Abstract
Background/purpose
Implant assisted removable partial dentures (IARPDs) improved biomechanical behavior of removable partial dentures (RPDs), but information of the effect of attachment type and implant position is limited. This study aimed to investigate the effect of implant position and attachment type on the stress distribution of IARPDs.
Material and methods
Four implants, 10 mm in length and 4.1 mm in diameter, were bilaterally placed close to first premolar and second molar regions of a mandibular Kennedy class I model having artificial dentition from canine to canine, vertical to the occlusal plane. Five IARPDs were fabricated to accommodate locator and magnetic attachments. Strain gauges were placed on the model surface to measure the strain around implants during loading. Unilateral vertical loading was applied to the right first molar area with magnitude of 120 N and crosshead speed of 10 mm/min. Measurements were recorded under following conditions: premolar IARPDs with locator or magnetic attachments, molar IARPDs with locator or magnetic attachments. Two-way multiple analysis of variance was performed to compare the maximum principal strain (MPS) around the implants with a significance level of 0.05.
Results
Implant position had significant effect on the MPS of IARPD on loading and nonloading sides while attachment type only significant on nonloading side. Molar implants showed larger MPS than premolar implants with both locator and magnetic attachments during unilateral loading.
Conclusion
The stress distribution of the IARPD is significantly affected by implant position wherein anteriorly placed implants exhibit lower MPS than relatively posteriorly placed implants.
Keywords: Dental attachments, Implant-assisted removable partial denture, Implant position, Stress distribution, Strain gauge
Introduction
Implant-assisted removable partial dentures (IARPDs), which can convert a Kennedy class I or II partially edentulous arch to a Kennedy class III rehabilitation, have become a well-known treatment option in recent years.1, 2, 3, 4 The vertical and lateral displacement of the IARPD is limited, resulting in a reduction in bone resorption under the distal free-end denture base. However, the location of the implant along the distal edentulous residual ridge has been controversial in both clinical and in vitro studies, as this location may play a crucial role in the stress distribution of IARDPs and influence the clinical outcomes of treatment modality.5, 6, 7
IARPDs are connected to supporting implants via attachment systems. Splinted attachments (for example, bar attachments) and nonsplinted (stud) attachments (for example, balls, locators) and magnetic attachments, with different biomechanical characteristics are commonly used. The incorporation of different attachments may also improve denture retention and quality of stress distribution, and enhance esthetics by avoiding buccal retentive clasps.8 In the past decade, the resiliency of stud attachments has greatly improved, resulting in less strain on implants.9,10 Locator attachments are available in several vertical heights and possess numerous advantages such as resilience, retention, durability, easy replacement, and angulation compensation.11, 12, 13, 14 Magnetic attachments have been used as retention systems for both natural teeth and dental implants for many years15,16 as they may reduce lateral forces, which have a negative effect on the supporting teeth or implants.17,18
Several in vitro studies have investigated the stress distribution of IARPDs in terms of implant size, denture supporting area, mucosal thickness, and loading conditions. Model studies by Ohkubo et al.6 and Sato et al.19 showed that implant placement in the distal edentulous ridge (molar area) prevents displacement of the IARPD. Placing the implant at the first molar region improves the biomechanical behavior of the IARPD and reduces the stress exerted on the soft tissue under the distal extension of the IARPD.7,8 Despite the advantages of distal implant placement, in some clinical cases, implants are placed in the premolar region because of the inadequate volume of the alveolar ridge. In addition, a model study by Matsudate et al.,20 reported that the placement of a supporting implant near the abutment tooth (premolar area) prevented vertical movement of the denture and transferred less force to the abutment tooth. Therefore, placing an implant along the distal alveolar ridge has several advantages in terms of the stress distribution of IARPDs, regardless of implant position. Previous studies have evaluated the stress around the implant and abutment teeth with IARPD.2,3,20 However, the effect of different types of attachment on the stress distribution of IARPD supported by different implant locations was not investigated. Therefore, this in vitro study investigated the effect of attachment type and the association between implant location and attachment type on the stress distribution of IARPDs.
The application of measuring devices in in vivo experimental studies on IARPD load distribution is difficult because of ethical issues, lack of compatible equipment, and the complexities of oral function.20 Therefore, in vitro analysis of load distribution to implants and surrounding structures using finite element analysis (FEA) or strain gauges on an experimental model has become a widely accepted option. The results yielded by these two approaches have been shown to be highly correlated. Although several differences exist between FEA and strain gauges, these two methods have mutual agreement and compatibility in determining the quality of induced strains under the applied load.21
The aim of this study was to investigate the effect of implant position and type of attachment system on the stress distribution of IARPDs by using strain gauges. The null hypothesis was that the IARPD stress distribution was not influenced by implant position and type of attachment system.
Materials and methods
Fabrication of testing model and IARPDs
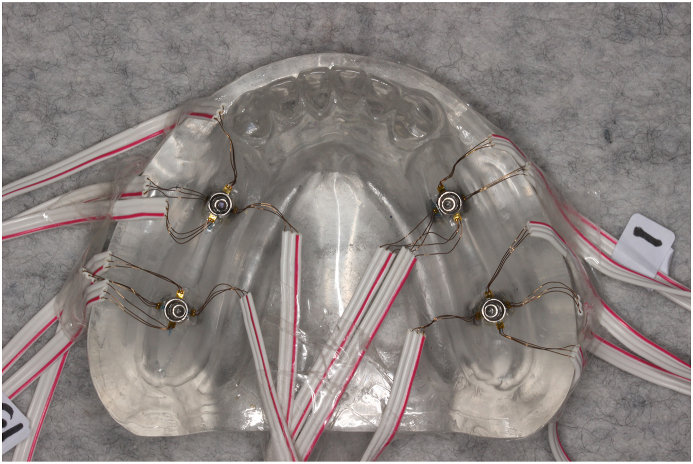
This in vitro study was performed on a mandibular bilateral distal extension model (Kennedy class I) with artificial dentition from canine to canine. The model was constructed with heat-polymerized acrylic resin (Acron, GC, Tokyo, Japan) using a commercially available partially edentulous model (Nissin E1-550; Nissin Dental Products, Kyoto, Japan). A uniform 2-mm thickness of resin was removed from distal edentulous ridge area of the model and replaced with silicone impression material (Exahiflex; GC) to simulate the ridge mucosa. Four implants of length 10 mm and diameter 4.1 mm (BL Tapered SLA, Straumann, Basel, Switzerland) were placed, one each close to the first premolar and second molar regions on both sides of the model, perpendicular to the occlusal plane (Fig. 1a). The implants were retained using rapid self-polymerizing acrylic resin (Unifast III Trad: GC). Five conventional cobalt-chrome RPDs with the same design (a lingual bar along with occlusal rests and wire clasps on the canines) were fabricated to accommodate two different types of attachments, namely locator attachments (blue; Zest Anchors, Carlsbad, CA, USA; Fig. 1b) and magnetic attachments (IFD30BR 1911102; Aichi Steel, Aichi, Japan; Fig. 1c). The matrices, metal housings for the locator attachments and magnets for magnetic attachments, were retained in the dentures using rapid self-polymerizing acrylic resin (Unifast III Trad: GC). An acrylic occlusal rim was then constructed and attached to the metal framework using heat-polymerized acrylic resin (Acron, GC) according to the manufacturer's instructions.
Figure 1.
(a) Experimental model with implants. (b) IARPD with locator attachment. (c) IARPD with magnetic attachment. IARPD, implant-assisted removable partial denture.
Strain gauge attachment and measurement of the strain applied to the implant
Uniaxial strain gauges were used in this study. The acrylic surfaces around each implant were flattened and smoothed with fine sandpaper and wipe with alcohol pad for strain gauge bonding. The fine lead wires of the strain gauges (KFRS-02-120-C1-13L3M3R; Kyowa Electronic Instruments, Tokyo, Japan) were then attached to the flattened and smoothed surface of the experimental model using a strain gauge instantaneous adhesive (CC-33A; Kyowa Electronic Instruments). These wires were placed at the mesial, distal, buccal, and lingual sides of each implant (Fig. 2) and were used to measure the maximum principal strain (MPS) around the implants during loading. The other end of each strain gauge was connected to the sensor interface board (PCD 300A; Kyowa Electronic Instruments), which converted the electrosignals to microstrain by using software (DAS 200A, ver. 2.22, Kyowa Electronic Instruments). Before the strain gauge measurement, a cyclic load ranging from 10 N to 60 N was applied five times on the occlusal surface of the dentures, to age the strain gauges to prevent hysteresis, which is lagging or retardation of the electric signal when forces acting upon the denture are changed.22 A vertical load of 120 N was applied using a universal testing machine (Instron 5544; Instron, Tokyo, Japan) at a crosshead speed of 10 mm/min (Fig. 3). The 120 N load represents the standard bite force of a patient with an IARPD3,23 and the load that the resin model could withstand without deformation. The central region of the right first molar was selected as the loading point and notched with a diamond bur to prevent slipping of the loading pin. The IARPD (n = 5) stress distribution was measured five times under each of the following conditions, with a 5-min recovery time for heat dissipation:
-
a)
Premolar IARPD with locator attachment.
-
b)
Molar IARPD with locator attachment.
-
c)
Premolar IARPD with magnetic attachment; and
-
d)
Molar IAPRD with magnetic attachment.
Figure 2.
Strain gauges attached to mesial, buccal, distal, and lingual sides of implants.
Figure 3.

Vertical loading of experimental model with universal testing machine.
The unused implants were made inactive by eliminating contact with the impression surface of the denture.20
Statistical analysis
Statistical analysis was performed using IBM SPSS software (version 25.0; IBM Corp., Armonk, NY, USA) and significance level of 0.05. Two-way multiple analysis of variance (MANOVA) was performed to compare the strain around the implants on the loading and nonloading sides under different experimental conditions.
Results
Table 1 shows the results of the two-way MANOVA for the effect of independent variables (implant position and attachment type) on dependent variables (strain on the loading and nonloading sides). Statistically significant differences were found in the effects of implant position (P < 0.001), attachment type (P = 0.002), and the interaction between implant position and attachment type on the dependent variables (P < 0.001). The statistical significance in the interaction indicated that the influence of the attachment type on strain was not the same for premolar and molar implant positions.
Table 1.
Results of two-way multiple analysis of variance (Wilk's Lambda Test) for implant position, attachment type, and interaction of implant position and attachment type at a significance level of 0.05.
| Effect | Value | F | Hypothesis df | Error df | P value |
|---|---|---|---|---|---|
| Implant position | 0.607 | 127.847 | 2.000 | 395.000 | <0.001 |
| Attachment type | 0.969 | 6.222 | 2.000 | 395.000 | 0.002 |
| Implant positiona Attachment type | 0.761 | 62.053 | 2.000 | 395.000 | <0.001 |
df = degrees of freedom.
Interaction between implant position and attachment type.
Fig. 4 shows the mean strain and standard error (SE) on the loading side in unilateral loading under different experimental conditions. On the loading side, the stress distribution of the IARPD was significantly influenced by implant position (P < 0.001; Table 2), but not by attachment type (P = 0.089; Table 2). The largest strain was observed in the molar IARPD with the magnetic attachment (236.15με, SE = 9.14) followed by the molar IARPD with the locator attachment (145.07με, SE = 9.14), premolar IARPD with the locator attachment (107.07με, SE = 9.14) and, finally, premolar IARPD with the magnetic attachment (47.2με, SE = 9.14). However, the MPS for the molar IARPDs on the nonloading side (Fig. 5) was significantly smaller than that for premolar IAPRDs with both locator and magnetic attachments. On the nonloading side, the stress distribution of the IARPD was significantly influenced by implant position (P < 0.001; Table 2) and attachment type (P = 0.001; Table 2). The smallest strain on the nonloading side was found in the molar IARPD with the locator attachment (4.15με, SE = 2.94), which recorded the second largest strain on the loading side. The largest strain on the nonloading side was recorded in the premolar IARPD with locator attachment (57.01με, SE = 2.94) followed by the premolar IARPD with magnetic attachment (28.15με, SE = 2.94) and the molar IARPD with magnetic attachment (13.8με, SE = 2.94). The influence of the interaction of implant position and attachment type was statistically significant on the loading (P < 0.001; Table 2) and nonloading sides (P < 0.001; Table 2) in unilateral loading, as analyzed by two-way MANOVA. This indicated that the MPS of the IARPD was significantly influenced by attachment type supported by different implant positions on both the loading and nonloading sides in unilateral loading.
Figure 4.
Mean strain and standard error (SE) on loading side under unilateral loading, with significance level of 0.05.
Table 2.
Results of two-way multiple analysis of variance (tests of between-subjects effects) for implant position, attachment type, and interaction of implant position and attachment type at a significance level of 0.05.
| Source | Dependent Variable | F | P value |
|---|---|---|---|
| Implant position | LS | 154.167 | <0.001 |
| NLS | 130.323 | <0.001 | |
| Attachment type | LS | 2.912 | 0.089 |
| NLS | 10.639 | 0.001 | |
| Implant positiona Attachment type | LS | 68.199 | <0.001 |
| NLS | 42.791 | <0.001 |
LS = loading side, NLS = nonloading side.
Interaction between implant position and attachment type.
Figure 5.
Mean strain and standard error (SE) on nonloading side under unilateral loading, with significance level of 0.05.
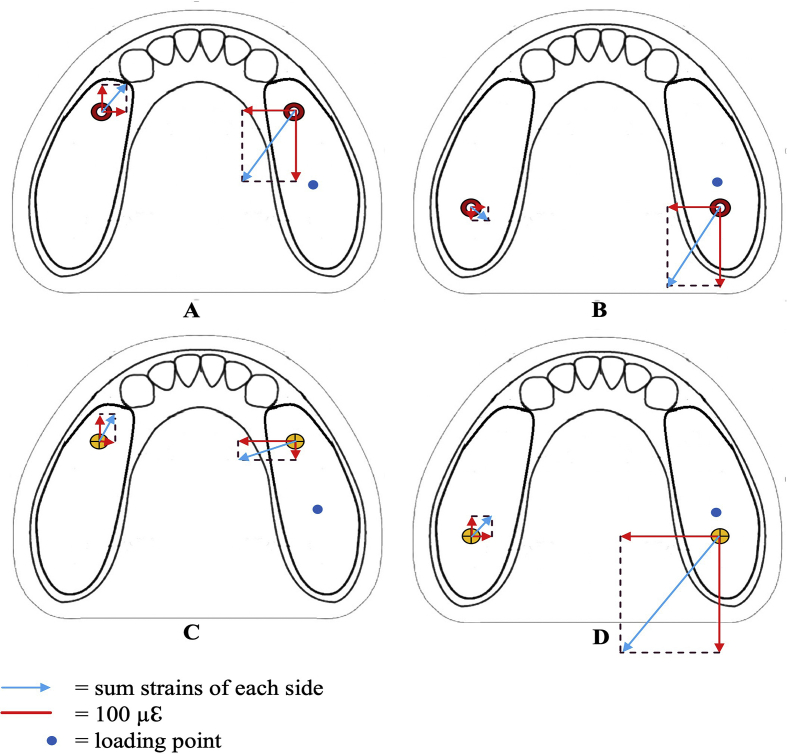
Fig. 6 shows the magnitude and direction of the MPS under different experimental conditions; the MPS was distolingually distributed on the loading side under all experimental conditions. In contrast, the MPS distribution on the nonloading side was slightly different for each experimental condition. The data shown in Fig. 6 were not statistically analyzed. On the nonloading side, the MPS distribution of the molar IARPD with the locator attachment (Fig. 6B) was in the distolingual direction, whereas the MPS distributions of the other experimental conditions (Fig. 6A, C, D) were mesiolingually distributed. In the premolar IARPD (Fig. 6A, C), the MPS of the locator attachment was greater than that of the magnetic attachment on the loading side. This indicated that the MPS was concentrated on the loading side in the locator attachment, whereas the magnetic attachment could distribute the MPS to the loading and nonloading sides. Nevertheless, in molar IARPDs (Fig. 6B, D), the MPS of the magnetic attachment was larger than that of the locator attachment on the loading side, and slight differences existed in the MPS on the nonloading side.
Figure 6.
Magnitude and direction of MPS in each experimental condition. (A) Premolar IARPD with locator attachment. (B) Molar IARPD with locator attachment. (C) Premolar IARPD with magnetic attachment. (D) Molar IARPD with magnetic attachment. IARPD, implant-assisted removable partial denture; MPS, maximum principal strain.
Discussion
The optimal implant position and attachment system for IARPDs with distal extensions remain unknown.1 In this study, the implant position, attachment type, and their interrelationship were investigated. The results showed that the attachment type did not have a significant effect on the MPS of IARPD on the loading side. However, implant position and the interaction between the implant position and attachment type had a significant effect on IARPD stress distribution. Therefore, the null hypothesis that IARPD stress distribution was not influenced by implant position and attachment system type was rejected.
Previous in vitro studies with Kennedy class I and II conditions have indicated that a posteriorly placed implant reduces the pressure on the alveolar ridge and restricts denture movement more than an implant positioned anteriorly.7,8,24,25 However, in some cases, implants need to be placed anteriorly in the distal edentulous ridge near the terminal abutment tooth because of severe atrophy of the posterior residual ridge. Therefore, studies on the stress distribution of IARPDs with anteriorly placed implants are necessary. Moreover, selection of the attachment system, which provides retention and stability to the denture, should be considered an important factor for treatment success.26,27
While the optimal forces transmitted to the implant and surrounding tissues are not yet well defined, the minimization of these forces is important to prevent implant failure. In the present in vitro study, vertical loading tests were performed under a 120 N load applied at the first molar region, where maximum bite forces are often exerted.23,28,29 The molar IARPD showed a larger MPS around the implant than the premolar IARPD with both locator and magnetic attachments on the loading side. In the molar IARPD, the MPS was mainly concentrated on the implant and surrounding tissues of the loading side, which may have caused excessive loading on one side of the ridge. In contrast, the MPS was also distributed to the nonloading side in premolar IARPDs with both locator and magnetic attachments. This result is similar to that of Matsudate et al.,20 who demonstrated that a mesially placed implant generates a smaller MPS around the implant. The distance between the implant and abutment tooth may influence this result. Implant placement closer to the abutment tooth can decrease the stress applied to the peri-implant tissue, as the abutment tooth and implant can share the loading force and distribute it to the surrounding tissues of the implant.28 Nevertheless, in premolar IARPDs, the implant acts as a fulcrum upon which the denture base rotates, thus generating a lateral force on the abutment tooth and implant. Consequently, microfracture of the peri-implant bone tissue and implant failure may occur.20 Therefore, attention should be given to the condition of the abutment teeth and surrounding tissues when placing implants on the distal part of the alveolar ridge in the unilateral loading condition.
Although the influence of the type of attachment system was not statistically significant on the loading side, a significant difference was found on the nonloading side. Locator and magnetic attachments, regarded as typical attachments for IARPDs, were used in the present study. Compared with the magnetic attachment, the locator attachment showed a smaller MPS around the implant on the loading side, with lesser MPS transferred to the nonloading side in the molar IARPDs. This could be due to the structural property of the locator attachment, as it contains a resilient nylon insert that can absorb the strain from the loading, thus improving the stress distribution to the peri-implant area.17,30 In contrast, the magnetic attachment has direct contact with the keeper without any intervening space, and this may be responsible for the distribution of MPS to the peri-implant area,31 particularly under unilateral vertical loading. Due to its flat and simple configuration, the magnetic attachment showed a more even stress distribution than the locator attachment in the premolar IARPD. According to Gillings and Samant,15 most magnetic attachment systems have a self-limiting potential, as they detach from the abutment when subjected to an excessive lateral force.
Strain gauges were used in this in vitro study because they provide a quantitative analysis of the strain around the implants. This technique is one of the most common methods for strain analysis in dental research, as it has advantages over other methods.32, 33, 34 In the present study, the strain gauges were attached to the mesial, buccal, distal, and lingual sides of the implant to provide an accurate and definitive measurement of a wide area around the implant and monitor the impact of the load to the peri-implant area.35 The results of this study provide supportive evidence for the use of IARPDs in mandibular Kennedy class I cases. Selection of the attachment system, as well as considering its interaction with the implant position, can provide a basis for better stress distribution with IARPDs under unilateral vertical loading.
Although the experimental model simulated clinical conditions, the results of this study may not accurately reflect values obtained in vivo. First, strain gauges could only measure surface strain at specific points and in predetermined directions. Second, implant osseointegration and the biomechanical condition of the abutment teeth were not considered. Finally, this study only assessed the strain of unilateral loading on a single IARPD and Kennedy class I model. Oblique loading, off-axis loading, and different loading points were not investigated. Therefore, additional in vitro investigations of IARPDs on models with different missing teeth, as well as clinical trials conducted among patients, are warranted.
Author contribution statement
Sai Tun Naing∗: Conceptualization, Methodology, Formal analysis, Investigation, Data Curation, Writing-Original Draft; Manabu Kanazawa∗: Conceptualization, Methodology, Funding-acquisition, Resources, Writing-Review & Editing, Supervision; Tamaki Hada: Investigation, Data curation, Review & Editing; Maiko Iwaki: Data curation, Resources; Yuriko Komagamine: Data curation, Review & Editing; Anna Miyayasu: Data curation; Yoko Uehara: Data curation; Shunsuke Minakuchi: Conceptualization, Funding support, Resources.
The corresponding author, Manabu Kanazawa, declares that all authors contributed to the conduct of this research and the writing of the manuscript.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
The authors would like to acknowledge Aichi Steel Company, Aichi, Japan for providing the magnetic attachments that were used in this study.
References
- 1.de Freitas R.F.C.P., de Carvalho Dias K., da Fonte Porto Carreiro A., Barbosa G.A.S., Ferreira M.A.F. Mandibular implant-supported removable partial denture with distal extension: a systematic review. J Oral Rehabil. 2012;39:791–798. doi: 10.1111/j.1365-2842.2012.02326.x. [DOI] [PubMed] [Google Scholar]
- 2.Kono K., Kurihara D., Suzuki Y., Ohkubo C. Pressure distribution of implant-supported removable partial dentures with stress-breaking attachments. J Prosthodont Res. 2014;58:115–120. doi: 10.1016/j.jpor.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Shahmiri R., Aarts J.M., Bennani V., Das R., Swain M.V. Strain distribution in a Kennedy class I implant assisted removable partial denture under various loading conditions. Int J Dent. 2013;2013:351279. doi: 10.1155/2013/351279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zancopé K., Abrão G.M., Karam F.K., Neves F.D. Placement of a distal implant to convert a mandibular removable Kennedy class I to an implant-supported partial removable Class III dental prosthesis: a systematic review. J Prosthet Dent. 2015;113:528–533. doi: 10.1016/j.prosdent.2014.12.011. e3. [DOI] [PubMed] [Google Scholar]
- 5.Grossmann Y., Nissan J., Levin L. Clinical effectiveness of implant-supported removable partial dentures: a review of the literature and retrospective case evaluation. J Oral Maxillofac Surg. 2009;67:1941–1946. doi: 10.1016/j.joms.2009.04.081. [DOI] [PubMed] [Google Scholar]
- 6.Ohkubo C., Kobayashi M., Suzuki Y., Hosoi T. Effect of implant support on distal-extension removable partial dentures: in vitro assessment. J Oral Rehabil. 2007;23:1095–1101. doi: 10.1111/j.1365-2842.2006.01641.x. [DOI] [PubMed] [Google Scholar]
- 7.Ortiz-Puigpelat O., Lázaro-Abdulkarim A., de Medrano-Reñé J.M., Gargallo-Albiol J., Cabratosa-Termes J., Hernández-Alfaro F. Influence of implant position in implant-assisted removable partial denture: a three-dimensional finite element analysis. J Prosthodont. 2019;28:e675–e681. doi: 10.1111/jopr.12722. [DOI] [PubMed] [Google Scholar]
- 8.Memari Y., Geramy A., Fayaz A., Rezvani H.A.S., Mansouri Y. Influence of implant position on stress distribution in implant-assisted distal extension removable partial dentures: a 3D finite element analysis. J Dent. 2014;11:523–530. [PMC free article] [PubMed] [Google Scholar]
- 9.Cakarer S., Can T., Yaltirik M., Keskin C. Complications associated with the ball, bar and Locator attachments for implant-supported overdentures. Med Oral Patol Oral Cir Bucal. 2011;16:e953–e959. doi: 10.4317/medoral.17312. [DOI] [PubMed] [Google Scholar]
- 10.Takahashi T., Gonda T., Maeda Y. Effect of attachment type on implant strain in maxillary implant overdentures: comparison of ball, locator, and magnet attachments. Part 1. Overdenture with palate. Int J Oral Maxillofac Implants. 2017;32:1308–1314. doi: 10.11607/jomi.5737. [DOI] [PubMed] [Google Scholar]
- 11.Chikunov I., Doan P., Vahidi F. Implant-retained partial overdenture with resilient attachments. J Prosthodont. 2008;17:141–148. doi: 10.1111/j.1532-849X.2007.00261.x. [DOI] [PubMed] [Google Scholar]
- 12.Chung K.H., Chung C.Y., Cagna D.R., Cronin R.J. Retention characteristics of attachment systems for implant overdentures. J Prosthodont. 2004;13:221–226. doi: 10.1111/j.1532-849X.2004.04042.x. [DOI] [PubMed] [Google Scholar]
- 13.Kleis W.K., Kämmerer P.W., Hartmann S., Al-Nawas B., Wagner W.A. A comparison of three different attachment systems for mandibular two-implant overdentures: one-year report. Clin Implant Dent Relat Res. 2010;12:209–218. doi: 10.1111/j.1708-8208.2009.00154.x. [DOI] [PubMed] [Google Scholar]
- 14.Trakas T., Michalakis K., Kang K., Hirayama H. Attachment systems for implant retained overdentures: a literature review. Implant Dent. 2006;15:24–34. doi: 10.1097/01.id.0000202419.21665.36. [DOI] [PubMed] [Google Scholar]
- 15.Gillings B.R., Samant A. Overdentures with magnetic attachments. Dent Clin. 1990;34:683–709. [PubMed] [Google Scholar]
- 16.Jackson T.R. New rare earth magnetic technology: the Jackson solid state attachment system. Trends Tech Contemp Dent Lab. 1986;3:31–39. [PubMed] [Google Scholar]
- 17.Omar A., Omran M., Fouad M.M., Elsyad M.A. Effect of different attachments designs used for implant assisted mandibular distal extension RPD. An in vitro study of stresses transmitted to abutment teeth. Mansoura J Dent. 2014;1:56–62. [Google Scholar]
- 18.Tokuhisa M., Matsushita Y., Koyano K. In vitro study of a mandibular implant overdenture retained with ball, magnet, or bar attachments: comparison of load transfer and denture stability. Int J Prosthodont. 2003;16:128–134. [PubMed] [Google Scholar]
- 19.Sato M., Suzuki Y., Kurihara D., Shimpo H., Ohkubo C. Effect of implant support on mandibular distal extension removable partial dentures: relationship between denture supporting area and stress distribution. J Prosthodont Res. 2013;57:109–112. doi: 10.1016/j.jpor.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Matsudate Y., Yoda N., Nanba M., Ogawa T., Sasaki K. Load distribution on abutment tooth, implant and residual ridge with distal-extension implant-supported removable partial denture. J Prosthodont Res. 2016;60:282–288. doi: 10.1016/j.jpor.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 21.Akça K., Cehreli M.C., Iplikçioglu H. A comparison of three-dimensional finite element stress analysis with in vitro strain gauge measurements on dental implants. Int J Prosthodont. 2002;15:115–121. [PubMed] [Google Scholar]
- 22.Elsyad M.A., Elhddad A.A., Khirallah A.S. The effect of implant diameter on strain around implants retaining a mandibular overdenture with Locator attachments: an in vitro study. Dent Mater J. 2016;35:938–945. doi: 10.4012/dmj.2016-181. [DOI] [PubMed] [Google Scholar]
- 23.Miyaura K., Morita M., Matsuka Y., Yamashita A., Watanabe T. Rehabilitation of biting abilities in patients with different types of dental prostheses. J Oral Rehabil. 2000;27:1073–1076. doi: 10.1046/j.1365-2842.2000.00620.x. [DOI] [PubMed] [Google Scholar]
- 24.Cunha L.D.A.P., Pellizzer E.P., Verri F.R., Pereira J.A. Evaluation of the influence of location of osseointegrated implants associated with mandibular removable partial dentures. Implant Dent. 2008;17:278–287. doi: 10.1097/ID.0b013e31818363b2. [DOI] [PubMed] [Google Scholar]
- 25.Oh W.S., Oh T.J., Park J.M. Impact of implant support on mandibular free-end base removable partial denture: theoretical study. Clin Oral Implants Res. 2016;27:e87–e90. doi: 10.1111/clr.12534. [DOI] [PubMed] [Google Scholar]
- 26.Kanazawa M., Minakuchi S., Hayakawa I., Hirano S., Uchida T. In vitro study of reduction of stress transferred onto tissues around implants using a resilient material in maxillary implant overdentures. J Med Dent Sci. 2007;54:17–23. [PubMed] [Google Scholar]
- 27.Pellizzer E.P., Verri F.R., Falcón-Antenucci R.M., Goiato M.C., Gennari Filho H. Evaluation of different retention systems on a distal extension removable partial denture associated with an osseointegrated implant. J Craniofac Surg. 2010;21:727–734. doi: 10.1097/SCS.0b013e3181d8098a. [DOI] [PubMed] [Google Scholar]
- 28.Hegazy S.A.F., Elshahawi I.M., Elmotayam H. Stresses induced by mesially and distally placed implants to retain a mandibular distal-extension removable partial overdenture: a comparative study. Int J Oral Maxillofac Implants. 2013;28:403–407. doi: 10.11607/jomi.2155. [DOI] [PubMed] [Google Scholar]
- 29.Sadowsky S.J., Caputo A.A. Stress transfer of four mandibular implant overdenture cantilever designs. J Prosthet Dent. 2004;92:328–336. doi: 10.1016/j.prosdent.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen C.T., Masri R., Driscoll C.F., Romberg E. The effect of denture cleansing solutions on the retention of pink Locator attachments: an in vitro study. J Prosthodont. 2010;19:226–230. doi: 10.1111/j.1532-849X.2009.00550.x. [DOI] [PubMed] [Google Scholar]
- 31.Takeshita S., Kanazawa M., Minakuchi S. Stress analysis of mandibular two-implant overdenture with different attachment systems. Dent Mater J. 2011;30:928–934. doi: 10.4012/dmj.2011-134. [DOI] [PubMed] [Google Scholar]
- 32.Cehreli M.C., Iplikçioglu H. In vitro strain gauge analysis of axial and off-axial loading on implant supported fixed partial dentures. Implant Dent. 2002;11:286–292. [PubMed] [Google Scholar]
- 33.el Charkawi H.G., Zekry K.A., el Wakad M.T. Stress analysis of different osseointegrated implants supporting a distal extension prosthesis. J Prosthet Dent. 1994;72:614–622. doi: 10.1016/0022-3913(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 34.Rodrigues R.C.S., Faria A.C.L., Macedo A.P., de Mattos M.G.C., Ribeiro R.F. Retention and stress distribution in distal extension removable partial dentures with and without implant association. J Prosthodont Res. 2013;57:24–29. doi: 10.1016/j.jpor.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Elsyad M.A., Omran A.O., Fouad M.M. Strains around abutment teeth with different attachments used for implant-assisted distal extension partial overdentures: an in vitro study. J Prosthodont. 2017;26:42–47. doi: 10.1111/jopr.12370. [DOI] [PubMed] [Google Scholar]