Abstract
Purpose of Review
SARS-CoV-2 has had a devastating global effect, with vaccinations being paramount in the public health strategy against COVID-19. Vaccinations have uncoupled infection from adverse COVID-19 outcomes worldwide. While immune-modifying therapies are effective for the management of skin diseases such as psoriasis and atopic dermatitis, these medications also impair protective immune responses. There has been longstanding uncertainty and concern over the impact of immune-modifying therapies on the effectiveness of vaccines; for example, it is well recognised that methotrexate impairs humoral responses to both influenza and pneumococcal vaccines. This narrative review aims to discuss the evidence to date on the impact of immune-modifying therapies on the immune response to COVID-19 vaccines, with a focus on the first two vaccine doses.
Recent Findings
Individuals receiving immune-modifying therapy are more likely to have attenuated humoral responses to a single dose of COVID-19 vaccine compared to healthy controls; however, this may be improved by a complete course of vaccination. B cell targeted biologics such as rituximab markedly impair the humoral response to both the first and second COVID-19 vaccination. There remains a paucity of data on cellular immune responses, with the few available studies indicating lower responses to two vaccine doses in individuals receiving immune-modifying therapies compared to healthy controls, which may impact the durability of immune responses.
Summary
Inadequate humoral immune responses to a single dose of vaccine in the context of immune-modifying therapy are improved by a complete course of vaccination. Individuals receiving immune-modifying treatments should be encouraged to take up a complete vaccine course to mitigate their risk against COVID-19. Research in large patient populations on the longevity/kinetics of the complex humoral and cellular response to subsequent vaccine doses, including against newer variants of concern, is warranted, in addition to data on immune correlates of vaccine clinical effectiveness.
Keywords: COVID-19 vaccine, Immune-modifying therapy, Immunosuppression, Skin disease
Introduction
Immune-modifying therapies have improved clinical and quality of life outcomes of individuals with immune-mediated skin diseases such as psoriasis, atopic dermatitis and immunobullous disease. However, these medications can also impair protective immune responses [1, 2]. COVID-19 vaccination programmes have seen great success, with reassuring safety data and two doses of COVID-19 vaccines reported to be 89–97% effective against the development of symptomatic infection in the general population (data pertain to older SARS-CoV-2 variants such as Alpha, Beta, Delta, Gamma) [3]. Given that infection-acquired immunity is limited in duration and susceptible to variants, vaccines are important for mitigating against severe COVID-19 outcomes [4, 5]. Due to concerns over the effectiveness of vaccines in individuals who are receiving immune-modifying therapies, the impact of these medications on the immune response to COVID-19 vaccinations has been an area of intensive investigation [6].
Immune-modifying therapy can be divided into two broad groups: standard systemic and targeted. Standard systemic drugs include methotrexate, ciclosporin, azathioprine, mycophenolate mofetil, acitretin and fumaric acid esters. Targeted therapies used in dermatology include biologics such as TNF-inhibitors (TNFi: adalimumab, certolizumab pegol, etanercept, infliximab), IL-17 inhibitors (IL-17i: bimekizumab, brodalumab, ixekizumab, secukinumab), IL-23 inhibitors (IL-12/IL-23p40 inhibitor ustekinumab, IL-23p19 inhibitors: guselkumab, risankizumab, tildrakizumab), IL-4/IL-13 inhibitor dupilumab and CD20 inhibitor rituximab. Other targeted therapies include small molecule agents such as JAK inhibitors (JAKi: abrocitinib, baricitinib, upadacitinib) and phosphodiesterase inhibitors such as apremilast.
The UK was the first country to approve the use of COVID-19 vaccines in December 2020. Currently there are at least 37 different COVID-19 vaccines approved in different countries worldwide, with more in the development pipeline [7]. In the UK, this includes the BNT162b2 Pfizer/BioNTech, mRNA-1273 Moderna and the ChAdOx1-S Oxford/AstraZeneca COVID-19 vaccines (Table 1) [8]. In the USA, the BNT162b2 Pfizer/BioNTech, mRNA-1273 Moderna, the Janssen Ad26.COV2-S (recombinant) and Novavax COVID-19 vaccines are licensed for use [9, 10]. Both the BNT162b2 Pfizer/BioNTech and mRNA-1273 Moderna vaccine are modified messenger RNA (mRNA) based-vaccines, which utilise lipid nanoparticles to facilitate entry into host cells. Upon entering host cells, the nanoparticle inserts its mRNA into the cytoplasm, where it is translated into the SARS-CoV-2 structural surface glycoprotein (spike [S] protein), which then stimulates humoral and cellular immune responses [11]. The ChAdOx1-S Oxford/AstraZeneca vaccine comprises a replication-deficient chimpanzee adenoviral vector (ChAdOx1), which contains a gene encoding the S protein [12]. The Janssen Ad26.COV2-S COVID-19 vaccine uses a recombinant, replication-incompetent human adenovirus type 26 vector to deliver a gene encoding the S protein. The Novavax COVID-19 vaccine is a protein subunit-based vaccine that comprises recombinant S protein nanoparticle combined with Matrix-M adjuvant [10].
Table 1.
COVID-19 vaccines approved in the UK and/or the USA
| Vaccine | Vaccine platform | Mechanism of action | Posology for general population |
|---|---|---|---|
| BNT162b2 Pfizer/BioNTech | mRNA based | Lipid nanoparticles enter host cells and insert mRNA into the cytoplasm. Translation of S protein stimulates both humoral and cellular immune responses |
Primary vaccination course: 2 doses, at least 8 weeks apart Booster/reinforcing/third dose is recommended at least 3 months after the primary course |
|
mRNA-1273 (Moderna) |
mRNA based | Lipid nanoparticles enter host cells and insert mRNA into the cytoplasm. Translation of S protein stimulates both humoral and cellular immune responses |
Primary vaccination course: 2 doses, at least 8 weeks apart Booster/reinforcing/third dose is recommended at least 3 months after the primary course |
| ChAdOx1-S Oxford/AstraZeneca | Deficient chimpanzee adenovirus | Replication-deficient chimpanzee adenovirus contains DNA encoding S protein. The DNA is released into the cytoplasm, migrates into the cell nucleus and host enzymes transcribe mRNA, which migrates back to the cytoplasm. Here, it interacts with host cell ribosomes to enable S protein translation |
Primary vaccination course: 2 doses, at least 8 weeks apart Booster/reinforcing/third dose is recommended at least 3 months after the primary course |
| Janssen Ad26.COV2-S | Deficient adenovirus-26 | Replication-incompetent recombinant human adenovirus type 26 vector contains DNA encoding S protein. Host enzymes in the cell nucleus transcribe mRNA, which then migrates to the cytoplasm, where S protein translation takes place |
Primary vaccination course: 1 dose Booster/reinforcing/second dose of Janssen COVID-19 vaccine not recommended by US Advisory Committee on Immunization Practices due to reports of thrombosis with thrombocytopenia syndrome (TTS) [9]. Preferential use of mRNA COVID-19 vaccines recommended over the Janssen COVID-19 vaccine for primary and booster vaccination in all individuals aged ≥ 18 years in the USA [9] |
| Novavax COVID-19 Vaccine, Adjuvanted | Subunit protein | Recombinant S protein nanoparticle combined with Matrix-M adjuvant |
Primary vaccination course: 2 doses, at least 3 weeks apart Booster/reinforcing/third dose not yet approved |
The Impact of Immune-Modifying Therapy on the Immune Response to COVID-19 Vaccines
There has been longstanding uncertainty and concern over the impact of immune-modifying therapies on the effectiveness of different vaccines; for example, it is well recognised that methotrexate impairs humoral responses to both influenza and pneumococcal vaccines [13]. Since individuals receiving immune-modifying therapies were considered more vulnerable to adverse COVID-19 outcomes than the general population, they have been prioritised during the global COVID-19 vaccine roll-out. Public health policies across the world also advocated an additional COVID-19 vaccine dose as part of the primary course. Therefore, for individuals receiving immune-modifying therapies, a third vaccine dose (BNT162b2 Pfizer/BioNTech, mRNA-1273 Moderna, or ChAdOx1-S Oxford/AstraZeneca vaccines) is considered part of the primary vaccination course and this should be administered at least 8 weeks after the second dose [8]. A booster dose is then recommended at least 3 months following the third primary dose.
While data on clinical effectiveness of vaccines (i.e. in prevention of COVID-19 transmission or severe disease) requires longer-term population-level follow-up, the initial focus of the research community turned to the impact of immune-modifying therapies on the immune response to the COVID-19 vaccine, i.e. immunogenicity. The immune response to a vaccine involves a complex interplay between the humoral and cellular immune response; hence when assessing a vaccine’s immunogenicity, both humoral and cellular immune responses should be considered [14]. Within the humoral response, seroconversion and neutralising activity can be assessed. Seroconversion is the development of antibodies in the blood serum as a result of vaccination. Following COVID-19 vaccination, seroconversion is assessed by measuring IgG antibodies against the S1 domain of the SARS-CoV-2 S protein. Neutralising antibodies can also be measured which target S1 receptor binding domain (RBD), N-terminal domain (NTD) and S2 region of the S protein. These antibodies block viral entry into host cells by preventing the interaction between the host cell angiotensin-converting enzyme 2 (ACE2) and S protein [15, 16]. Finally, assessment of the cellular response to the vaccine involves the analysis of the frequency and function of T cells which recognise viral proteins indirectly and in association with Major Histocompatibility Complex (MHC) I and II molecules [17].
Methods: Literature Search Strategy
We performed a search of PubMed and Google Scholar databases on March 10, 2022, for studies that have investigated the effect of immune-modifying therapy for skin diseases on COVID-19 vaccine responses. Search terms included “immune therapy”, “immune-modifying therapy”, “immunosuppressant”, “vaccines”, “COVID-19 vaccines”, “COVID-19”, “dermatology” and “skin”, of which “COVID-19”, “COVID-19 vaccines”, “immunosuppressants”, “vaccines”, “skin” and “dermatology” are MESH terms. Outcomes that were analysed included the humoral (seroconversion and/or neutralisation) and cellular responses to the first and second doses of COVID-19 vaccinations. Studies that included individuals with non-skin immune-mediated inflammatory diseases (IMIDs) such as rheumatoid arthritis were included due to shared immune-modifying treatments. There was no minimum size of study and only papers written in English were included.
Results: Summary of Findings from Literature Search
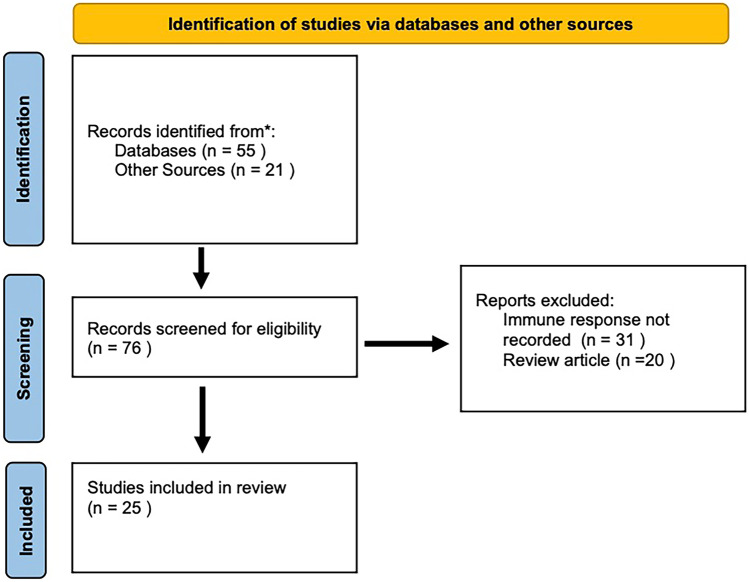
Twenty-five studies were identified (Fig. 1, Table 2) [18–32, 33•, 34•, 35–42].
Fig. 1.
PRISMA flowchart of literature search strategy
Table 2.
Details of studies included in this review
| Study | Study population (number of individuals, n) | Demographics | Immune-modifying therapy | COVID-19 vaccine | Immune response after first dose of COVID-19 vaccine | Immune response after second dose of COVID-19 vaccine |
|---|---|---|---|---|---|---|
| Al-Janabi et al. [18] |
IMIDs (n = 120) including psoriasis, PsA, RA, SLE and Crohn’s disease No controls |
Median age: 53 years Gender: 49 (41%) female Ethnicity 111 (92.5%) White, 9 (7.5%) Asian |
Standard systemic Apremilast, ciclosporin, dimethyl fumarate, methotrexate and prednisone Targeted Abatacept, adalimumab, brodalumab, certolizumab, etanercept, guselkumab, ixekizumab, risankizumab, secukinumab, tildrakizumab and ustekinumab |
BNT162b2 (60/120, 50%) ChAdOx1 nCoV-19 (60/120, 50%) |
Humoral Seroconversion 23/31 (74%) patients on standard immune-modifying therapy had detectable antibodies vs 73/81 (90%) on targeted immune-modifying therapy at 34 days post-vaccine Use of standard immune-modifying therapy reduced the odds of a detectable antibody response vs targeted immune-modifying therapy (adjusted OR 0.31) |
N/A |
| Ammitzbøll et al. [19] |
SLE (n = 61) and RA (n = 73) No controls |
Median age: SLE – 60 years RA – 70 years Gender: SLE – 41 (77.1%) female RA – 49 (67.1%) female Ethnicity: Not included |
Standard systemic Azathioprine, hydroxychloroquine, leflunomide, methotrexate, mycophenolate mofetil, prednisone and salazopurine Targeted Abatacept, belimumab, JAKi, IL-6i, rituximab, TNFi |
BNT162b2 | N/A |
Humoral Seroconversion 103/134 (77%) patients had detectable antibodies at 8 days post-second vaccine dose. A lower proportion of patients with RA than SLE had detectable antibodies (49/73 [67%] vs 54/61 [89%]) 4/17 (24%) patients receiving rituximab had detectable antibodies vs 0/6 (0%) receiving rituximab/methotrexate co-therapy |
| Boekel et al. [20] |
IMIDs including RA, PsA, ankylosing spondylitis, axial/peripheral spondyloarthritis, juvenile idiopathic arthritis, SLE, vasculitis, PMR, Sjögren’s disease, multiple sclerosis, sarcoidosis, systemic sclerosis, myositis, mixed connective tissue disease (n = 632) Healthy controls (n = 289) |
Mean age: IMIDs – 63 years Healthy controls – 63 years Gender: IMIDs – 423 (67%) female Healthy controls – 195 (67%) female Ethnicity: Not included |
Standard systemic Azathioprine, ciclosporin, hydroxychloroquine, leflunomide, methotrexate, prednisone and sulfasalazine Targeted Abatacept, ixekizumab, natalizumab, ocrelizumab, rituximab, secukinumab, tocilizumab, ustekinumab, and TNFi |
ChAdOx1 nCoV-19 (514/921, 56%) BNT162b2 (460/921, 50%) mRNA-1273 (55/921 6%) Ad.26.COV2.S (3/921, 0.3%) |
Humoral Seroconversion 210/432 (49%) individuals with IMIDs had detectable antibodies vs 154/210 (73%) healthy controls (adjusted OR 0·33; p < 0·0001) at 34 vs 36 days post vaccine, respectively 43/133 (32%) individuals with IMIDs on methotrexate, 1/18 (6%) on rituximab/ocrelizumab, and 24/36 (67%) on TNFi had detectable antibodies |
Humoral Seroconversion 97/106 (92%) individuals with IMIDs had detectable antibodies vs 38/40 (95%) healthy controls at 38 and 42 days post second dose, respectively 17/18 (94%) individuals with IMIDs on methotrexate, 3/7 (43%) on rituximab/ocrelizumab, and 14/14 (100%) on TNFi had detectable antibodies |
| Bonelli et al. [21] |
Rheumatological disease (n = 5) including immune-mediated necrotizing myopathy, ANCA-associated vasculitis, eosinophilic granulomatosis, SLE and mixed connective tissue disease Healthy controls: vaccinated (n = 4) and unvaccinated (n = 4) |
Median age: Rheumatological disease – 49 years Gender: Rheumatological disease – 3 (60%) females Ethnicity: Not included Demographics for controls not included |
Targeted Rituximab |
BNT162b2 | N/A |
Humoral Seroconversion 2 of 5 (40%) individuals receiving rituximab had detectable antibodies at 23 days post second vaccination Cellular IFN-γ response was detected in the rituximab-treated group (5/5, 100%) and vaccinated healthy control group (4/4, 100%), independent of the humoral immune response |
| Boyarsky et al. [22] |
Rheumatological disease (n = 123) including inflammatory arthritis (28%), SLE (20%), Sjogren’s syndrome (13%) and overlap connective tissue diseases (29%) No controls |
Mean age: 50 years Gender: 117 (95%) female Ethnicity: 111 (90%) White |
Standard systemic Azathioprine, hydroxychloroquine, leflunomide, methotrexate, mycophenolate mofetil, sulfasalazine and tacrolimus Targeted Abatacept, adalimumab, belimumab, certolizumab, etanercept, infliximab, ixekizumab rituximab, tocilizumab, tofacitinib, ustekinumab |
BNT162b2 (64/123, 52%) mRNA-1273 (59/123, 48%) |
Humoral Seroconversion 91/123 (74%) of individuals with rheumatological diseases had detectable antibodies 18–26 days post-vaccine 55/85 (65%) individuals receiving standard immune-modifying therapy had detectable antibodies vs 16/17 (94%) individuals receiving TNFi A lower proportion of individuals receiving rituximab (2/6, 33%) had an antibody response vs those receiving methotrexate (10/13, 77%) or TNFi (16/17, 94%) |
N/A |
| Braun-Moscovici et al. [23] |
Rheumatological disease (n = 264) including RA, PsA, SpA, sarcoidosis, SLE, systemic sclerosis, myositis, Sjogren’s syndrome, myositis and vasculitis Individuals recovered from COVID-19 (n = 26) |
Mean age: Rheumatological disease – 58 years Recovered from COVID-19 – 47 years Gender: Rheumatological disease – 200 (76%) female Recovered from COVID-19 – 19 (73%) female Ethnicity: Not included |
Standard systemic Azathioprine, ciclosporin, corticosteroids, hydroxychloroquine, leflunomide, methotrexate, mycophenolate mofetil, Purinethol and salazopurine Targeted Abatacept, adalimumab, anakinra, baricitinib, belimumab, certolizumab, etanercept, golimumab, infliximab, ixekizumab, JAKi, mepolizumab, risankizumab, rituximab, sarilumab, secukinumab, tocilizumab, tofacitinib, upadacitinib and ustekinumab |
BNT162b2 | N/A |
Humoral Seroconversion 68/78 (87%) methotrexate-treated individuals, 24/48 (50%) rituximab-treated individuals and 63/63 (100%) individuals on TNFi had detectable antibodies 4–6 weeks following the 2nd dose Neutralisation 227/264 (86%) individuals with rheumatological disease had detectable neutralising antibodies 4–6 weeks following the 2nd dose. 23/47 (49%) individuals on rituximab had detectable neutralising antibodies vs 5/8 (63%) individuals on abatacept, 17/21 (81%) individuals on mycophenolate mofetil and 4/5 (80%) individuals on IL-17i. Neutralising titres were higher in vaccinated individuals vs individuals with rheumatological disease who had recovered from COVID-19 (p < 0.05) |
| Bugatti et al. [24] |
Rheumatological disease (n = 140) including RA, PsA, SpA No controls |
Mean age: 56 years Gender: 95 (67.9%) female Ethnicity: Not included |
Standard systemic Ciclosporin, leflunomide, methotrexate, prednisone and sulfasalazine, Targeted Cytotoxic T lymphocyte associated protein-4 immunoglobulin (CTLA4Ig), IL-6Ri, IL-17/IL-23i, JAKi, PDE4i and TNFi |
BNT162b2 |
Humoral Seroconversion 85/140 (60%) individuals had detectable antibodies after 21 days. Use of methotrexate, glucocorticoids and CTLA4Ig was more common, and use of IL-17/23 inhibitors was less common, in individuals who did not mount detectable antibodies Seroconversion decreased from 85.4% among patients not on methotrexate or glucocorticoids to 33.3% among those on both therapies |
N/A |
| Chen et al. [25] |
IMIDs including RA, SLE, PsA, multiple sclerosis, ankylosing spondylitis, Sjögren’s syndrome, Hashimoto’s disease, psoriasis, combined variable immune deficiency, vasculitis, scleroderma, ANCA-associated vasculitis, IBD, alopecia areata, asthma and inflammatory arthritis (n = 75) Healthy controls (n = 25) |
Median age: 49 years Gender: 52 (68%) female Ethnicity: 69 (90%) White, 5 (6%) Black, 1 (1%) Asian Demographics for controls not included |
Standard Systemic Sulfasalazine, antimetabolites, systemic steroids Targeted anti-CD20, IL-23i and TNFi |
BNT162b2 | N/A |
Humoral Seroconversion Individuals receiving anti-CD20 had substantially lower levels of spike-specific IgG vs controls at 3 months post second dose. Most other drug treatment groups showed no statistically significant differences in spike-specific IgG titres vs controls Neutralisation 48/75 (64%) individuals with IMIDs on immune-modifying therapy developed adequate neutralization titres against Delta variant vs 23/25 (92%) healthy controls at 3 months post vaccine. 8/12 (67%) individuals on TNFi developed adequate neutralization titres compared to 2/9 (22%) on IL-23i and 4/12 (33%) on antimetabolites |
| Dailey et al. [26] |
IBD (n = 436) including Crohn’s disease, ulcerative colitis and IBD-unspecified. Only 33 were analysed post vaccination Adult and paediatric controls (number or other details not specified) |
Mean age: 17 years Gender: 183 (42%) female Ethnicity: Not included |
Standard systemic Corticosteroids and methotrexate Targeted Infliximab, vedolizumab |
BNT162b2 (21/33, 63.6%) mRNA-1273 (7/33, 21.2%) Ad26.COV2-S (5/33, 15.2%) |
N/A |
Humoral Seroconversion Spike-specific IgG responses were higher (~ 15 ×) following vaccination vs natural infection in the IBD subgroup between 3.1 and 3.3 weeks post 2nd dose (p < 0.0001) Neutralising All IBD subjects had higher (~ 10 ×) neutralising titres (against SARS-CoV-2 wild type [WT] or mutant [mt S-RBD] spike protein receptor binding domain) post 2nd vaccination vs those with history of natural infection, including patients receiving infliximab monotherapy or infliximab/methotrexate co-therapy |
| Deepak et al. [27] |
IMIDs including RA, spondyloarthritis, uveitis, SLE, vasculitis, Sjogren syndrome, multiple sclerosis and IBD (n = 133) Healthy controls (n = 53) |
Mean age: IMIDs – 45 years Healthy controls – 43 years Gender: IMIDs – 99 (74.4%) female Healthy controls – 29 (54.7%) female Ethnicity: IMIDs – 117 (88.0%) White, 9 (6.8%) Asian, 4 (3.0%) Black or African American, 3 (2.3%) others Healthy controls – 42 (79.2%) White, 7 (13.2%) Asian, 1 (1.9%) Black or African American, 3 (5.7%) other |
Standard systemic Azathioprine, hydroxychloroquine, leflunomide, methotrexate, mycophenolate mofetil, sulfasalazine and tacrolimus Targeted Adalimumab, certolizumab, etanercept, golimumab, guselkumab, infliximab, ocrelizumab, rituximab and ustekinumab |
BNT162b2 mRNA-1273 Number of individuals receiving specific vaccines not given |
N/A |
Humoral Seroconversion 118/133 (89%) individuals with IMIDs vs all healthy controls (53/53, 100%) seroconverted within 14–20 days post-vaccination. No difference between individuals with IMIDs on standard immune-modifying therapy vs those not on standard immune-modifying therapy 6/10 (60%) individuals with IMIDs receiving rituximab/ocrelizumab seroconverted Neutralising Neutralisation titres against the common variant (D614G) were 2391 (95% CI 1537 to 3719) in individuals with IMIDs on standard immune-modifying therapy vs 2270 (95% CI, 1650 to 3121) in those not on standard therapy at 20 days post-vaccination Individuals with IMIDs on rituximab/ocrelizumab had lower neutralisation titres vs individuals with IMIDs who were not on rituximab/ocrelizumab (neutralisation titres 723 (95% CI 233 - 2246) vs 2445 (95% CI 1890 - 3164), respectively) |
| Furer et al. [28] |
Rheumatological disease including RA, PsA, axial spondyloarthritis, SLE, systemic vasculitis, large vessel vasculitis (n = 686) Healthy controls (n = 121) |
Median age: Rheumatological disease – 59 years Healthy controls – 50 years Gender: Rheumatological disease – 475 (69.3%) female Healthy controls – 78 (65%) female Ethnicity: Not mentioned |
Standard systemic Glucocorticoids, hydroxychloroquine, leflunomide, methotrexate and mycophenolate mofetil Targeted Abatacept, IL-6i, IL-17i, JAKi, rituximab and TNFi |
BNT162b2 | N/A |
Humoral Seroconversion 590/686 (86%) patients with rheumatological diseases seroconverted vs 100% controls (p < 0.0001), 2–6 weeks after the second vaccination Compared to individuals receiving biologic monotherapy, those on methotrexate monotherapy or methotrexate in combination with other treatments had reduced seroconversion rates (> 97% vs 92%, p = 0.02 or 84%, p < 0.0001, respectively) Rituximab impaired seroconversion (39%) Spike specific IgG titres were significantly lower in individuals with rheumatological diseases compared with controls |
| Geisen et al. [29] |
IMIDs including psoriasis, IBD, SLE, RA, spondyloarthropathy, PsA (n = 26) Healthy controls (n = 42) |
Mean age: IMIDs – 51 years Healthy controls – 38 years Gender: IMIDs – 17 (64.3%) female Healthy controls – 29 (69.2%) female Ethnicity: Not included |
Standard systemic Azathioprine, leflunomide, hydroxychloroquine and sulfasalazine Targeted Adalimumab, belimumab, certolizumab, etanercept, golimumab, infliximab, ixekizumab, secukinumab, tocilizumab, ustekinumab and vedolizumab |
BNT162b2 (63/68, 92.6%) mRNA-1273 (5/68, 7.4%) |
N/A |
Humoral Seroconversion Spike specific IgG was detected in all individuals Lower titres were detected in individuals with IMIDs vs healthy controls (mean titre 2053 BAU/mL vs 2685 BAU/mL, p = 0.037) at 7 days post- second dose. No significant difference between standard immune-modifying therapy, TNFi and IL-17i Neutralising Individuals with IMIDs on immune-modifying therapy had lower levels of neutralising antibodies vs healthy controls (mean inhibitory level 87.42% vs 96.04%, p = 0.044) |
|
Haberman et al. [30] New York Cohort |
IMIDs including psoriasis, PsA, RA, vasculitis, dermatomyositis, adult-onset Still’s disease, sarcoidosis, PMR (n = 51) Healthy controls (n = 26) New York Cohort |
Mean age: IMIDs, not on methotrexate – 49 years IMIDs, on methotrexate – 63 years Healthy controls – 49 years Gender: IMIDs, not on methotrexate – 18 (69.2%) female IMIDs on methotrexate – 18 (66.7%) female Healthy controls – 16 (61.5%) female Ethnicity: IMIDs, not on methotrexate – 20 (76.9%), 2 (7.7%) Black, 3 (11.5%) Asian, 3 (11.5%) Hispanic IMIDs, on methotrexate – 17 (63%) White, 3 (11.1%) Black, 3 (11.1%) Asian, 5 (18.5%) Hispanic Healthy controls – 16 (61.5%) White, 1 (3.8%) Black, 9 (34.6%) Asian, 1 (3.8%) Hispanic |
Standard systemic Hydroxychloroquine, leflunomide, methotrexate, oral steroids, sulfasalazine Targeted Abatacept, apremilast, IL-17i, IL-23i, JAKi, rituximab and TNFi |
BNT162b2 | N/A |
Humoral Seroconversion 18/25 (72.0%) of IMID cohort on methotrexate had detectable antibodies vs 24/26 (92.3%) not on methotrexate (p = 0.045). 25/26 (96.1%) healthy controls had detectable antibodies Timing of sampling not specified Cellular Spike-specific B cells, activated CD4 + T cells and circulating T follicular helper cells were similarly induced in all groups Activated CD8+ T-cell responses were attenuated in methotrexate-treated group vs healthy controls or individuals with IMIDs not receiving methotrexate |
|
Haberman et al. [30] Erlangen cohort |
IMIDs including psoriasis, PsA, RA, vasculitis, dermatomyositis, adult-onset Still’s disease, sarcoidosis, PMR (n = 31) Healthy controls (n = 182) Erlangen cohort |
Mean age: IMIDs, not on methotrexate – 45 years IMIDs, on methotrexate – 55 years Healthy controls – 41 years Gender: IMIDs, not on methotrexate – 7 (58.3%) female IMIDs, on methotrexate – 15 (75.0%) female Healthy controls – 104 (57.1%) female Ethnicity: IMIDs, not on methotrexate–11 (100%) White IMIDs, on methotrexate – 19 (95%) White and 1 (5%) Asian Healthy controls – 178 (97.8%) White, 2 (1.1%) Asian, 1 (0.6%) Hispanic |
Standard systemic Methotrexate Targeted TNFi |
BNT162b2 | N/A |
Humoral Seroconversion 10/11 (90.9%) patients not on methotrexate, and 10/20 (50.0%) patients receiving methotrexate had detectable antibodies vs 179/182 (98.3%) healthy controls Timing of sampling not specified |
| Kappelman et al. [31] |
IBD (n = 317) No controls |
Mean age: 51 years Gender: 238 (75%) female Ethnicity: 301 (95%) White, 5 (2%) Asian |
Standard systemic 6-mercaptopurine, azathioprine, budesonide, methotrexate and sulfasalazine Targeted TNFi, ustekinumab and vedolizumab |
BNT162b2 (173/317, 55%) mRNA-1273 (144/317, 45%) |
N/A |
Humoral Seroconversion 300/317 (94.6%) had detectable antibodies at 64 days post-2nd vaccination. 11/13 (85%) individuals taking corticosteroids had detectable antibodies vs 289/304 (95%) non-steroid users 19/20 (95%) individuals on standard immune-modifying therapy had detectable antibodies vs 101/108 (94%) individuals on TNFi monotherapy |
| Kennedy et al. [32] |
IBD including Crohn’s disease, ulcerative colitis or IBD unclassified who have received one dose of vaccination (n = 1293) and two doses (n = 27) No healthy controls |
Mean age: Overall – 44 years Infliximab – 41 years Vedolizumab – 49 years Gender: Overall – 634 (49.2%) female Infliximab – 434 (50.3%) female Vedolizumab – 200 (47.1%) female Ethnicity: Overall – 1172 (91.1%) White, 78 (6.1%) Asian, 24 (1.9%) mixed, 8 (0.6%) Black Infliximab – 791 (91.8%) White, 46 (5.3%) Asian, 16 (1.9%) mixed, 6 (0.7%) Black Vedolizumab – 381 (89.9%) White, 32 (7.5%) Asian, 8 (1.9%) mixed, 2 (0.5%) Black |
Targeted Infliximab and vedolizumab |
BNT162b2 (589/1293, 45.6%) ChAdOx1 nCoV-19 (704/1293, 54.4%) |
Humoral Seroconversion Spike-specific IgG titres were lower in patients treated with infliximab vs vedolizumab, at 3–10 weeks following BNT162b2 (6.0 U/mL vs 28.8 U/mL, p < 0.0001) or ChAdOx1 nCoV-19 (4.7 U/mL vs 13.8 U/mL, p < 0.0001) |
Humoral Seroconversion 17/20 (85%) infliximab-treated individuals and 6/7 (86%) vedolizumab-treated individuals seroconverted at 3–10 weeks post-vaccination (p = 0.68) |
| Mahil et al. [33•] |
Psoriasis (n = 84) Healthy controls (n = 17) |
Median age: Methotrexate – 48 years TNFi–36 years IL-17i – 45 years IL-23i – 50 years Healthy controls – 34 years Gender: Methotrexate – 6 (35%) female TNFi – 14 (52%) female IL-17i – 7 (47%) female IL-23i – 10 (40%) female Healthy controls – 8 (47%) female Ethnicity: Methotrexate – 13 (76%), 1 (6%) Black, 3 (18%) South Asian TNFi – 24 (89%), 3 (11%) South Asian IL-17i – 13 (87%) White, 2 (13%) South Asian IL-23i – 21 (84%) White, 3(12%) South Asian, 1 (4%) mixed Healthy controls – 14 (82%) White, 3 (18%) South Asian |
Standard systemic Methotrexate Targeted Adalimumab, certolizumab, etanercept, guselkumab, infliximab, ixekizumab, risankizumab secukinumab and ustekinumab |
BNT162b2 |
Humoral Seroconversion 60/77 (78%) individuals receiving immune-modifying therapy vs 17/17 (100%) healthy controls seroconverted, at 28 days post-vaccine Individuals receiving methotrexate (7/15, 47%) had a lower seroconversion rate vs individuals receiving biologics including TNFi (19/24, 79%), IL-17i (15/15, 100%) and IL-23i (19/23, 83%) Neutralising Individuals receiving TNFi, IL-17i, and IL-23i had similar neutralisation titres against wild-type SARS-CoV-2 vs controls. Patients on methotrexate had lower neutralisation titres (median ID50 129 [IQR 40–236]) vs patients on biologics (269 [141–418], p = 0·011) or healthy controls (317 [213–487], p = 0.0032) Cellular T-cell response rates were similar in patients receiving methotrexate, biologics, and controls at 28 days post-vaccine |
N/A |
| Mahil et al. [34•] |
Psoriasis (n = 67) Healthy controls (n = 15) |
Median age: Methotrexate – 50 years TNFi – 36 years IL-17i – 43 years IL-23i – 51 years Healthy controls – 38 years Gender: Methotrexate – 6 (43%) female TNFi – 11 (58%) female IL-17i – 7 (50%) female IL-23i – 8 (40%) female Healthy controls – 7 (47%) female Ethnicity: Methotrexate – 11 (79%) White, 1 (7%) Black, 2 (14%) South Asian TNFi – 18 (95%) White, 1 (5%) South Asian IL-17i – 12 (86%) White, 2 (14%) South Asian IL-23i – 17 (85%) White, 2 (10%) South Asian, 1 (5%) mixed Healthy controls – 13 (87%) White, 2 (13%) South Asian |
Standard systemic Methotrexate Targeted IL-17i, IL-23i and TNFi |
BNT162b2 | N/A |
Humoral Seroconversion All participants seroconverted 14 days post-second vaccine The second vaccine boosted spike-specific IgG titres in all groups, with no significant differences between patients receiving immune-modifying therapy (median EC50 1816 [IQR 641–3645]) vs healthy controls (2749 [867–4770], p = 0·14). Median titres were lowest in individuals on methotrexate (median EC50 1751 [IQR 468–4976]) vs patients on biologics (1816 [787–3534], p = 0·65) or healthy controls (2749 [867–4770], p = 0·20) Neutralising All participants had detectable neutralising antibodies against wild-type, Alpha, and Delta variants post-second vaccine. All groups showed increased neutralising antibody titres post-second vs first dose. Individuals on methotrexate had similar neutralisation activity against the Alpha variant (ID50 440 [IQR 101–935]) vs those receiving biologics (453 [233–955], p = 0·97) or healthy controls (491 [264–1227], p = 0·63). Neutralisation activity against the Delta variant was similar across all groups i.e. individuals on methotrexate (ID50 856 [77–1476]), biologics (469 [232–1309], p = 0·76) and controls (863 [225–1297], p = 0·49) Cellular Those on methotrexate had lower induction of T-cell responses vs healthy controls. A lower proportion of patients receiving methotrexate had detectable T-cell responses (8/13, 62% [95%CI 32–86]) vs those on biologics (37/50, 74% [95%CI 60–85], p = 0·38) or controls (14/14, 100% [95%CI 77–100], p = 0·022) |
| Moor et al. [35] |
Patients including ANCA-associated vasculitis, RA, Sjogren’s syndrome, SLE, multiple sclerosis, pemphigus vulgaris, systemic sclerosis and pemphigoid (n = 96) Healthy controls (n = 29) |
Median age: Patients – 67 years Healthy controls – 54 years Gender: Patients – 51 (53%) female Healthy controls – 19 (66%) female Ethnicity: Not included |
Targeted Ocrelizumab or rituximab |
BNT162b2 (58/96, 60%) mRNA-1273 (38/96, 40%) |
N/A |
Humoral Seroconversion Detectable antibodies in 47/96 (49%) patients on rituximab/ocrelizumab at 1·79 months post-second vaccine dose, vs 29/29 (100%) controls at 1·81 months (p < 0·001) Cellular SARS-CoV-2-specific IFNγ responses detected in 14/44 (32%) patients on rituximab/ocrelizumab vs 22/25 (88%) healthy controls (p < 0·001) |
| Rubbert-Roth et al. [36] |
RA (n = 53) Healthy controls (n = 20) |
Mean age: RA – 65 years Healthy controls – 45 years Gender: RA – 29 (54.7%) female Healthy controls – 14 (70%) female Ethnicity: Not included |
Standard systemic Leflunomide, methotrexate and prednisone Targeted Anti-cytokine drugs (specific drugs not mentioned), abatacept, JAKi |
BNT162b2 (64/73, 87.7%) mRNA-1273 (9/73, 12.3%) |
Humoral Seroconversion 5/51 (10%) individuals with RA on immune-modifying therapy had detectable antibodies post-vaccine vs 18/20 (90%) controls (p < 0·001) Spike specific IgG titres were lower in patients with RA on immune-modifying therapy (median 0.4 U/ml, IQR 0.4–2.13) vs healthy controls (99.2 U/ml, 24.8–172, p < 0.0001) at 3 weeks post-vaccination |
Humoral Seroconversion Spike specific IgG titres were lower in individuals with RA (657 U/ml, IQR 188–2500) vs healthy controls (2500 U/ml, IQR 2500–2500, p < 0.0001) at 2 weeks after the second vaccination 45/51 (88%) individuals with RA on immune-modifying therapy had detectable antibody titres post-second vaccine. Of 6 individuals who did not have detectable antibodies, 4 were receiving JAKi monotherapy or combination therapy, 1 methotrexate/prednisolone co-therapy and 1 methotrexate/prednisolone co-therapy. Neutralising A neutralising humoral response was detected in 13/16 (81%) individuals on standard systemic therapy, 17/18 (94%) on cytokine targeted biologic therapy, 4/5 (80%) on abatacept, and 8/12 (67%) on JAKi therapy |
| Ruddy et al. [37] |
Rheumatological disease (n = 404) including RA, ankylosing spondylitis, PsA, reactive arthritis, SLE, Sjogren’s syndrome, myositis, systemic sclerosis and vasculitis No controls |
Median age: 44 years Gender: 385 (96%) female Ethnicity: 367 (91%) White |
Standard systemic Azathioprine, ciclosporin, dimethyl fumarate, hydroxychloroquine, leflunomide, methotrexate, mycophenolate mofetil, sirolimus, sulfasalazine and tacrolimus Targeted Abatacept, anakinra, belimumab, guselkumab, IL-6i, IL-17i, JAKi, rituximab, TNFi and ustekinumab |
BNT162b2 (198/404, 49%) mRNA-1273 (204/404, 51%) |
N/A |
Humoral Seroconversion 378/404 (94%) of individuals with rheumatological disease seroconverted at a median of 29 days after 2nd dose A greater proportion of those receiving TNFi had detectable antibodies (100%), vs those receiving mycophenolate (73%, p < 0.001), rituximab (26%, p < 0.001) or glucocorticoids (82%, p < 0.001) or those with a diagnosis of myositis (79%, p = 0.01) Lower median antibody titres in individuals receiving mycophenolate mofetil (8 U/mL) and rituximab (< 0.4 U/mL) vs individuals receiving glucocorticoid monotherapy (> 250 U/mL) |
| Seree-aphinan et al. [38] |
Cases: Individuals with pemphigus, psoriasis and chronic spontaneous urticaria who are receiving immune-modifying therapy (n = 14) Controls: individuals (with acne, melasma, androgenetic alopecia, seborrheic keratosis) who are not receiving immune-modifying therapy (n = 18) |
Mean age: Controls – 45 years Cases – 44 years Gender: Controls – 11 (61%) female Cases – 10 (71%) female Ethnicity: Not included |
Standard systemic Azathioprine, ciclosporin, methotrexate, mycophenolate mofetil and prednisone Targeted Ixekizumab, omalizumab and secukinumab |
CoronaVac (Sinovac) |
N/A |
Humoral Seroconversion No individuals (0/6, 0%) taking azathioprine, ciclosporin, mycophenolate mofetil, or moderate-to-high dose corticosteroids seroconverted 4 weeks post-second vaccine. 7/8 (87.5%) individuals on low dose methotrexate, low dose systemic corticosteroids, or biologics seroconverted Neutralising Patients on azathioprine, ciclosporin, mycophenolate mofetil, or moderate-to-high dose corticosteroids had lower neutralizing activity vs those receiving low dose methotrexate, low dose systemic corticosteroids or biologics |
| Seyahi et al. [39] |
IMIDs (n = 104) including RA, SLE, Sjogren’s syndrome, polymyositis, ankylosing spondylitis, PsA or psoriasis, Behcet’s syndrome, vasculitis, Familial Mediterranean Fever, IBD. This cohort comprises hospital workers (n = 82) and elderly individuals aged 65 and above (n = 22) Healthy controls (n = 347), comprising hospital workers (n = 300) and elderly individuals (n = 47) |
Mean age: Hospital workers with IMIDs – 42 years Elderly group with IMIDs – 71 years Control hospital workers – 71 years, Control elderly group – 71 years Gender: Hospital workers with IMIDs – 53 (64.6%) female Elderly group with IMIDs – 16 (72.7%) female Control hospital workers – 193 (64.3%) female Control elderly group – 24 (51.1%) female Ethnicity: Not included |
Standard systemic Azathioprine, leflunomide, methotrexate mycophenolate mofetil, prednisone, sulfasalazine and tacrolimus Targeted Anakinra, interferon-alpha, rituximab, secukinumab, TNFi and tocilizumab |
CoronaVac (Sinovac) |
N/A |
Humoral Seroconversion A lower proportion of hospital workers with IMIDs had detectable antibodies vs hospital worker controls (92.7% vs 99.7%, p < 0.001) at least 21 days following the second vaccination. A lower proportion of elderly individuals with IMIDs had detectable antibodies vs elderly controls (77.3% vs 97.9%, p = 0.011) at least 21 days post-second vaccine A lower proportion of individuals receiving rituximab (1/7, 14.3%) had detectable antibodies vs those receiving other targeted therapy (22/25, 88%), standard therapy (25/27, 92.6%) or no treatment (29/29, 100%) |
| Simon et al. [40] |
IMIDs including SpA, RA, IBD, psoriasis, SLE, systemic sclerosis, IgG4-related diseases, GCA, periodic fever syndromes, granulomatosis with polyangiitis and polymyalgia rheumatica (n = 84) Healthy controls (n = 182) |
Mean age: IMIDs – 53 years Healthy cohort – 41 years Gender: IMIDs – 55 (65.5%) female Healthy controls–104 (57.1%) female Ethnicity: Not included |
Standard systemic Hydroxychloroquine, methotrexate, sulfasalazine Targeted IL-17/23i, JAKi and TNFi |
BNT162b2 |
Humoral Seroconversion 79/84 (94%) individuals with IMIDs on immune-modifying therapy vs 182/182 controls (100%) had detectable antibodies at 11 days post-vaccine (p = 0.003) |
Humoral Seroconversion 79/84 (94%) individuals with IMIDs on immune-modifying therapy vs all (100%) controls had detectable antibodies up to 39 days post-second vaccine (p = 0.003). No difference between individuals with IMIDs on standard or targeted therapy or no treatment Neutralising 76/84 (90.5%) individuals with IMIDs on immune-modifying therapy vs 181/182 (99.5%) controls had neutralising antibodies (p = 0.0008) |
| Wieske et al. [41] |
IMIDs on immune-modifying therapy, including vasculitis, Sjogren’s syndrome, PMR, GCA, vitiligo, pemphigus, psoriasis, auto-immune hepatitis, auto-immune sclerosing cholangitis, chronic inflammatory demyelinating polyneuropathy, multifocal motor neuropathy, inflammatory myositis, neuromyelitis optica spectrum disorder (n = 1692) IMIDs not on immune-modifying therapy (n = 419) Healthy controls (n = 174) |
Mean age: 50 years overall Gender: 1470 (62.8%) female overall Ethnicity: Not included |
Standard systemic Ciclosporin, hydroxychloroquine, methotrexate, mycophenolate mofetil and sulfasalazine Targeted Abatacept, anti-CD20, belimumab, dupilumab, JAKi, IL-17i, IL-23i, interferon-beta, natalizumab, omalizumab, tocilizumab, TNFi, ustekinumab and vedolizumab Others: Intravenous or subcutaneous immunoglobulin, purine antagonists, and sphingosine-1-phosphate receptor modulators |
ChAdOx1 nCoV-19 (254/2339, 11%) BNT162b2 (1324/2339, 57%) mRNA-1273 (712/2339, 30%) Ad.26.COV2.S (49/2339, 2%) |
N/A |
Humoral Seroconversion 39/128 (30·5%) on anti-CD20 therapy seroconverted vs 479/493 (97·2%) controls Compared with controls, relative risk of seroconversion post-second vaccine on anti-CD20 therapy was 0.32 (95% CI 0·19–0·49), while the relative risks for other immune-modifying drugs were not significantly reduced For those who seroconverted, anti-CD20 was associated with substantial reductions in antibody titres. TNFi, dupilumab, intravenous and subcutaneous immunoglobulin, and methotrexate were associated with moderate reductions in antibody titres Neutralisation Neutralisation capacity of individuals on immune-modifying monotherapy was similar to controls |
| Wong et al. [42] |
IBD (n = 48) Vaccinated healthcare workers (HCWs, n = 14) Healthy controls (n = 29) |
Mean age: IBD – 49 years HCWs – 35 years Healthy controls – 32 years Gender: IBD – 25 (52%) female HCWs -7 (50%) female Healthy controls – 11 (37.9%) female Ethnicity: IBD – 42 (87.5%) White HCWs – 10 (71.4%) White Healthy controls – 18 (62.1%) White |
Targeted Guselkumab, TNFi, vedolizumab and vedolizumab with thiopurine |
BNT162b2 (54/91, 59.3%) mRNA-1273 (37/91, 40.7%) |
N/A |
Humoral Seroconversion 26/26 (100%) individuals with IBD on targeted therapy had detectable antibodies at 8–18 days post-second vaccine. Vedolizumab was associated with lower spike specific IgG titres vs controls (p = 0.0043) |
IMIDs immune-mediated inflammatory diseases, PsA psoriatic arthritis, RA rheumatoid arthritis, SLE systemic lupus erythematosus, TNFi tumour necrosis factor inhibitor, JAKi Janus kinase inhibitor, IL-6i interleukin-6 inhibitor, ANCA antineutrophil cytoplasmic antibodies, PMR polymyalgia rheumatica, IFN-γ interferon-γ, IL-17i interleukin-17 inhibitor, SpA spondyloarthritis, IL-23i interleukin-23 inhibitor, PDE4i phosphodiesterase 4 inhibitor, IQR interquartile range, 95% CI 95% confidence interval, IBD inflammatory bowel disease, GCA giant cell arteritis, HCWs healthcare workers
Immune Response to the 1st Dose of COVID-19 Vaccine
Eight of twenty-five included studies investigated the effects of immune-modifying therapy on the immune response to a first dose of COVID-19 vaccine [18, 20, 22, 24, 32, 33•, 36, 40]. All eight studies evaluated the impact of immune-modifying therapy on seroconversion and one study additionally analysed neutralisation and cellular responses [33•]. Assessment of the serological response to vaccination (i.e. IgG antibody specific to the SARS-CoV-2 S protein) is highly represented due to the accessibility and convenience of the antibody assay.
Seroconversion
The Standard Systemic Immune-Modifying Therapy Methotrexate May Impair Seroconversion Following the First Vaccine Dose More Than Targeted Therapies Such As TNF Inhibitors
All 8 studies analysing seroconversion following the first vaccine dose showed that individuals who were receiving immune-modifying therapy were less likely to mount a detectable antibody response compared to healthy controls [18, 22, 24, 32, 33, 36 40]. Use of standard systemic immune-modifying therapies had a greater impact on seroconversion than targeted therapies. For example, Boyarsky et al. found that 16 of 17 (94%) individuals receiving TNF-inhibitor biologic therapy had detectable antibodies, compared to 55 of 85 (65%) individuals receiving standard systemic therapy [22]. Specifically, methotrexate was associated with lower seroconversion rates post-vaccination compared with targeted biologics such as TNF-inhibitors [18, 20, 22, 24, 33•]. For example, Al-Janabi et al. (n = 120) found that use of methotrexate was associated with a reduced odds of a detectable antibody response compared with targeted therapies (adjusted odds ratio 0.31) [18]. Bugatti et al. (n = 140) showed that seroconversion rates decreased from 85% among individuals who were not receiving methotrexate or glucocorticoids to 33% among those receiving both therapies [24]. Our own study (individuals with psoriasis, n = 84; healthy controls, n = 17) similarly found that individuals receiving methotrexate had lower seroconversion rates (7/15, 47%) compared to those receiving targeted biologic therapy (53/62, 85%, p = 0.0001) or healthy controls (17/17, 100%, p = 0.0001) [33•].
Rituximab Attenuates Seroconversion Following the First Vaccine Dose Compared to Other Immune-Modifying Therapies
Rituximab has a marked effect on seroconversion after the first vaccine dose: Boyarsky et al. found that a lower proportion of individuals receiving rituximab developed an antibody response (2/6, 33%), compared to individuals receiving TNF-inhibitors (16/17, 94%) or standard systemic therapy including methotrexate (10/13, 77%), leflunomide (2/4, 50%), sulfasalazine (4/5, 80%) and hydroxychloroquine (27/37, 73%) [22].
Individuals Receiving Immune-Modifying Therapy Have Lower Median Spike-Specific IgG Titres Following the First Vaccine Dose Compared to Healthy Controls
Individuals receiving either standard or targeted systemic immune-modifying therapy who successfully seroconverted after the first vaccine dose had evidence of lower median antibody titres against S protein compared to healthy controls [34•, 36]. For example, Rubbert-Roth et al. found that antibody titres against S protein at 3 weeks after the first vaccine dose were significantly lower in individuals receiving standard or targeted immune-modifying therapy (median titre 0·4 U/mL [IQR 0.4–2.13], n = 53) compared to healthy controls (median titre 99·2 U/mL [IQR 24.8–172], n = 20, p < 0.0001) [36].
Neutralisation Response
Methotrexate Is Associated with Lower Median Neutralisation Titres Following the First Vaccine Dose Compared to Targeted Immune-Modifying Therapy
In our study of neutralisation response to the first dose of COVID-19 vaccine BNT162b2, individuals receiving targeted biologic therapy (TNFi, IL-17i or IL-23i) had similar neutralisation titres against wild-type or Alpha SARS-CoV-2 compared to healthy controls [33•]. Methotrexate use, however, was associated with lower median neutralisation titres (ID50 129 [IQR 40–236]) compared to either healthy controls (ID50 317 [IQR 213–487], p = 0.0032) or patients receiving biologic therapy (ID50 269 [IQR 141–418], p = 0·011) [33•].
Cellular Response
Methotrexate or Targeted Immune-Modifying Therapy Does Not Significantly Impair Cellular Responses Following the First Vaccine Dose
Our study also analysed cellular responses, which involved quantifying T cells secreting interferon-γ, IL-2 or IL-21 in response to stimulation with two peptide pools spanning the entire length of the S protein [33•]. Methotrexate or targeted biologics did not impair the cellular response to the first dose of COVID-19 vaccine BNT162b2 as all study groups including the healthy control group showed comparable spike-specific T-cell responses.
Immune Response to the 2nd Dose of COVID-19 Vaccine
Twenty-one studies analysed the effects of immune-modifying therapy on the immune response to two doses of COVID-19 vaccine [19–21, 23, 25–32, 34•, 35–42]. All studies analysed seroconversion following the second vaccine dose. Ten and four studies additionally analysed neutralisation and cellular responses, respectively.
Seroconversion
The Majority of Individuals Receiving Standard Systemic or Targeted Immune-Modifying Therapy (Except Rituximab) Have Evidence of Successful Seroconversion Following the Second Vaccine Dose
The second COVID-19 vaccine dose led to successful seroconversion in the majority of individuals receiving either standard or targeted immune-modifying therapy (excluding rituximab) [19–21, 23, 25, 27–29, 31, 34•, 35–42]. One study showed that only 10 of 20 (50%) patients with IMIDs who were receiving methotrexate seroconverted compared with 179/182 (98%) healthy controls; however, this involved a limited patient sample, and the mean age of healthy controls (41 years) was lower than those receiving methotrexate (55 years) [30]. Although data are limited, prior studies indicate that JAK inhibitors (JAKi) do not impair seroconversion: Furer et al. and Braun-Moscovici et al. found that 19/21 (90%) and 9/9 (100%) individuals receiving JAKi successfully seroconverted, respectively, after the second vaccine dose [23, 28].
Rituximab Impairs Seroconversion After the Second Vaccine Dose Compared to Other Immune-Modifying Therapies
All studies assessing rituximab showed that a lower proportion of individuals receiving rituximab seroconverted after the second vaccine dose compared to those who were receiving standard systemic or other targeted immune-modifying therapy, or healthy controls (at 2–4 weeks post second vaccine dose) [19–21, 23, 25, 27–32, 33•, 34•, 35–39, 41]. Seroconversion rates in individuals receiving rituximab were as low as 14.3% after the second COVID-19 vaccine [39]. Vaccinations were administered between 1.5 and 12 months after rituximab treatment. The degree of B cell recovery at the time of vaccination correlated with the extent of humoral vaccine response; i.e. a more favourable humoral response was achieved when there was a greater time interval between rituximab treatment and vaccination [27, 28]. For example, Furer et al. (n = 86 on rituximab) found that 50% of individuals seroconverted when their vaccination was 1-year after rituximab treatment, compared with less than 20% of those who were vaccinated within 6 months after rituximab treatment [28].
Individuals Receiving Immune-Modifying Therapy Have Lower Spike-Specific IgG Titres Following the Second Vaccine Dose, Compared to Healthy Controls
Individuals receiving immune-modifying therapy had lower titres of spike-specific IgG compared to healthy controls [28, 29]. For example, Furer et al. identified mean antibody titres of 132.9 BAU/ml in individuals with rheumatological diseases who were receiving immune-modifying therapy (including methotrexate, mycophenolate mofetil, leflunomide, hydroxychloroquine, TNFi, IL-6i, IL-17i, rituximab, abatacept and JAKi, n = 686) compared to 218.6 BAU/mL in the healthy control group (n = 121, p < 0.0001) [28]. Furer et al. also found that use of methotrexate as monotherapy or in combination with other treatments was associated with lower titres of spike-specific IgG compared with controls. Similarly, our study identified lower median spike-specific IgG titres following the second vaccine dose in those receiving methotrexate (EC50 1751 [IQR 468–4976]) compared with those receiving targeted biologics (EC50 1816 [IQR 787–3534], p = 0.65) or healthy controls (EC50 2749 [IQR 867–4770], p = 0.2), albeit not statistically significant [34•]. Wieske et al. (n = 26 on JAKi; n = 57 on dupilumab) reported that use of JAKi or dupilumab was associated with a moderate decrease in antibody titres compared to healthy controls (n = 174) [41].
Despite emerging research on longer-term antibody responses to COVID-19 vaccines in the general population, there remains a paucity of knowledge on the durability of antibody responses in individuals receiving immune-modifying treatment [43]. Data from the general population highlight that the humoral immune response to the second COVID-19 vaccination wanes over time. For example, one study in Estonia involving 122 infection-naïve individuals without significant comorbidities (age range 21–69 years) who were not receiving immune-modifying therapies showed a progressive decline of spike-specific IgG levels at 12 weeks (5226 AU/mL) and 6 months (1383 AU/mL) following the second COVID-19 vaccine [43]. At 6 months after the second vaccine, spike-specific IgG levels were similar to levels in people who had received only one vaccine dose or in those with previous COVID-19 infection (and no vaccination). A large-scale UK study of individuals infected with the Omicron variant (n = 86,774), Delta variant (n = 204,154) and uninfected controls (n = 1,572,621) found that 2 vaccine doses (ChAdOx1 nCoV-19 or BNT162b2) were more effective at protecting against symptomatic disease arising from the Delta variant compared to the Omicron variant [44]. Vaccine effectiveness waned rapidly, with limited effects detected after 20 weeks of the second dose of either vaccine. These general population data underscore the importance of subsequent vaccine doses, particularly in the context of newer variants of concern.
Neutralisation Response
The Majority of Individuals Receiving Immune-Modifying Therapy Develop a Neutralising Response After the Second Vaccine Dose
In ten studies where neutralisation was investigated [23, 25–27, 29, 34•, 36, 38, 40, 41], the majority of individuals receiving immune-modifying therapy developed a neutralising response after the second vaccine dose (range 63–100%, with the exception of those receiving rituximab); however, neutralisation titres were lower compared to healthy controls in 3 studies [27, 29, 38]. Our own study (individuals with psoriasis, n = 67; healthy controls, n = 15) showed that all study participants had detectable neutralising antibodies against wild-type, Alpha and Delta SARS-CoV-2 variants following the second vaccine dose, and there were higher neutralising antibody titres after the second dose compared to the first [34•]. Neutralisation activity against the Alpha variant was similar in individuals receiving methotrexate (median ID50 440 [IQR 101–935]) compared to those receiving targeted therapy (median ID50 453 [IQR 233–955], p = 0·97) or healthy controls (median ID50 491 [IQR 264–1227], p = 0·63). With respect to the Delta variant, neutralisation activity was also detected at similar levels across all groups, i.e. in individuals receiving methotrexate (median ID50 856 [IQR 77–1476] versus those receiving targeted therapy (median ID50 469 [IQR 232–1309], p = 0·76) or healthy controls (median ID50 863 [IQR 225–1297], p = 0·49) [34•]. In contrast, in a smaller study (n = 14), Seree-aphinan et al. found that individuals receiving azathioprine, ciclosporin, mycophenolate mofetil or moderate-to-high dose corticosteroids monotherapy had a lower neutralising response compared to those who received low dose methotrexate or low dose systemic corticosteroids or biologics [38].
Rituximab Impairs Neutralisation Responses to the Second Vaccine Dose Compared to Other Immune-modifying Therapies
Patients receiving rituximab were less likely to develop detectable neutralising antibodies after the second vaccine dose compared to controls or those receiving other immune-modifying therapies. For example, Deepak et al. (individuals with IMIDs, n = 133; healthy controls, n = 53) found that neutralisation titres in individuals with IMIDs (including RA, spondyloarthritis, uveitis, SLE, vasculitis, Sjogren syndrome, multiple sclerosis and IBD) who were receiving anti-CD20 therapy were lower compared with those who were not receiving anti-CD20 therapy (half-maximal dilution titres 723 vs 2445, respectively) [27].
Cellular Responses
Methotrexate May Impair the Cellular Immune Response to the Second Vaccine Dose
In comparison to data available on humoral responses, there is a relative paucity of data on cellular immune responses to the COVID-19 vaccine [45]. This represents an important knowledge gap because studies indicate that a robust cellular response is critical in the protection against severe COVID-19 by enabling accelerated viral clearance [17]. SARS-CoV-2-specific T cell responses may help to prevent infection and may also support the development of robust immunological memory since CD4 spike-specific T cell responses promote antibody generation, with follicular helper T cells correlating with long-term/durable humoral immunity [45]. Furthermore, unlike humoral responses, which seem to be evaded by many variants of concern, cellular responses seem to show stronger cross-protection highlighting their importance in the face of ongoing viral evolution [46].
The four studies identified in this review that investigated cellular responses in individuals receiving immune-modifying therapy yielded broadly similar findings [21, 30, 34•, 35]. For example, our own study found that a lower proportion of individuals receiving methotrexate (8/13 [62%], 95% CI 32–86) had detectable T-cell responses following the second vaccine dose compared to those receiving targeted biologics (37/50 [74%], 95% CI 60–85; p = 0·38) or controls (14/14 [100%], 95% CI 77–100%, p = 0·022) [34•]. Similarly, Haberman et al. (individuals with IMIDs, n = 51; healthy controls, n = 26) reported attenuated activated CD8+ T-cell responses in methotrexate-treated individuals following the second COVID-19 vaccine dose compared to healthy controls or individuals with IMIDs not on methotrexate [30]. Of note, Moor et al. found that individuals receiving B cell targeted biologics (rituximab or ocrelizumab) also had reduced T cell responses compared to healthy controls (14/44 [32%] vs 22/25 [88%], p < 0.001) [35].
Other Factors that May Impact the Immune Response to the COVID-19 Vaccine in the Context of Immune-Modifying Therapy
Timing of Immune Response Readout Relative to Vaccination
The majority of studies in this review analysed immune responses to COVID-19 vaccines at 2 to 6 weeks following the first or second dose of the vaccine (Table 2). A smaller number of studies analysed immune responses at 7–8 days [19, 29] or up to 10 weeks following the second dose [31, 32].
Immune Response to Different SARS-CoV-2 Variants
Of twenty-five studies included in this review, only four analysed the immune response against different SARS-CoV-2 variants [25, 26, 33•, 34•]. Dailey et al. (n = 33) found similar neutralising antibody responses following vaccination in an IBD population against wild-type and Alpha variants [26]. Our studies analysed neutralising activity against wild type, Alpha and Delta variants [33•, 34•]. Neutralising activity against wild-type SARS-CoV-2 was significantly lower after the first vaccine dose in patients receiving methotrexate compared to controls, but was preserved in those receiving targeted biologics. Neutralising titres against the Alpha variant were similarly low in all study participants [33•]. We subsequently found that neutralising antibody titres against wild-type, Alpha and Delta SARS-CoV-2 variants following the second vaccine dose were similar in patients receiving methotrexate, targeted biologics, and healthy controls [34•]. Chen et al. (individuals with IMIDs, n = 75; healthy controls, n = 25) also found no statistically significant differences in antibody responses in their IMID cohort against wild type, Alpha, Beta and Delta variants at 3 months following a second dose of vaccine [25]. Importantly, there remains a paucity of data on newer variants of concern. This remains an area of active investigation since the impact of a lower titre antibody vaccine response in the context of immune-modifying therapy is likely to be exacerbated when considering protection against newer variants such as Omicron [44].
Omission of Immune-Modifying Therapy Around the Time of Vaccination
Prior studies found that temporary discontinuation of methotrexate for 2–4 weeks after seasonal influenza vaccination in patients with rheumatoid arthritis led to greater antibody titres [47, 48]. There has thus been active investigation into whether the omission of methotrexate doses around the time of COVID-19 vaccination is beneficial. The VROOM trial was a UK open-label two-arm parallel-group multicentre (n = 26 sites) randomised controlled superiority trial studying the effects on COVID-19 booster vaccine responses of temporarily suspending methotrexate for 2 weeks post-vaccination versus continued methotrexate [49•]. The study included 254 adults with IMIDs (127 in the ‘continue methotrexate’ group and 127 in the ‘suspend methotrexate’ group). Their mean age was 59 years, 155 (61%) were female, 130 (51%) had rheumatoid arthritis and 86 (34%) had psoriasis with or without arthritis. After 4 weeks, the mean S1-RBD antibody titre was 22,750 U/mL (95% CI 19,314–26,796) in the ‘suspend methotrexate’ group versus 10,798 U/mL (95% CI 8970–12 997) in the ‘continue methotrexate’ group (geometric mean ratio 2·19, 95% CI 1·57–3·04; p < 0·0001). Thus, a 2-week interruption of methotrexate treatment post-booster vaccine may lead to increased vaccine efficacy and greater duration of protection [49•]. A greater proportion of participants in the ‘suspend methotrexate’ group self-reported at least one disease flare in the first 4 weeks post-vaccination compared to the ‘continue methotrexate’ group (56% vs 31%); however, most flares were self-managed in both groups. Further research into the temporary suspension of other standard and targeted immune-modifying drugs around the time of vaccination is warranted.
Total Number of Vaccine Doses
While there remains a paucity of data on the immune response to more than two COVID-19 vaccine doses, there are emerging reports. For example, Schmiedeberg et al. (n = 17) found that individuals with rheumatoid arthritis who were receiving standard systemic and/or targeted immune-modifying therapy who had not seroconverted after the first two COVID-19 vaccine doses mounted a significant antibody response following the third dose [50]. Wieske et al. showed that a third vaccine dose successfully boosted seroconversion rates in individuals receiving mycophenolate mofetil combination treatments, from 52.6% after the second vaccination to 89.5% after the third [41]. However, the study found that use of anti-CD20 biologics continued to impair humoral responses, with seroconversion rates of 36.9% and 45.6% after the second and third vaccine doses, respectively [41]. In further support, Simon et al. found that while a third vaccine enabled seroconversion in some individuals on rituximab who had not responded to previous vaccine doses, seroconversion rates remained lower in this group compared to previous non-responders who were not receiving rituximab (6/33 [18.2%] vs 26/33 [78.8%], respectively) [51].
With respect to clinical effectiveness, a study by Shen et al. using electronic health records in the Michigan Medicine US healthcare system (n = 154,519) found that individuals receiving immune-modifying drugs (standard systemic and/or targeted immune-modifying therapy) who had a third vaccine dose had a lower incidence of SARS-CoV-2 infection compared to those who did not have a third dose [52•]. Immune responses were not studied. Additionally, Risk et al.’s analysis of Michigan Medicine data (n = 168,414) indicated that three doses of BNT162b2 or mRNA-1273 vaccine was strongly protective against COVID-19-related hospitalisation in both individuals receiving immune-modifying therapy (vaccine effectiveness 87%, 95% CI 74–93) and those who were immunocompetent (92%, 95% CI 87–95) [53]. Further large-scale clinical effectiveness data from populations receiving immune-modifying therapies are awaited.
Conclusions
SARS-CoV-2 has had a devastating effect around the world, with vaccinations being paramount in the public health strategy against COVID-19. While vaccination programmes have seen great success, there are still limited data on the clinical effectiveness of these vaccines in the global population who are receiving treatment with immune-modifying drugs, including those with skin IMIDs [54].
Research to date indicates that while individuals receiving immune-modifying therapy are more likely to have attenuated humoral responses to a single dose of COVID-19 vaccine compared to healthy controls, this may be improved by a complete course of vaccination. Hence, individuals receiving immune-modifying treatments should be encouraged to take up a complete vaccine course to mitigate their risk against severe COVID-19 outcomes [55]. Of specific note are B cell targeted biologics such as rituximab, which markedly impair the humoral response to both the first and second COVID-19 vaccination. Although this remains an area of active research, the impact of rituximab on vaccine responses may be improved by increasing the time interval between the rituximab treatment and vaccination [56]. Clinicians should also consider temporary cessation of methotrexate following vaccination given the emerging trial data [49•].
There remains a paucity of data on cellular immune responses, with the few available studies indicating lower responses to two vaccine doses in individuals receiving immune-modifying therapies compared to healthy controls, which may impact the durability of immune responses. Research in large patient populations on the longevity/kinetics of the complex humoral and cellular response to subsequent vaccine doses, including against newer variants of concern, is now warranted, in addition to data on immune correlates of vaccine clinical effectiveness.
Funding
Dr Mahil is supported by a National Institute for Health and Care Research (NIHR) Advanced Fellowship (NIHR302258).
Compliance with Ethical Standards
Conflict of Interest
Su-Yi Liew declares that she has no conflict of interest. Catherine Smith reports grants from Abbvie, grants from Sanofi, grants from Novartis, and grants from Pfizer, outside the submitted work. Satveer Mahil reports departmental income from Abbvie, Almirall, Eli Lilly, Novartis, Sanofi, UCB, outside the submitted work. Timothy Tree reports grants from GlaxoSmithKline, Sanofi and Imcyse SA, and consultancy fees from GlaxoSmithKline, Novartis, UCB and Quell Therapeutics, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Covid-19 in Dermatology
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.van Aalst M, Langedijk A, Spijker R, de Bree G, Grobusch M, Goorhuis A. The effect of immunosuppressive agents on immunogenicity of pneumococcal vaccination: a systematic review and meta-analysis. Vaccine. 2018;36:5832–5845. doi: 10.1016/j.vaccine.2018.07.039. [DOI] [PubMed] [Google Scholar]
- 2.Bemben N, Berg M. Efficacy of inactivated vaccines in patients treated with immunosuppressive drug therapy. Pharmacother J Human Pharmacol Drug Ther. 2022;42:334–342. doi: 10.1002/phar.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng C, Lu C, Chang Y, Sun Y, Chu H, Lee C, et al. Effectiveness of the WHO-authorized COVID-19 vaccines: a rapid review of global reports till 30 June 2021. Vaccines. 2021;9:1489. doi: 10.3390/vaccines9121489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall V, Foulkes S, Insalata F, et al. Protection against SARS-COV-2 after covid-19 vaccination and previous infection. N Engl J Med. 2022;386:1207–1220. doi: 10.1056/NEJMoa2118691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rennert L, Ma Z, McMahan CS, Dean D. Effectiveness and protection duration of COVID-19 vaccines and previous infection against any SARS-COV-2 infection in young adults. Nat Commun. 2022 doi: 10.1038/s41467-022-31469-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andersen K, Bates B, Rashidi E, et al. Long-term use of immunosuppressive medicines and in-hospital COVID-19 outcomes: a retrospective cohort study using data from the National COVID Cohort Collaborative. Lancet Rheumatol. 2022;4:e33–e41. doi: 10.1016/S2665-9913(21)00325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Craven J. COVID-19 vaccine tracker. Raps.org. 2022. https://www.raps.org/news-and-articles/news-articles/2020/3/covid-19-vaccine-tracker. Accessed 13 Jun 2022.
- 8.Assets.publishing.service.gov.uk. 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1057798/Greenbook-chapter-14a-28Feb22.pdf. Accessed 2 May 2022.
- 9.Oliver SE, Wallace M, See I, et al. Use of the janssen (Johnson & Johnson) COVID-19 vaccine: Updated interim recommendations from the Advisory Committee on Immunization Practices – United States, December 2021. MMWR Morb Mortal Wkly Rep. 2022;71:90–95. doi: 10.15585/mmwr.mm7103a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rubin R. Despite its fan base, newly authorized “traditional” Novavax Covid-19 vaccine is having trouble gaining a foothold in the US. JAMA. 2022 doi: 10.1001/jama.2022.13661. [DOI] [PubMed] [Google Scholar]
- 11.Mascellino M, Di Timoteo F, De Angelis M, Oliva A. Overview of the main anti-SARS-CoV-2 vaccines: mechanism of action, efficacy and safety. Infect Drug Resist. 2021;14:3459–3476. doi: 10.2147/IDR.S315727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voysey M, Clemens S, Madhi S, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rondaan C, Furer V, Heijstek M, et al. Efficacy, immunogenicity and safety of vaccination in adult patients with autoimmune inflammatory rheumatic diseases: a systematic literature review for the 2019 update of EULAR recommendations. RMD Open. 2019;5:e001035. doi: 10.1136/rmdopen-2019-001035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sadarangani M, Marchant A, Kollmann T. Immunological mechanisms of vaccine-induced protection against COVID-19 in humans. Nat Rev Immunol. 2021;21:475–484. doi: 10.1038/s41577-021-00578-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Addetia A, Crawford K, Dingens A, Zhu H, Roychoudhury P, Huang M, et al. Neutralizing antibodies correlate with protection from SARS-CoV-2 in humans during a fishery vessel outbreak with a high attack rate. J Clin Microbiol. 2020 doi: 10.1128/jcm.02107-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salimi-Jeda A, Abbassi S, Mousavizadeh A, Esghaie M, Bokharaei-Salim F, Jeddi F, et al. SARS-CoV-2: Current trends in emerging variants, pathogenesis, immune responses, potential therapeutic, and vaccine development strategies. Int Immunopharmacol. 2021;101:108232. doi: 10.1016/j.intimp.2021.108232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bertoletti A, Tan A, Le Bert N. The T-cell response to SARS-CoV-2: kinetic and quantitative aspects and the case for their protective role. Oxford Open Immunol. 2021 doi: 10.1093/oxfimm/iqab006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Janabi A, Littlewood Z, Griffiths C, Hunter H, Chinoy H, Moriarty C, et al. Antibody responses to single-dose SARS-CoV-2 vaccination in patients receiving immunomodulators for immune-mediated inflammatory disease. Br J Dermatol. 2021;185:646–648. doi: 10.1111/bjd.20479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ammitzbøll C, Bartels L, Bøgh Andersen J, et al. Impaired antibody response to the BNT162b2 messenger RNA coronavirus disease 2019 vaccine in patients with systemic lupus erythematosus and rheumatoid arthritis. ACR Open Rheumatol. 2021;3:622–628. doi: 10.1002/acr2.11299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boekel L, Steenhuis M, Hooijberg F, et al. Antibody development after COVID-19 vaccination in patients with autoimmune diseases in the Netherlands: a substudy of data from two prospective cohort studies. Lancet Rheumatol. 2021 doi: 10.1016/s2665-9913(21)00222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bonelli M, Mrak D, Perkmann T, Haslacher H, Aletaha D. SARS-CoV-2 vaccination in rituximab-treated patients: evidence for impaired humoral but inducible cellular immune response. Ann Rheum Dis. 2021;80:1355–1356. doi: 10.1136/annrheumdis-2021-220408. [DOI] [PubMed] [Google Scholar]
- 22.Boyarsky B, Ruddy J, Connolly C, Ou M, Werbel W, Garonzik-Wang J, et al. Antibody response to a single dose of SARS-CoV-2 mRNA vaccine in patients with rheumatic and musculoskeletal diseases. Ann Rheum Dis. 2021;80:1098–1099. doi: 10.1136/annrheumdis-2021-220289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braun-Moscovici Y, Kaplan M, Braun M, Markovits D, Giryes S, Toledano K, et al. Disease activity and humoral response in patients with inflammatory rheumatic diseases after two doses of the Pfizer mRNA vaccine against SARS-CoV-2. Ann Rheum Dis. 2021;80:1317–1321. doi: 10.1136/annrheumdis-2021-220503. [DOI] [PubMed] [Google Scholar]
- 24.Bugatti S, De Stefano L, Balduzzi S, et al. Methotrexate and glucocorticoids, but not anticytokine therapy, impair the immunogenicity of a single dose of the BNT162b2 mRNA COVID-19 vaccine in patients with chronic inflammatory arthritis. Ann Rheum Dis. 2021;80:1635–1638. doi: 10.1136/annrheumdis-2021-220862. [DOI] [PubMed] [Google Scholar]
- 25.Chen RE, Gorman MJ, Zhu DY, et al. Reduced antibody activity against SARS-COV-2 B.1.617.2 delta virus in serum of mRNA-vaccinated individuals receiving tumor necrosis factor-α inhibitors. Med. 2021 doi: 10.1016/j.medj.2021.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dailey J, Kozhaya L, Dogan M, et al. Antibody responses to SARS-CoV-2 after infection or vaccination in children and young adults with inflammatory bowel disease. Inflamm Bowel Dis. 2021 doi: 10.1093/ibd/izab207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deepak P, Kim W, Paley M, et al. Effect of immunosuppression on the immunogenicity of mRNA vaccines to SARS-CoV-2. Ann Intern Med. 2021;174:1572–1585. doi: 10.7326/M21-1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Furer V, Eviatar T, Zisman D, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis. 2021;80:1330–1338. doi: 10.1136/annrheumdis-2021-220647. [DOI] [PubMed] [Google Scholar]
- 29.Geisen U, Berner D, Tran F, et al. Immunogenicity and safety of anti-SARS-CoV-2 mRNA vaccines in patients with chronic inflammatory conditions and immunosuppressive therapy in a monocentric cohort. Ann Rheum Dis. 2021;80:1306–1311. doi: 10.1136/annrheumdis-2021-220272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haberman RH, Herati R, Simon D, et al. Methotrexate hampers immunogenicity to BNT162B2 mRNA COVID-19 vaccine in immune-mediated inflammatory disease. Ann Rheum Dis. 2021;80:1339–1344. doi: 10.1136/annrheumdis-2021-220597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kappelman M, Weaver K, Boccieri M, et al. Humoral immune response to messenger RNA COVID-19 vaccines among patients with inflammatory bowel disease. Gastroenterology. 2021;161:1340–1343.e2. doi: 10.1053/j.gastro.2021.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kennedy N, Lin S, Goodhand J, et al. Infliximab is associated with attenuated immunogenicity to BNT162b2 and ChAdOx1 nCoV-19 SARS-CoV-2 vaccines in patients with IBD. Gut. 2021;70:1884–1893. doi: 10.1136/gutjnl-2021-324789. [DOI] [PubMed] [Google Scholar]
- 33.• Mahil S, Bechman K, Raharja A, et al. The effect of methotrexate and targeted immunosuppression on humoral and cellular immune responses to the COVID-19 vaccine BNT162b2: a cohort study. Lancet Rheumatol. 2021;3:e627–37. A longitudinal cohort study of humoral and cellular immune responses to the first dose of COVID-19 vaccine in individuals with psoriasis who were receiving immune-modifying therapy. [DOI] [PMC free article] [PubMed]
- 34.• Mahil S, Bechman K, Raharja A, et al. Humoral and cellular immunogenicity to a second dose of COVID-19 vaccine BNT162b2 in people receiving methotrexate or targeted immunosuppression: a longitudinal cohort study. Lancet Rheumatol. 2022;4:e42–52. A longitudinal cohort study of humoral and cellular immune responses to the second dose of COVID-19 vaccine in individuals with psoriasis who were receiving immune-modifying therapy. [DOI] [PMC free article] [PubMed]
- 35.Moor MB, Suter-Riniker F, Horn MP, et al. Humoral and cellular responses to mRNA vaccines against SARS-COV-2 in patients with a history of CD20 B-cell-depleting therapy (RITUXIVAC): an investigator-initiated, single-centre, open-label study. Lancet Rheumatol. 2021 doi: 10.1016/s2665-9913(21)00251-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rubbert-Roth A, Vuilleumier N, Ludewig B, Schmiedeberg K, Haller C, von Kempis J. Anti-SARS-CoV-2 mRNA vaccine in patients with rheumatoid arthritis. Lancet Rheumatol. 2021;3:e470–e472. doi: 10.1016/S2665-9913(21)00186-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ruddy J, Connolly C, Boyarsky B, Werbel W, Christopher-Stine L, Garonzik-Wang J, et al. High antibody response to two-dose SARS-CoV-2 messenger RNA vaccination in patients with rheumatic and musculoskeletal diseases. Ann Rheum Dis. 2021;80:1351–1352. doi: 10.1136/annrheumdis-2021-220656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seree-aphinan C, Chanprapaph K, Rattanakaemakorn P, Setthaudom C, Suangtamai T, Pomsoong C, et al. Inactivated COVID-19 vaccine induces a low humoral immune response in a subset of dermatological patients receiving immunosuppressants. Front Med. 2021 doi: 10.3389/fmed.2021.769845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seyahi E, Bakhdiyarli G, Oztas M, et al. Antibody response to inactivated COVID-19 vaccine (CoronaVac) in immune-mediated diseases: a controlled study among hospital workers and elderly. Rheumatol Int. 2021 doi: 10.1007/s00296-021-04910-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simon D, Tascilar K, Fagni F, et al. SARS-CoV-2 vaccination responses in untreated, standardly treated and anticytokine-treated patients with immune-mediated inflammatory diseases. Ann Rheum Dis. 2021;80:1312–1316. doi: 10.1136/annrheumdis-2021-220461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wieske L, van Dam KP, Steenhuis M, et al. Humoral responses after second and third SARS-COV-2 vaccination in patients with immune-mediated inflammatory disorders on immunosuppressants: a cohort study. Lancet Rheumatol. 2022 doi: 10.1016/s2665-9913(22)00034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wong S, Dixon R, Martinez Pazos V, et al. Serologic response to messenger RNA coronavirus disease 2019 vaccines in inflammatory bowel disease patients receiving biologic therapies. Gastroenterology. 2021;161:715–718.e4. doi: 10.1053/j.gastro.2021.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Naaber P, Tserel L, Kangro K, et al. Dynamics of antibody response to BNT162b2 vaccine after six months: a longitudinal prospective study. Lancet Reg Health Eur. 2021;10:100208. doi: 10.1016/j.lanepe.2021.100208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Andrews N, Stowe J, Kirsebom F, et al. Covid-19 vaccine effectiveness against the omicron (B.1.1.529) variant. N Engl J Med. 2022;386:1532–1546. doi: 10.1056/NEJMoa2119451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moss P. The T cell immune response against SARS-CoV-2. Nat Immunol. 2022;23:186–193. doi: 10.1038/s41590-021-01122-w. [DOI] [PubMed] [Google Scholar]
- 46.Skelly DT, Harding AC, Gilbert-Jaramillo J, et al. Two doses of SARS-COV-2 vaccination induce robust immune responses to emerging SARS-COV-2 variants of concern. Nat Commun. 2021 doi: 10.1038/s41467-021-25167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Park J, Lee M, Lee E, Song Y, Choi Y, Winthrop K, et al. Effect of methotrexate discontinuation on efficacy of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis. 2017;76:1559–1565. doi: 10.1136/annrheumdis-2017-211128. [DOI] [PubMed] [Google Scholar]
- 48.Mehta P, Sanchez E, Moraitis E, Longley N, Lendrem D, Giles I, et al. Influenza vaccination and interruption of methotrexate in adult patients in the COVID-19 era: an ongoing dilemma. Lancet Rheumatol. 2021;3:e9–e10. doi: 10.1016/S2665-9913(20)30392-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.• Abhishek A, Boyton R, Peckham N, et al. Effect of a 2-week interruption in methotrexate treatment versus continued treatment on COVID-19 booster vaccine immunity in adults with inflammatory conditions (VROOM study): a randomised, open label, superiority trial. Lancet Respir Med. 2022. 10.1016/s2213-2600(22)00186-2. A randomised, open label, superiority trial showing that temporary discontinuation of methotrexate for 2 weeks after COVID-19 booster vaccination in individuals with IMIDs led to greater antibody titres. [DOI] [PMC free article] [PubMed]
- 50.Schmiedeberg K, Vuilleumier N, Pagano S, Albrich WC, Ludewig B, Jvon K, et al. Efficacy and tolerability of a third dose of an mRNA anti-SARS-cov-2 vaccine in patients with rheumatoid arthritis with absent or minimal serological response to two previous doses. Lancet Rheumatol. 2022 doi: 10.1016/s2665-9913(21)00328-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Simon D, Tascilar K, Fagni F, et al. Efficacy and safety of SARS-COV-2 revaccination in non-responders with immune-mediated inflammatory disease. Ann Rheum Dis. 2021;81:1023–1027. doi: 10.1136/annrheumdis-2021-221554. [DOI] [PubMed] [Google Scholar]
- 52.• Shen C, Risk M, Schiopu E, Hayek SS, Xie T, Holevinski L, Akin C, et al. Efficacy of COVID-19 vaccines in patients taking immunosuppressants. Ann Rheumat Dis. 2022;81:875–80. Clinical effectiveness study showing that individuals receiving immune-modifying drugs (standard systemic and/or targeted immune-modifying therapy) who had a third COVID-19 vaccine dose had a lower incidence of SARS-CoV-2 infection compared to those who did not have a third dose. [DOI] [PMC free article] [PubMed]
- 53.Risk M, Hayek SS, Schiopu E, Yuan L, Shen C, Shi X. Covid-19 vaccine effectiveness against Omicron (b.1.1.529) variant infection and hospitalisation in patients taking immunosuppressive medications: A retrospective cohort study. Lancet Rheumatol. 2022 doi: 10.1016/s2665-9913(22)00216-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Coronavirus Pandemic (COVID-19). Our World in Data; 2022. https://ourworldindata.org/covid-vaccinations. Accessed 11 Jun 2022.
- 55.Bechman K, Cook E, Dand N, et al. Vaccine hesitancy and access to psoriasis care during the COVID-19 pandemic: findings from a global patient-reported cross-sectional survey. Br J Dermatol. 2022 doi: 10.1111/bjd.21042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Troldborg A, Thomsen MK, Bartels LE, et al. Time since rituximab treatment is essential for developing a humoral response to COVID-19 mRNA vaccines in patients with rheumatic diseases. J Rheumatol. 2022;49:644–649. doi: 10.3899/jrheum.211152. [DOI] [PubMed] [Google Scholar]