Abstract
In this article, we argue for a change in how professionals in speech-language pathology think and talk about dialect diversity in the US and elsewhere. Our recommendation is evidence-based and reflects a change we have made to better serve children and advocate for the field of communication disorders. The change involves replacing the phrase dialect vs. disorder with disorder within dialect. While this change in wording may seem superficial, it generates dramatically different types of conversations a professional can have with others about childhood language impairment across different dialects of English.
Clinician 1: Teachers at my school refer children to me all the time, and I send the children back because they speak a nonmainstream dialect of English. Clinician 2: That happens to me too. Dialects are not disorders but teachers don’t always understand this.
Clinician 3: I just went to a talk about some of the dialects our children are using in our schools. Clinician 4: That’s great. You can help us decide who is speaking a dialect and who is presenting a language disorder. Clinician 3: Yes – the dialect vs. disorder conundrum – if the child’s language reflects a dialect difference, we don’t want to misdiagnosis the child’s language as disordered.
The above conversations are typical of many we have heard at various conferences, work settings, and social gatherings, and the content within them should not be surprising. The dialect vs. disorder phrase was introduced to the field in the 1980s (ASHA, 1983), and it has been further endorsed through presentations of linguistic contrast analysis as a method to determine whether a child’s language productions should be classified as dialectal differences or as errors (McGregor, Williams, Hearst, & Johnson, 1997; Seymour, Bland-Stewart, & Green, 1998). As a professional meme, the dialect vs. disorder phrase has helped unify the thoughts and discussions of generations of speech-language pathologists. However, over the past few decades, we have learned a great deal about the ways a childhood language impairment1 manifests within the contexts of different dialects. Recently, we have also learned that children from minority backgrounds (African American and Hispanic), some of whom may speak a nonmainstream dialect of English, are less likely to receive services by a speech-language pathologist than otherwise similar White children (Morgan et al., 2015; 2016). In this article, we recommend changing our field’s meme to more accurately reflect the scientific evidence and better meet the needs of children with language impairments. By making this change, clinicians will also find themselves better able to advocate for their services and the field of speech-language pathology.
Change Dialect vs. Disorder to Disorder within Dialect
Dialects of a language do not reflect a language disorder. This statement remains as true today as it was in the 1970s and 1980s. Our interest in changing the dialect vs. disorder phrase does not relate to this truth statement. Instead, a change is needed because: 1) the preposition versus within the phrase suggests that dialects and disorders are conceptually equivalent, which is inaccurate, and 2) the placement of dialect first within the phrase leads to conversations about dialects rather than conversations about the nature, identification, and treatment of childhood language impairment.
Consider first the preposition versus, which serves to express opposition between conceptually equivalent terms such as boys vs. girls and children vs. adults. For any equivalent X vs. Y proposition, the two boxes in Figure 1 work well -- items or concepts reflecting X can be placed in the first box and items or concepts reflecting Y can be placed in the second. As illustrated by the labels within the boxes, the dialect vs. disorder phrase characterizes the clinician’s task as determining which box is most relevant for any given child.
Figure 1.
Dialect vs. Disorder
Now think about the terms, dialects and disorders. Unlike boys and girls, children and adults, or any other equivalent pair of X and Y terms, dialects and disorders are not conceptually equivalent. Dialects are spoken by sizeable groups of speakers, and many members of the same school or community can be speakers of same dialect. In contrast, language disorders are present in only a small percentage of speakers within the same school or community. In a large epidemiology study of kindergarteners, Tomblin et al. (1997) calculated the prevalence of childhood language impairment at 7.4%. Within rural Louisiana kindergartens, where we have extensively studied the African American English (AAE) and Southern White English (SWE) dialects spoken in the schools, we have also found rates of childhood language impairment to be low (e.g., children classified as language impaired represented 8% of those who returned signed consent forms in Oetting, McDonald, Seidel, & Hegarty, 2015). These prevalence rates for childhood language impairment are far lower than the near 100% prevalence of nonmainstream English speakers we have identified within the same schools. Given this and as shown in Figure 2, we have re-sized the dialect and disorder boxes to better represent important differences between the prevalence at which dialects are spoken by children and the prevalence of childhood language impairment.
Figure 2.
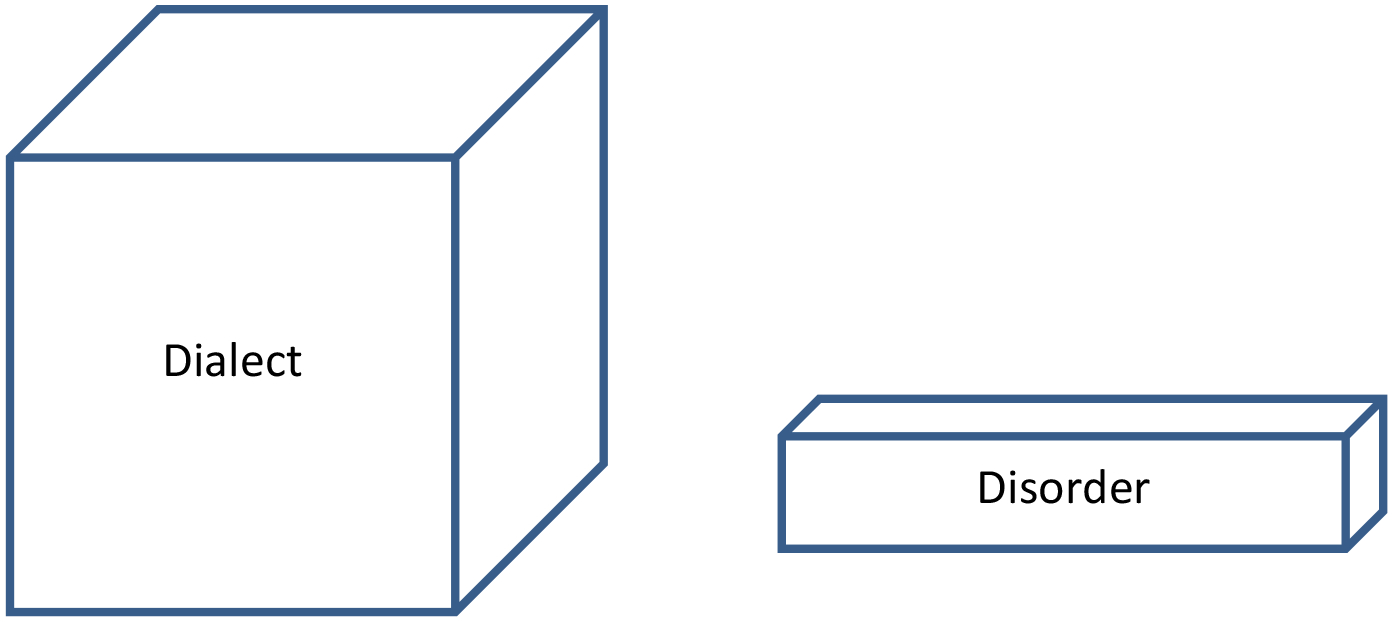
Dialect and Disorder
The re-sized boxes in Figure 2 are also useful for representing differences in the ease at which dialects and disorders can be identified. Typical dialect variation among speakers is extremely easy to detect. Studies supporting this statement have included listeners who were well-trained researchers familiar with the dialects being evaluated (Cottrell & Taran, 2011; Garrity & Oetting, 2010; Oetting & McDonald, 2002; Oetting et al., 2015; Pruitt & Oetting, 2009), untrained speech-language clinicians with minimal exposure to the dialects being evaluated (Robinson & Stockman, 2009), untrained landlords solicited from the general public and untrained college students (Purnell, Idsardi, & Baugh, 1999), and even untrained, young adults who presented with high-functioning Autism (Clopper, Rohrbeck, & Wagner, 2012). Anecdotally, we also know that very young children are able to detect dialects that differ from their own fairly easily. It is not uncommon to hear queries such as Where you from? and You from X? (with X usually referring to a local community some distance from the child’s school) when our dialect(s) do not match those of the pre-kindergarteners and kindergarteners we are testing.
In contrast, childhood language disorders are extremely difficult to identify. Within Tomblin et al.’s (1997) epidemiology study, less than 30% of the kindergarteners classified as language impaired presented with a history of parental or teacher concern. This finding is similar to the 25% of children Oetting et al. (2015) classified as language impaired who were also receiving services by a speech-language pathologist in the schools. While unfortunate, this finding may be expected. Teachers have been shown to refer children to special education services more often for behavioral reasons than for academic reasons (Gottlieb, Gottlieb, & Trongone, 1991), and speech and language screenings conducted by pediatricians, nurses, and other uncertified professionals have yet to be deemed accurate and effective (Voiǵt & Accardo, 2015; Wallace et al., 2015). As members of a relatively small profession among others in education and medicine, speech-language pathologists are uniquely trained to identify children with language impairments, and our training requires an advance degree from an accredited graduate program, numerous hours of supervised clinical hours, and a supervised clinical fellowship, post degree.
Yet the boxes in Figure 2 still do not fully capture the relationship between the terms dialect and disorder for the speech-language pathologist, because it is not possible to discuss a child’s language disorder without reference to his or her dialect. Anyone who speaks a language speaks a dialect of that language. For this reason and as shown in Figure 3, we have replaced the two-box model with a single box that recognizes all children as speakers of some type of dialect, and the smaller box is placed within the larger one to represent those few children who present with a language disorder within the context of their dialect(s). Note that the preposition within rather than vs. or and is ideally suited to describe the single box model. Unlike the dialect vs. disorder phrase, disorder within dialect characterizes the speech-language pathologist’s task as one of identifying those children who present linguistic weaknesses within the context of any given dialect.
Figure 3.
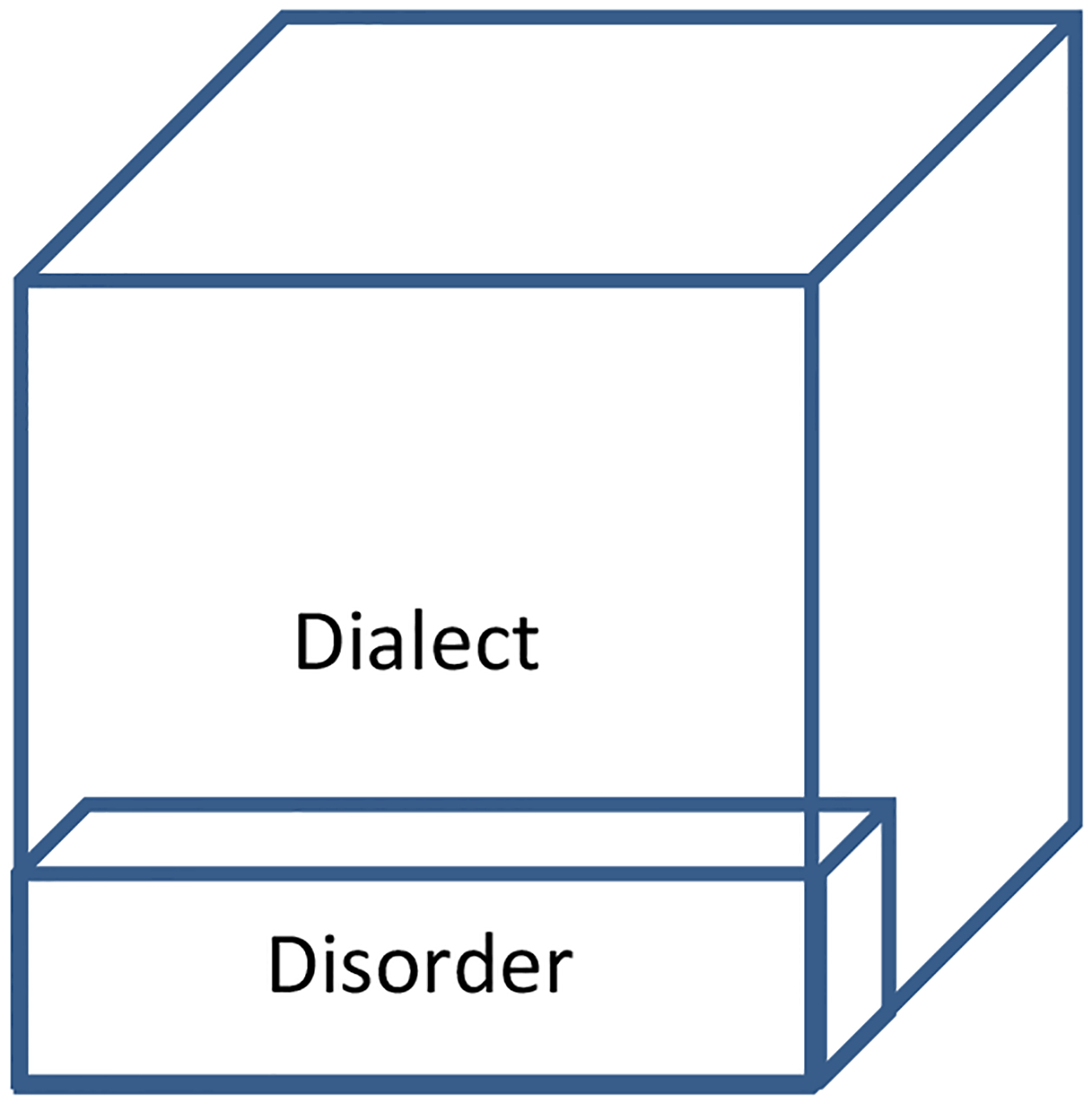
Disorder within Dialect
Now consider the order in which we talk about dialects and disorders. Dialects are fascinating, as is evident by the many documentaries produced about them and the many cartoons and social media posts that celebrate the different ways humans speak. In fact, it is easy to engage just about anyone into a conversation about the prestige and stigmatization of different dialects within the US and elsewhere. It is also easy to engage others into discussions about different local dialects within their communities. While there is nothing wrong with these conversations, notice the lack of content within them that is related to the nature, identification, and treatment of childhood language impairment. Revisit the hypothetical conversations offered at the beginning of this article – they too lack content related to childhood language impairment.
Disorder within dialect as a phrase places the speech-language pathologist’s area of expertise at the forefront of the conversation. Conversations about the nature and prevalence of childhood language disorders across dialects are naturally generated by the wording change as are opportunities for the speech-language pathologist to talk about a host of professional topics. Among others, these topics include positive family history as an important risk factor for childhood language impairment across dialects; active involvement of the speech-language pathologists in universal language screenings across dialects; and the use of diagnostic accuracy indices when selecting dialect-appropriate tests and measures. In the space remaining, we present examples of information about these topics that the disorder within dialect phrase has helped us think about and highlight when talking to families, teachers, and others about the services speech-language pathologists provide to children in pre-kindergarten and kindergarten. We present these topics broadly, recognizing that speech-language pathologists are likely working with children, families, and teachers in a variety of ways and as part of, or in concert with different models of response-to-intervention (RTI) or multitier systems of supports (MTSS; see Joint Report of DEC-CEC, NAEYC, & NHSA, 2013; Ehren & Nelson, 2005; Reschly, 2014).
Positive family history as an important risk factor for childhood language impairment.
Delayed acquisition of early language developmental milestones and a positive family history of oral and/or written language impairment are documented risk factors for childhood language impairment in both monolingual and bilingual samples (Grimm & Schulz, 2014). Of these, the predictive value of a positive family history of impairment is probably the least likely to be utilized in clinical practice. In a review of 14 studies, Leonard notes the repeated finding of a higher-than-expected familial concentration of speech and language impairments in samples of children with language impairment. Across studies, the percentage of family members with a positive history of impairment among children with impairments ranged from 20% to 63%. For those studies with typically developing controls, percentages of family members with a positive history of speech and language impairment were much lower, ranging from 3% to 19%.
Pruitt, Garrity, and Oetting (2010) and Oetting et al. (2015) also found higher-than expected concentrations of familial speech and language impairment in children who spoke either AAE or SWE. In the former, the data were from 161 African American children who attended daycares, pre-kindergartens, or kindergartens known to enroll high numbers of AAE speakers. In this study, the children classified as language impaired were two times more likely to present a positive family history of impairment than those with typical development (50% vs. 21%). In the latter, the data were from 70 kindergarteners who spoke AAE and 36 who spoke SWE. In this study, 45% of those classified as impaired presented a positive family history of speech and language impairment compared to 15% of those classified as typically developing. As indicated by these findings, not all children with a language impairment present with a positive family history of impairment, and not all children with a positive family history present with a language impairment. Nevertheless, we consider the evidence from the family history studies sufficient to warrant the collection and consideration of this information across dialects as part of our screenings and comprehensive language evaluations.
For screenings, family history information can be collected ahead of time through an easy-to-read document that informs caregivers about the nature and goals of the screening, asks about their concerns for their child, and requests information about others in their child’s family who presented with difficulties in speech, language, reading, writing, or hearing. For comprehensive language evaluations, information about a family’s history can then be more thoroughly discussed so that this information can be considered along with direct measures when making decisions about a child’s language impairment status. Following Lewis and Freebairn (1993), when we inquire about family history information within an evaluation, we first ask families to list all of the child’s immediate and extended blood-related family members. Then for each family member listed, we ask about his or her history of speech and language difficulties, reading and writing difficulties, spelling difficulties, learning disabilities, stuttering, and hearing loss.
Universal language screenings in preschool and kindergarten.
Language screenings typically take less than 30 minutes and are often designed to determine if broad, criterion-based developmental milestones have been attained by a child (Pindzola, Plexico, & Haynes, 2016). In traditional models of service delivery, screenings also identify children for whom a comprehensive language evaluation is required to rule in or rule out a diagnosis of language impairment. In RTI or MTSS models of service delivery, screenings identify children for whom positive supports and progress monitoring can be offered as part of the regular education curriculum at Tier 1 or as part of a more intensive level of service at Tier II. In each of these cases, screenings should include the speech-language pathologist and over-identify rather than under-identify children with language impairments. Findings from Tomblin et al.’s (1997) study support this claim. In their school-wide screening of 7,218 kindergarteners, 26.2% of the children failed the initial screening. This fail rate was over three times that of the 7.4% of children eventually classified as language impaired.
Although Tomblin et al., (1997) did not report screening fail rates by the children’s dialects, two dissertations in our lab have evaluated different screeners for AAE- and SWE-speaking children. Moland (2013) examined the validity of the Diagnostic Evaluation of Language Variation-Screener (Seymour, Roeper, & de Villiers, 2003), the Fluharty Preschool Speech and Language Screening Test - 2 (Fluharty, 2001), and an experimental language screener by Washington and Craig (2004). The data came from 73 AAE-speaking children, aged four to five years, who attended public pre-kindergartens or Head Starts. All three screeners were given to each child, and the order of administration was counter-balanced so that practice effects could be evaluated. Results showed that the three screeners did not differ in their fail rates. Fail rates also did not differ by the children’s gender, caregiver education, or use of nonmainstream AAE forms. After the first screener, fail rates ranged from 46% to 57%, and these fail rates were deemed too high to be valid or clinically feasible. However, during the second session and when the third screener was administered, fail rates decreased to a more manageable 33%.
Using data from 77 kindergartners, Gregory (2015) evaluated the validity of five different screeners. The data came from 26 children classified as language impaired (with some also presenting low nonverbal IQ scores) and 51 classified as developing language typically; 35 were speakers of AAE and 42 were speakers of SWE. The screeners included two teacher questionnaires, the Children’s Communication Checklist-2 (Bishop, 2006) and the Teacher Rating of Oral Language and Literacy (Dickinson, McCabe, & Sprague, 2001), and three other screeners, the Diagnostic Evaluation of Language Variation-Screener (Seymour et al., 2003), the Peabody Picture Vocabulary Test-IV (Dunn & Dunn, 2007), and the Dynamic Indicators of Basic Early Literacy Skills Next (Good, Gruba, & Kaminski, 2009). Results indicated that scores from all five screeners differed by the children’s clinical status (impaired < typical developing); however, all five under-identified the children with language impairments when cut scores taken from the screeners’ manuals were employed. Using those cut scores, the sensitivity of the screeners ranged from .12 to .62. In other words, only 12% to 62% of the children classified as impaired failed one or more of the screeners.
Fortunately, the accuracy of the screeners improved through the use of empirically-derived cut scores and step-wise discriminate function analysis. Empirically-derived cut scores maximize the number of children correctly classified as impaired or typical within a sample, and step-wise discriminant function analysis allows scores from the best screener(s) to be combined to further maximize the number of children correctly classified. When these methods were employed, the Peabody Picture Vocabulary Test-IV by itself with a standard score of 89 as the cut score was 95% accurate in classifying the clinical status of the children, and this same screening outcome was obtained by using a cut score of 92 on the Teacher Rating of Oral Language and Literacy and a standard score of 89 on the Peabody Picture Vocabulary Test-IV. The results of this study (and the established cut scores) need to be tested with a larger, independent sample, but if they replicate, they suggest a two-step approach to screening in kindergarten, with the first step involving a teacher questionnaire and the second step involving direct testing of only those children who scored lower than desired on the teacher questionnaire. For clinicians working within a RTI or MTSS model of service delivery, we recommend the use of both a teacher questionnaire and direct testing to maximize the number of children identified for positive supports and progress monitoring. To support this recommendation, note that the 95% accuracy rate for the teacher questionnaire and Peabody Picture Vocabulary Test-IV did not over-identify the children with language impairments. Instead, the 95% accuracy rate corresponded to 88% of the children with impairment correctly identified as impaired and 98% of the typically developing children correctly identified as typical.
Findings from the Moland (2013) and Gregory (2015) studies are consistent with those of Washington and Craig (2004) who also found screening fail rates of nonmainstream English-speaking children to be higher in pre-kindergarten than in kindergarten. Importantly, though, in both the Moland and Gregory studies and the Washington and Craig study, results were dependent upon the speech-language pathologist’s use of more than one screening instrument. Given this, when we talk with families, teachers, and other professionals about screening services for children in pre-kindergarten and kindergarten, we advocate for not only active involvement of the speech-language pathologist, but also for the use of more than one type of screener. Based on Tomblin’s et al.’s (1997) findings, we also state that the goal for screening to over-identify and refer those screened for a comprehensive language evaluation, with the expectation that a formal diagnosis of impairment will be ruled out for most of these children. For clinicians working within a RTI or MTSS framework, we recommend the ~30% fail rate at Tier I for supports and monitoring within the regular classroom, with the expectation that this percent of children with needs will dramatically decrease as part of Tier II and Tier III services.
Using diagnostic accuracy indices to select dialect-appropriate tests and measures.
Regardless of whether clinicians are working within a traditional service delivery system or within an RTI or MTSS system, they will complete comprehensive language evaluations for some children. When this occurs, dialect-appropriate testing methods are necessary. Cultural and linguistic biases within comprehensive language tests are well-recognized concerns within the field, and many commercially available tests recommend scoring modifications for different dialects of English. This practice is consistent with a dialect vs. disorder approach to assessment, because scoring modifications make it less likely to classify a child’s nonmainstream dialect responses as errors. However, with a disorder within dialect approach, scoring modifications are appropriate only if the test with the modified scoring accurately identifies children with language impairments across dialects. If test developers have not established the diagnostic accuracy of the test with the scoring modifications, we recommend against this practice.
Scoring nonmainstream dialectal responses produced by a child as correct reduces the number of items available on the test to identify children with language impairments. Scoring these items as correct for all speakers of a particular dialect also makes it impossible to document rate-based differences between children with and without language impairments on these items. Untested modified scoring systems are particularly problematic for tests of grammar because children with language impairments across dialects (and across languages) typically do not differ from their typically developing, same dialect-speaking peers in the nature of their grammatical productions. Instead, across dialects and languages, children with and without language impairments differ in the frequency and/or rate at which they produce particular types of grammatical structures -- and these grammatical structures include some that also vary across dialects.
Craig and Washington (2000) documented this finding in a study of 72 AAE-speaking children, aged four to 11 years. Their study included some grammatical structures (e.g., conjunctions, such as and, but, so) that do not vary across dialects but also some that do (e.g., relative clause markers, such as the truck that …, and infinitival TO, such as …need to stand). For the structures combined, the AAE-speaking children with language impairments produced lower rates of overt marking than did their typically developing, same dialect-speaking peers. We have replicated this finding for relative clause markers and infinitival TO structures in other groups of nonmainstream dialect speakers (Oetting & Newkirk, 2008; Rivière, 2016). In a series of studies, we have also identified other grammatical structures that both vary across dialects and lead to rate-based differences between same dialect-speaking children with and without language impairments (Oetting, Lee, & Porter, 2013). Tests targeting grammar are unable to capture these types of frequency-based differences between children with and without language impairments when clinicians score children’s dialectal productions targeting these grammar structures as correct.
As an alternative to untested modified scoring systems, we recommend language tests with high levels of diagnostic accuracy across dialects. Currently, the Diagnostic Evaluation of Language Variation-Norm Referenced (Seymour, Roeper, & de Villiers, 2005) is the only standardized tool that meets this criterion. This test is normed for children, aged four to nine years, and its diagnostic accuracy, as measured by sensitivity and specificity indices, is reported by the test developers to be above .90 when – 1 standard deviation below the mean is used as the cut off for impairment. Sensitivity reflects the percentage of children classified as language impaired who are identified on the test as impaired, and specificity reflects the percentage of children classified as typical who are identified as typical. Sensitivity and specificity values at or above .90 are considered ideal, and values at or above .80 are considered fair (Mant, 1999).
When dialect-appropriate tests and measures are not available, we recommend existing tests and tasks with scoring modifications when the modifications yield high levels of diagnostic accuracy across dialects. To offer an example, Oetting et al. (2015) administered a 36-item sentence recall task to 106 AAE- or SWE-speaking children. Half of the children were language impaired, and the others were typically developing controls. Rather than crediting all nonmainstream dialect responses as correct, we strategically credited only those nonmainstream responses not found to differentiate children with and without language impairments across dialects. These included was for were productions (Bert and Ernie was…), is for are productions (Bert and Ernie is…) and zero marking of verbal –s (Big Bird wonderØ when…). We also scored the children’s responses using an elaborate two-point system and two simpler systems involving +/− scoring for each response. Using dialect-strategic coding, all three scoring systems led to statistical differences between the children with and without language impairments. However, dialect-strategic coding along with the simplest +/− scoring system led to the highest level of diagnostic accuracy. For the AAE-speaking children, this system yielded sensitivity and specificity values of .89 and .87, respectively. For the SWE-speaking children, sensitivity and specificity values were .94 and .83, respectively. These results not only support the use of the sentence recall task for AAE- and SWE-speaking children, but they also illustrate the importance of using diagnostic accuracy indices when deciding if a test or task should be used to identify childhood language impairment within the context any given dialect.
Changing Conversations and Clinical Practice
As we hope we have persuasively argued, adopting disorder within dialect as a phrase and professional meme can change how speech-language pathologists think and talk about dialect variation in the US and elsewhere. Identifying and treating children with speech and language impairments remains a primary goal of the speech-language pathologist regardless of a child’s dialect status and regardless of whether a school implements a traditional model of service delivery or one of the many models of RTI or MTSS. As a final illustration of the benefits of the wording change, compare the conversations at the beginning of the article to those below, which we have reframed using a disorder within dialect approach to professional practice and advocacy.
Clinician 1: Teachers at my school refer children to me all the time, and I send the children back because they speak a nonmainstream dialect. Clinician 2: Are we collecting family history information as part of our screenings and screening children within the context of their dialects? Nationally, universal language screening fail rates in kindergarten should be around 30%, with the prevalence of childhood language impairments lower, around 7–15%. What is the screening fail rate and prevalence of childhood language impairment in our schools?
Clinician 3: I just went to a talk about some of the dialects our children are using in our schools. Clinician 4: That’s great. What did you learn about screening and the identification of childhood language impairment within the context of these dialects? Do we use screeners, tests, and measures at our schools that have levels of accuracy above .80 across dialects?
Acknowledgements
Appreciation is extended to Jessica Berry, Ryan James, Christy Seidel, and Tina Villa for discussions about dialect variation and the services we provide to children whose dialects are socially stigmatized.
Financial Disclosures
The writing of this article was made possible with funding to Janna B. Oetting from NIDCD RO1DC009811.
Non-Financial Disclosures
Janna Oetting, Kyomi Gregory, and Andrew Rivière have no nonfinancial interests related to the content of this article.
Continuing Education Questions
Answers: c,a,b,d,c
- The dialect vs. disorders phrase was introduced to the field of speech-language pathology in the
- 1950s.
- 1960s.
- 1980s.
- 1990s.
- The number of people who speak a dialect(s) within a school or community is typically
- higher than the number who present a childhood language impairment.
- lower than the number who present a childhood language impairment.
- the same as the number who present a childhood language impairment.
- in flux depending upon the time of day the children are tested.
- Dialectal differences are
- more difficult to detect than identifying children with language impairments.
- easier to detect than identifying children with language impairments.
- detectable only after a person undergoes extensive training.
- Detectable after a brief training session.
- Disorder within dialect as a phrase leads to conversations about
- dialect differences among speakers.
- the social value and stigmatization of different dialects.
- the importance of dialect shifting for later reading and writing achievement.
- the nature, identification, and treatment of childhood language disorders within the context of any given dialect.
- Modified scoring systems of tests for speakers of particular dialects
- are always recommended.
- are never recommended.
- are recommended when they lead to high levels of diagnostic accuracy across dialects.
- increase the number of items on the test that can be used to identify children with language impairments.
Learner Outcome
After reading this article, the participant will be able to describe: a role of the speech-language pathologist as identifying and serving children with language impairments within the context of any given dialect, the importance of a positive family history as a risk factor for language impairment across dialects, the importance of active involvement of the speech-language pathologist and the use of multiple screeners in universal pre-kindergarten and kindergarten screenings, and the importance of using diagnostic accuracy indices when selecting dialect-appropriate tests and measures.
Footnotes
This manuscript was accepted for publication in 2016. The link to the published study is as follows: https://pubs.asha.org/doi/10.1044/persp1.SIG16.28
We use the term language impairment to refer to children typically classified by researchers as specifically language impaired. These children may be the most difficult to identify in schools because they do not have other developmental conditions such as Autism or Down syndrome. For a discussion about childhood language impairment labels, see volume 14 of the International Journal of Communication Disorders, 2014.
References
- American Speech-Language-Hearing Association. (1983). Social dialects [position statement].
- Bishop DVM (2006), Children’s Communication Checklist-2, San Antonio, TX: Pearson. [Google Scholar]
- Clopper CG, Rohrbeck KL, & Wagner L (2012). Perception of dialect variation by young adults with high-functioning Autism. Journal of Autism and Developmental Disorders, 42, 740–754. [DOI] [PubMed] [Google Scholar]
- Cottrell S, & Taran V (2011). A validation study of listener judgments of AAE. Paper presented at the annual convention of the American Speech-Language-Hearing Association. San Diego, CA. [Google Scholar]
- Dickinson D, McCabe A, & Sprague K (2001). Teacher rating of oral language and literacy: A research-based tool. Ann Arbor, MI: Center for the Improvement of Early Reading Achievement, University of Michigan. [Google Scholar]
- Division for Early Childhood of the Council of Exceptional Children, National Association for the Education of Young Children, & National Head Start Association. (2014). Frameworks for response to intervention in early childhood: Description and implications. Communication Disorders Quarterly, 35, 108–119. Retrieved from http://cdq.sagepub.com/content/35/2/108. [Google Scholar]
- Dunn LM, & Dunn DM (2007) Peabody Picture Vocabulary Test, Fourth Edition. Bloomington, MN: PsychCorp. [Google Scholar]
- Ehren BJ, & Nelson NW (2005). The responsiveness to intervention approach and language impairment. Topics in Language Disorders, 25, 120–131. [Google Scholar]
- Fluharty NB (2001). Fluharty Preschool Speech and Language Screening Test (2nd ed.). Austin: Pro-Ed. [Google Scholar]
- Garrity AW, & Oetting JB (2010). Auxiliary BE production by AAE-speaking children with and without specific language impairment. Journal of Speech, Language, and Hearing Research, 53, 1307–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good RH, Gruba J, & Kaminski RA (2009). Dynamic Indicators of Basic Early Literacy Skills Next. Longmont, CO: Cambrium Learning Group. [Google Scholar]
- Gottlieb J, Gottlieb BW, & Trongone S (1991). Parent and teacher referrals for a psychoeducational evaluation. Journal of Special Education, 25, 155–167. [Google Scholar]
- Gregory KD (2015). Evaluation of teacher ratings to improve child language screenings in speech-language pathology. Unpublished dissertation. Louisiana State University. [Google Scholar]
- Grimm A, & Schulz P (2014). Specific language impairment and early second language acquisition: The risk of over- and under-diagnosis. Child Indicators Report, 7, 821–841. [Google Scholar]
- Leonard LB (2014). Children with specific language impairment (2nd ed.). Cambridge, MA: MIT Press. [Google Scholar]
- Lewis BA, & Freebairn L(1993). A clinical tool for evaluating the familial basis of speech and language disorders. American Journal of Speech-Language Pathology, 2, 38–43. [Google Scholar]
- Mant J (1999). Studies assessing diagnostic tests. In Dawes M, Davis P, Gray A, Mant J, Seers K, & Snowball R. Evidence-based practice: A primer for health care professionals (pp. 67–78). New York: Churchill Livingston. [Google Scholar]
- McGregor K, Williams D, Hearst S, & Johnson A (1997). The use of contrastive analysis in distinguishing difference from disorder: A tutorial. American Journal of Speech Language Pathology, 6, 45–56. [Google Scholar]
- Moland CW (2013). Comparison of the Diagnostic Evaluation of Language Variation-Screening Test (DELV-ST) to two other screeners for low-income, African American children. Unpublished dissertation, Louisiana State University. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan PL Farkas G, Hillemeier MM, Mattison R, Maczuga S Li H, & Cook M (2015). Minorities are disproportionately underrepresented in special education: Longitudinal evidence across five disability conditions. Educational Researcher, 44, 278–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan PL, Hammer CS, Farkas G, Hillemeier MM, Maczuga S, Cook M, & Morano S (2016). Who receives speech/language services by 5 years of age in the United States? American Journal of Speech-Language Pathology. Retrieved from http://ajslp.pubs.asha.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oetting JB, Lee R, & Porter KL (2013). Evaluating the grammars of children who speak nonmainstream dialects of English. Topics in Language Disorders, 33, 140–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oetting JB, & McDonald J (2002). Methods for characterizing participants’ nonmainstream dialect use within studies of childhood language impairment. Journal of Speech, Language, and Hearing Research. 45, 505–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oetting JB, McDonald J, Seidel C, & Hegarty M (2015). Sentence recall by children with SLI across two nonmainstream dialects of English. Journal of Speech, Language, and Hearing Research. [Advance online publication]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oetting JB, & Newkirk B (2008). Subject relatives by children with and without SLI across different dialects of English. Clinical Linguistics and Phonetics, 22, 111–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruitt S, Garrity AW, & Oetting JB (2010). Family history of speech and language impairment in African American children: Implications for assessment. Topics in Language Disorders, 30 (2), 154–164. [Google Scholar]
- Pruitt S, & Oetting JB (2009). Past tense marking by African American English-speaking children reared in poverty. Journal of Speech, Language, and Hearing Research, 52, 2–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purnell T, Idsardi W, & Baugh J (1999). Perceptual and phonetic experiments on American English dialects identification. Journal of Language and Social Psychology, 18, 10–30. [Google Scholar]
- Reschly DJ, (2014). Response to intervention and the identification of specific learning disabilities. Topics in Language Disorders, 34, 39–58. [Google Scholar]
- Rivière AM (2016). Va-et-vient, the goin’ and comin’ of infinitival ‘TO’: A study of children with and without specific language impairment in Cajun English. Unpublished dissertation, Louisiana State University. [Google Scholar]
- Robinson GC, & Stockman IJ (2009). Cross-dialectal perceptual experiences of speech-language pathologists in predominantly Caucasian-American school districts. Language, Speech, Hearing Services in Schools, 40, 138–149. [DOI] [PubMed] [Google Scholar]
- Seymour H, Bland-Stewart L, & Green L (1998). Difference versus deficit in child African American English. Language, Speech, Hearing Services in Schools, 29, 96–108. [DOI] [PubMed] [Google Scholar]
- Seymour HN, Roeper TW, & de Villiers J (2005). Diagnostic Evaluation of Language Variation-Norm Referenced. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Seymour HN, Roeper TW, & de Villiers J (2003). Diagnostic Evaluation of Language Variation-Screener. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Sun L, & Wallach GP (2014). Language disorders are learning disabilities: Challenges on the divergent and diverse paths to language learning disabilities, Topics in Language Disorders, 34, 25–38. [Google Scholar]
- Tomblin JB, Records NL, Buckwalter P, Zhang X, Smith E, & O’Brien M (1997). Prevalence of specific language impairment in kindergarten children. Journal of Speech, Language, and Hearing Research, 40, 1245–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troia GA, (2005). Response to intervention: Roles for speech-language pathologists in the prevention and identification of learning disabilities. Topics in Language Disorders, 25, 106–119. [Google Scholar]
- Voiǵt RG, & Accardo PJ (2015). Formal speech-language screening not shown to help children. Pediatrics 2015;136;e494; originally published online July 7, 2015. [DOI] [PubMed] [Google Scholar]
- Wallace IF, Berkman ND, Watson LR, Coyne-Beasley T, Wood CT, Cullen K, & Lohr KN (2015). Screening for speech language delay in children 5 years old and younger: A systematic review. Pediatrics, 136; e448; originally published online July 7, 2015. [DOI] [PubMed] [Google Scholar]
- Washington JA, & Craig HK (2004). A language screening protocol for use with young African American children in urban settings. American Journal of Speech-Language Pathology, 13, 329–340. [DOI] [PubMed] [Google Scholar]
- Wolfram W (1979). Speech pathology and dialect differences. Center for Applied Linguistics. Washington, DC. [Google Scholar]


