Abstract
We report a rare case of persistent patent arterial duct (PDA) in the combination of diverticulum of Kommerell, aberrant left subclavian artery, and total anomalous pulmonary venous connection (TAPVC). Surgical correction of the defect was done by ligating and dividing the PDA and correcting the TAPVC. (Level of Difficulty: Intermediate.)
Key Words: aortic ring, Komerrell’s diverticulum, persistent patent arterial duct, right aortic arch
Abbreviations and Acronyms: PDA, patent ductus arteriosus; TAPVC, total anomalous pulmonary venous connection; VSD, ventricular septal defect
Central Illustration
History of Presentation
We report a case of a 9-day-old male baby, who presented with shortness of breath and tachypnea. The baby was born at 39 weeks of gestation by elective lower-segment cesarean section with a birth weight of 3.62 kg and Apgar score of 5/10, 6/10, 9/10. At presentation, the baby was active and alert with weight 3.4 kg, length 51 cm, head circumference 37 cm, respiratory rate 66 breaths/min, heart rate 136 beats/min, temperature 36.5°C, preductal SPO2 88%, postductal SPO2 90%, and blood pressure 74/37 mm Hg. All peripheral pulses were palpable. On examination, facial asymmetry as a deviation of angle of mouth to right on crying and congenital deformity of the left ear (low-set ears, small in size, having outward protrusion with intact external auditory meatus) were noted. A cardiovascular system examination revealed a wide-split second heart sound with a soft systolic ejection murmur.
Learning Objectives
-
•
To diagnose a combination of rare congenital heart diseases with the use of multimodality imaging.
-
•
To demonstrate the efficacy of a less invasive treatment strategy in managing Kommerell’s diverticulum.
Differential Diagnosis
Differential diagnosis of tetralogy of Fallot, atrioventricular septal defect, double outlet right ventricle, ventricular septal defect with pulmonary stenosis, and critical pulmonary stenosis is considered when a newborn presents with a systolic heart murmur and low oxygen saturation.
Investigations
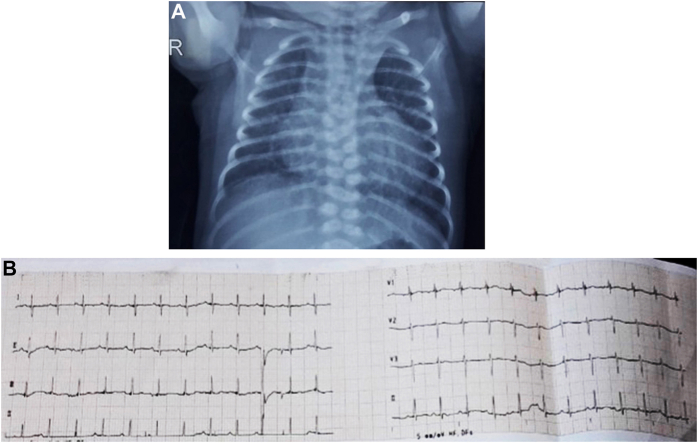
Chest x-ray showed cardiomegaly with pulmonary congestion (Figure 1A). Electrocardiogram demonstrated right axis deviation with Right bundle branch block (Figure 1B). Echocardiography evaluation showed intracardiac total anomalous pulmonary venous connection (TAPVC) to the coronary sinus and right atrium, unrestricted patent foramen oval with a right-to-left shunt, dilated coronary sinus, dilated right atrium and right ventricle, and a perimembranous ventricular septal defect (VSD) with a long patent ductus arteriosus (PDA) and right-side aortic arch.
Figure 1.
Preoperative Investigations
(A) Chest X-ray: posteroanterior view showing cardiomegaly with pulmonary congestion. (B) Electrocardiogram showing right axis deviation with right bundle branch block.
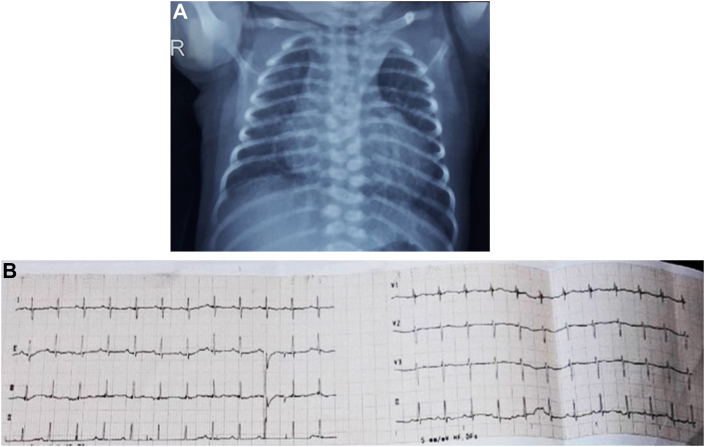
Computed tomographic (CT) angiography confirmed the right aortic arch with Kommerell’s diverticulum connected to a large and long PDA. An aberrant origin of the left subclavian artery from the Kommerell’s diverticulum was detected (Figure 2A). A well-formed vertical vein with good-sized pulmonary veins draining into the coronary sinus was identified (Figure 2B).
Figure 2.
Computed Tomographic Angiography
(A) Aberrant origin of the left subclavian artery from the Kommerell’s diverticulum. (B) Well formed vertical vein with good-sized pulmonary veins draining into the coronary sinus. AA = aortic arch; Ao = aorta; AT = anonymous trunk; CS = coronary sinus; DTA = descending thoracic aorta; KD = Kommerell’s diverticulum; LPA = left pulmonary artery; LPV = left pulmonary vein; LSA = left subclavian artery; MPA = main pulmonary artery; PDA = patent ductus arteriosus; RPA = right pulmonary artery; RPV = right pulmonary vein; VV = vertical vein.
Management
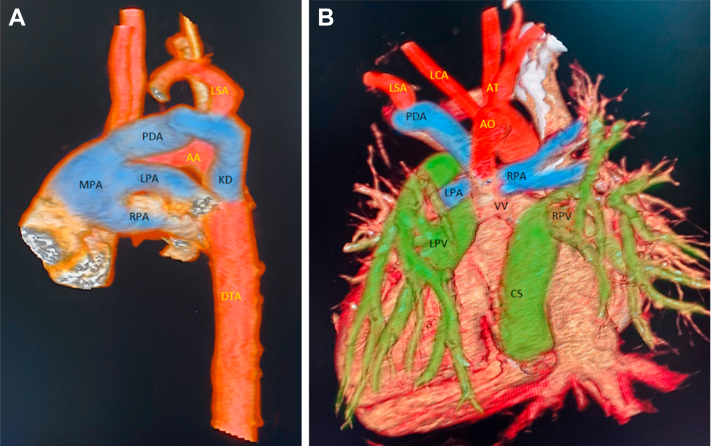
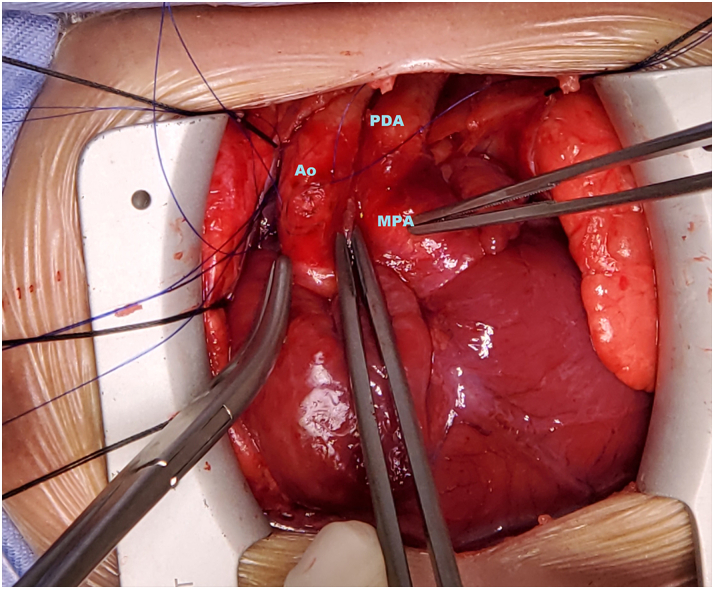
A median sternotomy was done. Cardiopulmonary bypass was established; the patient cooled down to 28 °C. During surgery, a right-side aortic arch was confirmed. The PDA was long and large and connected to the main pulmonary trunk (Figure 3). The proximal part of the PDA was a continuation to Kommerell’s diverticulum, which was an elongated and dilated tubular structure arising from the descending aorta, making a vascular ring encircling the trachea. The left subclavian artery was originating from the middle portion of the PDA and Kommerell’s diverticulum. Considering the long cylindrical structure of the PDA and the Kommerell’s diverticulum, resection or other intervention on the diverticulum was avoided. After ligation and separation of the PDA near the main pulmonary artery, the proximal part of the PDA and left subclavian artery was retracted back toward the aorta. TAPVC was repaired by means of cutback technique (deroofing the coronary sinus and diverting the coronary sinus to the left atrium with closure of the atrial septal defect with an autologous pericardial patch). The VSD was closed with an autologous pericardial patch. The postoperative period was uneventful; the baby was extubated after 8 hours of surgery. The baby was discharged on the 10th day after surgery. At 12-month follow-up, the baby remained asymptomatic with SPO2 98% in room air, developmentally normal, and was gaining weight. Repeated CT aortography at 1-year follow-up showed patent left subclavian artery without any aneurysmatic dilatation of the aorta (Figure 4).
Figure 3.
Long and Large Patent Ductus Arteriosus Connected to the Main Pulmonary Trunk
Abbreviations as in Figure 2.
Figure 4.
Patent Left Subclavian Artery With Normal-Looking Aorta at 1-Year Follow-Up
Asc Ao = ascending aorta; LCA = left carotid artery; other abbreviations as in Figure 2.
Discussion
Right-side aortic arch in combination with an aberrant left subclavian artery is a very rare congenital anomaly occurring in 0.005% of the population.1 The Edwards classification describes 3 types of the right-side aortic arch: mirror-image branching of the major arteries; aberrant left subclavian artery, as demonstrated in this case; and isolation of the left subclavian artery.2
Kommerell’s diverticulum is an aneurysmal dilation of the aorta at the origin of the aberrant subclavian artery or proximal descending aorta.3 The diverticulum is most frequently present in cases of right-side aortic arch with an aberrant left subclavian artery.4,5
Van Mierop,6 decades ago, pointed out that the presence of a diverticulum was indicative that the retroesophageal subclavian artery had initially also been connected to the arterial duct. Thus, the presence of the diverticulum implies the existence of a ligament.
In the case presented, factually, it is isolation of the left subclavian artery, but without the isolation. Because the fetal ductus arteriosus, at the origin of the aberrant left subclavian artery, carries a large volume of blood, it leads to a well dilated diverticulum of Kommerell from the aorta when the duct had been patent. When usually seen, either the duct would have closed or the dorsal aorta would have attenuated.
In contrast, patients who have tetralogy of Fallot and a right-side aortic arch do not develop an aortic diverticulum.7 Those patients have low ductal flow during fetal life because infundibular stenosis limits the normal right-to-left flow.
The presence of a left ductus arteriosus or a ligamentum arteriosum between the left subclavian artery and the left pulmonary artery in such patients results in a vascular ring. This is the most common type of vascular ring.4,5 The ring is generally loose; therefore, tracheal or esophageal compression symptoms are often mild or absent.
In a case report and literature review by Cina et al,8 most of the reports presented were in adult patients. This is because children are asymptomatic until the vascular ring or Kommerell’s diverticulum starts to compress underlying structures. We diagnosed this case at an early age owing to the presence of TAPVC causing early symptoms in the baby.
An association of Kommerell’s diverticulum with TAPVC has not been previously reported in the literature. However, Backer et al9 reported its association with VSD, tetralogy of Fallot, transposition of the great arteries, and dextrocardia.9 They proposed surgical treatment of the right arch/left ligamentum through a left thoracotomy. However, in our case, we approached it through median sternotomy because concomitant congenital defects had to be corrected. In 13 cases out of 32 reported by Cina et al,8 an aberrant subclavian artery was ligated or occluded, and in a few cases, it was reimplanted or transpositioned. In the pediatric age group, Roberts et al10 reported 30 patients with right or left aberrant subclavian arteries. The treatment included ligation of the ductus arteriosus alone in 17 patients and of the subclavian artery in 7. No symptoms of subclavian steal or arm claudication were reported over a follow-up of 16 years. In contrast, in this present case, owing to the long and large PDA, we ligated and divided only the PDA at the junction of the main pulmonary artery, letting the left subclavian artery retract toward the aorta and breaking the aortic ring anatomy.
Sometimes, the surgical strategy to manage the aneurysm depends on the anatomy, size, and presence of a concomitant thoracic aortic aneurysm. Endoaneurysmorraphy or interposition graft is usually necessary for large Kommerell’s aneurysms or if associated with an aneurysm of the descending thoracic aorta.9 Nevertheless, in this case, because of the small size of the aneurysm and its cylindrical continuity as PDA giving origin to the left subclavian artery, no aneurysmatic change at the origin of the diverticulum, and considering the early age of the baby, Kommerell’s diverticulum was not excised.
Follow-Up
At 1-year follow-up, the baby remained asymptomatic and was gaining normal weight. In the follow-up scan, the left subclavian artery was patent and there was no aneurysmatic dilation of the descending aorta. Regular follow-up of the baby has been advised to monitor the long-term outcome of this surgical strategy.
Conclusions
Early diagnosis of a combination of multiple rare congenital heart diseases is possible with the use of CT-angiography. A less invasive approach, not to excise the Kommerell’s diverticulum, seems to be acceptable for infants.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Shuford W.H., Sybers R.G., Gordon I.J., et al. Circumflex retro esophageal right aortic arch simulating mediastinal tumor or dissecting aneurysm. Am J Roentgenol. 1986;3:491–496. doi: 10.2214/ajr.146.3.491. [DOI] [PubMed] [Google Scholar]
- 2.Edwards J.E. Anomalies of the derivatives of the aortic arch system. Med Clin North Am. 1948;32:925–949. doi: 10.1016/s0025-7125(16)35662-0. [DOI] [PubMed] [Google Scholar]
- 3.Ichikawa T., Koizumi J., Tanno K., et al. Kommerell diverticulum in adults: evaluation of routine CT examinations. Tokai J Exp Clin Med. 2016;41:65–69. [PubMed] [Google Scholar]
- 4.Backer C.L., Ilbawi M.N., Idriss F.S., et al. Vascular anomalies causing tracheoesophageal compression. Review of experience in children. J Thorac Cardiovasc Surg. 1989;97:725–731. [PubMed] [Google Scholar]
- 5.van Son J.A., Julsrud P.R., Hagler D.J., et al. Surgical treatment of vascular rings: the Mayo Clinic experience. Mayo Clin Proc. 1993;68:1056–1063. doi: 10.1016/s0025-6196(12)60898-2. [DOI] [PubMed] [Google Scholar]
- 6.van Mierop L.H.S., Patterson D.F., Schnarr W.R. Pathogenesis of persistent truncus arteriosus in light of observation made in dog embryo with the anomaly. Am J Cardiol. 1978;41(4):755–762. doi: 10.1016/0002-9149(78)90828-7. [DOI] [PubMed] [Google Scholar]
- 7.Velasquez G., Nath P.H., Castaneda-Zuniga W.R., et al. Aberrant left subclavian artery in tetralogy of Fallot. Am J Cardiol. 1980;45:811–818. doi: 10.1016/0002-9149(80)90126-5. [DOI] [PubMed] [Google Scholar]
- 8.Cina C.S., Althani H., Pasenau J., et al. Kommerell’s diverticulum and right-sided aortic arch: a cohort study and review of the literature. J Vasc Surg. 2004;39:131–139. doi: 10.1016/j.jvs.2003.07.021. [DOI] [PubMed] [Google Scholar]
- 9.Backer C.L., Mavroudis C., Rigsby C.K., et al. Trends in vascular ring surgery. J Thorac Cardiovasc Surg. 2005;129:1339–1347. doi: 10.1016/j.jtcvs.2004.10.044. [DOI] [PubMed] [Google Scholar]
- 10.Roberts C.S., Othersen H.B.J., Sade R.M., et al. Tracheoesophageal compression from aortic arch anomalies: analysis of 30 operatively treated children. J Pediatr Surg. 1994;29:334–337. doi: 10.1016/0022-3468(94)90343-3. [DOI] [PubMed] [Google Scholar]