Abstract
Idiopathic nephrotic syndrome is the most frequent pediatric glomerular disease, affecting from 1.15 to 16.9 per 100,000 children per year globally. It is characterized by massive proteinuria, hypoalbuminemia, and/or concomitant edema. Approximately 85–90% of patients attain complete remission of proteinuria within 4–6 weeks of treatment with glucocorticoids, and therefore, have steroid-sensitive nephrotic syndrome (SSNS). Among those patients who are steroid sensitive, 70–80% will have at least one relapse during follow-up, and up to 50% of these patients will experience frequent relapses or become dependent on glucocorticoids to maintain remission. The dose and duration of steroid treatment to prolong time between relapses remains a subject of much debate, and patients continue to experience a high prevalence of steroid-related morbidity. Various steroid-sparing immunosuppressive drugs have been used in clinical practice; however, there is marked practice variation in the selection of these drugs and timing of their introduction during the course of the disease. Therefore, international evidence-based clinical practice recommendations (CPRs) are needed to guide clinical practice and reduce practice variation. The International Pediatric Nephrology Association (IPNA) convened a team of experts including pediatric nephrologists, an adult nephrologist, and a patient representative to develop comprehensive CPRs on the diagnosis and management of SSNS in children. After performing a systematic literature review on 12 clinically relevant PICO (Patient or Population covered, Intervention, Comparator, Outcome) questions, recommendations were formulated and formally graded at several virtual consensus meetings. New definitions for treatment outcomes to help guide change of therapy and recommendations for important research questions are given.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00467-022-05739-3.
Keywords: Steroid-sensitive nephrotic syndrome, SSNS, Children, Frequently relapsing nephrotic syndrome, Steroid-dependent nephrotic syndrome, Steroid toxicity, Pediatrics, Immunosuppressive treatment
Introduction
Idiopathic nephrotic syndrome (INS), characterized by massive proteinuria, hypoalbuminemia, and/or concomitant edema is the most frequent glomerular disease in children. Its incidence ranges from 1.15 to 16.9 per 100,000 children and varies by ethnicity and region [1, 2]. Until the discovery of glucocorticoids as an effective treatment to induce remission in the 1950s, childhood nephrotic syndrome (NS) was associated with a high mortality (ca. 40%) due to acute kidney injury (AKI), chronic kidney disease (CKD), systemic infections, and thromboembolic events. The majority of affected children (ca. 85%) show complete remission of proteinuria within 4–6 weeks with daily prednisolone/prednisone (PDN) and have steroid-sensitive NS (SSNS). However, about 70–80% of patients will experience at least one relapse during follow-up. About 50% of patients have frequent relapses or are steroid-dependent [1, 3–5]. Childhood onset SSNS may resolve spontaneously following puberty; however, 10–30% continue to have a relapsing course into young adulthood [6–8]. Kidney biopsies are not routinely performed in children with SSNS because they have limited prognostic or clinical utility. If a biopsy is done the most common diagnoses are minimal change disease (MCD) showing either minimal changes, i.e., podocyte foot process effacement, or mild mesangial proliferation with IgM deposition, or less commonly focal-segmental glomerulosclerosis (FSGS) [9].
Management of relapsing SSNS is a great challenge. Long or frequent use of high-dose steroids is associated with steroid toxicity and reduction in quality of life (QOL) [10]. Several steroid-sparing agents are available but they can be associated with significant adverse effects [11–14]. The long-term goal of treatment of NS is to achieve freedom from recurrence, minimize side effects and improve QOL.
There are no international, evidence-based, systematically developed recommendations for the diagnosis and management of children with SSNS with the exception of a focused document from KDIGO [15]. Therefore, the International Pediatric Nephrology Association (IPNA) convened a clinical practice recommendation (CPR) workgroup in October 2019 to develop CPRs for the diagnosis and management of children with SSNS. This guideline provides evidence-based recommendations as well as a pragmatic approach to the management of SSNS. New definitions differing from previous ones, e.g., from KDIGO, for treatment outcomes are provided to help guide change of therapy in order to minimize the frequency of relapses and drug toxicity. Recommendations for future research to improve outcomes on children with INS are also presented.
Methods
Overview of the guideline project
We followed the RIGHT (Reporting Items for practice Guidelines in HealThcare) Statement for Practice Guidelines [16]. Three groups were assembled: a core leadership group, an external expert group, and a voting panel. The core group comprised 16 members of IPNA, including pediatric nephrologists and epidemiologists, an adult nephrologist, and a patient representative. The individual expertise and responsibilities of the core group members are given in Supplementary Table S1. The external expert group included three patient representatives, a general pediatrician, two pediatric endocrinologists, two experts in transition, and three dieticians. The patient representatives discussed the manuscript provided by the core group members within their local patient and family associations, and their suggestions were then incorporated into the manuscript. The voting panel included 32 pediatric nephrologists including 3–7 representatives of each IPNA Regional Society with expertise in the management of SSNS in children. Voting group members were asked by electronic questionnaire to provide a level of agreement on a 5-point scale (strongly disagree, disagree, neither agree/disagree, agree, strongly agree) (Delphi method). For topics that failed to achieve a 70% level of consensus, the recommendations were re-evaluated and modified by the core group and then reviewed again by the voting panel until a consensus level of > 70% was achieved.
Developing the PICO questions
We developed PICO (Patient or Population covered, Intervention, Comparator, Outcome) questions as follows [17]: Population: Children (> 3 months and < 18 years) with SSNS; Intervention and Comparators: Treatment compared with no treatment, other treatment or placebo; Outcomes Addressed: Recommendations for the treatment, and follow-up of children with SSNS (including efficacy to induce remission and side effects of medications). Definitions of nephrotic syndrome were reviewed and new definitions of treatment outcomes were developed.
Literature search
The PubMed database was searched for studies published by January 11, 2022; all systematic reviews of randomized controlled trials (RCTs) on the treatment of SSNS in children, prospective uncontrolled trials, observational studies, and registry studies on diagnosis and treatment of children with SSNS, restricted to human studies in English were retrieved. Where possible, risk ratios (RR) with 95% confidence intervals (CI) were cited from two Cochrane systematic reviews evaluating RCTs of interventions for childhood SSNS updated in 2020 [10, 12]. Further details and a summary of the publications used for this CPR are given in the supplementary material (Supplementary Tables S2-S10).
Grading system
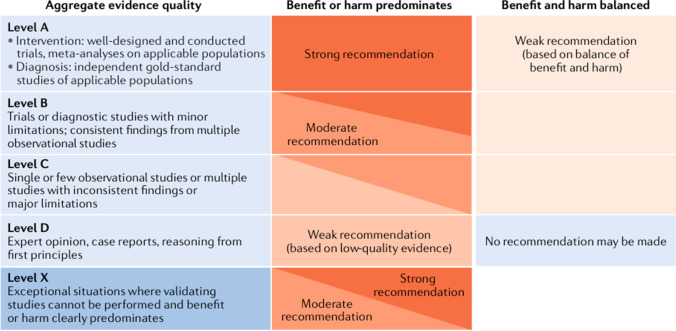
We followed the grading system of the American Academy of Pediatrics [18] (Fig. 1). The quality of evidence was graded as High (A), Moderate (B), Low (C), Very low (D), or Not applicable (X). The latter refers to exceptional situations where validating studies cannot be performed because benefit or harm clearly predominates. The letter X was used to grade contra-indications of therapeutic measures and safety parameters. The strength of a recommendation was graded as strong, moderate, weak, or discretionary (when no recommendation can be made).
Fig. 1.
Matrix for grading of evidence and assigning strength of recommendations as currently used by the American Academy of Pediatrics. Reproduced with permission from [23]
Clinical practice recommendations
Definitions and diagnostic work-up
Definitions
We recommend using the definitions given in Table 1 for the diagnosis and management of children with SSNS (grade X, moderate recommendation).
Table 1.
Definitions
| Term | Definition |
|---|---|
| Nephrotic-range proteinuriaa | Urinary protein creatinine ratio (UPCR) ≥ 200 mg/mmol (2 mg/mg) in a spot urine, or proteinuria ≥ 1000 mg/m2 per day in a 24-h urine sample corresponding to 3 + (300–1000 mg/dL) or 4 + (≥ 1000 mg/dL) by urine dipstick |
| Nephrotic syndrome | Nephrotic-range proteinuria and either hypoalbuminemia (serum albumin < 30 g/L) or edema when serum albumin is not available |
| Complete remission | UPCR (based on first morning void or 24 h urine sample) ≤ 20 mg/mmol (0.2 mg/mg) or < 100 mg/m2 per day, respectively, or negative or trace dipstick on three or more consecutive days |
| Partial remission | UPCR (based on first morning void or 24 h urine sample) > 20 but < 200 mg/mmol (> 0.2 mg/mg but < 2 mg/mg) and serum albumin ≥ 30 g/L |
| Steroid-sensitive nephrotic syndrome (SSNS) | Complete remission within 4 weeks of PDN at standard dose (60 mg/m2/day or 2 mg/kg/day, maximum 60 mg/day) |
| Steroid-resistant nephrotic syndrome (SRNS) | Lack of complete remission within 4 weeks of treatment with PDN at standard dose |
| Confirmation period | Time period between 4 and 6 weeks from PDN initiation during which responses to further oral PDN and/or pulses of IV MPDN and RAASi are ascertained in patients achieving only partial remission at 4 weeks. A patient not achieving complete remission by 6 weeks, although partial remission was achieved at 4 weeks, is defined as SRNS |
| SSNS late responder | A patient achieving complete remission during the confirmation period (i.e. between 4 and 6 weeks of PDN therapy) for new onset NS |
| Relapse | Urine dipstick ≥ 3 + (≥ 300 mg/dl) or UPCR ≥ 200 mg/mmol (≥ 2 mg/mg) on a spot urine sample on 3 consecutive days, with or without reappearance of edema in a child who had previously achieved complete remission |
| Infrequently relapsing nephrotic syndrome | < 2 relapses in the 6 months following remission of the initial episode or fewer than 3 relapses in any subsequent 12-month period |
| Frequently relapsing nephrotic syndrome (FRNS) | ≥ 2 relapses in the first 6-months following remission of the initial episode or ≥ 3 relapses in any 12 months |
| Steroid-dependent nephrotic syndrome (SDNS) | A patient with SSNS who experiences 2 consecutive relapses during recommended PDN therapy for first presentation or relapse or within 14 days of its discontinuation |
| Steroid toxicity | New or worsening obesity/overweight, sustained hypertension, hyperglycemia |
| Behavioral/psychiatric disorders, sleep disruption | |
| Impaired statural growth (height velocity < 25th percentile and/or height < 3rd percentile) in a child with normal growth before start of steroid treatment | |
| Cushingoid features, striae rubrae/distensae, glaucoma, ocular cataract, bone pain, avascular necrosis | |
| Sustained remission | No relapses over 12 months with or without therapy |
| SSNS controlled on therapy | Infrequently relapsing NS or sustained remission while on immunosuppression in the absence of significant drug-related toxicity |
| SSNS not controlled on therapy | Either frequently relapsing NS despite immunosuppression or significant drug-related toxicity while on immunosuppression |
| Secondary steroid resistance | SSNS patient who at a subsequent relapse does not achieve complete remission within 4 weeks of PDN at standard dose |
| Complicated relapse | A relapse requiring hospitalization due to one or more of the following: severe edema, symptomatic hypovolemia or AKI requiring IV albumin infusions, thrombosis, or severe infections (e.g., sepsis, peritonitis, pneumonia, cellulitis) |
aIn adults, nephrotic range proteinuria is defined by proteinuria > 3.5 g/24 h (or > 3000 mg/g or > 3 g/10 mmol creatinine) [15]. These cut-offs should also apply to adolescents (> 16 years)
Evidence and rationale
The definitions presented in this CPR agree with previously published IPNA Clinical Practice Recommendations for the diagnosis and management of children with steroid-resistant nephrotic syndrome (SRNS) [19] and the KDIGO 2021 Guideline for the Management of Glomerular Diseases [15, 20]. In addition, new definitions for treatment outcomes to help guide change of therapy, e.g., the introduction of steroid-sparing agents, are provided. Of note, patients with late response, i.e., remission between 4 and 6 weeks of PDN therapy, are defined as “SSNS late responder” and should be managed as SSNS but anticipating a potentially more severe course.
The proposed definition of frequently relapsing nephrotic syndrome (FRNS) differs from previous ones including those from KDIGO. The prescription for the first episode of SSNS usually amounts to a PDN exposure of ~ 115 mg/kg. Each relapse adds ~ 40–45 mg/kg; three relapses would mean 120–130 mg/kg, and four relapses would mean 160 mg/kg over 12 months. A child with 4 relapses in a year would thus be exposed to ~ 0.5 mg/kg/day PDN, which may not be acceptable in terms of toxicity risk. Therefore, we propose to revise the definition of FRNS to include children with 2 or more relapses in the first 6 months of the disease, or 3 or more relapses in any 12-month period. The definition of FRNS as a disease classification serves as a clinical indicator that treatment strategies should be transitioned from responsive, ad hoc therapy to preventive or proactive therapy to reduce relapses and corticosteroid toxicity. Considering the spectrum of steroid-associated adverse effects, the anxiety that the fear of relapses causes in patients and families and the patient/family preferences for steroid minimization, the rationale for this change is two-fold. First, the new definition of FRNS promotes a discussion and selection of therapy for patients with FRNS, which incorporates patient/family preferences. Second, the new definition acknowledges the fact that many pediatric nephrology centers throughout the globe already implement this threshold in routine clinical practice to optimize steroid minimization.
Regarding steroid-dependent nephrotic syndrome (SDNS), the wording of the definition has been fine-tuned. The term “recommended PDN” has been added to promote a uniform steroid treatment in all children with NS both in relapse and in remission. Moreover, “PDN for first presentation or relapse” aims to clarify that patients relapsing during or 14 days after low-dose maintenance treatment with PDN are not steroid-dependent. It is only a relapse during or within 14 days after completing high-dose PDN (i.e., 2 mg/kg per day or 1.5 mg/kg on alternate days) discontinuation, that qualifies for this definition.
Regarding the definition of hypoalbuminemia, usually a cut-off of 30 g/L is used. However, there is significant variation between serum albumin assays in different laboratories. The 2021 KDIGO guideline states: “Laboratory-specific values: serum albumin should be measured by bromocresol purple (BCP; colorimetric) capillary electrophoresis (CE), or immunonephelometric (iMN) methods. Bromocresol green (BCG) methods can give erroneously high results” [20]. The values of serum albumin measured by BCG are about 5.5 g/L higher than those measured by the BCP, CE, or iMN methods [21], so the definition of the degree of hypoalbuminemia required to meet a definition of NS varies according to the method used for quantifying serum albumin concentration. The bias between different albumin assays may affect clinical decision-making [22]. However, as long as a specific method is used consistently based on local laboratory practice, changes in serial albumin concentration can be monitored over time.
Regarding statural growth, we suggest using the definition for impaired statural growth as recommended for children with CKD, i.e., a height velocity < 25th percentile and/or height < 3rd percentile [23]. Height velocity should be calculated based on an observation period of at least 6 months. We also suggest using the body mass index (BMI) cut off values for age and sex to define overweight (25–30 kg/m2) or obese (≥ 30 kg/m2) as recommended by the International Obesity Taskforce [24]. For all anthropometric analysis, national reference values should be applied, or if not available the World Health Organization (WHO) standards should be applied (https://www.who.int/tools/child-growth-standards/standards).
Clinical assessment
We recommend a work-up for the diagnosis of nephrotic syndrome (NS) in all children with gravity-dependent edema (grade A, strong recommendation).
We recommend using spot urine samples, preferably a first morning void, or alternatively a 24-h urine sample to assess proteinuria (grade B, moderate recommendation).
We recommend confirming nephrotic range proteinuria at least once by quantification of proteinuria before initiating treatment for the first episode (grade B, moderate recommendation).
Evidence and rationale
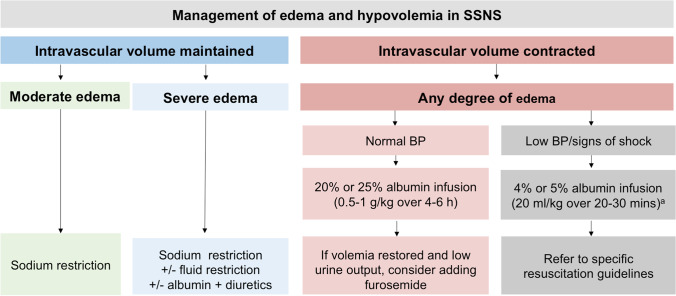
Periorbital edema is the leading clinical sign of NS in children with a typical presentation. It may be asymmetrical initially and is frequently misdiagnosed as allergy. Edema is gravity-dependent, localized to the lower extremities in the upright position, and to the eyelids and the dorsal part of the body in a reclining position. The edema is painless, soft and pitting, keeping the marks of clothes or finger pressure. Anasarca may develop with ascites, and pleural and pericardial effusions. Efforts are underway to standardize the assessment of edema. Complications of NS may be the presenting symptoms or signs of the disease (e.g., abdominal pain related to severe hypovolemia, ascites, peritonitis, or pneumonia, dyspnea as a consequence of pleural effusion, ascites, pneumonia, or pulmonary embolism).
Extrarenal causes of edema should be considered including hepatic (hepatocellular insufficiency, cirrhosis, Budd-Chiari syndrome), digestive (exudative enteropathy, coeliac disease, lymphangiectasis), severe malnutrition, heart failure, hereditary angioneurotic edema, capillary leak syndrome, and thyroid abnormalities.
The diagnostic laboratory finding in children with NS is nephrotic range proteinuria (Table 1) defined by 3 + on urine dipstick in a spot urine, a urinary protein creatinine ratio (UPCR) ≥ 200 mg/mmol (≥ 2 mg/mg) or proteinuria > 40 mg/m2/h or ≥ 1000 mg/m2/day in a 24-h urine collection (Table 1). The use of a spot urine may be preferred to avoid sampling error and because of its excellent correlation with 24-h urine protein excretion [25]. Although urinary dipstick analysis is useful for screening and home monitoring, we recommend confirming nephrotic range proteinuria at least once by quantification of proteinuria either by spot urine sampling (if possible, first-morning void) or on a 24-h sample before initiating treatment for the first episode. First morning urine samples help rule out orthostatic proteinuria during follow-up to diagnose relapses [25, 26]. Typical semiquantitative dipstick results are shown in Supplementary Table S11. UPCr is preferentially used in SSNS as the urinary albumin creatinine ratio, although more specific, is less relevant in nephrotic range proteinuria. In addition, there are no universally accepted definitions for nephrotic range proteinuria when using urinary albumin creatinine ratio.
Initial diagnostic work-up
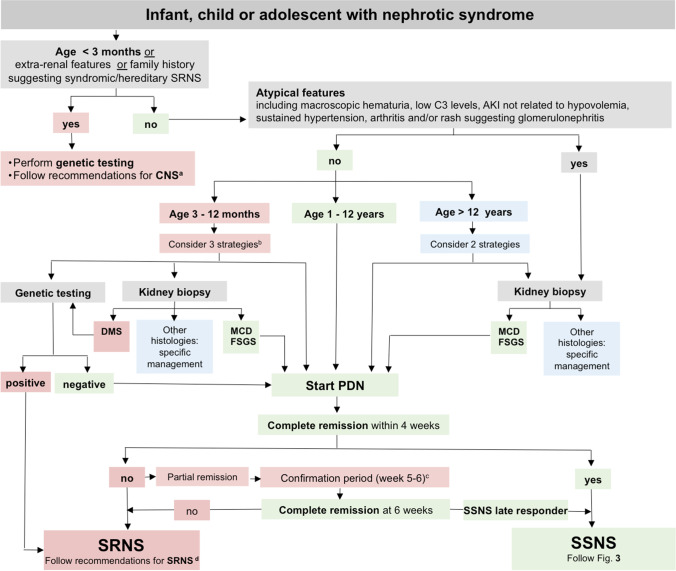
We recommend that children presenting with NS undergo a diagnostic work-up as outlined in Fig. 2 and Table 2 (grades are given in the table).
We do not recommend routine kidney biopsy and genetic testing in the initial diagnostic work-up of children with NS who present with typical features and age > 1 year (grade B, moderate recommendation).
We recommend considering genetic testing and/or kidney biopsy in infantile onset NS (age 3–12 months) (grade B, weak recommendation).
Fig. 2.
Algorithm for the initial management of a child with nephrotic syndrome. Patients are managed according to age, clinical presentation, and response to a 4-week treatment with oral prednisolone/prednisone (PDN). aIn children with congenital NS, we recommend following the published guideline for CNS [27]. bIn children between 3 and 12 months of age at onset (infantile NS), there is no evidence-based clear-cut approach to management. We suggest following one of the following three options in children without extrarenal manifestations: (i) primary genetic testing, if the results are rapidly available, with standard PDN treatment given if genetic testing is negative; (ii) primary kidney biopsy, followed by standard PDN treatment in the case of MCD and FSGS, genetic testing in the case of DMS, and specific treatment in the case of other underlying kidney histopathologies; (iii) starting standard PDN treatment, assessing at 4 weeks and then initiating genetic testing and kidney biopsy in case of SRNS. Patients > 1 year of age at onset are characterized according to response to a 4-week-treatment with oral prednisolone (PDN). We suggest that the decision of performing a kidney biopsy in older children (> 12 years) be made on a case-by-case basis. cPatients showing incomplete remission at 4 weeks enter the confirmation period in which responses to further oral prednisolone (PDN) with or without methylprednisolone (MPDN) pulses in conjunction with either angiotensin-converting enzyme inhibitors (ACEi) or angiotensin-receptor blockers (ARBs) are ascertained, and genetic and histopathological evaluation is initiated [19]. dIn children with SRNS, we recommend following the published recommendations for SRNS [19]. Further details are given in Table 2 and in the text. NS nephrotic syndrome, AKI acute kidney injury, CNS congenital NS, SSNS steroid-sensitive NS, SRNS steroid-resistant NS, MCD minimal change disease, FSGS focal segmental glomerulosclerosis, DMS diffuse mesangial sclerosis
Table 2.
Initial work-up for a child with nephrotic syndrome
| Investigations | Comments |
|---|---|
| Clinical evaluation | |
| Relevant patient history | |
| Presence of gravity-dependent edema | (grade A, strong recommendation) |
| Fever episodes, pain, abdominal discomfort, fatigue | |
|
Search for risk factors for secondary causes (e.g., sickle cell disease, HIV, systemic lupus erythematosus, hepatitis B, malaria, parvovirus B19, medications) Screen for tuberculosis |
Consider especially in patients from endemic areas before starting immunosuppressant medications (grade C, weak recommendation) |
| Physical examination | |
|
Blood pressure, assess volume status and extent of edema (ascites, pericardial and pleural effusions), lymphadenopathy Signs of infection (respiratory tract, skin, peritonitis, urinary tract) |
(grade A, strong recommendation) |
| Extrarenal features, e.g., dysmorphic features or ambiguous genitalia or eye abnormalities (microcoria, aniridia), rash, arthritis | Further work-up is recommended (grade A, strong recommendation) |
| Anthropometry | |
| Growth chart: height/length, weight, and head circumference (< 2 years) | We recommend comparing data with appropriate national standards or WHO-MGRS charts (grade A, strong recommendation) |
| Vaccination status | |
| Check/complete according to national standards esp., for encapsulated bacteria: pneumococcal, meningococcal, Haemophilus influenzae, Hep B, SARS-CoV2, influenza vaccine, and varicella | This is recommended before starting immunosuppressant medications other than PDN (grade B, moderate recommendation) |
| Family history | |
|
Kidney disease in family members Extrarenal manifestations HIV or tuberculosis in endemic regions Consanguinity |
(grade A, strong recommendation) |
| Biochemistry | |
| Spot urine | |
| Protein/creatinine ratio (in first morning void) | Recommended at least once before starting treatment of the first episode (grade B, moderate recommendation) |
| Urinalysis: including hematuria | |
| Blood | |
| Complete blood count, creatinine, eGFR, urea, electrolytes, albumin |
eGFR (mL/min/1.73 m2) = k height (cm)/serum creatinine (mg/dl), where k is a constant = 0.413 or eGFR (mL/min/1.73 m2) = k height (cm)/serum creatinine (µmol/l), where k is a constant = 36.5 [300, 301] |
| Complement C3, C4, antinuclear and anti-streptococcal antibodies, and ANCA | Recommended in patients with macroscopic hematuria (grade A, strong recommendation) |
| Varicella and MMR specific IgG, in non-immunized children | Consider before start of PDN treatment (grade D, weak recommendation) |
| Imaging | |
| Kidney ultrasound | Consider a kidney ultrasound in all children with INS to exclude kidney malformations and venous thrombosis and in patients with reduced eGFR, hematuria or abdominal pain and always before kidney biopsy (grade D, weak recommendation) |
| Chest X-ray | Recommended in case of suspected lymphoma (grade D, weak recommendation) |
| Histopathology | |
| Kidney biopsy | Recommended in patients with atypical features including macroscopic hematuria, low C3 levels, AKI not related to hypovolemia, sustained hypertension, arthritis and/or rash (grade A, strong recommendation) |
| Consider in patients with infantile onset NS if genetic screening is not available (age 3–12 months) (grade B, weak recommendation) (Fig. 2) | |
| Consider in patients > 12 years of age on a case-by-case basis (grade C, weak recommendation) | |
| Consider in patients with persistent microscopic hematuria in specific populations with a high incidence of glomerular diseases such as IgA nephropathy in East Asia (grade C, weak recommendation) | |
| Recommended in patients diagnosed with SRNS (grade A, strong recommendation) | |
| Genetic testing | Recommended in patients with congenital NS, extrarenal features and/or family history suggesting syndromic/hereditary SRNS (grade A, strong recommendation) |
|
Consider in patients with infantile onset NS (age 3–12 months) (grade C, weak recommendation) (Fig. 2) Recommended in patients diagnosed with SRNS (grade A, strong recommendation) | |
AKI acute kidney injury, eGFR estimated glomerular filtration rate, ANCA antineutrophil cytoplasmic antibodies
Evidence and rationale–Syndromic and familial NS
A physical examination for extrarenal features suggestive of genetic conditions is recommended (Table 2). Patients with extrarenal features suggestive of monogenic SRNS should primarily undergo genetic testing. Diagnostic work-up in patients with congenital NS (age < 3 months) should be done according to recent clinical practice recommendations [27, 28]. After the neonatal period, if family history is positive for SSNS, PDN therapy should be started as per this SSNS guideline. If family history is positive for a monogenic cause of SRNS, we recommend primary genetic testing.
Impact of typical presentation and age
In children, NS with onset at age above 1 year and typical presentation is most often SSNS associated with MCD. The likelihood of MCD is highest between ages 2 and 7 and decreases thereafter [9, 29]. Kidney biopsy allows the exclusion of the differential diagnoses (e.g., membranous nephropathy) and the confirmation of a primary podocytopathy (MCD, FSGS, or diffuse mesangial sclerosis (DMS)). Findings of DMS or membranous nephropathy have therapeutic implications as these entities are treated with specific protocols (membranous nephropathy) or may require genetic testing (DMS). Moreover, it allows the detection and grading of tubular atrophy, interstitial fibrosis, and glomerulosclerosis as prognostic markers [9].
However, there is not enough evidence to identify a clear age limit above which the probability is high enough for non-MCD pathology (e.g., membranous nephropathy), and thus the need for a kidney biopsy in children with NS. Therefore, we suggest that the decision of performing a kidney biopsy in older children (> 12 years) be made on a case-by-case basis. Atypical features suggesting the need for a kidney biopsy include macroscopic hematuria, low C3 levels, sustained hypertension, low estimated glomerular filtration rate (eGFR) not related to hypovolemia, arthritis and/or rash, or other extrarenal findings suggesting glomerulonephritis.
We also suggest a kidney biopsy be performed in patients with nephrotic syndrome and persistent microscopic hematuria in populations with a high incidence of glomerular diseases such as IgA nephropathy in East Asia. To reduce unnecessary kidney biopsies, the finding of more than 30 RBCs/HPF of fresh voided urine may be used as a criterion for performing a kidney biopsy in clinical practice [30].
Infantile onset NS
About 50% of children with infantile onset NS (age 3–12 months) have a genetic cause of NS which usually does not respond to PDN treatment [31, 32]. The finding of DMS on kidney biopsy is highly suggestive for an underlying genetic defect, i.e., pathogenic variants in WT1, PLCE1, or PDSS2 genes [33–36]. Therefore, we suggest following one of three strategies for infantile NS without extrarenal manifestations (Fig. 2): (i) primary genetic testing, if the results are rapidly available, with standard PDN treatment given if genetic testing is negative; (ii) primary kidney biopsy, followed by standard PDN treatment in the case of MCD and FSGS, genetic testing in the case of DMS, and specific treatment in the case of other underlying kidney histopathologies; and (iii) starting standard PDN treatment and then initiating genetic testing and kidney biopsy in case of SRNS.
Indications for referral to a pediatric nephrologist
- We recommend referral to a pediatric nephrologist in case of:
- Atypical features not consistent with idiopathic NS
- Positive family history for NS
- Congenital or infantile onset NS
- Age at onset of NS above 12 years
- Secondary NS
- SRNS
- SSNS late responder
- FRNS or SDNS
- SSNS patient with drug toxicities or complicated relapses (grade X, moderate recommendation)
Evidence and rationale
SSNS follows a chronic course in most children and ideally all children with SSNS should be cared for by or in conjunction with a pediatric nephrologist at the outset. In some countries, the scarcity of pediatric nephrologists or the distance from tertiary referral centres, require general pediatricians to take primary responsibility [37].
Primary immunosuppressive treatment of idiopathic NS
Dose, duration, and dosing strategy of PDN in the initial episode of NS
- After completing the initial diagnostic workup of a child presenting with nephrotic syndrome as outlined above, and a decision is made to start PDN, we recommend that infants > 3 months and children or adolescents (1–18 years) with their first episode of idiopathic NS should receive daily PDN for either:
- 4 weeks at 60 mg/m2 or 2 mg/kg (maximum dose 60 mg/day), followed by alternate day PDN at 40 mg/m2 or 1.5 mg/kg (maximum dose of 40 mg on alternate days) for 4 weeks, or
- 6 weeks at 60 mg/m2 or 2 mg/kg (maximum dose 60 mg/day), followed by alternate day PDN at 40 mg/m2 or 1.5 mg/kg (maximum dose of 40 mg on alternate days) for 6 weeks (grade A, strong recommendation).
We recommend administering oral PDN as a single morning dose for the treatment of the initial episode and subsequent relapses (grade B, moderate recommendation).
We do not recommend a tapering schedule during alternate day dosing (grade A, strong recommendation).
We suggest that PDN dose should be calculated by either weight or body surface area based on the estimated dry weight (grade B, weak recommendation).
Evidence and rationale
Glucocorticoids are widely used in the treatment of NS, and their efficacy is well-established in children > 1 year of age with a typical presentation. In children between 3 and 12 months of age at onset, there is no evidence-based clear-cut approach to management. The management approach should consider the availability of time-sensitive genetic testing. In the absence of extrarenal features, priority may be given either to genetic testing, kidney biopsy or starting PDN, and assessing at 4 weeks (vide supra) (Fig. 2).
Because approximately 50% of children will develop FRNS or SDNS, the use of PDN in longer initial courses has been extensively studied for its efficacy to reduce relapses (Supplementary Table S3). Contrary to earlier evidence suggesting a benefit of longer courses of PDN [38], four recently published well-designed RCTs at low risk of bias, which evaluated 775 children, demonstrated that prolongation of PDN therapy beyond 2 or 3 months in the initial episode of SSNS does not reduce the risk of relapse [39–42]. Since there are no adequately powered well-designed RCTs comparing 2 months with 3 months of PDN therapy, we recommend either an 8-week or a 12-week course of treatment of the initial episode of SSNS in line with KDIGO [15, 20] (Supplementary Table S3). The recent PREDNOS 2019 identified no differences in behavioral effects between different treatment durations [42]. Based on the available evidence, we recommend single daily PDN dosing.
Adverse effects of PDN in children with SSNS are common. An analysis of the adverse effects with PDN in 14 RCTs evaluating PDN therapy in the initial episode of SSNS with observation periods of 12–24 months found that hypertension (13%), psychological disorders (21%), cushingoid appearance (41%), and infections (22%) were common regardless of the total PDN induction dose used [10] (Supplementary Table S4). Future research recommendations are given in Supplementary Table S12.
Single daily dosing
Two small RCTs [43, 44] and one observational study [45] have demonstrated no differences in efficacy with a lower toxicity profile when PDN is administered as a single morning dose rather than divided doses. The potential benefits of the single-daily dose regimen include better adherence to therapy, lesser risk of hypothalamic–pituitary–adrenal (HPA) axis suppression and sleep disturbances. Dividing the dose has some practical considerations for medication use in children by minimizing the number of pills or volume of the liquid with each dose.
We do not recommend a tapering schedule during alternate day dosing. None of the four RCTs cited above used a tapering schedule of PDN in the experimental arm. Of the 775 children enrolled, there was only one possible case of adrenal suppression and that occurred in the control arm [41]. Treatment regimens in these four RCTs are shown in Table 3.
Table 3.
PDN treatment regimens in four well-designed RCTs at low risk of bias
| Initial dose and duration | Subsequent dose and duration (tapering) | ||
|---|---|---|---|
| Teeninga (2013) [40] | Arm 1 (3-month group) | 60 mg/m2 daily for 6 weeks | 40 mg/m2 AD for 6 weeks followed by placebo AD for 12 weeks |
| Arm 2 (6-month group) |
60 followed by *50 mg/m2daily for total 6 weeks *Switch to trial medication at remission |
40 and 20 mg/m2 AD for 4 weeks each followed by 10 mg/m2 AD for 10 weeks | |
| Sinha (2015) [39] | Arm 1 (3-month group) | 2 mg/kg daily for 6 weeks | 1.5 mg/kg AD for 6 weeks followed by placebo AD for 12 weeks |
| Arm 2 (6-month group) | 2 mg/kg daily for 6 weeks | 1.5 mg/kg AD for 6 weeks followed by 1, 0.75, and 0.5 mg/kg AD for 4 weeks each | |
| Yoshikawa (2015) [41] | Arm 1 (2-month group) | 60 mg/m2 daily for 4 weeks (Max. 80 mg) | 40 mg/m2 AD for 4 weeks (Max. 50 mg) |
| Arm 2 (6-month group) | 60 mg/m2 daily for 4 weeks (Max. 80 mg) | 60, 45, 30, 15, and 7.5 mg/m2 AD for 4 weeks each (Max. 80, 60, 40, 20, and 10 mg each) | |
| Webb (2019) [42] | Arm 1 (2-month group) | 60 mg/m2 daily for 4 weeks (Max. 80 mg) | 40 mg/m2 AD for 4 weeks (Max. 60 mg) |
| Arm 2 (4-month group) | 60 mg/m2 daily for 4 weeks (Max. 80 mg) | 60, 50, 40, 30, 20, and 10 mg/m2 AD for 2 weeks each (Max. 80 at start) |
AD on alternate days
Maximum dose of PDN
The traditional dose of PDN for induction of remission during the first episode of NS is 60 mg/m2 per day or 2 mg/kg per day. Most country-based or international guidelines [15, 46–48] recommend a maximum dose of 60 mg/day though the German guidelines recommend a maximum dose of 80 mg/day [46, 49]. No studies have formally evaluated the efficacy of doses higher than 60 or 80 mg/day in SSNS.
Although lower doses of PDN are associated with reduced risk of side effects, these doses may not be as effective. A single small RCT (n = 60) showed that a lower dose of PDN (40 mg/m2/day) during the initial episode of NS was associated with a longer time to remission compared to the standard dose (60 mg/m2 per day; 11.4 ± 4.0 vs. 9.6 ± 2.6 days) [50]. At 24 months, the sustained remission rate was lower in boys receiving 40 mg/m2 per day but there was no difference in girls [51]. A retrospective cohort of children with SSNS demonstrated that a lower cumulative dose of PDN (< 2500 mg/m2) used during the induction therapy for the first episode of NS is associated with shorter time to first relapse, higher rate of relapses and higher use of steroid-sparing agents, compared to higher doses (> 3000 mg/m2) [52]. Therefore, we recommend treating the first episode of NS with a dose of 60 mg/m2 per day (or 2 mg/kg per day).
Dosing by body surface area or weight
Younger children in particular will receive higher mg of PDN (up to 15% [53]) using a body surface area (BSA) compared to weight per kilogram dosing strategy. Limited knowledge exists regarding whether PDN dose should be calculated by weight or BSA. To avoid PDN overdosing in fluid-overloaded children, we suggest calculating the PDN dose based on the estimated dry weight. Two small RCTs [54, 55] with 146 participants compared weight-based dosing with BSA-based dosing in young children (weight < 30 kg, BSA < 1 m2) with their initial episode of SSNS and with relapse of SSNS. There were no statistically significant differences for efficacy or steroid toxicity when comparing weight-based versus BSA-based dosing of PDN but follow-up duration was short in both studies. One patient in the BSA group developed hypertensive encephalopathy [55]. Mean cumulative PDN dose was lower with weight-based dosing in both studies [54, 55]. When height is not available, PDN doses which approximate to 60 mg/m2 and 40 mg/m2 can be estimated from the formulae: 2 × weight + 8 and weight + 11, respectively [56].
Combined treatment with steroids and a non-steroidal agent for the initial episode of SSNS
We do not recommend adding other immunomodulatory or immunosuppressive drugs to PDN for the treatment of the initial episode of NS (grade C, weak recommendation).
Evidence and rationale
Studies aiming to reduce the number of relapses by adding a non-glucocorticoid immunosuppressive (steroid-sparing) agent to PDN therapy for the initial episode of NS are scarce. Zhang et al. studied the efficacy of adding azithromycin in combination with PDN therapy in children with their first presentation of NS [57]. The median duration before remission was 6 days in the group that received azithromycin in addition to PDN, and 9 days in the PDN alone group (p < 0.0001). There were no differences in terms of relapses at 6 months.
An RCT demonstrated that adding 8 weeks of cyclosporine (CsA) to PDN within the first 4 weeks of treatment of the first episode of NS (after establishing remission over 3 days) reduced the risk of first relapse within the first 6 months (RR 0.33, 95% CI 0.13–0.83), but no difference was observed at 12 months (RR 0.72, 95% CI 0.46–1.13) [58]. There are RCTs in progress in children studying the benefits of adding mycophenolate mofetil (MMF) [59] or levamisole (LEV) [60] to PDN during the initial episode of NS, as soon as children have entered remission, but there are no published results to inform the guideline. Moreover, a significant percentage of children with SSNS are infrequent relapsers and will never require a steroid-sparing agent. Therefore, due to the potential unnecessary side effects and to added cost, initial therapy combining steroids and a steroid-sparing agent cannot be currently recommended.
Type of steroid agent to induce remission/maintaining remission in children with SSNS
We recommend that prednisone and prednisolone be used interchangeably, and at the same dose, in both the initial presentation and relapse (grade B, moderate recommendation).
Evidence and rationale
For the management of childhood NS, both prednisone and prednisolone have been used interchangeably, and at an equivalent dose. Prednisone is a prodrug of prednisolone [61]. The conversion of prednisone to the biologically active prednisolone occurs mainly in the liver. This interconversion is not a limiting factor, even in patients with severely impaired liver function [62, 63]. NS does not influence the conversion of prednisone to prednisolone [64, 65]. Acute NS and the hypoalbuminemic state do not reduce absorption of PDN or the conversion of prednisone to prednisolone [65, 66]. In clinical practice, prednisolone and prednisone are usually given orally. Prednisolone is palatable and is the preferred choice for young children [67, 68].
Deflazacort vs. prednisone/prednisolone
Deflazacort is a synthetic glucocorticoid oxazoline derivative of prednisolone. Six milligrams of deflazacort have approximately the same anti-inflammatory potency as 5 mg of prednisolone or prednisone. There was no difference between deflazacort and PDN in the number achieving remission in the first episode of SSNS in two small RCTs [69, 70]. However, fewer children relapsed following deflazacort treatment compared with PDN [69, 71]. There is a report of toxic epidermal necrolysis in two children with NS who received deflazacort [72]. At this time, there are insufficient data to recommend the use of deflazacort rather than PDN in the treatment of NS.
Intravenous methylprednisolone at equivalent doses of oral prednisone (equivalent dose is 5 mg for every 4 mg of IV methylprednisolone) may be used in situations where a patient is unable to tolerate oral medications or if adherence may be a problem. Intravenous therapy should be limited to a short duration with the intent to switch back to oral medication at the earliest opportunity.
Monitoring during the acute phase and follow-up
- We recommend educating families to monitor urine protein at home to enable early identification of response to PDN and of relapses (grade X, moderate recommendation).
- We suggest using the heat coagulation or sulfosalicylic acid test as alternative methods for home monitoring if dipstick testing for proteinuria is not available (grade C, weak recommendation).
- We recommend regular monitoring for patients with NS during the acute phase and during follow up as outlined in Table 4 (grades are given in the table).
- We recommend considering a kidney biopsy in patients with SSNS during follow-up if the findings may influence therapy or clarify prognosis. This includes patients on prolonged CNI exposure (> 2 years) especially with high doses, and/or with signs of CNI toxicity such as unexplained decrease in eGFR (grade B moderate recommendation).
Table 4.
Monitoring during the acute phase and follow-up of a child with NS
| Investigations | Comments |
|---|---|
| Home monitoring | |
| Dipstick assessment (preferably in first morning void) | We recommend daily home urine dipstick testing until remission (grade X, moderate recommendation) |
| We suggest home urine dipstick testing, at least twice weekly in the first year, individualize thereafter (grade D, weak recommendation) | |
| We recommend daily testing if 1 + or more or during episodes of fever, infections and/or suspected relapse (edema) (grade X, moderate recommendation) | |
| Clinical evaluation | |
| Frequency of outpatient visits | We suggest outpatient visits every 3 months within the first year, individualized thereafter with more frequent visits in cases of relapse (grade D, weak recommendation) |
| Patient history | |
| Fever episodes, pain, abdominal discomfort, swelling, fatigue, increased appetite, weight gain, sleep disturbances, behavioral changes | Recommended at every visit. Points to infection or drug toxicity (grade A, strong recommendation) |
| Physical examination | |
| Blood pressure | Recommended at every visit (grade A, strong recommendation) |
| Assessment of volume status, including edema (ascites, pericardial and pleural effusions) | Recommended at every visit in patients in relapse (grade A, strong recommendation) |
| Drug toxicity (e.g., striae, Cushingoid features, avascular necrosis, acne, tremor, hirsutism, gum hyperplasia) | Recommended at every visit in patients on medication (grade A, strong recommodation) |
| Signs of infection (respiratory tract, skin, peritonitis, urinary tract) | Recommended at every visit (grade A, strong recommodation) |
| Ophthalmological exam (glaucoma, cataract) | Recommended yearly in patients on PDN (grade A, strong recommendation) |
| Anthropometry | |
| Growth chart: height/length, weight, and head circumference (< 2 years) | Recommended at every visit; data should be compared with appropriate national standards or WHO-MGRS charts (grade A, strong recommodation) |
| Calculation of BMI and annual height velocity | Recommended in patients who received PDN treatment within the last 12 months (grade A, strong recommendation) |
| Vaccination status | |
| Check/complete according to national standards esp., for encapsulated bacteria: pneumococcal, meningococcal, Hemophilus influenzae, Hep B, SARS-CoV2, influenza, and varicella-zoster | Suggested as appropriate (grade D, weak recommendation) |
| Biochemistry | |
| Spot urine | |
| Protein/creatinine ratio (preferably in first morning void) | Suggested as appropriate (pos. dipstick) (grade C, weak recommendation) |
| Blood | |
| Complete blood count, creatinine, eGFR, urea, electrolytes, albumin | Recommended as appropriate in patients on medication or with complicated relapses (grade A, strong recommendation) |
| MPA, CsA, TAC | We recommend (pharmacokinetic) blood monitoring in patients on medication as given in Table 5 (grade B, moderate recommendation) |
| 25-OH-vitamin D | Annually in patients with SDNS or FRNS (after three months of remission); aiming for levels > 20 ng/mL (> 50 nmol/l) (grade C, weak recommendation) |
| Imaging | |
| Kidney ultrasound | Recommended before kidney biopsy (grade A, strong recommendation) |
| Histopathology | |
| Kidney biopsy | We recommend considering a kidney biopsy in patients with SSNS during follow-up if the findings may potentially influence therapy or help assess prognosis (grade X, moderate recommendation) |
MPA mycophenolate acid, CsA cyclosporin A, TAC tacrolimus
Evidence and rationale
Monitoring of disease activity and potential complications is mandatory for adequate management of relapses and prevention of complications including drug toxicity as given in Table 4. Secondary SRNS should lead to further diagnostic work-up as previously recommended [19].
The mainstay of disease surveillance lies with regular home monitoring, usually by urine dipstick. In case of non-availability of dipsticks, the heat coagulation test or semi-quantitative testing with sulfosalicyclic acid may be used for detecting urine protein [73–76]. Details of performing the heat coagulation test are available in the supplementary material.
The main reason for clinical assessment during follow-up is to evaluate evidence of adverse effects of the disease and/or treatment. Chronic CNI exposure may result in nephrotoxicity, which is associated with dose and duration of CNI use [77]. Therefore, a kidney biopsy may influence therapy in patients with SSNS, i.e. transition to a non-CNI-based treatment regimen. This includes patients on prolonged CNI exposure (> 2 years) especially with high doses, and/or with signs of CNI toxicity such as unexplained decrease in eGFR.
First line therapy of relapsing SSNS
We recommend that SSNS relapse be treated with single daily dose of PDN (2 mg/kg per day or 60 mg/m2 per day, maximum 60 mg) until complete remission (UPCr ≤ 20 mg/mmol (0.2 mg/mg) or negative or trace dipstick on 3 or more consecutive days) and then decreased to alternate day PDN (1.5 mg/kg per dose or 40 mg/m2 per dose, maximum 40 mg) for 4 weeks (grade B, moderate recommendation).
We do not recommend a tapering schedule during alternate day dosing (grade A, strong recommendation).
Evidence and rationale
Children with uncomplicated, infrequent relapses are treated with daily PDN, 60 mg/m2 until complete remission followed by conversion to a reduced dose (40 mg/m2 per dose) on alternate days for 4 weeks [78] (see Supplementary Table S3.3). A single RCT assessed whether reducing the duration of alternate day PDN relapse therapy to 2 weeks after remission is non-inferior to the standard 4-week duration [79]. The time to first relapse, development of FRNS or SDNS, and adverse effects were similar in both groups. Cumulative dose of PDN was lower in the short duration group. Non-inferiority was not proven with this trial. A further RCT evaluated extension of the alternate-day treatment period from 36 to 72 days in children with FRNS/SDNS, with a comparable cumulative PDN dose in both groups [80]. The proportion of children relapsing within 6 months was not different between the study arms (58% long duration vs. 42% short duration, p = 0.26). A further study comparing a 2-week and 6-week period of alternate-day PDN with different cumulative PDN doses is ongoing [81] (Supplementary Table S3.3). As presented in the Section Hypothalamic–pituitary–adrenal axis suppression, below, the risk for adrenal suppression following limited use of PDN as prescribed for relapsing SSNS is very small and does not justify tapering of PDN following standard relapse treatment regimen as recommended.
Daily PDN treatment at onset of infection to prevent relapse
We do not recommend the routine use of a short course of low-dose daily PDN at the onset of an upper respiratory tract infection (URTI) for prevention of relapses (grade B, moderate recommendation).
We suggest considering a short course of low dose daily PDN at the onset of an URTI in children who are already taking low dose alternate day PDN and have a history of repeated infection-associated relapses (grade D, weak recommendation).
Evidence and rationale
The PREDNOS 2 RCT [82], which was adequately powered, generalizable to the overall SSNS population, and at low risk of bias, evaluated 271 children with NS and URTI. The study found no benefit of administering five days of low dose PDN (15 mg per m2 BSA which is equivalent to 0.5 mg/kg) at the onset of URTI in preventing relapse. The finding was consistent among subgroups of children receiving alternate day PDN or children receiving alternate day PDN and other immunosuppressive agents, although the study was powered for whole group analysis only. In contrast, four smaller RCTs [83–86] including between 36 and 89 patients, reported that using low dose daily PDN at the onset of a URTI reduced the number of children with a subsequent relapse. These four studies were all at high risk of bias for one or more study attributes and were conducted in different geographic regions as compared to the low risk of bias study. Poorly designed RCTs at increased risk of bias are more likely to overestimate the efficacy of a treatment due to confounding, and/or selective or underreporting of outcomes in treatment groups [87, 88]. The baseline risk of an URTI triggering a relapse determines the number needed to treat to prevent one relapse with the intervention. Within most of the studies considered here [83–86] and in a demographic study [89], the risk is approximately 50%, but it was much lower (20%) in PREDNOS 2. Overall, there is insufficient evidence to recommend the routine use of a short course of low-dose daily PDN at the onset of an URTI for prevention of relapses. However, such an approach may be considered in children already taking low-dose alternate day PDN and at a greater risk of URTI triggering relapse. A cost-effectiveness analysis of PREDNOS 2 showed giving daily oral PDN to be dominant in health economic terms [90]. This was due to a small cost benefit driven largely by the low-cost of PDN, and reduced health-related quality-of-life associated with a relapse for the small (but clinically non-significant) additional number of children who relapsed in the placebo arm [90]. (Further information is given in Supplementary Table S5).
Relapsing SSNS: second line treatment
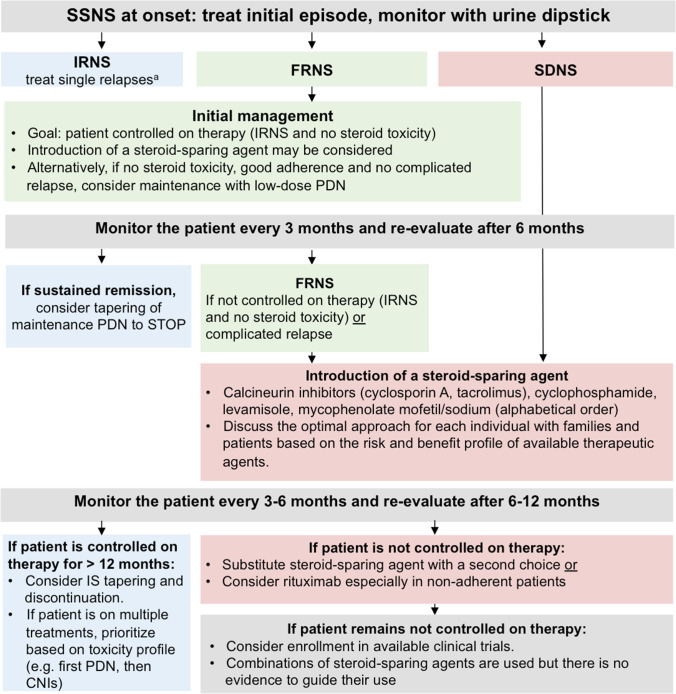
Optimal approach to children with FRNS and SDNS
We recommend the use of maintenance treatment (see Table 5) in all patients with FRNS or SDNS (grade B, moderate recommendation).
In patients with FRNS, we recommend either the introduction of a steroid-sparing agent as detailed below or low-dose maintenance PDN given as an alternate-day or a daily dose (grade A, strong recommendation).
- We recommend introduction of a steroid-sparing agent in children:
- who are not controlled on therapy, or
- who suffer a complicated relapse, or
- with SDNS (grade B, strong recommendation)
We recommend that the selection of the steroid-sparing agent be made in conjunction with patients or guardians in order to choose the most appropriate medication for each individual according to their values and preferences. This requires not only information on the efficacy of these medications, but also disclosure of possible side effects as listed in Table 5 (grade X, strong recommendation).
We recommend the introduction of one of the following steroid-sparing agents (alphabetical order): calcineurin inhibitors (CNIs), cyclophosphamide (CYC), levamisole (LEV), and mycophenolate mofetil (MMF)/mycophenolic sodium (MPS) (grade A, strong recommendation).
We recommend using RTX as a steroid-sparing agent in children with FRNS or SDNS who are not controlled on therapy after a course of treatment with at least one other steroid-sparing agent at adequate dose, especially in case of non-adherence (grade B, moderate recommendation).
We recommend switching to a different steroid-sparing agent when a patient is not controlled on therapy with the initial agent (grade X, strong recommendation).
We recommend considering tapering and discontinuation of maintenance treatment with PDN, LEV, MMF/MPS, or a CNI in all children in sustained remission for at least 12 months (grade X, moderate recommendation).
Table 5.
Dose, monitoring, adverse effects, and cost of all agents used as maintenance in FRNS and SDNS patients
| Therapeutic agent Dose |
Monitoring | Adverse Effects | Cost |
|---|---|---|---|
|
Low Dose Alternate-Day PDN ≤ 0.5 mg/kg/alt day, max 20 mg alt day |
Quarterly: blood pressure, height, weight Yearly: ophthalmological examination |
Obesity/weight gain, hypertension, diabetes mellitus, behavioral/psychiatric disorders, sleep disruption, growth failure, cushingoid features, striae rubrae/distensae, glaucoma, cataract, bone pain, avascular necrosis | Low |
|
Low Dose Daily PDN ≤ 0.25 mg/kg/day, max 10 mg/day | |||
|
Calcineurin inhibitors Cyclosporin A Start: 3–5 mg/kg per day (maximum dose 250 mg) in 2 divided doses, Target: C0 60–100 ng/mL or C2 300–550 ng/mL (aiming for the lowest possible dose to maintain remission) Tacrolimus Start: 0.1–0.2 mg/kg per day (maximum dose 10 mg) in 2 divided doses Target: C0 level between 3 and 7 ng/mL (aiming for the lowest possible dose to maintain remission) |
Quarterly: Blood pressure CBC, creatinine, eGFR, K+ LFTs, lipids Uric acid (CsA) Mg+ (TAC) Fasting glucose (TAC) Drug levels Consider discontinuation or a kidney biopsy after 2–3 years to avoid/detect toxicity |
Acute and chronic nephrotoxicity, hypertension, seizures, tremor, posterior reversible encephalopathy syndrome (PRES) Hirsutism (CsA), gum hyperplasia (CsA), diabetes mellitus (TAC) TAC drug levels can increase in case of intense diarrhea Consider risk of toxicity due to drug interactions (e.g., macrolide antibiotics, certain anti-epileptic agents, and grapefruit juice increase drug levels) |
Intermediate price, CsA less than TAC |
|
Cyclophosphamide 2 mg/kg per day (maximum dose 150 mg) over 12 weeks (oral) or 3 mg/kg per day (maximum dose 150 mg) over 8 weeks Single morning dose preferable No more than a single course (max TCD 168 mg/kg) Give in conjunction with alternate day oral PDN starting with a dose of 40 mg/m2 (1.5 mg/kg) and reducing to 10 mg/m2 (0.3 mg/kg) over the duration of treatment |
CBC every 14 days during therapy |
Leukopenia, severe infections, alopecia, nail discoloration, seizure, infertility, GI upset (abdominal pain, diarrhea), hemorrhagic cystitis, jaundice Fertile individuals must be warned of the need to avoid unplanned pregnancy (CYC can cause fetal malformation) |
Low |
|
Levamisole 2–2.5 mg/kg/alternate day (maximum dose 150 mg) In some cases, LEV is initially alternated with oral PDN on non-LEV days |
Quarterly: CBC, LFTs Twice-yearly: ANCA titers (also at baseline) |
Arthritis, vasculitic rash, neutropenia, abnormal LFTs | Low |
|
Mycophenolate mofetil (MMF)/mycophenolic sodium (MPS) MMF: Start: 1200 mg/m2 per day in two divided doses every 12 hoursa (maximum dose 3000 mg) MPS: 360 mg corresponds to 500 mg of MMF Therapeutic drug monitoring using a limited sampling strategy: The most effective MPA AUC0–12 is above 50 mg × h/Lb |
Quarterly: CBC LFTs |
Abdominal pain, diarrhea, weight loss (may be improved by the use of MPS). Leukopenia, anemia and abnormal LFTs Verrucae Fertile females must be warned of the need to avoid unplanned pregnancy (MMF/MPS can cause fetal malformations) |
High; MPS more expensive than MMF |
|
Rituximab 375 mg/m2 for 1–4 doses per course (maximum single dose 1000 mg) at weekly intervals Aim for CD19 depletion (< 5 cells/mm3 or < 1% total lymphocytes) Premedication is often used with antihistamine, paracetamol and steroids Repeated courses can be given Administer in remission after appropriate pre-medication under close supervision and monitoring Exclude hepatitis B and C, HIV, EBV, tuberculosis / any active infection |
Quarterly: CBC LFTs CD19 counts and % IgG (at baseline, quarterly in the 1st year, then yearly) |
Infusion reactions, infection, activation of latent viruses, transient or persistent IgG deficiency Serious adverse effects: tuberculosis, hepatitis B, or JC virus infection, myocardial dysfunction, risk of progressive multifocal leukoencephalopathy (PML) If infection is suspected, undertake diagnostic work-up including chest x-ray etc |
High |
CBC complete blood count, C0 trough level, C2 2 h post dosing, eGFR estimated glomerular filtration rate, CBC complete blood cells, LFTs liver function test, LEV levamisole; cyclosporin A, CsA; TAC, tacrolimus; GI gastrointestinal, AUC area under the curve
Evidence and grading are given in the text
aPatients may be started on half dose. Dosage may be increased after 1 week in case of no side effects, e.g., leucopenia or GI discomfort
bA limited sampling strategy for assessing pharmacokinetic profiles was validated in children with NS being in remission on MMF monotherapy. It requires three measurements of plasma MPA at times 0 min (before administration, C0), 60 min (C1), 120 min (C2) after administration), and allows a good estimation of MPA-AUC0-12 using the formula eMPA − AUC0−12 = 8.70 + 4.63 * C0 + 1.90 * C1 + 1.52 * C2 [152]. Alternatively, the formula: eMPA—AUC0−12 = 7.75 + (6.49 * C0) + (0.76 * C0.5) + (2.43 * C2) which was originally established in adult heart transplant patients treated with concomitant CsA can be used [108, 152, 153]
Evidence and rationale
SSNS is a relapsing–remitting condition. Children with frequent relapses, who require frequent courses of oral PDN, particularly in the presence of comorbidities, may develop steroid toxicity (Table 5). In children with FRNS or SDNS, it is necessary to balance risks and benefits of the intervention on an individual basis. The objective is to keep each patient controlled on therapy with minimal adverse effects. In some centers, the initial approach in children with FRNS is low-dose maintenance oral PDN, while in other centers a steroid-sparing agent is immediately started.
Low-dose maintenance PDN
The use of low-dose PDN in children with FRNS to maintain remission is primarily based on two historic small single-arm, uncontrolled studies with alternate day [91] or daily dosing [92]. Alternate-day dosing has been more widely adopted, although this is not evidence-based. A single open-label RCT [93] involving 61 patients with FRNS found that low dose daily (0.25 mg/kg) compared with alternate-day (0.5 mg/kg) PDN reduced the risk for relapse during 12 months of follow-up (0.55 relapses/person-year compared with 1.94 relapses/person-year) and lowered one year of PDN exposure (0.27 ± 0.07 versus 0.39 ± 0.19 mg/kg/day) with no differences in adverse effects. There was some clinical evidence of reduced glucocorticoid toxicity with the daily dosing schedule. The preferred use of daily or alternate-day low dose PDN for relapse prevention in FRNS requires additional study. Transition to steroid-sparing agents is recommended in patients not controlled on therapy as defined in Table 1.
Steroid-sparing agents
Steroid-sparing agents used in children with SSNS include CNIs (cyclosporin A (CsA), tacrolimus (TAC)), cyclophosphamide (CYC), immune modulators (levamisole (LEV), anti-proliferative agents (mycophenolate mofetil (MMF)/mycophenolic sodium (MPS)), and anti-CD20 monoclonal antibodies, primarily rituximab (RTX). There is insufficient evidence to establish the best initial option and the optimal sequence of agents from least to most effective or least to most toxic. The choice of agent should be based on family and physician preferences and the risk profile for drug-associated complications. Factors to consider include disease type/severity, age—including onset of puberty, potential adherence, side-effect profile, comorbidities, cost and availability. In the following sections, we discuss the pros and cons of each available agent and provide a roadmap, based on the available evidence, of reasonable choices based on the clinical features of each patient with SSNS. Regarding a switch from one steroid-sparing agent to another, the same considerations apply. Moreover, we have added the definition of “controlled on therapy” to provide a timeframe for this decision.
In Table 5, we provide dose, monitoring, adverse effects, and considerations on cost for therapeutic agents that are currently used for relapsing SSNS patients. In Supplementary Table S6, we provide GRADE-based evidence, given the available RCTs (Supplementary Table S7), on the different steroid-sparing therapeutic agents. An overview of recent observational studies on steroid-sparing therapeutic agents is given in Supplementary Table S8.
Calcineurin inhibitors
When using CNIs, we recommend therapeutic drug monitoring to ensure optimal dosing (see below) (grade B, moderate recommendation).
When using cyclosporin A (CsA), we recommend a starting dose of 3–5 mg/kg/day (maximum dose 250 mg) divided into 2 doses (every 12 h) to achieve trough blood levels of 60–100 ng/mL or 2 h post-dose levels of 300–550 ng/mL (grade B, moderate recommendation).
When using tacrolimus (TAC), we recommend a starting dose of 0.1–0.2 mg/kg/day (maximum dose 10 mg) in 2 doses (every 12 h) to achieve trough blood levels of 3–7 ng/mL (grade C, moderate recommendation).
We recommend that the lowest effective CNI dose should be given to maintain patients controlled on therapy (grade X, strong recommendation).
We recommend avoiding prolonged use of CNIs for more than a total of 2–3 years (grade B, moderate recommendation).
If CNIs have to be continued, we recommend that a kidney biopsy be considered after 2–3 years to exclude toxicity (grade B, moderate recommendation).
Evidence and rationale–Evidence for efficacy of CNIs in SSNS
CNIs have been used to treat relapsing SSNS for nearly 30 years [94–98]. Because of the lack of cosmetic side effects, TAC may be preferred to CsA. A Cochrane systematic review did not identify any RCTs comparing CsA with TAC in children with SSNS [12]. In Japan, an RCT comparing TAC and CsA is currently underway (jRCTs031180132, UMIN000004204).
Cyclosporin A
CNIs are effective in maintaining remission in children with FRNS and SDNS. A single RCT performed in Japan and including 108 children with FRNS/SDNS demonstrated that CsA compared with placebo reduced the risk of relapse (relapse rate ratio 0.55 (95% CI 0.37–0.82)) [99]. Observational studies have also demonstrated reduced relapse rates with CsA compared with PDN [95, 100–105]. However, many patients suffer relapses when CsA is ceased [101–104, 106]. Ishikura et al. reported that 84.7% of patients had a relapse within 2 years after completion of the 2-year CsA therapy and 59.2% of patients had regression to FRNS [106]. There are small RCTs comparing alkylating agents or MMF with CsA. Compared with alkylating agents, the number of patients relapsing by the end of therapy (6–9 months) on CsA may not differ (2 studies, 95 children: RR 0.91, 95% CI 0.55 to 1.48). However, following cessation of these medications and because the effect of alkylating agents but not CsA is prolonged after cessation, fewer children relapse after receiving alkylating agents compared with CsA alone (risk of relapse at 12–24 months; 2 studies, 95 children: RR 0.51, 95% CI 0.35 to 0.74) [12].
Two small RCTs suggested that the number of patients relapsing by 12 months may not differ between MMF and CsA (2 studies, 82 children: RR 1.90, 95% CI 0.66 to 5.46) but there is considerable imprecision in these findings. The addition of a third study to the meta-analysis indicated that the relapse rate/year may be higher with MMF than with CsA (mean difference 0.83 (95% CI 0.33 to 1.33) [12].
In RCTs, MMF is less likely to cause hypertrichosis and gum hypertrophy compared with CsA [12, 107–109] but no differences in other adverse effects (hypertension, impaired kidney function and infections) were identified. Three large observational studies [14, 110, 111] found higher efficacy in maintaining remission with CNIs compared with MMF. However, adverse effects were more common with CNIs.
Tacrolimus
The use of TAC in SSNS is based on the effectiveness of CsA in SSNS [95], on the results of observational studies [14, 97, 110] and the efficacy of TAC in pediatric kidney transplantation.
Cyclosporin A versus tacrolimus
There are no RCTs that compare TAC to CsA. A trial of TAC versus CsA for FRNS in children is being conducted in Japan (jRCTs031180132, UMIN000004204). Only small-number case series are available [98, 112–114]. Switching from CsA to TAC is only effective in reducing cosmetic side effects but warrants caution for the potential onset of diabetes mellitus [114].
Monitoring of CNIs
Patients should be monitored for side effects as indicated in Tables 4 and 5. Therapeutic drug monitoring indications are given below.
Cyclosporin A: toxicity profile
Nephrotoxicity is the most problematic side effect of CsA, and its risk is increased after use for > 2 years [115, 116]. CsA-induced chronic nephrotoxicity cannot be diagnosed based only on urinalysis or blood tests. It is advisable to avoid prolonged use of CsA and to consider its discontinuation or to perform a kidney biopsy after 2–3 years to avoid/detect toxicity. However, there is no definitive evidence supporting the necessity of kidney biopsy in SSNS treated with CNIs. Recent clinical studies of micro emulsified CsA [100, 117] have demonstrated a lower incidence of nephrotoxicity.
Cosmetic side effects, such as hypertrichosis and gum hyperplasia, are common with CsA [100–105]. Infections, hypertension, and posterior reversible encephalopathy syndrome (PRES) are also known complications of CsA therapy [100–105, 118].
Tacrolimus: toxicity profile
Among the side effects of TAC, new-onset diabetes mellitus is important. Particular caution is required when TAC is used in patients with a family history of diabetes mellitus or if risk factors for impaired glucose tolerance (e.g., obesity) are present [119]. Renal interstitial fibrosis has also been reported, as with CsA. One report described a significant association between higher TAC trough levels and renal interstitial fibrosis [112].
Cyclosporin A: therapeutic drug monitoring
The dose of CsA should be adjusted with drug monitoring based on assays validated against tandem mass spectrometry. According to a multicenter, prospective RCT of Sandimmun® conducted in Japan on 44 children with FRNS, sustained remission was significantly higher in the dose-adjusted group (initially the dose was adjusted to maintain blood trough levels within 80–100 ng/mL for the first 6 months, and then within 60–80 ng/mL for the next 18 months) compared with the 2.5 mg/kg fixed-dose group (initially the dose was adjusted to maintain blood trough levels within 80–100 ng/mL for the first 6 months, but then fixed at 2.5 mg/kg for the next 18 months) (50 vs. 15%; p < 0.01) [95]. A multicenter observational study assessed Neoral® [101], a microemulsified preparation of CsA, in 62 children with FRNS, with adjustment of the dose using the same target trough levels as stated above. This study reported that microemulsified CsA was effective and safe (relapse-free survival rate at month 24, 58%; incidence of nephrotoxicity, 8.6%), similar to conventional CsA [100].
The AUC0–4 (area under the time-concentration curve) of CsA is best predicted by C2 (CsA blood concentration at 2 h post-dose) in kidney transplant patients [120]. Similar findings were reported in children with NS [121]. A multicenter, prospective, RCT in Japan on 93 children with FRNS compared two different target C2 levels: a higher C2 group (target C2 600–700 ng/mL for the first 6 months, followed by 450–550 ng/mL for the next 18 months) and a lower C2 group (target C2 450–550 ng/mL for the first 6 months, followed by 300–400 ng/mL for the next 18 months) [94]. At 24 months, the relapse rate was significantly lower in the higher C2 group than the lower C2 group (0.41 vs. 0.95 times/person-year; hazard ratio, 0.43; 95% confidence interval, 0.19 to 0.84; p < 0.05). The rate and severity of adverse events were similar in both treatment groups [94].
Absorption of oral CsA after pre-meal administration (15–30 min prior to a meal) is greater than post-meal administration so it may be preferable to administer CsA before meals. The main priority is to give it in a consistent manner. Concomitant use with other drugs requires adequate attention since macrolide antimicrobials and many other drugs can affect metabolism. Grapefruit juice should be avoided as it inhibits metabolism of CsA and causes increased blood concentrations of the drug.
Tacrolimus: therapeutic drug monitoring
Tacrolimus requires adjustment of dosage by monitoring blood concentration. However, safe and effective dosage and mode of administration of TAC have not yet been established in children with SSNS. Suggested dosage and blood levels are extrapolated from data on kidney transplant recipients.
General considerations of benefit/risk of using CNIs
CsA is very effective in the treatment of FRNS/SDNS and allows steroid tapering and discontinuation in the majority of patients [95, 100–105]. The shortcoming of CsA therapy is that many patients experience relapse after termination of CsA therapy (CsA dependence) [101–104, 106]. Moreover, CNIs have a variety of side effects, including nephrotoxicity. In comparison to CsA, TAC has fewer cosmetic side effects.
Tapering and discontinuing of CNIs
If a child remains in sustained remission for at least 12–24 months and off steroids, CNI discontinuation should be considered to avoid nephrotoxicity [115, 116]. Tapering CNI dose to zero over about 3 months rather than discontinuing abruptly may be preferable because in case of a reappearance of proteinuria during tapering, reestablishing the initial CNI dose may be sufficient to avoid a relapse and a course of oral PDN while establishing that the patient still needs maintenance therapy.
Cyclophosphamide
When using cyclophosphamide (CYC):
We recommend starting when the patient is in steroid-induced remission and using either a single course of 2 mg/kg per day (maximum dose 150 mg) given orally for 12 weeks (grade B, moderate recommendation). or a single course of 3 mg/kg per day (maximum dose 150 mg) for 8 weeks given orally (grade B, moderate recommendation).
We recommend that the maximal cumulative dose of CYC not exceed 168 mg/kg (grade C, moderate recommendation).
We recommend that, if adherence is uncertain, a single course of monthly intravenous CYC (500 mg/m2 per dose (max single dose 1 g) × 6 months) can be given (grade B, moderate recommendation).
We suggest administering CYC in combination with alternate-day oral PDN starting with a dose of 40 mg/m2 (1.5 mg/kg) and reducing to 10 mg/m2 (0.3 mg/kg) over the course of treatment (grade D, weak recommendation).
We recommend monitoring for neutropenia (absolute neutrophil count < 1500/µL) with complete blood counts every 2 weeks (grade D, weak recommendation) and ceasing CYC if the child develops leukopenia (< 4000/µL) or neutropenia (< 1500/µL) or significant thrombocytopenia (< 50,000/µL) (grade X, strong recommendation) and restarting after recovery of blood cell counts using a lower dose (grade X, strong recommendation).
We recommend maintaining a high fluid intake to ensure a high urine output during treatment (grade C, moderate recommendation).
Evidence and rationale–Efficacy of CYC
A meta-analysis of 4 RCTs with 161 participants [12] comparing CYC with PDN or placebo showed a reduction in the number of relapses by 6 to 12 months (4 studies, 161 children; RR 0.47 [95% CI 0.34, 0.66]) [12]. A single course of monthly intravenous doses of CYC at a dose of 500 mg/m2 per dose (max single dose 1 g) × 6 months can be given when adherence is an issue [122, 123].
A review of 38 RCTs and observational studies assessing alkylating agents (CYC and chlorambucil) [13] including 1504 patients and 1573 courses and published between 1960 and 2000, indicated sustained remission rates of 72% after 2 years and 36% after 5 years for FRNS; the rates were 40% and 24%, for SDNS respectively. The maintenance of sustained remission declines with time, i.e., 44–57% at 1 year, 28–42% at 2 years, 13–31% at 5 years [124–128]. The effect may be lower in children below 3–5.5 years of age [125, 127, 129].
In comparison with CsA courses limited to 6–12 months (two RCTs), the actual percentage of sustained remission at 2 years for alkylating agents was higher, indicating that the effect of alkylating agents lasted longer than CsA after cessation of therapy [12]. One non-randomized comparator trial ([130], n = 46) suggests that RTX is non-inferior to CYC in maintaining remission over 1 year.
Cyclophosphamide treatment should be initiated after the patient has achieved remission and has been treated with the recommended dose of PDN for relapse. Published literature examining the use of CYC does not directly address whether co-intervention with PDN is necessary to reduce relapses or risk of adverse effects. Descriptions of continuation of PDN or concomitant administration of PDN while on CYC vary widely in the literature. Protocols ranged from PDN 10–40 mg/m2 either daily or alternate days, to 60 mg/m2 every other day. Tapering at the end of treatment was also highly variable [13, 96, 124, 131]. Due to substantial variation in practice, administering CYC in combination with alternate-day oral PDN starting with a dose of 40 mg/m2 (1.5 mg/kg) and reducing to 10 mg/m2 (0.3 mg/kg) over the duration of treatment was considered as reasonable practice by the guideline committee. Alternate-day oral PDN may help to reduce the risk of neutropenia when starting CYC initially.
Toxicity profile
Leukopenia occurred in 32.4% of patients on CYC and was more common with CYC alone than with CYC plus PDN protocols (22/38 vs. 8/52) [13]. The Latta meta-analysis reported reversible alopecia in 17.8%, infections in 1.5%, hemorrhagic cystitis in 2.2%, and malignancy in 0.2%. However, the cumulative dose used in many of the included studies was higher than current recommendations [13]. Studies using lower cumulative doses [124, 132] report transient leukopenia (7 to 23%) as the main adverse effect with transient alopecia and hemorrhagic cystitis occurring in ≤ 1%. However, long-term follow-up studies in patients who have been treated with these lower doses are lacking.
The incidence of gonadal dysfunction (amenorrhea and premature menopause in females and infertility for males and females) is dependent upon the patient’s age, sex, and cumulative dose of CYC, regardless of how the medication is administered [133–135]. Data compiled from 8 studies on 119 male patients [13] demonstrated a strong dose-dependent risk for infertility (see Supplementary Table S9).
Females: CYC may induce depletion of ovarian follicles and shrinkage and fibrosis of the ovaries. Women treated before the age of 25 are at a lower risk of infertility than those treated after the age of 30 [136]. CYC is associated with congenital (or fetal) malformations and should be avoided during the first 10 weeks of gestation.
Girls and younger women are less likely to experience ovarian failure with CYC exposure as they have a greater ovarian reserve. Thus, it appears that women < 20 years are unlikely to experience ovarian failure with an initial course of CYC (0 to 4%), whereas the risk is significant in women > 30 (23 to 54%) and > 40 (75%) [133, 137].
Males: CYC causes a decrease in sperm count and with higher doses and treatment duration can lead to irreversible azoospermia. The severity and risk of gonadal toxicity due to CYC depend on the gonadal activity at the time of treatment (prepubertal vs. sexually mature males) and the total cumulative dose. Testicular injury is reported to occur in boys and men after 7 to 9 g of CYC; recovery is documented in some patients [134]. Lentz et al. reported no increased risk of gonadal injury at total doses below 168 mg/kg [138]. Patients should be monitored for side effects as indicated in Tables 4 and 5.
Balance of risks and benefits
Alkylating agents, in particular CYC, have been used in pediatric NS for over 5 decades. Considering that other alkylating agents, i.e., chlorambucil, are currently rarely used for children with SSNS and showed a worse safety profile compared to CYC [13], we have focused on CYC. CYC is relatively inexpensive and monitoring requirements involve relatively inexpensive and readily available standard tests. Compared to agents like LEV, MMF and CNI, CYC is administered for a short-term course with a sustained effect after discontinuation. Thus, safety monitoring is needed for a shorter duration. The risk of gonadal toxicity is reduced with appropriate restriction of total cumulative dose. CYC should be used with caution in peri-pubertal males. The risk of hemorrhagic cystitis is very low with oral therapy at this recommended dose and with maintenance of fluid intake and diuresis. Leukopenia/neutropenia is the most common AE expected, and dose adjustment is a component of all protocols. Of note, CYC’s use requires additional treatment with oral PDN, which may promote further steroid toxicity. On balance, the potential risks of CYC may favor the use of other steroid-sparing agents, if available.
Levamisole
We recommend levamisole at a dose of 2–2.5 mg/kg given on alternate days (with maximum dose of 150 mg) after remission was achieved by PDN at recommended dose (grade B, moderate recommendation).
We recommend ANCA measurement at baseline, if available and every 6–12 months during therapy (grade X, moderate recommendation).
We recommend monitoring clinically for rash and measuring complete blood count and hepatic transaminases every 3–4 months (grade X, moderate recommendation).
Evidence and rationale–Efficacy evidence for levamisole
A recent international multicentre RCT has enhanced the quality of evidence for the effectiveness and safety of LEV. Gruppen (2018) [139] compared LEV therapy to placebo in 99 children with FRNS or SDNS and found a significant reduction in the number of relapses at 12 months (RR of relapses on LEV 0.77, 95% CI 0.61 to 0.97) [12]. Thus, 26% of children in the LEV group compared with 6% in the placebo group remained in remission at 12 months. Eight RCTs (474 participants) combined in a meta-analysis [12] indicated a benefit of LEV over PDN, placebo or no treatment (RR 0.52, 95% CI 0.33 to 0.82).
Small comparative RCTs comparing LEV with CYC [140, 141] showed no difference in efficacy but were not powered to show a difference. An RCT found no difference in efficacy between MMF and LEV but MMF levels were not measured [142]. The Gruppen 2018 [139] and Sinha 2019 [142] studies suggest that LEV may be more effective in FRNS than SDNS. These recent RCTs [139, 142] used a dose of LEV of 2.5 mg/kg/alternate day, maximum 150 mg, for 12 months. Most other recent studies used doses of 2–3 mg/kg on alternate days for 6–24 months. Some observational studies have used doses of 2–2.5 mg/kg daily for 4–24 months [143–149] with three studies [147–149] suggesting reductions in relapse rates in patients who had not responded to alternate-day LEV. These data require further larger RCTs, powered to detect a difference, if any, for confirmation.
Toxicity profile
Common adverse effects include rashes, leukopenia, and abnormal liver function tests. These are generally transient and reversible on discontinuation of therapy. Rarely ANCA positive arthritis (2% in Gruppen 2018 [139]), rash and other vasculitis symptoms have been reported, which resolve upon LEV discontinuation.
Balance of risks and benefits
While most adverse effects are transient and reversible on discontinuation, the main emerging threat is ANCA-positive vasculitis particularly with prolonged use. Regular monitoring as indicated in Tables 4 and 5 is advised with cessation of therapy if ANCA titers are positive.
Tapering/discontinuation
Available studies do not comment on this. Discontinuation without tapering should be considered once the patient is in sustained remission and off steroids for at least 12 months.
General considerations on the use of levamisole
LEV is an immunomodulant which has been used for over 3 decades in NS. Its low cost makes it a useful option, particularly in low resource settings. However, it is unavailable in some countries. Lack of nephrotoxicity and ease of monitoring are other major advantages. When introducing this agent, some physicians prefer to maintain low-dose alternate-day PDN on non-LEV days for a few months, then oral PDN is tapered and stopped, and the patient remains on LEV alone.
Mycophenolate mofetil/mycophenolic sodium
When using mycophenolate mofetil MMF, we recommend a starting dose of 1200 mg/m2 BSA (maximum dose 3000 mg) divided into two oral doses every 12 h (grade B, moderate recommendation).
Alternatively, we recommend using the corresponding mycophenolic sodium (MPS) dose, i.e., 360 mg of MPS corresponds to 500 mg MMF (grade B, moderate recommendation).
We suggest starting MMF/MPS therapy while the child is still receiving alternate-day steroid therapy since the immunosuppressive effect of MMF/MPS is delayed (grade C, weak recommendation). In most children, alternate-day steroids can then be tapered and discontinued within 6–12 weeks.
We recommend using therapeutic drug monitoring, aiming for a 12-h mycophenolic acid (MPA) area under the curve above 50 mg h/L in patients not controlled on MMF therapy despite using recommended dosing (grade B, moderate recommendation).
We recommend that sexually active adolescent females only receive MMF/MPS if they are using adequate contraception (grade X, strong recommendation).
Evidence and rationale–Dosing and therapeutic drug monitoring
The standard dose for MMF in RCTs is 1200 mg/m2/day divided into two doses every 12 h orally with a maximum daily dose of 3000 mg. Five hundred mg of MMF corresponds to 360 mg of MPS. Patients may be started on half dose and dosage may be increased after 1 week in case of no side effects, e.g., leukopenia or GI discomfort.
Monitoring of MMF/MPS
Patients should be monitored for side effects as indicated in Tables 4 and 5. Therapeutic drug monitoring indications are given below.
Therapeutic drug monitoring
Assessment of mycophenolic acid (MPA) trough levels is not recommended as there is a poor correlation with efficacy and safety using single pre-dose measurements [150, 151]. A limited sampling strategy for assessing pharmacokinetic profiles was established in children with NS on MMF monotherapy being in remission [152], whereas such a profile is not available for those on MPS. It requires three measurements of plasma MPA at times 0 min (before administration, C0), 60 min (C1), and 120 min (C2) after administration, and allows a good estimation of MPA-AUC0-12 using the formula eMPA − AUC0−12 = 8.70 + 4.63 * C0 + 1.90 * C1 + 1.52 * C2 [152]. In children with FRNS with MPA AUC0-12 > 50 mg × h/L estimated using the formula eMPA—AUC = 7.75 + (6.49 * C0) + (0.76 * C0.5) + (2.43 * C2) [108, 153], the efficacy of MMF was similar to that of CsA [108]. The latter formula was originally established in adult heart transplant patients treated with concomitant CsA. We recommend using therapeutic drug monitoring in patients not controlled on MMF therapy despite adequate dosing aiming for eMPA-AUC0-12 > 50 mg × h/L. For this purpose, either one of the above mentioned formulas can be used [108, 152, 153]. It should be noted that immunoassays for the determination of MPA plasma levels measure 10–20% higher MPA plasma levels than high-performance liquid chromatography (HPLC) or mass spectrometry (MS) due to cross-reactivity with MPA metabolites [154, 155].
Efficacy of MMF/MPS
No RCTs have compared MMF or MPS with PDN in children with FRNS or SDNS. However, numerous observational studies [156–160] (Supplementary Table S8) have reported that MMF or MPS are more effective than PDN in maintaining remission in children with FRNS or SDNS. These studies showed an approximately 50% reduction in the relapse rate on MMF/MPS, enabling reduction in dose or cessation of PDN. Studies have not specifically compared the relative efficacies of MMF/MPS in children with FRNS or SDNS.
Four RCTs compared MMF with other steroid-sparing agents in FRNS and SDNS. Three RCTs compared MMF with CsA in 142 children. Two RCTs [107, 108] combined in meta-analysis found no difference in the number of children with relapse between MMF and CsA (82 children: RR 1.90, 95% CI 0.66 to 5.46) [12]. However, the relapse rate/year was higher in children treated with MMF compared with CsA (3 studies, 142 children: mean difference 0.83, 95% CI 0.33 to 1.33) when a third study was included [12]. One RCT compared MMF with LEV and found no difference in the number of children with relapse at 12 months between treatments [142]. MPA levels were not measured in this study.
Three observational studies involving 312 children with FRNS or SDNS compared MMF with TAC [14, 110] or CsA [111]. MPA levels were not monitored in these studies. Two of these studies [14, 111] found better efficacy for maintaining remission with CNIs compared with MMF though adverse effects were more common with CNIs.
Toxicity profile
The most common adverse effects of MMF are abdominal pain, loss of appetite, diarrhea, and weight loss. This is less likely to occur with enteric-coated MPS. However, some individuals tolerate MMF better than MPS. Other adverse effects are leukopenia, anemia and elevated hepatic transaminases. These adverse effects are uncommon and usually mild. Monitoring for side effects should be done as indicated in Tables 4 and 5. MMF/MPS is teratogenic in the early months of pregnancy so effective contraception should be used by all sexually active female adolescents during MMF/MPS therapy. In males, recent evidence in patients receiving MMF/MPS after kidney transplantation and a large meta-analysis of different drugs [161] indicates that the risk of congenital malformations is comparable to that of the general population [162].
General considerations of benefit/risk of using MMF/MPS
There is now extensive documentation of the successful and safe use of MMF in children with FRNS and SDNS but studies did not differentiate between these groups. In clinical practice, MMF appears more effective in children with FRNS. Its advantages consist in lack of nephrotoxicity and of cosmetic side effects compared to CNIs.
Tapering and discontinuing of MMF/MPS
There are no studies on the duration of MMF/MPS use or on when to discontinue MMF/MPS. If the child achieves control on therapy for at least 12 months, then consideration may be given to tapering MMF over 3–6 months and then discontinuing it. As with CNIs, the advantage of tapering over abrupt discontinuation is that in case of proteinuria, re-establishment of MMF at initial dose may be sufficient to avoid a relapse while establishing that the child still requires maintenance treatment. The use of more extended periods may be considered, especially in peri-pubertal age or in the presence of previous severe steroid toxicity.
Rituximab
We recommend using RTX as a steroid-sparing agent in children with FRNS or SDNS who are not controlled on therapy after a course of treatment with at least one other steroid-sparing agent at adequate dose, especially in case of non-adherence (grade B, moderate recommendation). This is especially preferable, both in terms of safety and of effectiveness, above the age of 7–9 years (grade C, weak recommendation).
When using RTX, we recommend a dosage of 375 mg/m2 for each infusion, ranging from 1 to 4 infusions (maximum single dose 1000 mg) preferably when the patient is in remission (grade C, moderate recommendation).
We recommend monitoring CD19( +) total B cell counts at baseline and following RTX treatment at 7 days post-infusion to ensure adequate B cell depletion indicated by an absolute CD19 cell count < 5 cells/mm3 or < 1% of total lymphocytes (grade B, strong recommendation).
We recommend monitoring IgG levels at baseline and periodically following RTX treatment to detect hypogammaglobulinemia (IgG below age-related normal range) (grade B, strong recommendation).
We recommend premedication with paracetamol/acetaminophen, antihistamines and/or steroids (grade B, moderate recommendation).
Following RTX infusion/s, we recommend tapering off oral PDN and other steroid-sparing agents within 2–3 months (grade B, strong recommendation).
Evidence and rationale
In terms of dosing regimen, the original course of RTX used for lymphoma patients required 375 mg/m2 given as an IV infusion weekly for 4 doses. The RTX protocols used in the available RCTs and observational studies in children with FRNS/SDNS included single, 2, 4, and 7 infusions. In addition to variability in the number of RTX infusions, there has been variation in RTX dosing, ranging from 375 to 1500 mg/m2 per treatment, although most studies used 375 mg/m2. The dose of 750 mg/m2 has not been associated with a better response rate than 375 mg/m2; however, a lower dose of RTX (100 mg/m2) has been associated with the risk of earlier relapse (reviewed in [163] and in [164]). In terms of infusion number per course of RTX treatment, the use of a single infusion at standard dose followed by monitoring of CD19 ( +) cells at 7 days is derived from studies performed in adults with ANCA-associated renal vasculitis and membranous nephropathy. If at 7 days post-infusion, the percentage of total B cells is < 1% of total lymphocytes this indicates adequate B cell depletion [165]. Reconstitution of B cells is defined when total B cell counts are > 5/mm3 in absolute number [166].
Efficacy of RTX
During the last decade, a number of RCTs have shown that RTX is reasonably safe in the short term and relatively effective when compared to other immunosuppressants as a steroid-sparing treatment. However, studies differ in terms of populations, number of doses of RTX, additional medications and comparators. Unlike other immunosuppressants, the lack of long-term follow-up in RTX-treated patients must be considered at the time of clinical decision.
Eight RCTs have evaluated the efficacy of RTX in children with FRNS or SDNS. Four RCTs evaluated 1 to 4 doses of RTX in children with SDNS and CNI dependence compared with placebo [167, 168] or CNIs [169, 170]. Four studies compared 1 to 2 doses of RTX in children with SDNS or FRNS on low-dose PDN compared with TAC [171], low dose PDN [172, 173], or low dose MMF [174]. A meta-analysis showed that the number of patients with relapse fell by 80% by 6 months and 50% by 12 months after treatment [12]. Longer duration of remission was seen in children whose relapses were previously managed with PDN alone [172, 173]. Moreover, a large retrospective study assessing RTX use in more than 500 children with FRNS/SDNS showed that patients were 19% more likely to relapse for each additional steroid-sparing agent received prior to RTX, and that younger age at first infusion was associated with earlier relapse [164, 175, 176].
Toxicity profile
Adverse events were generally limited to mild infusion reactions. There was no increase in infections. RTX-related neutropenia (RRN) has been well documented in the literature, although the exact mechanism is not well known. In children, RRN is usually not associated with serious bacterial or viral infections and most of the reported infections are self-limiting. Supplementation with granulocyte colony stimulating factor (G-CSF) may not be needed, especially in late onset neutropenia, i.e., neutropenia occurring 4 weeks after last RTX infusion [177–179].
No deaths or serious adverse reactions were recorded in RCTs on the use of RTX in children with SSNS. While there are case reports of fatal lung fibrosis, immune-mediated ulcerative colitis, fulminant myocarditis, Pneumocystis jiroveci pneumonia following RTX use in children with SSNS, a retrospective survey of 511 children with SSNS and treated with RTX [180] identified only two children with life-threatening but non-fatal complications (Pneumocystis jiroveci pneumonia, myocarditis). However, prolonged and significant reduction of total memory and switched memory B cells together with hypogammaglobulinemia has been demonstrated in patients following RTX, particularly in young patients with SSNS [181].
Monitoring
Exclusion of certain infections and monitoring for side effects should be done as indicated in Tables 4 and 5.
General considerations of risk and benefit
RTX treatment has proven reasonably safe and effective for both FRNS and SDNS. Given its uncertain long-term safety profile, it is advisable to use RTX as a second-line steroid-sparing agent in children who are not controlled on therapy with a first-line steroid-sparing agent. Since long-term side effects such as hypogammaglobulinemia appear to be more likely and efficacy appears to be less convincing in younger children, the use of RTX may be reserved for older children.
Repeat infusion treatment with RTX
Following the first course of RTX, diverse approaches to repeated courses have been proposed, based either on disease relapse, on B cell reconstitution or on time elapsed from the initial treatment. Evidence for the most correct approach is lacking [164]. Based on a recent retrospective survey, 30 of 346 included children tolerated up to 7 courses of RTX infusions (mainly dosed with 375 mg/m2/course) with an acceptable side effect profile (most common hypogammaglobulinema, followed by infections and neutropenia) and good efficacy [182].
Tapering and discontinuing of other immunosuppressive agents post-RTX
It is unknown to what degree other immunosuppressive agents should be tapered or discontinued following RTX administration. In most studies, PDN at alternate-day doses was tapered off within 2 months before CNIs were reduced and stopped. If patients were taking MMF and mizoribine, these drugs were discontinued after the first dose of RTX. A recent study [180] demonstrated that treatment response depends on both RTX dose and on the use of maintenance immunosuppression. The study documented that in complicated FRNS and SDNS patients, giving “low dose”, i.e., 375 mg/m2 RTX and maintaining immunosuppression (IS), most frequently with MMF but in some cases with either CNI or oral PDN, was equivalent in terms of median relapse-free period to giving higher doses without maintaining IS after RTX [180]. In SDNS, a small prospective cohort study found that relapse-free survival 12 months after RTX therapy was higher in children receiving MMF than in children not receiving MMF [183]. An RCT evaluating MMF post-RTX treatment in “complicated” FRNS and SDNS showed that this approach was helpful in preventing relapse in 80% of patients [166]. An RCT comparing maintenance MMF to repeated RTX infusions in children with SDNS is ongoing (RITURNS II Study, NCT03899103). The use of CNIs following RTX infusions may be equally helpful, but this has not been formally assessed. These data suggest that in children with SDNS not controlled on RTX alone, following subsequent RTX infusions, the strategy of maintaining an oral steroid-sparing agent (MMF or a CNI) for at least 6 months may promote sustained remission.
RTX discontinuation
As with all steroid-sparing agents and even more with RTX given its long-lasting effect, once the child is controlled on therapy, RTX infusions should be discontinued.
Other anti-CD20 monoclonal antibodies
In addition to RTX, other monoclonal antibodies targeting B cells or modulating their function or depleting plasma cells have been employed in the treatment of SSNS.
Ofatumumab
Ofatumumab, in contrast to rituximab, is a fully humanized anti-CD20 monoclonal antibody. A case report described two boys, aged 3 and 14 years, with persistent SSNS, who were allergic to rituximab. Both children achieved a prolonged remission exceeding 12 months following the administration of a single dose of ofatumumab [184]. However, a recent clinical trial comparing RTX and ofatumumab in randomized 140 children with SDNS and found that there was no difference in the percentage of participants who relapsed at 12 or 24 months [185].
Combination of more than one steroid-sparing agent
We recommend enrolling children with severe FRNS or SDNS who have failed to achieve stable remission or who present significant treatment toxicity despite at least one steroid-sparing agent at adequate dose, in a clinical trial, if available (grade X, strong recommendation).
Evidence and rationale
The combination of different steroid-sparing agents is not supported by adequate evidence. There are no RCTs that compare the combination of CNI plus MMF vs. CNI or MMF alone. There is a single observational study involving 130 Pakistani children with SSNS. Of these 20 had suboptimal response to MMF and CsA was added. Nineteen out of 20 benefited but only 4 had CR and 9 were CNI-dependent. In a retrospective publication on the use of RTX [180], the prolonged use of MMF or other steroid-sparing agents following a single cycle of RTX was found to induce stable remission in those receiving low-dose RTX (375 mg/m2 per course) but there was no increase in benefit in those receiving higher doses of RTX (750 mg/m2 or higher). We suggest that if children with FRNS or SDNS are controlled on therapy with more than one immunosuppressant (i.e., steroid-sparing agent plus maintenance PDN or CNI plus MMF), discontinuation of the most toxic agent be implemented.
Other steroid-sparing agents
We recommend that mizoribine, azithromycin, azathioprine or adrenocorticotropic hormone (ACTH) not be used to treat children with SSNS (grade B, moderate recommendation).
Evidence and rationale
A single RCT found no definitive benefit of azithromycin compared with PDN in the initial episode of SSNS [57]. Single RCTs found no benefit of azathioprine, ACTH or mizoribine in children with FRNS/SDNS [186–188].
Adjunctive measures
Management of volume status, edema, and blood pressure
General measures
We recommend evaluating the volume status of a child in the acute nephrotic state (grade A, strong recommendation).
We do not recommend routine fluid restriction in SSNS patients (grade C, moderate recommendation).
We suggest fluid restriction in case of hyponatremia (< 130 meq/L) and/or severe edema in a hospital setting (grade C, weak recommendation).
We recommend a low-salt diet (suggested maximum dose of 2–3 meq/kg/day) during relapses with moderate or severe edema, and normal salt intake while in remission (grade C, moderate recommendation).
We recommend monitoring for hypertension in all children with SSNS and following current hypertension guidelines in children with confirmed, persistent hypertension (grade A, strong recommendation).
We recommend against ACEi or ARBs administration in SSNS to control edema or high blood pressure in relapse (grade X, strong recommendation).
In case of hypovolemia or AKI
In patients with signs of hypovolemia, we recommend withholding diuretics due to the risk of thrombosis, hypovolemic shock and AKI, and discontinuing ACEi or ARBs (grade X, strong recommendation).
We recommend using 20% or 25% albumin infusions in patients with signs of hypovolemia (including oliguria, AKI, prolonged capillary refill time, tachycardia, and abdominal discomfort) and adding furosemide (1–2 mg/kg given i.v.) in the middle and/or at the end of the infusion if volume has been restored and urine output is insufficient (grade C, moderate recommendation).
In cases of hypovolemic shock and/or hypotension, we suggest using 4% or 5% albumin without furosemide (grade C, weak recommendation).
In cases of AKI without hypovolemia, we recommend general management of AKI including fluid management, avoidance of nephrotoxic agents and modification of medication dosage when appropriate (grade X, strong recommendation) (Fig. 3).
Fig. 3.
Algorithm for management of children with SSNS. Details on the risk and benefit profile of the various steroid-sparing agents are given in Table 5 and Supplementary Table S6. IRNS infrequently relapsing nephrotic syndrome, FRNS frequently relapsing nephrotic syndrome, SDNS steroid-dependent nephrotic syndrome, PDN prednisone/prednisolone, CNI calcineurin inhibitors. aAs recommended in the text
Management of severe edema
In patients with severe edema, we recommend albumin infusions of 0.5–1 g/kg of 20% or 25% albumin given over a period of 4–6 h and adding furosemide (1–2 mg/kg given i.v. over 5–30 min) in the middle and/or at the end of the infusion in the absence of marked intravascular volume contraction and/or hyponatremia (grade C, moderate recommendation).
We recommend careful use of albumin infusions especially in hypertensive patients or those with decreased urine output to prevent hypervolemia and pulmonary edema (grade X, strong recommendation).
In a fluid-overloaded, edematous, hypertensive child, we suggest considering antihypertensive treatment with diuretics combined with fluid and salt restriction (grade C, weak recommendation).
Evidence and rationale
Severe edema in SSNS may be associated with either intravascular volume contraction (hypovolemia, “underfilled patient”), maintained intravascular volume or hypervolemia (“overfilled patient”) [189–192]. All measures should be tailored according to the clinical assessment of the degree of edema and volume status (Fig. 4). Clinical indicators for intravascular volume contraction are peripheral vasoconstriction (prolonged capillary refill time), tachycardia, hypotension, oliguria, AKI, or reduced cardio-thoracic index on a chest X-ray. In contrast, hypertension would suggest an overfilled patient. Moderate edema is not harmful, but an inappropriate fluid restriction and/or use of diuretics may lead to AKI, hypovolemic shock and thromboses. Measurement of the fractional urinary excretion of sodium may be helpful in discriminating underfill vs. overfilled patients [193]. Fluid restriction is indicated in case of hyponatremia < 130 meq/L (after considering false hyponatremia due to hyperlipidemia [194]). When administering albumin infusions, we recommend careful monitoring of vital signs during and after albumin infusions, which can be complicated by pulmonary edema and high blood pressure.
Fig. 4.
Algorithm for the management of edema and hypovolemia in SSNS. First, the volemic state of the child should be assessed. In case of maintained intravascular volume, we suggest treating moderate edema by low salt diet only, approximately 2 to 3 mEq per day (2000 mg/day in larger children), the amount of sodium required for a growing child, but not fluid restriction. In case of severe edema, fluid restriction is advocated in a hospital setting, with loop diuretics. Fluid restriction is also indicated in case of hyponatremia < 130 meq/L (considering false hyponatremia due to hyperlipidemia). In case of contracted intravascular volume but normal blood pressure, IV albumin infusion (20% or 25% to avoid fluid overload) should be administered over 4–6 h + / − furosemide if volemia is restored. Hypovolemic shock should be treated following specific resuscitation guidelines, starting with volume expansion by 20 mL/kg of 4% or 5% albumin over 20–30 min. aAlternatively, isotonic saline can be used if 4% or 5% albumin is not readily available. BP blood pressure
Due to the risk of thrombosis and AKI in children with hypovolemia, we recommend not to administer diuretics in uncomplicated edema. If diuretics are required in severe edema, intravascular volume depletion should be excluded first, and diuretics should be used with caution and with careful monitoring of the volume status. Similarly, we recommend against ACEi or ARBs administration to control high blood pressure in SSNS.
The reported prevalence of hypertension in childhood SSNS is variable between 7 and 34% [195–200]. It occurs in children with SDNS and FRNS [200] and also in children in remission and/or 1–10 years off medication [196], especially in case of positive family history [195, 196]. The etiology is multifactorial and includes medication side effects, in particular gluco-corticoids and CNIs, and fluid overload due to inappropriate use of albumin infusion during relapses. The choice of antihypertensive agent in the acute nephrotic state and/or supportive measures (moderate fluid restriction and low salt-diet) should therefore be carefully adapted to the fluid status of the child. In children with chronic hypertension in remission, we refer to the current hypertension guidelines [201, 202].
Prevention of thrombosis
We recommend avoiding immobilization (grade X, strong recommendation), and intravascular volume contraction (grade C, moderate recommendation) during acute nephrotic episodes.
We recommend counseling patients and families to make them aware of possible risk factors and of the symptoms of thromboembolic complications (grade X, moderate recommendation).
We do not recommend routine prophylactic anticoagulation or antiplatelet treatment for children and adolescents in the acute nephrotic stage (grade C, weak recommendation).
We suggest considering preventive anticoagulation during relapses in case of identified increased risks for thromboembolic complications (grade C, weak recommendation).
We suggest that children with known familial thrombophilic predisposition and those with laboratory indicators suggesting possible familial predisposition be evaluated by a hematologist (grade D, weak recommendation).
Evidence and rationale
Children in the acute nephrotic state are at increased risk for venous and arterial thromboembolic events that disappears when the child achieves remission. The clinical spectrum includes cerebral venous thrombosis, deep venous thrombosis, pulmonary embolism, and arterial infarction but the majority of children have deep venous thromboses rather than arterial thromboses [203, 204]. The reported incidence of symptomatic thromboembolic events, mainly diagnosed within 3 months after disease onset [204], is about 3% in all forms of NS with peaks in infancy and adolescence (summarized in [205]) and is much lower than in adults (27%). The incidence is lower in children with SSNS (1.5%) than in complicated NS/SRNS (3.8%) [206]. Associated risk factors include the disease-related hypercoagulability, hypovolemia, immobilization, infections with hospitalization, indwelling central venous lines, and underlying hereditary thrombotic predisposition [204, 207, 208].
There is insufficient evidence to recommend routine prophylactic anticoagulation during the acute nephrotic state in children and adolescents. It is essential to assess the individual clinical risk profile of each child by taking a detailed history of previous thromboembolic events and hereditary predisposition, evaluating the volume status, and avoiding iatrogenic thrombotic risk factors. If preventive anticoagulation is needed, based on the individual clinical risk profile, we suggest using low-molecular weight heparin [209]. There are insufficient data to give recommendations on the use of antiplatelet treatment with aspirin in children with NS.
Prevention and treatment of viral and bacterial infections
Antibiotics
We suggest that antibiotic prophylaxis should not be given routinely to children with SSNS (grade C, weak recommendation).
We recommend prompt antibiotic treatment in the case of a suspected bacterial infection (grade A, strong recommendation).
We recommend treating peritonitis with IV antibiotics targeting Streptococcus pneumoniae (grade A, strong recommendation).
We suggest giving cotrimoxazole prophylaxis to patients on RTX therapy during CD19+ B cell depletion, if receiving additional immunosuppressive co-medications (grade D, weak recommendation).
Evidence and rationale
Infections are a major concern in children with SSNS. These children are prone to infections not only during relapses because of urinary losses of IgG and complement opsonins (particularly encapsulated bacteria such as pneumococci), but also because of treatments (glucocorticoids or immunosuppressive agents) during remission. Thirty to 50% of infections are due to pneumococcal infection, with the rest due to gram-negative bacteria principally Escherichia coli [29, 210–214]. These infections may be severe and 60% of NS-associated deaths are due to infection [210]. However, prophylactic antibiotics are not indicated because they are not associated with a significant reduction in the occurrences of sepsis. Primary peritonitis is one of the most common major infections in hospitalized children with NS [215], with a reported incidence of 1.5–16% [211, 212, 216, 217] during relapses [218], or rarely occurring as the presenting feature of NS [219]. It may itself induce a relapse [220]. Immunosuppressive drugs and defects in humoral and non-specific immune mechanisms play a role [221, 222].
In patients with abdominal pain or discomfort and fever, diagnostic paracentesis with microbiological and biochemical analysis should be considered [211, 223, 224], especially in those with inadequate response to initial empirical antibiotic therapy. While waiting for the microbiological results of ascitic fluid, we recommend prompt treatment with IV antibiotics targeting S. pneumoniae such as cephalosporins or high doses of amoxicillin. IVIG in combination with parenteral antibiotics may be useful to treat septic episodes in children with low plasma IgG levels.
Peritonitis
There are no controlled trials on the use of penicillin prophylaxis to prevent peritonitis in children with NS [211].
Pneumocystis
Given the low incidence but high mortality of Pneumocystis jirovecii pneumonia and the drug side effects, we suggest giving cotrimoxazole prophylaxis in patients on RTX therapy during CD19+ B cell depletion if receiving additional immunosuppression [225]. Prophylactic cotrimoxazole dosing is recommended with 5–10 mg trimethoprim (TMP)/kg per day or 150 mg TMP/m2 per day in infants (at least 4 weeks of age) and children, given as single daily dose or in two divided doses every 12 h thrice weekly (on consecutive or alternate days) with a maximum TMP dose of 320 mg/day [226]. The oral dosing in adolescents is 80 to 160 mg TMP daily or 160 mg TMP 3 times per week [227]. A 50% dose reduction of cotrimoxazole is required when eGFR < 30 mL/min per 1.73 m2 and cotrimoxazole is not recommended when eGFR < 15 mL/min per 1.73 m2.
Immunoglobulin infusions
We suggest considering preventive IVIG infusions in the case of persistent low plasma total IgG levels (e.g., related to RTX infusion) and recurrent and/or severe infections (grade D, weak recommendation).
Evidence and rationale
Children with SSNS can have extremely low levels of circulating IgG owing to urinary losses during relapses. The routine use of prophylactic intravenous immunoglobulins (IVIGs) is not indicated since levels quickly return to normal ranges after remission. However, preventive IVIG infusions may be considered in the case of low plasma total IgG levels and recurrent and/or severe infections, similar to the management of secondary hypogammaglobulinemia owing to causes other than SSNS [228]. For instance, we suggest considering prophylactic IgG substitution in case of RTX-induced hypogammaglobulinemia in patients presenting with recurrent and/or severe infections. Families of children on maintenance immunosuppression and low IgG levels should be counseled about the increased risks of infections, immediate medical evaluation in case of fever and consecutive prompt start of antibiotics in case of suspected bacterial infection and additionally IVIG in case of severe and/or bacterial infection [228].
Vaccinations
We recommend reviewing the child’s vaccination status at disease onset and completing all inactivated vaccinations following the vaccination schedule that is recommended for healthy children without delay, especially for encapsulated bacteria (pneumococcus, meningococcus, haemophilus influenzae) (grade A, strong recommendation).
We recommend administering inactivated influenza vaccine annually (grade A, strong recommendation).
We recommend anti-COVID-19 vaccination in children with SSNS following the national recommendations (grade X, strong recommendation).
We recommend following national vaccination guidelines for the administration of live attenuated vaccines in immunocompromised patients (grade A, strong recommendation).
We do not recommend live vaccinations in patients on high-dose immunosuppression and in the first 6 months after RTX treatment (grade X, strong recommendation).
We recommend vaccinating the household against influenza annually, against COVID-19 and with live vaccines if live vaccines are contraindicated in the child with SSNS (grade A, strong recommendation).
Evidence and rationale
Vaccination with inactivated vaccines should follow the recommended schedule for healthy children, including vaccinating against encapsulated bacteria (especially meningococcal, H. influenza, and pneumococcal). The risk of vaccine-induced relapses has been shown to be low in numerous studies [229–232]. We recommend annual vaccination against influenza [232–234].
Live vaccines should generally be avoided in immunocompromised children [235, 236]. However, the risk of live attenuated vaccine-induced infectious diseases in children with SSNS in relapse or who are receiving immunosuppressive drugs appears to be low in the literature and in pharmacovigilance databases. This includes children receiving low-dose PDN, possibly combined with immunosuppressive treatments provided that the immunological assessment is normal [237, 238]. Depending on the context and after specialized advice from infectious diseases specialists and/or immunologists, live attenuated vaccination may be considered in children with SSNS and immunosuppressive therapy if the doses/trough levels are low and immunological tests are normal [237].
Regarding the use of anti-CD20 monoclonal antibodies such as RTX which deplete antibody-producing cells, all efforts should be made to immunize children as fully as possible before administering these therapeutic agents, at least 1 month before infusion for live vaccines. Subsequently, vaccinations can be restarted 6–9 months following RTX, non-live vaccines before this timeframe if necessary [239]. Immunization titers may be affected by the use of these agents even many years post-infusion [240], therefore it may be prudent to verify vaccination titers in children who have received these monoclonal antibodies once B cells are reconstituted and they are in stable remission.
Varicella
In case of exposure to chickenpox in children with immunosuppressive treatment who have not been immunized against VZV, we recommend prophylactic treatment with specific VZV IVIGs or oral acyclovir or valacyclovir for 5–7 days starting within 7–10 days of the exposure (grade A, strong recommendation).
We suggest treatment of VZV infection with intravenous high-dose acyclovir for 7–10 days (grade C, weak recommendation).
In the case of chickenpox, we suggest reducing doses of immunosuppressive drugs (grade D, weak recommendation).
We recommend vaccinating non-immunized patients while in remission and not on high-dose immunosuppressive medications, as well as vaccinating non-immunized siblings and parents against VZV (grade A, strong recommendation).
Evidence and rationale
Varicella in an immunocompromised patient is a serious infection [241]. The severity of varicella in a PDN-treated patient depends on at least three factors, including the initial disease for which glucocorticoids were administered, the duration and dosage of PDN therapy, and the therapeutic manipulations of the clinician in managing the situation (e.g., abrupt discontinuation, increase or decrease of steroid dose) during various stages of varicella [242–244].
In case of exposure to chickenpox, we recommend treating susceptible patients (i.e., those with hypogammaglobulinemia who are not immunized against VZV and do not have a history of chickenpox) with VZV immunoglobulins (VZIGs) as soon as possible. This strategy may be effective for reducing the severity of chickenpox symptoms when VZIGs are given up to 10 days after exposure [245, 246]. If VZIGs are not available, we recommend prophylactic treatment with oral acyclovir (10 mg/kg four times a day for 7 days) within 7–10 days of exposure to chickenpox [19, 247, 248].
We recommend treatment of VZV infection with intravenous high-dose acyclovir (1500 mg/m2 per day in three doses) or oral acyclovir or valacyclovir for 7–10 days [244]. We suggest reducing immunosuppression in case of overt varicella infection, considering the risk of HPA axis suppression in case of abrupt reduction in steroid dosage.
COVID-19
We recommend treating COVID-19 in children with SSNS as in the general pediatric population (grade X, strong recommendation).
We suggest not reducing the immunosuppressive therapy in case of mild symptoms (grade C, weak recommendation).
Evidence and rationale
Children seem to have a lower incidence and milder clinical course of coronavirus disease 2019 (COVID-19) than adults [249, 250]. Immunosuppressive treatment does not seem to be a risk factor to develop COVID-19 in children and young adults with NS on immunosuppression, and most children with NS on immunosuppressive therapy who had COVID-19 experienced a mild disease course [251–253]. There is no evidence of any association between immunosuppressive medication number and the severity of COVID-19 in children.
Preservation of bone health
We recommend avoiding prolonged steroid exposure as a risk factor for osteopenia by administering the minimum effective dose, by changing to alternate-day therapy while in remission after relapses, by limiting the duration, and by considering steroid-sparing agents in case of emerging toxicity (grade X, strong recommendation).
We recommend ensuring adequate dietary calcium intake in all children with SSNS and oral calcium supplementation in those with insufficient calcium intake (grade C, moderate recommendation).
We suggest assessing 25-OH-vitamin D levels annually in patients with SDNS or FRNS during the remission phase (after three months of remission, if possible) aiming for levels > 20 ng/mL (> 50 nmol/L) (grade C, weak recommendation).
In case of vitamin D deficiency, we recommend following national treatment guidelines (grade A, strong recommendation).
Evidence and rationale
Conflicting data have been published on the risk of glucocorticoid-induced osteoporosis (GIO) in pediatric SSNS. Some studies reported low bone mineral density (BMD), correlating with disease severity and cumulative steroid intake [254–257]. In contrast, others have reported no change in BMD after initial, intermittent or long-term alternate-day therapy [258–262]. Children and adolescents with FRNS/SDNS seem to be at a higher risk of developing low BMD [263, 264]. In summary, bone mineral loss may occur early with high-dose daily PDN (which is usually given at start of therapy) but is less significant with subsequent intermittent or low-dose alternate-day regimens. The reported incidence of fracture is low (6–8%) [263, 264]. No data are available on the use of biphosphonates in children with NS. The prevention or limitation of GIO by minimizing steroid exposure to the lowest dose and shortest effective regimen is recommended. Nutritional and lifestyle measures to maintain bone strength should also be continued.
Calcium and vitamin D supplementation
Both the vitamin D-binding protein (VDBP) and albumin bound fractions of vitamin D are lost in urine in NS relapse, and several reports have documented low levels of total serum 25(OH)D in and after NS relapse [265–267]. The total serum 25(OH)D levels were shown to return to levels similar to healthy controls after 3 months of attaining remission by Banerjee et al. [268], whereas two other studies reported persistent low 25(OH)D levels at 3 months [267, 269]. In contrast, the biologically active fraction of free 25(OH)D levels were found to be similar to levels in healthy children both in remission and relapse of NS [270].
In patients with SSNS on steroid therapy, there are conflicting results about improvement of BMD when treated with vitamin D and calcium [271–274]. Calcium and vitamin D supplementation does not specifically treat GIO and there is insufficient evidence to recommend routine supplementation of vitamin D3 and oral calcium at onset of SSNS or during relapses of usually short duration. However, ensuring adequate calcium intake and normal 25(OH)D serum levels is suggested to optimise bone health. Vitamin D supplementation should be guided by serum levels, checked after remission of at least 3 months, and by national pediatric guidelines for vitamin D deficiency [275]. Excess supplementation has been associated with hypercalciuria [274, 276]. Note that higher 25(OH)D target levels are recommended in children with CKD stages 2–5D [277].
Intermittent endocrine and metabolic changes during the acute nephrotic state
Hypothalamic–pituitary–adrenal axis suppression
We recommend prevention measures for adrenal insufficiency including shortening the duration and lowering the dose of PDN as much as possible (grade X, strong recommendation).
Evidence and rationale
Supraphysiological and prolonged glucocorticoid therapy carries the risk of suppression of the hypothalamic–pituitary–adrenal axis with transient central adrenal insufficiency after abrupt withdrawal or discontinuation of glucocorticoid therapy. This risk is especially high during periods of stress such as febrile illnesses, surgery with general anaesthesia, or major trauma. Symptoms may include that of glucocorticoid deficiency but not of mineralocorticoid axis.
There are no relevant data available on the duration, frequency, and complications of transient adrenal insufficiency in childhood NS. Clinically apparent transient adrenal insufficiency seems to be a rare event. It was reported as suspected in only one child out of 775 patients included in 4 large RCTs evaluating steroid therapy for SSNS, presenting with transient fatigue and headache with spontaneous improvement.
The time required to achieve suppression depends upon the dose and varies among patients, likely due to differences in their rates of glucocorticoid metabolism. Risk factors for glucocorticoid-induced adrenal insufficiency include (1) daily steroid therapy for more than a few weeks, (2) evening/bedtime doses for more than a few weeks, and (3) any patient who has a Cushingoid appearance (also NS diagnosed before age 5 years and steroid dependence [278]. Children receiving daily PDN therapy for fewer than 3 weeks or on alternate-day PDN therapy are less likely to present adrenal insufficiency [279].
In at-risk children, the initial screening step in the laboratory diagnosis of adrenal insufficiency is measurement of serum cortisol in the early morning. Normal values depend on the patient age and assessment technique. If basal serum cortisol is low, adrenal insufficiency is likely. If the result is indeterminate (low-normal), then an early morning ACTH serum level or stimulation test is advisable to make a definitive diagnosis.
In case of confirmed adrenal insufficiency, patients should be referred to pediatric endocrinologists for a switch to hydrocortisone, patient information/education, and adrenal insufficiency card and emergency treatments. Hydrocortisone substitution in stress doses should be considered without delay in case of acute crisis especially when presenting with infections, fever, and/or acute symptoms of central adrenal insufficiency, which are more likely to occur in the first 8–12 weeks after end of PDN treatment. In case of acute adrenal crisis, emergency treatment with high-dose hydrocortisone, fluids and glucose is required.
Prevention measures for transient adrenal insufficiency include (1) shortening the duration and lowering the dose of PDN as much as possible, (2) in the case of prolonged use of PDN associated with steroid toxicity, slow tapering of PDN, and (3) informing patients and families of the risks and symptoms of adrenal insufficiency and crisis and of the emergency procedure in case of symptoms.
Transient abnormalities
We do not recommend routine thyroid hormone substitution during SSNS relapses (grade D, weak recommendation).
We do not recommend routine lipid-lowering agents during SSNS relapses (grade D, weak recommendation).
Evidence and rationale
Intermittent thyroid dysfunction can be observed during SSNS relapses due to urinary loss of albumin and thyroxine-binding proteins. Usually, thyroid hormone status normalizes with achieving remission and thyroxine replacement is not required.
Similarly, dyslipidemia occurs in SSNS during the initial episode and relapses but this abnormality usually resolves with remission of the NS. Therefore, treatment is not required unless these anomalies persist in remission. In case of prolonged nephrotic-range proteinuria, we recommend monitoring thyroid function and fasting lipids and referring to the recommendations for SRNS [19].
Lifestyle and nutrition
We recommend supporting regular physical activity in order to prevent thromboembolic events during relapses, weight gain on prednisolone treatment, and loss of muscle and bone mass (grade A, strong recommendation).
We recommend healthy nutrition (avoiding high fat and/or high caloric food) while on steroids (grade A, strong recommendation).
We recommend a low salt diet (suggested maximum dose of 2–3 meq/kg/day, 2000 mg/day in larger children) during relapse with moderate or severe edema, and normal salt intake while in remission (grade C, weak recommendation).
We recommend a dietary protein intake as recommended for the general pediatric population (grade C, weak recommendation).
When available, we suggest advice by a dietician to patients and families requiring suitable low salt and low fat foods during relapses (grade D, weak recommendation).
Evidence and rationale
Regular physical activity can prevent thrombosis and skeletal changes. Healthy nutrition is recommended and should be guided by a specialized dietician. Eating home-prepared meals using fresh ingredients instead of canned, frozen, or packaged meals is preferable, since the latter have a much higher salt content. As increased oral protein intake has not shown to improve serum albumin levels or patient outcomes, a regular oral protein intake is recommended [280].
Sun protection
We recommend using sun protection measures, especially in all children on maintenance immunosuppression with steroid-sparing agents (grade X, moderate recommendation).
Evidence and rationale
Sun protection as a general supportive measure is important in all children, especially in those on long-term immunosuppression. Measures include reducing exposure to UV radiation, avoiding sunbathing, covering the skin with adequate clothing, and using sun protection creams with high to very high sun protection factor.
Childhood-adult transition
Rate of transition, support of transition
We recommend assessing the need for continued adulthood nephrology care in children with FRNS/SDNS at the age of 12–14 years, and at least 2–3 years before transition (grade X, moderate recommendation).
We suggest regular assessment of the readiness of a patient for transition to adult care using standardized evaluation forms and questionnaires (grade D, weak recommendation).
We suggest that the definitions and treatment advice for adolescents and young adults should be compatible with those for adults (grade D, weak recommendation).
We suggest that a patient with childhood-onset SSNS transition to adult care when his/her medical condition is controlled on or off therapy and the patient and caregivers are prepared for transition (grade D, weak recommendation).
We suggest that the decision regarding transition to primary care physician, local adult nephrology, or academic hospital care be based on the condition and history of the patient (grade D, weak recommendation).
Upon transition, we recommend a complete review of the patient’s detailed medical history and proper transfer of all relevant information (grade X, moderate recommendation).
Evidence and rationale
While children are less likely to relapse as they grow older [281], more than 10% (6.8–42.2%) of childhood-onset SSNS patients still experience relapses during adulthood [6, 7, 282–286]. Risk factors of continued active disease during adulthood are earlier onset of NS [129, 282, 285], early relapse after onset [6, 287], FRNS or SDNS [6, 7, 284–287], and duration of remission < 6 years [283, 288]. Accordingly, some adolescents are still using maintenance immunosuppressive therapy [285, 289] (Supplementary Table S10). Many also have experienced comorbidity from the treatment or the disease, such as hypertension, short stature, obesity, osteoporosis, cataract, dyslipidemia, infertility, and even psychiatric illness and thrombosis [6, 285, 287, 289–292]. These conditions need to be cared for without interruption, necessitating appropriate transition when the patient becomes an adult. Since a long time may be required for patients and their caregivers to prepare for transition to adult care, plans for transition should be started when the patient becomes an adolescent.
Transition is defined as a “process that involves planned efforts to prepare the patient from caregiver-directed care to self-disease management in the adult unit” according to the consensus statement on transition endorsed by ISN and IPNA [293]. For a successful transition, a young adult should be competent in self-disease management, which can be evaluated by questionnaires such as the Ready Steady Go and the Transition scale. Examples are provided in Supplementary Tables S13 and S14. Risk of nonadherence at the time of transfer from pediatric to adult care is high [294, 295] which can be aggravated if treatment policy of adult care is different from that of pediatric care. Because disease definitions, treatment protocols, and monitoring and follow-up differ between adults and children [296–298] (Supplementary Table S15), the patient should be educated and made aware of these differences during the period of transition to ensure adaptation and adherence to adult care.
Upon transition, a decision should be made about whether to transfer the patient to a primary care physician, local adult nephrology practice, or an academic hospital center, based on the condition and history of the patient. If the patient is prepared for transition, in remission for a long period without any immunosuppressive therapy, without additional support of other members of the multidisciplinary team (psychologist, social workers, educators), and his/her kidney function and blood pressure are normal, he/she can be referred to primary care with instructions about management, health-care checks, and when to consult hospital physicians. Otherwise, the patient should be prepared for transition to adult nephrology care. Patients who require low-complexity care can be transitioned to a nephrologist in a regional center, when the treatment plan is defined and the clinical condition of the patient is stable. When in doubt, we suggest that patients be transitioned to a nephrologist in an academic center, who can decide to share management with his/her colleague in a regional center.
Evaluation on transition
For uninterrupted care, the adult nephrologist needs to know the patient thoroughly by comprehensive history-taking and evaluation (Table 6).
Table 6.
Patient evaluation form to assist transition care
| Category | To evaluate | |
|---|---|---|
| Medical history | Disease characteristics | Age of onset, FRNS or SDNS, number of relapses, last relapse date, time of response to PDN |
| Medication history | Dosage of PDN for remission induction, current medication, cumulative dosage of PDN, CNIs, cytotoxic agents, cytostatic agents, anti-CD20s, other biologics | |
| Complications of the disease | History of AKI, thrombosis | |
| Side effects of medications | Multiple; e.g., skin, growth, infections, mental problems | |
| Kidney biopsy | Date of biopsy, review of biopsy report; discuss with pathologist if in doubt | |
| Physical examination |
Blood pressure Anthropometry Body mass index General physical exam |
Hypertension, growth failure, obesity, striae, skin problems, gum hypertrophy, hirsutism, hair loss/alopecia |
| Laboratory evaluation | Blood chemistry | Kidney function impairment |
| Blood lipid | Dyslipidemia | |
| Blood cell count | Neutropenia | |
| IgG (antiCD20mAb user) | Hypogammaglobulinemia | |
| Blood glucose, Hb A1c | Diabetes mellitus | |
| ANCA (levamisole user) | Vasculitis | |
| Radiologic evaluation | Consider DEXA in patients with low muscle mass, frail or low intensity fractures | Osteopenia/osteoporosis |
| Consultation; when indicated from medical history | Ophthalmologic evaluation | Cataract, glaucoma |
| Cardiologic evaluation | Pulmonary hypertension, venous insufficiency (thrombosis history) | |
| Social & other considerations |
Education/occupation/lifestyle Quality of Life Ongoing support by psychologists, social workers etc Knowledge of self-management |
Friends, partners, menstrual cycle Planned parenthood |
Implementation of supportive programs of transition
We suggest that supportive programs of transition be implemented for childhood-onset SSNS patients (grade D, week recommendation).
Evidence and rationale
There are few data regarding transition care focusing on patients with SSNS [299]. Considering that quite a number of patients with childhood-onset NS persistently relapse during adulthood, a formal supportive program of transition is required.
Requirements for transition care
It is advised that the patient is seen jointly by the pediatric and adult nephrologist during one or more outpatient visits. A detailed history should be transferred, which should include various aspects of the disease history as listed in Table 6. Ideally, a specialized nurse or case manager is involved in transition. This person can be the person who is primarily the key liaison for the patient.
Patient education
While children are instructed to check their urine regularly, and to increase drug dose in case of a positive test, relapse during adulthood is usually not as frequent as during childhood, and the relapse rate decreases with age. Many patients may have low-grade proteinuria, or develop short-lasting proteinuria during fever, infections, or exercise. In addition, the risk of severe morbidity caused by a relapse, such as hypovolemia or thrombo-embolic events is low in adults. Therefore, patients need to be educated to rely on their own observation of signs and symptoms such as foamy urine, edema, abdominal pain, instead of relying on dipstick tests to detect a relapse, which accompanies urinary change (foamy urine) and edema at later stage. However, dipstick evaluations are recommended in any case of clinically suspected relapse.
Management strategy
There should be a discussion on overall management, including how to monitor and manage relapse and how to modify maintenance immunosuppression. Although many patients will experience a relapse, tapering of immunosuppressive therapy should be tried at least every 2 years, although it remains a matter of trial and error. In addition, it is important to discuss the strategy to prevent relapses during infections or stress. Likewise, information on prevention of glucocorticoid deficiency should be available and clear.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors acknowledge the valuable contributions of the members of the voting panel representing the IPNA regional societies, i.e., ESPN: Antonia Bouts (Amsterdam, Netherlands), Claire Dossier (Paris, France), Francesco Emma (Rome, Italy), Markus Kemper (Hamburg, Germany), Rezan Topaloglu (Ankara, Turkey), Aoife Waters (London, United Kingdom), Lutz Thorsten Weber (Cologne, Germany), Alexandra Zurowska (Gdansk, Poland); ASPN: Keisha L. Gibson (Chapel Hill, United States), Larry Greenbaum (Atlanta, United States), Susan Massengill (Charlotte, United States), David Selewski (Charleston, United States), Tarak Srivastava (Kansas City, United States), Chia-shi Wang (Atlanta, United States), Scott Wenderfer (Vancouver, Canada); ANZPNA: Lilian Johnstone (Clayton, Australia), Nicholas Larkins (Perth, Australia), William Wong (Auckland, New Zealand); AsPNA: Agnes A. Alba (Quezon City, Philippines), TS Ha (Cheongju, Korea), Masoumeh Mokham (Tehran, Iran), Xuhui Zhong (Bejing, China); JSPN: Riku Hamada (Tokyo, Japan), Kazumoto Iijima (Kobe, Japan), Kenji Ishikura, (Sagamihara, Japan), Kandai Nozu (Kobe, Japan); ALANEPE: Nilzete Bresolin (Florianópolis, Brazil), Nilka De Jesus Gonzalez (San Juan, Puerto Rico), Jaime Restrepo (Cali, Colombia); AFPNA: Ifeoma Anochie (Port Harcourt, Nigeria), Mignon McCulloch (Cape Town, South Africa).
The authors would also like to thank the following acting as external experts; pediatric endocrinologists: Agnes Linglart (Paris, France), Dirk Schnabel (Berlin, Germany); general pediatricians: Adamu Sambo (Gloucestershire, United Kingdom); experts in transition: Marjo van Helden (Nijmegen, Netherlands), Ben Sprangers (Leuven, Belgium); dieticians: Stefanie Steinmann (Hannover, Germany), Sheridan Collins (Sydney, Australia), Katie Byrne (Ann Arbor, United States); and patient representatives: Clemens and Juliane Brauner (Hannover, Germany), Chandana Guha (Sydney, Australia), Stephane Serre (Toulouse, France).
Funding
Open Access funding enabled and organized by Projekt DEAL. Open Access funding provided by Project DEAL. The International Pediatric Nephrology Association launched, organized, and funded this initiative. The funder had no influence on the content of the guideline.
Declarations
Competing interests
D.H. has received research grants from Kyowa Kirin and Amgen and has received speaker and/or consultant fees from Amgen, Sandoz, Kyowa Kirin, Pfizer, Merck Serono, Horizon, and Chiesi. O.B. has received speaker and/or consultant fees from Amgen, Chiesi, Novartis, and Octapharma. These were all unrelated to the topic of this guideline. M.V. has received research grants from Alexion and speaker and/or consultant fees from Alexion, Apellis, Chemocentrix, Novartis, Roche and Travere. These did not influence the content of this guideline. H.K. has been participating in clinical trials by Alexion, Amgen, Astellas, Bayer, Chong Kun Dang, Handok, and Kyowa Kirin, and has received speaker and/or consultant fees from Alexion, Bayer, Chong Kun Dang, Handok, and Kyowa Kirin. M.C. has received consultancy fees from Novartis and educational grants from Recordati. The other authors declare no competing interests.
Footnotes
Agnes Trautmann and Olivia Boyer contributed equally and should therefore serve as co-first authors, Dieter Haffner and Marina Vivarelli contributed equally as well and should serve as co-last authors.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dieter Haffner, Email: Haffner.Dieter@mh-hannover.de.
on behalf of the International Pediatric Nephrology Association:
Antonia Bouts, Claire Dossier, Francesco Emma, Markus Kemper, Rezan Topaloglu, Aoife Waters, Lutz Thorsten Weber, Alexandra Zurowska, Keisha L. Gibson, Larry Greenbaum, Susan Massengill, David Selewski, Tarak Srivastava, Chia-shi Wang, Scott Wenderfer, Lilian Johnstone, Nicholas Larkins, William Wong, Agnes A. Alba, T. S. Ha, Masoumeh Mokham, Xuhui Zhong, Riku Hamada, Kazumoto Iijima, Kenji Ishikura, Kandai Nozu, Nilzete Bresolin, Nilka De Jesus Gonzalez, Jaime Restrepo, Ifeoma Anochie, and Mignon McCulloch
References
- 1.Noone DG, Iijima K, Parekh R. Idiopathic nephrotic syndrome in children. Lancet. 2018;392:61–74. doi: 10.1016/S0140-6736(18)30536-1. [DOI] [PubMed] [Google Scholar]
- 2.Tullus K, Webb H, Bagga A. Management of steroid-resistant nephrotic syndrome in children and adolescents. Lancet Child Adolesc Health. 2018;2:880–890. doi: 10.1016/S2352-4642(18)30283-9. [DOI] [PubMed] [Google Scholar]
- 3.Tarshish P, Tobin JN, Bernstein J, Edelmann CM., Jr Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol. 1997;8:769–776. doi: 10.1681/ASN.V85769. [DOI] [PubMed] [Google Scholar]
- 4.Carter SA, Mistry S, Fitzpatrick J, Banh T, Hebert D, Langlois V, Pearl RJ, Chanchlani R, Licht CPB, Radhakrishnan S, Brooke J, Reddon M, Levin L, Aitken-Menezes K, Noone D, Parekh RS. Prediction of short- and long-term outcomes in childhood nephrotic syndrome. Kidney Int Rep. 2020;5:426–434. doi: 10.1016/j.ekir.2019.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arbeitsgemeinschaft für Pädiatrische Nephrologie (APN) Effect of cytotoxic drugs in frequently relapsing nephrotic syndrome with and without steroid dependence. N Engl J Med. 1982;306:451–454. doi: 10.1056/NEJM198202253060803. [DOI] [PubMed] [Google Scholar]
- 6.Rüth EM, Kemper MJ, Leumann EP, Laube GF, Neuhaus TJ. Children with steroid-sensitive nephrotic syndrome come of age: long-term outcome. J Pediatr. 2005;147:202–207. doi: 10.1016/j.jpeds.2005.03.050. [DOI] [PubMed] [Google Scholar]
- 7.Korsgaard T, Andersen RF, Joshi S, Hagstrøm S, Rittig S. Childhood onset steroid-sensitive nephrotic syndrome continues into adulthood. Pediatr Nephrol. 2019;34:641–648. doi: 10.1007/s00467-018-4119-8. [DOI] [PubMed] [Google Scholar]
- 8.Marchel DM, Gipson DS. Adult survivors of idiopathic childhood onset nephrotic syndrome. Pediatr Nephrol. 2021;36:1731–1737. doi: 10.1007/s00467-020-04773-3. [DOI] [PubMed] [Google Scholar]
- 9.Vivarelli M, Massella L, Ruggiero B, Emma F. Minimal Change Disease. Clin J Am Soc Nephrol. 2017;12:332–345. doi: 10.2215/CJN.05000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hahn D SS, Willis NS, Craig JC, Hodson EM (2020) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev 2020(8):CD001533 [DOI] [PubMed]
- 11.Gellermann J, Querfeld U. Frequently relapsing nephrotic syndrome: treatment with mycophenolate mofetil. Pediatr Nephrol. 2004;19:101–104. doi: 10.1007/s00467-003-1300-4. [DOI] [PubMed] [Google Scholar]
- 12.Larkins NG, Liu ID, Willis NS, Craig JC, Hodson EM (2020) Non-corticosteroid immunosuppressive medications for steroid-sensitive nephrotic syndrome in children. Cochrane Database Syst Rev 4:CD002290 [DOI] [PMC free article] [PubMed]
- 13.Latta K, von Schnakenburg C, Ehrich JH. A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children. Pediatr Nephrol. 2001;16:271–282. doi: 10.1007/s004670000523. [DOI] [PubMed] [Google Scholar]
- 14.Basu B, Babu BG, Mahapatra TK. Long-term efficacy and safety of common steroid-sparing agents in idiopathic nephrotic children. Clin Exp Nephrol. 2017;21:143–151. doi: 10.1007/s10157-016-1266-8. [DOI] [PubMed] [Google Scholar]
- 15.Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, Chan TM, Cook HT, Fervenza FC, Gibson KL, Glassock RJ, Jayne DRW, Jha V, Liew A, Liu ZH, Mejía-Vilet JM, Nester CM, Radhakrishnan J, Rave EM, Reich HN, Ronco P, Sanders JF, Sethi S, Suzuki Y, Tang SCW, Tesar V, Vivarelli M, Wetzels JFM, Lytvyn L, Craig JC, Tunnicliffe DJ, Howell M, Tonelli MA, Cheung M, Earley A, Floege J. Executive summary of the KDIGO 2021 guideline for the management of glomerular diseases. Kidney Int. 2021;100:753–779. doi: 10.1016/j.kint.2021.05.015. [DOI] [PubMed] [Google Scholar]
- 16.Chen Y, Yang K, Marusic A, Qaseem A, Meerpohl JJ, Flottorp S, Akl EA, Schunemann HJ, Chan ES, Falck-Ytter Y, Ahmed F, Barber S, Chen C, Zhang M, Xu B, Tian J, Song F, Shang H, Tang K, Wang Q, Norris SL. A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med. 2017;166:128–132. doi: 10.7326/M16-1565. [DOI] [PubMed] [Google Scholar]
- 17.Guyatt GH, Oxman AD, Kunz R, Atkins D, Brozek J, Vist G, Alderson P, Glasziou P, Falck-Ytter Y, Schunemann HJ. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol. 2011;64:395–400. doi: 10.1016/j.jclinepi.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Pediatrics (AAP) Classifying recommendations for clinical practice guidelines. Pediatrics. 2004;114:874–877. doi: 10.1542/peds.2004-1260. [DOI] [PubMed] [Google Scholar]
- 19.Trautmann A, Vivarelli M, Samuel S, Gipson D, Sinha A, Schaefer F, Hui NK, Boyer O, Saleem MA, Feltran L, Müller-Deile J, Becker JU, Cano F, Xu H, Lim YN, Smoyer W, Anochie I, Nakanishi K, Hodson E, Haffner D. IPNA clinical practice recommendations for the diagnosis and management of children with steroid-resistant nephrotic syndrome. Pediatr Nephrol. 2020;35:1529–1561. doi: 10.1007/s00467-020-04519-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group Clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;100:S1–S276. doi: 10.1016/j.kint.2021.05.021. [DOI] [PubMed] [Google Scholar]
- 21.Clase CM, St Pierre MW, Churchill DN. Conversion between bromcresol green- and bromcresol purple-measured albumin in renal disease. Nephrol Dial Transplant. 2001;16:1925–1929. doi: 10.1093/ndt/16.9.1925. [DOI] [PubMed] [Google Scholar]
- 22.van de Logt AE, Rijpma SR, Vink CH, Prudon-Rosmulder E, Wetzels JF, van Berkel M. The bias between different albumin assays may affect clinical decision-making. Kidney Int. 2019;95:1514–2151. doi: 10.1016/j.kint.2019.01.042. [DOI] [PubMed] [Google Scholar]
- 23.Drube J, Wan M, Bonthuis M, Wuhl E, Bacchetta J, Santos F, Grenda R, Edefonti A, Harambat J, Shroff R, Tonshoff B, Haffner D. Clinical practice recommendations for growth hormone treatment in children with chronic kidney disease. Nat Rev Nephrol. 2019;15:577–589. doi: 10.1038/s41581-019-0161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284–294. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 25.Hogg RJ, Portman RJ, Milliner D, Lemley KV, Eddy A, Ingelfinger J. Evaluation and management of proteinuria and nephrotic syndrome in children: recommendations from a pediatric nephrology panel established at the National Kidney Foundation conference on proteinuria, albuminuria, risk, assessment, detection, and elimination (PARADE) Pediatrics. 2000;105:1242–1249. doi: 10.1542/peds.105.6.1242. [DOI] [PubMed] [Google Scholar]
- 26.Slev PR, Bunker AM, Owen WE, Roberts WL. Pediatric reference intervals for random urine calcium, phosphorus and total protein. Pediatr Nephrol. 2010;25:1707–1710. doi: 10.1007/s00467-010-1544-8. [DOI] [PubMed] [Google Scholar]
- 27.Boyer O, Schaefer F, Haffner D, Bockenhauer D, Hölttä T, Bérody S, Webb H, Heselden M, Lipska-Zie˛tkiewicz BS, Ozaltin F, Levtchenko E, Vivarelli M (2021) Management of congenital nephrotic syndrome: consensus recommendations of the ERKNet-ESPN Working Group. Nat Rev Nephrol 17:277-289 [DOI] [PMC free article] [PubMed]
- 28.Lipska-Ziętkiewicz BS, Ozaltin F, Hölttä T, Bockenhauer D, Bérody S, Levtchenko E, Vivarelli M, Webb H, Haffner D, Schaefer F, Boyer O. Genetic aspects of congenital nephrotic syndrome: a consensus statement from the ERKNet–ESPN inherited glomerulopathy working group. Eur J Human Genet. 2020;28:1368–1378. doi: 10.1038/s41431-020-0642-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eddy AA, Symons JM. Nephrotic syndrome in childhood. Lancet. 2003;362:629–639. doi: 10.1016/S0140-6736(03)14184-0. [DOI] [PubMed] [Google Scholar]
- 30.Hama T, Nakanishi K, Shima Y, Sato M, Mukaiyama H, Togawa H, Hamahira K, Tanaka R, Kaito H, Nozu K, Iijima K, Yoshikawa N. Renal biopsy criterion in idiopathic nephrotic syndrome with microscopic hematuria at onset. Pediatr Nephrol. 2015;30:445–450. doi: 10.1007/s00467-014-2946-9. [DOI] [PubMed] [Google Scholar]
- 31.Hinkes BG, Mucha B, Vlangos CN, Gbadegesin R, Liu J, Hasselbacher K, Hangan D, Ozaltin F, Zenker M, Hildebrandt F. Nephrotic syndrome in the first year of life: two 3rds of cases are caused by mutations in 4 genes (NPHS1, NPHS2, WT1, and LAMB2) Pediatrics. 2007;119:E907–E919. doi: 10.1542/peds.2006-2164. [DOI] [PubMed] [Google Scholar]
- 32.Sadowski CE, Lovric S, Ashraf S, Pabst WL, Gee HY, Kohl S, Engelmann S, Vega-Warner V, Fang H, Halbritter J, Somers MJ, Tan W, Shril S, Fessi I, Lifton RP, Bockenhauer D, El-Desoky S, Kari JA, Zenker M, Kemper MJ, Mueller D, Fathy HM, Soliman NA, Hildebrandt F. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. J Am Soc Nephrol. 2015;26:1279–1289. doi: 10.1681/ASN.2014050489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Niaudet P, Gubler MC. WT1 and glomerular diseases. Pediatr Nephrol. 2006;21:1653–2166. doi: 10.1007/s00467-006-0208-1. [DOI] [PubMed] [Google Scholar]
- 34.Gbadegesin R, Hinkes BG, Hoskins BE, Vlangos CN, Heeringa SF, Liu J, Loirat C, Ozaltin F, Hashmi S, Ulmer F, Cleper R, Ettenger R, Antignac C, Wiggins RC, Zenker M, Hildebrandt F. Mutations in PLCE1 are a major cause of isolated diffuse mesangial sclerosis (IDMS) Nephrol Dial Transplant. 2007;23:1291–1297. doi: 10.1093/ndt/gfm759. [DOI] [PubMed] [Google Scholar]
- 35.Iványi B, Rácz GZ, Gál P, Brinyiczki K, Bódi I, Kalmár T, Maróti Z, Bereczki C. Diffuse mesangial sclerosis in a PDSS2 mutation-induced coenzyme Q10 deficiency. Pediatr Nephrol. 2018;33:439–446. doi: 10.1007/s00467-017-3814-1. [DOI] [PubMed] [Google Scholar]
- 36.Ranganathan S. Pathology of podocytopathies causing nephrotic syndrome in children. Front Pediatr. 2016;4:32. doi: 10.3389/fped.2016.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Glenn D, Ocegueda S, Nazareth M, Zhong Y, Weinstein A, Primack W, Cochat P, Ferris M. The global pediatric nephrology workforce: a survey of the International Pediatric Nephrology Association. BMC Nephrol. 2016;17:83. doi: 10.1186/s12882-016-0299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hodson EM, Willis NS, Craig JC (2007) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev 4:CD001533 [DOI] [PubMed]
- 39.Sinha A, Saha A, Kumar M, Sharma S, Afzal K, Mehta A, Kalaivani M, Hari P, Bagga A. Extending initial prednisolone treatment in a randomized control trial from 3 to 6 months did not significantly influence the course of illness in children with steroid-sensitive nephrotic syndrome. Kidney Int. 2015;87:217–224. doi: 10.1038/ki.2014.240. [DOI] [PubMed] [Google Scholar]
- 40.Teeninga N, Kist-van Holthe JE, van Rijswijk N, de Mos NI, Hop WC, Wetzels JF, van der Heijden AJ, Nauta J. Extending prednisolone treatment does not reduce relapses in childhood nephrotic syndrome. J Am Soc Nephrol. 2013;24:149–159. doi: 10.1681/ASN.2012070646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoshikawa N, Nakanishi K, Sako M, Oba MS, Mori R, Ota E, Ishikura K, Hataya H, Honda M, Ito S, Shima Y, Kaito H, Nozu K, Nakamura H, Igarashi T, Ohashi Y, Iijima K. A multicenter randomized trial indicates initial prednisolone treatment for childhood nephrotic syndrome for two months is not inferior to six-month treatment. Kidney Int. 2015;87:225–232. doi: 10.1038/ki.2014.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Webb NJA, Woolley RL, Lambe T, Frew E, Brettell EA, Barsoum EN, Trompeter RS, Cummins C, Deeks JJ, Wheatley K, Ives NJ. Long term tapering versus standard prednisolone treatment for first episode of childhood nephrotic syndrome: phase III randomised controlled trial and economic evaluation. BMJ. 2019;365:l1800. doi: 10.1136/bmj.l1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ekka BK, Bagga A, Srivastava RN. Single- versus divided-dose prednisolone therapy for relapses of nephrotic syndrome. Pediatr Nephrol. 1997;11:597–599. doi: 10.1007/s004670050344. [DOI] [PubMed] [Google Scholar]
- 44.Li X, Li Z, Cheng Z. Treatment of children with simple nephrotic syndrome using prednisone once per day. Acta Acad Med Hubei. 1994;15:386–388. [Google Scholar]
- 45.Warshaw BL, Hymes LC. Daily single-dose and daily reduced-dose prednisone therapy for children with the nephrotic syndrome. Pediatrics. 1989;83:694–699. doi: 10.1542/peds.83.5.694. [DOI] [PubMed] [Google Scholar]
- 46.Hren R, Benz MR, Brinkkötter PT, Dötsch J, Eberl WR, Gellermann J, Hoyer PF, Jordans I, Kamrath C, Kemper MJ, Latta K, Müller D, Oh J, Tönshoff B, Weber S, Weber LT; German Society for Pediatric Nephrology (2021) Pediatric idiopathic steroid-sensitive nephrotic syndrome: diagnosis and therapy -short version of the updated German best practice guideline (S2e) - AWMF register no. 166-001, 6/2020. Pediatr Nephrol 36:2971-2985 [DOI] [PMC free article] [PubMed]
- 47.Pasini A, Benetti E, Conti G, Ghio L, Lepore M, Massella L, Molino D, Peruzzi L, Emma F, Fede C, Trivelli A, Maringhini S, Materassi M, Messina G, Montini G, Murer L, Pecoraro C, Pennesi M. The Italian Society for Pediatric Nephrology (SINePe) consensus document on the management of nephrotic syndrome in children: Part I - Diagnosis and treatment of the first episode and the first relapse. Ital J Pediatr. 2017;43:41. doi: 10.1186/s13052-017-0356-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gipson DS, Massengill SF, Yao L, Nagaraj S, Smoyer WE, Mahan JD, Wigfall D, Miles P, Powell L, Lin JJ, Trachtman H, Greenbaum LA. Management of childhood onset nephrotic syndrome. Pediatrics. 2009;124:747–757. doi: 10.1542/peds.2008-1559. [DOI] [PubMed] [Google Scholar]
- 49.Deschenes G, Vivarelli M, Peruzzi L. Variability of diagnostic criteria and treatment of idiopathic nephrotic syndrome across European countries. Eur J Pediatr. 2017;176:647–654. doi: 10.1007/s00431-017-2891-2. [DOI] [PubMed] [Google Scholar]
- 50.Borovitz Y, Alfandary H, Haskin O, Levi S, Kaz S, Davidovits M, Dagan A. Lower prednisone dosing for steroid-sensitive nephrotic syndrome relapse: a prospective randomized pilot study. Eur J Pediatr. 2020;179:279–283. doi: 10.1007/s00431-019-03506-5. [DOI] [PubMed] [Google Scholar]
- 51.Hiraoka M, Tsukahara H, Haruki S, Hayashi S, Takeda N, Miyagawa K, Okuhara K, Suehiro F, Ohshima Y, Mayumi M. Older boys benefit from higher initial prednisolone therapy for nephrotic syndrome. The West Japan Cooperative Study of Kidney Disease in Children. Kidney Int. 2000;58:1247–1252. doi: 10.1046/j.1523-1755.2000.00279.x. [DOI] [PubMed] [Google Scholar]
- 52.Sibley M, Roshan A, Alshami A, Catapang M, Jöbsis JJ, Kwok T, Polderman N, Sibley J, Matsell DG, Mammen C. Induction prednisone dosing for childhood nephrotic syndrome: how low should we go? Pediatr Nephrol. 2018;33:1539–1545. doi: 10.1007/s00467-018-3975-6. [DOI] [PubMed] [Google Scholar]
- 53.Feber J, Al-Matrafi J, Farhadi E, Vaillancourt R, Wolfish N. Prednisone dosing per body weight or body surface area in children with nephrotic syndrome: is it equivalent? Pediatr Nephrol. 2009;24:1027–1031. doi: 10.1007/s00467-008-1089-2. [DOI] [PubMed] [Google Scholar]
- 54.Basu B, Bhattacharyya S, Barua S, Naskar A, Roy B. Efficacy of body weight vs body surface area-based prednisolone regimen in nephrotic syndrome. Clin Exp Nephrol. 2020;24:622–629. doi: 10.1007/s10157-020-01875-y. [DOI] [PubMed] [Google Scholar]
- 55.Raman V, Krishnamurthy S, Harichandrakumar KT. Body weight-based prednisolone versus body surface area-based prednisolone regimen for induction of remission in children with nephrotic syndrome: a randomized, open-label, equivalence clinical trial. Pediatr Nephrol. 2016;31:595–604. doi: 10.1007/s00467-015-3285-1. [DOI] [PubMed] [Google Scholar]
- 56.Emma F, Montini G, Gargiulo A. Equations to estimate prednisone dose using body weight. Pediatr Nephrol. 2019;34:685–688. doi: 10.1007/s00467-018-4127-8. [DOI] [PubMed] [Google Scholar]
- 57.Zhang B, Liu T, Wang W, Zhang X, Fan S, Liu Z, Liu Z, Wu X. A prospective randomly controlled clinical trial on azithromycin therapy for induction treatment of children with nephrotic syndrome. Eur J Pediatr. 2014;173:509–515. doi: 10.1007/s00431-013-2192-3. [DOI] [PubMed] [Google Scholar]
- 58.Hoyer PF, Brodeh J. Initial treatment of idiopathic nephrotic syndrome in children: prednisone versus prednisone plus cyclosporine A: a prospective, randomized trial. J Am Soc Nephrol. 2006;17:1151–1157. doi: 10.1681/ASN.2005090922. [DOI] [PubMed] [Google Scholar]
- 59.Ehren R, Benz MR, Doetsch J, Fichtner A, Gellermann J, Haffner D, Höcker B, Hoyer PF, Kästner B, Kemper MJ, Konrad M, Luntz S, Querfeld U, Sander A, Toenshoff B, Weber LT. Initial treatment of steroid-sensitive idiopathic nephrotic syndrome in children with mycophenolate mofetil versus prednisone: protocol for a randomised, controlled, multicentre trial (INTENT study) BMJ Open. 2018;8:e024882. doi: 10.1136/bmjopen-2018-024882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Veltkamp F, Khan DH, Reefman C, Veissi S, van Oers HA, Levtchenko E, Mathôt RAA, Florquin S, van Wijk JAE, Schreuder MF, Haverman L, Bouts AHM. Prevention of relapses with levamisole as adjuvant therapy in children with a first episode of idiopathic nephrotic syndrome: study protocol for a double blind, randomised placebo-controlled trial (the LEARNS study) BMJ Open. 2019;9:e027011. doi: 10.1136/bmjopen-2018-027011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Czock D, Keller F, Rasche FM, Häussler U. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet. 2005;44:61–98. doi: 10.2165/00003088-200544010-00003. [DOI] [PubMed] [Google Scholar]
- 62.Schijvens AM, Ter Heine R, de Wildt SN, Schreuder MF. Pharmacology and pharmacogenetics of prednisone and prednisolone in patients with nephrotic syndrome. Pediatr Nephrol. 2019;34:389–403. doi: 10.1007/s00467-018-3929-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jenkins JS, Sampson PA. Conversion of cortisone to cortisol and prednisone to prednisolone. Br Med J. 1967;2:205–207. doi: 10.1136/bmj.2.5546.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rostin M, Barthe P, Houin G, Alvinerie M, Bouissou F. Pharmacokinetics of prednisolone in children with the nephrotic syndrome. Pediatr Nephrol. 1990;4:470–473. doi: 10.1007/BF00869822. [DOI] [PubMed] [Google Scholar]
- 65.Gatti G, Perucca E, Frigo GM, Notarangelo LD, Barberis L, Martini A. Pharmacokinetics of prednisone and its metabolite prednisolone in children with nephrotic syndrome during the active phase and in remission. Br J Clin Pharmacol. 1984;17:423–431. doi: 10.1111/j.1365-2125.1984.tb02367.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rocci ML, Jr, Assael BM, Appiani AC, Edefonti A, Jusko WJ. Effect on nephrotic syndrome on absorption and disposition of prednisolone in children. Int J Pediatr Nephrol. 1982;3:159–166. [PubMed] [Google Scholar]
- 67.Mitchell JC, Counselman FL. A taste comparison of three different liquid steroid preparations: prednisone, prednisolone, and dexamethasone. Acad Emerg Med. 2003;10:400–403. doi: 10.1197/aemj.10.4.400. [DOI] [PubMed] [Google Scholar]
- 68.Regan TD, Lewis D, Norton SA. Taste comparison of corticosteroid suspensions. J Drugs Dermatol. 2006;5:835–837. [PubMed] [Google Scholar]
- 69.Singhal R, Pandit S, Dhawan N. Deflazacort versus Prednisolone: randomized controlled trial in treatment of children with idiopathic nephrotic syndrome. Iran J Pediatr. 2015;25:e510. doi: 10.5812/ijp.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Agarwal IGJ, Moses PD, Mathew L, Prashanth P. Open randomized clinical study to evaluate efficacy and safety of deflazacort versus prednisolone in idiopathic nephrotic syndrome (abstract no: 558) Pediatr Nephrol. 2010;25:1906. [Google Scholar]
- 71.Broyer M, Terzi F, Lehnert A, Gagnadoux MF, Guest G, Niaudet P. A controlled study of deflazacort in the treatment of idiopathic nephrotic syndrome. Pediatr Nephrol. 1997;11:418–422. doi: 10.1007/s004670050308. [DOI] [PubMed] [Google Scholar]
- 72.Lee EC, Kim GA, Koo JW. Toxic epidermal necrolysis associated with deflazacort therapy with nephrotic syndrome. Kidney Res Clin Pract. 2014;33:222–225. doi: 10.1016/j.krcp.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saxena I, Kapoor S, Gupta RC. Detection of proteinuria in pregnancy: comparison of qualitative tests for proteins and dipsticks with urinary protein creatinine index. J Clin Diagn Res. 2013;7:1846–1848. doi: 10.7860/JCDR/2013/6656.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Robert CF, Mauris A, Bouvier P, Rougemont A. Proteinuria screening using sulfosalicylic acid: advantages of the method for the monitoring of prenatal consultations in West Africa. Soz Praventivmed. 1995;40:44–49. doi: 10.1007/BF01615661. [DOI] [PubMed] [Google Scholar]
- 75.Dissanayake VH, Morgan L, Broughton Pipkin F, Vathanan V, Premaratne S, Jayasekara RW, Seneviratne HR. The urine protein heat coagulation test—a useful screening test for proteinuria in pregnancy in developing countries: a method validation study. BJOG. 2004;111:491–494. doi: 10.1111/j.1471-0528.2004.00128.x. [DOI] [PubMed] [Google Scholar]
- 76.Penagos JAVTJ, Jaramillo JDL, Marulenda NLG, Gallego JG. Use of sulfosalicylic acid in the detection of proteinuria and its application to hypertensive problems in pregnancy. IATREIA. 2011;24:259–266. [Google Scholar]
- 77.Kengne-Wafo S, Massella L, Diomedi-Camassei F, Gianviti A, Vivarelli M, Greco M, Stringini GR, Emma F. Risk factors for cyclosporin A nephrotoxicity in children with steroid-dependent nephrotic syndrome. Clin J Am Soc Nephrol. 2009;4:1409–1416. doi: 10.2215/CJN.01520209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Arbeitsgemeinschaft für Pädiatrische Nephrology (APN) Alternate-day versus intermittent prednisone in frequently relapsing nephrotic syndrome. A report of "Arbeitsgemeinschaft für Pädiatrische Nephrologie". Lancet. 1979;1:401–403. [PubMed] [Google Scholar]
- 79.Kainth D, Hari P, Sinha A, Pandey S, Bagga A. Short-duration Prednisolone in children with nephrotic syndrome relapse: a noninferiority randomized controlled trial. Clin J Am Soc Nephrol. 2021;16:225–232. doi: 10.2215/CJN.06140420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gargiulo A, Massella L, Ruggiero B, Ravà L, Ciofi Degli Atti M, Materassi M, Lugani F, Benetti E, Morello W, Molino D, Mattozzi F, Pennesi M, Maringhini S, Pasini A, Gianoglio B, Pecoraro C, Montini G, Murer L, Ghiggeri GM, Romagnani P, Vivarelli M, Emma F. Results of the PROPINE randomized controlled study suggest tapering of prednisone treatment for relapses of steroid sensitive nephrotic syndrome is not necessary in children. Kidney Int. 2021;99:475–483. doi: 10.1016/j.kint.2020.09.024. [DOI] [PubMed] [Google Scholar]
- 81.Schijvens AM, Dorresteijn EM, Roeleveld N, Ter Heine R, van Wijk JAE, Bouts AHM, Keijzer-Veen MG, van de Kar N, van den Heuvel L, Schreuder MF. REducing STEroids in Relapsing Nephrotic syndrome: the RESTERN study—protocol of a national, double-blind, randomised, placebo-controlled, non-inferiority intervention study. BMJ Open. 2017;7:e018148. doi: 10.1136/bmjopen-2017-018148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Christian MT, Webb NJA, Mehta S, Woolley RL, Afentou N, Frew E, Brettell EA, Khan AR, Milford DV, Bockenhauer D, Saleem MA, Hall AS, Koziell A, Maxwell H, Hegde S, Prajapati H, Gilbert RD, Jones C, McKeever K, Cook W, Ives N. Evaluation of daily low-dose prednisolone during upper respiratory tract infection to prevent relapse in children with relapsing steroid-sensitive nephrotic syndrome: the PREDNOS 2 randomized clinical trial. JAMA Pediatr. 2021;3:236–243. doi: 10.1001/jamapediatrics.2021.5189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Abeyagunawardena AS, Trompeter RS. Increasing the dose of prednisolone during viral infections reduces the risk of relapse in nephrotic syndrome: a randomised controlled trial. Arch Dis Child. 2008;93:226–228. doi: 10.1136/adc.2007.116079. [DOI] [PubMed] [Google Scholar]
- 84.Gulati A, Sinha A, Sreenivas V, Math A, Hari P, Bagga A. Daily corticosteroids reduce infection-associated relapses in frequently relapsing nephrotic syndrome: a randomized controlled trial. Clin J Am Soc Nephrol. 2011;6:63–69. doi: 10.2215/CJN.01850310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mattoo TK, Mahmoud MA. Increased maintenance corticosteroids during upper respiratory infection decrease the risk of relapse in nephrotic syndrome. Nephron. 2000;85:343–345. doi: 10.1159/000045684. [DOI] [PubMed] [Google Scholar]
- 86.Abeyagunawardena AS, Thalgahagoda RS, Dissanayake PV, Abeyagunawardena S, Illangasekera YA, Karunadasa UI, Trompeter RS. Short courses of daily prednisolone during upper respiratory tract infections reduce relapse frequency in childhood nephrotic syndrome. Pediatr Nephrol. 2017;32:1377–1382. doi: 10.1007/s00467-017-3640-5. [DOI] [PubMed] [Google Scholar]
- 87.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–412. doi: 10.1001/jama.1995.03520290060030. [DOI] [PubMed] [Google Scholar]
- 88.Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, Tugwell P, Klassen TP. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet. 1998;352:609–613. doi: 10.1016/S0140-6736(98)01085-X. [DOI] [PubMed] [Google Scholar]
- 89.Moorani KN, Khan KM, Ramzan A. Infections in children with nephrotic syndrome. J Coll Physicians Surg Pak. 2003;13:337–339. [PubMed] [Google Scholar]
- 90.Christian MT, Webb NJA, Woolley RL, Afentou N, Mehta S, Frew E, Brettell EA, Khan AR, Milford DV, Bockenhauer D, Saleem MA, Hall AS, Koziell A, Maxwell H, Hegde S, Finlay ER, Gilbert RD, Jones C, McKeever K, Cook W, Ives N. Daily low-dose prednisolone to prevent relapse of steroid-sensitive nephrotic syndrome in children with an upper respiratory tract infection: PREDNOS2 RCT. Health Technol Assess. 2022;26:1–94. doi: 10.3310/WTFC5658. [DOI] [PubMed] [Google Scholar]
- 91.Elzouki AY, Jaiswal OP. Long-term, small dose prednisone therapy in frequently relapsing nephrotic syndrome of childhood. Effect on remission, statural growth, obesity, and infection rate. Clin Pediatr. 1988;27:387–392. doi: 10.1177/000992288802700807. [DOI] [PubMed] [Google Scholar]
- 92.Srivastava RN, Vasudev AS, Bagga A, Sunderam KR. Long-term, low-dose prednisolone therapy in frequently relapsing nephrotic syndrome. Pediatr Nephrol. 1992;6:247–250. doi: 10.1007/BF00878359. [DOI] [PubMed] [Google Scholar]
- 93.Yadav M, Sinha A, Khandelwal P, Hari P, Bagga A. Efficacy of low-dose daily versus alternate-day prednisolone in frequently relapsing nephrotic syndrome: an open-label randomized controlled trial. Pediatr Nephrol. 2019;34:829–835. doi: 10.1007/s00467-018-4071-7. [DOI] [PubMed] [Google Scholar]
- 94.Iijima K, Sako M, Oba MS, Ito S, Hataya H, Tanaka R, Ohwada Y, Kamei K, Ishikura K, Yata N, Nozu K, Honda M, Nakamura H, Nagata M, Ohashi Y, Nakanishi K, Yoshikawa N. Cyclosporine C2 monitoring for the treatment of frequently relapsing nephrotic syndrome in children: a multicenter randomized phase II trial. Pediatr Nephrol. 2014;9:271–278. doi: 10.2215/CJN.13071212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ishikura K, Ikeda M, Hattori S, Yoshikawa N, Sasaki S, Iijima K, Nakanishi K, Yata N, Honda M. Effective and safe treatment with cyclosporine in nephrotic children: a prospective, randomized multicenter trial. Kidney Int. 2008;73:1167–1173. doi: 10.1038/ki.2008.24. [DOI] [PubMed] [Google Scholar]
- 96.Niaudet P. Comparison of cyclosporin and chlorambucil in the treatment of steroid-dependent idiopathic nephrotic syndrome: a multicentre randomized controlled trial. The French Society of Paediatric Nephrology. Pediatr Nephrol. 1992;6:1–3. doi: 10.1007/BF00856817. [DOI] [PubMed] [Google Scholar]
- 97.Wang W, Xia Y, Mao J, Chen Y, Wang D, Shen H, Fu H, Du L, Liu A. Treatment of tacrolimus or cyclosporine A in children with idiopathic nephrotic syndrome. Pediatr Nephrol. 2012;27:2073–2079. doi: 10.1007/s00467-012-2228-3. [DOI] [PubMed] [Google Scholar]
- 98.Sinha MD, MacLeod R, Rigby E, Clark AGB. Treatment of severe steroid-dependent nephrotic syndrome (SDNS) in children with tacrolimus. Nephrol Dial Transplant. 2006;21:1848–1854. doi: 10.1093/ndt/gfi274. [DOI] [PubMed] [Google Scholar]
- 99.Tojo S. Clinical evaluation of ciclosporin in the treatment of nephrotic syndrome; a multi-center double blind study. Kidney Dial. 1994;37:565–608. [Google Scholar]
- 100.Ishikura K, Yoshikawa N, Hattori S, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Yata N, Ando T, Honda M. Treatment with microemulsified cyclosporine in children with frequently relapsing nephrotic syndrome. Nephrol Dial Transplant. 2010;25:3956–3962. doi: 10.1093/ndt/gfq318. [DOI] [PubMed] [Google Scholar]
- 101.Niaudet P, Broyer M, Habib R. Treatment of idiopathic nephrotic syndrome with cyclosporin A in children. Clin Nephrol. 1991;35(Suppl 1):S31–S36. [PubMed] [Google Scholar]
- 102.El-Husseini A, El-Basuony F, Mahmoud I, Sheashaa H, Sabry A, Hassan R, Taha N, Hassan N, Sayed-Ahmad N, Sobh M. Long-term effects of cyclosporine in children with idiopathic nephrotic syndrome: a single-centre experience. Nephrol Dial Transplant. 2005;20:2433–2438. doi: 10.1093/ndt/gfi059. [DOI] [PubMed] [Google Scholar]
- 103.Kitano Y, Yoshikawa N, Tanaka R, Nakamura H, Ninomiya M, Ito H. Ciclosporin treatment in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol. 1990;4:474–477. doi: 10.1007/BF00869823. [DOI] [PubMed] [Google Scholar]
- 104.Tanaka R, Yoshikawa N, Kitano Y, Ito H, Nakamura H. Long-term ciclosporin treatment in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol. 1993;7:249–252. doi: 10.1007/BF00853209. [DOI] [PubMed] [Google Scholar]
- 105.Inoue Y, Iijima K, Nakamura H, Yoshikawa N. Two-year cyclosporin treatment in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol. 1999;13:33–38. doi: 10.1007/s004670050558. [DOI] [PubMed] [Google Scholar]
- 106.Ishikura K, Yoshikawa N, Nakazato H, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Ito S, Yata N, Ando T, Honda M. Two-year follow-up of a prospective clinical trial of Cyclosporine for frequently relapsing nephrotic syndrome in children. Clin J Am Soc Nephrol. 2012;7:1576–1583. doi: 10.2215/CJN.00110112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dorresteijn EM, Kist-van Holthe JE, Levtchenko EN, Nauta J, Hop WC, van der Heijden AJ. Mycophenolate mofetil versus cyclosporine for remission maintenance in nephrotic syndrome. Pediatr Nephrol. 2008;23:2013–2020. doi: 10.1007/s00467-008-0899-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gellermann J, Weber L, Pape L, Tonshoff B, Hoyer P, Querfeld U. Mycophenolate mofetil versus cyclosporin A in children with frequently relapsing nephrotic syndrome. J Am Soc Nephrol. 2013;24:1689–1697. doi: 10.1681/ASN.2012121200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Uddin GMRM, Rahman MH, Roy RR, Begum A, Huque SS. Comparative efficacy of mycophenolate mofetil and cyclosporine in children with frequent relapse nephrotic syndrome [abstract] Pediatr Nephrol. 2016;31:1852–1853. [Google Scholar]
- 110.Wang J, Mao J, Chen J, Fu H, Shen H, Zhu X, Liu A, Shu Q, Du L. Evaluation of mycophenolate mofetil or tacrolimus in children with steroid sensitive but frequently relapsing or steroid-dependent nephrotic syndrome. Nephrology (Carlton) 2016;21:21–27. doi: 10.1111/nep.12537. [DOI] [PubMed] [Google Scholar]
- 111.Fujinaga S, Someya T, Watanabe T, Ito A, Ohtomo Y, Shimizu T, Kaneko K. Cyclosporine versus mycophenolate mofetil for maintenance of remission of steroid-dependent nephrotic syndrome after a single infusion of rituximab. Eur J Pediatr. 2013;172:513–518. doi: 10.1007/s00431-012-1913-3. [DOI] [PubMed] [Google Scholar]
- 112.Morgan C, Sis B, Pinsk M, Yiu V. Renal interstitial fibrosis in children treated with FK506 for nephrotic syndrome. Nephrol Dial Transplant. 2011;26:2860–2865. doi: 10.1093/ndt/gfq813. [DOI] [PubMed] [Google Scholar]
- 113.Sinha A, Bagga A, Gulati A, Hari P. Short-term efficacy of rituximab versus tacrolimus in steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2012;27:235–241. doi: 10.1007/s00467-011-1997-4. [DOI] [PubMed] [Google Scholar]
- 114.Dötsch J, Dittrich K, Plank C, Rascher W. Is tacrolimus for childhood steroid-dependent nephrotic syndrome better than ciclosporin A? Nephrol Dial Transplant. 2006;21:1761–1763. doi: 10.1093/ndt/gfl222. [DOI] [PubMed] [Google Scholar]
- 115.Iijima K, Hamahira K, Tanaka R, Kobayashi A, Nozu K, Nakamura H, Yoshikawa N. Risk factors for cyclosporine-induced tubulointerstitial lesions in children with minimal change nephrotic syndrome. Kidney Int. 2002;61:1801–1805. doi: 10.1046/j.1523-1755.2002.00303.x. [DOI] [PubMed] [Google Scholar]
- 116.Fujinaga S, Kaneko K, Muto T, Ohtomo Y, Murakami H, Yamashiro Y. Independent risk factors for chronic cyclosporine induced nephropathy in children with nephrotic syndrome. Arch Dis Child. 2006;91:666–670. doi: 10.1136/adc.2005.080960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Suzuki K, Oki E, Tsuruga K, Aizawa-Yashiro T, Ito E, Tanaka H. Benefits of once-daily administration of cyclosporine a for children with steroid-dependent, relapsing nephrotic syndrome. Tohoku J Exp Med. 2010;220:183–186. doi: 10.1620/tjem.220.183. [DOI] [PubMed] [Google Scholar]
- 118.Ishikura K, Ikeda M, Hamasaki Y, Hataya H, Nishimura G, Hiramoto R, Honda M. Nephrotic state as a risk factor for developing posterior reversible encephalopathy syndrome in paediatric patients with nephrotic syndrome. Nephrol Dial Transplant. 2008;23:2531–2536. doi: 10.1093/ndt/gfn013. [DOI] [PubMed] [Google Scholar]
- 119.Dittrich K, Knerr I, Rascher W, Dötsch J. Transient insulin-dependent diabetes mellitus in children with steroid-dependent idiopathic nephrotic syndrome during tacrolimus treatment. Pediatr Nephrol. 2006;21:958–961. doi: 10.1007/s00467-006-0102-x. [DOI] [PubMed] [Google Scholar]
- 120.David-Neto E, Araujo LP, Feres Alves C, Sumita N, Romano P, Yagyu EM, Nahas WC, Ianhez LE. A strategy to calculate cyclosporin A area under the time-concentration curve in pediatric renal transplantation. Pediatr Transplant. 2002;6:313–318. doi: 10.1034/j.1399-3046.2002.02019.x. [DOI] [PubMed] [Google Scholar]
- 121.Filler G. How should microemulsified Cyclosporine A (Neoral®) therapy in patients with nephrotic syndrome be monitored? Nephrol Dial Transplant. 2005;20:1032–1034. doi: 10.1093/ndt/gfh803. [DOI] [PubMed] [Google Scholar]
- 122.Prasad N, Gulati S, Sharma RK, Singh U, Ahmed M. Pulse cyclophosphamide therapy in steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2004;19:494–498. doi: 10.1007/s00467-003-1404-x. [DOI] [PubMed] [Google Scholar]
- 123.Abeyagunawardena ATRS (2006) Intravenous pulsed vs oral Cyclophosphamide therapy in steroid-dependent nephrotic syndrome (abstract no: COD.PP 54). Pediatr Nephrol 21:1535
- 124.Azib S, Macher MA, Kwon T, Dechartres A, Alberti C, Loirat C, Deschênes G, Baudouin V. Cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2011;26:927–932. doi: 10.1007/s00467-011-1830-0. [DOI] [PubMed] [Google Scholar]
- 125.Vester U, Kranz B, Zimmermann S, Hoyer PF. Cyclophosphamide in steroid-sensitive nephrotic syndrome: outcome and outlook. Pediatr Nephrol. 2003;18:661–664. doi: 10.1007/s00467-003-1170-9. [DOI] [PubMed] [Google Scholar]
- 126.Zagury A, de Oliveira AL, de Moraes CA, de Araujo Montalvão JA, Novaes RH, de Sá VM, de Carvalho M, Dde B, Matuck T. Long-term follow-up after cyclophosphamide therapy in steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2011;26:915–920. doi: 10.1007/s00467-011-1825-x. [DOI] [PubMed] [Google Scholar]
- 127.Cammas B, Harambat J, Bertholet-Thomas A, Bouissou F, Morin D, Guigonis V, Bendeddouche S, Afroukh-Hacini N, Cochat P, Llanas B, Decramer S, Ranchin B. Long-term effects of cyclophosphamide therapy in steroid-dependent or frequently relapsing idiopathic nephrotic syndrome. Nephrol Dial Transplant. 2010;26:178–184. doi: 10.1093/ndt/gfq405. [DOI] [PubMed] [Google Scholar]
- 128.Bajeer IA, Khatri S, Tresa V, Hashmi S, Mubarak M, Lanewala AA. Histopathological spectrum and short-term outcome of treatment with Cyclophosphamide in relapsing steroid-sensitive nephrotic syndrome. J Coll Physicians Surg Pak. 2018;28:436–439. doi: 10.29271/jcpsp.2018.06.436. [DOI] [PubMed] [Google Scholar]
- 129.Kyrieleis HAC, Levtchenko EN, Wetzels JFM. Long-term outcome after Cyclophosphamide treatment in children with steroid-dependent and frequently relapsing minimal change nephrotic syndrome. Am J Kidney Dis. 2007;49:592–597. doi: 10.1053/j.ajkd.2007.02.270. [DOI] [PubMed] [Google Scholar]
- 130.Kari JA, Alhasan KA, Albanna AS, Safdar OY, Shalaby MA, Böckenhauer D, El-Desoky SM. Rituximab versus cyclophosphamide as first steroid-sparing agent in childhood frequently relapsing and steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2020;35:1445–1453. doi: 10.1007/s00467-020-04570-y. [DOI] [PubMed] [Google Scholar]
- 131.Ponticelli C, Edefonti A, Ghio L, Rizzoni G, Rinaldi S, Gusmano R, Lama G, Zacchello G, Confalonieri R, Altieri P, et al. Cyclosporin versus cyclophosphamide for patients with steroid-dependent and frequently relapsing idiopathic nephrotic syndrome: a multicentre randomized controlled trial. Nephrol Dial Transplant. 1993;8:1326–1332. [PubMed] [Google Scholar]
- 132.Sandhu J, Bhat D, Dhooria GS. Oral cyclophosphamide therapy in 100 children with steroid-sensitive nephrotic syndrome: experience from a developing country. Pediatr Nephrol. 2021;36:2759–2767. doi: 10.1007/s00467-021-05052-5. [DOI] [PubMed] [Google Scholar]
- 133.Boumpas DT, Austin HA, 3rd, Vaughan EM, Yarboro CH, Klippel JH, Balow JE. Risk for sustained amenorrhea in patients with systemic lupus erythematosus receiving intermittent pulse cyclophosphamide therapy. Ann Intern Med. 1993;119:366–369. doi: 10.7326/0003-4819-119-5-199309010-00003. [DOI] [PubMed] [Google Scholar]
- 134.Pooni PA, Bhargava S, Kakkar S, Gill KS, Rivkees SA, Crawford JD. The relationship of gonadal activity and chemotherapy-induced gonadal damage. Pediatr Nephrol. 1988;259:2123–2125. [PubMed] [Google Scholar]
- 135.Clowse MB, McCune WJ (2021) General toxicity of cyclophosphamide in rheumatic disease. https://www.uptodate.com. Accessed 13 August 2020
- 136.Watson AR, Taylor J, Rance CP, Bain J. Gonadal function in women treated with cyclophosphamide for childhood nephrotic syndrome: a long-term follow-up study. Fertil Steril. 1986;46:331–333. doi: 10.1016/S0015-0282(16)49537-3. [DOI] [PubMed] [Google Scholar]
- 137.Wang CL, Wang F, Bosco JJ. Ovarian failure in oral cyclophosphamide treatment for systemic lupus erythematosus. Lupus. 1995;4:11–14. doi: 10.1177/096120339500400103. [DOI] [PubMed] [Google Scholar]
- 138.Lentz RD, Bergstein J, Steffes MW, Brown DR, Prem K, Michael AF, Vernier RL. Postpubertal evaluation of gonadal function following cyclophosphamide therapy before and during puberty. J Pediatr. 1977;91:385–394. doi: 10.1016/S0022-3476(77)81305-X. [DOI] [PubMed] [Google Scholar]
- 139.Gruppen MP, Bouts AH, Jansen-van der Weide MC, Merkus MP, Zurowska A, Maternik M, Massella L, Emma F, Niaudet P, Cornelissen EAM, Schurmans T, Raes A, van de Walle J, van Dyck M, Gulati A, Bagga A, Davin JC. A randomized clinical trial indicates that levamisole increases the time to relapse in children with steroid-sensitive idiopathic nephrotic syndrome. Kidney Int. 2018;93:510–518. doi: 10.1016/j.kint.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 140.Donia AF, Ammar HM, El-Agroudy Ael B, Moustafa Fel H, Sobh MA. Long-term results of two unconventional agents in steroid-dependent nephrotic children. Pediatr Nephrol. 2005;20:1420–1425. doi: 10.1007/s00467-005-1943-4. [DOI] [PubMed] [Google Scholar]
- 141.Sural S, Pahari D, Mitra K, Bhattacharya S, Mondal S, Taraphder A. Efficacy of levamisole compared to cyclophosphamide and steroid in frequently relapsing (FR) minimal change nephrotic syndrome (MCNS) J Am Soc Nephrol. 2001;12:126A. [Google Scholar]
- 142.Sinha A, Puraswani M, Kalaivani M, Goyal P, Hari P, Bagga A. Efficacy and safety of mycophenolate mofetil versus levamisole in frequently relapsing nephrotic syndrome: an open-label randomized controlled trial. Kidney Int. 2019;95:210–218. doi: 10.1016/j.kint.2018.08.039. [DOI] [PubMed] [Google Scholar]
- 143.Ekambaram S, Mahalingam V, Nageswaran P, Udani A, Geminiganesan S, Priyadarshini S. Efficacy of levamisole in children with frequently relapsing and steroid-dependent nephrotic syndrome. Ind Pediatr. 2014;51:371–373. doi: 10.1007/s13312-014-0419-7. [DOI] [PubMed] [Google Scholar]
- 144.Moorani KN, Zubair AM, Veerwani NR, Hotchandani HJ. Efficacy of Levamisole in children with frequent relapsing and steroid dependent nephrotic syndrome at tertiary care Center-Karachi. Pak J Med Sci. 2020;36:1193–1198. doi: 10.12669/pjms.36.6.2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Chen SY, Wu CY, Tsai IJ, Tsau YK. Treatment course of steroid-dependent nephrotic syndrome: emphasized on treatment effect. Nephrology (Carlton) 2010;15:336–339. doi: 10.1111/j.1440-1797.2009.01190.x. [DOI] [PubMed] [Google Scholar]
- 146.Sümegi V, Haszon I, Iványi B, Bereczki C, Papp F, Túri S. Long-term effects of levamisole treatment in childhood nephrotic syndrome. Pediatr Nephrol. 2004;19:1354–1360. doi: 10.1007/s00467-004-1608-8. [DOI] [PubMed] [Google Scholar]
- 147.Fu LS, Shien CY, Chi CS. Levamisole in steroid-sensitive nephrotic syndrome children with frequent relapses and/or steroid dependency: comparison of daily and every-other-day usage. Nephron Clin Pract. 2004;97:c137–c141. doi: 10.1159/000079172. [DOI] [PubMed] [Google Scholar]
- 148.Abeyagunawardena AS, Karunadasa U, Jayaweera H, Thalgahagoda S, Tennakoon S, Abeyagunawardena S. Efficacy of higher-dose levamisole in maintaining remission in steroid-dependant nephrotic syndrome. Pediatr Nephrol. 2017;32:1363–1367. doi: 10.1007/s00467-017-3616-5. [DOI] [PubMed] [Google Scholar]
- 149.Kiruba Samuel EM, Krishnamurthy S, Bhanudeep S, Muske S. Levamisole in Frequently-relapsing and Steroid-dependent Nephrotic Syndrome. Ind Pediatr. 2017;54:831–834. doi: 10.1007/s13312-017-1144-9. [DOI] [PubMed] [Google Scholar]
- 150.Fujinaga S, Ohtomo Y, Umino D, Takemoto M, Shimizu T, Yamashiro Y, Kaneko K. A prospective study on the use of mycophenolate mofetil in children with cyclosporine-dependent nephrotic syndrome. Pediatr Nephrol. 2007;22:71–76. doi: 10.1007/s00467-006-0294-0. [DOI] [PubMed] [Google Scholar]
- 151.Fujinaga S, Ohtomo Y, Hirano D, Nishizaki N, Someya T, Ohtsuka Y, Kaneko K, Shimizu T. Mycophenolate mofetil therapy for childhood-onset steroid dependent nephrotic syndrome after long-term cyclosporine: extended experience in a single center. Clin Nephrol. 2009;72:268–273. [PubMed] [Google Scholar]
- 152.Benz MR, Ehren R, Kleinert D, Müller C, Gellermann J, Fehrenbach H, Schmidt H, Weber LT. Generation and validation of a limited sampling strategy to monitor Mycophenolic acid exposure in children with nephrotic syndrome. Drug Monit. 2019;41:696–702. doi: 10.1097/FTD.0000000000000671. [DOI] [PubMed] [Google Scholar]
- 153.Pawinski T, Kunicki PK, Sobieszczanska-Malek M, Gralak B, Szlaska I. A limited sampling strategy for estimating mycophenolic acid area under the curve in adult heart transplant patients treated with concomitant cyclosporine. J Clin Pharm Ther. 2009;34:89–101. doi: 10.1111/j.1365-2710.2008.00973.x. [DOI] [PubMed] [Google Scholar]
- 154.van Gelder T, Berden JHM, Berger SP. To TDM or not to TDM in lupus nephritis patients treated with MMF? Nephrol Dial Transplant. 2014;30:560–564. doi: 10.1093/ndt/gfu184. [DOI] [PubMed] [Google Scholar]
- 155.Weber LT, Shipkova M, Armstrong VW, Wagner N, Schütz E, Mehls O, Zimmerhackl LB, Oellerich M, Tönshoff B. Comparison of the Emit immunoassay with HPLC for therapeutic drug monitoring of mycophenolic acid in pediatric renal-transplant recipients on mycophenolate mofetil therapy. Clinical Chem. 2002;48:517–525. doi: 10.1093/clinchem/48.3.517. [DOI] [PubMed] [Google Scholar]
- 156.Afzal K, Bagga A, Menon S, Hari P, Jordan SC. Treatment with mycophenolate mofetil and prednisolone for steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2007;22:2059–2065. doi: 10.1007/s00467-007-0617-9. [DOI] [PubMed] [Google Scholar]
- 157.Banerjee S, Pahari A, Sengupta J, Patnaik SK. Outcome of severe steroid-dependent nephrotic syndrome treated with mycophenolate mofetil. Pediatr Nephrol. 2013;28:93–97. doi: 10.1007/s00467-012-2278-6. [DOI] [PubMed] [Google Scholar]
- 158.Karunamoorthy S, Thanigachalam D, Jeyachandran D, Ramanathan S, Natarajan G, Thoppalan B. The safety and efficacy of mycophenolate mofetil in children and adolescents with steroid-dependent nephrotic syndrome: a single-centre study. Clin Kidney. 2020;J13:179–183. doi: 10.1093/ckj/sfz061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Nandi M, Mandal SK, Samanta M, Majhi A, Das MK. Efficacy of Mycophenolate Mofetil as a remission maintaining agent in idiopathic childhood nephrotic syndrome. Ind J Nephrol. 2019;29:34–41. doi: 10.4103/ijn.IJN_330_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kapoor K, Saha A, Kaur M, Dubey NK, Upadhyay AD. Mycophenolate sodium for children with frequently relapsing or steroid dependent nephrotic syndrome. Ind Pediatr. 2017;54:885–886. doi: 10.1007/s13312-017-1156-5. [DOI] [PubMed] [Google Scholar]
- 161.Mouyis M, Flint JD, Giles IP. Safety of anti-rheumatic drugs in men trying to conceive: a systematic review and analysis of published evidence. Semin Arthritis Rheuma. 2019;48:911–920. doi: 10.1016/j.semarthrit.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 162.Kuypers DRJ, Van Mieghem T, Meijers B, Claes K. Updated manufacturer and european medicines agency recommendations on the use of mycophenolate acid. Transplant. 2016;100:e50–e51. doi: 10.1097/TP.0000000000001342. [DOI] [PubMed] [Google Scholar]
- 163.Kallash M, Smoyer WE, Mahan JD. Rituximab use in the management of childhood nephrotic syndrome. Front Pediatr. 2019;7:178. doi: 10.3389/fped.2019.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Chan EY, Tullus K. Rituximab in children with steroid sensitive nephrotic syndrome: in quest of the optimal regimen. Pediatr Nephrol. 2021;36:1397–1405. doi: 10.1007/s00467-020-04609-0. [DOI] [PubMed] [Google Scholar]
- 165.Bhatia D, Sinha A, Hari P, Sopory S, Saini S, Puraswani M, Saini H, Mitra DK, Bagga A. Rituximab modulates T- and B-lymphocyte subsets and urinary CD80 excretion in patients with steroid-dependent nephrotic syndrome. Pediatr Res. 2018;84:520–526. doi: 10.1038/s41390-018-0088-7. [DOI] [PubMed] [Google Scholar]
- 166.Iijima K, Sako M, Oba M, Tanaka S, Hamada R, Sakai T, Ohwada Y. Mycophenolate Mofetil after rituximab for childhood-onset complicated frequently-relapsing or steroid-dependent nephrotic syndrome. J Am Soc Nephrol. 2022;33:401–419. doi: 10.1681/ASN.2021050643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Iijima K, Sako M, Nozu K, Mori R, Tuchida N, Kamei K, Miura K, Aya K, Nakanishi K, Ohtomo Y, Takahashi S, Tanaka R, Kaito H, Nakamura H, Ishikura K, Ito S, Ohashi Y. Rituximab for childhood-onset, complicated, frequently relapsing nephrotic syndrome or steroid-dependent nephrotic syndrome: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2014;384:1273–1281. doi: 10.1016/S0140-6736(14)60541-9. [DOI] [PubMed] [Google Scholar]
- 168.Boumediene A, Vachin P, Sendeyo K, Oniszczuk J, Zhang SY, Henique C, Pawlak A, Audard V, Ollero M, Guigonis V, Sahali D. NEPHRUTIX: A randomized, double-blind, placebo vs Rituximab-controlled trial assessing T-cell subset changes in Minimal Change Nephrotic Syndrome. J Autoimm. 2018;88:91–102. doi: 10.1016/j.jaut.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 169.Ravani P, Magnasco A, Edefonti A, Murer L, Rossi R, Ghio L, Benetti E, Scozzola F, Pasini A, Dallera N, Sica F, Belingheri M, Scolari F, Ghiggeri GM. Short-term effects of Rituximab in children with steroid- and calcineurin-dependent nephrotic syndrome: a randomized controlled trial. Clin J Am Soc Nephrol. 2011;6:1308–1315. doi: 10.2215/CJN.09421010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ahn YH, Kim SH, Han KH, Choi HJ, Cho H, Lee JW, Shin JI, Cho MH, Lee JH, Park YS, Ha IS, Cheong HI, Kim SY, Lee SJ, Kang HG. Efficacy and safety of rituximab in childhood-onset, difficult-to-treat nephrotic syndrome: a multicenter open-label trial in Korea. Medicine. 2018;97:e13157. doi: 10.1097/MD.0000000000013157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Basu B, Sander A, Roy B, Preussler S, Barua S, Mahapatra TKS, Schaefer F. Efficacy of Rituximab vs Tacrolimus in pediatric corticosteroid-dependent nephrotic syndrome: a randomized clinical trial. JAMA Pediatr. 2018;172:757–764. doi: 10.1001/jamapediatrics.2018.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ravani P, Rossi R, Bonanni A, Quinn RR, Sica F, Bodria M, Pasini A, Montini G, Edefonti A, Belingheri M, De Giovanni D, Barbano G, Degl’Innocenti L, Scolari F, Murer L, Reiser J, Fornoni A, Ghiggeri GM (2015) Rituximab in children with steroid-dependent nephrotic syndrome: a multicenter, open-label, noninferiority, randomized controlled trial. J Am Soc Nephrol 26:2259-2266 [DOI] [PMC free article] [PubMed]
- 173.Ravani P, Lugani F, Pisani I, Bodria M, Piaggio G, Bartolomeo D, Prunotto M, Ghiggeri GM. Rituximab for very low dose steroid-dependent nephrotic syndrome in children: a randomized controlled study. Pediatr Nephrol. 2020;35:1437–1444. doi: 10.1007/s00467-020-04540-4. [DOI] [PubMed] [Google Scholar]
- 174.Ravani P, Lugani F, Drovandi S, Caridi G, Angeletti A, Ghiggeri GM. Rituximab vs low-dose Mycophenolate Mofetil in recurrence of steroid-dependent nephrotic syndrome in children and young adults: a randomized clinical trial. JAMA Pediatr. 2021;175:631–632. doi: 10.1001/jamapediatrics.2020.6150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Fujinaga S, Hirano D, Mizutani A, Sakuraya K, Yamada A, Sakurai S, Shimizu T. Predictors of relapse and long-term outcome in children with steroid-dependent nephrotic syndrome after rituximab treatment. Clin Exp Nephrol. 2017;21:671–676. doi: 10.1007/s10157-016-1328-y. [DOI] [PubMed] [Google Scholar]
- 176.Hogan J, Dossier C, Kwon T, Macher MA, Maisin A, Couderc A, Niel O, Baudouin V, Deschênes G. Effect of different rituximab regimens on B cell depletion and time to relapse in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2019;34:253–259. doi: 10.1007/s00467-018-4052-x. [DOI] [PubMed] [Google Scholar]
- 177.Lim ZRS, Teh KL, Das L, Arkachaisri T (2021) Neutropenia following Rituximab in paediatric non-malignant diseases: case series and review of the literature. Singapore Med J. 10.11622/smedj.2021188 [DOI] [PMC free article] [PubMed]
- 178.Monaco WE, Jones JD, Rigby WF. Rituximab associated late-onset neutropenia-a rheumatology case series and review of the literature. Clin Rheumatol. 2016;35:2457–2462. doi: 10.1007/s10067-016-3313-y. [DOI] [PubMed] [Google Scholar]
- 179.Besada E, Koldingsnes W, Nossent J. Characteristics of late onset neutropenia in rheumatologic patients treated with rituximab: a case review analysis from a single center. QJM. 2012;105:545–550. doi: 10.1093/qjmed/hcs015. [DOI] [PubMed] [Google Scholar]
- 180.Chan EY, Webb H, Yu E, Ghiggeri GM, Kemper MJ, Ma AL, Yamamura T, Sinha A, Bagga A, Hogan J, Dossier C, Vivarelli M, Liu ID, Kamei K, Ishikura K, Saini P, Tullus K. Both the rituximab dose and maintenance immunosuppression in steroid-dependent/frequently-relapsing nephrotic syndrome have important effects on outcomes. Kidney Int. 2020;97:393–401. doi: 10.1016/j.kint.2019.09.033. [DOI] [PubMed] [Google Scholar]
- 181.Colucci M, Carsetti R, Serafinelli J, Rocca S, Massella L, Gargiulo A, Lo Russo A, Capponi C, Cotugno N, Porzio O, Onetti Muda A, Palma P, Emma F, Vivarelli M. Prolonged impairment of immunological memory after anti-CD20 treatment in pediatric idiopathic nephrotic syndrome. Front Immunol. 2019;10:1653. doi: 10.3389/fimmu.2019.01653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Chan EY-H, Yu ELM, Angeletti A, Arslan Z, Basu B, Boyer O, Chan C-Y, Colucci M, Dorval G, Dossier C, Drovandi S, Ghiggeri GM, Gipson DS, Hamada R, Hogan J, Ishikura K, Kamei K, Kemper MJ, Ma AL-T, Parekh RS, Radhakrishnan S, Saini P, Shen Q, Sinha R, Subun C, Teo S, Vivarelli M, Webb H, Xu H, Yap HK, Tullus K. Long-term efficacy and safety of repeated rituximab to maintain remission in idiopathic childhood nephrotic syndrome: an international study. J Am Soc Nephrol. 2022;33:1193–1207. doi: 10.1681/ASN.2021111472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Ito S, Kamei K, Ogura M, Sato M, Fujimaru T, Ishikawa T, Udagawa T, Iijima K. Maintenance therapy with mycophenolate mofetil after rituximab in pediatric patients with steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2011;26:1823–1828. doi: 10.1007/s00467-011-1886-x. [DOI] [PubMed] [Google Scholar]
- 184.Vivarelli M, Colucci M, Bonanni A, Verzani M, Serafinelli J, Emma F, Ghiggeri G. Ofatumumab in two pediatric nephrotic syndrome patients allergic to rituximab. Pediatr Nephrol. 2017;32:181–184. doi: 10.1007/s00467-016-3498-y. [DOI] [PubMed] [Google Scholar]
- 185.Ravani P, Colucci M, Bruschi M, Vivarelli M, Cioni M, DiDonato A, Cravedi P, Lugani F, Antonini F, Prunotto M, Emma F, Angeletti A, Ghiggeri GM. Human or chimeric monoclonal anti-CD20 antibodies for children with nephrotic syndrome: a superiority randomized trial. J Am Soc Nephrol. 2021;32:2652–2663. doi: 10.1681/ASN.2021040561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Abramowicz M, Barnett HL, Edelmann CM, Jr, Greifer I, Kobayashi O, Arneil GC, Barron BA, Gordillo PG, Hallman N, Tiddens HA. Controlled trial of azathioprine in children with nephrotic syndrome. A report for the international study of kidney disease in children. Lancet. 1970;1:959–961. doi: 10.1016/S0140-6736(70)91093-7. [DOI] [PubMed] [Google Scholar]
- 187.Wang C-s, Travers C, McCracken C, Leong T, Gbadegesin R, Quiroga A, Benfield MR, Hidalgo G, Srivastava T, Lo M, Yadin O, Mathias R, Araya CE, Khalid M, Orjuela A, Zaritsky J, Al-Akash S, Kamel M, Greenbaum LA. Adrenocorticotropic hormone for childhood nephrotic syndrome. Clin J Am Soc Nephrol. 2018;13:1859–1865. doi: 10.2215/CJN.06890618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Yoshioka K, Ohashi Y, Sakai T, Ito H, Yoshikawa N, Nakamura H, Tanizawa T, Wada H, Maki S. A multicenter trial of mizoribine compared with placebo in children with frequently relapsing nephrotic syndrome. Kidney Int. 2000;58:317–324. doi: 10.1046/j.1523-1755.2000.00168.x. [DOI] [PubMed] [Google Scholar]
- 189.Vande Walle JG, Donckerwolcke RA, van Isselt JW, Derkx FH, Joles JA, Koomans HA. Volume regulation in children with early relapse of minimal-change nephrosis with or without hypovolaemic symptoms. Lancet. 1995;346:148–152. doi: 10.1016/S0140-6736(95)91210-X. [DOI] [PubMed] [Google Scholar]
- 190.Bockenhauer D. Over- or underfill: not all nephrotic states are created equal. Pediatr Nephrol. 2013;28:1153–1156. doi: 10.1007/s00467-013-2435-6. [DOI] [PubMed] [Google Scholar]
- 191.Cadnapaphornchai MA, Tkachenko O, Shchekochikhin D, Schrier RW. The nephrotic syndrome: pathogenesis and treatment of edema formation and secondary complications. Pediatr Nephrol. 2014;29:1159–1167. doi: 10.1007/s00467-013-2567-8. [DOI] [PubMed] [Google Scholar]
- 192.Schrier RW, Fassett RG. A critique of the overfill hypothesis of sodium and water retention in the nephrotic syndrome. Kidney Int. 1998;53:1111–1117. doi: 10.1046/j.1523-1755.1998.00864.x. [DOI] [PubMed] [Google Scholar]
- 193.Kapur G, Valentini RP, Imam AA, Mattoo TK. Treatment of severe edema in children with nephrotic syndrome with diuretics alone—a prospective study. Clin J Am Soc Nephrol. 2009;4:907–913. doi: 10.2215/CJN.04390808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Kapur G, Valentini RP, Imam AA, Jain A, Mattoo TK. Serum osmolal gap in patients with idiopathic nephrotic syndrome and severe edema. Pediatrics. 2007;119:e1404–e1407. doi: 10.1542/peds.2006-2554. [DOI] [PubMed] [Google Scholar]
- 195.Kontchou LM, Liccioli G, Pela I. Blood pressure in children with minimal change nephrotic syndrome during oedema and after steroid therapy: the influence of familial essential hypertension. Kidney Blood Press Res. 2009;32:258–262. doi: 10.1159/000238823. [DOI] [PubMed] [Google Scholar]
- 196.Keshri S, Sharma S, Agrawal N, Bansal S, Guilliani BP, Aggrawal KC. Hypertension and its severity in children with steroid sensitive nephrotic syndrome during remission. Clin Exp Nephrol. 2018;22:1157–1162. doi: 10.1007/s10157-018-1565-3. [DOI] [PubMed] [Google Scholar]
- 197.Shatat IF, Becton LJ, Woroniecki RP. Hypertension in childhood nephrotic syndrome. Front Pediatr. 2019;7:287. doi: 10.3389/fped.2019.00287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Küster S, Mehls O, Seidel C, Ritz E. Blood pressure in minimal change and other types of nephrotic syndrome. Am J Nephrol. 1990;10(Suppl 1):76–80. doi: 10.1159/000168198. [DOI] [PubMed] [Google Scholar]
- 199.(1981) The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr 98:561–564 [DOI] [PubMed]
- 200.Gabban NIA, Abdullah AE, Abd HN. Nephrotic syndrome and hypertension. Iraqi J Comm Med. 2010;4:271–276. [Google Scholar]
- 201.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904. doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 202.Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, Invitti C, Litwin M, Mancia G, Pall D, Rascher W, Redon J, Schaefer F, Seeman T, Sinha M, Stabouli S, Webb NJ, Wuhl E, Zanchetti A. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34:1887–1920. doi: 10.1097/HJH.0000000000001039. [DOI] [PubMed] [Google Scholar]
- 203.Suri D, Ahluwalia J, Saxena AK, Sodhi KS, Singh P, Mittal BR, Das R, Rawat A, Singh S. Thromboembolic complications in childhood nephrotic syndrome: a clinical profile. Clin Exp Nephrol. 2014;18:803–813. doi: 10.1007/s10157-013-0917-2. [DOI] [PubMed] [Google Scholar]
- 204.Kerlin BA, Blatt NB, Fuh B, Zhao S, Lehman A, Blanchong C, Mahan JD, Smoyer WE. Epidemiology and risk factors for thromboembolic complications of childhood nephrotic syndrome: a Midwest Pediatric Nephrology Consortium (MWPNC) study. J Pediatr. 2009;155(105–110):110.e101. doi: 10.1016/j.jpeds.2009.01.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Kerlin BA, Ayoob R, Smoyer WE. Epidemiology and pathophysiology of nephrotic syndrome-associated thromboembolic disease. Clin J Am Soc Nephrol. 2012;7:513–520. doi: 10.2215/CJN.10131011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Lilova MI, Velkovski IG, Topalov IB. Thromboembolic complications in children with nephrotic syndrome in Bulgaria (1974–1996) Pediatr Nephrol. 2000;15:74–78. doi: 10.1007/s004679900253. [DOI] [PubMed] [Google Scholar]
- 207.Zaffanello M, Franchini M. Thromboembolism in childhood nephrotic syndrome: a rare but serious complication. Hematology. 2007;12:69–73. doi: 10.1080/10245330600940048. [DOI] [PubMed] [Google Scholar]
- 208.Carpenter SL, Goldman J, Sherman AK, Selewski DT, Kallash M, Tran CL, Seamon M, Katsoufis C, Ashoor I, Hernandez J, Supe-Markovina K, D'Alessandri-Silva C, DeJesus-Gonzalez N, Vasylyeva TL, Formeck C, Woll C, Gbadegesin R, Geier P, Devarajan P, Smoyer WE, Kerlin BA, Rheault MN. Association of infections and venous thromboembolism in hospitalized children with nephrotic syndrome. Pediatr Nephrol. 2019;34:261–267. doi: 10.1007/s00467-018-4072-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Kerlin BA, Haworth K, Smoyer WE. Venous thromboembolism in pediatric nephrotic syndrome. Pediatr Nephrol. 2014;29:989–997. doi: 10.1007/s00467-013-2525-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.(1984) Minimal change nephrotic syndrome in children: deaths during the first 5 to 15 years' observation. Report of the International Study of Kidney Disease in Children. Pediatrics 73:497–501 [PubMed]
- 211.Uncu N, Bulbul M, Yildiz N, Noyan A, Kosan C, Kavukcu S, Caliskan S, Gunduz Z, Besbas N, Gur Guven A. Primary peritonitis in children with nephrotic syndrome: results of a 5-year multicenter study. Eur J Pediatr. 2010;169:73–76. doi: 10.1007/s00431-009-0989-x. [DOI] [PubMed] [Google Scholar]
- 212.Gorensek MJ, Lebel MH, Nelson JD. Peritonitis in children with nephrotic syndrome. Pediatrics. 1988;81:849–856. doi: 10.1542/peds.81.6.849. [DOI] [PubMed] [Google Scholar]
- 213.Krensky AM, Ingelfinger JR, Grupe WE. Peritonitis in childhood nephrotic syndrome: 1970–1980. Am J Dis Child. 1982;136:732–736. doi: 10.1001/archpedi.1982.03970440076023. [DOI] [PubMed] [Google Scholar]
- 214.McCaffrey J, Lennon R, Webb NJ. The non-immunosuppressive management of childhood nephrotic syndrome. Pediatr Nephrol. 2016;31:1383–1402. doi: 10.1007/s00467-015-3241-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Kumar M, Ghunawat J, Saikia D, Manchanda V. Incidence and risk factors for major infections in hospitalized children with nephrotic syndrome. J Bras Nephrol. 2019;41:526–533. doi: 10.1590/2175-8239-jbn-2019-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Feinstein EI, Chesney RW, Zelikovic I. Peritonitis in childhood renal disease. Am J Nephrol. 1988;8:147–165. doi: 10.1159/000167575. [DOI] [PubMed] [Google Scholar]
- 217.Gulati S, Kher V, Gupta A, Arora P, Rai PK, Sharma RK. Spectrum of infections in Indian children with nephrotic syndrome. Pediatr Nephrol. 1995;9:431–434. doi: 10.1007/BF00866719. [DOI] [PubMed] [Google Scholar]
- 218.Hingorani SR, Weiss NS, Watkins SL. Predictors of peritonitis in children with nephrotic syndrome. Pediatr Nephrol. 2002;17:678–682. doi: 10.1007/s00467-002-0890-6. [DOI] [PubMed] [Google Scholar]
- 219.Teo S, Walker A, Steer A. Spontaneous bacterial peritonitis as a presenting feature of nephrotic syndrome. J Paediatr Child Health. 2013;49:1069–1071. doi: 10.1111/jpc.12389. [DOI] [PubMed] [Google Scholar]
- 220.Manta M, Singh S. Infection associated relapses in children with nephrotic syndrome: A short-term outcome study. Saudi J Kidney Dis Transpl. 2019;30:1245–1253. doi: 10.4103/1319-2442.275468. [DOI] [PubMed] [Google Scholar]
- 221.Yetgin S, Gur A, Saatci U. Non-specific immunity in nephrotic syndrome. Acta Paediatr Scand. 1980;69:21–24. doi: 10.1111/j.1651-2227.1980.tb07023.x. [DOI] [PubMed] [Google Scholar]
- 222.Matsell DG, Wyatt RJ. The role of I and B in peritonitis associated with the nephrotic syndrome of childhood. Pediatr Res. 1993;34:84–88. doi: 10.1203/00006450-199307000-00019. [DOI] [PubMed] [Google Scholar]
- 223.Tain YL, Lin G, Cher TW. Microbiological spectrum of septicemia and peritonitis in nephrotic children. Pediatr Nephrol. 1999;13:835–837. doi: 10.1007/s004670050710. [DOI] [PubMed] [Google Scholar]
- 224.Tapaneya-Olarn C, Tapaneya-Olarn W. Primary peritonitis in childhood nephrotic syndrome: a changing trend in causative organisms. J Med Assoc Thailand. 1991;74:502–506. [PubMed] [Google Scholar]
- 225.Bagga A, Sinha A, Moudgil A. Rituximab in patients with the steroid-resistant nephrotic syndrome. N Engl J Med. 2007;356:2751–2752. doi: 10.1056/NEJMc063706. [DOI] [PubMed] [Google Scholar]
- 226.HHS Panel on Opportunistic Infections in HIV-Exposed and HIV-Infected Children (2013) Guidelines for the prevention and treatment of opportunistic infections in HIV-exposed and HIV-infected children. https://clinicalinfo.hiv.gov/en/guidelines/pediatric-opportunistic-infection [Dosing Table Pneumocystis jirovecii, p.32]. Accessed December 2020
- 227.HHS Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV (2019) Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection. Accessed December 2020
- 228.BMJ Best Practice (2021) Secondary hypogammglobulinemia. https://bestpractice.bmj.com/. Accessed 14 November 2021
- 229.Angeletti A, Bruschi M, Bianchin S, Bonato I. Vaccines and disease relapses in children with nephrotic syndrome. Clin J Am Soc Nephrol. 2021;16:937–938. doi: 10.2215/CJN.01890221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Ishimori S, Kamei K, Ando T, Yoshikawa T, Kano Y, Nagata H, Saida K, Sato M, Ogura M, Ito S, Ishikura K. Influenza virus vaccination in children with nephrotic syndrome: insignificant risk of relapse. Clin J Am Soc Nephrol. 2020;24:1069–1076. doi: 10.1007/s10157-020-01930-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Fernandes P, Jorge S, Lopes JA. Relapse of nephrotic syndrome following the use of 2009 pandemic influenza A (H1N1) vaccine. Clin Exp Nephrol. 2010;56:185–186. doi: 10.1053/j.ajkd.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 232.Klifa R, Toubiana J, Michel A, Biebuyck N, Charbit M, Heidet L, Krid S, Krug P, Salomon R, Boyer O. Influenza vaccination among children with idiopathic nephrotic syndrome: an investigation of practices. BMC Nephrol. 2019;20:65. doi: 10.1186/s12882-019-1240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Ishimori S, Ando T, Kikunaga K, Terano C, Sato M, Komaki F, Hamada R, Hamasaki Y, Araki Y, Gotoh Y, Nakanishi K, Nakazato H, Matsuyama T, Iijima K, Yoshikawa N, Ito S, Honda M, Ishikura K. Influenza virus vaccination in pediatric nephrotic syndrome significantly reduces rate of relapse and influenza virus infection as assessed in a nationwide survey. Sci Rep. 2021;11:23305. doi: 10.1038/s41598-021-02644-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Tanaka S, Saikusa T, Katafuchi Y, Ushijima K, Ohtsu Y, Tsumura N, Ito Y. Serologic response after vaccination against influenza (A/H1N1)pdm09 in children with renal disease receiving oral immunosuppressive drugs. Vaccine. 2015;33:5000–5004. doi: 10.1016/j.vaccine.2015.06.049. [DOI] [PubMed] [Google Scholar]
- 235.Tran CL, Selewski DT, Oh GJ, Troost JP, Massengill SF, Al-Akash SI, Mahesh S, Amin R, Ashoor IF, Chanchlani R, Kallash M, Woroniecki RP, Gipson DS. Pediatric immunization practices in nephrotic syndrome: an assessment of provider and parental knowledge. Front Pediatr. 2020;8:619548. doi: 10.3389/fped.2020.619548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Robinson CL, Bernstein H, Poehling K, Romero JR. Szilagyi P (2020) Advisory committee on immunization practices recommended immunization schedule for children and adolescents aged 18 years or younger—United States. MMWR Morb Mortality Wkly Rep. 2020;69:130–132. doi: 10.15585/mmwr.mm6905a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Kamei K, Miyairi I, Ishikura K, Ogura M, Shoji K, Funaki T, Ito R, Arai K, Abe J, Kawai T, Onodera M, Ito S. Prospective study of live attenuated vaccines for patients with nephrotic syndrome receiving immunosuppressive agents. J Pediatr. 2018;196:217–222.e211. doi: 10.1016/j.jpeds.2017.12.061. [DOI] [PubMed] [Google Scholar]
- 238.Furth SL, Arbus GS, Hogg R, Tarver J, Chan C, Fivush BA. Varicella vaccination in children with nephrotic syndrome: a report of the Southwest Pediatric Nephrology Study Group. J Pediatr. 2003;142:145–148. doi: 10.1067/mpd.2003.37. [DOI] [PubMed] [Google Scholar]
- 239.Sinha R, Agrawal N, Xue Y, Chanchlani R, Pradhan S, Raina R, Marks SD. Use of rituximab in paediatric nephrology. Arch Dis Child. 2021;106:1058–1065. doi: 10.1136/archdischild-2020-321211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Fribourg M, Cioni M, Ghiggeri G, Cantarelli C, Leventhal JS, Budge K, Bin S, Riella LV, Colucci M, Vivarelli M, Angeletti A, Perin L, Cravedi P. CyTOF-enabled analysis identifies class-switched B cells as the main lymphocyte subset associated with disease relapse in children with idiopathic nephrotic syndrome. Arch Dis Child. 2021;12:726428. doi: 10.3389/fimmu.2021.726428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Finkel KC. Mortality from varicella in children receiving adrenocorticosteroids and adrenocorticotropin. Pediatrics. 1961;28:436–441. doi: 10.1542/peds.28.3.436. [DOI] [PubMed] [Google Scholar]
- 242.Falliers CJ, Ellis EF. Corticosteroids and varicella. Six-year experience in an asthmatic population. Arch Dis Child. 1965;40:593–599. doi: 10.1136/adc.40.214.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Dowell SF, Bresee JS. Severe varicella associated with steroid use. Pediatrics. 1993;92:223–228. doi: 10.1542/peds.92.2.223. [DOI] [PubMed] [Google Scholar]
- 244.Committee on Infectious Diseases, American Academy of Pediatrics (2012) Varicella-zoster infections. In: Pickering LK, Baker CJ, Kimberlin DW, Long SS (eds) Red book: 2012 report of the Committee on Infectious Diseases, 29th ed. American Academy of Pediatrics, Elk Grove Village, IL, pp 774–789
- 245.United States Food and Drug Administration (2012) FDA approves VariZIG for reducing chickenpox symptoms. US FDA, Silver Spring, MD
- 246.Levin MJ, Duchon JM, Swamy GK, Gershon AA. Varicella zoster immune globulin (VARIZIG) administration up to 10 days after varicella exposure in pregnant women, immunocompromised participants, and infants: Varicella outcomes and safety results from a large, open-label, expanded-access program. PLoS One. 2019;14:e0217749. doi: 10.1371/journal.pone.0217749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Goldstein SL, Somers MJ, Lande MB, Brewer ED, Jabs KL. Acyclovir prophylaxis of varicella in children with renal disease receiving steroids. Pediatr Nephrol. 2000;14:305–308. doi: 10.1007/s004670050764. [DOI] [PubMed] [Google Scholar]
- 248.Lin TY, Huang YC, Ning HC, Hsueh C. Oral acyclovir prophylaxis of varicella after intimate contact. Pediatr Infect Dis J. 1997;16:1162–1165. doi: 10.1097/00006454-199712000-00012. [DOI] [PubMed] [Google Scholar]
- 249.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Lipsitch M, Swerdlow DL, Finelli L. Defining the Epidemiology of Covid-19 - Studies Needed. N Engl J Med. 2020;382:1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 251.Emmi G, Bettiol A, Mattioli I, Silvestri E, Di Scala G, Urban ML, Vaglio A, Prisco D. SARS-CoV-2 infection among patients with systemic autoimmune diseases. Autoimm Rev. 2020;19:102575. doi: 10.1016/j.autrev.2020.102575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Angeletti A, Drovandi S, Sanguineri F, Santaniello M, Ferrando G, Forno R, Cipresso G, Caridi G (2020) COVID-19 in Children with Nephrotic Syndrome on Anti-CD20 Chronic Immunosuppression Clin J Am Soc Nephrol 15:1494–1495 [DOI] [PMC free article] [PubMed]
- 253.Morello W, Vianello FA, Proverbio E, Peruzzi L, Pasini A, Montini G. COVID-19 and idiopathic nephrotic syndrome in children: systematic review of the literature and recommendations from a highly affected area. Pediatr Nephrol. 2022;37:757–764. doi: 10.1007/s00467-021-05330-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.El-Mashad GM, El-Hawy MA, El-Hefnawy SM, Mohamed SM. Bone mineral density in children with idiopathic nephrotic syndrome. J Pediatr (Rio J) 2017;93:142–147. doi: 10.1016/j.jped.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 255.Gulati S, Godbole M, Singh U, Gulati K, Srivastava A. Are children with idiopathic nephrotic syndrome at risk for metabolic bone disease? Am J Kidney Dis. 2003;41:1163–1169. doi: 10.1016/S0272-6386(03)00348-2. [DOI] [PubMed] [Google Scholar]
- 256.Lettgen B, Jeken C, Reiners C. Influence of steroid medication on bone mineral density in children with nephrotic syndrome. Pediatr Nephrol. 1994;8:667–670. doi: 10.1007/BF00869084. [DOI] [PubMed] [Google Scholar]
- 257.Ribeiro D, Zawadynski S, Pittet LF, Chevalley T, Girardin E, Parvex P. Effect of glucocorticoids on growth and bone mineral density in children with nephrotic syndrome. Eur J Pediatr. 2015;174:911–917. doi: 10.1007/s00431-014-2479-z. [DOI] [PubMed] [Google Scholar]
- 258.Mishra OP, Meena SK, Singh SK, Prasad R, Mishra RN. Bone mineral density in children with steroid-sensitive nephrotic syndrome. Ind J Pediatr. 2009;76:1237–1239. doi: 10.1007/s12098-009-0256-1. [DOI] [PubMed] [Google Scholar]
- 259.Esbjörner E, Arvidsson B, Jones IL, Palmér M. Bone mineral content and collagen metabolites in children receiving steroid treatment for nephrotic syndrome. Acta Paediatr. 2001;90:1127–1130. doi: 10.1111/j.1651-2227.2001.tb03241.x. [DOI] [PubMed] [Google Scholar]
- 260.Moon RJ, Gilbert RD, Page A, Murphy L, Taylor P, Cooper C, Dennison EM, Davies JH. Children with nephrotic syndrome have greater bone area but similar volumetric bone mineral density to healthy controls. Bone. 2014;58:108–113. doi: 10.1016/j.bone.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Leonard MB, Feldman HI, Shults J, Zemel BS, Foster BJ, Stallings VA. Long-term, high-dose glucocorticoids and bone mineral content in childhood glucocorticoid-sensitive nephrotic syndrome. N Engl J Med. 2004;351:868–875. doi: 10.1056/NEJMoa040367. [DOI] [PubMed] [Google Scholar]
- 262.Polito C, La Manna A, Todisco N, Cimmaruta E, Sessa G, Pirozzi M. Bone mineral content in nephrotic children on long-term, alternate-day prednisone therapy. Clin Pediatr. 1995;34:234–236. doi: 10.1177/000992289503400501. [DOI] [PubMed] [Google Scholar]
- 263.Feber J, Gaboury I, Ni A, Alos N, Arora S, Bell L, Blydt-Hansen T, Clarson C, Filler G, Hay J, Hebert D, Lentle B, Matzinger M, Midgley J, Moher D, Pinsk M, Rauch F, Rodd C, Shenouda N, Siminoski K, Ward LM. Skeletal findings in children recently initiating glucocorticoids for the treatment of nephrotic syndrome. Osteoporosis Int. 2012;23:751–760. doi: 10.1007/s00198-011-1621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Phan V, Blydt-Hansen T, Feber J, Alos N, Arora S, Atkinson S, Bell L, Clarson C, Couch R, Cummings EA, Filler G, Grant RM, Grimmer J, Hebert D, Lentle B, Ma J, Matzinger M, Midgley J, Pinsk M, Rodd C, Shenouda N, Stein R, Stephure D, Taback S, Williams K, Rauch F, Siminoski K, Ward LM. Skeletal findings in the first 12 months following initiation of glucocorticoid therapy for pediatric nephrotic syndrome. Osteoporos Int. 2014;25:627–637. doi: 10.1007/s00198-013-2466-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Grymonprez A, Proesmans W, Van Dyck M, Jans I, Goos G, Bouillon R. Vitamin D metabolites in childhood nephrotic syndrome. Pediatr Nephrol. 1995;9:278–281. doi: 10.1007/BF02254183. [DOI] [PubMed] [Google Scholar]
- 266.Barragry JM, France MW, Carter ND, Auton JA, Beer M, Boucher BJ, Cohen RD. Vitamin-D metabolism in nephrotic syndrome. Lancet. 1977;2:629–632. doi: 10.1016/S0140-6736(77)92498-9. [DOI] [PubMed] [Google Scholar]
- 267.Weng FL, Shults J, Herskovitz RM, Zemel BS, Leonard MB. Vitamin D insufficiency in steroid-sensitive nephrotic syndrome in remission. Pediatr Nephrol. 2005;20:56–63. doi: 10.1007/s00467-004-1694-7. [DOI] [PubMed] [Google Scholar]
- 268.Banerjee S, Basu S, Sengupta J. Vitamin D in nephrotic syndrome remission: a case-control study. Pediatr Nephrol. 2013;28:1983–1989. doi: 10.1007/s00467-013-2511-y. [DOI] [PubMed] [Google Scholar]
- 269.Biyikli NK, Emre S, Sirin A, Bilge I. Biochemical bone markers in nephrotic children. Pediatr Nephrol. 2004;19:869–873. doi: 10.1007/s00467-004-1537-6. [DOI] [PubMed] [Google Scholar]
- 270.Banerjee S, Basu S, Akhtar S, Sinha R, Sen A, Sengupta J. Free vitamin D levels in steroid-sensitive nephrotic syndrome and healthy controls. Pediatr Nephrol. 2020;35:447–454. doi: 10.1007/s00467-019-04433-1. [DOI] [PubMed] [Google Scholar]
- 271.Bak M, Serdaroglu E, Guclu R. Prophylactic calcium and vitamin D treatments in steroid-treated children with nephrotic syndrome. Pediatr Nephrol. 2006;21:350–354. doi: 10.1007/s00467-005-2118-z. [DOI] [PubMed] [Google Scholar]
- 272.Choudhary S, Agarwal I, Seshadri MS. Calcium and vitamin D for osteoprotection in children with new-onset nephrotic syndrome treated with steroids: a prospective, randomized, controlled, interventional study. Pediatr Nephrol. 2014;29:1025–1032. doi: 10.1007/s00467-013-2720-4. [DOI] [PubMed] [Google Scholar]
- 273.Gulati S, Sharma RK, Gulati K, Singh U, Srivastava A. Longitudinal follow-up of bone mineral density in children with nephrotic syndrome and the role of calcium and vitamin D supplements. Nephrol Dial Transplant. 2005;20:1598–1603. doi: 10.1093/ndt/gfh809. [DOI] [PubMed] [Google Scholar]
- 274.Gargiulo A, Bettini C, Lo Russo A, Emma F, Banerjee S. The effect of vitamin D and calcium supplementation in pediatric steroid-sensitive nephrotic syndrome. Pediatr Nephrol. 2017;32:2063–2070. doi: 10.1007/s00467-017-3716-2. [DOI] [PubMed] [Google Scholar]
- 275.Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, Michigami T, Tiosano D, Mughal MZ, Mäkitie O, Ramos-Abad L, Ward L, DiMeglio LA, Atapattu N, Cassinelli H, Braegger C, Pettifor JM, Seth A, Idris HW, Bhatia V, Fu J, Goldberg G, Sävendahl L, Khadgawat R, Pludowski P, Maddock J, Hyppönen E, Oduwole A, Frew E, Aguiar M, Tulchinsky T, Butler G, Högler W. Global Consensus Recommendations on Prevention and Management of Nutritional Rickets. J Clin Endocrinol Metab. 2016;101:394–415. doi: 10.1210/jc.2015-2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Malihi Z, Wu Z, Stewart AW, Lawes CM, Scragg R. Hypercalcemia, hypercalciuria, and kidney stones in long-term studies of vitamin D supplementation: a systematic review and meta-analysis. Am J Clin Nutr. 2016;104:1039–1051. doi: 10.3945/ajcn.116.134981. [DOI] [PubMed] [Google Scholar]
- 277.Shroff R, Wan M, Nagler EV, Bakkaloglu S, Fischer DC, Bishop N, Cozzolino M, Bacchetta J, Edefonti A, Stefanidis CJ, Vande Walle J, Haffner D, Klaus G, Schmitt CP. Clinical practice recommendations for native vitamin D therapy in children with chronic kidney disease Stages 2–5 and on dialysis. Nephrol Dial Transplant. 2017;32:1098–1113. doi: 10.1093/ndt/gfx065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Basu S, Sen A, Sengupta J, Abu Bakar K, Khalil K, Lim YN, Yap YC, Appadurai M, Sidhu S, Lai CS, Anuar Zaini A, Samingan N, Jalaludin MY. Adrenal insufficiency in children with nephrotic syndrome on corticosteroid treatment. Pediatr Nephrol. 2020;8:164. doi: 10.3389/fped.2020.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Furst DE, Saag KG (2021) Glucocorticoid withdrawal. https://www.uptodate.com. Accessed 20 December 2021
- 280.Rodrigo R, Bravo I, Pino M. Proteinuria and albumin homeostasis in the nephrotic syndrome: effect of dietary protein intake. Nutr Rev. 1996;54:337–347. doi: 10.1111/j.1753-4887.1996.tb03800.x. [DOI] [PubMed] [Google Scholar]
- 281.Siegel NJ, Goldberg B, Krassner LS, Hayslett JP. Long-term follow-up of children with steroid-responsive nephrotic syndrome. J Pediatr. 1972;81:251–258. doi: 10.1016/S0022-3476(72)80291-9. [DOI] [PubMed] [Google Scholar]
- 282.Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS. Long-term outcome for children with minimal-change nephrotic syndrome. Lancet. 1985;1:368–370. doi: 10.1016/S0140-6736(85)91387-X. [DOI] [PubMed] [Google Scholar]
- 283.Lewis MA, Baildom EM, Davies N, Houston IB, Postlethwaite RJ. Steroid-sensitive minimal change nephrotic syndrome. Long-term follow-up Contrib Nephrol. 1988;67:226–228. doi: 10.1159/000415405. [DOI] [PubMed] [Google Scholar]
- 284.Takeichi S, Tazawa M, Morooka M, Minowa S, Yasaki T. Long-term follow-up study of children with minimal change nephrotic syndrome. Nihon Jinzo Gakkai Shi. 1997;39:155–160. doi: 10.2329/perio.39.Supplement3_155. [DOI] [PubMed] [Google Scholar]
- 285.Fakhouri F, Bocquet N, Taupin P, Presne C, Gagnadoux MF, Landais P, Lesavre P, Chauveau D, Knebelmann B, Broyer M, Grünfeld JP, Niaudet P. Steroid-sensitive nephrotic syndrome: from childhood to adulthood. Am J Kidney Dis. 2003;41:550–557. doi: 10.1053/ajkd.2003.50116. [DOI] [PubMed] [Google Scholar]
- 286.Skrzypczyk P, Panczyk-Tomaszewska M, Roszkowska-Blaim M, Wawer Z, Bienias B, Zajgzkowska M, Kilis-Pstrusinska K, Jakubowska A, Szczepaniak M, Pawlak-Bratkowska M, Tkaczyk M. Long-term outcomes in idiopathic nephrotic syndrome: from childhood to adulthood. Clin Nephrol. 2014;81:166–173. doi: 10.5414/CN108044. [DOI] [PubMed] [Google Scholar]
- 287.Aydin M, Franke I, Kurylowicz L, Ganschow R, Lentze M, Born M, Hagemann R. The long-term outcome of childhood nephrotic syndrome in Germany: a cross-sectional study. Clin Exp Nephrol. 2019;23:676–688. doi: 10.1007/s10157-019-01696-8. [DOI] [PubMed] [Google Scholar]
- 288.Lewis MA, Baildom EM, Davis N, Houston IB, Postlethwaite RJ. Nephrotic syndrome: from toddlers to twenties. Lancet. 1989;1:255–259. doi: 10.1016/S0140-6736(89)91266-X. [DOI] [PubMed] [Google Scholar]
- 289.Kyrieleis HA, Löwik MM, Pronk I, Cruysberg HR, Kremer JA, Oyen WJ, van den Heuvel BL, Wetzels JF, Levtchenko EN. Long-term outcome of biopsy-proven, frequently relapsing minimal-change nephrotic syndrome in children. Clin J Am Soc Nephrol. 2009;4:1593–1600. doi: 10.2215/CJN.05691108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Motoyama O, Iitaka K. Final height in children with steroid-sensitive nephrotic syndrome. Pediatr Int. 2007;49:623–625. doi: 10.1111/j.1442-200X.2007.02429.x. [DOI] [PubMed] [Google Scholar]
- 291.Lechner BL, Bockenhauer D, Iragorri S, Kennedy TL, Siegel NJ. The risk of cardiovascular disease in adults who have had childhood nephrotic syndrome. Pediatr Nephrol. 2004;19:744–774. doi: 10.1007/s00467-004-1460-x. [DOI] [PubMed] [Google Scholar]
- 292.Matsukura H, Inaba S, Shinozaki K, Yanagihara T, Hara M, Higuchi A, Takada T, Tanizawa T, Miyawaki T. Influence of prolonged corticosteroid therapy on the outcome of steroid-responsive nephrotic syndrome. Am J Nephrol. 2001;21:362–367. doi: 10.1159/000046275. [DOI] [PubMed] [Google Scholar]
- 293.Watson AR, Harden P, Ferris M, Kerr PG, Mahan J, Ramzy MF. Transition from pediatric to adult renal services: a consensus statement by the International Society of Nephrology (ISN) and the International Pediatric Nephrology Association (IPNA) Pediatr Nephrol. 2011;26:1753–1757. doi: 10.1007/s00467-011-1981-z. [DOI] [PubMed] [Google Scholar]
- 294.Dobbels F, Ruppar T, De Geest S, Decorte A, Van Damme-Lombaerts R, Fine RN. Adherence to the immunosuppressive regimen in pediatric kidney transplant recipients: a systematic review. Pediatr Transplant. 2010;14:603–613. doi: 10.1111/j.1399-3046.2010.01299.x. [DOI] [PubMed] [Google Scholar]
- 295.Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol. 2000;14:469–472. doi: 10.1007/s004670050794. [DOI] [PubMed] [Google Scholar]
- 296.Beck L, Bomback AS, Choi MJ, Holzman LB, Langford C, Mariani LH, Somers MJ, Trachtman H, Waldman M. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for glomerulonephritis. Am J Kidney Dis. 2013;62:403–441. doi: 10.1053/j.ajkd.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 297.Floege J, Barbour SJ, Cattran DC, Hogan JJ, Nachman PH, Tang SCW, Wetzels JFM, Cheung M, Wheeler DC, Winkelmayer WC, Rovin BH. Management and treatment of glomerular diseases (part 1): conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int. 2019;95:268–280. doi: 10.1016/j.kint.2018.10.018. [DOI] [PubMed] [Google Scholar]
- 298.Rovin BH, Caster DJ, Cattran DC, Gibson KL, Hogan JJ, Moeller MJ, Roccatello D, Cheung M, Wheeler DC, Winkelmayer WC, Floege J. Management and treatment of glomerular diseases (part 2): conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95:281–295. doi: 10.1016/j.kint.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 299.Honda M, Iijima K, Ishikura K, Kaneko K. The problem of transition from pediatric to adult healthcare in patients with steroid-sensitive nephrotic syndrome (SSNS): a survey of the experts. Clin Exp Nephrol. 2014;18:939–943. doi: 10.1007/s10157-014-0941-x. [DOI] [PubMed] [Google Scholar]
- 300.Schwartz GJ, Work DF. Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol. 2009;4:1832–1843. doi: 10.2215/CJN.01640309. [DOI] [PubMed] [Google Scholar]
- 301.Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20:629–637. doi: 10.1681/ASN.2008030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.