Abstract
Objective
To comprehensively summarize the evidence on the preferences, expectations, and values of hypertension management and treatment in hypertensive patients.
Methods
From inception through January 2022, PubMed, Embase, Web of Science, EBSCO, and China National Knowledge Infrastructure were searched for studies with hypertension value, preference, or expectation. A qualitative retrospective analysis was performed.
Results
A total of 24 studies involving 8701 participants were included. Although studies on the preferences of hypertensive patients are difficult to standardize, considerable convergence has occurred: 1) Patients preferred treatment regimens with lower incidence of comorbidities, faster response, lower cost, more frequent blood pressure monitoring, fewer side effects, and more convenient medication. 2) Patients have a crucial role in the treatment, and their physicians are expected to develop a shared patient-centered decision-making model.
Conclusion
The results of this systematic review demonstrated that side effects, cost, and convenience are important factors for patients when selecting a treatment regimen for hypertension. Patients often obtain hypertension information from their physicians and prefer shared patient-centered decision-making.
Keywords: patient preferences, hypertension, hypertension management, systematic review
Introduction
Hypertension is a critical risk factor for cardiovascular and cerebrovascular disease, affecting the heart, brain, kidneys, and other human organs.1 The high prevalence and low control rate of hypertension in the United States are worrying, and the global trend is not optimistic, particularly in low- and middle-income countries.2 Effective antihypertensive treatment can reduce all-cause and cardiovascular mortality, as well as the risk of cardiovascular events, including coronary heart disease (CHD), stroke, and heart failure.3 Although hypertension is a preventable and controllable condition, its outcomes are largely dependent on government disease control measures, doctor treatment strategies, patient adherence, and family member help.4 Furthermore, most hypertensive patients are asymptomatic and may be unaware of the need for treatment since they have no symptoms that compel them to seek treatment, even if they have mild clinical symptoms.5
Although definitions of hypertension vary among guidelines, the indications and treatment regimens for antihypertensive treatment are relatively similar. Currently, the major treatment options for hypertension are divided into non-pharmacological (including lifestyle interventions and various device-based therapies) and pharmacological management. Based on the recommended guidelines, ACEI inhibitors, Angiotensin Receptor Blockers (ARBs), calcium channel blockers, and thiazide or thiazide-like diuretics are usually selected as the first-line agents, and β-blockers as first-line therapy in patients with severe comorbidities.6,7 Despite the well-established treatment options for hypertension, the actual awareness, treatment, and control rates of hypertension are disappointingly low, necessitating urgent improvements in patient screening, diagnosis, treatment, and follow-up.8 Hence, it becomes even more essential to consider that patient values and treatment preferences positively impact the management and treatment of hypertension.
In the medical process, patient preferences and values are increasingly considered critical components of evidence-based medicine. Simultaneously, when making decisions, the patient’s voice should be fully considered.9 Although the skillful application of guidelines can help clinicians make easier, faster, and better decisions about the diagnosis and treatment of disease, guidelines cannot replace clinicians’ compassionate and mindful engagement with the patients in shared decision-making when patient preferences and values are important.10 Due to differences in patients’ backgrounds, goals, and values, it is difficult for clinicians to effectively understand each patient’s preferences. Clinicians’ diagnosis and treatment conceptions may be inconsistent with patients’ preferences and values. Investigating the preferences, expectations, and values of hypertensive patients helps manage and treat hypertension. In this study, a systematic literature review was conducted to comprehensively summarize the evidence.
Methods
Eligibility Criteria
The study included systematic literature searches meeting the following criteria: 1) The study population was adult patients with hypertension, including patients with normal hypertension and resistant hypertension; 2) The research content was associated with the patient preferences, expectations, and values for the management and treatment of hypertension; 3) To study the decision-making of hypertensive patients to receive hypertension treatment and the factors that influence the patient’s choice. The exclusion criteria were as follows: 1) Not related to hypertension or patient preferences, expectations, and values; 2) Letters, reviews, case reports, and posters.
Data Sources and Search Strategy
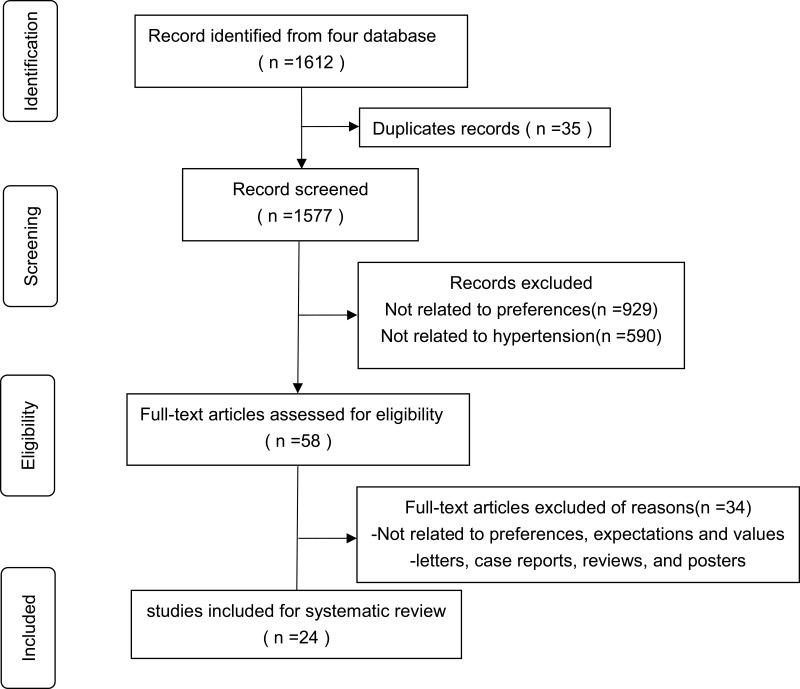
From their inception to January 2022, five electronic databases were systematically searched (PubMed, Embase, Web of Science, EBSCO, and China National Knowledge Infrastructure). Key phrases included “hypertension”, “high blood pressure”, or “blood pressure” in combination with “preferences”, “expectations”, or “values”. We searched the PubMed database for MeSH terms as well as all relevant search terms to find potential articles that used the terms “hypertension” in combination with “patient preference”. Table 1 represents the search strategy for PubMed, and Figure 1 depicts the specific systematic literature screening process.
Table 1.
Search Strategy for PubMed
| Query | Search Term |
|---|---|
| #1 | Hypertension [Mesh] |
| #2 | Hypertension[Title/Abstract] OR High Blood Pressure[Title/Abstract] OR Blood Pressure[Title/Abstract] |
| #3 | #1 OR #2 |
| #4 | Patient Preference [Mesh] |
| #5 | Patient*Preference*[title/abstract] OR Patient*Expectation*[title/abstract] OR Patient*Value*[title/abstract] OR Patient*View*[title/abstract] OR Patient*Perspective*[title/abstract] OR patient*perception*[title/abstract] OR Patient*Decision*[title/abstract] |
| #6 | #4 OR #5 |
| #7 | #3 AND #6 |
Figure 1.
Flow diagram of the selection process.
Data Extraction and Quality Assessment
Two reviewers independently conducted the literature screening and information extraction, and any discrepancies were resolved through discussion. Data on the first author, date of publication, sample size, study design, study description, results, and demographics were extracted by the reviewers.
The quality of the literature was independently assessed by two independent reviewers using instruments recommended by the Agency for Healthcare Research and Quality (AHRQ),11 and the disagreement was resolved through a third-party discussion. The AHRQ checklist is a commonly used tool for evaluating observational studies, consisting of 11 items that are answered with “yes” (scored 1), “no” (scored 0),) and “unclear” (scored 0). The quality was classified into three levels: low quality = 0–3; moderate quality = 4–7; high quality = 8–11.
Results
Characteristics of Included Studies
A total of 1612 articles were obtained with electronic search, of which 58 full-text studies were selected after the screening of the title and abstract. The full text of the remaining 58 articles was then screened, and finally, 24 articles meeting the inclusion criteria were selected (Figure 1). Most studies on patient preferences in patients with hypertension were conducted in patients from American (n = 7), Europe (n = 6), Asia (n = 5), Africa (n = 3), and Canada (n = 3). Table 2 provides an overview of the research, including the date of the study, sample size, study design, study description, preferences, and methodological quality.
Table 2.
Characteristics of Included Studies and Summary of Results
| Author | Country | Date | Study Design | Sample Size | Study Description | Preferences, Expectations, and Values | Score |
|---|---|---|---|---|---|---|---|
| Howren et al12 | American | 2020 | Cross-sectional | 598 | Using sharing subscale of the patient-practitioner orientation scale (PPOS). | Patients generally tended to be provider-centered in discussing medication use | 8 |
| Ogedegbe et al13 | American | 2004 | Cross-sectional | 93 | In-depth, open-ended individual interviews | Expected to play an active role in treatment, follow their physicians’ recommendations, and know the side effects of medication and prevention of complications | 10 |
| Morecroft et al14 | United Kingdom | 2006 | Cross-sectional | 120 | Questionnaire | Tended to leave the decision to the physician and actively participate in the management of hypertension | 8 |
| Lisper et al15 | Sweden | 1997 | Cross-sectional | 21 | Semi-structured interviews | Preferred to receive information about medicines from physicians and concerning possible side-effects | 7 |
| Schoenthaler et al16 | American | 2018 | Prospective study | 75 | Using electronic monitoring device (EMD) to measure patient’s medication behavior | Expected to more active decision-making style and expected to leave decision-making to physicians | 9 |
| Metcalfe et al17 | Canada | 2020 | Cross-sectional | 183 | Focus groups and interviews | Pregnant hypertensive patients would prefer to hear more information and make the final decision with physicians | 9 |
| Bulgin et al18 | American | 2021 | Cross-sectional | 96 | Semi-structured interviews | Expected to receive information on hypertension and understood the benefits of lifestyle changes | 8 |
| Mah et al19 | Malaysia | 2016 | Cross-sectional | 210 | Questionnaire | Preferred decision-making roles and collaborative roles | 9 |
| Halifax et al20 | Canada | 2007 | Cross-sectional | 24 | Focus group meetings | Expected to learn more about hypertension and develop collaborative relationships with physicians. | 7 |
| Kario et al21 | Japan | 2021 | Cross-sectional | 2392 | Online survey | A total of 755 patients (31.6%) expressed a preference for RDN | 8 |
| Schmieder et al22 | Germany | 2018 | Cross-sectional | 1101 | Questionnaire | Many younger male patients would choose catheter-based RDN over lifelong medical therapy, and physicians were the critical mediator of treatment choice. | 10 |
| McAlister et al23 | Canada | 2000 | Cross-sectional | 146 | Questionnaire and a face-to-face interview | Patients generally required more potential benefit than physicians to offset the inconvenience, cost, and side effects of antihypertensive drugs | 8 |
| Montgomery et al24 | United Kingdom | 2001 | Cross-sectional | 52 | Interview | Nearly half of the patients would refuse treatment if there were a preference for health outcomes, especially the side effects of drugs | 8 |
| Rahman et al25 | Asia | 2015 | Cross- sectional | 904 | Qualitative interviews and focus groups with patients | 79% of Asian patients were most concerned about the possibility of a stroke, with more than half (57%) neglecting to monitor their blood pressure | 9 |
| Nasothimiou et al26 | Greece | 2014 | Prospective study | 104 | Participants were evaluated with ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM) | HBPM was superior to ABPM in terms of overall acceptance and preference by hypertensive patients | 9 |
| Konlan et al27 | Ghana | 2020 | Cross-sectional | 16 | In-depth interviews | Patients preferred timely pain management, ie, when they felt pain, they expected the nurses to respond to their needs promptly | 8 |
| Gebrezgi et al28 | Eritrea | 2017 | Cross-sectional | 48 | In-depth interviews and focus group investigations | Participants reported financial constraints inhibiting their ability to follow the recommended diet management | 7 |
| Fletcher et al29 | United Kingdom | 2019 | Cross-sectional | 167 | Semi-structured interviews | Patients preferred scenarios that had more significant reduction in cardiovascular risk, more frequent BP monitoring, and lower costs. | 10 |
| Cremers et al30 | Nigeria | 2019 | Cross-sectional | 328 | Structured-interviews | Patient concerned about side effects of medication and cost of treatment | 8 |
| Flynn et al31 | American | 2013 | Randomized clinical trial | 30 | Focus group investigations | Both patient and family member participants recognized family members as important facilitators to patients’ hypertension self-care | 9 |
| Gibson et al32 | American | 2018 | Cross-sectional | 60 | Semi-structured interviews | Frequently focused on short-term benefits rather than long-term benefits | 8 |
| Fairchild et al33 | American | 2016 | Cross-sectional | 60 | Semi-structured interviews | Most participants felt that adding lifestyle changes would allow them to stop the medication and even cure their disease; almost all participants (97%) wanted to hear about their disease from their physician | 9 |
| Anthony et al34 | Israel | 2012 | Cross-sectional | 86 | Focus groups and interviews | Patients did not perceive high blood pressure as a chronic disease requiring adherence to treatment recommendations but rather as a health condition primarily related to stress | 8 |
| Nishigaki et al35 | Japan | 2019 | Cross-sectional | 881 | Online survey | About 33.5% of patients reported no changes in their diet or exercise regimen since diagnosis, 29.1% believed that hypertension could be treated casually, and 10–15% responded that they felt it was unnecessary when they were asymptomatic | 8 |
The Preferences and Expectations for Decision-Making
The preferences and expectations for decision-making were reported in nine studies. Most patients knowing they had hypertension, anticipated an essential role in their treatment. They expected their physicians to develop a patient-centric model of shared decision-making. At the same time, because most patients lacked pertinent knowledge on hypertension, they anticipated learning more about it from doctors during the diagnostic and treatment processes, including treatment courses, side effects of medication and complications, etc. Patients usually let doctors make the final call in the end.
Howren et al examined patient preference data from a randomized clinical trial designed to test the efficacy of a patient activation intervention in encouraging the prescribing of thiazides to uncontrolled hypertensive patients. They found that those who were provider-centric in the most intensive intervention sectors started discussing thiazides more than others.12 According to a different study,13 patients expected their physicians to educate them about hypertension treatments and the medications that would decrease their blood pressure and protect them from heart attacks, strokes, and kidney failure. In this study, 27% of patients to anticipated actively participating in their treatment, and 57% expected to be aware of the benefits, risks, and potential problems of their blood pressure medications. According to Morecroft et al,14 patients needed to believe that their general practitioner was in charge of their treatment and that decision-making on what blood pressure level is considered appropriate should be left to them. Lisper et al15 revealed that the patients preferred to get information about their medications from their physicians, and they reported a desire to do so before starting their pharmaceutical regimen, particularly about potential adverse effects. As per Schoenthaler et al,16 over two-thirds of patients (57.3%) preferred to participate in shared decision-making (SDM) during the clinic visit, which involved making a choice together and considering the doctor’s advice. In another study,17 most of the pregnant hypertensive patients said they would prefer information about pregnancy hypertension from their physicians (79%), and nearly 82% wanted this information when they were at risk for pregnancy hypertension before they experienced hypertension. According to Bulgin et al,18 patients were expected to learn about hypertension and comprehend the advantages of making lifestyle adjustments. According to the research by Mah et al,19 51.4% of patients chose a collaborative role with a doctor, 44.8% preferred a passive role, and only 1.9% preferred an active role. In preferred decision-making roles. In another study,20 patients stated that they lacked a working knowledge of the most fundamental terms related to hypertension and the health effects of high or low blood pressure. However, they acknowledged that they were responsible for their health, made responsible choices, and developed physician partnerships.
The Preferences and Expectations for Management and Treatment
The preferences and expectations for management and treatment were reported in ten studies. In terms of management and treatment, regimens that that decrease the incidence of comorbidities, respond quicker, are less expensive, monitor blood pressure more frequently, have fewer side effects, and make medication more convenient are preferred, with side effects being a consideration for the vast majority of patients.
In a countrywide survey of Japanese patients, the Kario et al 2022 study looked into patients’ preferences for renal denervation.21 The study discovered that nearly one-third of the patients preferred RDN, among which patients with resistant hypertension, poor adherence to antihypertensive medications, younger patients, and patients with side effects during antihypertensive treatment were more likely to prefer RDN.21 A similar study conducted in Germany22 revealed that RDN was favored by 38.2% of individuals who were not already taking medicine and by 28.2% of those who were. Patients’ preferences were found to be influenced by antihypertensive effects, the experience of side effects, and medication adherence. The study by McAlister et al showed that patients generally needed greater potential benefits than physicians to make up for the difficulty, expense, and side effects of antihypertensive medications.23 The study by Montgomery et al found that among patients with a 5-year absolute risk of >10% and those with systolic blood pressure greater than 160 mmHg, nearly half would avoid treatment if the patient’s preference for health outcomes, particularly drug side effects and complications, was taken into consideration.24 In the study by Rahman et al, 79% of Asian patients were concerned about the possibility of a stroke, with more than half (57%) neglecting monitoring their blood pressure.25 AAs per the study by Nasothimiou et al,26 which compared the patients’ preferences for ambulatory blood pressure monitoring and home blood pressure monitoring, discovered that HBPM significantly performed better than ABPM in terms of overall patient acceptance and preference, with broad availability, lower cost, and higher patient acceptance, and should be the process of choice for out-of-office blood pressure assessment in most patients in clinical practice. A 2020 in-depth interview by Konlan et al stated that when patients were enquired about their expectations for care prior to admission, patients reported that they expected nurses to be very responsive to their needs and should proactively meet those needs, to treat pain as an emergency, and comfort them when they are in pain.27
A study by Gebrezgi et al found that a patient’s economic status can affect the management of hypertension in different ways. Eritrea provides antihypertensive medications free of charge, and economic status does not appear to affect patients’ adherence to antihypertensive medications. However, financial status affects patients’ adherence to lifestyle changes, such as dietary management and purchasing blood pressure management devices.28 The study by Fletcher et al29 in the UK found that patients preferred options with a greater reduction in cardiovascular risk, more frequent blood pressure monitoring, and lower cost, revealing that cost is an important factor influencing patient preference even in developed countries. A mixed methods research found that half of the patients face financial constraints and sometimes difficulties in purchasing medicines, with the economic downturn significantly impacting patients’ ability to afford medicines.30
Additional Perspectives on Patients’ Preferences
Flynn et al compared urban African American patients and family members’ perceptions of facilitators and barriers to hypertension self-management and found that both patient and family member participants believed family members were essential facilitators of patients’ hypertension self-care factors.31 The study by Gibson et al32 showed that there are significant information gaps in the short-term and long-term benefits of hypertensive medication usage in hypertensive patients. However, the most important advantage of these drugs was a reduction in the risk of long-term complications due to improved disease control; nonetheless, these benefits were mentioned by less than half of patients with hypertension.32 The majority of the participants believed that strengthening lifestyle changes would enable them to stop the medication, avoid additional medication, or cure their hypertension. These participants were quite optimistic about their ability to improve their lifestyle, attributing their expectations to scientific progress, good social and medical support, and stress relief.33 In another study, from the patient’s point of view, patients generally did not perceive high blood pressure as a chronic disease requiring adherence to treatment recommendations but rather as a primarily stress-related health condition with no consequences if left untreated.34 In a study by Nishigaki et al,35 33.5% of patients reported no changes in their diet or exercise regimen since diagnosis, 29.1% believed that hypertension could be treated casually, and 10–15% believed that there is no need to take antihypertensive medications or inform their physicians when they are asymptomatic or have stable blood pressure.
Discussion
This systematic literature review involving 24 publications summarizes the preferences, values, and expectations of hypertensive patients in managing and treating hypertension. Both patients and physicians should focus on patient preferences, values, and expectations because they can help determine the trade-offs between the benefits and harms associated with various treatment options, allowing the patient to select the optimal treatment regimen at a particular level.36 Controlling blood pressure levels is the primary objective of hypertension management and treatment. In the absence of novel antihypertensive medications, it is critical that healthcare providers focus on how to use the medications better.37 Patient refusal and non-adherence to treatment for hypertension appear to be a common phenomenon, indicating conscious choices made by patients based on their knowledge and perceptions of their medical condition and its treatment.
People’s understanding of health and disease is limited to their bodies or personal experiences; thus, during their visits, patients seek as much information on hypertension as possible from healthcare professionals. In a study, most of the patients looked to healthcare professionals as sources of information on hypertension, expecting them to inform about the side effects of antihypertensive medications and their mechanisms of action and learn about the physiology of antihypertensive medications and the prevention of complications.13 In clinical exposure reports, patients with shared decision-making were more likely to have positive health outcomes, such as improved self-reported health status, self-management behaviors, emotional well-being, fewer referrals for diagnostic tests, nursing satisfaction, adherence to treatment plans, less invasive treatment options, and shorter hospital stays.16 SDM is a patient-centered care model in which patient-provider information on available options is shared, preferences and goals for the possible outcomes of a decision are expressed, and physicians and patients collaborate in making the final decision, discussing various treatment options to meet patient priorities and health care needs.38,39 The patient-centered decision-making model did not completely transform the passive position of the patient in decision-making, suggesting that even with sufficient information about hypertension, the patient may consider the provider’s recommendations while participating in shared decision-making.16 A study found that patients’ preference for shared decision-making was significantly related to their age and education level, with younger and more educated patients preferring SDM.19
Furthermore, the findings of this study suggest that patients’ preferences and expectations for the management and treatment of hypertension are diverse, and different patient groups have different preferences for treatment options. Patients usually prefer treatment options with fewer comorbidities, faster responses, lower costs, more frequent blood pressure monitoring, fewer side effects, and easier medication administration. Age and gender differences are crucial for hypertension management and treatment preferences, and there are significant age and gender differences in the acceptance of management and treatment methods.21,23 After decades of development, despite its clinical efficacy data have been mixed, renal denervation (RDN) has emerged as a potential emerging treatment modality, with catheter-based RDN being one of the important options for patients with resistant hypertension.40–42 In a study where approximately one-third of the patients surveyed expressed a preference for RDN, younger patients were more likely to prefer RDN than older patients, and patients who experienced side effects during antihypertensive treatment were more likely to prefer RDN.21 A project evaluating the use of RDN as a treatment option in hypertensive patients in Germany revealed that younger men are more likely to receive RDN, which may be related to the fact that men are more likely to take risks than women, and younger individuals are more likely to take risks than older.
Moreover, a significant issue is that many patients usually do not believe that high blood pressure is a chronic disease that requires adherence to treatment recommendations. On the contrary, they believe that improving lifestyles such as diet and exercise can avoid taking antihypertensive drugs or even cure the disease. How to change the concept of these patients and improve their understanding of the risk of hypertension is also a significant issue for medical personnel.33–35
Limitations
This qualitative review analysis has some limitations. First, only a few studies fully met the inclusion criteria for this review. Some studies met the inclusion criteria for this review but did not provide sufficient detail regarding patient preferences, expectations, and values, which may have influenced our analysis. Second, there is currently a lack of standardized reporting and evidence for determining patient preferences for the definitions of preferences, expectations, and values. Systematic literature review approaches to summarizing the evidence are tentative and empirical, therefore, outcomes may be variable.
Conclusions
In summary, the present systematic review demonstrated that side effects, cost, and convenience are major factors for patients when selecting a treatment regimen for hypertension. For hypertension treatment decisions, patients often obtain hypertension information from their physicians and prefer shared patient-centered decision-making.
Disclosure
The authors declare that there are no conflicts of interest.
References
- 1.McManus RJ, Little P, Stuart B, et al. Home and online management and evaluation of blood pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial. BMJ. 2021;372. doi: 10.1136/bmj.m4858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qamar A, Braunwald E. Treatment of hypertension: addressing a global health problem. JAMA. 2018;320(17):1751–1752. doi: 10.1001/jama.2018.16579 [DOI] [PubMed] [Google Scholar]
- 3.Brunström M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36. doi: 10.1001/jamainternmed.2017.6015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mancia G, Rea F, Corrao G, Grassi G. Two-drug combinations as first-step antihypertensive treatment. Circ Res. 2019;124(7):1113–1123. doi: 10.1161/CIRCRESAHA.118.313294 [DOI] [PubMed] [Google Scholar]
- 5.Musinguzi G, Anthierens S, Nuwaha F, Van Geertruyden JP, Wanyenze RK, Bastiaens H. Factors influencing compliance and health seeking behaviour for hypertension in Mukono and Buikwe in Uganda: a qualitative study. Int J Hypertens. 2018;2018:8307591. doi: 10.1155/2018/8307591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams B, Mancia G, Spiering W, et al. 2018 practice guidelines for the management of arterial hypertension of the European society of cardiology and the European society of hypertension ESC/ESH task force for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 7.Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2017;2018(71):e127–e248. [DOI] [PubMed] [Google Scholar]
- 8.Brouwers S, Sudano I, Kokubo Y, Sulaica EM. Arterial hypertension. Lancet. 2021;398(10296):249–261. doi: 10.1016/S0140-6736(21)00221-X [DOI] [PubMed] [Google Scholar]
- 9.Swift JK, Mullins RH, Penix EA, Roth KL, Trusty WT. The importance of listening to patient preferences when making mental health care decisions. World Psychiatry. 2021;20(3):316–317. doi: 10.1002/wps.20912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montori VM, Brito JP, Murad MH. The optimal practice of evidence-based medicine: incorporating patient preferences in practice guidelines. JAMA. 2013;310(23):2503–2504. doi: 10.1001/jama.2013.281422 [DOI] [PubMed] [Google Scholar]
- 11.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-2 [DOI] [PubMed] [Google Scholar]
- 12.Howren MB, Vander Weg MW, Christensen AJ, Kaboli PJ. Association of patient preferences on medication discussion in hypertension: results from a randomized clinical trial. Soc Sci Med. 2020;262:113244. doi: 10.1016/j.socscimed.2020.113244 [DOI] [PubMed] [Google Scholar]
- 13.Ogedegbe G, Mancuso CA, Allegrante JP. Expectations of blood pressure management in hypertensive African-American patients: a qualitative study. J Natl Med Assoc. 2004;96(4):442–449. [PMC free article] [PubMed] [Google Scholar]
- 14.Morecroft C, Cantrill J, Tully MP. Individual patient’s preferences for hypertension management: a Q-methodological approach. Patient Educ Couns. 2006;61(3):354–362. doi: 10.1016/j.pec.2005.04.011 [DOI] [PubMed] [Google Scholar]
- 15.Lisper L, Isacson D, Sjödén PO, Bingefors K. Medicated hypertensive patients views and experience of information and communication concerning antihypertensive drugs. Patient Educ Couns. 1997;32(3):147–155. doi: 10.1016/s0738-3991(97)00033-5 [DOI] [PubMed] [Google Scholar]
- 16.Schoenthaler A, Rosenthal DM, Butler M, Jacobowitz L. Medication adherence improvement similar for shared decision-making preference or longer patient-provider relationship. J Am Board Fam Med. 2018;31(5):752–760. doi: 10.3122/jabfm.2018.05.180009 [DOI] [PubMed] [Google Scholar]
- 17.Metcalfe RK, Harrison M, Hutfield A, et al. Patient preferences and decisional needs when choosing a treatment approach for pregnancy hypertension: a stated preference study. Can J Cardiol. 2020;36(5):775–779. doi: 10.1016/j.cjca.2020.02.090 [DOI] [PubMed] [Google Scholar]
- 18.Bulgin D, Biola HR, Whitney CA, et al. Patient expectations and preferences for community-based hypertension classes with implications for action. Worldviews Evid Based Nurs. 2022;19(1):42–46. doi: 10.1111/wvn.12550 [DOI] [PubMed] [Google Scholar]
- 19.Mah HC, Muthupalaniappen L, Chong WW. Perceived involvement and preferences in shared decision-making among patients with hypertension. Fam Pract. 2016;33(3):296–301. doi: 10.1093/fampra/cmw012 [DOI] [PubMed] [Google Scholar]
- 20.Halifax NV, Cafazzo JA, Irvine MJ, et al. Telemanagement of hypertension: a qualitative assessment of patient and physician preferences. Can J Cardiol. 2007;23(7):591–594. doi: 10.1016/s0828-282x(07)70807-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kario K, Kagitani H, Hayashi S, Hanamura S, Ozawa K, Kanegae H. A Japan nationwide web-based survey of patient preference for renal denervation for hypertension treatment. Hypertens Res. 2022;45(2):232–240. doi: 10.1038/s41440-021-00760-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schmieder RE, Högerl K, Jung S, Bramlage P, Veelken R, Ott C. Patient preference for therapies in hypertension: a cross-sectional survey of German patients. Clin Res Cardiol. 2019;108(12):1331–1342. doi: 10.1007/s00392-019-01468-0 [DOI] [PubMed] [Google Scholar]
- 23.McAlister FA, O’Connor AM, Wells G, Grover SA, Laupacis A. When should hypertension be treated? The different perspectives of Canadian family physicians and patients. CMAJ. 2000;163(4):403–408. [PMC free article] [PubMed] [Google Scholar]
- 24.Montgomery AA, Harding J, Fahey T. Shared decision making in hypertension: the impact of patient preferences on treatment choice. Fam Pract. 2001;18(3):309–313. doi: 10.1093/fampra/18.3.309 [DOI] [PubMed] [Google Scholar]
- 25.Rahman AR, Wang JG, Kwong GM, et al. Perception of hypertension management by patients and doctors in Asia: potential to improve blood pressure control. Asia Pac Fam Med. 2015;14(1):2. doi: 10.1186/s12930-015-0018-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nasothimiou EG, Karpettas N, Dafni MG, Stergiou GS. Patients’ preference for ambulatory versus home blood pressure monitoring. J Hum Hypertens. 2014;28(4):224–229. doi: 10.1038/jhh.2013.104 [DOI] [PubMed] [Google Scholar]
- 27.Konlan KD, Armah-Mensah M, Aryee R, Appiah TA. Expectation and satisfaction with nursing care among hypertensives receiving care at a resource-constrained hospital in Ghana. Nurs Res Pract. 2020;2020:6094712. doi: 10.1155/2020/6094712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gebrezgi MT, Trepka MJ, Kidane EA. Barriers to and facilitators of hypertension management in Asmara, Eritrea: patients’ perspectives. J Health Popul Nutr. 2017;36(1):11. doi: 10.1186/s41043-017-0090-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fletcher B, Hinton L, McManus R, Rivero-Arias O. Patient preferences for management of high blood pressure in the UK: a discrete choice experiment. Br J Gen Pract. 2019;69(686):e629–e637. doi: 10.3399/bjgp19X705101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cremers AL, Alege A, Nelissen HE, et al. Patients’ and healthcare providers’ perceptions and practices regarding hypertension, pharmacy-based care, and mHealth in Lagos, Nigeria: a mixed methods study. J Hypertens. 2019;37(2):389–397. doi: 10.1097/HJH.0000000000001877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flynn SJ, Ameling JM, Hill-Briggs F, et al. Facilitators and barriers to hypertension self-management in urban African Americans: perspectives of patients and family members. Patient Prefer Adherence. 2013;7:741–749. doi: 10.2147/PPA.S46517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gibson DS, Nathan AG, Quinn MT, Laiteerapong N. Patient expectations of hypertension and diabetes medication: excessive focus on short-term benefits. SAGE Open Med. 2018;6:2050312118821119. doi: 10.1177/2050312118821119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fairchild PC, Nathan AG, Quinn M, Huang ES, Laiteerapong N. Patients’ future expectations for diabetes and hypertension treatments: ”Through the Diet… I Think This is Going to Go Away”. J Gen Intern Med. 2017;32(1):49–55. doi: 10.1007/s11606-016-3871-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anthony H, Valinsky L, Inbar Z, Gabriel C, Varda S. Perceptions of hypertension treatment among patients with and without diabetes. BMC Fam Pract. 2012;13:24. doi: 10.1186/1471-2296-13-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nishigaki N, Shimasaki Y, Yoshida T, Hasebe N. Physician and patient perspectives on hypertension management and factors associated with lifestyle modifications in Japan: results from an online survey. Hypertens Res. 2020;43(5):450–462. doi: 10.1038/s41440-020-0398-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Herzog TJ, Armstrong DK, Brady MF, et al. Ovarian cancer clinical trial endpoints: society of gynecologic oncology white paper. Gynecol Oncol. 2014;132(1):8–17. doi: 10.1016/j.ygyno.2013.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burnier M, Egan BM. Adherence in hypertension. Circ Res. 2019;124(7):1124–1140. doi: 10.1161/CIRCRESAHA.118.313220 [DOI] [PubMed] [Google Scholar]
- 38.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367. doi: 10.1007/s11606-012-2077-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murray E, Pollack L, White M, Lo B. Clinical decision-making: patients’ preferences and experiences. Patient Educ Couns. 2007;65(2):189–196. doi: 10.1016/j.pec.2006.07.007 [DOI] [PubMed] [Google Scholar]
- 40.Bhatt DL, Kandzari DE, O’Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370(15):1393–1401. doi: 10.1056/NEJMoa1402670 [DOI] [PubMed] [Google Scholar]
- 41.Esler MD, Krum H; Symplicity HTN-2 Investigators. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010;376(9756):1903–1909. doi: 10.1016/S0140-6736(10)62039-9 [DOI] [PubMed] [Google Scholar]
- 42.Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009;373(9671):1275–1281. doi: 10.1016/S0140-6736(09)60566-3 [DOI] [PubMed] [Google Scholar]