | • Contains general information on principles as well as specific evidence for and against deprescribing for each class • Algorithm for deprescribing included (based on Scott et al,44 article on deprescribing) • Medication-specific algorithm in each fact sheet |
• Needs more evidence of use in practice or effect on health outcomes |
|
| |||||||
| Overuse and underuse | START and STOPP Criteria | Article | O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 2015; 44(2):213–8. | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4339726/ | If/then indicators for starting medication (34 indicators) or stopping medication (80 indicators) in specific clinical situations | • Relatively stronger content, face, and predictive validity than other tools • Potential use as part of computerized decision support |
• Time-consuming to implement without a Web tool or device application |
|
| |||||||
| Overuse and PIM use | MedStopper | Web tool | University of British Columbia, funded by Canadian Institute for Health Information | http://medstopper.com/ | Web-based tool in which clinical information and medication list are entered and a ranked list is provided for medications to be reduced or stopped. Rankings were made by a consensus of experts based on a medication’s potential to improve symptoms, to reduce the risk of future illness, and likelihoodof harm | • Tapering recommendations also given • Incorporates recommendations from Beers Criteria and STOPP Criteria |
• Consensus and ranking process unclear and not published in a peer-reviewed publication |
|
| |||||||
| PIM use | Beers Criteria | Article | American Geriatrics Society Beers Criteria Update Expert Panel. J Am Geriatr Soc 1015;63:2227–46. | http://onlinelibrary.wiley.com/store/10.1111/jgs.13702/asset/jgs13702.pdf?v51&t5j3aupnid&s58bf6c9562ef7ebc924588cfc510941afdb12fb3e | Criteria developed by a 13-member expert panel and periodically updated. Contains a list of drugs to avoid, drug-disease combinations to avoid, drugs to use with caution in renal impairment, and drugs with strong anticholinergic properties |
• Frequently updated to incorporate current evidence • Renal dosing and anticholinergic lists are relative strengths |
• Recommendation is to use in conjunction with other tools, such as the STOPP criteria • Time-consuming to use without Web or computer decision support • Can be searched with a device application that is proprietary ($9.99/year) • Needs more information on alternative medications |
|
| |||||||
| Overuse | Polypharmacy Guidance | Web page and device application | National Health Service Scotland | http://www.polypharmacy.scot.nhs.uk/ | List of 7 steps for medication review and polypharmacy reduction | • Includes evidence that is updated on efficacy and safety of medications, with data presented in terms of number needed to treat and common adverse drug reactions | • Tool is more implicit and may be difficult to use in a busy encounter |
Note: In addition to the tools presented here, several others are available.45
Most busy clinicians are likely to prefer interactive online tools because much of clinical practice now involves use of an electronic medical record (EMR) and online resources. MedStopper (http://medstopper.com/) is one such notable tool.27 The tool focuses on deprescribing of medications and was designed with frail older patients in mind.28 It is important to note that the MedStopper tool only addresses overuse and PIM use, not underuse. It is generally easy to use and intuitive. After indicating whether a patient is frail or not, the user then enters a drug and the condition for which it was prescribed. This process is repeated for each of the drugs that a patient is taking. The tool returns information on whether the drug is likely to improve symptoms, reduce the risk for future illness, and increase the risk for future harm. It also returns advice on tapering, which is especially popular among users.28 No studies have confirmed that use of the tool can improve the efficiency of screening for medication appropriateness.
Utilization of Pharmacists
As medication experts, pharmacists (especially those trained in geriatrics) are ideally suited on the health care team to lead screening efforts for medication appropriateness in older adults.29 Even without geriatrics training, pharmacists across all care settings can learn key principles of geriatric pharmacotherapy to apply to screening activities. One of the main components of screening for medication appropriateness that pharmacists can lead is medication reconciliation. After that, pharmacists can conduct a comprehensive medication review to assess for the presence of overuse, PIM use, or underuse. One specific area that pharmacists can reduce medication-related risk among older adults is regarding fall risk. Importantly, the Centers for Disease Control and Prevention and the American Pharmacists Association recently released a free, online, application-based module called The Pharmacist’s Role in Older Adult Fall Prevention.30 Pharmacists can learn how to identify modifiable risk factors, such as medication use, and how to use effective clinical and community strategies to reduce risk.
Challenges and Considerations
General
The process of screening for medication appropriateness in older adults is challenging and time consuming. Although this process can confer tremendous benefits, it is important to recognize the barriers that might arise. Most notably, in the US health care system, clinical information exists in many different, and often disconnected, systems. Simply obtaining an accurate medical problem list and up-to-date medication list is often a rate-limiting step in this process. Unique challenges and considerations to each care setting are now discussed.
Community
In the community setting, older adults often obtain medications from multiple pharmacies. For example, a study of more than 900,000 Medicare Part D beneficiaries found that 38.1% used multiple pharmacies in a single year.31 Unfortunately, pharmacies from different chains (and sometimes even different pharmacy locations within the same chain) often do not have the capability of real-time data sharing. This lack of data sharing makes obtaining an accurate medication list challenging. In addition, older adults in the community frequently obtain over-the-counter medications and supplements, which are notorious for not being recorded on the older adult’s medication list. Several over-the-counter medications may impose a significant risk for older adults (eg, diphenhydramine, aspirin). Comprehensive medication reconciliation is, therefore, critical to safe and effective screening for medication appropriateness in the community.
Hospital
Transitions between the hospital and other care settings are a major challenge because the clinicians caring for the patient in the hospital often have limited information about the patient’s medication history. When the patient is discharged from the hospital, information about the medication-related decisions made during the hospital course may not be forwarded to the next care setting. Numerous studies have identified medication discrepancies occurring on hospital discharge.32–34 Moreover, medication discrepancies are also likely to arise in the hospital setting because the patient’s critical illness is given priority; medications are stopped or regimens are modified to help stabilize the patient’s acute condition. Furthermore, medication formularies used by hospitals also necessitate medication interchanges and dosage modifications. Clinicians must therefore keep track of a large number of in-hospital medication changes. Even when information regarding medications is available, gaps in communication between the hospital and other settings represent a major barrier.35,36
Nursing home
Major barriers to screening for medication appropriateness in the nursing home (NH) are low physician involvement in daily care and high staff turnover.37,38 Low physician involvement and high staff turnover often translate into limited provider-pharmacist and staff-pharmacist interaction, creating an additional barrier to screening because the pharmacist might not have the necessary information to perform medication appropriateness screening. A lack of connectivity between the NH and other care settings often creates additional communication challenges that prevent meaningful screening. Health care professionals have many competing demands on their time. Literature has shown that when clinicians are faced with multiple competing tasks, one task will often dominate the agenda of a patient encounter, and medication appropriateness screening is often not that dominating task.39 The high clinical complexity of NH residents, especially after they transition from an acute care setting, places even more demands on the clinician. Finally, there is a significant lack of evidence about the outcomes of medication use for frail older individuals with multiple comorbidities, such as those who reside in the NH setting.40 The absence of evidence for NH residents undermines clinicians’ ability to screen for medication appropriateness by creating uncertainty over whether residents will benefit from prescribing or discontinuation of many treatments.
FUTURE DIRECTIONS TO IMPROVE SCREENING FOR MEDICATION APPROPRIATENESS
Adoption of screening for appropriate medication use in older adults can be viewed as a stepwise process (Fig. 1). This process begins with awareness and prioritization, followed by passive and then active screening, and finally full integration. It is important for health care systems to identify their starting point in this process in order to effectively plan their efforts. Two key areas for future directions are development and integration of semiautomated medication appropriateness screening and advancing a US-based national consortium for these efforts.
Fig. 1.
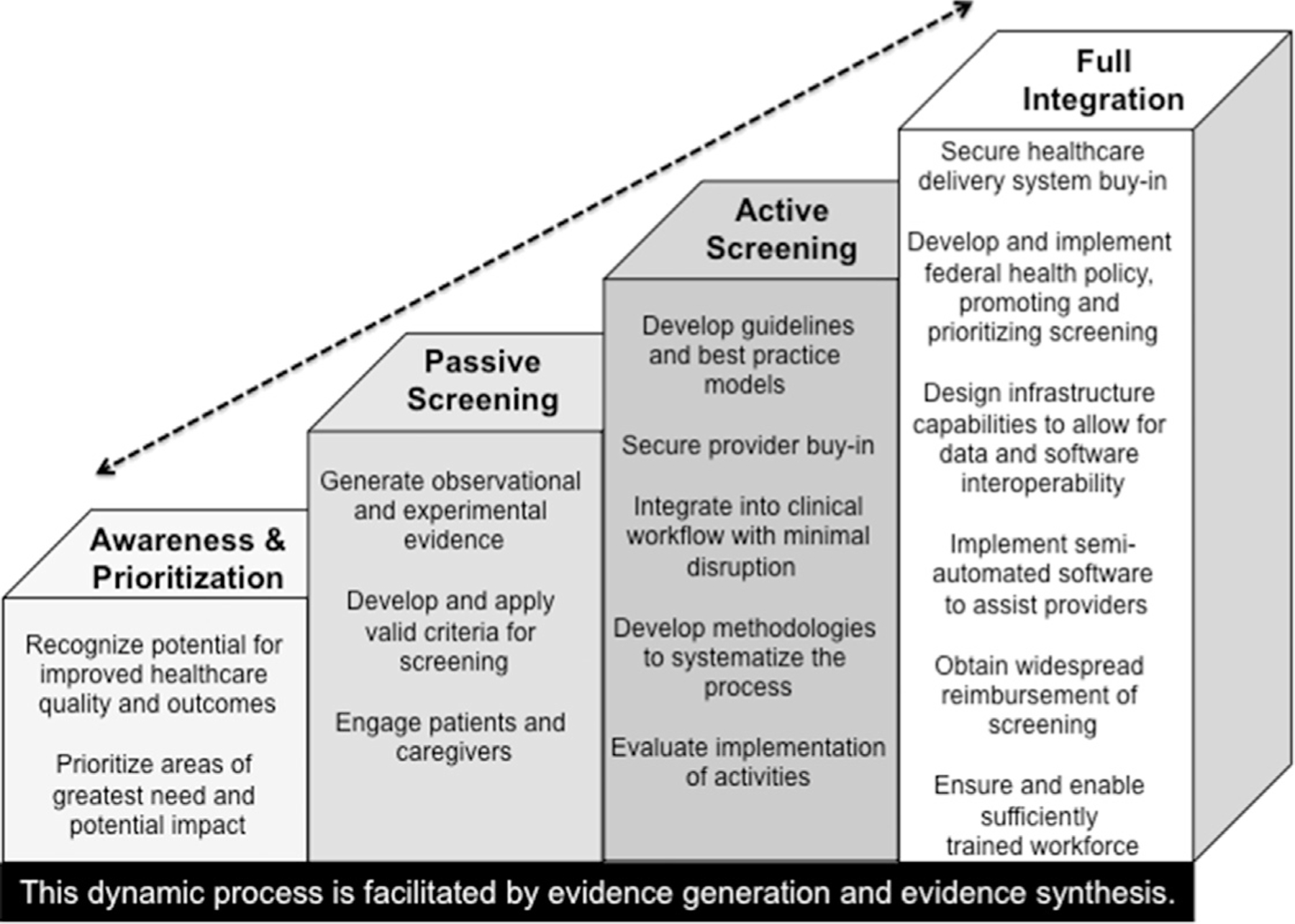
Adoption of appropriate medication use screening in the elderly. (Adapted from IMS Institute for Healthcare Informatics. Patient adoption of mhealth: use, evidence and remaining barriers of mainstream acceptance 2015)
Semiautomation for Faster Medication Appropriateness Screening
The time and effort required to conduct medication appropriateness screening create a critical need for the development of efficient and innovative approaches and tools. The field of computer science may offer some potentially relevant approaches and techniques. In particular, computer science techniques using semiautomated medication appropriateness screening are promising. Semiautomated medication appropriateness screening would rely on the application of text-mining techniques to the EMR. The application of text mining algorithms to EMR data would help to distinguish the highest priority or most urgent problems from those that are lower priority or nonurgent (Fig. 2). After the initial training of the text mining algorithms, little additional effort would be required from the clinician or medical team while the algorithms work in the background as care is provided to patients.
Fig. 2.
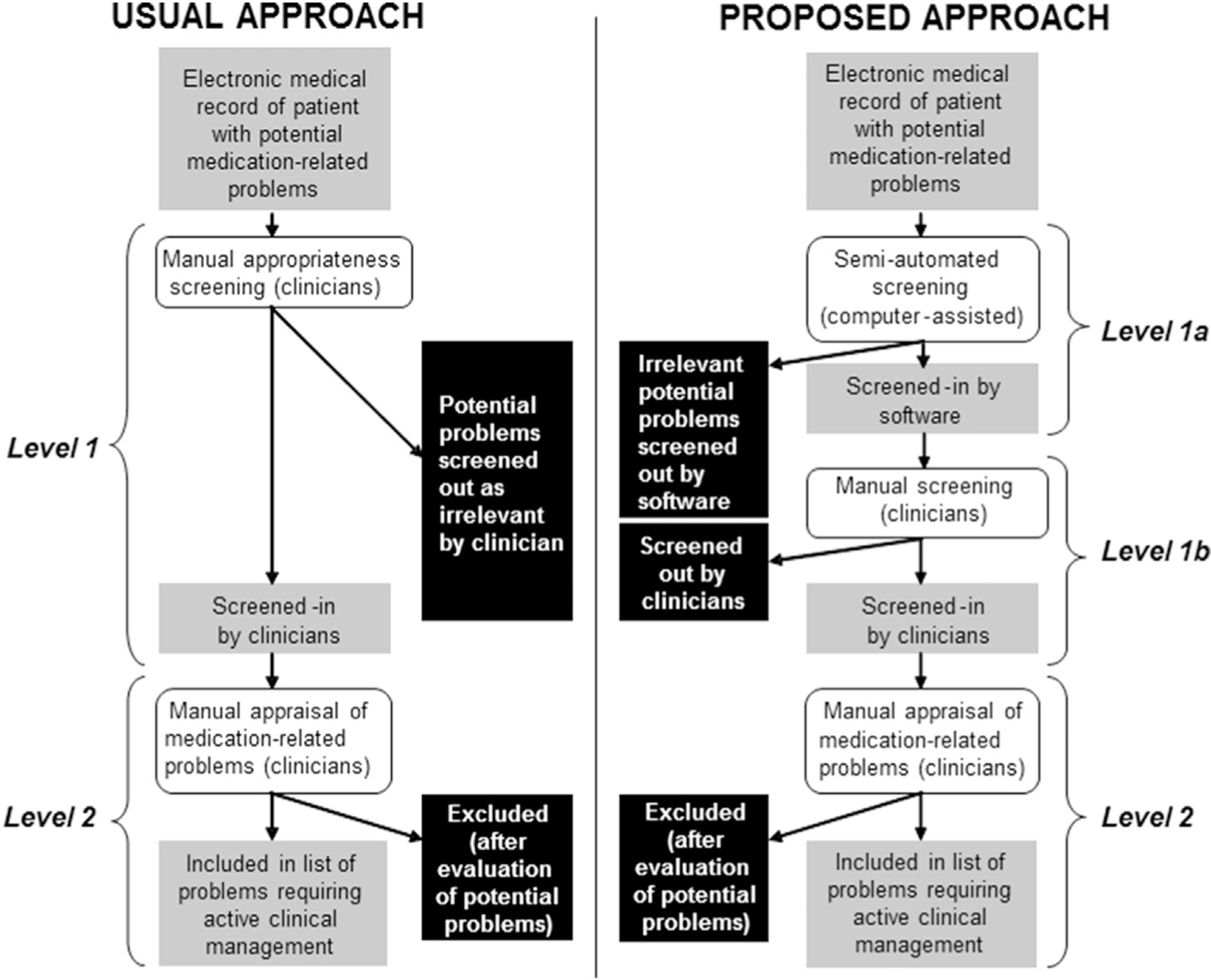
Potential application of statistical pattern learning algorithms to medication appropriateness screening. (Courtesy of Thomas Trikalinos, MD, PhD, Brown University School of Public Health, Providence, RI; adapted with permission.)
National Efforts
Policymakers, health care institutions, and consortia of researchers and clinicians combining efforts might be the best way to address improvements in medication appropriateness. However, to the best of the authors’ knowledge, the US does not currently have such efforts in place. One example is the SIMPATHY Project (Stimulating Innovative Management of Polypharmacy and Adherence in the Elderly). SIMPATHY is a consortium of health care providers, researchers, and policymakers across 10 institutions in several EU countries and led by the Scottish Government. The goal is to promote community-based interventions that will empower patients and provide resources to address appropriate medication use and adherence.41 Similarly, the SENATOR project (Software ENgine for the Assessment & optimization of drug and non-drug Therapy in Older peRsons) is a multinational consortium of researchers from 12 institutions in the EU that is developing a Web-based platform to improve the appropriateness of pharmacologic as well as nonpharmacologic therapy in older adults.42 The group is developing a Web-based medication screening tool based on the START/STOPP criteria and is conducting clinical trials using the tool.42
STRATEGIES FOR IMPROVING SCREENING FOR MEDICATION APPROPRIATENESS
What can we do to improve screening for medication appropriateness in older adults today in light of the current evidence available? The following are some key strategies that are supported by the literature:
Use a team-based approach to ensure accurate medical problem and medication lists. A large body of literature points to the many difficulties associated with medication reconciliation across care settings. In order to minimize these challenges, a team-based approach is ideal for collecting, documenting, and communicating medication reconciliation information. Health care settings with access to a pharmacist should leverage their medication expertise.
Eliminate unnecessary medications. Confirm clinical indications for all medications that a patient is taking; discontinue medications without an indication. Determine the effectiveness of medications for the patient; discontinue medications that are not sufficiently effective. Consider the risk/benefit profile of medications on a routine basis because it may change over time. Focus on commonly used medications that are often overprescribed, have questionable benefit, or have safer alternatives available (eg, PPIs, benzodiazepines, hypnotics).
Identify PIMs and consider dose reduction or discontinuation. Use up-to-date explicit criteria (eg, Beers Criteria, STOPP) as a starting point. Leverage technology to automate as much of this as possible, using dashboards and computer decision support systems.
Identify conditions that are not being treated. Look for reasons that medications might not be used (eg, limited life expectancy, patient preferences, unfavorable risk/benefit profile) and document those in the EMR. Common clinical scenarios that are undertreated in older adults include cardiovascular conditions, osteoporosis, and conditions requiring anticoagulation.
Note that some of the most clinically necessary medications can also be high risk in certain older adults. Although much attention is given to those PIMs listed on explicit criteria such as the Beers Criteria, other medications, such as anticoagulants and glucose-lowering agents, are implicated in the most serious adverse drug events (ie, hospitalization). Avoid focusing solely on those medications listed in explicit criteria for medication appropriateness. Reassess the risk/benefit of these other high-risk medications and relax therapeutic goals (eg, A1c%) as needed.
Pay special attention to high-risk periods, such as following transitions of care. Older adults transitioning across care settings are at the highest risk for inappropriate medication use and the related negative health outcomes. “Double down” on these screening efforts for older adults who have recently had a transition of care.
Take into account the patients’ and caregivers’ preferences about medication use. Attention should be given to understanding patient preferences and goals of care. Only then can patient-specific medication recommendations be made and medication regimen monitoring plans developed and implemented. Shared decision making between the patient and the provider is the goal.
KEY POINTS.
Medication appropriateness is a critical issue in older adults, who are exposed to multiple medications and are more vulnerable to medication-related problems.
Improving medication appropriateness needs to be addressed in all care settings; each care setting (community, hospital, nursing home) presents unique challenges and opportunities regarding appropriate medication use.
Focused screening and intervention to improve medication appropriateness can be accomplished using readily available tools that can be integrated into clinical processes and, in some cases, into the electronic medical record.
Footnotes
Disclosure Statement: Drs A.R. Zullo and Z.A. Marcum are supported by awards from the Agency for Healthcare Research and Quality (5K12HS022998 and 5K12HS022982). Dr H.M. Holmes is supported by a grant from the Cancer Prevention and Research Institute of Texas (RP160674). Dr S.L. Gray is supported by awards from the National Institute on Aging (AG006781 and AG045050–03S1). The authors have no other relevant conflicts of interest to disclose.
REFERENCES
- 1.Newman AB, Cauley JA. The epidemiology of aging Dordrecht (The Netherlands): Springer; 2012. [Google Scholar]
- 2.The American Geriatrics Society Expert Panel Members. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. J Am Geriatr Soc 2012;60(10):E1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiPiro JT. Pharmacotherapy: a pathophysiologic approach 10th edition. New York: McGraw-Hill Education; 2017. [Google Scholar]
- 4.Patterson SM, Cadogan CA, Kerse N, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 2014;(10):CD008165. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher P, Ryan C, Byrne S, et al. STOPP (Screening Tool of Older Person’s prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008;46(2):72–83. [DOI] [PubMed] [Google Scholar]
- 6.Chang CB, Chan DC. Comparison of published explicit criteria for potentially inappropriate medications in older adults. Drugs Aging 2010;27(12):947–57. [DOI] [PubMed] [Google Scholar]
- 7.Radcliff S, Yue JR, Rocco G, et al. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2015;63(11):2227–46. [DOI] [PubMed] [Google Scholar]
- 8.Barry PJ, Gallagher P, Ryan C, et al. START (screening tool to alert doctors to the right treatment)–an evidence-based screening tool to detect prescribing omissions in elderly patients. Age Ageing 2007;36(6):632–8. [DOI] [PubMed] [Google Scholar]
- 9.Tjia J, Velten SJ, Parsons C, et al. Studies to reduce unnecessary medication use in frail older adults: a systematic review. Drugs Aging 2013;30(5):285–307. [DOI] [PubMed] [Google Scholar]
- 10.Marcum ZA, Amuan ME, Hanlon JT, et al. Prevalence of unplanned hospitalizations caused by adverse drug reactions in older veterans. J Am Geriatr Soc 2012;60(1):34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fried TR, O’Leary J, Towle V, et al. Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc 2014;62(12):2261–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marcum ZA, Pugh MJ, Amuan ME, et al. Prevalence of potentially preventable unplanned hospitalizations caused by therapeutic failures and adverse drug withdrawal events among older veterans. J Gerontol A Biol Sci Med Sci 2012; 67(8):867–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meid AD, Lampert A, Burnett A, et al. The impact of pharmaceutical care interventions for medication underuse in older people: a systematic review and meta-analysis. Br J Clin Pharmacol 2015;80(4):768–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: updating the cost-of-illness model. J Am Pharm Assoc (Wash) 2001;41(2):192–9. [DOI] [PubMed] [Google Scholar]
- 15.Bootman JL, Harrison DL, Cox E. The health care cost of drug-related morbidity and mortality in nursing facilities. Arch Intern Med 1997;157(18): 2089–96. [PubMed] [Google Scholar]
- 16.Centers for Medicare and Medicaid Services. Readmissions reduction program (HRRP) 2016. Available at: https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed May 5, 2017.
- 17.Zaydfudim V, Dossett LA, Starmer JM, et al. Implementation of a real-time compliance dashboard to help reduce SICU ventilator-associated pneumonia with the ventilator bundle. Arch Surg 2009;144(7):656–62. [DOI] [PubMed] [Google Scholar]
- 18.Anderson D, Zlateva I, Khatri K, et al. Using health information technology to improve adherence to opioid prescribing guidelines in primary care. Clin J Pain 2015;31(6):573–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dixon BE, Jabour AM, Phillips EO, et al. An informatics approach to medication adherence assessment and improvement using clinical, billing, and patient-entered data. J Am Med Inform Assoc 2014;21(3):517–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American College of Clinical Pharmacy, McBane SE, Dopp AL, et al. Collaborative drug therapy management and comprehensive medication management-2015. Pharmacotherapy 2015;35(4):e39–50. [DOI] [PubMed] [Google Scholar]
- 21.Peterson JF, Kripalani S, Danciu I, et al. Electronic surveillance and pharmacist intervention for vulnerable older inpatients on high-risk medication regimens. J Am Geriatr Soc 2014;62(11):2148–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meulendijk MC, Spruit MR, Drenth-van Maanen AC, et al. Computerized decision support improves medication review effectiveness: an experiment evaluating the STRIP assistant’s usability. Drugs Aging 2015;32(6):495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Sullivan D, O’Mahony D, O’Connor MN, et al. Prevention of adverse drug reactions in hospitalised older patients using a software-supported structured pharmacist intervention: a cluster randomised controlled trial. Drugs Aging 2016;33(1):63–73. [DOI] [PubMed] [Google Scholar]
- 24.Tamblyn R, Huang A, Perreault R, et al. The medical office of the 21st century (MOXXI): effectiveness of computerized decision-making support in reducing inappropriate prescribing in primary care. CMAJ 2003;169(6):549–56. [PMC free article] [PubMed] [Google Scholar]
- 25.Yourman L, Concato J, Agostini JV. Use of computer decision support interventions to improve medication prescribing in older adults: a systematic review. Am J Geriatr Pharmacother 2008;6(2):119–29. [DOI] [PubMed] [Google Scholar]
- 26.Grion AM, Gallo U, Tinjala DD, et al. A new computer-based tool to reduce potentially inappropriate prescriptions in hospitalized geriatric patients. Drugs Aging 2016;33(4):267–75. [DOI] [PubMed] [Google Scholar]
- 27.Beta MedStopper. 2017. Available at: http://medstopper.com/. Accessed April 27, 2017.
- 28.Cassels A. ‘Can I stop even one of these pills?’ The development of a tool to make deprescribing easier. Eur J Hosp Pharm Sci Pract 2017;24(1):3–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee JK, Slack MK, Martin J, et al. Geriatric patient care by U.S. pharmacists in healthcare teams: systematic review and meta-analyses. J Am Geriatr Soc 2013;61(7):1119–27. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. STEADI - Older Adult Fall Prevention 2017. Available at: https://www.cdc.gov/steadi/training.html. Accessed April 27, 2017.
- 31.Marcum ZA, Driessen J, Thorpe CT, et al. Effect of multiple pharmacy use on medication adherence and drug-drug interactions in older adults with Medicare Part D. J Am Geriatr Soc 2014;62(2):244–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boockvar KS, Liu S, Goldstein N, et al. Prescribing discrepancies likely to cause adverse drug events after patient transfer. Qual Saf Health Care 2009;18(1):32–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boockvar KS, Carlson LaCorte H, Giambanco V, et al. Medication reconciliation for reducing drug-discrepancy adverse events. Am J Geriatr Pharmacother 2006;4(3):236–43. [DOI] [PubMed] [Google Scholar]
- 34.Boockvar K, Fishman E, Kyriacou CK, et al. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long-term care facilities. Arch Intern Med 2004;164(5):545–50. [DOI] [PubMed] [Google Scholar]
- 35.King BJ, Gilmore-Bykovskyi AL, Roiland RA, et al. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc 2013;61(7):1095–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shah F, Burack O, Boockvar KS. Perceived barriers to communication between hospital and nursing home at time of patient transfer. J Am Med Dir Assoc 2010;11(4):239–45. [DOI] [PubMed] [Google Scholar]
- 37.Shield R, Rosenthal M, Wetle T, et al. Medical staff involvement in nursing homes: development of a conceptual model and research agenda. J Appl Gerontol 2014; 33(1):75–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stone R, Harahan MF. Improving the long-term care workforce serving older adults. Health Aff 2010;29(1):109–15. [DOI] [PubMed] [Google Scholar]
- 39.Miles RW. Cognitive bias and planning error: nullification of evidence-based medicine in the nursing home. J Am Med Dir Assoc 2010;11(3):194–203. [DOI] [PubMed] [Google Scholar]
- 40.Crystal S, Gaboda D, Lucas J, et al. Assessing medication exposures and outcomes in the frail elderly: assessing research challenges in nursing home pharmacotherapy. Med Care 2010;48(6 Suppl):S23–31. [DOI] [PubMed] [Google Scholar]
- 41.Scottish Government Health and Social Care Directorates. Stimulating innovation management of polypharmacy and adherence in the elderly 2017. Available at: http://www.simpathy.eu/. Accessed June 10, 2017.
- 42.SENATOR. Development and clinical trials of a new Software ENgine for the Assessment & optimization of drug and non-drug Therapy in Older peRsons 2017. Available at: https://www.senator-project.eu/. Accessed June 10, 2017.
- 43.Tannenbaum C, Martin P, Tamblyn R, et al. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med 2014;174(6):890–8. [DOI] [PubMed] [Google Scholar]
- 44.Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med 2015;175(5):827–34. [DOI] [PubMed] [Google Scholar]
- 45.Bulloch MN, Olin JL. Instruments for evaluating medication use and prescribing in older adults. J Am Pharm Assoc (2003) 2014;54(5):530–7. [DOI] [PubMed] [Google Scholar]


