The incidence of differentiated thyroid cancer (DTC) has increased sharply in high-income countries over the last few decades; however, prognosis remains excellent, with 5-year survival rates above 95% even with regional disease spread. Health-related quality of life (HRQOL) is therefore a critical outcome measure in DTC, as complications from treatment can result in lifelong morbidity. Understanding factors that HRQOL after surgery can guide patient-centered care, from decisions on surgical extent to provision of resources to optimize patients’ postoperative psychosocial well-being, and enable further refinement of current HRQOL assessment tools. Existing tools to measure HRQOL include general or disease-specific domains of well-being. The validated THYCA-QoL assessment focuses on common symptoms caused by thyroid cancer and its treatment, including voice changes, hypocalcemia-related complaints, mood disturbances, and fatigue.1 Yet, additional factors not captured in the assessment may modulate the subjective experience of these symptoms and independently affect HRQOL.
We correlated qualitative codes assigned to patient interviews with HRQOL assessment scores to identify domains likely to have a significant, but overlooked, impact on HRQOL in thyroid cancer patients. We leveraged a unique dataset from a randomized controlled trial assessing surgical intervention for low-risk DTC. Each patient was evaluated at up to five set time-points before and after surgery, and at each visit, participated in a semi-structured interview (qualitatively coded by trained researchers) and also completed several validated HRQOL assessments.2, 3 These data allowed us to directly associate HRQOL scores with the concepts and elements of discussion from transcribed patient interviews, identified by the qualitative codes. Using methods similar to those previously described in the literature,4, 5 we trained ElasticNet regularized regression, an algorithm similar to logistic regression but which penalizes overly complex models, to predict HRQOL scores from the qualitative codes assigned to each transcript (up to 5 per patient). As ElasticNet is designed to identify a subset of explanatory variables from among all candidate features, we used this property to find the most salient qualitative codes from all possible candidates. We fitted ElasticNet models to the summary scores of each HRQOL assessment, using the scikit-learn module of Python (0.23.2; Pedregosa, 2011).6 We chose parameters using cross-validation, and assessed accuracy using the average R2 score over 1000 runs of the algorithm in order to ensure model stability, and account for multicollinearity of the independent variables. We then ranked features by how frequently they were included in the model, and the most frequently selected features are reported.7 The Figure gives an overview of the data source, pre-processing, and analysis steps. As the THYCA model was the most accurate, we present the qualitative codes selected by this model.
Figure:
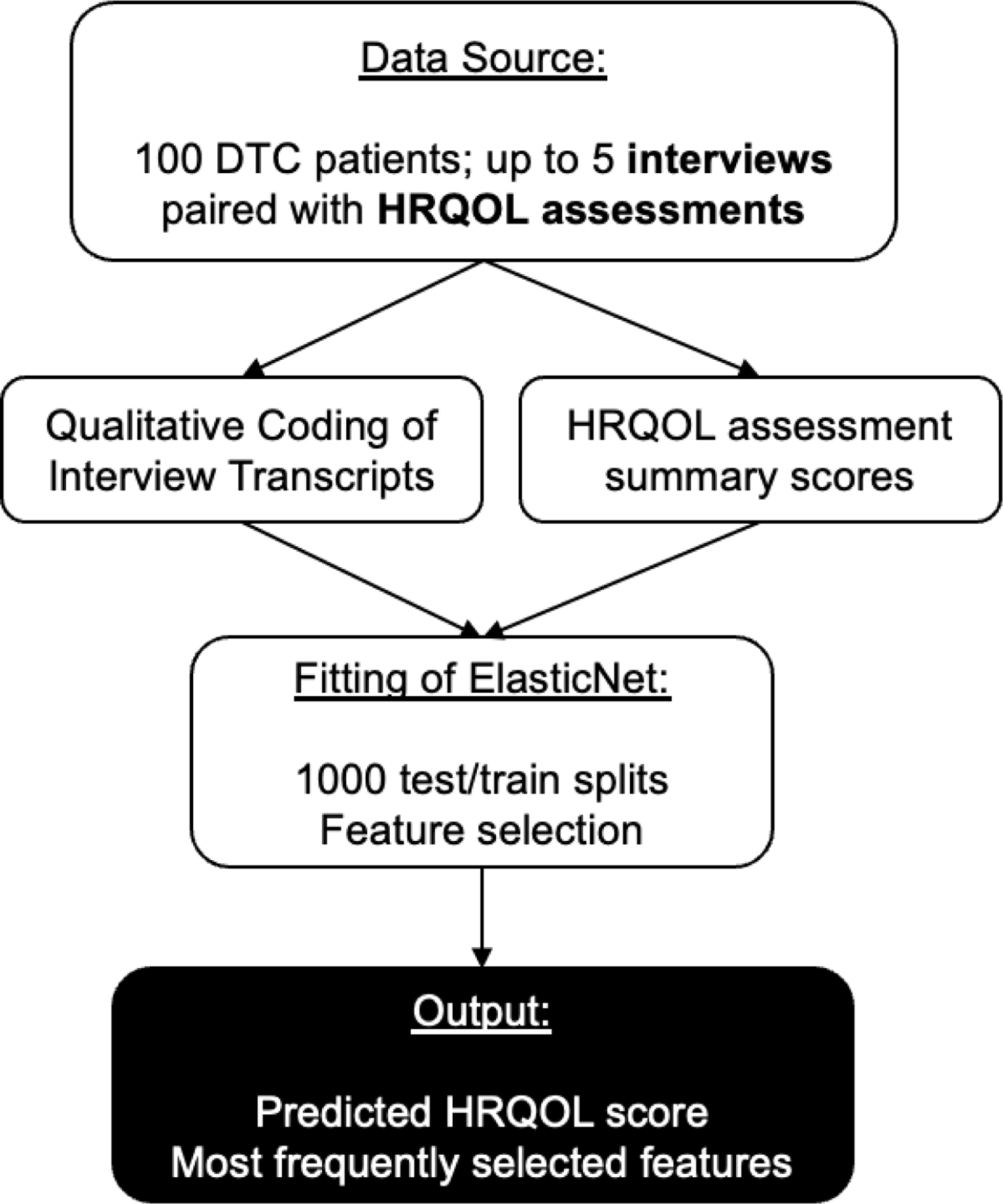
Data source, preprocessing and analysis.
Abbreviations: DTC, Differentiated Thyroid Cancer; HRQOL, Health-related Quality of Life
Patients participated in up to 5 semi-structured interviews each. At the time of each interview, patients also completed several HRQOL assessments, including THYCA-QoL. Interviews were transcribed and qualitatively coded by trained researchers. Over 1000 runs using random splits of the dataset into training (80%) and test (20%) sets, ElasticNet models were used to predict HRQOL assessment summary scores from the assigned qualitative codes. The model was fitted using the training set and evaluated on the test set. Model parameters were selected using 5-fold cross validation. ElasticNet penalizes overly complex models; on each run, only a subset of features (qualitative codes) are included in the fitted model. The average R2 value over 1000 runs was used to determine model accuracy. The most frequently selected features across the 1000 runs were recorded.
In total, 100 patients completed 380 interviews. Each transcript received a mean of 125 qualitative codes. Multiple researchers coded the same material, with excellent intercoder reliability (κ = 0.79). When fitting the ElasticNet to average THYCA score, 8 qualitative codes were selected in all 1000 runs. These codes were related to concepts of lifestyle modification by avoidance of activities, treatment interactions, frustration, sadness, symptom onset, tiredness, and patients feeling “not myself” (associated with lower HRQOL as measured by average THYCA), and happiness (associated with higher HRQOL) (Table). Other codes also associated with higher HRQOL appeared further in the ranking, such as sharing cancer experiences with others (included in 97.8% of runs), and relief (97.6%).
Table:
Most Frequently Selected Features in Average THYCA Value Prediction
| 95% Confidence Interval |
||||
|---|---|---|---|---|
| Code | Selection Frequency | Average Coefficient | Lower | Upper |
| Compensation Strategies: Lifestyle Modification: Avoidance | 1.000 | 0.840 | 0.487 | 1.404 |
| Procedures: Symptom/Complication Treatment: Treatment Interactions | 1.000 | 1.244 | 0.595 | 2.331 |
| Shared Properties: Emotions: Frustrated | 1.000 | 1.387 | 0.918 | 2.259 |
| Shared Properties: Emotions: Happy | 1.000 | −0.923 | −1.628 | −0.486 |
| Shared Properties: Emotions: Sadness | 1.000 | 1.333 | 0.783 | 2.370 |
| Shared Properties: Timeline: Onset | 1.000 | 1.127 | 0.694 | 1.873 |
| Symptoms: Fatigue: Tiredness | 1.000 | 1.262 | 0.816 | 1.972 |
| Thyroid Cancer: Recovery: Normality: Not Myself | 1.000 | 2.352 | 1.290 | 4.813 |
| Shared Properties: Support: Financial | 0.999 | 2.277 | 0.972 | 4.247 |
| Shared Properties: Support: Non-Monetary | 0.999 | 0.855 | 0.404 | 1.587 |
| Interview Section: Impact: Interferes: Most | 0.998 | 0.920 | 0.518 | 1.597 |
| Shared Properties: Attribution: To Thyroid | 0.998 | 0.889 | 0.460 | 1.579 |
| Symptoms: Voice | 0.998 | 0.902 | 0.549 | 1.515 |
| Shared Properties: Timeline: Narrative | 0.997 | 0.930 | 0.452 | 1.575 |
| Symptoms: Mental: Mood: Depression | 0.997 | 0.973 | 0.497 | 1.560 |
| Symptoms: Sleep: Difficulty Sleeping | 0.997 | 0.781 | 0.407 | 1.314 |
| Symptoms: Fatigue | 0.996 | 0.992 | 0.580 | 1.556 |
| Symptoms: Hypoparathyroidism: Location: Hands | 0.995 | 0.804 | 0.300 | 1.496 |
| Symptoms: Temperature Intolerance: Cold | 0.994 | 1.342 | 0.330 | 2.598 |
| Shared Properties: Support | 0.991 | 0.734 | 0.250 | 1.163 |
The 20 qualitative codes most frequently included in the ElasticNet regression model for the prediction of Average THYCA score. 8 codes were included in 100% of the 1000 runs performed. Positive coefficients indicate that the presence of the code predicted higher average THYCA; negative coefficients indicate the presence of the code predicted lower average THYCA. Note that as higher THYCA scores correspond to decreased HRQOL, positive coefficients imply features that predict a higher Average THYCA score, and thus a lower HRQOL.
The feature selection property of the ElasticNet revealed domains of HRQOL not explicitly captured by surveys. Many of the codes that pertain to these domains do appear among the most commonly selected features: fatigue, voice symptoms, cold intolerance, and hypoparathyroidism symptoms in the hands encompass five of the twenty-four items on the THYCA-QoL questionnaire, and all appear among the top twenty codes selected by the model. This indicates that the results are consistent with the disease-specific HRQOL scale. Importantly, the feature selection process also pointed to concepts that were not part of the THYCA-QoL questionnaire, but that were highly predictive of average THYCA score, which could indicate domains of HRQOL not specifically captured by the THYCA tool but do correlate with summative measures of HRQOL. Some of these codes were expected (such as sadness, fatigue, and depression); others were not necessarily obvious. For example, the THYCA-QoL does not explicitly ask about lifestyle modification by avoidance of certain activities, but this code was selected in 100% of the ElasticNet runs with a significant association with average THYCA score. Hence, we infer that a return to normalcy is valued by patients, which may be difficult to capture with questions that focus on specific symptoms. Similarly, the code corresponding to treatment interactions in the context of symptom and complication treatment was also selected in 100% of the runs. Such discussion of symptoms and complications might pertain to problems scheduling multiple medications (e.g., calcium, vitamin D, and levothyroxine), and side effects from one treatment influencing adherence to another. While the items of THYCA-QoL ask about each individual symptom or complication of thyroid cancer treatment, the questionnaire does not address interactions between these symptoms, or about how the interactions between treatments compound the seriousness of these symptoms. This information is thus emergent from the content of the annotated interviews themselves.
Using HRQOL data in conjunction with annotated narrative data to reveals important determinants of HRQOL in thyroid cancer not explicitly stated by surveys. While the ElasticNet model has some predictive capability, our primary focus here is on its feature selection property; the results are thus not meant to conclude definitively what determines HRQOL for each individual patient, but rather to provide a starting point for potential issues to explore pertaining to HRQOL. We found that current assessments may overemphasize the presence or absence of specific symptoms. In counseling patients, surgeons often focus on oncologic outcomes such as completeness of neck dissection, as well as specific complications such as hypocalcemia, recurrent laryngeal nerve palsy, and hematoma. In doing so we may miss what patients value most: to have their fears and emotions addressed; we may thus fail to set expectations regarding the possibilities of depression, fatigue, and difficulty sleeping after surgery, or to provide an adequate roadmap of postoperative recovery and return to normalcy. We often do not solicit information regarding these emotional states, and miss opportunities to provide support.
We also found that discussion of financial support was associated with a worse THYCA score. This is in line with a growing body of literature showing that thyroid cancer has a significant financial impact and is associated with bankruptcy.8 Thyroid cancer does not shorten life expectancy as many other malignancies do, and survivors require lifelong medications, laboratory assessments, imaging, and visits for surveillance and treatment. Financial difficulty has a significant impact on quality of life, and should be considered in recommendations regarding frequency of surveillance in low risk cancers. We must also consider patient finances and insurance when ordering more expensive options such as CT scans or radioactive iodine therapy and discuss cost with patients as an aspect of thyroid cancer treatment.
While we must still assess the extent of symptoms, we must also understand and acknowledge the emotional aspects of the patient’s treatment experience, which are tied to, but not wholly explained by the presence of symptomatology, and consider more global aspects such as the financial burden of thyroid cancer treatment when advising patients. In the future, it may also be interesting to repeat this analysis on data from patients with more advanced malignancies, who may suffer higher complication rates, but also experience more immense feelings of relief after treatment.
Acknowledgements:
The authors would like to thank the original study team and qualitative health research team for providing access to this data.
Funding:
This work was supported by the National Institute on Deafness and Other Communication Disorders [grant T32DC009401] and by the National Institutes of Health/National Center for Advancing Translational Sciences [grant UL1TR002373].
Footnotes
Conflicts/Disclosures:
None
References
- 1.Husson O, Haak HR, Mols F, et al. Development of a disease-specific health-related quality of life questionnaire (THYCA-QoL) for thyroid cancer survivors. Acta Oncol Feb 2013;52(2):447–54. doi: 10.3109/0284186X.2012.718445 [DOI] [PubMed] [Google Scholar]
- 2.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst Mar 3 1993;85(5):365–76. [DOI] [PubMed] [Google Scholar]
- 3.Bhandari NR, Kathe N, Hayes C, Payakachat N. Reliability and validity of SF-12v2 among adults with self-reported cancer. Research in Social and Administrative Pharmacy 2018;14(11):1080–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morozova O, Levina O, Uusküla A, Heimer R. Comparison of subset selection methods in linear regression in the context of health-related quality of life and substance abuse in Russia. BMC Med Res Methodol 2015;15(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mu W, Muriello M, Clemens JL, et al. Factors affecting quality of life in children and adolescents with hypermobile Ehlers‐Danlos syndrome/hypermobility spectrum disorders. American Journal of Medical Genetics Part A 2019;179(4):561–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pedregosa F, Varoquaux G, Gramfort A, et al. Scikit-learn: Machine learning in Python. The Journal of Machine Learning research 2011;12:2825–2830. [Google Scholar]
- 7.Abdel Majeed Y, Awadalla SS, Patton JL. Regression techniques employing feature selection to predict clinical outcomes in stroke. PLoS One 2018;13(10):e0205639. doi: 10.1371/journal.pone.0205639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mongelli MN, Giri S, Peipert BJ, Helenowski IB, Yount SE, Sturgeon C. Financial burden and quality of life among thyroid cancer survivors. Surgery 2020;167(3):631–637. [DOI] [PubMed] [Google Scholar]


