Abstract
Senior housing properties provide tailored lifestyle, housing, and personal care services to aging adults. Having emerged from needs-based settings, senior housing is typically viewed as a necessity. As a result, demand estimates often rely on assumed utilization rates. We use monthly data beginning in 2017 to model occupied senior housing units as a function of price and a time trend. Our two-stage least squares approach provides an estimate of senior housing’s price elasticity of demand. Results show elasticity coefficients of greater than one, implying senior housing market is more of a luxury than a necessity.
Keywords: Elasticity, Senior, Housing, Retirement
Introduction
By 2030, one-in-five people will be of retirement age in the United States, every Baby Boomer will be at least 65 years of age, and approximately 10,000 people will turn 85 each day (US Census Bureau 2020). For this population, numerous life transitions impact their housing needs. Many of these transitions are positive: an emptied nest, retirement, grandchildren, travel, and leisure. Households may want to downsize or relocate near their children or grandchildren. Other transitions, like increased frailty, healthcare episodes, the death of a spouse or caregiver, or memory loss are more serious and require some form of personal care or support. In addition to more traditional options like single- or multi-family housing, seniors have tailored housing and care options available to them. Properties marketing active adult, senior apartments, independent living, assisted living, and memory care abound and discussions around senior housing demand have reemerged. In a recent white paper, the National Investment Center for the Seniors Housing and Care Industry (NIC), projects an additional 80,000–140,000 new senior housing units will be needed to meet the demands of aging Baby Boomers by the late 2030s, an investment that could reach 100 billion dollars (National Investment Center for the Seniors Housing and Care Industry 2019).
Because the senior housing property sector emerged from needs-based settings, assessment of new market opportunities or demand traditionally assumed some percentage of need subject to an income qualification. When senior housing was a relatively new housing segment, demand exceeded supply and feasibility methods showing unmet need were naturally reinforced. Suppose a new development opportunity was evaluated in the late 1990s, constructed in 2000, opened in 2001, and became fully occupied by 2003? The needs-based methods used to assess new markets were a part of a positive feedback loop contributing to oversupply.
Our approach estimates a simple model where demand is a function of price. This allows for an estimate of price elasticities, which inform several decisions for industry stakeholders: pricing, new market selection, renovation decisions, and competitive strategy. Moreover, it allows us to examine whether senior housing is considered a necessity or luxury by its consumers. We focus on independent living units separately and combine assisted living and memory care units since both services are often combined on the same campus. Section two provides an industry background, section three reviews the relevant literature, section four discusses the methods and data, section five presents results, and section six concludes.
Industry background
Before a review of the relevant literature, some background on the senior housing property sector is helpful. The sector experienced rapid growth over the last two decades and become an increasingly competitive operating environment. Moreover, both the operators—the providers of care—and property owners are fragmented, which implies senior housing is a competitive market. In addition, there are relatively modest entry barriers. Our price elasticity of demand estimates will help assess the bargaining power of senior housing residents.
Property and unit types
As a property sector, senior housing includes independent living, assisted living, and memory care. Senior housing properties provide room, board, and care services to age-qualified residents, usually 62 or 65 and older for properties subsidized by the U.S. Department of Housing and Urban Development, and at least 75 years of age for properties charging market rates (American Seniors Housing Association 2020). In independent living units, residents pay a monthly rent for their unit, an apartment, townhome, or villa, and additional fees for dining, housekeeping, and transportation. Residents often substitute home ownership for ease of maintenance and social activities (Worzala et al. 2009). Assisted living residents pay a monthly rent for their apartment unit, meals, and community fees with additional fees commiserate with their activities of daily living needs (i.e., eating, bathing, dressing, toileting, transferring, and continence). Memory care, a subset of assisted living, provides specialized support for older adults with dementia and Alzheimer’s disease (CBRE 2017). In 2020, standalone memory care properties only represented between 6 and 7% of senior housing properties (American Seniors Housing Association). Independent living is not licensed at the state level. While assisted living and memory care are licensed by the state, only four states regulate it under a more restrictive certificate-of-need process where developers are required to demonstrate public need.
There are a few related but distinct segments as well. Active adult and senior apartments are age-restricted but provide minimal, if any, services and are traditionally considered multi-family housing. In-home care can compete with senior housing but is often more expensive than assisted living, implying a higher level of need since room and board is not provided (Genworth Financial, Inc 2022). Moreover, such services are not provided at all hours of the day, so the senior would require some support from a spouse or adult child when not provided by the home care agency. Long-term care or nursing care is provided in federally licensed healthcare facilities and is a distinct segment from senior housing (CBRE 2017; Eichholtz et al. 2007). Skilled nursing and/or nursing care facilities accept Medicare and Medicaid and provide around-the-clock (24/7) nursing care. Long-term care is available in licensed skilled nursing/nursing care facilities and is paid out-of-pocket until the resident is Medicaid eligible. Short-term rehabilitation is also provided in licensed skilled nursing facilities and is paid for by Medicare and private insurance. While long-term care can be provided within senior housing properties, it is traditionally considered more of a healthcare segment than a housing segment.
Historical performance
Today’s options available to seniors is a relatively new phenomenon. Brecht (2002) traces the emergence of specialized housing for aging adults through the twentieth century. What began as housing for elderly clergy and religious was extended to congregants who outlived their resources, and continuing care retirement communities (CCRCs) providing a full range of services emerged. Growth in life expectancies, financial resources, social support systems like Social Security and Medicare, and dual-income earning households all contributed to new housing options for aging adults. In the 1980s and 1990s, freestanding assisted living emerged from CCRCs offering a “homelike” alternative to nursing homes for residents paying out-of-pocket (Zimmerman et al. 2022; Brecht 2002). Annual senior housing inventory growth surged from about 2% in 1994 to 9% in 1999 (CBRE 2017). In fact, over half of independent living units and two-thirds of assisted living units were developed in the last 20–30 years (National Investment Center for Senior Housing and Care 2020).
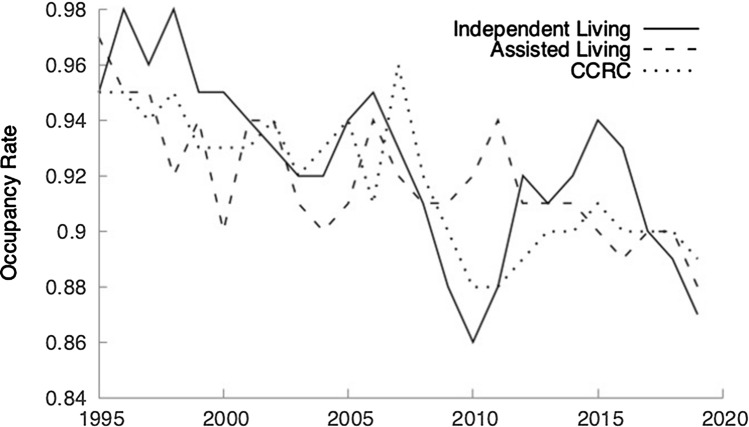
Survey data reported by the American Senior Housing Association (2020) indicate an increasingly more competitive operating environment over time. Median occupancy rates in Fig. 1 for stabilized properties, generally open for at least 2 years, declined for all property types.
Fig. 1.
Median occupancy rate, stabilized properties
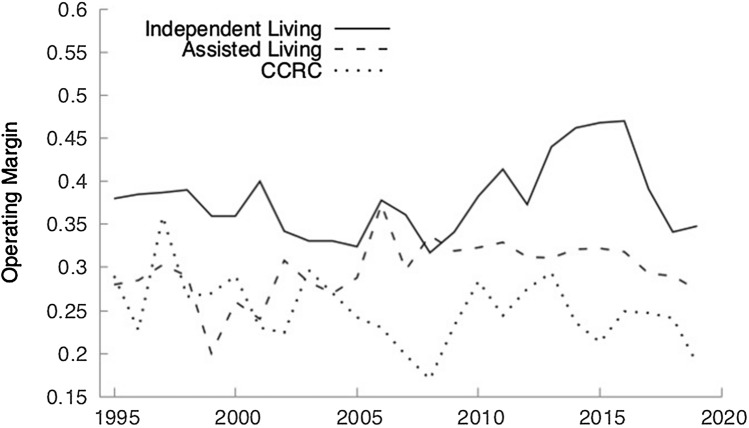
Operating margins reported by the American Senior Housing Association (2020) shown in Fig. 2 trend up following the Great Recession for independent living properties and trend down for assisted living properties and CCRCs. Given the higher levels of care in assisted living and CCRCs, the segment faces a higher, rising cost structure. State regulations require staffing ratios for nursing and care aid staff, and average hourly earnings for employees in nursing and residential care facilities increased 25% since July 2009 (Bureau of Labor Statistics 2022). The federal minimum wage remained unchanged at $7.25 per hour and offers a comparison for independent living since the services provided, food service and housekeeping for example, can be provided at lower wages.
Fig. 2.
Median operating margins
Market structure
A market share analysis for the largest senior housing operators suggests high levels of competition. Table 1 presents the market shares (in terms of units) for the top operators tracked by NIC MAP® Data Service (2020).
Table 1.
Top four senior housing operators
| Operator | Unit share (%) |
|---|---|
| Brookdale | 6 |
| Sunrise senior living | 3 |
| Atria | 3 |
| Holiday retirement | 3 |
| Four-firm concentration ratio | 14 |
While operators certainly may own the properties themselves, often there is another entity that owns the property, renting it to the operator. Investment grade senior housing and care properties had a market capitalization of $475 billion and, according to the National Council of Real Estate Investment Fiduciaries, see 3-, 5- and 10-year returns exceeding apartment, hotel, office, and retail segments (National Investment Center for Senior Housing and Care 2020). Since 2010, additional capital was attracted to the industry with the rolling four-quarter average transaction volume growing from under $2.5 billion in 2010 to $15 billion by the end of 2019 (National Investment Center for Senior Housing and Care 2020). Publicly traded real estate investment trusts (REITs) owned 26% of the total market capitalization. While ownership is more concentrated within publicly traded REITs, Table 2 shows that it is less concentrated when considering the total market capitalization.
Table 2.
Top four public senior housing REITs
| REIT | % REIT market capitalization | % Senior housing market capitalization |
|---|---|---|
| Welltower | 28% | 7% |
| Ventas | 18% | 5% |
| HealthPeak Properties, Inc. | 14% | 4% |
| Medical Properties Trust, Inc. | 9% | 2% |
| Four-firm concentration ratio | 68% | 18% |
When relating market structure to competitive strategy, the bargaining power of buyers is crucial (Porter, 2008). The price elasticity of demand helps assess buyer bargaining power. Larsen and Coleman (2014) find that seniors may be at a bargaining power disadvantage when selling their home, a critical step prior to residency in a senior housing property. Certainly, the assistance with activities of daily living offered by assisted living properties and memory support offered in memory care suggest an element of necessity in senior housing. That said, the growth in senior housing unit supply certainly gives senior housing prospects more options. We next review the relevant literature on senior housing demand and older adult migration to explore the factors influencing move-in decisions that contribute to the necessity or luxury characteristics of senior housing.
Literature review
Wiseman (1980) provides a cross-disciplinary framework of push and pull factors that clarify the tensions in older adult migration decisions. Push factors include healthcare episodes or the death of spouse and speak to the desire of older adults to remain in their current residence. Pull factors include lifestyle preferences, amenities, or location and are those current and future influences that inform a decision to move. The push/pull framework is not “either/or”; rather, it is “both/and.” Moschis et al. (2005) find that 48% of retirement community residents aged 55–64, 45% aged 65–74, and 47% aged 75 or older note the death of a spouse as one of the primary reasons for moving. For each age group, however, access to social contacts and activities ranks first (77%, 72%, and 59%, respectively). Kramer and Pfaffenbach (2016) find older adults have a strong preference for home or their immediate neighborhood, implying a preference to “age in place.”
Empirical work in real estate provides the foundations for mainstream demand analysis for the senior housing property sector, establishes support for age-qualifications, and suggests inelastic senior housing demand. Edelstein and Lacayo (1998) use 1990 census data to estimate senior housing demand using age, sex, and location (urban vs. rural) but find no overwhelming drivers. Anikeeff (1999) combines residential care and nursing care and estimates a regression model that includes population aged 65–74, 75–84, and 85 and over with a high R2. Only the population aged 85 and over is significant. Macpherson and Sirmans (1999) build five multinomial logit models to forecast older adult housing demand across five settings: no care in owner-occupied housing, no care in renter-occupied housing, assisted living, congregate care, and nursing home care. Results vary by race and sex, but older age groups generally see larger estimated coefficients for assisted living and congregate care demand. Moreover, older age is negatively associated with owner- and renter-occupied housing with no care. Doctrow et al. (1999) provide recommendations for sizing trade areas and Tessier and Mueller (1999) argue for demand adjustments incorporating likelihood of moving and unit turnover. By assuming some utilization rate, also called a penetration rate, consultants can quickly gauge the depth of demand within a given trade area. Tessier and Mueller (1999) examine resident characteristics and community demographics for varying mile radii from four assisted living communities, providing a basis for analysts to carve out trade or primary market areas like a standard 15-mile radius. Doctrow et al. (1999) also provide a high-level estimate of assisted living need that incorporates the senior population, ability to pay, and disability rates with adjustments for seniors likely to move and for unit turnover (i.e., seniors moving out of units).
Chiu and Ho (2006) estimate elderly housing demand in Hong Kong after accounting for latent demographic trends, preferences, and housing arrangements. They find that public rental housing was preferred regardless of ability to afford. Gibler and Sherwood Clements III (2010) develop a logistic regression using age, race, marital status, education, and income as independent variables. While findings indicate increasing age drives a move into senior housing, the model lacks explanatory power with a pseudo R2 of 0.07 (Gibler and Sherwood Clements III 2010). DeLellis et al. (2012) estimate county-level nursing home utilization in Michigan and find age and income as key drivers amongst other demographic controls with income being negatively related to utilization, which implies needs-based settings are inferior goods.
Empirical work on aging and housing in economics generally focuses on household migration or housing transitions. Household migration research suggests elastic senior housing demand while housing transition literature suggests inelastic demand. The literature on age-specific migration extends from Tiebout (1956) who hypothesizes that households seek to maximize some bundle of amenities and public goods in deciding where to reside. Graves and Linneman (1979) develop and test a consumption-oriented model of migration for location-specific goods in the framework of lifetime utility. Changes in demand for a location-specific good create an incentive to migrate where some households migrate and those that remain are in some way compensated because utility must be equal across alternative locations in equilibrium (Graves and Linneman 1979). For example, households may be compensated in the form of lower rents when farther away from desirable amenities, implying some level of substitutability in housing locations.
Interesting findings emerged from migration research and point to Wiseman’s (1980) pull factors. In contrast to the popularly held belief that retirees flock to warmer weather destinations, Graves (1979) finds retirees are not particularly deterred by cold weather, perhaps indicating a preference to relocate near children and grandchildren. Clark and Hunter (1992) confirm adding that older adults prefer locations with amenities better fitting to their lifestyles indicating a preference for daytime activities in contrast to nighttime activities. Conway and Houtenville (2001) incorporate local taxes into a migration flow model and find a preference for lower tax states amongst the elderly.
Housing transition literature in economics suggests inelastic senior housing demand often highlighting the impact of push factors in housing transitions. Since strongly negative shocks are never desired, seldom expected, and rarely planned for, the housing transition becomes more of a necessity than a luxury. Jones (1997) finds that elderly households sell their homes only when “wealth-impairing” events occur. Another line of research suggests that only the most severe healthcare episodes or life events (i.e., death of a spouse) prompt housing transitions (Feinstein and McFadden 1989; Feinstein and Ho 2001; Venti and Wise 2001, 2004). Engelhardt and Greenhalgh-Stanley (2010) confirm while studying shifts in Medicare’s home health benefits showing that even moderately negative shocks to health and functionality do not notably impact home ownership among the elderly.
We add to the literature by estimating the price elasticity of senior housing demand. By placing push/pull factors in an elasticity framework and controlling for longer-run trends, we can isolate the impact of price on senior housing demand. Doing so enables an analysis of whether push factors dominate, implying inelastic demand, or if pull factors dominate, implying elastic demand.
Data and methods
Our occupied units model at a fixed point in time (t) begins with a constant-elasticity demand function.1
| 1 |
where A is a positive constant and ε is the price elasticity of demand. A linearized version is below.
| 2 |
The data are a monthly time series beginning in January 2017 through March 2022 (63 months) from a sample of market rate, investment grade properties and operators tracked by NIC MAP® Data Service’s Senior Housing Actual Rates initiative. The sample represents approximately 23% of comparable properties and 36% of comparable units.2 Metrics tracked include occupancy rate, move-ins and move-outs as a percent of existing unit supply, and three price metrics. The price metrics include monthly asking rent, rent for the first month of occupancy, and the monthly in-place rent beginning in the second month of occupancy. All rent metrics include room, board, and care fees where applicable.
The advantage of this dataset is a more precise estimate of price (rent). Other cross-sectional and panel datasets from NIC MAP® Data Service only contain asking rents. As a result, we calculate unit supply using Q4:2019 unit counts from the NIC Investment Guide, 6th Edition and subtract tract out units opened in years prior by incorporating the average proportion of units opened by month from 2010 to 2016 to allocate new units across months within a given year. NIC MAP® Data Service tracks properties in 140 U.S. metro areas.
Occupied units, our demand variable, is calculated using occupancy rate and unit supply in a given month (t).
| 3 |
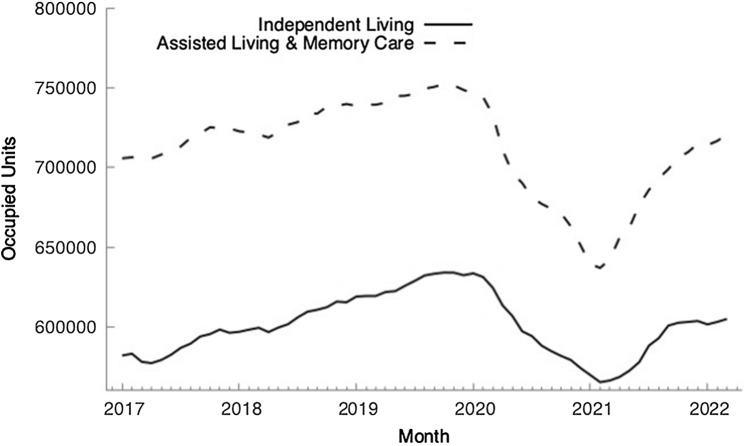
For the time series, Fig. 3 shows an upward trend in occupied units for both independent living and assisted living/memory care which began to taper before 2020. During Covid-19, occupied units plummeted until January 2021 and then began to recover with the introduction of vaccines.
Fig. 3.
Occupied units
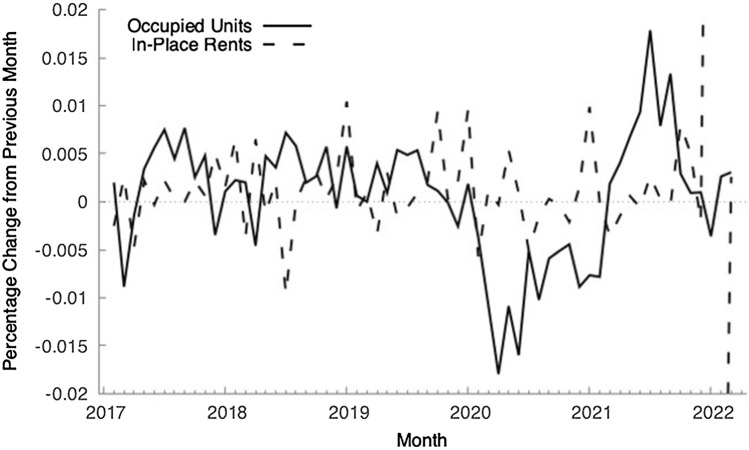
Like occupied units, the time series of in-place rents in Fig. 4 indicates an upward trend. In fact, unit root tests in Tables 7 and 8 of the Appendix suggest the log of occupied units and log of rent are nonstationary, raising concerns of a spurious regression (Granger and Newbold 1974).
Fig. 4.
Log of in-place rents
Table 7.
Independent living ADF-GLS unit root test
| H0: series has a unit root | |
|---|---|
| Levels | |
| Log occupied units | − 0.99 |
| Log rent | 1.01 |
| First differences | |
| Log occupied units | − 3.31*** |
| Log rent | − 11.04*** |
Statistically significant at the *** 1% level ** 5% level * 10% level
February 2017–February 2020 (T = 37)
Table 8.
Assisted living/memory care ADF-GLS unit root test
| H0: Series has a unit root | |
|---|---|
| Levels | |
| Log occupied units | − 0.18 |
| Log rent | − 0.13 |
| First differences | |
| Log occupied units | − 1.99* |
| Log rent | − 5.64*** |
Statistically significant at the *** 1% level ** 5% level * 10% level
February 2017–February 2020 (T = 37)
As a result, we compare the log-differences in rental rates with occupied units to purge inflation and overall demographic trends from the analysis. Figures 5 and 6 compare month-to-month percentage changes (log-differences) in occupied units and rental rate growth. Spikes in rental rate growth are associated with demand declines in early 2017, early 2018, and again in late 2019 and early 2020. During Covid-19, occupied units declined month-to-month until early 2021. For both occupied units and rents, Covid-19 was a volatile period.
Fig. 5.
Independent living | occupied units vs. in-place rent, log-differenced
Fig. 6.
Assisted living/memory care | occupied units vs. in-place rent, log-differenced
Assessing the log-differences helps explain variations around the trendline but hides the impact of demographic growth, tastes and preferences, and overall economic activity. Our approach estimates the price elasticity of demand using a constant-elasticity demand function. To specify a constant-elasticity demand curve, we use a double-log form of the undifferenced series for both occupied units and rent (Figs. 7, 8).
Fig. 7.
Independent living, log of occupied units vs. log of in-place rents
Fig. 8.
Assisted living/memory care, log of occupied units vs. log of in-place rents
Because we are using the undifferenced series for occupied units and rent, the series must be cointegrated in order to draw any conclusions from the model. The results from Engle-Granger tests for the log of occupied units and log of rent (from the first stage) in Table 9 of the Appendix allow us to reject the null hypothesis that the cointegrating regression equations have a unit root. As a result, the time series for independent living and assisted living/memory care are cointegrated, and we can reliably use the undifferenced series.
Table 9.
Engel–Granger cointegration test
| Without constant | |
|---|---|
| H0: residuals from cointegrating regression have a unit root | |
| Independent living | Assisted living/memory care |
| − 3.354** | − 4.380*** |
Statistically significant at the *** 1% level ** 5% level * 10% level
February 2017–February 2020 (T = 37)
A time trend controls for demographic influences, tastes and preferences, and the overall economy. Because price (rent) and quantity demanded (occupied units) are simultaneously determined, we use two-stage least squares. Our rent variable is the log of in-place rent, which is the average rent paid by residents who have at least completed their second month of occupancy because the first month often contains discounts and move-in incentives. To instrument log rent in the first stage, we use the time trend, a relevant labor force variable, and lagged log of occupied units (Reed 2015). The time trend in the first stage controls for inflation. The labor force variable is the first difference of the continuing care retirement and assisted living community workforce in Florida, New York, New Jersey, and California from the U.S. Bureau of Labor Statistics (2022) and the Federal Reserve Bank of St. Louis (2022). We also limit the time period to the pre-Covid portion of the time series given the volatility and operational shocks during Covid-19.
Our model is below, and Table 3 describes the variables.
| 4 |
Table 3.
Descriptive statistics
| Variables | Independent living | Assisted living/memory care | ||
|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | |
| Dependent | ||||
| Log occupied units | 13.321 | 0.029 | 13.504 | 0.019 |
| Independent | ||||
| Log rent | expected sign: (–) | 8.083 | 0.015 | 8.588 | 0.019 |
| Time trend | expected sign: (+) | February 2017–February 2020 (T = 37) | |||
Results
The independent living demand model explains 95% of the variability in occupied units. The coefficients for the independent variables are statistically significant and are of the expected signs. Holding rent constant, each additional month sees a 0.005% increase in occupied units. Holding time constant, a 1% increase in rent is associated with a 1.6% decline in occupied units. This implies a price elasticity of demand of 1.6, which indicates elastic independent living demand (Table 4).3
Table 4.
Independent living demand model
| Independent variable | Coefficient estimate | Standard error | |
|---|---|---|---|
| Constant | 26.125 | 6.797 | *** |
| Log rent | − 1.597 | 0.844 | * |
| Time period | 0.005 | 0.001 | *** |
| Mean-dependent variable | 13.317 | S.D dependent variable | 0.03 |
| Sum squared residuals | 0.001 | S.E. of regression | 0.007 |
| R2 | 0.956 | Adjusted R2 | 0.954 |
| F(2,34) | 368.059*** | ||
| Test | H0 | p-value |
|---|---|---|
| Jarque–Bera | Error normally distributed | 0.46 |
| Pesaran–Taylor Heteroskedascticity | Heteroskedasticity not present | 0.59 |
| LM | No autocorrelation | 0.34 |
| Hausman | OLS estimates are consistent | 0.03 |
Statistically significant at the *** 1% level ** 5% level * 10% level
The residuals are normally distributed, the Pesaran–Taylor test indicates heteroskedasticity is not present, and the LM test indicates no autocorrelation. The Hausman test indicates that two-stage least squares is appropriate. Since the time series for the natural log of occupied units and rent are cointegrated, modeling the levels of the variables is reliable.
The assisted living and memory care model explains 71% of the variability in occupied units. The coefficients for the independent variables are statistically significant and are of the expected signs. Holding rent constant, each additional month sees a 0.004% increase in occupied units. Holding time constant, a 1% increase in rent is associated with a 1.7% decline in occupied units. This implies a price elasticity of demand of 1.7, which indicates elastic-assisted living and memory care demand (Table 5).4
Table 5.
Assisted living & memory care demand model
| Independent variable | Coefficient estimate | Standard error | |
|---|---|---|---|
| Constant | 27.615 | 5.052 | *** |
| Log rent | − 1.654 | 0.591 | *** |
| Time period | 0.004 | 0.001 | *** |
| Mean-dependent variable | 13.504 | S.D dependent variable | 0.019 |
| Sum squared residuals | 0.005 | S.E. of regression | 0.012 |
| R2 | 0.721 | Adjusted R2 | 0.705 |
| F(2,32) | 24.355*** | ||
| Test | H0 | p-value |
|---|---|---|
| Jarque–Bera | Error normally distributed | 0.07 |
| LM test | No autocorrelation | 0.67 |
| Hausman test | OLS estimates are consistent | 0 |
Statistically significant at the *** 1% level ** 5% level * 10% level
Estimated using Robust Standard Errors
The assisted living/memory care model is estimated using robust standard errors because a Pesaran–Taylor test indicated heteroskedasticity was present. The Hausman test indicates that two-stage least squares is appropriate. An LM test indicates no autocorrelation is present. Like independent living, the time series for the natural log of occupied units and rent are cointegrated and modeling the undifferenced series is appropriate.
The models predict reasonably well with a mean absolute percentage error of 3.9% for independent living and 6.7% for assisted living/memory care. Taking the anti-log of the mean for each predicted value allows us to translate the results back into terms of units. The independent living mean is 609,869 units compared to an actual mean of 609,820 for the time series. Assisted living/memory care’s is 732,340 compared to 732,510 for the time series (Table 6).
Table 6.
Descriptive statistics for predicted values
| Setting | Mean | Standard deviation | MAPE (%) | Anti-log of mean |
|---|---|---|---|---|
| Independent living | 13.321 | 0.028 | 3.90 | 609,869 |
| Assisted living/memory care | 13.504 | 0.215 | 6.70 | 732,340 |
MAPE mean absolute percentage error
Conclusion
Because our aim is to estimate the price elasticity of demand, we are particularly concerned with potential sources of bias in the estimated coefficients. Our demand models are simple, so there is the potential for omitted variable bias. Nevertheless, evidence suggests that the risk of such bias is small. First, metrics related to economic activity, housing markets, and substitutes also follow a trend pattern, which is included in the model. Second, unexpected push factors like a healthcare episode or death of a spouse or caregiver that prompt a move into senior housing are unrelated with economic activity and housing markets, so the impact of omitted variables is mitigated. Third, senior housing units are occupied, by and large, by retired, elderly persons living off retirement savings and pensions and are relatively insulated from economic pressures. Fourth, while in-home care or homemaker services provided by home care agencies can compete with senior housing, the senior would still require assistance from a spouse or adult child and would likely have not yet entered Wiseman’s (1980) push/pull framework. Finally, the alternative models that account for the influence of substitutes in Tables 10 and 11 in the Appendix still show elastic demand.
Table 10.
Alternative independent living demand model
| Independent variable | Coefficient estimate | Standard error | |
|---|---|---|---|
| Constant | 23.62 | 5.982 | *** |
| Log rent | − 1.285 | 0.743 | * |
| Time period | 0.004 | 0.001 | *** |
| Home Price Index, first difference | − 0.0004 | 0.001 | |
| Mean-dependent variable | 13.317 | S.D dependent variable | 0.03 |
| Sum squared residuals | 0.001 | S.E. of regression | 0.006 |
| R2 | 0.968 | Adjusted R2 | 0.965 |
| F(3,33) | 331.100*** | ||
| Test | H0 | p-value |
|---|---|---|
| Jarque–Bera | Error normally distributed | 0.65 |
| Pesaran–Taylor Heteroskedascticity | Heteroskedasticity not present | 0.2 |
| LM | No autocorrelation | 0.45 |
| Hausman | OLS estimates are consistent | 0.11 |
Statistically significant at the *** 1% level ** 5% level * 10% level
Table 11.
Alternative-assisted living/memory care demand model
| Independent variable | Coefficient estimate | Standard error | |
|---|---|---|---|
| Constant | 31.425 | 8.55 | *** |
| Log rent | − 2.1 | 1 | ** |
| Time period | 0.005 | 0.002 | *** |
| Home care emp., first difference | 0.001 | 0.001 | |
| Mean-dependent variable | 13.504 | S.D dependent variable | 0.019 |
| Sum squared residuals | 0.007 | S.E. of regression | 0.015 |
| R2 | 0.615 | Adjusted R2 | 0.578 |
| F(3,31) | 9.472*** | ||
| Test | H0 | p-value |
|---|---|---|
| Jarque–Bera | Error normally distributed | 0.17 |
| LM test | No autocorrelation | 0.12 |
| Hausman test | OLS estimates are consistent | 0 |
Statistically significant at the *** 1% level ** 5% level * 10% level
Estimated using Robust Standard Errors
We conclude, therefore, that demand for independent living and assisted living/memory care units is price elastic. As such, occupied units show a more than proportional response to a change in price. There are several practical applications of the estimated price elasticities across independent living and assisted living/memory care. First, a simple model of demand is explanatory, accurate, and intuitive. Local market research for new senior housing developments, however, defines demand using some age-, income-, and frailty-qualified householder assumptions, which presumes senior housing is more of a necessity than a luxury. As a result, more nuanced analysis, especially on pricing, the local competition, and prospect tastes and preferences is warranted. Second, our results show that senior housing is a competitive industry. As previously examined, the four firm concentration ratios for owners (18%) and operators (14%) of senior housing properties are low and unit inventory grew rapidly over the last few decades. When placed in a Porter’s “five forces” framework, our elasticity estimates imply relatively strong bargaining power of buyers compared to suppliers (Porter 2008). Finally, the results imply a shift from a needs-based or necessity-based focus to a service- and lifestyle-based focus in design, development, operations, and marketing of senior housing properties.
As more data points are added further research might consider structural breaks in the time series and test elasticities following Covid-19’s pre-vaccine trough. Once the volatility settles, it is possible that the slope of the trend changes. Moreover, cross-sectional data allows for incorporation of more local influences. This would enable analysts to derive new methodologies for a more service- and lifestyle-based senior housing property sector and better position operators facing a competitive industry with declining profit margins.
Acknowledgements
The author would like to thank Dr. James McGibany for helpful comments on an early draft. All errors are my own.
Notes
This paper received the 2022 NABE Contributed Paper award.
Daniel G. Lindberg
is the principal of Applied Economic Insight LLC, a boutique consultancy providing analytic and econometric services to owners, operators, and developers of multi-family, senior housing, and healthcare real estate. He has a Master of Science in Applied Economics and is also an instructor of practice at Marquette University teaching courses in business analytics and microeconomics.
Appendix
Footnotes
Varian (2014, p. 283) provides an overview of constant-elasticity demand curves.
Total count for comparable units and properties derived from Table IV in Appendix III in Harris-Kojetin et al. (2019).
To test the robustness of elastic demand, the first difference for the S&P/Case-Schiller U.S. National Home Price Index was added in an alternative model because a senior’s current home substitutes for independent living. In this model, independent living’s price elasticity of demand estimate is 1.3. Please refer to Table 10 in the Appendix.
To test the robustness of elastic demand, the first difference for home care agency employment was added in an alternative model to account for the influence of in-home care as a substitute to assisted living and memory care. In this model, assisted living and memory care’s price elasticity of demand estimate is 2.1. Please refer to Table 11 in the Appendix.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Anikeef Michael A. Estimating the Demand for Seniors Housing and Home Health Care. Journal of Real Estate Portfolio Management. 1999;5(3):247–258. doi: 10.1080/10835547.1999.12089580. [DOI] [Google Scholar]
- American Seniors Housing Association. 2020. The State of Seniors Housing. Retrieved from www.seniorshousing.org
- Brecht Susan. Analyzing Seniors’ Housing Markets. Washington, D.C.: ULI-the Urban Land Institute; 2002. [Google Scholar]
- CBRE. 2017. Senior Housing and Care Market Insight: 2017 Q2 Review. Retrived from www.cbre.com/nationalseniorhousing.
- Chiu Rebecca, Ho Michael. Estimation of Elderly Housing Demand in an Asian City: Methodological Issues and Policy Implications. Habitat International. 2006;30:965–980. doi: 10.1016/j.habitatint.2005.08.001. [DOI] [Google Scholar]
- Clark David E, Hunter William J. The Impact of Economic Opportunity, Amenities and Fiscal Factors on Age-Specific Migration Rates. Journal of Regional Science. 1992;32(3):349–365. doi: 10.1111/j.1467-9787.1992.tb00191.x. [DOI] [Google Scholar]
- Conway Karen S, Houtenville Andrew J. Elderly Migration and State Fiscal Policy: Evidence from the 1990 Census Migration Flows. National Tax Journal. 2001;54(1):103–123. doi: 10.17310/ntj.2001.1.05. [DOI] [Google Scholar]
- DeLellis Nailya O, Manthei Lauren, Woodworth Jacob. Predicting Nursing Home Utilization at the County Level in Michigan: Influence of Demographic and Market Variables. Seniors Housing & Care Journal. 2012;20(1):35–44. [Google Scholar]
- Doctrow J, Mueller G, Craig L. Survival of the Fittest: Competition, Consolidation and Growth in the Assisted Living Industry. Journal of Real Estate Portfolio Management. 1999;13(3):225–234. doi: 10.1080/10835547.1999.12089581. [DOI] [Google Scholar]
- Edelstein Robert H, Lacayo Allan J. Forecasting Seniors Housing Demand. In: Anikeeff Michael A, Mueller Glenn R., editors. Seniors Housing, Research Issues in Real Estate. Boston, MA: Springer; 1998. pp. 205–235. [Google Scholar]
- Eichholtz Piet M.A., Kok N, Wolnicki BG. Who Should Own Senior Housing? The Journal of Real Estate Portfolio Management. 2007;13(3):205–218. doi: 10.1080/10835547.2007.12089782. [DOI] [Google Scholar]
- Engelhardt Gary V, Greenhalgh-Stanley Nadia. Home Health Care and the Housing and Living Arrangements of the Elderly. Journal of Urban Economics. 2010;67:226–238. doi: 10.1016/j.jue.2009.09.007. [DOI] [Google Scholar]
- Feinstein, Jonathan, and Daniel McFadden. 1989. The dynamics of housing demand by the elderly: Wealth, cash flow, and demographic effects. The economics of aging, 55–86.
- Feinstein, Jonathan, and Chin-Chin Ho. 2001. Elderly asset management and health. In Rethining Estate and Gift Taxation, ed. Gale W. Hines, J., and Slemrod, J., 457–498. Washington DC: Brookings Institution Press.
- Genworth Financial, Inc. 2022. Genworth Cost of Care Survey. Retrieved from www.genworth.com.
- Gibler Karen M, Sherwood Clements III J. Testing a Forecast Model to Predict Movement of Older Americans into Retirement Housing. International Journal of Housing Markets and Analysis. 2011;4(1):18–30. doi: 10.1108/17538271111111811. [DOI] [Google Scholar]
- Granger CWJ, Newbold P. Spurious Regression in Econometrics. Journal of Econometrics. 1974;2:111–120. doi: 10.1016/0304-4076(74)90034-7. [DOI] [Google Scholar]
- Graves Philip E. A Life-Cycle Empirical Analysis of Migration and Climate, by Race. Journal of Urban Economics. 1979;6:135–147. doi: 10.1016/0094-1190(79)90001-9. [DOI] [PubMed] [Google Scholar]
- Graves, Phillip E. and P. D. Linneman. 1979. Household Migration: Theoretical and Empirical Results, Journal of Urban Economics 6 (3): 383–404. [DOI] [PubMed]
- Harris-Kojetin, Lauren D., Manisha Sengupta, Jessica Penn Lendon, Vincent Rome, Roberto Valverde, and Christine Caffrey. 2019. Long-term care providers and services users in the United States, 2015–2016. National Center for Health Statistics. Vital Health & Statistics 3(43). Retrieved from www.cdc.gov/nchs/data/series/sr_03/sr03_43-508.pdf. [PubMed]
- Jones Lawrence D. The Tenure Transition Decision for Elderly Homeowners. Journal of Urban Economics. 1997;41:243–263. doi: 10.1006/juec.1996.1099. [DOI] [Google Scholar]
- Kramer Caroline, Pfaffenbach Carmella. Should I Stay or Should I Go? Housing Preferences upon Retirement in Germany. Journal of Housing and the Built Environment. 2016;31(2):239–256. doi: 10.1007/s10901-015-9454-5. [DOI] [Google Scholar]
- Larsen James E, Coleman Joseph W. Senior Citizen’s Bargaining Power in Residential Real Estate Markets. International Journal of Housing Markets and Analysis. 2014;7(1):5–17. doi: 10.1108/IJHMA-09-2012-0047. [DOI] [Google Scholar]
- Macpherson David A., Stacy Sirmans G. Forecasting Seniors Housing Demand in Florida. Journal of Real Estate Portfolio Management. 1999;5(3):259–274. doi: 10.1080/10835547.1999.12089587. [DOI] [Google Scholar]
- Moschis George, Bellenger Danny, Curasi Carolyn. Marketing Retirement Communities to Older Consumers. Journal of Real Estate Practice and Education. 2005;8(1):99–113. doi: 10.1080/10835547.2005.12091608. [DOI] [Google Scholar]
- National Investment Center for Senior Housing and Care. 2019. Looking into the Future: How Much Seniors Housing Will Be Needed?. Retrieved from www.nic.org.
- National Investment Center for Senior Housing and Care. 2020. NIC Investment Guide: Investing in Seniors Housing and Care Properties, 6th Edition. Retrieved from www.nicmap.org.
- Porter Michael E. The Five Competitive Forces That Shape Strategy. Harvard Business Review. 2008;86:78–93. [PubMed] [Google Scholar]
- Reed William Robert. On the Practice of Lagging Variables to Avoid Simultaneity. Oxford Bulletin of Economics and Statistics. 2015;77(6):897–905. doi: 10.1111/obes.12088. [DOI] [Google Scholar]
- S&P Dow Jones Indices LLC, S&P/Case-Shiller U.S. National Home Price Index [CSUSHPISA]. Retrieved from FRED, Federal Reserve Bank of St. Louis, https://fred.stlouisfed.org/series/CSUSHPISA.
- Eleanor Tessier, Mueller Glen R. Trade Area Demand Analysis for Private Pay Assisted Living Facilities. Journal of Real Estate Portfolio Management. 1999;5(3):275–286. doi: 10.1080/10835547.1999.12089589. [DOI] [Google Scholar]
- Tiebout C. A Pure Theory of Local Expenditures. Journal of Political Economy. 1956;64(5):416–424. doi: 10.1086/257839. [DOI] [Google Scholar]
- U.S. Bureau of Labor Statistics and Federal Reserve Bank of St. Louis. 2022. All Employees: Education and Health Services: Continuing Care Retirement Communities and Assisted Living Facilities for the Elderly in California [SMU06000006562330001SA]. Retrieved from FRED, Federal Reserve Bank of St. Louis, https://fred.stlouisfed.org/series/SMU06000006562330001SA.
- U.S. Bureau of Labor Statistics and Federal Reserve Bank of St. Louis. 2022. All Employees: Education and Health Services: Continuing Care Retirement Communities and Assisted Living Facilities for the Elderly in Florida [SMU12000006562330001SA]. Retrieved from FRED, Federal Reserve Bank of St. Louis, https://fred.stlouisfed.org/series/SMU12000006562330001SA.
- U.S. Bureau of Labor Statistics and Federal Reserve Bank of St. Louis. 2022. All Employees: Education and Health Services: Continuing Care Retirement Communities and Assisted Living Facilities for the Elderly in New Jersey [SMU34000006562330001SA]. Retrieved from FRED, Federal Reserve Bank of St. Louis, https://fred.stlouisfed.org/series/SMU34000006562330001SA.
- U.S. Bureau of Labor Statistics and Federal Reserve Bank of St. Louis. 2022. All Employees: Education and Health Services: Continuing Care Retirement Communities and Assisted Living Facilities for the Elderly in New York [SMU36000006562330001SA]. Retrieved from FRED, Federal Reserve Bank of St. Louis, https://fred.stlouisfed.org/series/SMU36000006562330001SA.
- U.S. Bureau of Labor Statistics. 2022. All Employees, Home Health Care Services [CES6562160001]. Retrieved from FRED, Federal Reserve Bank of St. Louis, https://fred.stlouisfed.org/series/CES656216000.
- Varian, Hal R. 2014. Intermediate Microeconomics with Calculus: A Modern Approach. New York :W.W. Norton & Co.
- Venti, Steven F., and David A. Wise. 2001. Aging and housing equity. In Innovation for Financing Retirement Mitchell, O., Bodie, Z., Hammond, P., and Zeldes, S. (Eds.), pp. 254-281. University of Pennsylvania Press, Philadelphia
- Venti, Steven F., and David A. Wise. 2004. Aging and housing equity: Another look. In Perspectives on the Economics of Aging, pp. 127–180. University of Chicago Press
- Vespa, J., Armstrong, D.M. and Medina, L. Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports, P25-1144, U.S. Census Bureau, Washington, DC, 2020.
- Wiseman RF. Why Older People Move; Theoretical Issues. Research on Aging. 1980;2(2):141–154. doi: 10.1177/016402758022003. [DOI] [Google Scholar]
- Worzala Elaine, Karofsky JF, Davis JA. The Senior Living Property Sector: How is it Perceived by the Institutional Investor? The Journal of Real Estate Portfolio Management. 2009;15(2):141–156. doi: 10.1080/10835547.2009.12089839. [DOI] [Google Scholar]
- Sheryl Zimmerman, Carder Paula, Schwartz Lindsay, Silbersack Johanna, Temkin-Greener Helena, Thomas Kali S, Ward Kimberly, et al. The Imperative to Reimagine Assisted Living. Journal of the American Medical Directors Association. 2022;23:225–234. doi: 10.1016/j.jamda.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]