Abstract
Mental distress in medical learners and its consequent harmful effects on personal and professional functioning, a well-documented concern, draws attention to the need for solutions. The authors review the development of a comprehensive mental health service within a large and complex academic medical education system, created with special attention to offering equitable, accessible, and responsive care to all trainees. From the inception of the service in January 2017, the authors placed particular emphasis on eliminating obstacles to learners’ willingness and ability to access care, including concerns related to cost, session limits, privacy, and flexibility with modality of service delivery. Development of outreach initiatives included psychoeducational programming, consultation services, and cultivation of liaison relationships with faculty and staff. Significant utilization of clinical services occurred in the first year of the program and increased further over the course of 4 academic years (2017–2021); with a 2.2 times increase in trainees served and a 2.4 times increase in visits annually. In the 2020–2021 academic year, 821 medical learners received services (for a total 5,656 visits); 30% of all medical students and 25% of house staff and fellows sought treatment in that year. In 2021, 38% of graduating medical school students and 27% of graduating residents and fellows had used mental health services at some point in their training. Extensive use of services combined with very high patient satisfaction ratings by medical learners within this system demonstrate the perceived value of these services and willingness to pursue mental health care when offered a resource that is cognizant of, and responsive to, their unique needs. The authors reflect on potential factors promoting utilization of services—institutional financial support, outreach efforts, and design of services to increase accessibility and reduce barriers to seeking treatment—and propose future areas for investigation.
Mental health concerns in medical trainees remain a pervasive and significant issue; numerous studies have shown high rates of mental distress in medical students and residents. 1–7 These rates are elevated in comparison with the general population of the United States, 7 and may actually increase over the course of medical training. 8,9 Depressive and burnout symptoms in medical trainees can lead to a range of negative consequences: professional misconduct, increased rates of errors, and reduced empathy. 10–12 Recognition of the importance of this issue, for both medical learners and physicians, has spurred the creation of national calls to action, 13,14 collaborative initiatives, 15 and a national physician suicide awareness day. 16 Limited data exist regarding the delivery of mental health services for medical learners; available reports raise concerns about low utilization rates of services. 4,5,17–21 Barriers to seeking care include stigma surrounding mental health issues, treatment, and fear of repercussions; cost; time constraints; and access. 22–25 While multiple factors may affect the use of mental health services by medical learners, insufficient data have been gathered to indicate the relative importance of such obstacles. Given the wealth of research highlighting the mental health struggles that medical trainees experience, 1–8 the stigma associated with accessing mental health care, and other common barriers to seeking care, 22–25 in January of 2017, we developed a mental health services program at Indiana University School of Medicine (IUSM). After implementing the program, which we designed to minimize barriers to care, we evaluated utilization and learner response to this program over the course of 4 academic years (AYs): July 2017–June 2021.
Development of the IUSM Department of Mental Health Services
The largest medical school in the United States, IUSM is a complex system with a total of 9 campuses and over 3,000 medical trainees (medical and graduate students, residents, and fellows). The majority of trainees are located in Indianapolis (the main campus), but several hundred learners are distributed across 8 other campuses and affiliated graduate medical education (GME) programs. Over the course of several years leading up to 2017, trainees, faculty, staff, and administrators at IUSM reported increased awareness of medical learners’ distress and increased demand for mental health services, which led to a plan to reevaluate, restructure, and expand available mental health resources. Before 2017, the constraint of having a single therapist available limited the capacity for offering services. Additionally, for medical students, some counseling services were available through the university counseling centers; however, the accessibility and cost of these services varied across the IUSM campuses. An anticipated visit by the Liaison Committee on Medical Education (LCME) in April 2017 further highlighted the need to consider the adequacy and equity of mental health resources; the complexity of our system dictated special attention to the delivery of equitable, accessible, and responsive mental health services for all 9 IUSM campuses.
Therefore, in January 2017, IUSM created the new Department of Mental Health Services (DMHS) and hired a psychiatrist as the program director. The primary aims of examination, development, and oversight of the delivery of mental health services statewide, as well as the addition of psychiatric services for IUSM trainees, guided this hire. Unlike the delivery of mental health care in traditional university settings, particular constraints exist in medical training institutions: stigma, reluctance to seek treatment, fear of career repercussions, privacy concerns, and an LCME-mandated firewall (“The health professionals who provide health services, including psychiatric/psychological counseling, to a medical student have no involvement in the academic assessment or promotion of the medical student receiving those services, excluding exceptional circumstances.”). 26 Successful implementation of mental health services required addressing these obstacles.
Design of mental health service delivery
Initially, we focused on the creation of a mental health services team and a structure for the delivery of services designed specifically for medical learners to minimize resistance and remove barriers to treatment. To promote access and use, we enabled the following: no cost for treatment, no session limits, and increased accessibility (i.e., telehealth visits and evening hours). In the spring of 2017, we contracted with a crisis line to provide a safety net where trainees (or others on behalf of a trainee) could reach out 24/7 to speak with a mental health clinician working from customized plans for each of the 9 IUSM campuses. These algorithms guided referrals to campus-specific resources, vetted in advance to minimize the use of medical training sites as referral options. Creating a structure for the clinic included developing a private yet accessible space. This new space (into which we moved in October 2017 after being housed temporarily with Campus Health) included several offices, a waiting area, and a conference room. The suite location, in an administrative building on campus rather than in one of the main buildings housing medical student spaces, limited the likelihood of encounters with leadership or faculty. Maintenance of medical records occurred within an electronic medical record (EMR); initially, we used the campus health EMR, and then shifted in November 2020 to a different EMR designed specifically for university health and counseling centers. Both EMRs remained separate from all clinical training sites and not accessible to IUSM administration or faculty, to allay concerns regarding confidentiality. Further, the trainee’s academic record did not reflect the use of mental health services or accommodations, and DMHS team members did not participate in the supervision or evaluation of medical trainees. Finally, significant financial support from the dean’s office enabled growth of the team and services; allocations from GME and the dean’s office directly funded DMHS with salaried positions and no relative value unit expectations or clinical billing. These allocations increased proportionately over time as staffing scaled up to meet the increased demand. Combined, these design elements sent a message to trainees regarding the importance of this work to the institution. Supplemental Digital Appendix 1, at http://links.lww.com/ACADMED/B296, provides a timeline of the development of the service.
Outreach and programming
Expansion of services developed concomitantly with outreach and programming that centered on engagement with students, faculty, and staff at all 9 campuses and involved travel to regional campuses to facilitate these connections. This programming began in 2017 and by the 2019–2020 AY, staff offered 99 activities comprising 10 orientation sessions, 46 formal presentations or workshops, 30 mind–body medicine sessions co-facilitated by medical student education deans, and 13 additional outreach events (targeted typically toward learners but including faculty and staff). The outreach format ranged from psychoeducational didactics to discussion-based workshops or interactive group sessions, and covered topics such as suicide prevention, stress management, United States Medical Licensing Examination Step exam preparation, burnout, resiliency, mindfulness, and group debriefing in response to societal events.
Liaison work included consultations with faculty and staff on the management of crises as well as discussions of strategies for supporting struggling trainees. Extensive communication about services, the team, and mental health topics occurred through meetings, newsletters, emails, blogs, and social media posts.
Growth of the DMHS
In the first AY of expanded services, provisioned by 2 full-time equivalent (FTE) therapist and .4 FTE clinical psychiatry time, a large number of trainees (n = 376) sought treatment (n = 2,392 visits). Utilization of services quickly increased over the course of 4 AYs (Figure 1), as did the size of the team, which grew to a 10-person team (7 clinicians: 3.7 FTE therapists, 1.0 FTE program manager/therapist, .75 FTE psychiatrist, .8 FTE psychiatrist/director; and 3 administrative staff: 1.0 FTE program coordinator, 1.0 FTE administrative/medical assistant, .5 FTE program assistant) providing 4.2 FTE therapist and 1.0 FTE psychiatrist clinical time. Each subsequent clinical hire correlated temporally with increases in visit and patient numbers; Supplemental Digital Appendix 2, at http://links.lww.com/ACADMED/B296, shows clinical FTE in relation to monthly visit counts (from July 2018 to June 2021). A capacity-adjusted measure of utilization (average monthly visits divided by available FTE per year) remained roughly equivalent: 96.5 (AY18–19), 101.1 (AY19–20), and 98.3 (AY20–21), corroborating the idea that capacity changes may account for a substantial portion of utilization increases.
Figure 1.
DMHS utilization by patient and visit counts, AY2017–AY2021. Numbers of patients seen and numbers of patient visits over 4 successive academic years (July 1, 2017, to June 30, 2021). Abbreviations: DMHS, Department of Mental Health Services; AY, academic year.
As Figure 1 shows, the number of visits per year more than doubled (from 2,392 to 5,656 visits, a 2.4 times increase) as did the number of patients seen (from 376 to 821, a 2.2 times increase) over the course of 4 AYs. Despite the rapid expansion of the team, high clinical demand, at times, required the use of waiting lists.
Pandemic effect
The COVID-19 pandemic overlapped with the latter 16 months of the observation period. Pandemic-associated increased stress may account for some of the increased clinical need and utilization, as others have also observed. 27,28 However, utilization rates increased over the entire observation period; comparisons of monthly patient and visit counts (monthly data available from 2018–2021 in Supplemental Digital Appendices 3 and 4, at http://links.lww.com/ACADMED/B296) show, despite some month-to-month variability, a trend for increased usage in each subsequent AY both before and during the COVID-19 pandemic.
Visit numbers combine in-person and telehealth services. Due to the pandemic, starting in mid-March of 2020, all services shifted to telehealth delivery using a HIPAA-compliant platform. Because of the structure of IUSM’s multi-campus system, before this shift, the team offered both telehealth and in-person services, with telehealth visits making up approximately 16% of total visits between July 1, 2019, and February 29, 2020. Therefore, having Zoom virtual conferencing in place for health care, staff equipment, and training allowed for a smooth transition to 100% telehealth delivery without disruption despite the rapid pivot to remote work. In sessions, clinicians noted reports by learners of distress related to shifts in working and studying from home, disruptions in training combined with the stress of the pandemic, and the consequent impact on the Step exams.
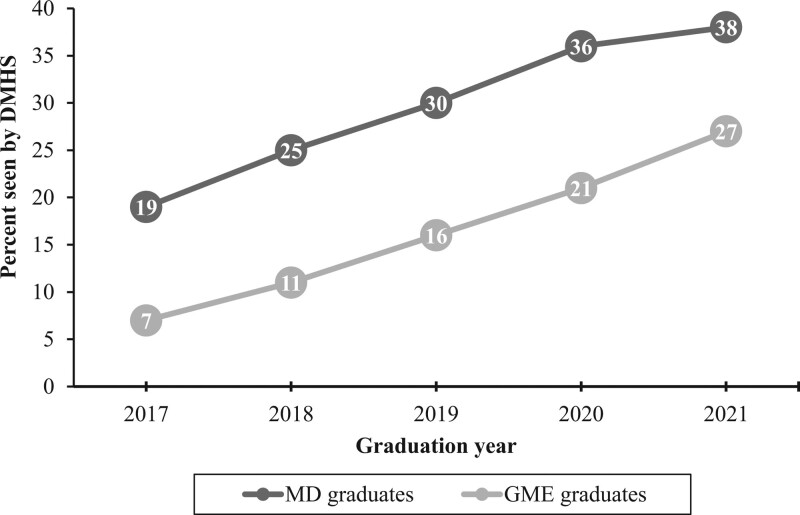
Utilization by graduating cohort
Usage of services by graduating cohorts provides another perspective on willingness to seek mental health services. Over the course of the 4 years (2017–2021), steadily increasing numbers of graduates have sought mental health services through the department during medical school training. In the IUSM Class of 2021, 38% of graduates (131 out of 345) used counseling and/or psychiatric services provided by DMHS at some point in their training. Utilization rates in Figure 2 reveal more medical school graduates seeking services than GME graduates, but still 27% (91/343) of 2021 GME graduates used DMHS services at some point in their training.
Figure 2.
Percentage of IUSM graduates seen by DMHS, by graduating year. Numbers of MD and GME graduates in each of 5 years (2017–2021) who sought treatment by DMHS at any time during their academic career. Abbreviations: IUSM, Indiana University School of Medicine; DMHS, Department of Mental Health Services; MD, medical school; GME, graduate medical education.
AY 2020–2021 utilization of mental health services
A total of 821 patients engaged with DMHS in the 2020–2021 AY; this includes 430 medical students (MD and MD–PhD), 311 GME trainees (residents and fellows), 41 PhD students, 19 master’s-level students, 6 learners in transition (postgraduation), and 14 partners (in couples therapy). Thirty percent (430/1,441) of medical students and 25% (311/1,265) of GME trainees (residents and fellows) used services, including 85 GME trainees who participated in opt-out wellness checks but did not otherwise follow up in this AY. Further, 37% (304/821) of medical trainees seen by DMHS sought psychiatric services.
All medical students across the 9 campuses have access to DMHS as well as a local mental health resource (often the counseling services offered by the host university), although the type and design of these vary considerably across campuses. DMHS utilization includes intake appointments that can lead to DMHS delivery of services or referral to the local resource for that campus. The utilization of resources (DMHS and local) by regional campus trainees differs widely across campuses. In the 2020–2021 AY, there was 34% DMHS utilization by Indianapolis medical students versus 24% utilization DMHS utilization by regional campus students (ranging from 16% to 32%). This difference may indicate greater use of local resources by regional campus trainees and/or decreased comparative access to services (see Supplemental Digital Appendix 5, at http://links.lww.com/ACADMED/B296, for campus-specific utilization rates).
Medical learners participated in 5,656 visits to DMHS in this AY. Visit types included 327 intakes, 568 initial evaluations (362 counseling-individual/couples and 206 psychiatric), 3,632 counseling follow-ups (3,240 individual, 150 couples, and 242 group), 965 psychiatric follow-ups, 49 crisis sessions, and 111 opt-out wellness checks. Counseling follow-ups (64% or 3,632/5,656) made up the majority of visits, and psychiatric visits (initial, follow-up, and crisis: 1,176/5,656) comprised 21% of total visits in this AY. No-show rates of approximately 5% (measured between November 2020 and June 2021) provide one measure of adherence with treatment. Total visit numbers, but not counseling session totals, include wellness checks, a 30-minute outreach service in which residents meet with a therapist to complete a well-being survey or discuss a mental health/well-being issue.
Demographic analysis examining DMHS usage rates across racial groups shows similar representation of minoritized populations in DMHS patients (37%) in comparison with representation within the overall learner population (36%): Black (8% DMHS patients vs 6% IUSM trainees), Hispanic (9% DMHS patients vs 8% IUSM trainees), Asian (18% DMHS patients vs 17% IUSM trainees), Other (2% DMHS patients vs 5% IUSM trainees), Unknown (2% DMHS patients), and Caucasian (61% DMHS patients vs 64% IUSM trainees). Analysis of utilization by gender revealed an overrepresentation of trainees identifying as female in the DMHS patient population: females make up 63% of DMHS patients versus 48% of IUSM trainees. Tracking through our new EMR (available from November 2020 through June 2021) showed the following most common diagnoses (from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition 29): 383 anxiety disorders, 215 mood disorders, and 78 ADHD diagnoses with some patients noted to have more than one diagnosis. Analysis of Z codes (International Statistical Classification of Diseases, 10th Revision 30 visit encounter categories used in place of, or in combination with, a diagnosis) indicated the following most frequently assigned Z codes in the same time frame: 162 Phase of Life Problems, 67 Academic or Educational Problem, 59 Relationship Distress with Spouse or Intimate Partner, and 40 Parent–Child Relational Problems.
Satisfaction Survey Results
A satisfaction survey sent to all patients seen in 2020 garnered a response rate of 17% (122/720). It revealed high satisfaction with services, with 95% of respondents reporting being satisfied or very satisfied with mental health services and 98% reporting being satisfied or very satisfied with telehealth services. Likewise, 94% of respondents would recommend services to others (with an additional 5% stating “maybe”) and 93% would make another appointment if needed (with an additional 7% reporting “maybe”). The comments were overwhelmingly positive about services, with negative comments directed toward requests for more access to services (specifically, shorter wait times and more frequent visits). In December 2020, 11 out of 49 stakeholders (deans and staff who interact with medical learners) responded to a survey asking open-ended questions such as what is going well and what needs improvement; their comments echoed those of patients—extremely positive feedback about DMHS services with their primary request being additional availability.
Discussion and Lessons Learned
College counseling centers noted a 30% to 40% rise in utilization of services (compared with a 5% rise in enrollment) from 2009 to 2015. 31 Reports 31,32 corroborate increased mental distress and greater demand for services in the college student population leading to the creation of multiple higher education mental health task forces to address these issues. 33 Rising clinical need at the collegiate level may contribute to subsequent demand for services. However, limited comparable data about the development, delivery, and utilization of mental health services for medical trainees exists. Past reports indicate relatively low utilization rates 17–21 although one study showed that 25% of medical learners sought treatment when offered counseling. 20 Despite well-known obstacles and resistance to seeking mental health care, IUSM saw a positive response to the development of a mental health service for medical trainees. In the 2020–2021 AY, 821 trainees sought mental health services including 30% of all medical students and 25% of all residents and fellows. The latter portion of the 4-year observation period for utilization rates coincided with onset of the COVID pandemic, and the pandemic may have contributed to increased utilization. However, use of services grew considerably over the entire period and mirrored the expansion of, and increased capacity for, delivery of services. Utilization of services suggests both a clinical demand and a willingness to seek treatment. When provided with access to care, a significant portion of medical learners used services.
Potential elements contributing to successful utilization of services
Although the individual contribution of specific design elements remains unknown, a number of factors potentially contributed to the increased use of services and List 1 delineates recommendations for the successful implementation of a mental health services program. First and foremost, financial support from the dean’s office played a critical role in the development of services, enabling rapid expansion of the team in response to recognition of unmet clinical demand. Vocal support at all levels from the dean’s office, starting with the Dean of the medical school and extending across faculty and staff, accompanied the financial support. Crucial design elements for structuring services encompassed increasing accessibility (with no session limits, no copays, evening hours, and a crisis line) and minimizing barriers to seeking care (with a private and confidential space, easy access to HIPAA-compliant televisits, availability of both counseling and psychiatry services, as well as short-term and long-term care). Widespread communication (through a variety of outreach efforts) about the availability of services and the importance of attending to one’s mental health needs may have played a role in encouraging trainees to use services. Expansive wellness efforts developed by the medical school education teams co-occurred with the development of services, allowing close collaboration with stakeholders. Although intentional, it is not clear whether hiring a physician (psychiatrist) in the role of director also helped to establish the legitimacy of the service.
In many ways, the medical school (despite the multiple campuses) is a closed system so perceptions about mental health services could be very impactful. Anecdotally, medical trainees reported seeking services after a “word-of mouth” referral from classmates and colleagues. The perception of the department as trustworthy and helpful (as evidenced by satisfaction survey results) could have played a role in growth of the service. We observed high engagement in sessions, good follow-up, and low no-show rates; these factors appeared to contribute to clinical improvement, which may have reinforced the perceived efficacy of services. While DMHS certainly designed services to address barriers to care, simply the availability and perceived helpfulness of services may have impacted readiness to use services.
Areas for growth and further study
Outstanding program issues need to be addressed, particularly those related to access to treatment. Meeting the needs of minoritized medical learners through both the provision of culturally competent care and a diverse mental health team remains an important goal. A disparity exists between medical student and house staff utilization rates, reflecting a possible access issue as house staff have significantly less time and flexibility. GME trainees may be less likely to benefit from the “word-of-mouth” effect as there is less communication across residency and fellowship programs. Although large numbers of trainees used services, stigma concerns may still lead some trainees with mental distress not to seek treatment. Implementation of widespread screening initiatives may help to reach these trainees.
The strong response of IUSM medical learners to the development of a mental health service underscores the need for further study of the clinical needs of this population and the possible benefits of mental health services. Numerous questions arise that require investigation: which design elements best supported the increased utilization of services; did stigma decrease over time; what services are most needed and most impactful for the future well-being of medical trainees; what approaches best serve trainees with the most serious mental health concerns and would decrease the number of deaths by suicide; does utilization of mental health services correlate with successful navigation of medical education; would preventative efforts decrease distress and the need for treatment; and what is the cost–benefit analysis of providing such services. The creation of mental health services for medical learners meets an acute and pressing need and also creates a mechanism to explore these broader issues.
Conclusion
Significant concerns exist about distress in medical learners, their reluctance to seek help, and the negative consequences of this distress. The resourcing and development of a mental health service designed to improve accessibility and minimize barriers to seeking care led to increasing and substantial utilization rates, as well as high satisfaction ratings. This utilization reflects a clinical demand for services, and a willingness on the part of the learner to seek care. Use of the service also demonstrates that medical schools can feasibly assist learners in addressing mental health challenges.
List 1
Recommendations to Promote Successful Utilization of Mental Health Services for Medical Trainees, Incorporated Into Service Design and Delivery
Recognize unique barriers to seeking care
Enlist institutional support
Create accessibility and availability of services through adequate resourcing
Ensure confidentiality and protection of privacy
Develop and implement outreach efforts and widespread communication
Collaborate with stakeholders
Evaluate trainee perceptions of usefulness of and satisfaction with services
Acknowledgments:
The authors wish to acknowledge Stephen Bogdewic, PhD, for his vision and support and Jay Hess, MD, PhD, for his support and the critical financial backing that led to development of this program. The authors thank the larger Indiana University School of Medicine community and, in particular, the graduate medical education and medical student education offices for engaging in, supporting, and promoting the growth of this service. The authors express gratitude to Sarah Finke, LCSW, Jessica Fultz, LCSW, Marshall Garrick, MD, Suzanne Kunkle, PhD, Polly Lybrook, MD, Kathie Mullins, and Michael Trexler, PhD, for their contributions to this work. Finally, the authors wish to show their appreciation for all the IUSM medical learners who have attended to their mental health and engaged in the work of personal growth and development.
Supplementary Material
Footnotes
Supplemental digital content for this article is available at http://links.lww.com/ACADMED/B296.
Funding/Support: None reported.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Stacie L. Pozdol, Email: spozdol@iu.edu.
Brian K. Nichelson, Email: bnichels@iu.edu.
Stephanie J. Cunningham, Email: stejcunn@iu.edu.
Dana G. Lasek, Email: dlasek@iu.edu.
Mary E. Dankoski, Email: mdankosk@iu.edu.
References
- 1.Frajerman A, Morvan Y, Krebs MO, Gorwood P, Chaumette B. Burnout in medical students before residency: A systematic review and meta-analysis. Eur Psychiatry. 2019;55:36–42. [DOI] [PubMed] [Google Scholar]
- 2.Quek TTC, Tam WWS, Tran BX, et al. The global prevalence of anxiety among medical students: A meta-analysis. Int J Environ Res Public Health. 2019;16:2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodrigues H, Cobucci R, Oliveira A, et al. Burnout syndrome among medical residents: A systematic review and meta-analysis. PLoS One. 2018;13:e0206840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: A meta-analysis. Med Educ. 2016;50:456–468. [DOI] [PubMed] [Google Scholar]
- 5.Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA. 2016;316:2214–2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians. JAMA. 2015;314:2373–2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–451. [DOI] [PubMed] [Google Scholar]
- 8.Maser B, Danilewitz M, Guerin E, Findlay L, Frank E. Medical student psychological distress and mental illness relative to the general population. Acad Med. 2019;94:1781–1791. [DOI] [PubMed] [Google Scholar]
- 9.Brazeau CMLR, Shanafelt T, Durning SJ, et al. Distress among matriculating medical students relative to the general population. Acad Med. 2014;89:1520–1525. [DOI] [PubMed] [Google Scholar]
- 10.Baer TE, Feraco AM, Tuysuzoglu Sagalowsky S, Williams D, Litman HJ, Vinci RJ. Pediatric resident burnout and attitudes toward patients. Pediatrics. 2017;139:e20162163. [DOI] [PubMed] [Google Scholar]
- 11.Dewa CS, Loong D, Bonato S, Trojanowski L, Rea M. The relationship between resident burnout and safety-related and acceptability-related quality of healthcare: A systematic literature review. BMC Med Educ. 2017;17:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dyrbye LN, Massie FS, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among us medical students. JAMA. 2010;304:1173–1180. [DOI] [PubMed] [Google Scholar]
- 13.Moutier CY, Myers MF, Feist JB, Feist JC, Zisook S. Preventing clinician suicide: A call to action during the COVID-19 pandemic and beyond. Acad Med. 2021;96:624–628. [DOI] [PubMed] [Google Scholar]
- 14.Goldman ML, Shah RN, Bernstein CA. Depression and suicide among physician trainees: Recommendations for a national response. JAMA Psychiatry. 2015;72:411–412. [DOI] [PubMed] [Google Scholar]
- 15.National Academy of Medicine. Action collaborative on clinician well-being and resilience. https://nam.edu/initiatives/clinician-resilience-and-well-being. Published 2021. Accessed June 1, 2022.
- 16.Council of Residency Directors in Emergency Medicine. National physician suicide awareness day. https://www.cordem.org/npsa. Accessed June 1, 2022.
- 17.Nobleza D, Hagenbaugh J, Blue S, Skahan S, Diemer G. Resident mental health care: A timely and necessary resource. Acad Psychiatry. 2021;45:366–370. [DOI] [PubMed] [Google Scholar]
- 18.Sciolla AF, Haskins J, Chang CH, et al. The suicide prevention, depression awareness, and clinical engagement program for faculty and residents at the University of California, Davis Health. Acad Psychiatry. 2021;45:272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karp JF, Levine AS. Mental health services for medical students: Time to act. N Eng J Med. 2018;379:1196–1198. [DOI] [PubMed] [Google Scholar]
- 20.Ey S, Moffit M, Kinzie JM, Brunett PH. Feasibility of a comprehensive wellness and suicide prevention program: A decade of caring for physicians in training and practice. J Grad Med Educ. 2016;8:747–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chang E, Eddins-Folensbee F, Porter B, Coverdale J. Utilization of counseling services at one medical school. Southern Med J. 2013;106:449–453. [DOI] [PubMed] [Google Scholar]
- 22.Bynum WE, Sukhera J. Perfectionism, power, and process: What we must address to dismantle mental health stigma in medical education. Acad Med. 2021;96:621–623. [DOI] [PubMed] [Google Scholar]
- 23.Fletcher I, Castle M, Scarpa A, Myers O, Lawrence E. An exploration of medical student attitudes towards disclosure of mental illness. Med Educ Online. 2020;25:1727713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aaronson AL, Backes K, Agarwal G, Goldstein JL, Anzia J. Mental health during residency training: Assessing the barriers to seeking care. Acad Psychiatry. 2018;42:469–472. [DOI] [PubMed] [Google Scholar]
- 25.Dyrbye LN, Eacker A, Durning SJ, et al. The impact of stigma and personal experiences on the help-seeking behaviors of medical students with burnout. Acad Med. 2015;90:961–969. [DOI] [PubMed] [Google Scholar]
- 26.Liaison Committee on Medical Education. Functions and structure of a medical school: Standards for Accreditation of Medical Education Programs leading to the MD degree. https://lcme.org/publications/#Standards. Published 2021. Accessed June 1, 2022.
- 27.Halperin SJ, Henderson MN, Prenner S, Grauer JN. Prevalence of anxiety and depression among medical students during the COVID-19 pandemic: A cross-sectional study. J Med Educ Curric Dev. 2021;8:2382120521991150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaplan CA, Chan CC, Feingold JH, et al. Psychological consequences among residents and fellows during the COVID-19 pandemic in New York City: Implications for targeted interventions. Acad Med. 2021;96:1722–1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 30.World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders. Geneva, Switzerland: World Health Organization; 1993. [Google Scholar]
- 31.Lipson SK, Lattie EG, Eisenberg D. Increased rates of mental health service utilization by U.S. college students: 10-year population-level trends (2007–2017). Psychiatr Servs. 2019;70:60–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.LeViness P, Gorman K, Braun L, Koenig L, Bershad C. The Association for University and College Counseling Center Directors Annual Survey: 2019. https://www.aucccd.org/assets/documents/Survey/2019%20AUCCCD%20Survey-2020-05-31-PUBLIC.pdf. Accessed June 9, 2022.
- 33.Chessman HM, Vigil D, Soler MC. Mental health task forces in higher education. American Council on Education. https://www.acenet.edu/Documents/Mental-Health-Task-Forces-in-Higher-Education.pdf. Published 2020. Accessed June 1, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.