Abstract
The COVID-19 pandemic is a global mental health crisis that disproportionately impacts adolescents. Loneliness is a particularly salient pandemic psychosocial outcome to understand; however, research to date on this outcome is sparse and largely cross-sectional. In response, we examined pre-pandemic risk factors for pandemic loneliness. Further, we examined how risk may differ based on key demographics, and whether mediation or moderation models best explained potential disparities in experiencing loneliness. Self-reported, pre-pandemic mental health, trauma exposure, and family conflict survey data were collected at Wave 1 in a diverse sample of 369 adolescents (54.5% female, 45.5% male; 30.1% White; 30.9% Black; 18.4% Hispanic; Mage = 15.04; SDage = 1.10). Subsequently, self-reported experiences of loneliness during the pandemic were collected 6 months (April-June 2020) and 12 months (October-December 2020) later. Using a regression-based framework (i.e., PROCESS), we tested (a) which pre-pandemic risks uniquely predicted prospective loneliness and (b) whether loneliness risk was elevated for certain identities (i.e., mediation models) or whether certain identities were more sensitive to specific risks (i.e., moderation models). Overall, pre-pandemic depressive and aggression symptoms predicted early pandemic loneliness (6-month follow-up), whereas anxiety symptoms specifically predicted mid-pandemic loneliness (12-month follow-up). Environmental stressors were moderated by gender, such that females with pre-pandemic trauma exposure were more likely to report pandemic loneliness. Further, pre-pandemic internalizing distress for girls and externalizing symptoms for boys, reflected gender-specific pathways for loneliness. Implications for mental health prevention in the wake of national disasters are discussed.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12187-022-09984-8.
Keywords: COVID-19, Loneliness, Longitudinal, Developmental psychopathology
Introduction
In March 2020, the World Health Organization (World Health Organization, 2020) deemed COVID-19 a worldwide pandemic. Subsequently, necessary societal restrictions were installed to contain transmission within the United States (Ren, 2020). These restrictions disrupted daily activities and introduced new stressors within families (e.g., Adalja et al., 2020; Guessoum et al., 2020). These stressors have contributed to rising mental health concerns, in particular, adolescent psychological distress (e.g., Leeb et al., 2020; Patrick et al., 2020). In fact, the Surgeon General recently issued a warning for a youth mental health crisis in response to the COVID-19 pandemic (Richtel, 2021). Despite these developments, studies examining psychological sequelae among youth is lacking, with investigators (e.g., Racine et al., 2020) and organizations (e.g., United Nations, 2020) emphasizing the need to fill this gap. In response, the current study examined pre-pandemic predictors of loneliness, a critical and transdiagnostic mental health concern (Loades et al., 2020), during the pandemic in a diverse adolescent sample.
Loneliness during the COVID-19 Pandemic
Loneliness is defined as the discrepancy between adolescents’ actual and desired amount of social interaction (i.e., Perlman & Peplau, 1981), or the situation in which social needs are unfulfilled (Weiss, 1973). Loneliness is a normative state encompassing cognitive and affective components (deJong-Gierveld, 1987), with rates of loneliness demonstrating increasing trends worldwide (Twenge et al., 2021). However, when experienced for a long duration, loneliness is associated with a number of poor psychological adjustment outcomes among youth, including disruptions in sleep (Harris et al., 2013) and a higher frequency of suicide attempts (Schinka et al., 2013). Despite these findings, it is important to note that recent empirical literature has called for greater clarity in identifying risk mechanisms that lead to, and ameliorate, loneliness (Osborn et al., 2021). In response, investigators conceptualize loneliness as both an outcome, as well as a risk pathway for various forms of distress and impairment.
With regard to the COVID-19 pandemic, stay at home orders and social distancing have been hypothesized to contribute toward elevated levels of loneliness (Loades et al., 2020). It is estimated that adolescents may be uniquely vulnerable to experience loneliness during this pandemic (Beam & Kim, 2020; Groarke et al., 2020). During the early stages of the pandemic, opportunities to interact with family members were affiliated with lower levels of loneliness (Ellis et al., 2020). Others built upon these findings by demonstrating that emotional difficulties (i.e., internalizing distress) and conduct problems/hyperactivity-inattention (i.e., externalizing distress), were positively related to loneliness, while better familial relationships were inversely associated with levels of loneliness (Cooper et al., 2021). Although these studies provide some insight into this increasingly important outcome during the ongoing public health crisis, the scope of these findings are limited to concurrent associations. Prior investigations examining the psychological impact of public health crises have emphasized the significance of pre-crisis risk factors on mental health sequelae (e.g., Cohen et al., 2016), suggesting that the current lack of empirical work on longitudinal relations may render an incomplete picture of who is most vulnerable to pandemic-related loneliness.
Risk Mechanisms for Pandemic-Related Loneliness
A review of the theoretical literature (e.g., Vanhalst et al., 2014) highlights a number of intrapersonal and environmental processes contributing to experiences of loneliness in adolescence. At the individual level, psychological distress, including externalizing and internalizing symptoms are associated with relational tendencies that may disrupt the formation of healthy relationships (e.g., poor emotional regulation leading to hostility; Muris et al., 2003). Links between loneliness and depression appear particularly robust across adolescent identities, with depressive symptoms prospectively associated with higher levels of loneliness across community and at-risk youth samples (Lalayants & Prince, 2015; Schinka et al., 2013). Meanwhile, complementary research suggests anxiety and externalizing symptoms may lead to experiences of loneliness in adolescence via pathways unique from depression (e.g., London et al., 2007). During the COVID-19 pandemic, loneliness was uniquely associated with concurrent internalizing and externalizing symptoms (Cooper et al., 2021), suggesting unique relations between mental health subtypes and perceived isolation during the pandemic. The present study sought to build off these findings by examining the prospective relations between mental health and pandemic loneliness, and identifying if specific symptom subtypes lead to loneliness.
With regard to environment, trauma history and family relationships serve as salient predictors of loneliness. For instance, Matthews et al. (2022) found that potentially traumatic events (i.e., bullying) experienced throughout childhood predicted loneliness during adolescence. As for family contexts, previous investigators have demonstrated that perceived negative interactions with caregivers predict behaviors (e.g., withdrawal; Adams & Laursen, 2007) that may engender loneliness. While these findings explicate the relation between either trauma history or family environments for loneliness, they leave unanswered questions about incremental validity. Specifically, whether trauma history and family environments, along with psychological distress, confer incremental insight into adolescent loneliness. In addition, given the paucity of research examining the impacts of these contexts on COVID-19 pandemic adjustment outcomes (e.g., Harriger et al., 2021; Liu et al., 2021), further empirical evidence is needed to determine the validity of these relations as they exist within the current crisis.
Demographic Considerations
Historically, disasters exacerbate mental health disparities among racial and ethnic minority youth (e.g., La Greca et al., 1998; Lonigan et al., 1991), and COVID-19 may not be an exception (Condon et al., 2020). Most research concerning racial/ethnic mental health disparities posits a mediation model (e.g., Birkett et al., 2014; Reisner et al., 2015), in which exposure to elevated stressors explains increased mental health risk. For example, given longstanding patterns of racial/ethnic income inequality in the United States (Manduca, 2018), Black or Hispanic adolescents may be disproportionately exposed to potentially traumatic events. Consistent with the “double jeopardy” hypothesis (Widom et al., 2013), these experiences may leave youth less-equipped to regulate emotional responses to the pandemic. As for gender, epidemiological studies have consistently delineated higher rates of internalizing symptoms among adolescent girls compared to adolescent boys (e.g., Anderson & Mayes, 2010; Merikangas et al., 2010; Ramos et al., 2003). Within the context of the present study, this may suggest that females are more at-risk for loneliness during COVID-19 due to heightened pre-existing levels of emotional distress (i.e., support for a mediation model).
An alternative risk model for explaining potential mental health disparities is via moderation, such that greater sensitivity to particular stressors may render some individuals susceptible to higher levels of distress. The moderating effect of race/ethnicity on disaster-related stressors for adolescent mental health symptoms is inconclusive, possibly due to sample size issues (e.g., Rubens et al., 2018). In contrast, due to a myriad of biological, developmental, and social reasons, adolescent girls tend to demonstrate more sensitivity to certain types of stressors, such as parent–child conflict (Weymouth et al., 2016) compared to adolescent boys (Rudolph, 2002). This disparity in sensitivity may provide a useful explanation for the higher burden of post-disaster sequelae among adolescent girls (Cheng et al., 2018). Given the different translational implications conferred by a mediation or moderation model (Cole & Turner, 1993), clarifying the role of racial/ethnic and gender disparities in symptom manifestation may inform efforts to reduce the psychological consequences of COVID-19 and future crises.
The Present Study and Hypotheses
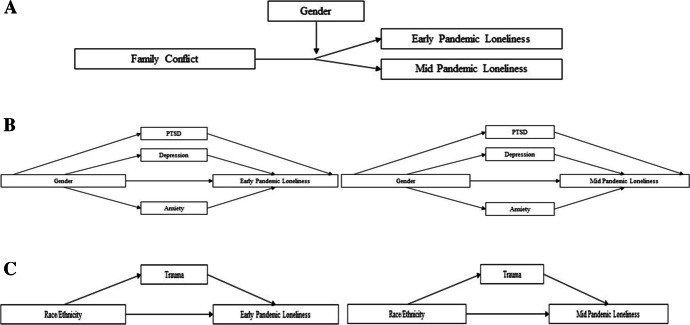
The overarching aim of the present study is to examine pre-pandemic risk factors for loneliness in a racially/ethnically diverse adolescent sample. Based on prior research, we expected pre-pandemic trauma exposure (Hyland et al., 2019), mental health (e.g., Cooper et al., 2021) and familial conflict (e.g., Pan et al., 2021) to uniquely forecast loneliness. Recent research suggests qualitatively different responses to early pandemic and mid-pandemic contexts (e.g., Ravens-Sieberer et al., 2021), suggesting potentially different mechanisms underlying adjustment during different phases of the pandemic. Further, identifying pre-pandemic risks that predict loneliness above and beyond initial psychological responses may be particularly important for promoting long-term well-being in vulnerable youth. Thus, risk factors were examined to assess risk for both early and mid-pandemic loneliness. Finally, to address potential health disparities, we examined how risk factors varied across identities. Specifically, we tested whether loneliness risk was elevated for certain identities (i.e., mediation models) or whether certain demographic characteristics were more sensitive to our pre-selected risk factors (i.e., moderation models). Based on extant literature (e.g., López et al., 2017; Manduca, 2018; Rudolph & Hammen, 1999), we hypothesized female adolescents would demonstrate heightened pre-pandemic internalizing symptoms (support for a mediation model) and greater sensitivity to family conflict (support for a moderation model), while adolescents who identified as non-White would report greater pre-pandemic adversity, and thus, be more at risk for loneliness via a mediation model. These hypotheses are illustrated in Fig. 1 for clarity.
Fig. 1.
A Visual depiction of hypothesis for the relation between family conflict and loneliness being stronger for females. B Visual depiction of hypothesis for the mediating role of pre-pandemic internalizing symptoms for loneliness among females. C Visual depiction of hypothesis for the mediating role of pre-pandemic trauma exposure for loneliness among non-White adolescents. Note: Gender = Female = 0, Male = 1; Loneliness = Three items adapted from the Roberts Version of the UCLA Loneliness Scale including the prompt “Since learning about the Corona Virus, have you felt the following” (Roberts et al., 1993); Family conflict = Negative interactions factor of the Network of Relationships Inventory: Behavioral Systems Version – Short Form (NRI: BSV-SF; Furman & Buhrmester, 2009). PTSD = Post traumatic stress subscale of the Trauma Symptom Checklist for Children (TSCC; Briere, 1996); Depression = Depression subscale of the TSCC (Briere, 1996); Anxiety = Anxiety subscale of the TSCC (Briere, 1996); Trauma = Adverse Childhood Experiences questionnaire (ACEs; Finkelhor et al., 2013); Race/Ethnicity = Self-reported race/ethnicity
Materials and methods
Participants
Participants for the current study were recruited as part of an ongoing longitudinal study examining pathways to distress and resilience across different forms of trauma exposure within adolescence. The baseline visit of the study occurred prior to the COVID-19 lockdown procedures. Given the widespread effect of the pandemic, the investigators introduced questions assessing responses (e.g., loneliness) to the potentially traumatic experience of the public health crisis. Adolescents who participated in the second wave of data collection during the pandemic (March-August 2020) were included in this study. Of 584 adolescents at baseline, those completing the second survey before the pandemic (N = 58) and those with missing data for the second wave (N = 157) were excluded. To examine potential biases in our subsample, we created two groups, one group signifying those who were not included in the study (N = 215) and the other group capturing those who were included in the study (N = 369). We then conducted independent sample t-tests to compare the mean levels of baseline measures across these two groups. Surprisingly, participants in the present study demonstrated significantly higher means for PSTD (t(208, 359) = -2.59, p < 0.01), anxiety (t(208, 360) = -2.92, p < 0.01) and depressive symptoms (t(208, 359) = -2.59, p < 0.01) compared to those who did not complete the Wave 2 COVID-19 measures. Therefore, if anything, hypotheses were tested within a sample at higher vulnerability for emotional distress. Meanwhile, non-significant differences emerged for aggression, trauma exposure, family conflict, and age. Chi-square tests found significant differences between the two groups regarding gender, χ2(215,369) = 12.13, p < 0.05, with a higher percentage of female identifying individuals included in the study (54.5% vs 45.5%) compared to those who did not complete Wave 2 COVID-19 measures. Meanwhile, chi-square tests across race/ethnicity found no significant differences between the two groups, χ2(215,369) = 1.05, p = 0.79.
Participants were recruited from three schools in a large, urban setting in southeast Texas (N = 342), as well as juvenile justice system (JJS)-involved youth in a small Midwestern city (N = 27). Analyses revealed that the JJS-involved sample was younger (MAge = 13.56, SD = 1.31) than the school sample (MAge = 15.16, SD = 1.00), t(27,341) = 7.85, p < 0.001. In addition, the two samples differed significantly in race/ethnicity, χ2 (3, N = 369) = 10.03, p = 0.02, such that more participants in the JJS-involved sample identified as White (51.9%) compared to the school sample (28.4%), while more participants in the school sample identified as Hispanic (19.9%) compared to the JJS-involved sample (0%). No significant differences were found for gender, p = 0.85. The two samples were equivalent across all other study variables, ps > 0.05, with the exception of baseline family conflict, with the JJS-involved sample reporting greater levels, t(367) = 6.09, p < 0.001. Given the relative similarity between the two samples, and the small size of the JJS-involved sample, they were combined to increase the overall power of our analyses. The final sample consisted of 369 youths between the ages of 12 and 18 (Mage = 15.04; SDage = 1.10). The sample was demographically diverse, with regard to gender (54.5% female, 45.5% male) and race/ethnicity (e.g., 30.1% White; 30.9% Black; 18.4% Hispanic; 20.6% Other).
Procedure
All study procedures for the current study were approved by the Institutional Review Board at the first author’s home institution. For the school sample, students were introduced to the study during class by research personnel. If interested, students brought home a description of the study along with a parental consent form. For the JJS-involved sample, a member of the study team reached out to adolescents who were either referred by a case manager at a juvenile diversion program, or recruited from a community-event that the diversion program attended. Across both sites, once child assent and parental consent were obtained, adolescents completed a 45-min survey on demographic characteristics, life events, and mental health for the baseline assessment. These adolescents were then contacted 6 months and 1 year later for Wave 2 and Wave 3, respectively. The baseline visits of this study occurred from October through December 2019, Wave 2 from April through June 2020, and Wave 3 from October through December 2020. Baseline assessments were completed both with paper and pencil measures as well as online using tablets, while all Wave 2 and Wave 3 assessments were completed online via a Qualtrics survey. Adolescents provided a self-generated code to prevent linking their data to their identity, allowing adolescents to more comfortably answer questions concerning potentially traumatic events and risky behavior (Yurek et al., 2008). Adolescents were compensated with a $20 (USD) gift card to a nationwide retailer (e.g., Amazon) upon completion of each Wave, as well as an additional $15 (USD) if they completed all three waves. Pre-pandemic risk factors were derived from the baseline assessment, while early- and mid-pandemic loneliness data were derived from Wave 2 and Wave 3, respectively.
Measures
Loneliness
Adolescents’ early- and mid-pandemic loneliness was assessed using a three-item measure adapted from the Roberts Version of the UCLA Loneliness Scale (Roberts et al., 1993), developed specifically for the brief measurement of loneliness within adolescents. Participants were asked to indicate on a scale of 1 (rarely) to 3 (often) how much, since learning about the Corona Virus, they felt they “lack friends,” are “left out,” and are “lonely.” In the present study, Cronbach’s alpha for the loneliness scale was 0.78 (Wave 2) and 0.82 (Wave 3), suggesting good internal consistency.
Pre-existing Mental Health
34 items from the Trauma Symptom Checklist for Children (TSCC; Briere, 1996) were used to assess for pre-pandemic levels of psychological distress, consisting of the post-traumatic stress (PTSD; 10 items), depression (8 items), anxiety (7 items), and anger/aggression (9 items) subscales. Adolescents were asked to indicate the frequency of symptoms during the past 6 months, rating responses on a scale of 0 (never) to 3 (almost all of the time). Example items included, “Having bad dreams or nightmares (PTSD),” “Feeling afraid something bad might happen (anxiety),” “Feeling lonely (depression),” and “Arguing too much (anger/aggression).” Past research has established the TSCC to be a reliable and valid measure among adolescents (Sadowski & Friedrich, 2000). In the present study, Cronbach’s alphas were 0.90 (PTSD), 0.86 (depression), 0.86 (anxiety), and 0.88 (aggression), suggesting good to excellent internal consistency across all four subscales.
Prior Trauma Exposure
Pre-pandemic trauma exposure was assessed using an adapted 10-item Adverse Childhood Experiences questionnaire (ACES; Finkelhor et al., 2013). Adolescents were asked to answer either yes or no to questions including, “Did you often or very often feel lonely, rejected or that nobody liked you?” and “Did a household member go to prison?”. The ACES is widely used to assess for negative early life experiences, and has been found to be associated with a variety of detrimental health and social consequences in adolescents (Balistreri & Alvira-Hammond, 2016). In the current study, the ACES had a Cronbach’s alpha of 0.95, suggesting excellent internal consistency.
Family Conflict
Pre-pandemic family conflict was assessed through the negative interactions factor of the Network of Relationships Inventory: Behavioral Systems Version – Short Form (NRI: BSV-SF; Furman & Buhrmester, 2009). After identifying a primary caregiver, adolescents were asked six questions regarding the frequency of negative interactions with their primary caregiver, including “How much do you and this person get upset or mad at each other?” on a scale of 1 (little or none) to 3 (very much). Cronbach alpha was 0.98, reflecting excellent internal consistency.
Data Analytic Approach
Descriptive statistics were computed and a missing data analysis was conducted prior to testing study aims. All hypotheses were tested within a multiple regression framework with separate models for early pandemic (Wave 2) and mid-pandemic loneliness (Wave 3). Pre-pandemic risks were entered into an initial simultaneous model. As emotional distress tends to vary by age and gender (Hankin & Cohen, 2020), these characteristics were entered as covariates in all analytic models. Given the high rates of comorbidity between symptom subtypes, we utilized standardized residuals, resulting from the regression of each pre-existing mental health subscale on the remaining pre-existing mental health entities, as independent variables within analytic models. For instance, anxiety symptoms were captured via a standardized residual that reflected the unique variance of anxiety symptoms once partialing out shared variance with depression, PTSD, and aggression. To help control for false positives in the wake of partitioning (see Lynam et al., 2006), subsequent analyses tested whether the residuals, as well as the raw mental health symptom subscale scores, were identified as significant within independent regression models. Raw scores were used to index pre-pandemic environmental stressors (i.e., family conflict, ACEs). For models that used mid-pandemic loneliness as the criterion, early pandemic loneliness was entered as a covariate. Indices that were significant across simultaneous and individual models were considered predictive of our outcomes.
To test our profiles of risk within the context of race/ethnicity and gender, multiple regression models using the PROCESS framework were conducted (Hayes, 2017). Mediation models tested whether heightened levels of a given risk index explained the relation between a demographic profile and loneliness. Subsequently, moderation analyses were conducted to examine whether either gender or race/ethnicity interacted with a risk index to predict loneliness. If any risk index demonstrated both mediation and moderation (e.g., family conflict mediates the relation between gender and loneliness and gender moderates the relation between family conflict and loneliness), we tested mediation and moderation simultaneously via an exposure-mediation model (Valeri & VanderWeele, 2013). This provides a more robust test of disentangling whether a third variable mediates or moderates a given relation (Valeri & VanderWeele, 2013). Analyses were conducted using SPSS v25.0.
Interpretation of mediation and moderation models followed extant recommendations (Hayes & Preacher, 2014; Hayes & Rockwood, 2017). For mediation models, indirect effects were calculated via the product approach. Bias-corrected bootstrap interval estimates of the product between a and b divided by the standard deviation of the outcome was used as our effect size. This effect size provides a more reliable and robust estimate of the true indirect effect compared to alternative strategies (e.g., ratio effect sizes) and can provide an effect size across a greater range of mediation contexts (e.g., inconsistent mediation; Miočević et al., 2018). Meanwhile, predicted values from significant moderators based on demographic characteristics and high (1 standard deviation above the mean) and low (1 standard deviation below the mean) levels of risk were depicted visually to illustrate profiles of risk and resilience.
Results
Preliminary Analysis
Table 1 provides means for all study variables. Of note, adolescents in our sample reported a marginal increase in loneliness from the beginning of the pandemic until the middle of the pandemic (t(368) = -1.93, p = 0.05). Examination of mean differences in loneliness across demographics suggested higher levels of loneliness among females compared to males, both with regard to early, t(367) = 4.98, p < 0.001 and mid t(367) = 6.82, p < 0.001 pandemic measures, while no differences were found across race/ethnicity, ps > 0.10. Across most variables there was minimal missing data, with the exception of mid-pandemic loneliness in which 17.1% of the data was missing (the variable with the next most missing data was family conflict: 3.3%). To examine whether the pattern of missing data was systematic, we conducted the Little’s Missing Completely at Random (MCAR) statistic, in which the null hypothesis is that the data is MCAR. Results suggested the data was MCAR, χ2(392) = 432.79, p = 0.08, and data was subsequently imputed using the expectation maximization algorithm (Schafer & Graham, 2002). The imputed dataset was used for all subsequent analyses to reduce biases related to listwise deletion. The interrelatedness of our predictors was assessed via the Variance Inflation Factor (VIF), with values greater than 10 adversely affecting parameter estimation (Belsley, 1991). Results from a VIF analysis on our imputed dataset suggested minimal threat to interpretation (Supplemental Tables S1-S2). In Table 2, bivariate correlations are reported between all continuous variables. All variables demonstrated multiple positive correlations.
Table 1.
Means and standard deviations for all measures
| Measures | Mean | SD | Number of Items |
|---|---|---|---|
| Gender | 0.46 (0.46) | 0.50 (0.50) | 1 |
| Age | 4.05 (4.05) | 1.11 (1.11) | 1 |
| Loneliness_W2 | 5.28 (5.29) | 1.96 (1.97) | 3 |
| Loneliness_W3 | 5.46 (5.53) | 1.89 (2.01) | 3 |
| PTSD | 18.65 (18.70) | 6.79 (6.85) | 10 |
| Depression | 14.45 (14.49) | 5.03 (5.07) | 8 |
| Anxiety | 13.14 (13.15) | 4.54 (4.57) | 7 |
| Aggression | 15.49 (15.52) | 5.46 (5.50) | 9 |
| Trauma | 2.31 (2.32) | 2.55 (2.58) | 10 |
| Family conflict | 1.62 (1.61) | 0.74 (0.74) | 6 |
Gender = Female = 0, Male = 1; Age = 1 = 12, 2 = 13, 3 = 14, 4 = 15, 5 = 16, 6 = 17, 7 = 18; Loneliness = Three items adapted from the Roberts Version of the UCLA Loneliness Scale including the prompt “Since learning about the Corona Virus, have you felt the following” (Roberts et al., 1993); PTSD = Post traumatic stress subscale of the Trauma Symptom Checklist for Children (TSCC; Briere, 1996); Depression = Depression subscale of the TSCC (Briere, 1996); Anxiety = Anxiety subscale of the TSCC (Briere, 1996); Aggression = Aggression subscale of the TSCC (Briere, 1996); Trauma = Adverse Childhood Experiences questionnaire (ACEs; Finkelhor et al., 2013); Family conflict = Negative interactions factor of the Network of Relationships Inventory: Behavioral Systems Version – Short Form (NRI: BSV-SF; Furman & Buhrmester, 2009); W2 = Wave 2 assessment; W3 = Wave 3 assessment
Values in parentheses indicate means and standard deviations before imputing the missing data
Table 2.
Bivariate correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | – | |||||||||
| 2. Age | –0.048 | – | ||||||||
| 3. Lonely_W2 | –0.25** | 0.047 | – | |||||||
| 4. Lonely_W3 | –0.34** | –0.005 | .56** | – | ||||||
| 5. PTSD | –0.27** | –0.034 | .33** | .33** | – | |||||
| 6. Depression | –0.30** | –0.006 | .35** | .38** | .86** | – | ||||
| 7. Anxiety | –0.40** | –0.042 | .37** | .42** | .84** | .82** | – | |||
| 8. Aggression | –0.32** | –0.054 | .27** | .30** | .86** | .85** | .76** | – | ||
| 9. Trauma | –0.14** | –0.072 | .21** | .16** | .48** | .46** | .39** | .47** | – | |
| 10. Family Conflict | –0.21** | –0.056 | .18** | .20** | .33** | .34** | .30** | .37** | .24** | – |
Gender = Female = 0, Male = 1; Age = 1 = 12, 2 = 13, 3 = 14, 4 = 15, 5 = 16, 6 = 17, 7 = 18; Lonely = Three items adapted from the Roberts Version of the UCLA Loneliness Scale including the prompt “Since learning about the Corona Virus, have you felt the following” (Roberts et al., 1993); PTSD = Post traumatic stress subscale of the Trauma Symptom Checklist for Children (TSCC; Briere, 1996); Depression = Depression subscale of the TSCC (Briere, 1996); Anxiety = Anxiety subscale of the TSCC (Briere, 1996); Aggression = Aggression subscale of the TSCC (Briere, 1996); Trauma = Adverse Childhood Experiences questionnaire (ACEs; Finkelhor et al., 2013); Family conflict = Negative interactions factor of the Network of Relationships Inventory: Behavioral Systems Version – Short Form (NRI: BSV-SF; Furman & Buhrmester, 2009); W2 = Wave 2 assessment; W3 = Wave 3 assessment. Correlations represent relations within the imputed dataset
**p < .01
Multiple Regression Models
For our simultaneous model, all symptom indices were significant and neither ACEs nor family conflict were significant. Within our independent residualized and raw symptom analyses, only aggression and depression remained significant (ps < 0.05, Table 3). We next examined models concerning mid-pandemic loneliness. Within our simultaneous model, neither ACEs nor family conflict were significant, while all symptom variables were significant. Within our independent residualized and raw symptom analyses, only anxiety remained significant (ps < 0.05, Table 3).
Table 3.
Identification of convergent significant predictors for early and mid-pandemic loneliness
| Lonely_W2 | |||||||||
| Simultaneous residualized model | Individual residualized model (Gender and Age as Covariates in each) | Individual raw model (Gender and Age as Covariates in each) | |||||||
| Variable | β | SE | t | β | SE | t | β | SE | t |
| (Intercept) | 4.81 | 0.46 | 10.36** | – | – | – | – | – | – |
| Gender | –0.54 | 0.21 | –2.57* | – | – | – | – | – | – |
| Age | 0.083 | 0.086 | 0.97 | – | – | – | – | – | – |
| PTSD | 1.13 | 0.28 | 4.01** | 0.12 | 0.10 | 1.15 | 0.081 | 0.015 | 5.52** |
| Aggression | 0.69 | 0.25 | 2.80** | –0.25 | 0.10 | –2.47* | 0.075 | 0.019 | 3.97** |
| Depression | 1.14 | 0.26 | 4.41** | 0.25 | 0.10 | 2.47* | 0.12 | 0.02 | 6.01** |
| Anxiety | 1.03 | 0.25 | 2.80** | 0.13 | 0.10 | 1.22 | 0.14 | 0.023 | 6.031** |
| Family Conflict | 0.16 | 0.14 | 1.13 | – | – | – | 0.35 | 0.14 | 2.57* |
| Trauma | 0.058 | 0.043 | 1.37 | – | – | – | 0.14 | 0.039 | 3.63** |
| Lonely_W3 | |||||||||
| Simultaneous residualized model | Individual residualized model (Gender, Age, Lonely_W2 as Covariates in each) | Individual raw model (Gender, Age, Lonely_W2 as Covariates in each) | |||||||
| Variable | β | SE | t | β | SE | t | β | SE | t |
| (Intercept) | 3.56 | 0.44 | 8.073** | – | – | – | – | – | – |
| Gender | –0.54 | 0.18 | –3.047** | – | – | – | – | – | – |
| Age | –0.051 | 0.071 | –0.72 | – | – | – | – | – | – |
| PTSD | 0.70 | 0.24 | 2.90** | –0.079 | 0.081 | –0.97 | 0.035 | 0.013 | 2.75** |
| Aggression | 0.54 | 0.21 | 2.61** | –0.068 | 0.082 | –0.83 | 0.038 | 0.016 | 2.43* |
| Depression | 0.79 | 0.22 | 3.54** | 0.13 | 0.081 | 1.58 | 0.062 | 0.017 | 3.63** |
| Anxiety | 0.75 | 0.19 | 3.92** | 0.18 | 0.084 | 2.11* | 0.081 | 0.02 | 4.12** |
| Family Conflict | 0.12 | 0.12 | 1.054 | – | – | – | 0.19 | 0.11 | 1.68 |
| Trauma | –0.028 | 0.036 | –0.78 | – | – | – | 0.017 | 0.032 | 0.52 |
| Lonely_W2 | 0.42 | 0.044 | 9.59** | – | – | – | 0.48 | 0.04 | 11.48** |
Gender = Female = 0, Male = 1; Age = 1 = 12, 2 = 13, 3 = 14, 4 = 15, 5 = 16, 6 = 17, 7 = 18;Lonely = Three items adapted from the Roberts Version of the UCLA Loneliness Scale including the prompt “Since learning about the Corona Virus, have you felt the following” (Roberts et al., 1993); PTSD = Post traumatic stress subscale of the Trauma Symptom Checklist for Children (TSCC; Briere, 1996); Depression = Depression subscale of the TSCC (Briere, 1996); Anxiety = Anxiety subscale of the TSCC (Briere, 1996); Aggression = Aggression subscale of the TSCC (Briere, 1996); Trauma = Adverse Childhood Experiences questionnaire (ACEs; Finkelhor et al., 2013); Family conflict = Negative interactions factor of the Network of Relationships Inventory: Behavioral Systems Version – Short Form (NRI: BSV-SF; Furman & Buhrmester, 2009); W2 = Wave 2 assessment; W3 = Wave 3 assessment
*p < .05; **p < .01
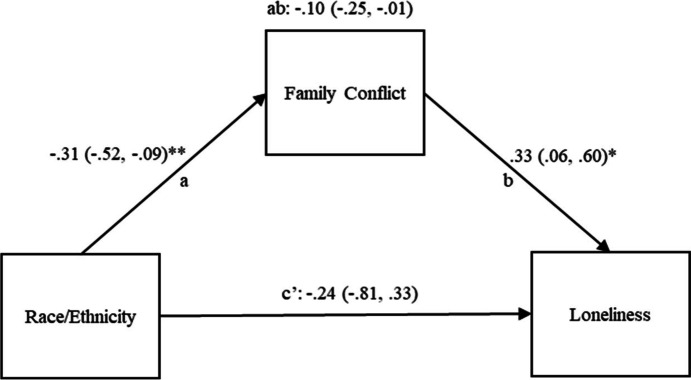
As for demographic considerations, our model first examined the relation between our risk factors and loneliness within the context of race/ethnicity. Regarding the mediation model, findings suggested that family conflict explained more variance in early pandemic loneliness for White adolescents compared to those who identified as Hispanic. These findings are reflected in Fig. 2. Meanwhile, we did not find support for any other mediation model for early or mid-pandemic loneliness with regard to race/ethnicity (i.e., all confidence intervals for the indirect effect included 0). Similarly, moderation models suggested that none of our risk indices varied as a function of race/ethnicity for early nor mid-pandemic loneliness, (ps > 0.07).
Fig. 2.
Relation between family conflict and early-pandemic loneliness for hispanic adolescents relative to white adolescents. Note: Race/Ethnicity = Self-reported race/ethnicity; Family conflict = Negative interactions factor of the Network of Relationships Inventory: Behavioral Systems Version – Short Form (NRI: BSV-SF; Furman & Buhrmester, 2009); Loneliness = Early pandemic loneliness measured using three items adapted from the Roberts Version of the UCLA Loneliness Scale including the prompt “Since learning about the Corona Virus, have you felt the following” (Roberts et al., 1993); Values in parentheses represent the lower limit and upper limits of 95% confidence intervals. Coefficients and confidence intervals represent unstandardized values. *p < .05; **p < .01
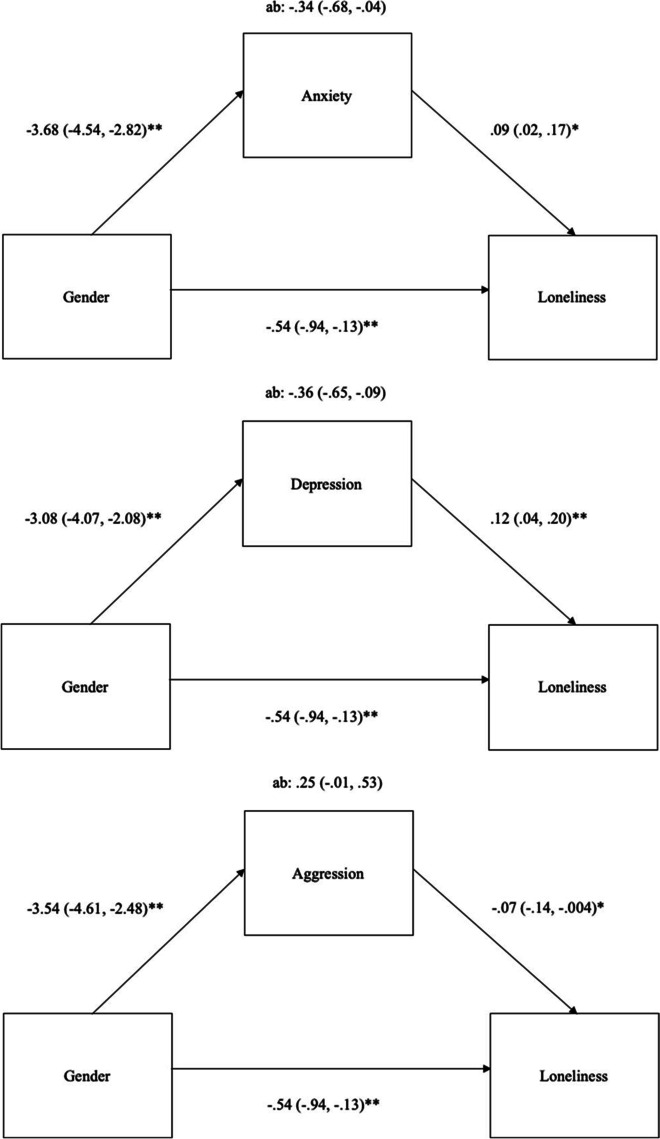
As for gender, family conflict, ACES, PTSD, anxiety, depression, and aggression all mediated the relation between gender and early-pandemic loneliness within independent models. In response, all risk indices were entered into a simultaneous model. ACES (abps = -0.02), family conflict (abps = -0.03), and PTSD (abps = -0.06) were iteratively eliminated from models as non-significant mediators. A final model identified anxiety and depression explaining heightened early-pandemic loneliness in girls, and anger/aggression explaining heightened loneliness in boys. Findings from this model are displayed in Fig. 3. As for mid-pandemic loneliness, PTSD (abps = -0.05), anxiety (abps = -0.13), depression (abps = -0.08), and aggression (abps = -0.06) all emerged as significant mediators within independent models. Within simultaneous models, aggression (abps = 0.04), depression (abps = -0.06), and PTSD (abps = 0.03) were all eliminated in iterative models, leaving only anxiety (abps = -0.13) as a mediator for heightened loneliness in females. These findings are displayed in Fig. 4.
Fig. 3.
Gender specific pathways for early pandemic loneliness. Note: Gender = Female = 0, Male = 1; Loneliness = Three items adapted from the Roberts Version of the UCLA Loneliness Scale including the prompt “Since learning about the Corona Virus, have you felt the following” (Roberts et al., 1993); Anxiety = Anxiety subscale of the TSCC (Briere, 1996); Depression = Depression subscale of the TSCC (Briere, 1996); Aggression = Aggression subscale of the TSCC (Briere, 1996). *p < .05; **p < .01
Fig. 4.
Gender specific pathways for mid-pandemic loneliness. Note: Gender = Female = 0, Male = 1; Loneliness = Three items adapted from the Roberts Version of the UCLA Loneliness Scale including the prompt “Since learning about the Corona Virus, have you felt the following” (Roberts et al., 1993); Anxiety = Anxiety subscale of the TSCC (Briere, 1996). *p < .05; **p < .01
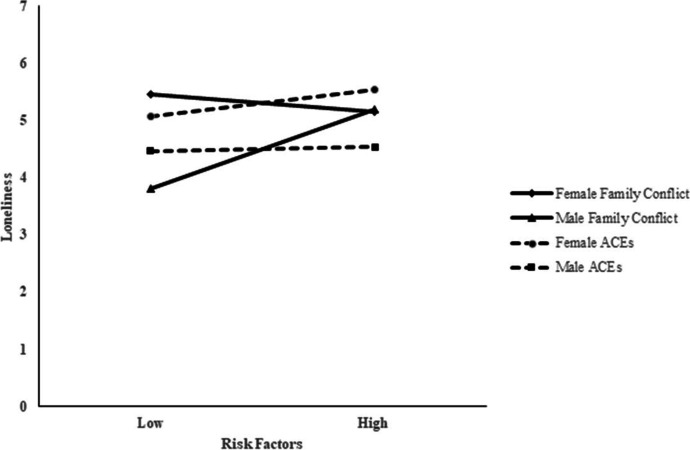
Finally, moderation models concerning gender were tested. For early pandemic loneliness, family conflict, B = 0.59; t(4, 363) = 2.12, p = 0.035, and trauma-exposure, B = -0.17; t(4,363) = -2.20, p = 0.029, were moderated by gender within independent models. Meanwhile, gender did not moderate any of the pre-pandemic symptoms, ps > 0.20. Family conflict and ACES emerged within the simultaneous model as significant as well, with the effects of ACES and conflict both varying as a function of gender. These findings are plotted in Fig. 5. As can be seen, all females (i.e., females exposed to low, average, and high levels of family conflict) experienced early pandemic loneliness above the mean, while only males who experienced high levels of family conflict reported elevated levels of loneliness. As for ACES, we found a sharp linear increase for loneliness for females, such that greater ACES-exposure led to heightened loneliness, while the simple slope for males was non-significant. As for mid-pandemic loneliness, none of the risk indices varied as a function of gender (ps > 0.15).
Fig. 5.
Gender interactions for family conflict and ACEs for early-pandemic loneliness. Note: Gender = Female = 0, Male = 1; Loneliness = Early pandemic loneliness measured using three items adapted from the Roberts Version of the UCLA Loneliness Scale including the prompt “Since learning about the Corona Virus, have you felt the following” (Roberts et al., 1993); Family conflict = Negative interactions factor of the Network of Relationships Inventory: Behavioral Systems Version – Short Form (NRI: BSV-SF; Furman & Buhrmester, 2009); ACEs = Adverse Childhood Experiences questionnaire (Finkelhor et al., 2013)
Conclusion
The COVID-19 pandemic has drastically changed the lives of youth across the United States. The goals of the present study were to (a) understand which risks may contribute towards feelings of loneliness during the pandemic and (b) how these pathways operate within the context of race/ethnicity and gender. Findings indicated that depressive and aggression symptoms prior to the pandemic predicted early pandemic loneliness, whereas only anxiety symptoms prior to the pandemic incrementally predicted mid-pandemic loneliness. As for demographic differences, minimal differences were found for race/ethnicity, but several intriguing results were identified within the context of gender. Specifically, environmental stressors were moderated by gender for early pandemic loneliness, and gender-specific symptom mediation pathways emerged for early and mid-pandemic loneliness. Below, we contextualize these findings within the emerging COVID-19 adolescent mental health literature (e.g., Cooper et al., 2021), as well as adolescent adjustment to national disasters more broadly.
In line with previous research during the pandemic (Cooper et al., 2021), we found that symptoms across internalizing and externalizing domains were associated with early pandemic loneliness. That depressive and externalizing symptoms both emerged as unique predictors for early pandemic loneliness suggests that each symptom profile may confer a unique risk mechanism. For instance, adolescents predisposed to depressive symptoms report cognitive styles (i.e., perceived rejection; Oosterhoff et al., 2020) that may be contributing toward experiences of loneliness during the onset of the pandemic. Alternatively, adolescents experiencing depressive symptoms may engage in behaviors, such as social withdrawal despite a desire to connect with others (Achterbergh et al., 2020), that potentiate the limited social connectedness associated with social distancing. With regard to externalizing symptoms, it may be that while some forms of aggression are tolerated, or even rewarded with positive peer attention in normative contexts (Rose et al., 2004), the demonstration of that behavior during periods of mandated social distancing may repel peer interaction. For instance, León Moreno and colleagues (2021) found that higher levels of cyberaggression were related to elevated reports of peer rejection. Finally, findings concerning anxiety’s relation with mid-pandemic loneliness signals an important contribution toward understanding perceived isolation in the later stages of the current crisis. A possibility is that although social distancing is an important and essential facet of virus containment, symptoms of anxiety may unnecessarily maintain engagement in these safeguarding practices (self-isolating in the absence of sufficient transmission risk; Shafran et al., 2020), causing these behaviors to persist in ways that increase the likelihood of loneliness. Collectively, these findings suggest that pre-existing mental health remains a potent predictor of youth adjustment during disaster experiences, thus building upon past research examining these relations within other disaster contexts (e.g., natural disasters; La Greca et al., 1998).
Interestingly, the significant influence of environmental risk, as measured by ACES and family conflict, on early pandemic loneliness was explained by intrapersonal symptoms and these factors did not relate to mid-pandemic experiences of loneliness. It is worth noting that we did find that parent–child conflict explained more of the variance in White adolescent loneliness compared to their peers who identified as Hispanic; however, given the little incremental validity of parent–child conflict compared to other variables, the translational significance of this finding is negligible. An alternate conceptualization for environmental processes may be that the influence of parent–child conflict and ACES is best understood via indirect pathways. For instance, in past disaster research, Cohen and colleagues (2016) found that environmental predictors (e.g., familial relationships) were best contextualized as a moderator of intrapersonal risks when predicting prospective internalizing outcomes within the context of a disaster. Thus, while ecological risks may not be the best domain to focus on for ameliorating pandemic loneliness in the general population, they may have some translational value in identifying who may be most sensitive to certain intrapersonal risks within the context of a pandemic.
As for demographic differences, we found that loneliness, and loneliness risk, did not vary as a function of race/ethnicity. These findings suggest the possibility that emerging adolescent loneliness interventions (see Eccles & Qualter, 2021) may be equitable from a race/ethnicity perspective. Alternatively, several gender specific pathways emerged for early and mid-pandemic loneliness via both mediation and moderation models. With regard to mediation, anxiety and depression explained more of the variance in levels of early pandemic loneliness, with anxiety remaining meaningful for mid-pandemic loneliness for girls, while externalizing distress explained more of the variance in early pandemic loneliness for boys. These findings are supported by prior research that establishes heightened anxiety and depression among females (e.g., Racine et al., 2021) and aggression among males (e.g., Francisco et al., 2020) during the COVID-19 pandemic. These results build upon prior research delineating the relation between pre-pandemic mental health and loneliness among adolescents (Hards et al., 2021) by highlighting the importance of specific pre-pandemic symptom profiles, as the role of these symptoms are unique for boys and girls. Further, our study showed that pre-pandemic anxiety may be particularly important for understanding prolonged experiences of loneliness in female adolescents. Given that females tend to disproportionately experience disaster-related distress (Cénat & Derivois, 2015), future research should examine how anxiety may uniquely contribute to this phenomenon.
Complementary to these findings was the insight gained from moderating analyses. Contrary to hypotheses, as well as past research (Flook, 2011), we found boys to experience more emotional reactivity within the context of family conflict compared to girls. However, as post-hoc results suggested that boys experiencing heightened conflict are experiencing symptoms comparable to girls experiencing low family conflict, the translational significance of this specific finding is limited. Instead, future disaster research may want to examine other familial processes that have been shown to be instrumental in well-being during COVID-19 (parental social support; Wang et al., 2022). Alternatively, examination of the interaction between trauma exposure and gender revealed a linear relation between pre-pandemic trauma exposure and loneliness among girls. These findings are in line with some broader research, which illustrates that females are more likely to experience internalizing symptoms after adversity (Foster et al., 2004), including natural disasters (Groome & Soureti, 2004). Together with our mediation findings, these findings echo recent calls (e.g., John et al., 2020) for more gender-focused preventive programming in the aftermath of national disasters.
Although this study is characterized by several strengths, including pre-pandemic risk indices and a large and diverse sample, a number of limitations are worth noting. First, though the study implemented several methods to alleviate common bias error, including an anonymized data collection and a focus on item simplicity within scales (i.e., few double negative items), measures were single informant. Although adolescents are well positioned to inform on distress and impairment (Smith, 2007), utilizing a multi-informant approach is recommended when examining risk and resilience in adolescents (see De Los Reyes et al., 2015). Second, although we extended previously identified relations between loneliness and predictors (e.g., Lalayants & Prince, 2015), our measure of loneliness was introduced in response to the COVID-19 pandemic, and thus not collected at baseline. As such, we were unable to examine the relation between loneliness and our predictors outside the context of the pandemic. In addition, although our study relied on a two timepoint study design, extending these findings into a multi-wave, longitudinal design within a multilevel structural equation or growth modeling framework may provide further insight into the temporal nature of the relations identified. Stressor characteristics may also impact the emergence of outcomes, such as loneliness. Thus, in line with other studies capturing how components of the COVID-19 pandemic are related to perceptions of negative outcomes (e.g., Mahmoud et al., 2022), such as loneliness, further evaluation of COVID-19 characteristics represents an important next direction. Finally, although our study intentionally selected loneliness as our criterion given its relevance within a post-disaster context, our study is unable to speak to other adjustment outcomes. For example, given the ties between pre-existing mental health concerns and other post-disaster responses (e.g., Cohen et al., 2016), it will be important to understand whether particular risk mechanisms relate to other patterns of distress and impairment as well. Despite these limitations, our findings provide new insight into youth adjustment during this unprecedented era. As the COVID-19 pandemic continues to affect adolescents worldwide, it will be important to build upon the findings from the current study to understand how the profiles identified may exacerbate risk for long-term responses, particularly as adolescents begin to transition into young adulthood.
Supplementary Information
Below is the link to the electronic supplementary material.
Authors Contribution
HT conceived of the current analysis and drafted the manuscript; MS drafted the manuscript; JC participated in data collection, data curation, project administration, and drafted the manuscript; JRT conceived the overall study and reviewed the manuscript, JRC conceived of the study, data curation, conceived and performed the statistical analysis, and drafted the manuscript.
Funding
This research was supported by the National Institute of Justice awarded to Joseph R. Cohen (2018-R2-CX-0022; 15PNIJ-21-GG-02803-MUMU). All study procedures for the current study were approved by the Institutional Review Board at the University of Illinois at Urbana-Champaign.
Declarations
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hena Thakur, Email: hthakur2@illinois.edu.
Morgan Stutts, Email: mstutts2@illinois.edu.
Jae Wan Choi, Email: jchoi98@illinois.edu.
Jeff R. Temple, Email: jetemple@utmb.edu
Joseph R. Cohen, Email: cohenj@illinois.edu
References
- Achterbergh L, Pitman A, Birken M, Pearce E, Sno H, Johnson S. The experience of loneliness among young people with depression: A qualitative meta-synthesis of the literature. BMC Psychiatry. 2020;20(1):1–23. doi: 10.1186/s12888-020-02818-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adalja AA, Toner E, Inglesby TV. Priorities for the US health community responding to COVID-19. JAMA. 2020;323(14):1343–1344. doi: 10.1001/jama.2020.3413. [DOI] [PubMed] [Google Scholar]
- Adams RE, Laursen B. The correlates of conflict: Disagreement is not necessarily detrimental. Journal of Family Psychology. 2007;21(3):445–458. doi: 10.1037/0893-3200.21.3.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson ER, Mayes LC. Race/ethnicity and internalizing disorders in youth: A review. Clinical Psychology Review. 2010;30(3):338–348. doi: 10.1016/j.cpr.2009.12.008. [DOI] [PubMed] [Google Scholar]
- Balistreri KS, Alvira-Hammond M. Adverse childhood experiences, family functioning and adolescent health and emotional well-being. Public Health. 2016;132:72–78. doi: 10.1016/j.puhe.2015.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beam CR, Kim AJ. Psychological sequelae of social isolation and loneliness might be a larger problem in young adults than older adults. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S58–S60. doi: 10.1037/tra0000774. [DOI] [PubMed] [Google Scholar]
- Belsley, D. A. (1991). A guide to using the collinearity diagnostics. Computer Science in Economics and Management, 4(1), 33–50.
- Birkett M, Russell ST, Corliss HL. Sexual-orientation disparities in school: The mediational role of indicators of victimization in achievement and truancy because of feeling unsafe. American Journal of Public Health. 2014;104(6):1124–1128. doi: 10.2105/AJPH.2013.301785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J. Trauma symptom checklist for children (TSCC) professional manual. Psychological Assessment Resources; 1996. [Google Scholar]
- Cénat JM, Derivois D. Long-term outcomes among child and adolescent survivors of the 2010 Haitian earthquake. Depression and Anxiety. 2015;32(1):57–63. doi: 10.1002/da.22275. [DOI] [PubMed] [Google Scholar]
- Cheng J, Liang Y, Fu L, Liu Z. Posttraumatic stress and depressive symptoms in children after the Wenchuan earthquake. European Journal of Psychotraumatology. 2018;9(1):1472992. doi: 10.1080/20008198.2018.1472992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JR, Adams ZW, Menon SV, Youngstrom EA, Bunnell BE, Danielson CK. How should we screen for depression following a natural disaster? An ROC approach to post-disaster screening in adolescents and adults. Journal of Affective Disorders. 2016;202:102–109. doi: 10.1016/j.jad.2016.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole DA, Turner JE., Jr Models of cognitive mediation and moderation in child depression. Journal of Abnormal Psychology. 1993;102(2):271–281. doi: 10.1037/0021-843X.102.2.271. [DOI] [PubMed] [Google Scholar]
- Condon EM, Dettmer AM, Gee DG, Hagan C, Lee KS, Mayes LC, Stover CS, Tseng WL. Commentary: COVID-19 and mental health equity in the United States. Frontiers in Sociology. 2020 doi: 10.3389/fsoc.2020.584390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper K, Hards E, Moltrecht B, Reynolds S, Shum A, McElroy E, Loades M. Loneliness, social relationships, and mental health in adolescents during the COVID-19 pandemic. Journal of Affective Disorders. 2021;289:98–104. doi: 10.1016/j.jad.2021.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong-Gierveld J. Developing and testing a model of loneliness. Journal of Personality and Social Psychology. 1987;53(1):119–128. doi: 10.1037/0022-3514.53.1.119. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DAG, Burgers DE, Rabinowitz J. The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin. 2015;141(4):858–900. doi: 10.1037/a0038498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles AM, Qualter P. Alleviating loneliness in young people–a meta-analysis of interventions. Child and Adolescent Mental Health. 2021;26(1):17–33. doi: 10.1111/camh.12389. [DOI] [PubMed] [Google Scholar]
- Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science/revue Canadienne Des Sciences Du Comportement. 2020;52(3):177–187. doi: 10.1037/cbs000215. [DOI] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, Hamby SL. Violence, crime, and abuse exposure in a national sample of children and youth: An update. JAMA Pediatrics. 2013;167(7):614–621. doi: 10.1001/jamapediatrics.2013.42. [DOI] [PubMed] [Google Scholar]
- Flook L. Gender differences in adolescents’ daily interpersonal events and well-being. Child Development. 2011;82(2):454–461. doi: 10.1111/j.1467-8624.2010.01521.x. [DOI] [PubMed] [Google Scholar]
- Foster JD, Kuperminc GP, Price AW. Gender differences in posttraumatic stress and related symptoms among inner-city minority youth exposed to community violence. Journal of Youth and Adolescence. 2004;33(1):59–69. doi: 10.1023/a:1027386430859. [DOI] [Google Scholar]
- Francisco, R., Pedro, M., Delvecchio, E., Espada, J. P., Morales, A., Mazzeschi, C., & Orgilés, M. (2020). Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Frontiers in Psychiatry,11. 10.3389/fpsyt.2020.570164 [DOI] [PMC free article] [PubMed]
- Furman W, Buhrmester D. The Network of Relationships Inventory: Behavioral Systems Version. International Journal of Behavioral Development. 2009;33(5):470–478. doi: 10.1177/0165025409342634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groarke JM, Berry E, Graham-Wisener L, McKenna-Plumley PE, McGlinchey E, Armour C. Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS ONE. 2020;15:e0239698. doi: 10.1371/journal.pone.0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groome D, Soureti A. Post-traumatic stress disorder and anxiety symptoms in children exposed to the 1999 Greek earthquake. British Journal of Psychology. 2004;95(3):387–397. doi: 10.1348/0007126041528149. [DOI] [PubMed] [Google Scholar]
- Guessoum, S. B., Lachal, J., Radjack, R., Carretier, E., Minassian, S., Benoit, L., & Moro, M. R. (2020). Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Research, 291, 113264. 10.1016/j.psychres.2020.113264 [DOI] [PMC free article] [PubMed]
- Hankin BL, Cohen JR. Child depression. In: Prinstein M, Youngstrom E, Mash E, Barkley R, editors. Assessment of Childhood Disorders. 5. Guildford Press; 2020. pp. 159–191. [Google Scholar]
- Hards E, Loades ME, Higson-Sweeney N, Shafran R, Serafimova T, Brigden A, Reynolds S, Crawley E, Chatburn E, Linney C, McManus M, Borwick C. Loneliness and mental health in children and adolescents with pre-existing mental health problems: A rapid systematic review. British Journal of Clinical Psychology. 2021 doi: 10.1111/bjc.12331. [DOI] [PubMed] [Google Scholar]
- Harriger JA, Joseph NT, Trammell J. Detrimental associations of cumulative trauma, COVID-19 infection indicators, avoidance, and loneliness with sleep and negative emotionality in emerging adulthood during the pandemic. Emerging Adulthood. 2021;9(5):479–491. doi: 10.1177/21676968211022594. [DOI] [Google Scholar]
- Harris RA, Qualter P, Robinson SJ. Loneliness trajectories from middle childhood to pre-adolescence: Impact on perceived health and sleep disturbance. Journal of Adolescence. 2013;36(6):1295–1304. doi: 10.1016/j.adolescence.2012.12.009. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach. 2. Guilford Press; 2017. [Google Scholar]
- Hayes AF, Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. British Journal of Mathematical and Statistical Psychology. 2014;67(3):451–470. doi: 10.1111/bmsp.12028. [DOI] [PubMed] [Google Scholar]
- Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy. 2017;98:39–57. doi: 10.1016/j.brat.2016.11.001. [DOI] [PubMed] [Google Scholar]
- Hyland P, Shevlin M, Cloitre M, Karatzias T, Vallières F, McGinty G, Fox R, Power JM. Quality not quantity: Loneliness subtypes, psychological trauma, and mental health in the US adult population. Social Psychiatry and Psychiatric Epidemiology. 2019;54(9):1089–1099. doi: 10.1007/s00127-018-1597-8. [DOI] [PubMed] [Google Scholar]
- John N, Casey SE, Carino G, McGovern T. Lessons never learned: Crisis and gender-based violence. Developing World Bioethics. 2020;20(2):65–68. doi: 10.1111/dewb.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Wasserstein SB. Children's predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. Journal of Consulting and Clinical Psychology. 1998;66(6):883–892. doi: 10.1037/0022-006X.66.6.883. [DOI] [PubMed] [Google Scholar]
- Lalayants M, Prince JD. Loneliness and depression or depression-related factors among child welfare-involved adolescent females. Child and Adolescent Social Work Journal. 2015;32(2):167–176. doi: 10.1007/s10560-014-0344-6. [DOI] [Google Scholar]
- Leeb, R. T., Bitsko, R. H., Radhakrishnan, L., Martinez, P., Njai, R., & Holland, K. M. (2020). Mental health–related emergency department visits among children aged< 18 years during the COVID-19 pandemic—United States, January 1–October 17, 2020. Morbidity and Mortality Weekly Report, 69(45), 1675–1680. 10.15585/mmwr.mm6945a3 [DOI] [PMC free article] [PubMed]
- León Moreno, C., Musitu Ochoa, G., Cañas Pardo, E., Estevez Lopez, E., & Callejas Jerónimo, J. E. (2021). Relationship between school integration, psychosocial adjustment and cyber-aggression among adolescents. International Journal of Environmental Research and Public Health, 18(1), 108–117. 10.3390/ijerph18010108 [DOI] [PMC free article] [PubMed]
- Liu J, Zhou T, Yuan M, Ren H, Bian X, Coplan RJ. Daily routines, parent–child conflict, and psychological maladjustment among Chinese children and adolescents during the COVID-19 pandemic. Journal of Family Psychology. 2021;35(8):1077–1085. doi: 10.1037/fam0000914. [DOI] [PubMed] [Google Scholar]
- Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, Linney C, McManus MN, Borwick C, Crawley E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child & Adolescent Psychiatry. 2020;59(11):1218–1239. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- London B, Downey G, Bonica C, Paltin I. Social causes and consequences of rejection sensitivity. Journal of Research on Adolescence. 2007;17(3):481–506. doi: 10.1111/j.1532-7795.2007.00531.x. [DOI] [Google Scholar]
- Lonigan CJ, Shannon MP, Finch AJ, Jr, Daugherty TK, Taylor CM. Children's reactions to a natural disaster: Symptom severity and degree of exposure. Advances in Behaviour Research and Therapy. 1991;13(3):135–154. doi: 10.1016/0146-6402(91)90002-R. [DOI] [Google Scholar]
- López CM, Andrews AR, III, Chisolm AM, de Arellano MA, Saunders B, Kilpatrick DG. Racial/ethnic differences in trauma exposure and mental health disorders in adolescents. Cultural Diversity and Ethnic Minority Psychology. 2017;23(3):382–387. doi: 10.1037/cdp0000126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam DR, Hoyle RH, Newman JP. The perils of partialling: Cautionary tales from aggression and psychopathy. Assessment. 2006;13(3):328–341. doi: 10.1177/1073191106290562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoud, A. B., Ball, J., Rubin, D., Fuxman, L., Mohr, I., Hack-Polay, D., & Wakibi, A. (2022). Pandemic pains to Instagram gains! COVID-19 perceptions effects on behaviours towards fashion brands on Instagram in sub-Saharan Africa: Tech-native vs non-native generations. Journal of Marketing Communications,1–25. 10.1080/13527266.2021.1971282
- Manduca, R. (2018). Income inequality and the persistence of racial economic disparities. Sociological Science, 5, 182–205.10.15195/v5.a8
- Matthews, T., Caspi, A., Danese, A., Fisher, H. L., Moffitt, T. E., & Arseneault, L. (2022). A longitudinal twin study of victimization and loneliness from childhood to young adulthood. Development and Psychopathology,1–11. 10.1017/S0954579420001005 [DOI] [PMC free article] [PubMed]
- Merikangas, K. R., He, J. P., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., ... & Swendsen, J. (2010). Lifetime prevalence of mental disorders in US adolescents: results from the national comorbidity survey replication–adolescent supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed]
- Miočević M, O'Rourke HP, MacKinnon DP, Brown HC. Statistical properties of four effect-size measures for mediation models. Behavior Research Methods. 2018;50(1):285–301. doi: 10.3758/s13428-017-0870-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Meesters C, van den Berg S. Internalizing and externalizing problems as correlates of self-reported attachment style and perceived parental rearing in normal adolescents. Journal of Child and Family Studies. 2003;12(2):171–183. doi: 10.1023/a:1022858715598. [DOI] [Google Scholar]
- Oosterhoff B, Palmer CA, Wilson J, Shook N. Adolescents' motivations to engage in social distancing during the COVID-19 pandemic: Associations with mental and social health. Journal of Adolescent Health. 2020;67(2):179–185. doi: 10.1016/j.jadohealth.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn T, Weatherburn P, French RS. Interventions to address loneliness and social isolation in young people: A systematic review of the evidence on acceptability and effectiveness. Journal of Adolescence. 2021;93:53–79. doi: 10.1016/j.adolescence.2021.09.007. [DOI] [PubMed] [Google Scholar]
- Pan, Y., Yang, Z., Han, X., & Qi, S. (2021). Family functioning and mental health among secondary vocational students during the COVID-19 epidemic: A moderated mediation model. Personality and Individual Differences,171. 10.1016/j.paid.2020.110490 [DOI] [PMC free article] [PubMed]
- Patrick SW, Henkhaus LE, Zickafoose JS, Lovell K, Halvorson A, Loch S, Letterie M, Davis MM. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics. 2020;146(4):e2020016824. doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Perlman D, Peplau LA. Toward a social psychology of loneliness. In: Duck S, Gilmour R, editors. Personal relationships in disorder. Academic Press; 1981. pp. 31–56. [Google Scholar]
- Racine N, Korczak DJ, Madigan S. Evidence suggests children are being left behind in COVID-19 mental health research. European Child & Adolescent Psychiatry. 2020 doi: 10.1007/s00787-020-01672-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatrics. 2021;175(11):1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos B, Jaccard J, Guilamo-Ramos V. Dual ethnicity and depressive symptoms: Implications of being Black and Latino in the United States. Hispanic Journal of Behavioral Sciences. 2003;25(2):147–173. doi: 10.1177/0739986303025002002. [DOI] [Google Scholar]
- Ravens-Sieberer U, Kaman A, Erhart M, Otto C, Devine J, Löffler C, Hurrelmann K, Bullinger M, Barkmann C, Siegel NA, Simon AM, Wieler LH, Schlack R, Hölling H. Quality of life and mental health in children and adolescents during the first year of the COVID-19 pandemic: Results of a two-wave nationwide population-based study. European Child & Adolescent Psychiatry. 2021 doi: 10.1007/s00787-021-01889-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Greytak EA, Parsons JT, Ybarra ML. Gender minority social stress in adolescence: Disparities in adolescent bullying and substance use by gender identity. The Journal of Sex Research. 2015;52(3):243–256. doi: 10.1080/00224499.2014.886321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren X. Pandemic and lockdown: A territorial approach to COVID-19 in China, Italy and the United States. Eurasian Geography and Economics. 2020;61(4–5):423–434. doi: 10.1080/15387216.2020.1762103. [DOI] [Google Scholar]
- Richtel, M. (2021). Surgeon general warns of Youth Mental Health Crisis. The New York Times. https://www.nytimes.com/2021/12/07/science/pandemic-adolescents-depression-anxiety.html. Accessed 9 Sept 2021.
- Roberts RE, Lewinsohn PM, Seeley JR. A brief measure of loneliness suitable for use with adolescents. Psychological Reports. 1993;72:1379–1391. doi: 10.2466/pr0.1993.72.3c.1379. [DOI] [PubMed] [Google Scholar]
- Rose, A. J., Swenson, L. P., & Waller, E. M. (2004). Overt and relational aggression and perceived popularity: developmental differences in concurrent and prospective relations. Developmental Psychology, 40(3), 378–387. 10.1037/0012-1649.40.3.378 [DOI] [PubMed]
- Rubens SL, Felix ED, Hambrick EP. A meta-analysis of the impact of natural disasters on internalizing and externalizing problems in youth. Journal of Traumatic Stress. 2018;31(3):332–341. doi: 10.1002/jts.22292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD. Gender differences in emotional responses to interpersonal stress during adolescence. Journal of Adolescent Health. 2002;30(4, Suppl):3–13. doi: 10.1016/S1054-139X(01)00383-4. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C. Age and gender as determinants of stress exposure, generation, and reactions in youngsters: A transactional perspective. Child Development. 1999;70(3):660–677. doi: 10.1111/1467-8624.00048. [DOI] [PubMed] [Google Scholar]
- Sadowski, C. M., & Friedrich, W. N. (2000). Psychometric properties of the trauma symptom checklist for children (TSCC) with psychiatrically hospitalized adolescents. Child Maltreatment, 5(4), 364–372. 10.1177/1077559500005004008 [DOI] [PubMed]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7(2):147–177. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Schinka KC, van Dulmen MH, Mata AD, Bossarte R, Swahn M. Psychosocial predictors and outcomes of loneliness trajectories from childhood to early adolescence. Journal of Adolescence. 2013;36(6):1251–1260. doi: 10.1016/j.adolescence.2013.08.002. [DOI] [PubMed] [Google Scholar]
- Shafran R, Coughtrey A, Whittal M. Recognising and addressing the impact of COVID-19 on obsessive-compulsive disorder. The Lancet Psychiatry. 2020;7(7):570–572. doi: 10.1016/s2215-0366(20)30222-4. [DOI] [PubMed] [Google Scholar]
- Smith SR. Making sense of multiple informants in child and adolescent psychopathology: A guide for clinicians. Journal of Psychoeducational Assessment. 2007;25(2):139–149. doi: 10.1177/0734282906296233. [DOI] [Google Scholar]
- Twenge JM, Haidt J, Blake AB, McAllister C, Lemon H, Le Roy A. Worldwide increases in adolescent loneliness. Journal of Adolescence. 2021;93:257–269. doi: 10.1016/j.adolescence.2021.06.006. [DOI] [PubMed] [Google Scholar]
- United Nations. (2020). Policy Brief: The impact of COVID-19 on children. https://unsdg.un.org/resources/policy-brief-impact-covid-19-children/. Accessed 9 Sept 2021.
- Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychological Methods. 2013;18(2):137–150. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanhalst J, Luyckx K, Goossens L. Experiencing loneliness in adolescence: A matter of individual characteristics, negative peer experiences, or both? Social Development. 2014;23(1):100–118. doi: 10.1111/sode.12019. [DOI] [Google Scholar]
- Wang, M. T., Henry, D. A., Scanlon, C. L., Del Toro, J., & Voltin, S. E. (2022). Adolescent psychosocial adjustment during COVID-19: An intensive longitudinal study. Journal of Clinical Child & Adolescent Psychology,1–16. 10.1080/15374416.2021.2007487 [DOI] [PubMed]
- Weiss RS. Loneliness: The experience of emotional and social isolation. The MIT Press; 1973. [Google Scholar]
- Weymouth BB, Buehler C, Zhou N, Henson RA. A meta-analysis of parent–adolescent conflict: Disagreement, hostility, and youth maladjustment. Journal of Family Theory & Review. 2016;8(1):95–112. doi: 10.1111/jftr.12126. [DOI] [Google Scholar]
- Widom CS, Czaja S, Wilson HW, Allwood M, Chauhan P. Do the long-term consequences of neglect differ for children of different races and ethnic backgrounds? Child Maltreatment. 2013;18(1):42–55. doi: 10.1177/1077559512460728. [DOI] [PubMed] [Google Scholar]
- World Health Organization . General's opening remarks at the media briefing on COVID-19-11 March 2020. World Health Organization; 2020. [Google Scholar]
- Yurek, L. A., Vasey, J., & Sullivan Havens, D. (2008). The use of self-generated identification codes in longitudinal research. Evaluation Review, 32(5), 435–452. 10.1177/01938 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.