Abstract
Objective:
The article seeks to assess the Brazilian health system ability to respond to the challenges imposed by the coronavirus disease 2019 (COVID-19) pandemic by measuring the capacity of Brazilian hospitals to care for COVID-19 cases in the 450 Health Regions of the country during the year 2020. Hospital capacity refers to the availability of hospital beds, equipment, and human resources.
Methods:
We used longitudinal data from the National Register of Health Facilities (CNES) regarding the availability of resources necessary to care for patients with COVID-19 in inpatient facilities (public or private) from January to December 2020. Among the assessed resources are health professionals (certified nursing assistants, nurses, physical therapists, and doctors), hospital beds (clinical, intermediate care, and intensive care units), and medical equipment (computed tomography scanners, defibrillators, electrocardiograph monitors, ventilators, and resuscitators). In addition to conducting a descriptive analysis of absolute and relative data (per 10,000 users), a synthetic indicator named Installed Capacity Index (ICI) was calculated using the multivariate principal component analysis technique to assess hospital capacity. The indicator was further stratified into value ranges to understand its evolution.
Results:
There was an increase in all selected indicators between January and December 2020. It was possible to observe differences between the Northeast and North regions and the other regions of the country; most Health Regions presented low ICI. The ICI increased between the beginning and the end of 2020, but this evolution differed among Health Regions. The average increase in the ICI was more evident in the groups that already had considerably high baseline capacity in January 2020.
Conclusions:
It was possible to identify inequalities in the hospital capacity to care for patients affected by COVID -19 in the Health Regions of Brazil, with a concentration of low index values in the Northeast and North of the country. As the indicator increased throughout the year 2020, inequalities were also observed. The information here provided may be used by health authorities, providers, and managers in planning and adjusting for future COVID-19 care and in dimensioning the adequate supply of hospital beds, health-care professionals, and devices in Health Regions to reduce associated morbidity and mortality. We recommend that the ICI continue to be calculated in the coming months of the pandemic to monitor the capacity in the country’s Health Regions.
Keywords: hospital capacity, COVID-19, regionalization of health
The coronavirus disease 2019 (COVID-19) pandemic has challenged health systems worldwide 1 and in Brazil where a public (Sistema Unico de Saude - SUS) and private health systems coexist. To face the pandemic, health services must be structured and able to adapt to emerging needs. Thus, in the context of treatment for those affected by the disease, actions are needed to plan and assess the installed capacity of health services to provide timely and adequate hospital care in different country regions.
The provision of health services depends on the installed capacity of health facilities to provide health care in due time and place, especially in facing the COVID-19 pandemic. Adequate hospital treatment can provide satisfactory outcomes for patients with COVID-19, 2 but this demands, especially in severe cases that require hospitalization in intensive care unit (ICU), specific equipment, specialized and trained human resources, and the provision of enough beds to meet the demand at any point in time. 3–5 In Brazil, what has been observed in the first year of the pandemic in several circumstances is that supply did not match demand, even though there has been an increase in hospital beds. 6 The uneven distribution among the country regions, with a deficit of beds in most Brazilian municipalities, 7 mainly in the North and Northeast regions, has been a significant factor in the loss of lives. 6 It is important to describe the hospital capacity to care for COVID-19 cases, thinking about the most critical supply elements, namely beds, devices and human resources, 4,8,9 understanding its evolution over time since the beginning of the pandemic.
This study aims to measure the installed capacity of all Brazilian hospitals (public and private) to care for COVID-19 cases in the country’s official Health Regions in 2020. Installed capacity refers to the availability of hospital beds, devices, and human resources.
Methods
This is a longitudinal analytical study carried out with data from the National Register of Health Facilities (CNES) regarding the availability of health professionals, hospital beds, and medical equipment in all hospitals registered in the system, both public and private. In Brazil, the CNES registry contains facility name, address, location, physical facilities, equipment, and responsible manager. It is also necessary to inform the categories of care offered, such as outpatient, exams, hospitalization, specialized and support services. There are also specific spaces for team professionals, such as registration in the Brazilian Classification of Occupations (CBO), workload, among others. To assure generalizability for the country, the registration is mandatory for health-care providers, because CNES is used to identify and monitor the entire Brazilian health system and facilities that are not included in the registry act irregularly and cannot receive any payment linked to SUS or health plan operators. Therefore, it is essential to keep the data correctly filled in, updating the records every month, or whenever there are changes in structure, operation, and human resources. The following types of establishments need CNES: offices in general (such as doctors and dentists), health clinics, polyclinics, and hospitals (can be day or specialized hospitals), physiotherapy, acupuncture, and Diagnostic and Therapeutic Support Services. Outpatient clinics located in organizations, such as companies, schools, and clubs, must also obtain their CNES number.
We used data from January to December 2020, distributed in the officially established 450 Health Regions in Brazil. A Health Region comprises a group of municipalities that share their resources, such as hospitals, emergency units, and primary care and financial resources into care networks for the provision of services to the populations of the municipalities. The regionalization of the Unified Health System (SUS) was determined as a strategy to optimize the management of the system, the rationalization of resources, and the institutional contribution to creating health-care networks. 10 Public domain data made available by the Ministry of Health were used, whose last update was on January 15, 2021.
Regarding the devices or equipment, computed tomography (CT scanners), defibrillators, electrocardiograph (ECG) monitors, ventilators, and resuscitators were included in the analysis, as they are considered necessary in treating severe cases of COVID-19. 5 All the devices accounted for had an indication in the CNES as “in use.” For hospital beds, only those types used in caring for patients with COVID-19 were taken into account. Two categories were proposed: the first with hospital beds of the clinical type, intermediate care, and ventilator support; the second with adult ICU beds in general or exclusive to COVID-19.
In accounting for health professionals, we considered the staff linked to hospitals that had at least 1 of the bed categories proposed. Among the professional specialties that work in these facilities, only certified nursing assistants, nurses, physicians, and physical therapists were used. This specification is justified by the more direct action of these workers in intensive care of patients diagnosed with COVID-19, a decision that is in line with the requirement of specialists for the qualification and implantation of an essential team in ICUs exclusive or not for patients with COVID-19 (MH/Ordinance No. 3,432, of August 12, 1998).
The number of hospital beds, devices, and health professionals in use or available in health facilities was broken down according to the type of funding or availability of equipment/beds/professionals. The supply of hospitals was stratified into 2 categories: those belonging exclusively to SUS (public system) and beneficiaries of private health insurance plans and/or private users. Although registered individually with their connection to the hospitals, the records were accounted for on the scale of the municipality and the (micro) Health Region where the hospital was located. Rates of beds, devices, and health professional availability were obtained, adding SUS and private (total) and exclusively in SUS (public only). To calculate the total rates, population data were obtained from the population estimates provided by the Brazilian Institute of Geography and Statistics (IBGE), with a reference date of July 1, 2020. The non-SUS data considered the number of beneficiaries of health insurance plans for medical assistance that included dental assistance or not, made available at the municipal level every quarter by the National Health Agency (ANS) in March, June, and September 2020, with municipal distribution of the number of beneficiaries. The total number of SUS users was also considered by subtracting health insurance plan beneficiaries from the total municipal population.
To obtain the data, the Microdatasus library 11 developed in R language was used, which allowed downloading and preprocessing the data available in the DATASUS platform to be carried out as a batch.
Initially, means and measures of relative dispersion of regional values around the mean were calculated, comparing total and exclusive SUS availability. We sought to represent a month before the pandemic and another during it. Therefore, we chose the months of January and December 2020, respectively.
We calculated total rates per 10,000 inhabitants for the number of devices, beds, and professionals in public and private networks. SUS rates were restricted to devices and professionals available exclusively in the Unified Health System, for which the population considered in the denominator were individuals who do not have private health insurance plans.
In the construction of the index, the Principal Component Analysis (PCA) method was used to present an empirical summary of the original dataset. The use of PCA allows the explanation of the variance and covariance structure of a vector of random variables by constructing linear combinations of the original variables. 12 PCA can reduce a large number of variables to a model composed of k main components that are not correlated with each other and can explain a relevant proportion of the total variance of the original variables. The existence of multicollinearity between the original variables is not, unlike in other techniques, a problem for calculating the component. We sought to obtain an indicator that captured the common behavior and, in a simplified way, from its linear convergence, observed in the original variables between the Health Regions, in addition to the time variation of these values.
Following guidelines from Mingoti, 12 to avoid excessive influence of discrepancies in the variances of the original variables, we chose to standardize the variables by their mean and standard deviation, where each of the 11 original variables X i were transformed, obtaining Z i = (X i – μ i )/σ i , where E(X i ) = μ i and Var(Xi) = σ i 2, with i = 1, 2, …, n = 11. At the end of the analysis, each of the resulting k main components could be calculated from simple linear equations with multiplicative constants β j,i (j = 1, 2, …, k) associated with each variable and identified by standardized eigenvectors for each component (Appendix 1).
The statistical software used was SPSS 26.0. The PCA was applied to monthly data from all Health Regions as separate records to allow for a time analysis, from which the indicator of the first component generated was obtained. The indicator synthesized most of the data variance, an expected result, given the relevant correlations between the original variables.
The calculation of the indicator allowed exploring regional differences in the installed capacity of hospital services in offering adequate care to patients affected by COVID-19, who presented severe conditions of the disease and needed hospital care and hospitalization.
To assess whether a principal component analysis could generate a model adequately adjusted to the original data, 2 adequacy measures were used: the Kaiser-Meyer-Olkin criterion (KMO) and Bartlett’s test of sphericity 12 first test, an adequate adjustment is considered when KMO > 0.8 is obtained. With Bartlett’s test, which consists of a chi-squared test that assesses the null hypothesis that the correlation matrix between the original variables is equal to the identity matrix, an adequate adjustment is reached in the rejection of the null hypothesis with a P-value of at least 0.05.
To facilitate the analysis of essential aspects of the Installed Capacity Index (ICI), an interpretative strategy was chosen to stratify the index into groups of value ranges where differences in the behavior of Health Regions were verified at different levels of installed capacity. The intervals for the groups were defined by applying the Jenks algorithm (“natural breaks”), which is an algorithm commonly implemented in geographic information systems (GIS) to stratify a data series where each class tends to have a smaller internal variance and at the same time presents a greater variance between different classes.
Results
Descriptive Statistics of Original Variables
When comparing the total and exclusively SUS rates, on average, it is possible to notice a more relative supply of resuscitators, respirators/ventilators, nursing professionals, physical therapy, physicians, and certified nursing assistants in SUS than in the total group, which also incorporates the private supply. The total rates indicate an advantage of the SUS only for the relative presence of defibrillators, ECG monitors, CT scanners, and hospital beds (either clinical or ICU).
It should be noted that there was an increase in all indicators between January and December 2020, both in Total and exclusively SUS. There was an increase of 192.9% in the rate of hospital beds in adult ICU in the Total.
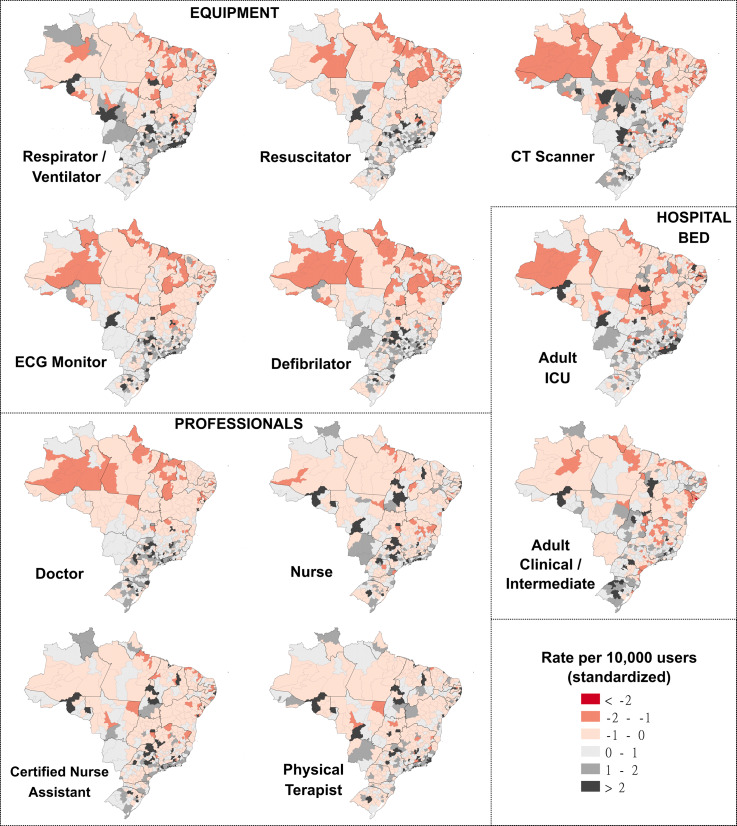
The data in Table 1 for the total rates in December 2020 are presented by Health Region (Figure 1). The values were standardized, that is, the calculation is the ratio between the value of the variable minus the mean and the standard deviation. The variables are divided into 5 groups in which shades of red represent the groups with the lowest proportion and shades of gray and black represent the highest proportion. The North and Northeast regions presented few Health Regions in shades of gray and black (when considering all variables) and many regions in shades of red, mainly in equipment. The regions with the highest proportion of devices, hospital beds, and health professionals are the South and Southeast.
Table 1.
Total and mean of region’s rates of devices, hospital beds, and health professionals per 10,000 inhabitants/users coefficient of variation and mean values, according to total or SUS-only availability: Brazilian Health Regions, January and December 2020
| Device/hospital bed/professional | Total | Total | SUS | SUS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (01/2020) | (12/2020) | (01/2020) | (12/2020) | |||||||||
| Total | Mean of region’s rates | CV of region’s rates | Total | Mean of region’s rates | CV of region’s rates | Total | Mean of region’s rates | CV of region’s rates | Total | Mean of region’s rates | CV of region’s rates | |
| Resuscitators | 130'350 | 4.77 | 66.7% | 143'662 | 5.23 | 65.7% | 95'403 | 4.90 | 74.4% | 105'644 | 5.42 | 74.3% |
| Respirators/ventilators | 61'219 | 1.80 | 76.3% | 79'766 | 2.55 | 65.8% | 43'579 | 1.83 | 80.2% | 60'168 | 2.73 | 70.4% |
| ECG monitors | 85'569 | 2.52 | 84.9% | 100'044 | 2.95 | 80.5% | 55'536 | 2.44 | 94.5% | 66'261 | 2.93 | 88.8% |
| Defibrillators | 41'151 | 1.54 | 58.0% | 45'468 | 1.69 | 56.0% | 27'049 | 1.45 | 63.2% | 30'052 | 1.61 | 60.4% |
| CT scanners | 4'846 | 0.19 | 69.9% | 5'319 | 0.21 | 67.1% | 2'356 | 0.13 | 83.0% | 2'635 | 0.15 | 79.5% |
| Clinical beds and adult Intermediate Care | 159'630 | 7.89 | 41.1% | 189'641 | 9.00 | 38.0% | 111'160 | 7.10 | 40.0% | 136'405 | 8.36 | 37.6% |
| Beds in adult ICU | 31'632 | 0.84 | 98.5% | 53'913 | 1.62 | 77.5% | 15'326 | 0.66 | 102.6% | 24'898 | 1.08 | 92.2% |
| Nurses | 168'931 | 5.35 | 59.7% | 199'242 | 6.27 | 57.7% | 139'650 | 5.91 | 66.1% | 166'219 | 6.97 | 63.8% |
| Physical therapists | 36'055 | 1.02 | 87.5% | 47'217 | 1.33 | 83.6% | 30'238 | 1.16 | 95.6% | 40'357 | 1.52 | 91.1% |
| Doctors/physicians | 575'820 | 19.22 | 79.3% | 631'549 | 20.46 | 78.5% | 451'642 | 20.76 | 85.6% | 494'008 | 22.22 | 85.0% |
| Certified nursing assistants | 524'933 | 18.00 | 54.9% | 587'573 | 19.89 | 55.2% | 431'707 | 19.77 | 61.0% | 486'425 | 21.93 | 61.0% |
Figure 1.
Standardized rates of Equipment, Professionals and Hospital Beds per 10,000 users.
PCA Results
The use of the KMO test for the 22 original variables, 11 Total and 11 SUS, performed separately, generated high KMO indexes, with values of 0.925 and 0.930, respectively, therefore, above the recommendation for an adequate adjustment (KMO > 0.8). Bartlett’s test showed results that satisfactorily made it possible to reject the test’s null hypothesis for both PCAs (P < 0.05).
The PCAs, with both total and exclusive data from SUS, resulted in only 1 component, each with an eigenvalue greater than 1, which in the literature is a sufficient criterion for choosing only this component to explain the original variables. For total data, component 1 can explain 67.1% of the data variance, while component 1 of the PCA for SUS only data can explain 66.1% of the variance of the original data.
Communality represents the proportion of variance for each variable included in the analysis explained by the extracted components. The component loadings indicate the degree of correlation between the original variable and the component. Both loadings and commonalities have a higher value in respirator/ventilator and a smaller 1 in clinical beds and adult intermediate care (Table 2).
Table 2.
Communalities of the PCA and loading of the original variable in relation to the first component: Brazilian Health Regions, 2020
| Device /hospital bed/professional | Total | SUS | ||
|---|---|---|---|---|
| Communalities PCA total | Loading component 1 | Communality PCA SUS | Loading component 1 | |
| Resuscitator | 0.706 | 0.840 | 0.679 | 0.824 |
| Respirator/ventilator | 0.847 | 0.920 | 0.836 | 0.914 |
| ECG monitor | 0.808 | 0.899 | 0.775 | 0.880 |
| Defibrillator | 0.716 | 0.846 | 0.680 | 0.825 |
| CT scanner | 0.462 | 0.680 | 0.381 | 0.617 |
| Clinical beds and adult intermediate care | 0.229 | 0.478 | 0.223 | 0.473 |
| Beds in adult ICU | 0.753 | 0.868 | 0.719 | 0.848 |
| Nursing professionals | 0.701 | 0.837 | 0.726 | 0.852 |
| Physical therapy professionals | 0.657 | 0.810 | 0.664 | 0.815 |
| Medical professionals | 0.742 | 0.861 | 0.792 | 0.890 |
| Certified nursing assistant professionals | 0.760 | 0.872 | 0.798 | 0.893 |
ICI
To meet the practical objective of proposing an indicator capable of capturing regional differences and the evolution of installed hospital capacity in coping with COVID-19, added to the intention of synthesizing both public and private capacity into a single indicator, we chose to present only a single index of installed capacity that derives from the component obtained in the PCA with the total data.
The use of the first principal component as a synthetic indicator was found to be sufficiently representative, thus here proposed as the ICI. Considering the vector Z = [Z 1, Z 2, …, Z 11] of the standardized total rates, or even rewriting the equation in the function of the original variables, the ICI is obtained from the explicit equations in Appendix 1. Keeping in mind the limitation that the index uses only data from 2020 as parameters, it is possible to calculate, for comparison purposes, the index of each region for any month of competence, including for more recent periods.
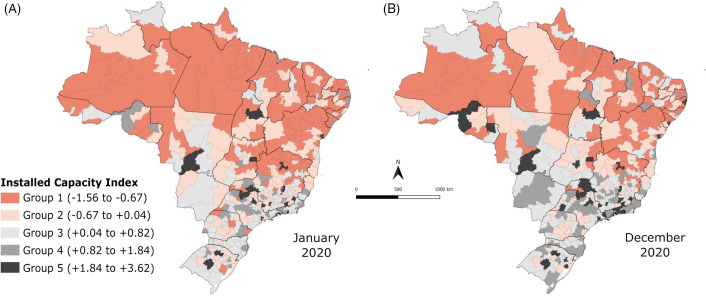
Figure 2 shows the evolution of the ICI between January and December 2020, indicating growth in all regions of Brazil, increasing the number of Health Regions in groups 4 and 5 of installed capacity (higher capacity). The North and Northeast regions have most of their Health Regions belonging to Groups 1 and 2, showing lower ICI.
Figure 2.
Installed Capacity Index in Brazilian Health Regions, January and December, 2020.
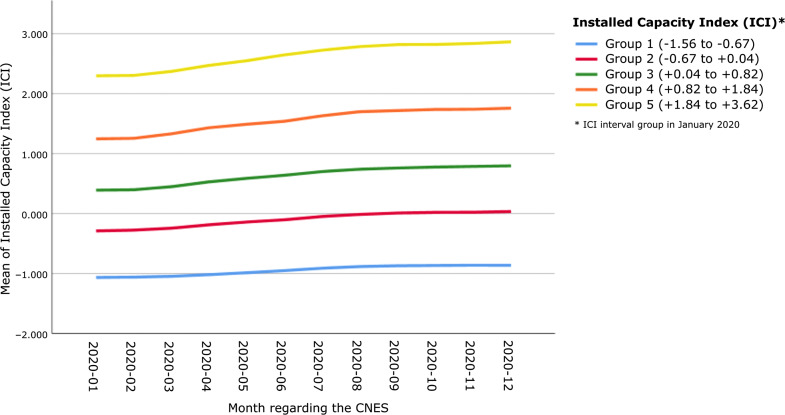
Figure 3 is stratified by groups according to the group where the Health Region was in December 2020. There is an evident increase in ICI in most groups, except for Group 1, which corresponds to the group with the lowest ICI.
Figure 3.
Mean Installed Capacity Index by month, 2020.
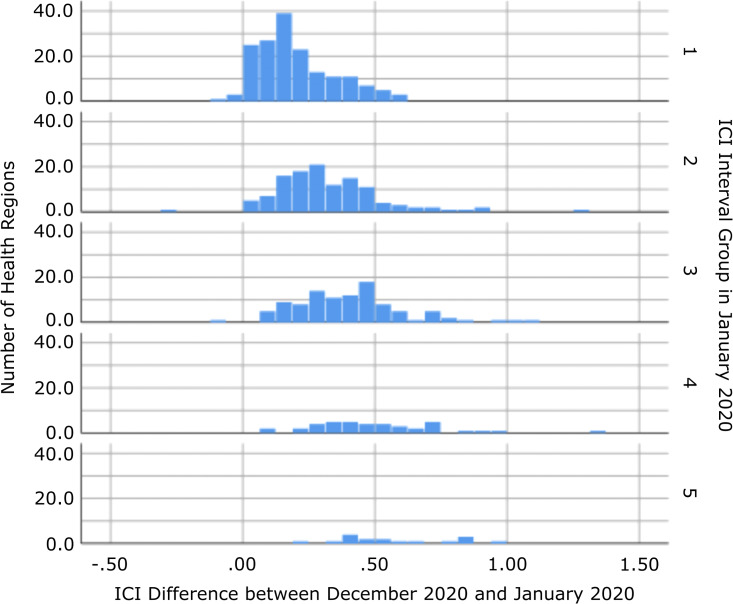
The histograms of the difference from the end of 2020 to the beginning of the year observed by groups of ICI intervals in January 2020 (Figure 4) show an exceedingly small number of Health Regions that presented decrease in their installed capacity (negative difference) and a growth between 0 and 0.5 points in the index in most regions. The ICI has a positive, albeit weak (R 2 adjusted of 0.252) correlation, with the differences observed from January to December in relation to the index itself, to certain extent corroborating the tendency of higher ICI growth in Health Regions that already had higher ICI values in January 2020.
Figure 4.
Difference in Installed Capacity Index between December and January, 2020.
Discussion
The present study is the first to present an ICI for hospital supply of care for COVID-19 patients, considering the country’s official Health Regions. Its importance lies in the fact that the COVID-19 pandemic made it essential to measure the capacity to provide the necessary health care, monitor, and measure any expansions in the response over the months of the pandemic.
First, there was an increase in all selected indicators between January and December 2020, both for the total and SUS-exclusive rates. Second, it was possible to observe differences between the Northeast and North regions and the other regions of the country, in which the majority of Health Regions presented low ICI. Third, the evolution of the ICI was observed between the beginning and the end of 2020, with an increase in the number of Health Regions in the groups with greater installed capacity, although the average increase in the ICI was more evident in the groups that already had high capacity in January 2020 (baseline).
The findings about Health Regions belonging to the Northeast and North regions are concerning, as they show the absence of improvements toward the disparities already observed in studies with cross-sectional data from CNES referring to the period before the pandemic. 4,5,13,14 Moreira 14 pointed out that in January 2020, almost 45% of the Health Regions that did not have an ICU were located in the Northeast region. Another study identified that the state of Amapá did not register any municipality on the list of those with initial structural capacity in February 2020 to treat severe COVID-19 cases, considering the availability of ICU beds and other devices listed as necessary. At the same time, Sergipe, Amazonas, and Roraima states presented only 1 municipality on the list 4,5 ; there were also significant care gaps regarding the availability of beds in the North, Northeast, and Midwest regions, emphasizing the absence of ICU beds in more than a quarter of the Health Regions in February 2020. The study carried out by Bezerra et al. 15 with CNES data from April 2020, when the pandemic was already underway, to calculate an infrastructure index for the states or Federation Units (UF), showed that the UF with the worst indexes were Amapa and Roraima (located in the North) and the best ranked were Sao Paulo and Minas Gerais (Southeast region). On the other hand, it is best to focus on more specific territorial sections, such as Health Regions (macro or micro-regions) or municipalities, because more aggregated analyses may fail to capture important differences within the UF. Noronha et al. 3 showed a worse situation for macro- and micro-Health Regions in the North and Northeast regions concerning the availability of hospital beds and assisted ventilation equipment, indicating a greater probability of system collapse even with low infection rates.
There was an advantage of the total supply (SUS and private) compared with SUS alone for the presence of defibrillators, ECG monitors, CT scanners, and hospital beds (either clinical or ICU). This finding is relevant, as it shows an expanded supply of clinical beds and ICU when considering the 2 health systems. Supplying hospital beds is of paramount importance in the treatment of moderate and severe cases of COVID-19. Requia et al. 7 estimated the deficit in the capacity of hospital beds in the municipalities of Brazil at the beginning of the pandemic, showing a worse scenario in the municipalities of the North and Northeast macro-regions. The study also suggested that restrictions on social contacts and an increase in hospital capacity could promote an improvement in this scenario. 7 In this regard, the present study observed an increase of almost 193% in the total rate of adult ICU beds between January and December 2020, although it did not occur equally among the Health Regions of the country. Conte et al. 6 also showed that the expansion of ICU beds did not reduce the inequities between regions and was not able to solve the insufficiency of hospital beds before the COVID-19 pandemic nor the provision of more health human resources.
An analysis of the first 250,000 hospitalizations in Brazil showed higher mortality in the North and Northeast regions. It also showed lower rates of hospital beds and ICUs in these regions and the concentration of these resources in state capitals. The difference in hospital mortality is also a consequence of inequities in the availability and access to services, reflecting the frailty of the health system in these regions. 16 The higher mortality in these regions had already been pointed out in the first months of the pandemic. 17 The regional inequalities observed in installed capacity and the greater difficulty in increasing the number of Health Regions with capacity shows the historically existing difficulties in the regionalization of health in Brazil and the low response capacity of the system to modify this scenario in a short period in the face of need. 6,18
The problem of installed capacity for hospital care, exposed by the present study, refers to 3 structural issues related to the funding of the health system, national autonomy in technological development and the production of devices for the service network, and the training and provision of health professionals.
Regarding the first issue, it is known that SUS, a health system whose principles are universally inscribed, is the only 1 in the world to provide care to more than 100 million people. However, what is enshrined in the Constitution and the Organic Health Laws has never been made possible because of insufficient funding. To make matters worse, in 2016, Amendment No. 95 was approved, which froze public spending in health for 20 y. The context of increased poverty in the country and an aging population, associated with inflation in the health sector, has caused severe underfunding. 19
The second issue is related to the technological dependence from other countries, thus resulting in high levels of importation of medical devices and other health items. Brazilian researchers have been investigating and advocating for the development of the Health Economic-Industrial Complex for years, understanding that the construction of a health system that allows the constitutional precepts of universality and wholeness 20 to be realized must be associated with the consolidation of a productive base and innovation in health so that the national health system is structurally sustained. In a continental country like Brazil, with more than 200 million people, the existence of a productive health system, involving the industry and health services in an articulated way, presents itself as a condition without which access to health cannot be guaranteed structurally. 21 The dependence on other countries to provide devices for expanding the number of ICU beds left the Brazilian population and health workers very vulnerable during the pandemic in 2020 and points to the need to face and overcome them. 18
The third issue is related to the training of human resources for health, especially doctors, nurses, certified nursing assistants, and specialized physical therapists, hospital care, and intensive care, in sufficient numbers to guarantee universal and comprehensive health care, 22 which requires medium and long-term planning, especially for the training of specialists and their equitable provision in all Health Regions. In the context of the outbreak of COVID-19 cases, this shortage of professionals is more evident. 23
It is worth emphasizing the importance of using CNES as a rich data source on the availability of hospital beds, equipment, and health professionals. In this database, all health establishments, public and private, of individuals or legal entities are registered. Comprehensively and nationally, it is the only public and unrestricted database capable of providing updated data, thus being of great value for decision-making. The proposal for an index encompassing several aspects of installed capacity is based on the principle that, in addition to the expansion of beds, the availability of devices and professionals is necessary to assess an adequate response capacity of the health system. 24 Nevertheless, investments should not be restricted to the provision of intensive care because other measures in public health, such as the articulation between epidemiological surveillance and primary health care, physical distancing, testing, contact tracing, and health communication, could be more efficient in saving lives in the short term without vaccine availability in 2020 to prevent individuals from getting sick in the first place. 25,26
It is vital to present some limitations identified in the present work. Despite the positive aspects of CNES as a data source, this system depends on self-completion and updating by the facilities, and for this reason, it can lead to errors or inaccuracies. Therefore, the study is limited to aspects of the reported supply of resources, and it does not reach the dimension of the demand for the use of these resources in the different Health Regions of the country. However, these difficulties sought to be overcome, given that the study used a relative measure to allow comparability of installed capacity between Health Regions.
Conclusions
The present study’s findings allowed the understating of inequalities in the installed capacity to care for patients affected by COVID-19 in the Health Regions of Brazil. We identified a concentration of regions with lower values of the capacity index in the Northeast and North regions of the country and inequality in the increase in the indicator over time, despite the average increase observed. These findings show the need to expand the availability of hospital beds, professionals, and devices in these regions to better cope with COVID-19 and to decrease associated morbidity and mortality. Future monthly follow-up with the ICI presented here will allow monitoring the supply dynamics and guide adjustments in the service supply and improvements in the organization of the care networks in the Health Regions of the country. We also hope other countries can develop similar indexes in future pandemics, by building and assembling similar registries such as CNES ahead of time or even by conducting smaller representative surveys to assess capacity needs. CNES is a powerful tool that should be strengthened in Brazil as it can support decision-making, planning, extension and knowledge by managers, researchers, workers, and society in general about the organization, existence and availability of services, workforce and installed capacity of health facilities and territories. It can serve as a model to other countries.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/dmp.2022.214.
click here to view supplementary material
References
- 1. World Health Organization. Strengthening the health system response to COVID-19: recommendations for the WHO European Region (1 April 2020). Published online April 1, 2020. Accessed September 8, 2022. https://apps.who.int/iris/handle/10665/333072
- 2. Peng Y, Xu B, Sun B, et al. Importance of timely management of patients in reducing fatality rate of coronavirus disease 2019. J Infect Public Health. 2020;13(6):890-892. doi: 10.1016/j.jiph.2020.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Noronha KVM de S, Guedes GR, Turra CM, et al. Pandemia por COVID-19 no Brasil: análise da demanda e da oferta de leitos hospitalares e equipamentos de ventilação assistida segundo diferentes cenários. Cad Saúde Pública. 2020;36(6):e00115320. doi: 10.1590/0102-311x00115320 [DOI] [PubMed] [Google Scholar]
- 4. Portela MC, Pereira CC de A, Lima SML, et al. Limites e Possibilidades Dos Municípios Brasileiros Para o Enfrentamento Dos Casos Graves de Covid-19. Nota Técnica. ENSP/FIOCRUZ; 2020. [Google Scholar]
- 5. Portela MC, Pereira CC de A, Andrade CLT de, et al. As Regiões de Saúde e a Capacidade Instalada de Leitos de UTI e Alguns Equipamentos Para o Enfrentamento Dos Casos Graves de Covid-19. Nota Técnica 2. ENSP/FIOCRUZ; 2020. [Google Scholar]
- 6. Conte DCAR, Bahia L, Laurentino de Carvalho EMC, et al. Oferta Pública e Privada de Leitos e Acesso Aos Cuidados à Saúde Na Pandemia de COVID-19 No Brasil. 2020. doi:10.1590/SciELOPreprints.1316
- 7. Requia WJ, Kondo EK, Adams MD, et al. Risk of the Brazilian health care system over 5572 municipalities to exceed health care capacity due to the 2019 novel coronavirus (COVID-19). Sci Total Environ. 2020;730:139144. doi: 10.1016/j.scitotenv.2020.139144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lopez FG, Palotti PLDM, Barbosa SCT, et al. Mapeamento dos profissionais de saúde no brasil: alguns apontamentos em vista da crise sanitária da covid-19. IPEA; 2020:20. Accessed February 1, 2021. http://repositorio.ipea.gov.br/bitstream/11058/9837/1/NT_30_Diest_Mapeamento%20dos%20Profissionais%20de%20Sa%c3%bade%20no%20Brasil.pdf [Google Scholar]
- 9. Rache B, Rocha R, Nunes L, et al. Necessidades de Infraestrutura do SUS em Preparo à COVID-19: Leitos de UTI, Respiradores e Ocupação Hospitalar. IEPS; 2020:5. https://observatoriohospitalar.fiocruz.br/sites/default/files/biblioteca/ESTUDO%20ANA%20MALIK%20NT3-vFinal.pdf_0.pdf [Google Scholar]
- 10. Xavier DR, Oliveira RAD de, Barcellos C, et al. As Regiões de Saúde no Brasil segundo internações: método para apoio na regionalização de saúde. Cad Saúde Pública. 2019;35(Suppl 2):e00076118. doi: 10.1590/0102-311x00076118 [DOI] [PubMed] [Google Scholar]
- 11. Saldanha R de F, Bastos RR, Barcellos C. Microdatasus: pacote para download e pré-processamento de microdados do Departamento de Informática do SUS (DATASUS). Cad Saúde Pública. 2019;35(9):e00032419. doi: 10.1590/0102-311x00032419 [DOI] [PubMed] [Google Scholar]
- 12. Mingoti SA. Análise de Dados Através de Métodos de Estatística Multivariada: Uma Abordagem Aplicada. Editora UFMG; 2005. [Google Scholar]
- 13. Portela MC, Martins M, Lima SML, et al. Disponibilidade de Recursos e Razão de Dependência Entre SUS e Saúde Suplementar. ENSP/FIOCRUZ; 2020. [Google Scholar]
- 14. Moreira R da S. COVID-19: unidades de terapia intensiva, ventiladores mecânicos e perfis latentes de mortalidade associados à letalidade no Brasil. Cad Saúde Pública. 2020;36(5):e00080020. doi: 10.1590/0102-311x00080020 [DOI] [PubMed] [Google Scholar]
- 15. Bezerra ÉCD, Santos PS dos, Lisbinski FC, et al. Análise espacial das condições de enfrentamento à COVID-19: uma proposta de Índice da Infraestrutura da Saúde do Brasil. Ciênc Saúde Coletiva. 2020;25(12):4957-4967. doi: 10.1590/1413-812320202512.34472020 [DOI] [PubMed] [Google Scholar]
- 16. Ranzani OT, Bastos LSL, Gelli JGM, et al. Characterisation of the first 250,000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9(4):407-418. doi: 10.1016/S2213-2600(20)30560-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Baqui P, Bica I, Marra V, et al. Ethnic and regional variations in hospital mortality from COVID-19 in Brazil: a cross-sectional observational study. Lancet Glob Health. 2020;8(8):e1018-e1026. doi: 10.1016/S2214-109X(20)30285-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Campos FCC de, Canabrava CM. O Brasil Na UTI: Atenção Hospitalar Em Tempos de Pandemia.; 2020. doi:10.1590/SciELOPreprints.1368
- 19. Funcia FR. Subfinanciamento e orçamento federal do SUS: referências preliminares para a alocação adicional de recursos. Ciênc Saúde Coletiva. 2019;24(12):4405-4415. doi: 10.1590/1413-812320182412.25892019 [DOI] [PubMed] [Google Scholar]
- 20. Constituição do Brasil. Constituição Da Republica Federativa Do Brasil. Senado Federal; 1988. [Google Scholar]
- 21. Gadelha CAG, Gadelha P, Noronha JC de, et al. , eds. Brasil Saúde Amanhã: Complexo Econômico-Industrial Da Saúde. Editora FIOCRUZ; 2017. doi: 10.7476/9786557080924 [DOI] [Google Scholar]
- 22. Oliveira APC de, Gabriel M, Poz MRD, et al. Desafios para assegurar a disponibilidade e acessibilidade à assistência médica no Sistema Único de Saúde. Ciênc Saúde Coletiva. 2017;22(4):1165-1180. doi: 10.1590/1413-81232017224.31382016 [DOI] [PubMed] [Google Scholar]
- 23. Agência Fiocruz de Notícias. Covid-19: Estudo avalia condições de trabalho na Saúde. Published March 22, 2021. Accessed April 6, 2021. https://agencia.fiocruz.br/covid-19-estudo-avalia-condicoes-de-trabalho-na-saude
- 24. Litton E, Bucci T, Chavan S, et al. Surge capacity of intensive care units in case of acute increase in demand caused by COVID-19 in Australia. Med J Aust. 2020;212(10):463-467. doi: 10.5694/mja2.50596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Halpern SD, Miller FG. The urge to build more intensive care unit beds and ventilators: intuitive but errant. Ann Intern Med. 2020;173(4):302-303. doi: 10.7326/M20-2071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Teixeira MG, Medina MG, Costa M da CN, et al. Reorganização da atenção primária à saúde para vigilância universal e contenção da COVID-19. Epidemiologia e Serviços de Saúde. 2020;29(4):1-5. doi: 10.5123/S1679-49742020000400015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/dmp.2022.214.
click here to view supplementary material