Abstract
Background:
Hospital visitation restrictions during the COVID-19 pandemic prompted concerns about unintended consequences for older patients, including an increased incidence of delirium and agitation. While first-line interventions for these conditions are non-pharmacologic, a lack of family support could result in increased use of benzodiazepines and antipsychotics, which are associated with poor outcomes in older adults. Little is known about the association of visitation policies with use of these medications among older adults.
Methods:
We conducted a retrospective cross-sectional study among adults age ≥65 hospitalized from March 1 through May 31, 2020 at four hospitals in the Mid-Atlantic. The dates of onset of visitation restrictions (i.e., hospital-wide guidelines barring visitors) were collected from hospital administrators. Outcomes were use of benzodiazepines and antipsychotics, assessed using patient-level electronic health record data. Using multivariable logistic regression with hospital and study-day fixed effects, the quasi-experimental study design leveraged the staggered onset of visitation restrictions across the hospitals to measure the odds of receiving each medication when visitors were vs were not allowed.
Results:
Among 2,931 patients, mean age was 76.6 years (SD, 8.3), 51.6% were female, 58.6% white, 32.5% Black, and 2.6% Hispanic. Overall, 924 (31.5%) patients received a benzodiazepine and 298 (10.2%) an antipsychotic. The adjusted odds of benzodiazepine use was lower on days when visitors were vs were not allowed (adjusted odds ratio [AOR], 0.62; 95% CI, 0.39, 0.99). Antipsychotic use did not significantly differ between days when visitors were vs were not allowed (AOR, 0.98; 95% CI, 0.43, 2.21).
Conclusions:
Among older patients hospitalized during the first wave of the pandemic, benzodiazepine use was lower on days when visitors were allowed. These findings suggest that the presence of caregivers impacts use of potentially inappropriate medications among hospitalized older adults, supporting efforts to recognize caregivers as essential members of the care team.
Keywords: Potentially inappropriate medications, visitation restrictions, acute care hospitals, older adults
INTRODUCTION
To limit the spread of coronavirus during the COVID-19 pandemic, acute care hospitals rapidly adopted visitation restrictions for hospitalized patients.1,2 These restrictions prompted concerns about unintended consequences for patients, especially older adults.3,4 For older adults, isolation from family members and caregivers while hospitalized may lead to increased incidence of delirium, agitation, and anxiety.4,5 First-line interventions for these conditions are non-pharmacologic, such as having a family member or caregiver present at the bedside who can help improve orientation and reduce agitation.6–8 A lack of family support may increase the use of medications to control these symptoms,9 such as benzodiazepines and antipsychotics.10 It is unknown whether visitation restrictions among hospitalized older adults are associated with use of these medications.11
Studies conducted in other care settings show that prescribing of psychotropic medications increased during the pandemic. Among Ontario nursing home residents, prescribing of antipsychotics and antidepressants increased.12 In England, the proportion of patients with dementia who were prescribed antipsychotics increased.13 However, these studies were not designed to examine the impacts of visitation restrictions on medication use. As the pandemic continues to affect hospital visitation policies, understanding this association is important to inform policies and interventions to limit use of potentially inappropriate medications among hospitalized older adults.
METHODS
Design overview
We conducted a retrospective cross-sectional study of patients ages 65 and older hospitalized between March 1 and May 31, 2020, at four acute care hospitals affiliated with a large health system in the Mid-Atlantic. Three hospitals were urban and one was suburban. The hospitals were in close geographic proximity with similar community COVID transmission rates. We extracted patients’ electronic health records (EHRs), including demographics, diagnoses, hospital admission and discharge dates, and medication administration records. We examined the association of visitation policies at each hospital with use of benzodiazepines and antipsychotics. The Institutional Review Board of the University of Pennsylvania reviewed and approved the study protocol with a waiver of informed consent.
Setting and participants
We included all patients aged 65 and older who were hospitalized during the study period in any of the four hospitals. Because criteria for use of benzodiazepines and antipsychotics differ for patients in the intensive care unit (ICU) and at the end of life, we excluded patients who were admitted to the ICU and those who died during the hospital stay. We excluded medication orders that were prescribed but not given (e.g., cancelled orders).
Measures
Outcomes
The co-primary outcomes were the use of two classes of potentially inappropriate medications, benzodiazepines and antipsychotics. Benzodiazepines and anti-psychotics are FDA-approved for the treatment of certain psychiatric conditions,14,15 but are often used off-label among older adults to treat delirium, agitation, anxiety, and behavioral symptoms associated with dementia.16,17 We defined “potentially inappropriate medications” using the American Geriatrics Society (AGS) 2019 Updated Beers Criteria (i.e., medications that should typically be avoided in older adults because the risk of harms outweighs the potential benefits).9
Time of medication administration was measured for each 24-hour patient-day of the hospital stay. Each outcome was a dichotomous indicator set to “1” if the patient received any doses of the medication during the 24-hour period and “0” if they did not receive any doses.
Exposure
The primary exposure was the presence of visitation restrictions on each hospital-day, defined as official hospital-wide guidelines that barred visitors to hospitalized patients. Visitation restrictions were implemented on different dates at the four hospitals. Restrictions were similar across hospitals and specified that no visitors were allowed, except for one designated healthy visitor for patients with special needs (defined as patients with disabilities involving compromised communication, such as dementia or developmental delays, whose caregiver is essential to their care). Exceptions were granted via an application process by patients’ families to the hospital care team; applications were rare during the study period. We collected information on dates of visitation restrictions from e-mails and interviews with hospital administrators. We used these sources to create a timeline of policies for each hospital. We validated timelines by sending them to administrators for review and correction.
Other measures
Patient characteristics included self-reported age (categorized as 65–74 years, 75–84, ≥85), race (white, Black, Asian, or other), ethnicity (Hispanic, non-Hispanic, unknown), gender, and comorbid conditions, measured using the Charlson Comorbidity Index based on hospital ICD-10 codes.18,19 To increase the sensitivity of the Charlson measure for dementia, we included ICD-10 dementia diagnoses from HEDIS measures20 and dementia-specific medications (i.e., donepezil, rivastigmine, galantamine, memantine).21 Other variables included hospital length of stay, total medications administered each day, day, and hospital.
Statistical analysis
To compare the characteristics of patients who were hospitalized when visitors were versus were not allowed, we used χ2 and Cochran-Mantel-Haenszel tests. To measure the association of visitation policy with use of each medication class, we estimated multivariable logistic regression models with an indicator for visitors allowed (yes/no) as the primary exposure and administration of a medication in each class as the outcome, at the level of the patient-day. To implement the staggered difference-in-difference design, models included hospital and study-day fixed effects. We adjusted analyses for age category, gender, race, ethnicity, Charlson comorbidities, total medications administered, and length of stay. Because the analysis was performed at the level of the patient-day and each patient could have multiple observations, we estimated cluster-robust standard errors at the patient level. All statistical testing was 2-tailed, with p-value <0.05 considered statistically significant. We conducted analyses using Stata 17 (College Station, TX).
RESULTS
Participant characteristics
Among the 2,931 patients, mean age was 76.6 years (SD, 8.3), 51.6% were female, 58.6% were white, 32.5% Black, 2.1% Asian, and 6.8% other race, and 2.6% were Hispanic (Table 1). Five hundred twenty-four patients (17.9%) were hospitalized while visitors were allowed, 2206 (75.3%) while visitors were not allowed, and 201 (6.9%) while hospital policies changed from visitors allowed to not allowed.
Table 1.
Baseline Characteristics of 2931 Hospitalized Older Adults
| Characteristic | Participants, No. (%)a (N=2931) |
|---|---|
| Age range, years | |
| 65–75 | 1428 (48.7) |
| 75–84 | 964 (32.9) |
| >=85 | 539 (18.4) |
| Gender | |
| Male | 1419 (48.4) |
| Female | 1512 (51.6) |
| Race | |
| White | 1717 (58.6) |
| Black or African American | 953 (32.5) |
| Asian | 62 (2.1) |
| Other race | 199 (6.8) |
| Ethnicity | |
| Not Hispanic | 2817 (96.1) |
| Hispanic | 76 (2.6) |
| Unknown | 38 (1.3) |
| Charlson Comorbidity Index | |
| 0 | 334 (11.4) |
| 1–2 | 929 (31.7) |
| 3–5 | 958 (32.7) |
| 6+ | 710 (24.2) |
Percentages may not sum to 100% due to rounding
The patients spent a total of 14,497 days hospitalized during the study period: 2,358 (16.3%) while visitors were allowed and 12,139 (83.7%) while visitors were not allowed (Table 2). A higher proportion of days when visitors were not allowed occurred among patients who were Black, Hispanic, had a Charlson Comorbidity Score of ≥3, received a higher mean number of medications, and had a longer length of stay.
Table 2.
Characteristics of Patient-Days in the Two Groups: Visitors Allowed vs. Visitors not Allowed (n=14,497 patient-days)
| Characteristica | Patient-days when visitors were allowed (n=2358) | Patient-days when visitors were not allowed (n=12139) | P-value |
|---|---|---|---|
| Patient Demographics, No. (%) | |||
| Age range, years | |||
| 65–75 | 1075 (45.6%) | 6163 (50.8%) | <.001 |
| 75–84 | 822 (34.9%) | 3889 (32.0%) | |
| >=85 | 461 (19.6%) | 2087 (17.2%) | |
| Gender | |||
| Male | 1238 (52.5%) | 6213 (51.2%) | .24 |
| Female | 1120 (47.5%) | 5926 (48.8%) | |
| Race | |||
| White | 1479 (62.7%) | 6553 (54.0%) | <.001 |
| Black or African American | 661 (28.0%) | 4616 (38.0%) | |
| Asian | 44 (1.9%) | 214 (1.8%) | |
| Other | 174 (7.4%) | 756 (6.2%) | |
| Ethnicity | |||
| Not Hispanic | 2285 (96.9%) | 11673 (96.2%) | <.001 |
| Hispanic | 33 (1.4%) | 331 (2.7%) | |
| Unknown | 40 (1.7%) | 135 (1.1%) | |
| Clinical Characteristics, No. (%) | |||
| Charlson Comorbidity Index | |||
| 0 | 234 (9.9%) | 963 (7.9%) | <.001 |
| 1–2 | 730 (31.0%) | 3041 (25.1%) | |
| 3–5 | 768 (32.6%) | 4344 (35.8%) | |
| 6+ | 626 (26.5%) | 3791 (31.2%) | |
| Hospitalization characteristics | |||
| Total medications, mean (SD) | 9.3 (11.4) | 7.5 (8.8) | <.001 |
| Length of stay, mean (SD) | 6.8 (5.8) | 10.0 (9.1) | <.001 |
Abbreviations: SD, standard deviation.
Percentages may not sum to 100% due to rounding.
Patterns of medication use
Overall, 924 patients received a benzodiazepine, of whom 164 (17.1%) were hospitalized while visitors were allowed, 672 (72.7%) while visitors were not allowed, and 88 (9.5%) while policies changed. Two hundred ninety-eight patients received an antipsychotic, of whom 35 (11.7%) were hospitalized while visitors were allowed, 241 (80.9%) while visitors were not allowed, and 22 (7.4%) while policies changed. One hundred eighteen patients (4.0%) received both medication classes; most received a benzodiazepine first (72 [61.0%]).
Association of visitation policies and other characteristics with medication use
The adjusted odds of benzodiazepine use was lower on days when visitors were allowed versus not allowed (AOR, 0.62, 95% CI, 0.39–0.99; Figure 1A). The adjusted odds of benzodiazepine use was lower among patients aged 75–84 and ≥85 versus those aged 65–74 (AOR 75–85 years, 0.74, 95% CI, 0.62–0.88; AOR ≥85 years, 0.70, 95% CI, 0.56–0.87) and patients who were Black versus white (AOR 0.55, 95% CI, 0.44–0.68). The adjusted odds of benzodiazepine use was higher among patients who were Hispanic (AOR, 1.64; 95% CI, 1.06–2.54) and received a higher number of medications (AOR 1.06; 95% CI, 1.05–1.07).
Figure 1. Association of Visitation Policies with Benzodiazepine and Antipsychotic Use per Patient-Day Among Hospitalized Older Adults.
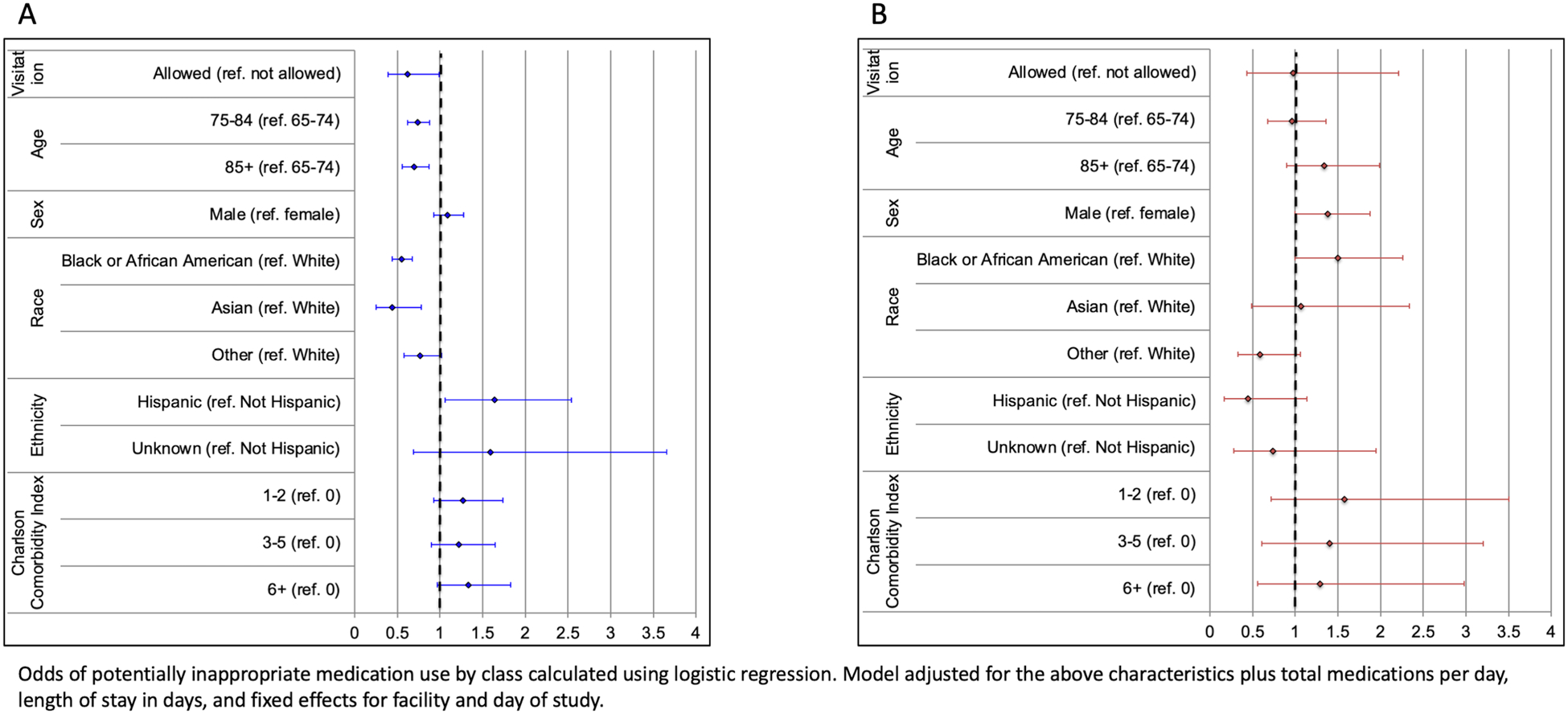
The figure shows the odds ratios and 95% confidence intervals for the association of visitation policies and other participant characteristics with benzodiazepine use (panel A) and antipsychotic use (panel B) per patient-day.
Antipsychotic use did not significantly differ between days when visitors were versus were not allowed (AOR 0.98; 95% CI 0.43, 2.21; Figure 1B). The adjusted odds of antipsychotic use was higher among men compared to women (AOR 1.38; 95% CI, 1.00–1.88). The adjusted odds of antipsychotic use was higher among patients with a higher number of medications (AOR, 1.04; 95% CI, 1.03–1.05) and a longer length of stay (AOR, 1.03; 95% CI, 1.01–1.05).
DISCUSSION
In this study of older adults hospitalized during the first wave of the COVID pandemic, allowing visitors was associated with lower odds of benzodiazepine and antipsychotic use, though only the odds of benzodiazepine use was significantly lower. These findings support efforts to limit visitation restrictions for hospitalized older adults and to recognize caregivers as essential members of the care team.
The association of visitation restrictions with benzodiazepine use is consistent with prior studies showing that prescribing of psychotropic medications increased during the pandemic among patients in nursing homes.12,13 While prior studies did not examine visitation policies, restrictions were prevalent in nursing homes during the pandemic. The mechanism through which visitation restrictions may be associated with benzodiazepine use is unclear. A lack of caregiver support may lead to increased incidence of delirium, agitation, or anxiety,22 which in turn leads to increased benzodiazepine use. Unfortunately, delirium is not well-documented in EHRs and we were unable to measure delirium in our dataset.
We did not observe significantly lower odds of antipsychotic use associated with visitation. Several factors may explain this finding. First, due to incomplete historical medication reconciliation data at hospital admission, we were unable to distinguish between medications prescribed before versus during hospitalization. It is possible that benzodiazepines were more often prescribed “as-needed” in the hospital and thus for their use to be sensitive to the presence of visitors, while antipsychotics were more often prescribed “standing” before admission. In additional analyses, we found that lorazepam and haloperidol were the most-used medications in each class. These are commonly prescribed as-needed, not long-term. However, quetiapine and olanzapine, which are commonly used long-term, comprised more than half of antipsychotic patient-days. Second, antipsychotics were used less frequently in our sample than benzodiazepines. Because our analytic approach was designed around visitation policies that changed over several days, infrequent antipsychotic use may have exacerbated the small-sample bias.
The role of caregivers for improving orientation and reducing agitation is a key component of evidence-based, multi-component interventions to reduce delirium among hospitalized older adults.6,23,24 Our findings suggest that the presence of caregivers also impacts quality of medication prescribing. The Caregiver Advise, Record, Enable (CARE) Act has been adopted by most states and requires some hospitals to involve caregivers in discharge planning, providing a platform to better integrate caregivers into care teams.25 Our findings emphasize the importance of the caregivers’ role throughout hospitalization, not just at discharge. Our findings also suggest that patients without caregivers should be recognized as a higher-risk group.
This study has several limitations. First, the observational design precludes conclusions about causality. Our quasi-experimental study design leveraged the differing onset of visitation restrictions at each hospital to measure change in medication use over time and relative to other hospitals. While change in medication use is potentially attributable to visitation restrictions, other events that occurred simultaneously may confound our findings. Second, we did not distinguish between medications used before hospitalization versus started during hospitalization. Nevertheless, benzodiazepines are not first-line agents for managing chronic conditions among older adults. Third, we were unable to identify medication use for procedural sedation. We excluded patients admitted to the ICU, who likely required sedation while intubated. Fourth, data were collected during spring 2020, when visitation restrictions were stringent and caregivers may have been less likely to advocate for visitation due to fears of COVID transmission; while our dataset did not include information on which patients received exemptions to visitation restrictions, exceptions were rarely requested during the study period. Since then, many hospitals have loosened visitation restrictions. These considerations limit the generalizability of our findings over time and to other settings.
Among older patients hospitalized during the first wave of the pandemic, benzodiazepine use was lower on days when visitors were allowed. This finding is consistent with the hypothesis that the presence of visitors improves orientation and reduces agitation among older adults, leading to reduced use of potentially inappropriate psychotropic medications.8 These medications are not only associated with adverse inpatient outcomes, but frequently lead to problems when continued after discharge.26,27 Our findings underscore the importance of caregivers for ensuring quality care for older adults and support efforts to better integrate caregivers into care teams.
Key points:
Among older adults hospitalized during the first wave of the COVID-19 pandemic, the adjusted odds of benzodiazepine use was lower on days when visitors were versus were not allowed
Antipsychotic use did not significantly differ between days when visitors were versus were not allowed
Why does this matter?
These findings suggest that the presence of caregivers impacts use of psychoactive medication use among hospitalized older adults, supporting efforts to recognize caregivers as essential members of the care team
ACKNOWLEDGEMENTS
Dr. Brown (corresponding author) affirms that she has listed everyone who contributed significantly to the work and has obtained written consent from all contributors who are not authors and are named in the Acknowledgment section.
Funding, presentations, and preprint disclosures:
This work was supported by grant K08AG052572 from the National Institute on Aging at the National Institutes of Health (Dr. Ryskina) and by grant K76AG057016 from the National Institute on Aging at the National Institutions of Health and the American Federation for Aging Research (Dr. Brown). This study was presented as a poster at the American Geriatrics Society Annual Scientific Meeting on Thursday, May 12, 2022. There are no other preprints of this or related manuscripts.
Sponsor’s Role:
The sponsors had no role in the design, methods, subject recruitment, data collections, analysis, or preparation of the manuscript. Dr. Brown is an employee of the Corporal Michael J. Crescenz VA Medical Center. The opinions expressed in this manuscript may not represent those of the Department of Veterans Affairs.
Footnotes
Conflict of Interest:
The authors have no conflicts.
REFERENCES
- 1.Weiner HS, Firn JI, Hogikyan ND, et al. Hospital visitation policies during the SARS-CoV-2 pandemic. Am J Infect Control. 2021;49(4):516–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jaswaney R, Davis A, Cadigan RJ, et al. Hospital policies during COVID-19: an analysis of visitor restrictions. J Public Health Manag Pract. 2021;28(1):E299–E306. [DOI] [PubMed] [Google Scholar]
- 3.Reinhard S, Drenkard K, Choula R, Curtis A. Alone and Confused: The Effects of Visitor Restrictions on Older Patients and Families. AARP Thinking Policy Blog. Available at: https://blog.aarp.org/thinking-policy/alone-and-confused-the-effects-of-visitor-restrictions-on-older-patients-and-families. Accessed March 25, 2022. [Google Scholar]
- 4.Karlawish J Hospitalized adults need their caregivers — they aren’t visitors. STAT News, First Opinion. Available at: https://www.statnews.com/2020/03/29/hospitalized-adults-need-their-caregivers-they-arent-visitors/. Accessed March 25, 2022. [Google Scholar]
- 5.Marcantonio ER. Delirium in Hospitalized Older Adults. N Engl J Med. 2017;377(15):1456–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–76. [DOI] [PubMed] [Google Scholar]
- 7.Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilensky GR. It is time for hospitals to liberalize their visitation policies. JAMA Health Forum. 2021;2(5):e211545. [DOI] [PubMed] [Google Scholar]
- 9.2019 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674–694. [DOI] [PubMed] [Google Scholar]
- 10.Wang H, Li T, Barbarino P, et al. Dementia care during COVID-19. Lancet. 2020;395(10231):1190–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moss SJ, Krewulak KD, Stelfox HT, et al. Restricted visitation policies in acute care settings during the COVID-19 pandemic: a scoping review. Crit Care. 2021;25(1):347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stall NM, Zipursky JS, Rangrej J, et al. Assessment of psychotropic drug prescribing among nursing home residents in Ontario, Canada, during the COVID-19 pandemic. JAMA Intern Med. 2021;181(6):861–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howard R, Burns A, Schneider L. Antipsychotic prescribing to people with dementia during COVID-19. Lancet Neurol. 2020;19(11):892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Food and Drug Administration. Atypical Antipsychotic Drugs Information. Available at: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/atypical-antipsychotic-drugs-information. Accessed March 25, 2022
- 15.U.S. Food and Drug Administration. Benzodiazepine Drug Information. Available at: https://www.fda.gov/drugs/information-drug-class/benzodiazepine-drug-information. Accessed March 25, 2022
- 16.Maher AR, Maglione M, Bagley S, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA.Sep282011;306(12):1359–69. [DOI] [PubMed] [Google Scholar]
- 17.Gerlach LB, Wiechers IR, Maust DT. Prescription benzodiazepine use among older adults: a critical review. Harv Rev Psychiatry. 2018;26(5):264–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 19.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9. [DOI] [PubMed] [Google Scholar]
- 20.HEDIS Measures and Technical Resources, National Committee for Quality Assurance. Medication Management in Older Adults. Available at: https://www.ncqa.org/hedis/measures/medication-management-in-the-elderly/. Accessed March 25, 2022.
- 21.Jaakkimainen RL, Bronskill SE, Tierney MC, et al. Identification of physician-diagnosed Alzheimer’s Disease and related dementias in population-based administrative data: a validation study using family physicians’ electronic medical records. J Alzheimers Dis. 2016;54(1):337–49. [DOI] [PubMed] [Google Scholar]
- 22.Nassar AP Junior, Besen BAMP, Robinson CC, Falavigna M, Teixeira C, Rosa RG. Flexible versus restrictive visiting policies in ICUs: a systematic review and meta-analysis. Crit Care Med. 2018;46(7):1175–1180. [DOI] [PubMed] [Google Scholar]
- 23.Martinez F, Tobar C, Hill N. Preventing delirium: should non-pharmacological, multicomponent interventions be used? A systematic review and meta-analysis of the literature. Age Ageing. 2015;44(2):196–204. [DOI] [PubMed] [Google Scholar]
- 24.Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK. Hospital Elder Life Program: systematic review and meta-analysis of effectiveness. Am J Geriatr Psychiatry. 2018;26(10):1015–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Friedman EM, Tong PK. A framework for integrating family caregivers into the health care team. RAND. Available at: https://www.rand.org/pubs/research_reports/RRA105-1.html. Accessed March 25, 2022. [Google Scholar]
- 26.Herzig SJ, Rothberg MB, Guess JR, et al. Antipsychotic use in hospitalized adults: Rates, indications, and predictors. J Am Geriatr Soc. 2016;64(2):299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bell CM, Fischer HD, Gill SS, et al. Initiation of benzodiazepines in the elderly after hospitalization. J Gen Intern Med. 2007;22(7):1024–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


