Abstract
Background/purpose
The narrow alveolar ridge in the maxillary premolars area limits the angle of implant placement and the shape of the prosthesis. The aim of this study was to evaluate which implant prosthesis, screw-and-cement-retained prosthesis (SCRP) or cement-retained prosthesis (CRP), was more suitable for the maxillary premolar area.
Materials and methods
We conducted virtual implantation on 58 implant images from 47 patients obtained using cone beam computed tomography (CBCT). The width and buccal inclination of the alveolar bone, the angulation of the implant fixture, and the angulation of abutment were measured and calculated.
Results
We determined that SCRP was feasible in 52% and 78.8% of first and second premolar areas, respectively. There was a positive relationship between the feasibility of SCRP and the premolar region in general (P = 0.031), although SCRP was more likely to be a possibility in the second premolar area. On multiple logistic regression analysis, the difference in the angle between the axis of the prosthesis and the axis of the alveolar bone (RA) was significantly associated with the type of prosthesis (P = 0.001). The RA was significantly higher for CRP implants (OR = 1.885; 95% CI: 1.31 to 2.70).
Conclusion
SCRP is not always feasible in the maxillary premolar area, especially in the first premolar area. If the difference between the angle of the axis of the prosthesis and the axis of the alveolar bone is large, it may be necessary for the clinician to consider CRP in the treatment planning stage.
Keywords: Dental implant, Screw-and-cement-retained prosthesis, Upper premolar
Introduction
The types of implant prostheses currently used in clinical practice include the screw-retained prosthesis (SRP), cement-retained prosthesis (CRP), and screw-and-cement-retained prosthesis (SCRP). The SCRP is preferred by clinicians because of its ease of retrievability, passive fit, complete removal of excess cement, and uncomplicated maintenance and management.1, 2, 3 However, SCRP has an aesthetic and prosthetic disadvantage because of the screw access hole (SAH) at the crown surface.3 When the implant fixture cannot be placed in the ideal position for SCRP due to certain anatomical limitations or practitioner inexperience, the SAH invades the buccal or palatal/lingual cusps, resulting in aesthetic and functional disadvantages.4 Many authors report that the presence of SAH at the occlusal surface of the crown could weaken the porcelain superstructure, resulting in decreased porcelain fracture strength.5, 6, 7, 8 Furthermore, if the SAH is not located in the center of the occlusal plane, it results in cantilevering, and screw loosening is more likely.9 Therefore, it is recommended that the SAH be located at the cingulum for anterior teeth and at the occlusal central fossa of the crown for posterior teeth, whenever possible.9,10
In order for the SAH not to deviate significantly from the cingulum or the fossa, the angle between the crown and the fixture should be straight; if it cannot be straight, the angulation should be as small as possible. If the position and angulation of the implant are inappropriate, the angulation of abutment increases; this, in turn, fails to satisfy cusp-fossa contact and increases stress on the implants and adjacent bone.11 If the angulation of abutment exceeds the acceptable range for SCRP, practitioners should instead select CRP.2 Ultimately, a clinician can achieve successful rehabilitation only by considering the position and angle of the implant fixture and the shape of the prosthesis at the same time during the planning phase.
The fixture should be placed perpendicular to the occlusal surface for straight abutment and for ideal SAH orientation; this can be challenging in the premolar area. First, the narrowness of the alveolar ridge in the area of the maxillary premolars makes it difficult to determine the bucco-palatal position of the implant fixture.12, 13, 14 In addition, the alveolar ridge in the maxillary premolar area has a large buccal inclination that could restrict the angle of the implant fixture.15 If the position and angle of the implant fixture does not take into consideration the alveolar bone morphology and inclination, fenestration and dehiscence could occur.16 Considering these anatomic limitations of the maxillary premolar area, it is questionable whether it is possible to use the SCRP and satisfy both the ideal angle and position of the implant fixture and the inclination of the alveolar ridge in the upper premolar area.
The purpose of this study was to evaluate whether SCRP or CRP was more suitable in the maxillary premolar area considering the angulation of abutment, the angulation of the implant fixture, and the alveolar bone morphology. Additionally, we attempted to investigate the anatomic factors that influenced mostly the type of prosthesis used in the premolar region.
Material and methods
Patient selection
The population of this retrospective cohort study comprised all patients who underwent implant therapy for oral rehabilitation between January 2016 and December 2019 at the Department of Oral and Maxillofacial Surgery, Seoul Metropolitan Government-Seoul National University (SMG-SNU) Boramae Medical Center in Seoul, Korea. Ethical approval was obtained from the institutional review board of the SMG-SNU Boramae Medical Center, Seoul (IRB No. 26-2017-51). The study was conducted in accordance with the declaration of Helsinki. The waiver was granted because the study was a retrospective chart review, not an interventional study, and because it was difficult to obtain consent from patients who had been treated several years prior.
The inclusion criteria were simple implant, placement in the upper first and second premolar areas and treated the final prosthesis. The exclusion criteria were ridge augmentation, ridge splitting and immediate implantation.
CBCT image acquisition and reconstruction
The CBCT images (Dinnova 3, HDX Corp., Seoul, Korea) were obtained using a scan time of 7 s at 95 kV and 9 mA, a voxel size of 0.3 mm, and a 9-mm field of view. All images were saved in Digital Imaging and Communication in Medicine (DICOM) format and reconstructed using INFINITT Picture Archiving and Communication System (INFINITT Healthcare, Seoul, Korea) at 0.5-mm thickness. All included patients had completed prosthetic treatment, and the shape of the prosthesis could be confirmed in a state of occlusion with the opposite teeth on postoperative CBCT images. All images were reoriented so that the maxilla was symmetric bilaterally and so that the coronal plane, defined as the line connecting the center of the platform part of the implant fixture and the central fossa of the prosthesis, was perpendicular to the ground (Fig. 1).
Figure 1.
Alveolar width measurements. Line ‘R’ is the long axis of the alveolar ridge, indicating the buccal inclination. Line ‘O’ is the occlusal plane. Line ‘A’ is the abutment axis connecting the central fossa and the center of the crestal part of the implant fixture. The alveolar width was measured at 3 points: coronal (CW), middle (MW) and apical (AW). The abbreviations RO, AO, and RA represent, respectively, the buccal inclination of the ridge from the occlusal plane, angulation of line ‘A’ from the occlusal plane, and angulation between line ‘R’ and ‘A’.
Measurement of the alveolar ridge and reference lines
To define the ridge morphology, the alveolar bone width was measured on CBCT images (Fig. 1). The alveolar height was divided into thirds, at intervals of 5 mm. At each point, the bucco-palatal width of the alveolar bone was measured perpendicular to the long axis of the alveolar bone (line ‘R’); the 3 measurements were the coronal width (CW), middle width (MW), and apical width (AW). Line ‘A’ represented the abutment axis connecting the central fossa and the center of the crestal part of the implant fixture. This line represented the angle of the ideal prosthesis and served as a reference line when measuring the angle of the virtual abutments and fixtures. In addition, buccal inclination of the ridge from the occlusal plane (RO), angulation of line ‘A’ from the occlusal plane (AO), and angulation between line ‘R’ and line ‘A’ (RA) were measured.
Virtual implantation and measurement of fixture angulation
For the purposes of virtual implantation, we used the specifications of the TS III 4010 implant (Osstem Implant, Seoul, Korea), which has a length of 10 mm and a diameter of 4.2 mm on the coronal aspect and 2.8 mm on the apical aspect. The shape and position of the prosthesis were used as they were confirmed on postoperative CT images, and the virtual implant fixture was newly placed according to the position of the abutment of the prosthesis (Fig. 2). The platform part of the implant was fixed as the rotation axis, and the apical part was allowed to move within a range that did not invade the cortical plate at the middle or apical third of the alveolar bone. The safety area was set at a distance 1 mm from the cortical bone. In this area, the virtual implant was installed and the buccal (BAF) and palatal angulations (PAF) of the fixture from line ‘A’ were measured.
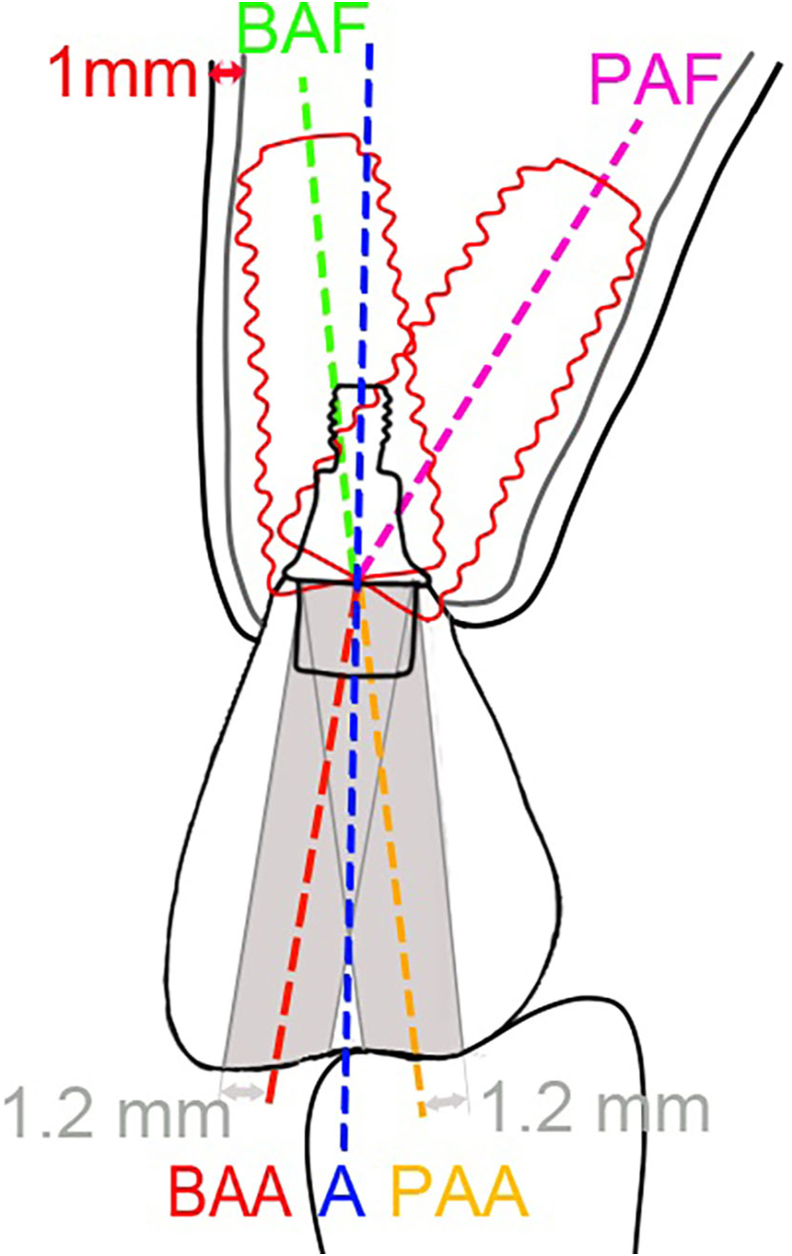
Figure 2.
Measurements related to the angulation of abutment and the angulation of fixture. The blue dotted line ‘A’ is the abutment axis connecting the central fossa and the center of the crestal part of the implant fixture. The green dotted line represents the buccal angulation of the fixture (BAF). The pink dotted line represents the palatal angulation of the fixture (PAF). The yellow dotted line represents the palatal angulation of the abutment (PAA). The red dotted line represents the buccal angulation of the abutment (BAA).
Measurement of virtual abutment angulation for SCRP
For aesthetic and functional reasons, we attempted to locate the screw hole of the SCRP implant between the buccal and palatal cusps (Fig. 2). A screw hole with an outer diameter of 2.4 mm was applied to the abutment of the SCRP. Therefore, an area 1.2 mm centrically from the buccal and palatal cusp tips was considered an acceptable range for the abutment angulation of the SCRP. We measured the buccal (BAA) and palatal angulations (PAA) of the abutment from line ‘A.’
Statistical analysis and determination of type of prosthesis
Statistical analysis was performed using SPSS, Ver. 28.0.1 (SPSS Inc., Chicago, IL, USA). All statistical results were considered significant if the P value was less than 0.05. The Shapiro–Wilk test was used to determine the normality of the data. We used Student's t-test to compare the alveolar width, angulation of abutment, angulation of the fixture, and angulation of line ‘R’ and ‘A’ between the upper first and second premolars.
If the PAA was smaller than the BAF, or if the BAA was smaller than the PAF, we judged that SCRP was a feasible implant prosthesis. For all other situations, CRP was deemed appropriate. We used the chi-square test to analyze the relationship between the region of the premolars (first or second) and the type of prosthesis (SCRP or CRP).
To identify the predictors that had a significant influence on the type of prosthesis deemed feasible (SCRP or CRP), we used a multistep approach. The predictor variables were CW, MW, AW, RO, AO, and RA. The outcome variable was the type of prosthesis. First, the Student's t-test was used to determine the statistical difference in predictor variables between SCRP and CRP. Based on these results, we performed a multiple logistic regression analysis using a backward stepwise procedure.
Results
Of the 521 patients who underwent implantation during the study period, 47 met the inclusion criteria (22 male and 25 female). The patients' mean ages were 66.84 ± 7.44 years. The total number of implants was 58; of these, 25 implants were placed in the first premolar area (43.1%), and 33 implants were placed in the second premolar area (56.9%).
The clinical characteristics of the premolar areas assessed in this study are listed in Table 1. Five factors were significantly different between the first and second premolar areas: MW (P = 0.002), AW (P = 0.001), BAF (P = 0.05), RO (P < 0.001), and AO (P = 0.002). All angulations of abutment and angulations of fixture were positive except for the BAF of the first premolar (−0.38 ± 9.80°). The mean difference in the BAF between the first and second premolar area was 9.06°.
Table 1.
Characteristics of the alveolar bone, the implant fixture and the implant abutment at the maxillary premolar area.
| First premolar (N = 25) | Second premolar (N = 33) | P valuea | Total (N = 58) | |
|---|---|---|---|---|
| Alveolar ridge width | ||||
| CW (mm) | 7.91 ± 1.20 | 8.26 ± 1.51 | 0.34 | 8.11 ± 1.38 |
| MW (mm) | 9.39 ± 1.61 | 11.10 ± 2.27 | 0.002 | 10.36 ± 2.17 |
| AW (mm) | 12.17 ± 2.39 | 15.33 ± 3.82 | 0.001 | 13.97 ± 3.62 |
| Angulation of abutment | ||||
| BAA (°) | 7.19 ± 1.46 | 8.47 ± 1.13 | 0.13 | 8.24 ± 1.30 |
| PAA (°) | 7.19 ± 1.41 | 7.24 ± 0.84 | 0.89 | 7.22 ± 1.11 |
| Angulation of fixture | ||||
| BAF (°) | −0.38 ± 9.80 | 8.68 ± 12.71 | 0.05 | 4.77 ± 12.31 |
| PAF (°) | 33.50 ± 9.77 | 36.67 ± 9.65 | 0.22 | 36.57 ± 10.16 |
| Angulation of line ‘R’ and line ‘A’ | ||||
| RO (°) | 116.12 ± 6.28 | 106.88 ± 9.85 | <0.001 | 110.86 ± 9.61 |
| AO (°) | 100.11 ± 7.09 | 93.75 ± 7.86 | 0.002 | 96.50 ± 8.12 |
| RA (°) | 16.01 ± 6.55 | 13.12 ± 5.86 | 0.09 | 14.37 ± 6.29 |
CW: coronal width; MW: middle width; AW: apical width; BAA: buccal angulation of the abutment; PAA: palatal angulation of the abutment; BAF: buccal angulation of the fixture; PAF: palatal angulation of the fixture; RO: angulation between line ‘R’ and the occlusal plane; AO: angulation between line ‘A’ and occlusal plane; RA: difference in angulation between RO and AO.
Result of Student's t-test.
Appropriate prosthesis types for the premolar area are represented in Table 2. We found that SCRP was feasible in 52% of first premolar areas and 78.8% of second premolar areas. There was a positive relationship between the feasibility of SCRP and the premolar region (P = 0.031). The likelihood of SCRP being feasible was higher in the second premolar area than in the first premolar area.
Table 2.
Relationship between the premolar region and type of prosthesis.
| First premolar | Second premolar | Total | x2 (P valuea) | |
|---|---|---|---|---|
| SCRP | 13 (52%) | 26 (78.8%) | 39 (100%) | 4.63 (0.031) |
| CRP | 12 (48%) | 7 (21.2%) | 19 (100%) | |
| Total | 25 (100%) | 33 (100%) |
SCRP: screw-and-cement-retained prosthesis; CRP: cement-retained prosthesis.
Result of chi-square test.
Four factors were identified as the best predictors for the type of prosthesis: MW (P = 0.042), AW (P < 0.001), RO (P < 0.001), and RA (P < 0.001) (Table 3). On multiple logistic regression, RA had a statistically significant association with the type of prosthesis (P = 0.001), being significantly higher in the CRP group (OR = 1.885; 95% CI: 1.31 to 2.70). The overall predictive accuracy of RA was 93.1% (Table 4).
Table 3.
Predictors of feasibility of implantation.
| Predictors | SCRP (N = 39) | CRP (N = 19) | P valuea |
|---|---|---|---|
| Alveolar ridge width | |||
| CW (mm) | 8.19 ± 1.37 | 7.94 ± 1.43 | 0.522 |
| MW (mm) | 10.76 ± 2.23 | 9.53 ± 1.85 | 0.042 |
| AW (mm) | 15.10 ± 3.74 | 11.65 ± 1.87 | <0.001 |
| Angulation of line ‘R’ and line ‘A’ | |||
| RO (°) | 107.72 ± 9.35 | 117.31 ± 6.54 | <0.001 |
| AO (°) | 96.62 ± 9.26 | 96.22 ± 5.26 | 0.83 |
| RA (°) | 11.09 ± 3.69 | 21.08 ± 5.04 | <0.001 |
CW: coronal width; MW: middle width; AW: apical width; RO: angulation between line ‘R’ and the occlusal plane; AO: angulation between line ‘A’ and occlusal plane; RA: difference in angulation between RO and AO; SCRP: screw-and-cement-retained prosthesis; CRP: cement-retained prosthesis.
Result of Student's t-test.
Table 4.
Factors associated with the feasibility of CRP: results from multiple logistic regression analysis.
| Predictor | Odds ratio | (95% CI) | P valuea |
|---|---|---|---|
| RA | 1.885 | (1.31–2.70) | 0.001 |
The initial logistic regression model was constructed using CRP as the outcome variable and MW, AW, RO, and RA as predictor variables, using a backward stepwise procedure. The final logistic regression model is presented here with CRP as the outcome variable and RA as the predictor variable.
CRP: cement-retained prosthesis; CI: confidence interval; MW: middle width; AW: apical width; RO: angulation between line ‘R’ and the occlusal plane; RA: difference in angulation between RO and AO.
Result of multiple logistic regression.
Discussion
The following factors should be considered when planning implant therapy with SCRP. First, it is recommended that the SAH should not invade the buccal and palatal/lingual cusps and should be located as close to the central fossa as possible, for both aesthetic and functional reasons.9,10 Second, straight abutment should be used whenever possible for decreasing stress on the implants and adjacent bone.11 Third, the implant fixture should be placed perpendicular to the occlusal surface, whenever possible, to generate axial loading.4 Bony fenestration and dehiscence should not occur when these 3 conditions are met.17,18
The alveolar ridge in the maxillary premolar area has a large buccal inclination.15 This anatomic feature could restrict angulation of the implant fixture because fenestration is more likely as the angulation difference increases between the alveolar ridge inclination and the implant fixture angle.17 Ribas et al. found that perforation and dehiscence rates were 8.8% and 2.7% in the premolar region.19 In our study, the RO (buccal inclination of the alveolar ridge at the maxillary premolar area) was significantly larger at the first premolar than at the second premolar, with a mean difference of 9.24°. Due to these anatomic conditions, ideal placement of an SCRP implant is limited; the first premolar area is more unfavorable for SCRP than the second premolar area (P = 0.031).
The anatomic conditions of a narrow alveolar width and a large buccal inclination at the maxillary premolar area limit the angulation of implant placement. In our study, the BAF (buccal angulation of the implant fixture) was statistically significantly smaller at the first premolar area than at the second premolar area, with negative values seen at the first premolar area. We judged that the small MW and AW, and the high RO, of the first premolar area could limit determination of the bucco-palatal position and angulation of the implant fixture. Thus, the possibility of fenestration and dehiscence is higher for the first premolars than for the second premolars. Large fenestration may lead to loss of initial fixation of the implant and to increase the risk of overload and bone loss.17,18
Use of an SCRP implant was not feasible in 48% of first premolars and 21.2% of the second premolars we analyzed. We found that the feasibility of CRP was 4.63 times higher in the first premolar area (P = 0.031). On multiple logistic regression analysis, a higher RA indicated a higher probability of choosing CRP. As RA increases by 1, the probability of choosing CRP increases by 1.885 times. Since RO and AO are clinically determined, it is difficult to change the RA. Therefore, if the RA is high, SCRP should not be selected. In these patients, it would be wise to choose CRP in the implant treatment planning stage.
When planning implant treatment, clinicians should keep in mind that SCRP is not always feasible at the maxillary premolar area, especially in the first premolar area. If the difference between the angle of the axis of the prosthesis and the axis of the alveolar bone is large, it may be necessary for the clinician to consider CRP in the treatment planning stage. One of the main limitations of this study is that our sample size was small. A larger clinical study is needed to verify our results.
Declaration of competing interest
The authors have no conflict of interest relevant to this article.
Acknowledgments
The authors thank Prof. Sohee Oh (Medical Research Collaborating Center, Seoul Metropolitan Government–Seoul National University Boramae Medical Center) for her help with respect to the statistical analysis.
References
- 1.Shadid R., Sadaqa N. A comparison between screw- and cement-retained implant prostheses. A literature review. J Oral Implantol. 2012;38:298–307. doi: 10.1563/AAID-JOI-D-10-00146. [DOI] [PubMed] [Google Scholar]
- 2.Wittneben J.G., Joda T., Weber H.P., Brägger U. Screw retained vs. cement retained implant-supported fixed dental prosthesis. Periodontol 2000. 2017;73:141–151. doi: 10.1111/prd.12168. [DOI] [PubMed] [Google Scholar]
- 3.Heo Y.K., Lim Y.J. A newly designed screw- and cement-retained prosthesis and its abutments. Int J Prosthodont. 2015;28:612–614. doi: 10.11607/ijp.4236. [DOI] [PubMed] [Google Scholar]
- 4.Chee W., Jivraj S. Screw versus cemented implant supported restorations. Br Dent J. 2006;201:501–507. doi: 10.1038/sj.bdj.4814157. [DOI] [PubMed] [Google Scholar]
- 5.Hebel K.S., Gajjar R.C. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997;77:28–35. doi: 10.1016/s0022-3913(97)70203-8. [DOI] [PubMed] [Google Scholar]
- 6.Al-Omari W.M., Shadid R., Abu-Naba'a L., El Masoud B. Porcelain fracture resistance of screw-retained, cement-retained, and screw-cement-retained implant-supported metal ceramic posterior crowns. J Prosthodont. 2010;19:263–273. doi: 10.1111/j.1532-849X.2009.00560.x. [DOI] [PubMed] [Google Scholar]
- 7.Torrado E., Ercoli C., Al Mardini M., Graser G.N., Tallents R.H., Cordaro L. A comparison of the porcelain fracture resistance of screw-retained and cement-retained implant-supported metal-ceramic crowns. J Prosthet Dent. 2004;91:532–537. doi: 10.1016/j.prosdent.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Zarone F., Sorrentino R., Traini T., Di lorio D., Caputi S. Fracture resistance of implant-supported screw- versus cement-retained porcelain fused to metal single crowns: sem fractographic analysis. Dent Mater. 2007;23:296–301. doi: 10.1016/j.dental.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Shinohara R., Ueda K., Watanabe F. Influence of the difference between implant body and screw materials on abutment screw loosening. Dent Mater J. 2019;38:150–156. doi: 10.4012/dmj.2018-023. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Gazaui S., Razzoog M., Sierraalta M., Saglik B. Fabrication of a screw-retained restoration avoiding the facial access hole: a clinical report. J Prosthet Dent. 2015;114:621–624. doi: 10.1016/j.prosdent.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Cavallaro J., Jr., Greenstein G. Angled implant abutments: a practical application of available knowledge. J Am Dent Assoc. 2011;142:150–158. doi: 10.14219/jada.archive.2011.0057. [DOI] [PubMed] [Google Scholar]
- 12.Vera C., De Kok I.J., Reinhold D., et al. Evaluation of buccal alveolar bone dimension of maxillary anterior and premolar teeth: a cone beam computed tomography investigation. Int J Oral Maxillofac Implants. 2012;27:1514–1519. [PubMed] [Google Scholar]
- 13.Rojo-Sanchis J., Viña-Almunia J., Peñarrocha-Oltra D., Peñarrocha-Diago M. Facial alveolar bone width at the first and second maxillary premolars in healthy patients: a cone beam computed tomography study. J Oral Implantol. 2017;43:261–265. doi: 10.1563/aaid-joi-D-16-00195. [DOI] [PubMed] [Google Scholar]
- 14.Cho H.J., Jeon J.Y., Ahn S.J., et al. The preliminary study for three-dimensional alveolar bone morphologic characteristics for alveolar bone restoration. Maxillofac Plast Reconstr Surg. 2019;41:33. doi: 10.1186/s40902-019-0216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nishihara K., Yoshimine S.I., Goto T., et al. Topographic analysis of the maxillary premolars relative to the maxillary sinus and the alveolar bone using cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;123:606–612. doi: 10.1016/j.oooo.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Wang T.Y., Kuo P.J., Fu E., et al. Risks of angled implant placement on posterior mandible buccal/lingual plated perforation: a virtual immediate implant placement study using cbct. J Dent Sci. 2019;14:234–240. doi: 10.1016/j.jds.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan H.L., Garaicoa-Pazmino C., Suarez F., et al. Incidence of implant buccal plate fenestration in the esthetic zone: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2014;29:171–177. doi: 10.11607/jomi.3397. [DOI] [PubMed] [Google Scholar]
- 18.Van Oosterwyck H., Duyck J., Vander Sloten J., Van Der Perre G., Naert I. Peri-implant bone tissue strains in cases of dehiscence: a finite element study. Clin Oral Implants Res. 2002;13:327–333. doi: 10.1034/j.1600-0501.2002.130314.x. [DOI] [PubMed] [Google Scholar]
- 19.Ribas B.R., Nascimento E.H.L., Freitas D.Q., et al. Positioning errors of dental implants and their associations with adjacent structures and anatomical variations: a cbct-based study. Imaging Sci Dent. 2020;50:281–290. doi: 10.5624/isd.2020.50.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]