Abstract
Purpose of review:
To present the latest developments in esophageal motility testing and summarize the current paradigm of esophageal motility disorders.
Recent findings:
While high-resolution esophageal pressure topography interpreted according to the Chicago Classification represents the gold standard to evaluate esophageal motility, recent studies highlight the additional value of novel manometric applications. Novel applications include provocative measures to assess for obstructive physiology at the esophagogastric junction (EGJ), esophageal peristaltic reserve, and rumination and supragastric belching disorders. Furthermore high-resolution impedance manometry provides assessment of bolus flow in relation to pressure changes. Distinct from manometry, the endolumenal functional lumen imaging probe examines esophageal motor response to distension to provide complementary and alternative data with regards to EGJ function and esophageal body motor function. Barium esophagram with timed swallow and barium tablet continues to be an important esophageal motility test. Furthermore, current use of multichannel intraluminal impedance pH monitoring extends beyond reflux monitoring to measure reflux clearance and esophageal epithelial integrity.
Summary:
The diagnostic armamentarium for esophageal motility disorders has expanded tremendously to include a multitude of sophisticated tools. Advancements in diagnostic technology and understanding of esophageal physiology have shifted the field to more precisely characterize esophageal motility and guide phenotype driven management.
Keywords: Esophageal manometry, pH monitoring, EndoFLIP, Mucosal impedance, barium esophagram, esophageal physiology, EGJ obstruction
INTRODUCTION
Major diagnostic advances in the twenty-first century have transformed the landscape of esophageal motility disorders. The transition from conventional line tracing manometry to high-resolution esophageal pressure topography plots marks the beginning of a dramatic evolution in esophageal motility. Today, clinicians are equipped with an array of diagnostic tools (i.e., high-resolution impedance manometry (HRIM), endolumenal functional lumen imaging probe (EndoFLIP), and barium esophagram), each with its own distinct applications, to evaluate esophageal motility [Table 1]. The rapid expansion of diagnostic technologies over the past five years has reframed the understanding of key physiologic concepts such as obstructive esophageal physiology, peristaltic responses to an intraluminal bolus and gastroesophageal reflux, and the function of the anti-reflux barrier. Leveraging these sophisticated tools and the increased appreciation of esophageal physiology, the clinical paradigm has shifted towards utilizing complimentary and novel technologies to guide phenotype driven treatment for esophageal motility disorders. Therefore, the purpose of this review is to present the latest developments in esophageal motility testing, and summarize the current day clinical paradigm to evaluate esophageal motility dysfunction.
Table 1.
Applications of current-day diagnostic tools to assess esophageal physiology
| Diagnostic Tool | EGJ Obstructive Physiology | Esophageal Peristalsis | Reflux Physiology | Epithelial integrity |
|---|---|---|---|---|
| HRIM | • IRP • Solid test meal • Rapid drink challenge • Bolus flow time, EII ratio |
• Distal contractile integral • Peristaltic reserve with multiple rapid swallow |
• EGJ morphology • Post-prandial HRIM |
|
| EndoFLIP | • EGJ distensibility index | • Distension induced contractile response | • EGJ distensibility index | |
| Barium Esophagram | • Timed swallow • Tablet transit |
• Barium transit | • Post-antireflux intervention anatomy | |
| MII-pH | • Post-reflux swallow peristaltic wave index (PSPWi) | • Acid exposure time • Reflux events (acid/weakly acidic/non-acidic) |
• Mean nocturnal baseline impedance | |
| Mucosal impedance | • Direct mucosal impedance |
Esophagogastric junction (EGJ), High-resolution impedance manometry (HRIM), Multichannel intraluminal impedance (MII); Functional lumen imaging probe (FLIP); Integrated relaxation pressure (IRP)
DEVELOPMENTS IN ESOPHAGEAL MOTILITY DIAGNOSTICS
High-Resolution Esophageal Pressure Topography
The current standard to evaluate non-obstructive esophageal dysphagia is esophageal manometry in the form of high-resolution manometry (HRM) with esophageal pressure topography (EPT). Compared with conventional line tracings, a major advantage of HRM with EPT is the ability to convert pressure tracings into sophisticated and illustrative spatiotemporal plots of esophageal contractility over esophageal length and time, also referred to as Clouse plots in recognition of the visionary Ray Clouse. (1) Along with the evolution of HRM with EPT, another landmark advancement in esophageal motility has been the development of the Chicago Classification, a standardized hierarchical diagnostic classification scheme of esophageal motility disorders, which is currently in version 3.0. (2–5) These technological and classification advances have transformed what was once considered a complex technology into a more easily understood and interpretable diagnostic tool. In a recent prospective study of twelve physicians, Carlson et al. found superior diagnostic accuracy and inter-rater agreement for HRM with EPT using the Chicago Classification compared to conventional line tracings and classification scheme across both experienced gastroenterologists and inexperienced gastroenterology trainees. (6) Despite improved diagnostic interpretation with HRM with EPT, the widespread adoption of HRM across clinical practices exceeds the ability to adequately train and ensure proficiency of interpretation. As such, developing a standardized method to train and assess competency of interpretation is current priority in clinical research. (7–11)
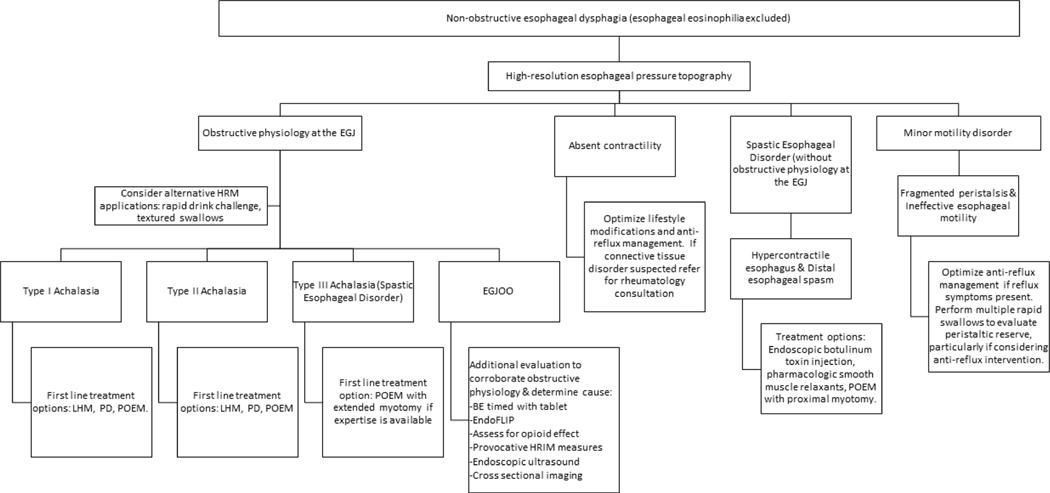
While the evolution of HRM with EPT and the Chicago Classification represent quintessential advancements in esophageal motility, novel applications of HRM have emerged over the past five years and currently play a critical role in the evaluation of esophageal motility. Multiple studies demonstrate that evaluation for obstructive physiology at the esophagogastric junction (EGJ) is imperfect when based solely on the Chicago Classification, and consequently recent studies have focused on identifying other HRM metrics to assess nuanced physiologic properties. For instance, provocation is increasingly used during HRM to evaluate for EGJ obstructive physiology and esophageal peristaltic reserve [Figure 1]. Furthermore, HRM catheters paired with multichannel impedance sensors provide valuable information regarding bolus flow properties. The specific physiologic roles of these novel HRM applications are discussed later in this review.
Figure 1.
Current day clinical approach to the evaluation of non-obstructive esophageal dysphagia.
Endolumenal Functional Lumen Imaging Probe (EndoFLIP)
The newest diagnostic advancement to assess esophageal motility is the endolumenal functional lumen imaging probe (EndoFLIP). Distinct from esophageal manometry, EndoFLIP leverages high-resolution impedance planimetry during volume controlled distension to assess esophageal motor responses to distension rather than deglutition. FLIP topography, the most recent version of EndoFLIP, enables real time topographical assessment of distension induced esophageal motor characteristics. EndoFLIP assemblies are available in two different balloon sizes: the shorter balloon (EF-325; 8 cm in length) primarily assesses the EGJ, and the longer balloon (EF-322; 16 cm in length) assesses both the EGJ and esophageal body. (12)
Barium Esophagram
Prior to widespread adoption of upper endoscopy and esophageal manometry, barium esophagram was the mainstay test to evaluate esophageal motility disorders and gastroesophageal reflux. Today, two applications of barium esophagram remain particularly useful in the evaluation of esophageal motility. Timed barium swallow assesses esophageal emptying of barium sulfate at 1, 2 and 5 minutes, and has previously been shown to have a prognostic role in predicting symptomatic remission following pneumatic dilation. (13) Barium esophagram with a 13-mm barium tablet is increasingly performed in the evaluation of solid food dysphagia. (14)
CURRENT DAY APPLICATIONS OF ESOPHAGEAL PHYSIOLOGY TESTING
Esophageal motility serves to transport oropharyngeal bolus into the stomach and prevent gastroesophageal reflux episodes. Bolus transport is predominantly achieved by primary peristalsis in response to swallowing. Following oropharyngeal transfer of bolus through a relaxed upper esophageal sphincter a coordinated esophageal motor response begins and proceeds distally while the lower esophageal sphincter relaxes to accommodate the bolus. Following bolus transit the lower esophageal sphincter closes with a prolonged contraction to prevent retrograde movement of bolus into the esophagus. At rest the lower esophageal sphincter is tonically contracted and overlaps with the crural diaphragm to maintain a high pressure barrier to gastroesophageal reflux.
Esophagogastric Junction Obstructive Physiology
Historically, the hallmark esophageal motility disorder was achalasia, characterized by abnormal relaxation of the lower esophageal sphincter and absence of esophageal peristalsis. In recent years the simplistic notion of “achalasia” has significantly evolved to recognize heterogeneous motility patterns presenting with obstructive physiology at the EGJ, each requiring a distinct management approach. Generally, obstruction at the EGJ manifests as dysphagia, regurgitation, and/or chest pain. HRM is the current gold standard to evaluate obstructive esophageal symptoms once a mechanical obstruction, eosinophilic esophagitis and other inflammatory disorders of the esophagus have been excluded [Figure 2].
EGJ Obstructive Physiology: HRM
According to the Chicago Classification v3.0 four esophageal motility disorders present with EGJ obstructive physiology, or an elevated median integrated relaxation pressure (IRP). The IRP is a measure of deglutitive relaxation based on four seconds of the lowest mean axial pressure, continuous or discontinuous, across the lower esophageal sphincter. The classic disorder is type I achalasia where 100% of esophageal peristalsis is failed (i.e., distal contractile integral 0 to 100 mmHg-cm-s). Type II achalasia is diagnosed when 100% of esophageal peristalsis is failed and 20% or more of swallows exhibit panesophageal pressurization; type II achalasia is considered to represent a precursor to type I achalasia in disease progression. Type III achalasia is present when 20% or more of swallows exhibit spasticity or prematurity (i.e., distal latency less than 4.5 seconds), and is akin to spastic achalasia. When criteria for achalasia subtypes are otherwise not met the diagnosis is esophagogastric junction (EGJ) outflow obstruction. (15)
Novel Applications of HRM to Assess for EGJ Obstructive Physiology
While the Chicago Classification of esophageal motility disorders relies on the median IRP of ten supine wet swallows to assess EGJ function, recent novel applications of HRM have been described as complementary means to assess for EGJ obstructive physiology [Figure 1]. These methods are particularly useful when the median IRP is borderline and/or the esophageal motor diagnosis per Chicago Classification is incongruent with other diagnostic testing.
Rapid Drink Challenge
The rapid drink challenge assesses EGJ response to intake of 200 mL of water within 30 seconds. In 2017, Marin et al. reported that an IRP during a rapid drink challenge of 8 mmHg or greater is indicative of EGJ outflow obstruction, and 12 mmHg or greater is consistent with achalasia. (16) In the setting of EGJ obstructive physiology, the rapid drink challenge may also incite panesophageal pressurization. (17, 18) When performed with high-resolution impedance manometry (HRIM), bolus height for up to 5 minutes following a rapid rink challenge can indicate adequacy of bolus clearance. (19)
Textured Swallows
Bolus consistency influences esophageal motor function. Sweis et al. previously demonstrated that solid swallows performed in an upright position were associated with elevated IRPs. (20) Along these lines, Ang and colleagues found that inclusion of solid swallows in the manometry protocol resulted in an increased diagnostic yield of a major motility disorder. (21) Therefore, evaluation of EGJ function during textured swallows seems to be particularly useful for patients in whom obstructive physiology is strongly suspected. (22)
Bolus Flow Properties Utilizing HRIM
HRM combined with multichannel intraluminal esophageal impedance sensors, referred to as high-resolution impedance manometry (HRIM), provides an enhanced assessment of esophageal motility in relation to bolus flow properties. Since the advent of HRIM, novel metrics to assess bolus retention and EGJ obstructive physiology have been described. The trans-EGJ bolus flow time (BFT) is a novel HRIM application to predict flow across the EGJ. In a study of 60 patients with achalasia and 15 healthy controls, Lin et al. reported a significantly lower median BFT among the achalasia group. Lin and colleagues additionally identified abnormal BFTs in patients with a clinical suspicion of achalasia yet normal median IRP values on HRM. (23) The esophageal impedance integral (EII) ratio is another new HRIM metric to compare the bolus volume during and following the swallow as a measure of bolus retention. In a recent study the EII ratio distinguished between patients with and without dysphagia despite normal or minor motility motor disorders on HRM. (24–28) Thus, HRIM metrics such as the BFT and EII ratio offer sophisticated and complimentary methods to assess bolus flow properties in the evaluation of dysphagia and EGJ outflow obstruction. However, inclusion of these metrics in software analytics and classification algorithms is needed to increase adoption in clinical settings.
EGJ Obstructive Physiology: EndoFLIP
Distinct from HRM, EndoFLIP evaluates esophageal motor responses to distension rather than deglutition. With regards to EGJ outflow obstructive physiology, EndoFLIP can be used to assess distensibility of the EGJ via the EGJ-distensibility index (EGJ-DI). The EGJ-DI is calculated by dividing the narrowest cross sectional area through the EGJ over the intra-bag pressure in units of mm2/mmHg. (12) Lower EGJ-DI values suggest reduced EGJ distensibility whereas higher EGJ-DI values suggest increased EGJ distensibility. (29) Synthesis of EGJ distensibility and esophageal contractile responses, gleaned from the catheter with the 16 cm balloon (EF-322), can reveal a FLIP topography motility classification. The esophageal contractile response in the setting of a low EGJ-DI can suggest particular subtypes of achalasia or EGJ outflow obstruction. For instance, a low EGJ-DI with an absent contractile response may be similar to an achalasia pattern with absent contractility such as manometric type I or type II achalasia. On the other hand a low EGJ-DI with the presence of repetitive retrograde contractions (RRCs) may represent a spastic achalasia pattern. (30) Recent studies examining EndoFLIP also report detection of impaired EGJ relaxation on EndoFLIP not otherwise observed with manometry, and suggest that EndoFLIP may have a complementary and/or alternative role to the gold standard of esophageal manometry in the evaluation of obstructive physiology at the EGJ.(31, 32)
EGJ Obstructive Physiology: Barium Esophagram
Barium esophagram continues to play a critical role in the evaluation of obstructive physiology at the EGJ. Blonski et al. recently examined barium esophagram findings among patients with achalasia or EGJ outflow obstruction compared to non-achalasia controls, and identified that a barium column height of 2 cm at 5 minutes was 85% sensitive and 86% specific for achalasia. Furthermore, combining the timed barium esophagram results with non-passage of a 13 mm barium tablet at 5 minutes increased the diagnostic yield from 79.5% to 100%. (14) When assessing for EGJ obstructive physiology, barium esophagram should be considered a complementary diagnostic tool, particularly when the protocol includes timed barium swallow and a barium tablet. Barium esophagram, timed with tablet, is also a reasonable diagnostic alternative if patients are unable to tolerate manometry.
EGJ Obstructive Physiology: Treatment
When EGJ relaxation is impaired with absent contractility (i.e., manometric type I and II achalasia) the treatment goal is to relieve the outflow obstruction across the EGJ. This can be accomplished by laparoscopic heller myotomy (LHM), pneumatic dilation, or per-oral endoscopy myotomy. Distinguishing achalasia sub-types has important management and prognostic implications. In the European achalasia trial combined success rates for LHM or pneumatic dilation for type II achalasia were 96% compared to 81% for type I and 66% for type III achalasia. LHM and PD had similar rates of success in type I achalasia, though the success rate of PD was 100% compared to LHM (93%) in type II achalasia. (33) Per-oral endoscopy myotomy (POEM) is the newest treatment option for motility disorders with EGJ obstructive physiology, with reported 90% success rates at 3-years across achalasia sub-types. (34)
While the treatment approaches for achalasia sub-types is well defined, the management for EGJ outflow obstruction remains a challenge. Etiologies of EGJ outflow obstruction vary from an early variant of achalasia, extrinsic vascular obstruction, sliding hiatal hernia, opiate effect, or even a false-positive measurement. Further diagnostic testing to corroborate the obstructive physiology and evaluate for sources of obstruction with cross-sectional imaging, endoscopic ultrasound, barium esophagram with tablet, and/or EndoFLIP are warranted prior to treatment of EGJ outflow obstruction. It is also imperative to attempt opioid discontinuation in the setting of a potential opioid effect. (35)
Spastic Esophageal Disorders
The common feature in spastic esophageal disorders is obstructive esophageal contractility, with or without obstructive physiology at the EGJ. In distal esophageal spasm the obstructive physiology is a manifestation of premature esophageal contractility (i.e., distal latency less than 4.5 seconds). Type III, or spastic, achalasia is diagnosed when premature obstructive contractility is paired with obstructive physiology at the EGJ. Obstructive esophageal contractility in hypercontractile, or Jackhammer, esophagus is a result of prolonged and concurrent contractions of the smooth muscle (i.e., distal contractile integral greater than 8,000 mmHg-cm-s) which delays the normal post-peristaltic recovery. (35) On FLIP topography spastic esophageal motility may manifest as three or more consecutively and consistently spaced retrograde contractions, referred to as repetitive retrograde contractions (RRCs). (29)
The current first line treatment option for type III achalasia is POEM when the expertise is available. (36) A recent meta-analysis of eight uncontrolled observational studies reported a weighted pooled response rate of 92% (95% CI 84–96%) to POEM in type III achalasia with an average extended myotomy length of 17.2 cm. (37) POEM with extended proximal myotomy is also a treatment option across the other spastic esophageal disorders. (37)
Hypomotile Esophageal Disorders
Hypomotile esophageal disorders encompass the group of major motility disorders where contractility is entirely absent (i.e., absent contractility) and minor motility disorders. Minor motility disorders are esophageal motility patterns in the setting of a normal median IRP that may be observed in healthy volunteers, and are often seen in gastro-esophageal reflux pathology. Manometric minor motility disorders include ineffective esophageal motility, which is diagnosed when 50% or more of swallows are ineffective (i.e., distal contractile integral < 450 mmHg-cm-s), and fragmented peristalsis, which is diagnosed when more than 50% of swallows have breaks longer than 5cm in the esophageal peristaltic body. (5)
Esophageal peristalsis is the primary innate mechanism to clear gastro-esophageal reflux, and over the past 5 years there has been a growing interest to link metrics of esophageal peristalsis with pathologic gastro-esophageal reflux disease. Multichannel intraluminal impedance pH (MII-pH) is increasingly used to specifically assess post-reflux clearance as well as bolus stasis as a marker of esophageal peristalsis.(38, 39) The post-reflux swallow induced peristaltic wave (PSPW) index on MII-pH assesses the efficacy of esophageal reflux clearance by measuring the proportion of reflux events that are restored within 30 seconds. The PSPW index is reportedly lower in erosive and non-erosive reflux compared to controls and patients with functional heartburn. (40) MII-pH also offers the opportunity to examine esophageal impedance as a surrogate of esophageal mucosal integrity and esophageal clearance. The mean nocturnal baseline impedance (MNBI) on MII-pH takes the mean of impedance measurements at three 10-minute time periods during the overnight rest period, and is reported to be lower among patients with gastroesophageal reflux disease that respond to anti-reflux measures compared to those who do not. (41) Building on the same concept, direct mucosal impedance was introduced over the past five years as a real-time technology performed during endoscopy to assess mucosal integrity. Direct esophageal mucosal impedance during endoscopy has been found to accurately identify patients with erosive esophagitis or positive ambulatory reflux monitoring in multiple studies. Also, mucosal impedance is significantly lower in patients with objective gastroesophageal reflux disease compared to those without, and furthermore, mucosal impedance increases after treatment with PPIs in gastroesophageal reflux disease. (42)
Another novel application of HRM as it relates to hypomotile esophageal conditions is the ability to prognosticate risk of post-operative dysphagia following anti-reflux surgery via the multiple rapid swallow. Multiple rapid swallows are administered through five 2-mL swallows taken less than 4 seconds apart and assess the integrity of deglutitive inhibition and peristaltic reserve. Reduced contractile reserve may indicate gastroesophageal reflux disease at an increased risk of dysphagia following fundoplication. (43–45)
Anti-Reflux Barrier
An additional value of HRM is the ability to assess the anatomy and function of the anti-reflux barrier. With regards to anatomy, HRM examines the spatial relationship between the crural diaphragm and LES, referred to as the EGJ morphology, to assess for hiatal hernia. (46) HRIM is also able to concurrently assess intragastric and intrathoracic pressure in relation to flow of gastric contents, and thereby identifies rumination, belching, and transient lower esophageal sphincter relaxation events. As such, post-prandial HRIM is a novel application that monitors symptoms and manometric characteristics following administration of an aversive digestive stimuli. (47–49) Post-prandial HRIM is increasingly used in the evaluation of non-response to proton pump inhibitors (PPIs) to assess for rumination or supragastric belching, and guide phenotype driven management. (50)
CONCLUSION
The evolution of HRM with EPT and the Chicago Classification transformed the field of esophageal motility by not only introducing sophisticated interpretation methods, but moreover generating a new excitement and appreciation for esophageal physiology. Today, the clinical approach to esophageal motility extends far beyond assessing whether EGJ relaxation is adequate with oral of intake of water while laying down. In recognition of the fact that the median IRP in a supine position is an imperfect measure of EGJ obstruction, a multitude of alternative methods to assess EGJ function are available such as provocative maneuvers on HRIM, volume controlled distension of the EGJ using EndoFLIP, and barium esophagram with timed swallow and a barium tablet. An enhanced appreciation of the obstructive physiology in the smooth muscle portion of the esophagus among spastic esophageal disorders enables more precise treatment via proximal myotomy with POEM to effectively alleviate spastic obstructions. Though reflux monitoring and esophageal motility testing were historically distinct diagnostic modalities, today a multitude of complementary tests (i.e., manometry, MII-pH, and direct mucosal impedance) are used to assess the complex relationship between gastroesophageal reflux physiology, esophageal peristalsis, and epithelial integrity.
Never before have gastroenterologists evaluating patients with suspected esophageal motility disorders found themselves with such a robust armamentarium of diagnostics and nuanced appreciation of physiology. The wealth of information enables gastroenterologists to synthesize sophisticated data points to guide personalized management of esophageal motility disorders. Furthermore, multimodal availability of diagnostic tools offers complementary information in borderline or unclear scenarios. Looking ahead, expanding roles of novel tools performed during upper endoscopy, such as EndoFLIP or mucosal impedance, may with further study obviate the need for more cumbersome testing. In addition, identifying clinically relevant phenotypes of EGJ outflow obstruction will enable precise treatment. Finally, in order to bridge the growth of research findings to optimized patient care future efforts must focus on patient-centered outcomes, assure competency in diagnostic interpretation, and upgrade software and classification schematics.
Disclosures/Declaration of Funding:
RY: Consultant for Ironwood, Diversatek Healthcare, Medtronic; Supported by NIH R01 DK092217 (Pandolfino), and ACG Junior Faculty Development Award (Yadlapati). GTF: NIH 1K24DK100303, Consultant for Shire, Co-Founder of EnteroTrack, Royalties from UpToDate
Abbreviations:
- EndoFLIP
Endoluminal functional luminal imaging probe
- MII-pH
Multichannel intraluminal impedance-pH
- HRM
High-resolution manometry
- EPT
Esophageal pressure topography
- EGJ
Esophagogastric junction
- IRP
Integrated relaxation pressure
- LES
Lower esophageal sphincter
- POEM
Per-oral endoscopy myotomy
- AGA
American Gastroenterological Association
- HRIM
High resolution impedance manometry
- EII
Esophageal impedance integral
- PPI
Proton pump inhibitor
- EJG-DI
EGJ-distensibility index
- RACs
Repetitive antegrade contractions
- RRCs
Repetitive retrograde contractions
- MNBI
Mean nocturnal baseline impedance
- GERD
Gastroesophageal reflux disease
- PSPW
Post-reflux swallow induced peristaltic wave
Footnotes
Compliance with Ethical Standards
Conflict of Interest
Rena Yadlapati is a consultant for Ironwood Pharmaceuticals, Diversatek, and Medtronic, and received grants from NIHNIDDK and the American College of Gastroenterology.
Glenn Furuta reports grants from NIHNIDDK and personal fees from Shire, outside the submitted workIn addition, Dr. Furuta has a patent (EnteroTrack) licensed, and a patent (UpToDate) with royalties paid. Paul Menard-Katcher declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
••Of major importance
- 1.Clouse RE, Prakash C. Topographic esophageal manometry: an emerging clinical and investigative approach. Dig Dis. 2000;18(2):64–74. [DOI] [PubMed] [Google Scholar]
- 2.Kahrilas PJ, Ghosh SK, Pandolfino JE. Esophageal motility disorders in terms of pressure topography: the Chicago Classification. J Clin Gastroenterol. 2008;42(5):627–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roman S, Holloway R, Keller J, Herbella F, Zerbib F, Xiao Y, et al. Validation of criteria for the definition of transient lower esophageal sphincter relaxations using high-resolution manometry. Neurogastroenterol Motil. 2016. [DOI] [PubMed]
- 4.Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293(4):G878–85. [DOI] [PubMed] [Google Scholar]
- 5. Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74. • The Chicago Classification version 3.0 was developed by the International High Resolution Manometry Working Group and published in 2015. It is the current classification scheme for esophageal high-resolution manometry and has transformed the clinical diagnostic approach to esophageal motility disorders.
- 6. Carlson DA, Ravi K, Kahrilas PJ, Gyawali CP, Bredenoord AJ, Castell DO, et al. Diagnosis of Esophageal Motility Disorders: Esophageal Pressure Topography vs. Conventional Line Tracing. Am J Gastroenterol. 2015;110(7):967–77; quiz 78. • This prospective study highlighted the improved diagnostic accuracy and ease of interpretation using high resolution manometry with esophageal pressure topography plots over conventional methods. This work emphasized the value of moving towards high-resolution manometry with esophageal pressure topography as the standard in esophageal manometry.
- 7.Rao SS, Parkman HP. Advanced training in neurogastroenterology and gastrointestinal motility. Gastroenterology. 2015;148(5):881–5. [DOI] [PubMed] [Google Scholar]
- 8.Yadlapati R, Gawron AJ, Keswani RN, Bilimoria K, Castell DO, Dunbar KB, et al. Identification of Quality Measures for Performance of and Interpretation of Data From Esophageal Manometry. Clin Gastroenterol Hepatol. 2016;14(4):526–34 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yadlapati R, Keswani RN, Ciolino JD, Grande DP, Listernick ZI, Carlson DA, et al. A System to Assess the Competency for Interpretation of Esophageal Manometry Identifies Variation in Learning Curves. Clin Gastroenterol Hepatol. 2016. • This prospective study of 20 gastroenterology trainees identified that learning curves for high resolution manometry vary, and that the volume based cutoff of 50 cases is an inadequate surrogate for competency interpretation. This work spring boarded subsequent efforts to standardize manometry interpretation training and assessment.
- 10.Yadlapati R, Keswani RN, Dunbar KB, Gawron AJ, Gyawali CP, Kahrilas PJ, et al. Benchmarks for the interpretation of esophageal high-resolution manometry. Neurogastroenterol Motil. 2016. [DOI] [PMC free article] [PubMed]
- 11.Yadlapati R, Keswani RN, Pandolfino JE. Competency based medical education in gastrointestinal motility. Neurogastroenterol Motil. 2016;28(10):1460–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hirano I, Pandolfino JE, Boeckxstaens GE. Functional Lumen Imaging Probe for the Management of Esophageal Disorders: Expert Review From the Clinical Practice Updates Committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15(3):325–34. •This paper is a current-day review of technical and diagnostic applications of the novel EndoFLIP technology.
- 13.Vaezi MF, Baker ME, Achkar E, Richter JE. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut. 2002;50(6):765–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Blonski W, Kumar A, Feldman J, Richter JE. Timed Barium Swallow: Diagnostic Role and Predictive Value in Untreated Achalasia, Esophagogastric Junction Outflow Obstruction, and Non-Achalasia Dysphagia. Am J Gastroenterol. 2018;113(2):196–203. •This retrospective cohort study found that barium timed swallow has good sensitivity and specificity for achalalsia, and timed barium esophagram with a barium tablet increased diagnostic yield.
- 15.Pandolfino JE, Kahrilas PJ. Presentation, diagnosis, and management of achalasia. Clin Gastroenterol Hepatol. 2013;11(8):887–97. [DOI] [PubMed] [Google Scholar]
- 16. Marin I, Cisternas D, Abrao L, Lemme E, Bilder C, Ditaranto A, et al. Normal values of esophageal pressure responses to a rapid drink challenge test in healthy subjects: results of a multicenter study. Neurogastroenterol Motil. 2017;29(6). • This prospective study of 105 heatlhy subjects identified normative manometric values in response to the rapid drink challenge test as a provocative maneuver to assess for outflow obstructive physiology at the EGJ.
- 17.Marin I, Serra J. Patterns of esophageal pressure responses to a rapid drink challenge test in patients with esophageal motility disorders. Neurogastroenterol Motil. 2016;28(4):543–53. [DOI] [PubMed] [Google Scholar]
- 18.Ang D, Hollenstein M, Misselwitz B, Knowles K, Wright J, Tucker E, et al. Rapid Drink Challenge in high-resolution manometry: an adjunctive test for detection of esophageal motility disorders. Neurogastroenterol Motil. 2017;29(1). [DOI] [PubMed] [Google Scholar]
- 19.Cho YK, Lipowska AM, Nicodeme F, Teitelbaum EN, Hungness ES, Johnston ER, et al. Assessing bolus retention in achalasia using high-resolution manometry with impedance: a comparator study with timed barium esophagram. Am J Gastroenterol. 2014;109(6):829–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sweis R, Anggiansah A, Wong T, Kaufman E, Obrecht S, Fox M. Normative values and inter-observer agreement for liquid and solid bolus swallows in upright and supine positions as assessed by esophageal high-resolution manometry. Neurogastroenterol Motil. 2011;23(6):509–e198. [DOI] [PubMed] [Google Scholar]
- 21. Ang D, Misselwitz B, Hollenstein M, Knowles K, Wright J, Tucker E, et al. Diagnostic yield of high-resolution manometry with a solid test meal for clinically relevant, symptomatic oesophageal motility disorders: serial diagnostic study. Lancet Gastroenterol Hepatol. 2017;2(9):654–61. • This study of 750 symptomatic patients found an increased diagnostic sensitivity of major motility disorders using high resolution manometry when a solid test meal was used compared with ten single water swallows. These results support the incorporation of solid swallows into manometry protocols when assessing for symptomatic dysphagia.
- 22.Katz PO, Schnoll-Sussman F. Oesophageal manometry with a solid test meal: ready for prime time? Lancet Gastroenterol Hepatol. 2017;2(9):621–3. [DOI] [PubMed] [Google Scholar]
- 23.Lin Z, Carlson DA, Dykstra K, Sternbach J, Hungness E, Kahrilas PJ, et al. High-resolution impedance manometry measurement of bolus flow time in achalasia and its correlation with dysphagia. Neurogastroenterol Motil. 2015;27(9):1232–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carlson DA, Omari T, Lin Z, Rommel N, Starkey K, Kahrilas PJ, et al. High-resolution impedance manometry parameters enhance the esophageal motility evaluation in non-obstructive dysphagia patients without a major Chicago Classification motility disorder. Neurogastroenterol Motil. 2017;29(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lin Z, Imam H, Nicodeme F, Carlson DA, Lin CY, Yim B, et al. Flow time through esophagogastric junction derived during high-resolution impedance-manometry studies: a novel parameter for assessing esophageal bolus transit. Am J Physiol Gastrointest Liver Physiol. 2014;307(2):G158–63. •This study highlights the value of the trans-EGJ bolus flow time as a high resolution impedance manometry measure of outflow obstruction across the EGJ in the evaluation of symptomatic dysphagia.
- 26.Lin Z, Nicodeme F, Lin CY, Mogni B, Friesen L, Kahrilas PJ, et al. Parameters for quantifying bolus retention with high-resolution impedance manometry. Neurogastroenterol Motil. 2014;26(7):929–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin Z, Yim B, Gawron A, Imam H, Kahrilas PJ, Pandolfino JE. The four phases of esophageal bolus transit defined by high-resolution impedance manometry and fluoroscopy. Am J Physiol Gastrointest Liver Physiol. 2014;307(4):G437–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carlson DA, Lin Z, Kou W, Pandolfino JE. Inter-rater agreement of novel high-resolution impedance manometry metrics: Bolus flow time and esophageal impedance integral ratio. Neurogastroenterol Motil. 2018;30(6):e13289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carlson DA, Kahrilas PJ, Ritter K, Lin Z, Pandolfino JE. Mechanisms of repetitive retrograde contractions in response to sustained esophageal distension: a study evaluating patients with postfundoplication dysphagia. Am J Physiol Gastrointest Liver Physiol. 2018;314(3):G334–G40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carlson DA, Kahrilas PJ, Lin Z, Hirano I, Gonsalves N, Listernick Z, et al. Evaluation of Esophageal Motility Utilizing the Functional Lumen Imaging Probe. Am J Gastroenterol. 2016;111(12):1726–35. •This was one of the first papers to propose a FLIP topography motility classification scheme for esophageal motility. This study also reiterated that FLIP topography identifies abnormalities of EGJ relaxation that are not identified on manometry.
- 31. Ponds FA, Bredenoord AJ, Kessing BF, Smout AJ. Esophagogastric junction distensibility identifies achalasia subgroup with manometrically normal esophagogastric junction relaxation. Neurogastroenterol Motil. 2017;29(1). •In this study EGJ distensibility using EndoFLIP identified impaired distensibility in patients with clinical and radiological features of achalasia thought normal EGJ relaxation on manometry, and these patients responded well to achalasia treatment. Therefore, EndoFLIP may have a complimentary role to manometry in assessment of EGJ relaxation.
- 32.Carlson DA, Lin Z, Kahrilas PJ, Sternbach J, Donnan EN, Friesen L, et al. The Functional Lumen Imaging Probe Detects Esophageal Contractility Not Observed With Manometry in Patients With Achalasia. Gastroenterology. 2015;149(7):1742–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rohof WO, Salvador R, Annese V, Bruley des Varannes S, Chaussade S, Costantini M, et al. Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology. 2013;144(4):718–25; quiz e13–4. [DOI] [PubMed] [Google Scholar]
- 34. Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, et al. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg. 2015;221(2):256–64. •In this study per-oral endoscopy myotomy had a success rate of 90% across achalasia sub-types at 3 years
- 35.Kahrilas PJ, Bredenoord AJ, Carlson DA, Pandolfino JE. Advances in Management of Esophageal Motility Disorders. Clin Gastroenterol Hepatol. 2018. [DOI] [PMC free article] [PubMed]
- 36.Kahrilas PJ, Katzka D, Richter JE. Clinical Practice Update: The Use of Per-Oral Endoscopic Myotomy in Achalasia: Expert Review and Best Practice Advice From the AGA Institute. Gastroenterology. 2017;153(5):1205–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Khan MA, Kumbhari V, Ngamruengphong S, Ismail A, Chen YI, Chavez YH, et al. Is POEM the Answer for Management of Spastic Esophageal Disorders? A Systematic Review and Meta-Analysis. Dig Dis Sci. 2017;62(1):35–44. •This recent metanalysis of 8 uncontrolled observational studies reported acceptable response rates of POEM in type III achalasia, distal esophageal spasm, and hypercontractile esophagus.
- 38.Desjardin M, Luc G, Collet D, Zerbib F. 24-hour pH-impedance monitoring on therapy to select patients with refractory reflux symptoms for antireflux surgery. A single center retrospective study. Neurogastroenterol Motil. 2016;28(1):146–52. [DOI] [PubMed] [Google Scholar]
- 39.Roman S, Gyawali CP, Savarino E, Yadlapati R, Zerbib F, Wu J, et al. Ambulatory reflux monitoring for diagnosis of gastro-esophageal reflux disease: Update of the Porto consensus and recommendations from an international consensus group. Neurogastroenterol Motil. 2017;29(10):1–15. [DOI] [PubMed] [Google Scholar]
- 40.Frazzoni M, de Bortoli N, Frazzoni L, Tolone S, Furnari M, Martinucci I, et al. The added diagnostic value of postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance in refractory reflux disease studied with on-therapy impedance-pH monitoring. Neurogastroenterol Motil. 2017;29(3). [DOI] [PubMed] [Google Scholar]
- 41.Patel A, Wang D, Sainani N, Sayuk GS, Gyawali CP. Distal mean nocturnal baseline impedance on pH-impedance monitoring predicts reflux burden and symptomatic outcome in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2016;44(8):890–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barrett C, Choksi Y, Vaezi MF. Mucosal Impedance: a New Approach to Diagnosing Gastroesophageal Reflux Disease and Eosinophilic Esophagitis. Curr Gastroenterol Rep. 2018;20(7):33. [DOI] [PubMed] [Google Scholar]
- 43.Shaker A, Stoikes N, Drapekin J, Kushnir V, Brunt LM, Gyawali CP. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol. 2013;108(11):1706–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stoikes N, Drapekin J, Kushnir V, Shaker A, Brunt LM, Gyawali CP. The value of multiple rapid swallows during preoperative esophageal manometry before laparoscopic antireflux surgery. Surg Endosc. 2012;26(12):3401–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carlson DA, Crowell MD, Kimmel JN, Patel A, Gyawali CP, Hinchcliff M, et al. Loss of Peristaltic Reserve, Determined by Multiple Rapid Swallows, Is the Most Frequent Esophageal Motility Abnormality in Patients With Systemic Sclerosis. Clin Gastroenterol Hepatol. 2016;14(10):1502–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gyawali CP, Patel A. Esophageal motor function: technical aspects of manometry. Gastrointest Endosc Clin N Am. 2014;24(4):527–43. [DOI] [PubMed] [Google Scholar]
- 47.Bravi I, Woodland P, Gill RS, Al-Zinaty M, Bredenoord AJ, Sifrim D. Increased prandial air swallowing and postprandial gas-liquid reflux among patients refractory to proton pump inhibitor therapy. Clin Gastroenterol Hepatol. 2013;11(7):784–9. [DOI] [PubMed] [Google Scholar]
- 48.Halland M, Parthasarathy G, Bharucha AE, Katzka DA. Diaphragmatic breathing for rumination syndrome: efficacy and mechanisms of action. Neurogastroenterol Motil. 2016;28(3):384–91. [DOI] [PubMed] [Google Scholar]
- 49.Soykan I, Chen J, Kendall BJ, McCallum RW. The rumination syndrome: clinical and manometric profile, therapy, and long-term outcome. Dig Dis Sci. 1997;42(9):1866–72. [DOI] [PubMed] [Google Scholar]
- 50.Yadlapati R, Tye M, Roman S, Kahrilas PJ, Ritter K, Pandolfino JE. Postprandial High-Resolution Impedance Manometry Identifies Mechanisms of Nonresponse to Proton Pump Inhibitors. Clin Gastroenterol Hepatol. 2018;16(2):211–8 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]