Abstract
The Association of Medical Laboratory Immunologists (AMLI) have developed a panel of antinuclear and anticytoplasmic antibody consensus sera that can be useful for enzyme immunoassay (EIA), Ouchterlony, and immunofluorescence assay methods. It was developed to assist in the evaluation of newly available EIA methods for the detection of autoantibodies. The panel of sera was evaluated in several clinical laboratories and a large number of laboratories owned by manufacturers of clinical autoantibody testing kits. The majority of sera performed well for the EIAs in both the clinical laboratories and the manufacturers' laboratories, but some samples had discrepant results. A major source of discrepancy is the current inability of the EIA results to be directly compared in a quantitative way as no standardization exists. The evaluation demonstrated lower sensitivity of detection by the Ouchterlony method. The limited evaluation of the sera with immunoblotting and Western blotting did not show good agreement with other methods. Further work must be done to standardize blotting methods prior to their use in routine clinical testing. The sera are now available to vendors and clinical laboratories for use in the detection of SS-A, SS-B, Sm, U1-RNP, Scl-70, Jo-1, double-stranded DNA, and centromere antibodies. The availability of the consensus sera will help evaluate and improve the EIA methods currently being used.
The detection of autoantibodies specific for eight common nuclear antigens has proved clinically useful for patients with systemic lupus erythematosus (SLE), Sjögren's syndrome, mixed connective tissue disease (MCTD), and scleroderma. Most of these eight antibodies were initially described using the Ouchterlony technique, but a variety of immunological methods have been used. Unfortunately, results from different methods have not shown good agreement. Efforts to standardize results from all methods have been hampered by low volumes of the sera used in the original characterizations and a lack of large volumes of other well-characterized positive control sera. Until recently most available reference sera have been characterized only by antinuclear antibody (ANA) and Ouchterlony methods.
The World Health Organization in conjunction with the International Union of Immunological Societies developed several standards for evaluation of ANAs, including WHO 66/233 for immunoglobulin G ANA, WHO/IUIS 480010 fluorescein isothiocyanate-conjugated anti-human immunoglobulin, and Wo/80 for antibodies to double-stranded DNA (dsDNA) (2). Standardization of other autoantibodies was initiated during a 4-year study by the European Consensus Study Group (11, 12). In 1980, the Arthritis Foundation (AF), in collaboration with the Centers for Disease Control (CDC), established a Committee on Antinuclear Antibody Serology in the United States. This organization prepared a panel of five AF-CDC reference sera, made available in 1982, that included specificities for ANA, dsDNA, SS-B, RNP, and Sm antibodies (7). Several international organizations joined to support the activities of the Committee on Antinuclear Antibody Serology: the International League Against Rheumatism, the International Union of Immunological Societies and the World Health Organization (8). This cooperative effort expanded the band of AF-CDC sera to a total of 10 different sera covering the following spectrum: five fluorescent ANA patterns (diffuse, nucleolar, centromere, and two speckled patterns) and seven ANA specificities (SS-A, SS-B, U1-RNP, Sm, Scl-70, and Jo-1). Although the European Consensus Study Group standards were found to be suitable for enzyme immunoassay (EIA) methods, some of the AF-CDC standards were found to yield inconsistent results with newer methods (4). The AF-CDC standards were recently reevaluated to define their usefulness for immunoblotting techniques, and most of the sera were found to produce the expected band patterns with the exception of the anti-SS-A(Ro) sample, which did not show a consistent band pattern (5). The AF-CDC serum panel was recently used to evaluate performance of EIA kits from nine manufacturers. The study demonstrated good performance with SS-A, SS-B, Scl-70, centromere, and Jo-1 kits while the dsDNA and Sm kits performed less well (10).
Beginning in 1994 a large number of manufacturers began producing EIA kits utilizing a variety of nuclear extracts, purified antigens, and recombinant protein preparations containing the most common nuclear antigens. Because of the lack of good reference materials to evaluate the large number of new EIA kits, it was determined by the Standards Committee of the Association of Medical Laboratory Immunologists (AMLI) in the summer of 1995 that a consensus panel of well-characterized serum samples should be produced. The immediate goals were (i) to produce a battery of consensus sera that would be produced in sufficient quantity to be used by both reagent manufacturers and clinical diagnostic laboratories and (ii) to gather information concerning the performance of EIA kits from different manufacturers. As EIAs have been used for nuclear autoantibody testing for a relatively short time, the committee felt that the development of a consensus serum panel was the most realistic approach to the initial efforts. As more laboratories adopt EIA techniques for routine testing and additional clinical information is gained about the performance of these assays, the long-term goal is to develop a reference serum panel for the most commonly encountered nuclear antigens. A specific battery of autoantibodies was selected for study because of their clinical relevance and because the antigens they are directed against are well characterized. The target antibodies included those against dsDNA, SS-A, SS-B, Sm, RNP, Scl-70, centromere, and Jo-1. Although the goal was to produce sera that would perform well in EIAs, evaluation of the sera was also performed with methods being currently used in the clinical laboratories carrying out the evaluation. The methods used included immunofluorescence assay (IFA) on Crithidia lucilliae for anti-dsDNA, IFA on HEp-2 cells for anti-centromere, and double immunodiffusion (DD) and hemagglutination (HA) for the extractable nuclear antigens (ENAs). During the course of the study, several manufacturers who were in the process of developing blotting methods (Western blotting [WB], dot blotting [DB], or immunoblotting [IB]) also evaluated the sera by these methods.
All clinical laboratories are experiencing severe fiscal restraints that dictate that testing be done as efficiently as possible. EIA methods can be automated to provide more cost-effective autoantibody testing than the classic manual methods of IFA and double immunodiffusion (4, 7, 8), but the lack of a reference panel suitable for EIA testing has been a hindrance to many laboratories adopting EIA methods. The project undertaken by the AMLI Standards Committee was intended to develop an autoantibody consensus serum panel suitable for the assays currently on the market. The evaluation studies described in this report show the successful production of eight sera and some comparison results for the different reagent manufacturers.
MATERIALS AND METHODS
Reference preparations.
Approximately 1 liter of plasma from each of three normal individuals and 11 patients was obtained by plasmapheresis. The patients were selected based on preliminary evaluations and samples obtained after review of the diagnosis in conjunction with the clinical rheumatologist treating the patients. Diagnostic criteria as outlined by the American College of Rheumatology (formerly American Rheumatism Association) were used to establish the diagnosis for each patient (1, 8, 9).
The plasma was converted to serum with 0.01 M CaCl2 and 0.01 M ɛ-amino-n-caproic acid. The fibrinogen was physically removed as a clot, and the bulk sera were then ultracentrifuged to remove any residual fibrin strands. A stabilizing agent was then added, 1.0-ml aliquots were prepared for use in testing, and the remainder of each serum sample was stored at −70°C until completion of the study. A sample of serum from each patient was tested and found to be negative for antibodies to human immunodeficiency virus type 1, hepatitis A, B, and C virus, and syphilis using Food and Drug Administration-approved procedures. The method of preparation of the sera differs from that previously described (5) which specifies that reference preparations should be freeze-dried (lyophilized). We were concerned that the lyophilization step may have an effect on the EIA (Robert Nakamura, personal observation); therefore, the sera in the AMLI reference panel were stabilized, stored in 1-ml aliquots at −70°C until shipped, and have a shelf life after shipping of 6 months.
Participant laboratories.
Nine AMLI members and 21 vendors participated in this study. AMLI members volunteered to participate in response to announcements in the AMLInteractions member newsletter. AMLI member participants' laboratories were geographically diverse, representing various regions of the United States and Canada (listed as A-1 through A-9 in tables). Vendors invited to participate included those who exhibit at AMLI annual meetings or advertised as supplying products used in autoantibody testing (1a). During the testing phase of the study, additional vendors who offer WB or IB assays for autoantibodies were requested to participate.
Participating vendors included, Clark Laboratories, Jamestown, N.Y.; Diamedix Corporation, Miami, Fla.; Elias USA, Inc., Osceola, Wis.; Gull Laboratories, Salt Lake City, Utah; Helix Diagnostics, West Sacramento, Calif.; Immco Diagnostics, Buffalo, N.Y.; ImmunoConcepts, Inc., Sacramento, Calif.; IncStar Corporation, Stillwater, Minn.; Inova Diagnostics, San Diego, Calif.; Kenstar Corporation, North Miami, Fla.; Kronus, Inc., San Clemente, Calif.; Life Codes Corporation, Stamford, Conn.; MarDx Diagnostics, Carlsbad, Calif.; Quest International, North Miami, Fla.; Sanofi Diagnostics Pasteur, Chaska, Minn.; Scimedx Corporation, Denville, N.J.; The Binding Site, Inc., San Diego, Calif.; TheraTest Laboratories, Chicago, Ill.; and Zeus Scientific, Inc., Branchburg, N.J.
Participating AMLI laboratories included the Lahey Clinic, Burlington, Mass. (Linda Cook); Presbyterian University Hospital, Pittsburgh, Pa. (Robert Kelly); Regional Medical Laboratories, Tulsa, Okla. (Gerald Miller); Lab Corporation of America, Raritan, N.J. (Anne Johnston); Royal Victoria Hospital, Montreal, Quebec, Canada (Kirk Osterland); Saint-Justine Hospital, Montreal, Quebec, Canada (Richard Marchand); Scripps Clinic, La Jolla, Calif. (Robert Nakamura); Sherbrooke University Hospital Center, Sherbrooke, Quebec, Canada (Gilles Boire); and Washington University School of Medicine, St. Louis, Mo. (Robin Lorenz).
Methods.
Methods used in this study included EIA, IFA, HA, DD, counterimmunoelectrophoresis, immunoelectrophoresis, radiolabeled immunoprecipitation (IP), and WB, IB, and DB as shown in Table 1. AMLI members used methods representative of all of the above methods except CIE, WB, and DB. Vendor methods were primarily EIA, but also included DD, HA, CIE, WB, IB, and DB.
TABLE 1.
Methods used by participating laboratories
| Laboratory study no. | Laboratory | Method(s)
|
||
|---|---|---|---|---|
| dsDNA | Centro | All others | ||
| AMLI-1 | Regional Medical Laboratories | EIA V6a, IFA V7 | IFA V19 | EIA V19 |
| AMLI-2 | Sherbrooke University Hospital Center | IFA V14 | IFA V7 | IFA V7 |
| AMLI-3 | Lab Corporation of America | EIA, HA V5 | ||
| AMLI-4 | Scripps Clinic | IFA V7 | IFA V7 | IP, IB (in house) |
| AMLI-5 | Presbyterian University Hospital | IFA V7 | IFA V7 | IP V19 |
| AMLI-6 | Washington University School of Medicine | IFA V15 | IFA V7 | EIA V19 |
| AMLI-7 | Lahey Clinic | EIA (in house) | IFA V15 | EIA V19 |
| AMLI-9 | Royal Victoria Hospital | IFA V7 | IFA V7 | IP V14 |
| AMLI-9 | Saint-Justine Hospital | EIA V19 | IFA V7 | EIA V19, IEPb (in house) |
| VENDOR-1 | MarDx Diagnostics | IFA | IFA | IP |
| VENDOR-2 | Gull Laboratories | EIA | ||
| VENDOR-3 | Helix Diagnostics | EIA, IFA | IFA | EIA |
| VENDOR-4 | Clark Laboratories | EIA | EIA | EIA |
| VENDOR-5 | Hemagen | HA, EIA | IFA | HA, EIA |
| VENDOR-6 | Diamedix | EIA | EIA | |
| VENDOR-7 | Sanofi Diagnostics Pasteur | EIA | EIA | |
| VENDOR-8 | Kronus | EIA | ||
| VENDOR-9 | Scimedx | IFA, WB | WB | EIA, WB, IB |
| VENDOR-10 | IncStar | EIA, IFA | IFA | EIA |
| VENDOR-11 | TheraTest | EIA | EIA | |
| VENDOR-12 | Quest-SeraQuest | EIA | EIA | |
| VENDOR-13 | Quest-Shield | EIA | EIA | |
| VENDOR-14 | Zeus Scientific | EIA, IFA | IFA | EIA, IP |
| VENDOR-15 | ImmunoConcepts | IFA | IFA | EIA |
| VENDOR-16 | Kenstar | EIA | EIA | EIA |
| VENDOR-17 | Binding Site | EIA, IFA | IFA | CIE |
| VENDOR-18 | Elias USA | EIA | EIA, WB | EIA, WB |
| VENDOR-19 | Inova Diagnostics | IFA | IFA | EIA, IP |
| VENDOR-20 | Immco Diagnostics | EIA, IFA, WB | IFA | EIA, IP, WB |
| VENDOR-21 | Life Codes | IB or WB | IB or WB | IB or WB |
V, vendor used by that laboratory, with the number corresponding to the vendor listed in the table.
IEP, immunoelectrophoresis.
Two different shipments of sera were used. In the first shipment, sent out in May 1996, eight samples were sent (samples A to H). In the second shipment, sent in February 1997, six samples, including three normal sera, were sent (samples I to N).
AMLI members who participated in the study used a combination of methods and/or vendor products that were being used in their laboratories for diagnostic testing or were currently under evaluation (Table 1). Each participating vendor reported results for the methods they were producing for clinical use or available in their research and development or reference laboratories. Because vendors and participants tested the specimens on more than one assay system while others did not test for some antibodies, the total number of results for each antibody is variable.
Antigen sources.
IFA methods for dsDNA used C. lucilliae as the substrate. EIA methods used calf thymus DNA, plasmid dsDNA, phage λ, or human recombinant DNA. One AMLI member performed a unique (unpublished) assay that captures the immunoglobulin G from patient sera and detects dsDNA by using intrinsically labeled, synthesized M13-dsDNA. One vendor for IB listed human K-562 as the antigen source for dsDNA; one vendor used human recombinant dsDNA. The EIA methods for SS-A used extracts of calf thymus, bovine spleen, or sheep spleen cells. The DD methods for SS-A used extracts of human spleen cells, Wil-2 whole cells, and calf thymus. The EIA methods for SS-B, Sm, RNP, Scl-70, and Jo-1 used extracts of calf or bovine thymus, rabbit thymus, bovine spleen, or sheep spleen. The EIA method that detects the U1-RNP antibody also detects the Sm antibody, while the Sm EIA method measures only Sm. Therefore, the RNP results will be termed RNP/Sm results in this paper. The DD methods for SS-B, Sm, RNP, Scl-70, and Jo-1 used extracts of calf thymus or rabbit thymus.
HEp-2 cells were the antigen source for the IFA methods for detecting centromere. One vendor's WB used human recombinant centromere antigen while two EIAs and one vendor's WB used an extract of HEp-2 cells to detect the centromere antibody. The IPP method for all of the ENAs used an extract of HeLa cells. One IB method used a HEp-2 cell extract for all of the ENAs.
Although not requested, 8 of 30 participants performed ANA testing on the samples, using HEp-2 cells as the substrate. One vendor performed an ANA by EIA using a cocktail of antigens, and another vendor performed an ANA by CIE using a sheep spleen extract.
Data analysis.
All of the data sheets were received and recorded by one of the study coordinators, and then the recorded data were compared to the raw data sheets by a second study member. Coded data were then sent to each participant and reviewed for correctness prior to the final analysis. Any methods that only contained results from one laboratory were not further analyzed because of the difficulty of comparing method specificities and sensitivities. Results for IP and HA methods are grouped together because of the low number of results from HA. For the purpose of the EIA data analysis, the few AMLI members' laboratory results were excluded from the summary tables because they all used kits from the same vendor. In all cases, the results from the AMLI laboratories were identical to those of the reagent vendor results.
For the purposes of classification, responses in which only one or two positive results were present while the majority of results for that method were negative were considered false positive. Results in which fewer than five negatives were present while a majority of results for that method were positive were considered false negatives. Results in which a significant minority of assays (>4 but <10) were positive were classified as inconclusive. The inconclusive results could not be determined to be false positives or false negatives based on the available data. This means of classification is arbitrary, as there is no clear “gold standard” to be used to unequivocally establish the validity of test results. Our method of result analysis provided an efficient means of viewing the data, although it is limited by the lack of a true gold standard. As our knowledge base increases with future studies and a true gold standard can be established, it is possible that we will find that some test results in this study need to be reclassified.
RESULTS
Results for all 14 samples evaluated by the participating laboratories and manufacturers are contained in Tables 2 to 5 for the IP, HA, IFA, and EIA methods. Table 6 contains the limited results for the samples when tested by WB or IB. A summary of the data will be discussed both for each sample studied and for each antibody evaluated.
TABLE 2.
SS-A and SS-B summary data
| Sample | No. of positive results for antibody/no. of tests performed
|
Antibody(-ies) present | |||
|---|---|---|---|---|---|
| SS-A
|
SS-B
|
||||
| IP or HA | EIA | IP or HA | EIA | ||
| A | 0/8 | 0/21 | 0/8 | 0/20 | None |
| B | 0/9 | 0/20 | 0/9 | 0/19 | None |
| C | 7/8 | 21/21 | 0/8 | 2/20 | SS-A |
| D | 6/9 | 19/21 | 0/9 | 0/20 | SS-A |
| E | 7/9 | 21/21 | 1/9 | 0/20 | SS-A |
| F | 7/9 | 18/21 | 1/9 | 0/20 | SS-A |
| G | 6/9 | 20/21 | 8/9 | 20/20 | SS-A, SS-B |
| H | 0/9 | 6/21 | 1/9 | 1/20 | SSA?a |
| I | 0/6 | 2/21 | 0/6 | 0/21 | None |
| J | 5/5 | 20/21 | 1/5 | 0/21 | SS-A |
| K | 0/5 | 0/21 | 0/7 | 0/21 | None |
| L | 0/5 | 0/20 | 0/5 | 0/20 | None |
| M | 0/5 | 0/21 | 0/5 | 0/21 | None |
| N | 0/5 | 0/21 | 0/5 | 0/21 | None |
?, inconclusive.
TABLE 5.
dsDNA and centromere summary data
| Sample | No. of results positive for antibody/no. of tests performed
|
Antibody present | |||
|---|---|---|---|---|---|
| dsDNA
|
Centromere
|
||||
| IFA | EIA | IFA | EIA | ||
| A | 0/13 | 0/16 | 14/14 | 2/2 | Centromere |
| B | 0/12 | 0/15 | 0/11 | 0/2 | None |
| C | 5/13 | 12/16 | 0/12 | 0/2 | dsDNA |
| D | 0/12 | 0/16 | 0/12 | 0/2 | None |
| E | 1/12 | 1/16 | 0/13 | 0/3 | None |
| F | 0/12 | 0/16 | 0/12 | 0/2 | None |
| G | 0/12 | 0/16 | 0/12 | 0/2 | None |
| H | 1/12 | 1/16 | 0/12 | 0/2 | None |
| I | 9/11 | 14/16 | 0/10 | 0/5 | dsDNA |
| J | 5/5 | 16/16 | 0/11 | 0/5 | dsDNA |
| K | 1/11 | 0/16 | 0/11 | 0/4 | None |
| L | 1/11 | 0/16 | 0/11 | 0/4 | None |
| M | 0/11 | 0/16 | 0/11 | 0/4 | None |
| N | 0/11 | 1/16 | 0/11 | 0/4 | None |
TABLE 6.
IB summary data
| Sample | No. of IB results positive for antibody/no. of tests performed
|
|||||||
|---|---|---|---|---|---|---|---|---|
| dsDNA | SS-A | SS-B | Sm | U1-RNP | Scl-70 | Jo-1 | Centromere | |
| A | NEGa | NEG | NEG | NEG | NEG | NEG | NEG | 1/3 |
| B | 1/3 | NEG | NEG | NEG | NEG | 5/5 | NEG | NEG |
| C | 2/3 | 5/5 | 3/5 | 4/5 | 4/5 | 1/5 | 1/4 | 1/5 |
| D | 1/3 | 2/4 | NEG | 2/5 | 4/5 | NEG | NEG | NEG |
| E | 1/3 | 5/5 | 2/5 | NEG | NEG | NEG | NEG | NEG |
| F | 1/3 | 1/4 | NEG | NEG | 1/5 | NEG | NEG | 5/5 |
| G | 1/3 | 3/5 | 5/5 | NEG | NEG | NEG | NEG | NEG |
| H | 2/3 | NEG | NEG | 2/5 | 2/5 | 2/5 | NEG | 1/5 |
| I | NEG | 1/2 | NEG | 3/3 | 2/3 | NEG | 1/3 | NEG |
| J | NEG | 2/3 | 2/3 | 2/3 | NEG | 1/3 | NEG | NEG |
| K | NEG | NEG | NEG | 1/2 | NEG | NEG | NEG | NEG |
| L | NEG | 1/2 | NEG | NEG | NEG | NEG | NEG | NEG |
| M | NEG | NEG | NEG | NEG | NEG | NEG | NEG | 1/1 |
| N | 1/2 | 1/2 | NEG | NEG | NEG | NEG | NEG | NEG |
NEG, all results were negative.
Summary by serum sample.
Sample A was from an individual with the clinical diagnosis of CREST syndrome. All test participants found centromere antibody in this sample using IFA (14 of 14) and EIA (2 of 2). The sample was completely negative for reactivity for SS-A, SS-B, Sm, RNP/Sm, dsDNA, and Jo-1 by all methods. Two laboratories out of eight, one using IP and one using HA, gave false-positive results for Scl-70. Only one of three vendors who tested this specimen for centromere antibodies by IB had a positive result.
Sample B was from an individual with the diagnosis of scleroderma. Essentially all laboratories found Scl-70 antibody in the sample; all 17 EIA assays were positive and 7 of 8 IP or HA results were positive. The sample was negative for all other antibodies by all methods.
Sample C was from a patient with the diagnosis of SLE. SS-A was found by most laboratories using 21 EIA assays and by 7 of 8 IP and HA assays. Assays for Sm and RNP/Sm were positive in the majority of EIA kits (11 of 19 SS-A; 10 of 19 RNP/Sm) but mostly negative by IP or HA (one of nine positive for SS-A and RNP/Sm). The sample was positive for dsDNA in the majority of EIAs (12 of 16) and some of the IFAs (5 of 13). Sample C was positive in only 2 of 20 laboratories for SS-B by EIA and negative for Scl-70, Jo-1, and centromere by all assays. By IB, the majority of vendors showed the presence of SS-A, Sm, and RNP, and three of five IB assays were also positive for SS-B that was not detected by the other methods. For Sm, the specific positive bands were B, B′, and D. This sample was falsely positive by IB in one laboratory each for Scl-70, centromere, and Jo-1 and was positive in the laboratory with a dsDNA IB assay.
Sample D was from a patient with the diagnosis of MCTD. Essentially all laboratories, 9 of 10 IP or HA methods and 19 of 19 EIA methods, had positive results for RNP/Sm. SS-A was also found in this sample by 19 of 21 EIA assays and 6 of 9 IP or HA assays. Because of the unusual finding of SS-A in a patient with MCTD, an investigation was done which revealed that the SS-A reactivity was a contaminant eluted off of a filtration system used to produce the evaluation samples. The SS-A reactivity is not present in the bulk sample and will not be present in subsequent reference panel specimens. All other sera were reevaluated using specimens before and after the filtration process. Sample D was the only specimen found to be contaminated. Sample D in the consensus panel does not contain anti-SS-A because it was freshly filtered prior to bottling for distribution. The sample was found to be negative by all methods for SS-B, Sm, Scl-70, Jo-1, dsDNA, and centromere. For the IB assays, four of five had positive RNP results, two of five had positive Sm results, and one of five had a positive SS-A result.
Sample E was from a patient with the diagnosis of Sjögren's syndrome and SLE. The majority of assays were positive for SS-A, with seven of nine positive by IP or HA and 21 of 21 positive by EIA. The sample was negative for all other antibodies tested with only two exceptions. One of 9 IP or HA results for SS-B and 1 of 12 IFA results for dsDNA were positive. For the IB assays, all were positive for SS-A and two of five were also positive for SS-B.
Sample F was from a patient with the diagnosis polymyositis. The Jo-1 antibody was detected in all 13 EIA assays and in 6 of 8 IP or HA assays. In addition, the majority of assays also were positive for SS-A, i.e., 7 of 9 by IP or HA and 18 of 21 by EIA. Some assays also were positive for RNP, i.e., 3 of 10 by IP or HA and 14 of 19 by EIA. Negative results were found for all assays for Sm, Scl-70, dsDNA, and centromere. All five IB assays detected Jo-1, but one of five assays for both SS-A and RNP were also positive.
Sample G was from a patient with the diagnosis of Sjögren's syndrome. Essentially all assays for SS-B were positive, i.e., 8 of 9 by IP or HA and 20 of 20 by EIA. Essentially all assays for SS-A were also positive, i.e., 6 of 9 by IP or HA and 20 of 21 by EIA. A minority of assays for RNP were also positive, i.e., 3 of 10 by IP or HA and 6 of 19 by EIA. The sample was also positive in two laboratories, i.e., one by IP or HA and one by EIA for SS-B, and in two laboratories for Jo-1. By IB three of five were positive for SS-A and all five were positive for SS-B.
Sample H was from a patient with the diagnosis of rheumatoid arthritis. The majority of assays were negative for all antibodies, but a significant minority of the EIAs was positive. For SS-A by EIA, 6 of 21 were positive; for Sm, 12 of 19 were positive; and for RNP, 6 of 19 were positive. There were also scattered positives for the other methods and antibodies—two assays positive for SS-B, three positive for Scl-70, two positive for Jo-1, and two positive for dsDNA. IB found one or two of the five positives found for SS-A, SS-B, Sm, RNP, Scl-70, and Jo-1.
Sample I was from a patient with the diagnosis of SLE. Essentially all assays were positive for dsDNA, i.e., 9 of 11 by IFA and 14 of 16 by EIA. All assays were positive for Sm, and the majority were positive for RNP, i.e., 5 of 7 by IP or HA and 19 of 19 by EIA. A significant minority, 5 of 16, was EIA positive for Scl-70. Rare positives, two by EIA for SS-A and one by IP or HA for Jo-1, were found, but all other assays for all other antibodies were negative. By IB, all three were positive for Sm, two of three were positive for RNP, and one of two was positive for SS-A and Jo-1.
Sample J was from a patient with the diagnosis of SLE. All assays were positive for dsDNA and SS-A. A minority of EIAs for RNP, 8 of 21, and for Scl-70, 7 of 17, were positive. All other assays were negative for other antibodies. By IB, the dsDNA result was negative for all three and two of three were positive for SS-A, SS-B, and Sm.
Sample M was from a patient with the diagnosis of SLE. It was negative by all assays except for two assays, one IP and one EIA for Scl-70. When tested by IFA, this sample was found to contain a positive speckled staining pattern consistent with PCNA. This serum was included to evaluate whether the PCNA antibody would be picked up in the EIA for other nuclear antibodies. Only a limited amount of serum was available, so it was not included in the final consensus panel.
Samples K, L, and N were from healthy individuals. These sera were included to provide laboratories with a source of tested autoantibody-negative sera. All assays were negative by all methods except for one IP with sample K for dsDNA, one IP with sample L for dsDNA, one EIA with sample N for dsDNA, and one EIA with sample N for SS-A. By IB, sample K had one positive result for Sm, sample L had one positive result for SS-A, and sample N had one positive result for dsDNA and SS-A.
Summary by antibody using IP or HA and EIA.
SS-A antibody was found in samples C, D, E, F, G, and J for essentially all EIAs (119 of 126 tests). A majority of IP or HA methods were also positive but less reactive; only 38 of 49 assays were positive. More problematic were the results for sample H, containing rheumatoid factor, for which 6 of 21 EIAs were positive while all 9 IP or HA results were negative. The explanation for the results of sample H is not known but may be a result of rheumatoid factor interference in some of the assays, an increased sensitivity to SS-A in a few EIA kits, or false-positive results due to some other interference.
SS-B antibody was found only in sample G. Slightly better sensitivity was found by the EIA method, by which all 20 samples were positive, while only eight of nine IP or HA results were positive. Four other probable false-positive results were found by IP or HA, one each in samples E, F, H, and J. One false-positive EIA result was seen for sample H.
Sm antibody was found in samples C, H, and I. For sample I all tests were positive by all methods. For samples C and H, the majority of IP or HA assays were negative, with only 1 positive result out of 17 assays. The IP or HA method was less often positive than the EIA for these two samples. One false-positive IP or HA result and two false-positive EIA results were seen.
RNP/Sm antibody was found in samples C, F, G, H, I, and J. For samples D and I essentially all results were positive by EIA, and most of the IP or HA assays were positive. For samples C and F, the majority of EIAs were positive and a minority of IP or HA assays was positive. These samples, C, D, F, and I, probably contain RNP/Sm antibody and demonstrate an increased positive rate for the EIA assays. For samples G, H, and J a significant minority of EIAs were positive, while only 3 of 24 IP or HA assays were positive. Based on the available data, it is not possible to determine whether the results for samples G, H, and J by EIA are false positives or true positives. The RNP/Sm antigen cannot be clearly distinguished from the Sm antigen with the EIA system, so a portion of the inconsistent results may be due to differences in the vendors' instructions concerning interpretation of EIAs where both the Sm and RNP EIA wells are positive. This could clearly influence the results for samples C and H, which were shown to contain Sm by EIA.
Scl-70 antibody was found in sample B and in a minority of IP or HA and EIA results for samples I and J. Given the diagnosis of SLE for the patients providing samples I and J it is probable that the positive results for these two samples are false positives. The explanation for this high rate of false positives is unknown but could be a result of an impure antigen preparation.
Jo-1 antibody was found in sample F. The EIA method was positive in all assays while the IP or HA method was positive in only six of eight assays. False-positive results were found in five EIAs for samples G and H and with one IP or HA result for sample I.
dsDNA antibody was found in samples C, I, and J. Sample C was positive in 12 of 16 EIAs but only positive in a minority, 5 of 13, of IFAs. This is consistent with a variety of published studies that have shown IFA to be a relatively insensitive method for detection of dsDNA antibodies (3). There was only one false-positive EIA result and four false-positive IFA results.
Centromere antibody was found in sample A. No false-positive results were seen for any of the other samples.
Method summary.
Results from evaluations to determine the number of false-negative, false-positive, and inconclusive results for the IFA, IP or HA, and EIA methods are found in Table 7. The EIAs had much lower numbers of false-positive and false-negative results than did the IP or HA assays. However, the EIAs had a significant number of inconclusive results, especially for the Sm and RNP assays. Interestingly, the assay that performed best was the IFA for centromere. The centromere EIA was only available from two vendors, so a good comparison evaluation was not possible. The assays with the largest number of false negatives were the IP or HA for SS-A and the IFA for dsDNA. The largest number of false-positive results was found for the Scl-70 IP or HA assay, the Jo-1 EIA, and the IP or HA SS-B assays.
TABLE 7.
Discrepant sample data summary
| Antibody | IFA
|
IP or HA
|
EIA
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of tests done | No. of false negatives (%) | No. of false positives (%) | No. of tests done | No. of false negatives | No. of false positives | No. of inconclusive resultsb | No. of tests done | No. of false negatives (%) | No. of false positives (%) | No. of inconclusive results (%)a | |
| dsDNA | 158 | 10 (6.9) | 4 (2.6) | 223 | 6 (2.7) | 3 (2.6) | 0 (0) | ||||
| Centromere | 163 | 0 | 0 | 43 | 0 | 0 | 0 | ||||
| SS-A | 101 | 11 | 0 | 0 | 292 | 7 | 2 | 6 | |||
| SS-B | 103 | 1 | 4 | 0 | 284 | 0 | 3 | 0 | |||
| Sm | 112 | 0 | 1 | 1 | 271 | 0 | 2 | 23 | |||
| U1-RNP | 113 | 3 | 0 | 7 | 270 | 0 | 1 | 42 | |||
| Scl-70 | 101 | 1 | 5 | 2 | 231 | 0 | 1 | 12 | |||
| Jo-1 | 85 | 3 | 1 | 0 | 190 | 0 | 5 | 0 | |||
| Total (%) | 615 | 19 (3.1) | 11 (1.8) | 10 (1.6) | 1,538 | 7 (0.5) | 14 (0.9) | 83 (5.4) | |||
EIA negative results in which a significant minority of results were positive. These results may be false negatives.
Ouchterlony assay negative results in which a significant majority of EIA results were positive. These results may be false negatives.
Results from the IB method were the least consistent and did not match well with either the EIA or IP or HA results. They were frequently positive when results from the other methods were negative and also negative when results from the other methods were convincingly positive. Although only three blot methods for dsDNA were done, the assay available from one of the vendors was positive with all of the first eight samples (the second six samples were not tested using this method). Based on these comparison results, patient results would be significantly different from the IP or HA or EIA results if the IB method were used.
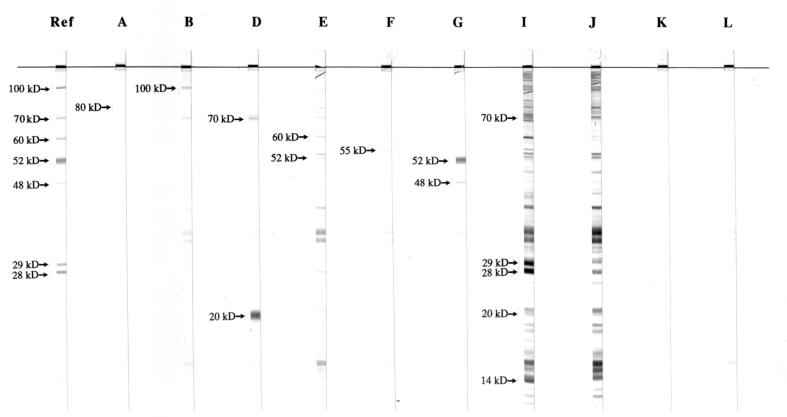
Results from these comparison evaluations were reviewed and then a reference panel of sera containing 10 sera was made available to the public in late 1997. Due to discrepant results sera C and H were omitted from the final panel. In addition, serum M was omitted due to a lack of sufficient volume of serum. The normal sera were included at the request of a number of AMLI members' laboratories that desired documented autoantibody-negative sera. The panel sample information and antibodies present are found in Table 8. This reference serum panel is available through the AMLI and SLR Research Corporation, Carlsbad, Calif. Figure 1 contains results from WBs done on the panel sera by SLR Research Corporation.
TABLE 8.
AMLI reference serum panel
| Specimen | Major antibody | WB band(s) observed | Other antibody(ies) present (by EIA) |
|---|---|---|---|
| A | Centromere | 80-kDa CENP-B, 18-kDa CENP-A (minor) | None |
| B | Scl-70 | 100-kDa Scl-70, 70-kDa Scl-70 (breakdown product) | None |
| D | U1-RNP | 70-kDa U1-RNP, 20 kDa U1-RNP-C | SS-A (contaminant) |
| E | SS-A | 60-kDa SS-A, 52-kDa SS-A | None |
| F | Jo-1 | 55-kDa Jo-1 | SS-A, RNP?a |
| G | SS-B | 52-kDa SS-B, 48-kDa SS-B (breakdown product) | SS-A, U1-RNP? |
| I | Sm | 29- and 28-kDa Sm-B, 14-kDa Sm-E and Sm-F, 70-kDa U1-RNP, 20-kDa U1-RNP-C | dsDNA, U1-RNP, Scl-70? |
| J | dsDNA | 29- and 28-kDa Sm-B, 14-kDa Sm-E Sm-F, 70-kDa U1-RNP, 20-kDa U1-RNP-C | SS-A, U1-RNP?, Scl-70? |
| K | None | None | None |
| L | None | None | None |
?, inconclusive.
FIG. 1.
Results from WBs performed at SLR Research Corporation on the serum samples in the AMLI consensus panel. The numbers correspond to the locations of the bands consistent with the characteristic antigens that are detected by the characterized antisera (Table 8).
DISCUSSION
This study can be used to compare results from the Ouchterlony method used by the majority of AMLI laboratories and the EIA results performed at the vendor laboratories. A total of 17 negative Ouchterlony results were seen with samples that were positive with essentially all EIA kits. For the SS-A antibody samples negatives were seen with samples C, D, E, F, and G; for the SS-B samples a negative was seen with sample G; for the U1-RNP antibody samples negative were seen with samples D and I; for the Scl-70 antibody samples a negative was seen with sample B; and for the Jo-1 antibody samples a negative was seen with sample F. The most likely explanation for these results is that the EIAs are slightly more sensitive than the Ouchterlony methods as performed by some of the testing laboratories. These false-negative results could also be a result of technical errors made during the testing. An alternate explanation could be that precipitation lines seen when multiantigen preparations were used were identified incorrectly. This type of error could result in either false-negative or false-positive results.
The Ouchterlony method also gave a total of 11 of false-positive results, when the majority of other Ouchterlony results were negative and essentially all EIA results were negative. This type of error could be a result of technical errors or incorrect identification of precipitation lines. In summary, a larger number of false positives and false negatives were seen with the Ouchterlony method that with the EIA method even though the EIA method had more than twice as many results. The Ouchterlony results that were the most problematic were the high rate of false-negative results with SS-A and the number of inconclusive results with U1-RNP.
The IFA method had mixed performance in this study. It was excellent for the detection of the centromere antibody in this panel. No false-positive or false-negative results were seen. In contrast, the IFA method for dsDNA gave some false negatives, for two of the three positive samples in the panel. Sample C was particularly problematic; it was negative by IFA in 8 of 13 laboratories while positive in 12 of 16 EIAs. Results for this sample by IFA could be a result of lack of sensitivity of some of the IFA slides or a problem with interpretation of the pattern present. Sample C was a low-titer antibody near the cutoff for many of the EIAs. The conflicting IFA and EIA results for samples C and I may also be a result of sensitivity difference between the two methods. These results were consistent with many previous studies of dsDNA assays, in which discrepant results have often been seen with various methods (3). In general, agreement is usually seen when high-titered, high-affinity, and high-avidity antibodies are present, but discrepant results are more often seen when testing lower-titered, lower-affinity, or lower-avidity antibodies. In addition, care must be taken when evaluating dsDNA assays to ensure that the assay is not reactive with ssDNA antibodies that are often in patient sera. We did not evaluate the study samples for ssDNA because assay kits for ssDNA are only available from a few vendors.
The EIA method in general had better performance than the Ouchterlony method. For samples that could be clearly determined, false negatives were only seen with the SS-A testing, and false positives were seen in only a few assays, with the highest number being for Jo-1 antibody results. The problem in the EIA testing was the very high number of inconclusive results in samples with significant numbers of positive EIA results and mostly negative Ouchterlony results. Of the 14 samples tested, the inconclusive EIA results were seen with five samples for U1-RNP, two samples for Sm, two samples for Scl-70, and one sample for SS-A. Most of the samples with high numbers of inconclusive results had lower reactivity in the assays than the samples that had consensus positive results. These indeterminant results illustrate the significant difference in the EIA kits from the different vendors and could reflect differences between the kits—e.g., different buffers affecting the binding of the antibodies, different antigen epitopes present, antigen coating concentration differences, different positive-negative cut-off levels, or the presence of other contaminating antigens in some of the antigen preparations. Similar results were seen in the recently published study by Tan et al. that demonstrated differences in kit performance between available kits (10). The EIAs with positive results used a variety of antigen sources so a single antigen preparation method could not be implicated. More study is necessary to determine the source of these discrepant results. For the consensus panel materials we did not use any of the samples with discrepant results as prototype sera. From a clinical perspective, the most problematic of these discrepant samples are the Sm and Scl-70 testing which should have disease specificity. At present there is no consistent method of standardizing result units from the EIAs. Because of this lack of standardization no direct comparison of results can be made between kits. Additional studies need to be done to make it possible to compare the quantity of antibody being measured. Until this is done the sensitivities and disease specificities of the EIA kits from the different manufacturers cannot be compared accurately.
The most surprising data was the lack of consensus results with the WB and DB data. Because these methods have been used extensively in the research laboratories to characterize and study the antigenic epitopes of many autoantigens, many researchers have begun using blotting methods as their gold standard method. The results of these studies demonstrated a significant difference in the results from the commercially available blotting materials. Our data are similar to those obtained during the European Consensus Studies of ENA antibody detection by immunoblot performed in 1991 and 1992 (11, 12). Further work must be done to standardize the details of the blotting methods prior to their use in routine clinical testing.
This study has demonstrated that consensus sera can be produced for EIA, Ouchterlony, and IFA testing methods. Sera are now available for use by vendors and clinical laboratories for detection of SS-A, SS-B, Sm, U1-RNP, Scl-70, Jo-1, dsDNA, and centromere antibodies. It is hoped that these sera will be used to improve the clinical laboratory testing for these antibody specificities.
TABLE 3.
Sm and U1-RNP summary data
| Sample | No. of positive results for antibody/no. of tests performed
|
Antibody(-ies) present | |||
|---|---|---|---|---|---|
| Sm
|
RNP
|
RNP/Sm
|
|||
| IP or HA | EIA | IP or HA | EIA | ||
| A | 0/9 | 0/19 | 0/9 | 0/19 | None |
| B | 0/10 | 0/18 | 0/10 | 0/18 | None |
| C | 1/9 | 11/19 | 1/9 | 10/19 | Sm?,a RNP? |
| D | 0/10 | 0/19 | 9/10 | 19/19 | RNP |
| E | 0/10 | 0/19 | 0/10 | 0/19 | None |
| F | 0/10 | 0/19 | 3/10 | 14/19 | RNP |
| G | 1/10 | 0/19 | 3/10 | 6/19 | RNP? |
| H | 0/8 | 12/19 | 0/9 | 6/19 | Sm?, RNP? |
| I | 7/7 | 20/20 | 5/7 | 19/19 | Sm, RNP |
| J | 0/5 | 2/21 | 0/5 | 8/21 | RNP? |
| K | 0/6 | 0/20 | 0/6 | 0/20 | None |
| L | 0/6 | 0/19 | 0/6 | 0/19 | None |
| M | 0/6 | 0/20 | 0/6 | 1/20 | None |
| N | 0/6 | 0/20 | 0/6 | 0/20 | None |
?, inconclusive.
TABLE 4.
Scl-70 and Jo-1 summary data
| Sample | No. of positive results for antibody/no. of tests performed
|
Antibody present | |||
|---|---|---|---|---|---|
| Scl-70
|
Jo-1
|
||||
| IP or HA | EIA | IP or HA | EIA | ||
| A | 2/8 | 0/17 | 0/6 | 0/14 | None |
| B | 7/8 | 17/17 | 0/8 | 0/13 | Scl-70 |
| C | 0/9 | 0/16 | 0/8 | 0/12 | None |
| D | 0/9 | 0/17 | 0/9 | 0/12 | None |
| E | 0/10 | 0/16 | 0/7 | 0/14 | None |
| F | 0/9 | 0/17 | 6/8 | 13/13 | Jo-1 |
| G | 0/9 | 0/17 | 0/7 | 3/14 | None |
| H | 2/9 | 1/17 | 0/7 | 2/14 | None |
| I | 1/6 | 5/16 | 1/5 | 0/14 | Scl-70?a |
| J | 1/4 | 7/17 | 0/4 | 0/14 | Scl-70?a |
| K | 0/5 | 0/16 | 0/4 | 0/14 | None |
| L | 0/5 | 0/16 | 0/4 | 0/13 | None |
| M | 1/5 | 0/16 | 0/4 | 0/15 | None |
| N | 0/5 | 0/16 | 0/4 | 0/14 | None |
?, inconclusive.
ACKNOWLEDGMENTS
The study was supported in part by QC Products, Pompano Beach, Fla., who supplied the sera for the panel, and by Elias USA, who did preliminary testing to determine suitability of sera for inclusion in the panel.
REFERENCES
- 1.Arnett F C, Edworthy S M, Bloch D A, McShane D J, Fries J F, Cooper N S, Healey L A, Kaplan S R, Liang M H, Luthra H S, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–324. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 1a.Medical Economics. Clinical laboratory reference. 22nd ed. 1995. Supplement to Medical Laboratory Observer. Medical Economics, Montvale, N.J. [Google Scholar]
- 2.Nakamura R M, Bylund J D, Tan E M. Current status of available standards for quality improvement of assays for detection of autoantibodies to nuclear and intracellular antigens. J Clin Lab Anal. 1994;8:360–368. doi: 10.1002/jcla.1860080605. [DOI] [PubMed] [Google Scholar]
- 3.Smeenk R J K, Berden J H M, Swaak A J G. dsDNA antibodies. In: Peter J B, Shoenfeld Y, editors. Autoantibodies. New York, N.Y: Elsevier Science; 1996. pp. 227–236. [Google Scholar]
- 4.Smolen J S, Steiner G, Tan E M. Standards of care: the value and importance of standardization. Arthritis Rheum. 1997;40:410–412. doi: 10.1002/art.1780400303. [DOI] [PubMed] [Google Scholar]
- 5.Smolen J S, Butcher B, Fritzler M J, Gordon T, Hardin J, Kalden J R, Lahita R, Maini R N, Reeves W, Reichlin M, Rothfield N, Takasaki Y, van Venrooij W J, Tan E M. Reference sera for antinuclear antibodies. II. Further definition of antibody specificities in international antinuclear antibody reference sera by immunofluorescence and Western blotting. Arthritis Rheum. 1997;40:413–418. doi: 10.1002/art.1780400304. [DOI] [PubMed] [Google Scholar]
- 6.Subcommittee for Scleroderma Criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Preliminary criteria for the classification of systemic sclerosis (scleroderma) Arthritis Rheum. 1990;21:581–590. doi: 10.1002/art.1780230510. [DOI] [PubMed] [Google Scholar]
- 7.Tan E M, Fritzler R J, McDougal J S, McDuffie F C, Nakamura R M, Reichlin M, Reiner C B, Sharp G C, Schur P H, Wilson M R, Winchester R J. Reference sera for antinuclear antibodies. I. Antibodies to native DNA, Sm, nuclear RNP, and SS-B/La. Arthritis Rheum. 1982;25:1003–1005. doi: 10.1002/art.1780250814. [DOI] [PubMed] [Google Scholar]
- 8.Tan E M. International cooperative activities in standardization of antinuclear antibodies. Manual Biol Markers Dis. 1993;A1:1–5. [Google Scholar]
- 9.Tan E M, Cohen A S, Fries J F, Masi A T, McShane D J, Rothfield N F, Schaller J G, Talal N, Winchester R J. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–1272. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 10.Tan E M, Smolen J S, McDougal J S, Butcher B T, Conn D, Dawkins R, Fritzler M J, Gordon T, Hardin J A, Kalden J R, Lahita R G, Maini R N, Rothfield N F, Smeenk R, Takasaki Y, van Venrooij W J, Wiik A, Wilson M, Koziol J A. A critical evaluation of enzyme immunoassays for detection of antinuclear autoantibodies of defined specificities. Arthritis Rheum. 1999;42:455–464. doi: 10.1002/1529-0131(199904)42:3<455::AID-ANR10>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 11.Van Venrooij W J, Charles P, Maini R N. The consensus workshops for the detection of autoantibodies to intracellular antigens in rheumatic diseases. J Immunol Methods. 1991;140:181–189. doi: 10.1016/0022-1759(91)90369-q. [DOI] [PubMed] [Google Scholar]
- 12.Van Venrooij W J, Maini R N the Consensus Finding Group for Autoantibodies. The consensus workshops for the detection of autoantibodies to intracellular antigens in rheumatic diseases. Clin Exp Rheumatol. 1992;10:507–511. [PubMed] [Google Scholar]