Abstract
Background
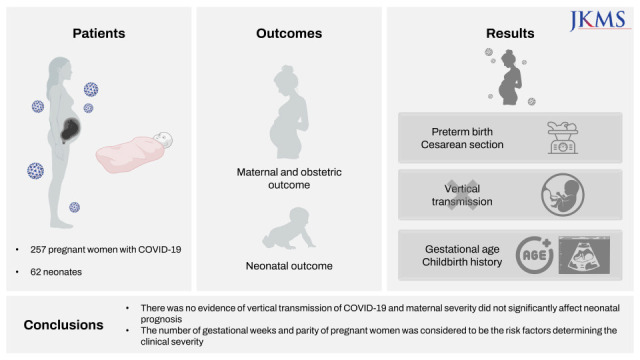
This study aimed to describe the maternal, obstetrical, and neonatal outcomes in pregnant women with coronavirus disease 2019 (COVID-19) and identify the predictors associated with the severity of COVID-19.
Methods
This multicenter observational study included consecutive pregnant women admitted because of COVID-19 confirmed using reverse transcriptase-polymerase chain reaction (RT-PCR) test at 15 hospitals in the Republic of Korea between January 2020 and December 2021.
Results
A total of 257 women with COVID-19 and 62 newborns were included in this study. Most of the patients developed this disease during the third trimester. Nine patients (7.4%) developed pregnancy-related complications. All pregnant women received inpatient treatment, of whom 9 (3.5%) required intensive care, but none of them died. The gestational age at COVID-19 diagnosis (odds ratio [OR], 1.096, 95% confidence interval [CI], 1.04–1.15) and parity (OR, 1.703, 95% CI, 1.13–2.57) were identified as significant risk factors of severe diseases. Among women who delivered, 78.5% underwent cesarean section. Preterm birth (38.5%), premature rupture of membranes (7.7%), and miscarriage (4.6%) occurred, but there was no stillbirth or neonatal death. The RT-PCR test of newborns’ amniotic fluid and umbilical cord blood samples was negative for severe acute respiratory syndrome coronavirus 2.
Conclusion
At the time of COVID-19 diagnosis, gestational age and parity of pregnant women were the risk factors of disease severity. Vertical transmission of COVID-19 was not observed, and maternal severity did not significantly affect the neonatal prognosis.
Keywords: Severe Acute Respiratory Syndrome Coronavirus 2, Coronavirus Disease 2019, Pregnancy, Neonate
Graphical Abstract
INTRODUCTION
The global pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has created a major global health concern. At the emergence of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2, the World Health Organization designated pregnant women as a vulnerable group based on preliminary studies, which reported poor obstetric and neonatal outcomes of previous outbreaks of respiratory virus infections, including SARS,1,2 Middle East respiratory syndrome (MERS),3,4 and influenza.5
The anatomical, physiological, and immunological changes that occur during normal pregnancy can have systematic effects, which make pregnant women more likely to develop complications from respiratory tract infections.6,7 However, the available data are insufficient and inconsistent to infer the impact of COVID-19 on pregnant women in terms of obstetric and neonatal outcomes. Although critical illness was relatively uncommon in both groups, the maternal and obstetric outcomes appeared to be worse in pregnant women, compared with that in non-pregnant women with COVID-19.8,9 Pregnant women will not only develop a more severe form of COVID-19 but also experience pregnancy-related complications such as preeclampsia, preterm birth, and stillbirth.9,10,11,12,13,14,15,16 However, other studies reported that with COVID-19 pregnant women have less severe consequences than those with other coronavirus infections such as SARS or MERS.17 Furthermore, the severity of COVID-19 in pregnant women is similar to that in non-pregnant women.13,14,18,19,20,21,22,23,24,25,26,27,28
In the Republic of Korea (ROK), a previous nationwide study using claims data suggested that the prevalence of COVID-19 was lower in pregnant women (0.02%) than in non-pregnant women aged 20–44 years (0.14%) from January 2020 to February 2021. The medical insurance systems in the ROK that cover all Korean citizens include the National Health Insurance (97%) and the Medical Aid program (3%), which provide easy access to medical institutions. In the ROK, at the beginning of this pandemic, all pregnant women with COVID-19 were admitted in order to receive intensive and careful management. Data concerning the impact of COVID-19 on pregnant women in Korea’s differentiated healthcare environment is extremely scarce. This fundamental information is essential to assess the clinical benefits and risks of COVID-19 vaccination for pregnant women.
This study aimed to describe the maternal, neonatal, and obstetrical outcomes of pregnant women with COVID-19; evaluate the possibility of vertical transmission; and investigate the predictors affecting the progression to severe diseases.
METHODS
Study design and population
This multicenter retrospective cohort study was conducted in 15 hospitals located in the ROK from January 2020 to December 2021. The study population included women diagnosed with COVID-19 during pregnancy and admitted to the hospital. COVID-19 was confirmed by a positive result on reverse transcription quantitative real-time polymerase chain reaction (RT-qPCR) of a nasopharyngeal swab or sputum specimen.
Each patient was classified using an 8-point COVID-19 ordinal scale developed by the National Institute of Allergy and Infectious Diseases.29 The study population was divided into two groups: those with mild diseases (≤ 4 points) and those with severe disease (≥ 5 points).
Primary and secondary outcomes
The primary outcomes of this study were to describe the maternal, obstetric, and neonatal outcomes in pregnant women with COVID-19. Maternal outcomes included intensive care unit (ICU) admission; oxygen supply including high-flow nasal cannula oxygen delivery, mechanical ventilation, and extracorporeal membrane oxygenation; renal replacement therapy; length of hospital stay; and mortality. Obstetric outcomes included preterm delivery and obstetric complications such as miscarriage, stillbirth, and premature rupture of membranes. Neonatal outcomes included vertical transmission, Apgar score, neonatal pneumonia, and death. The secondary outcome was to identify the risk factors associated with severe diseases in pregnant women.
Variables and data collection
The following data were retrieved from each hospital’s electronic medical records: maternal age, body mass index (BMI), parity, admission routes, occupation, comorbidities, gestational age at the time of diagnosis, symptoms, oxygen support, gestational complications, obstetric complications, treatment of COVID-19, laboratory findings, co-infection, length of hospital stay, mortality, gestational age at the time of delivery, mode of delivery, result of neonate COVID-19 screening, Apgar score, and neonatal complication and death.
Statistical analysis
Continuous variables were expressed as medians and interquartile ranges (IQRs), while categorical variables were expressed as frequency rates and percentages. The Kolmogorov-Smirnov test was used to determine the normality of continuous variables. The means of continuous variables were compared using independent samples t-test for parametric methods and Mann-Whitney U test for nonparametric methods. Chi-squared test or Fisher’s exact test was used to determine the normality of categorical variables. Multivariate logistic regression analysis was used to evaluate the risk factors associated with severe COVID-19 in pregnant women. Furthermore, receiver operating characteristic (ROC) curve and Youden’s index maximum principle were used to measure the area under the ROC curve (AUC) and determine the accuracy of the optimal cutoff value of all selected risk factors. All analyses were conducted using SPSS version 23.0 (IBM, Armonk, NY, USA).
Ethics statement
The study was approved by the Institutional Review Board (IRB) of Korea University Anam Hospital (IRB No. 2020AN0408). The requirement for obtaining informed consent was waived because of the retrospective nature of the study.
RESULTS
Demographic and clinical characteristics of pregnant women
A total of 257 pregnant women with COVID-19 were included in the study. The median age of the study population was 34 (IQR, 31–37) years, and 26 (10.12%) patients were aged ≥ 40 years (Table 1). Among 234 pregnant women whose parity was confirmed, 120 (51.3%) had given birth for the first time. The distribution of patients by gestational age was as follows: first trimester, 26.1%; second trimester, 33.1%; and third trimester, 40.9%. More pregnant women developed severe COVID-19 in the third trimester than those in the first or second trimester (Table 1). A total of 29 (11.3%) pregnant women had one or more underlying medical conditions. Nineteen (7.39%) pregnant women developed gestational complications (Table 1).
Table 1. Baseline characteristics of pregnant women with coronavirus disease 2019.
| Characteristics | Total pregnant women (N = 257) | Maternal disease severity | P value | ||
|---|---|---|---|---|---|
| Mild (n = 197) | Severe (n = 60) | ||||
| Age, yr | 34 (31–37) | 34 (31–37) | 34 (31–36.25) | 0.573a | |
| Age ≥ 40 yr | 26 (10.12) | 20 (10.15) | 6 (10) | 0.533b | |
| BMIe, kg/m2 | 23.63 (21.33–26.54) (n = 256) | 23.37 (21.17–26.29) (n = 196) | 24.99 (22.48–27.29) (n = 60) | 0.119a | |
| BMI ≥ 25 kg/m2 | 98/256 (38.28) | 69/196 (35.20) | 29/60 (48.33) | 0.261b | |
| Paritye | 0.361a | ||||
| 0 | 120/234 (51.28) | 97/176 (55.11) | 23/58 (39.66) | ||
| 1 | 81/234 (34.62) | 58/176 (32.95) | 23/58 (39.66) | ||
| 2 | 24/234 (10.26) | 16/176 (9.09) | 8/58 (13.79) | ||
| ≥ 3 | 9/234 (3.85) | 5/176 (2.84) | 4/58 (6.90) | ||
| Occupatione | 0.189d | ||||
| Unemployed | 155/252 (61.51) | 113/192 (58.85) | 42/60 (70) | ||
| Employed | 94/252 (37.30) | 77/192 (40.10) | 17/60 (28.33) | ||
| Student | 3/252 (1.19) | 2/192 (1.04) | 1/60 (1.67) | ||
| Trimester of SARS-CoV-2 infection | < 0.001c | ||||
| First trimester (< 14 wk) | 67 (26.07) | 66 (33.50) | 1 (1.67) | ||
| Second trimester (14–27 wk) | 85 (33.07) | 69 (35.03) | 16 (26.67) | ||
| Third trimester (≥ 28 wk) | 105 (40.86) | 62 (31.47) | 43 (71.67) | ||
| Comorbidities | 29 (11.28) | 22 (11.17) | 7 (11.67) | 1.000c | |
| Hypertension | 2 (0.78) | 2 (1.02) | 0 (0.00) | 1.000d | |
| Pregestational diabetes | 3 (1.17) | 2 (1.02) | 1 (1.67) | 0.551d | |
| Cardiac disease | 1 (0.39) | 1 (0.51) | 0 (0.00) | 1.000d | |
| Respiratory disease | 2 (0.78) | 2 (1.02) | 0 (0.00) | 1.000d | |
| Autoimmune disease | 4 (1.56) | 3 (1.52) | 1 (1.67) | 1.000d | |
| Malignancy | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A | |
| Neurologic disorder | 2 (0.78) | 2 (1.02) | 0 (0.00) | 1.000d | |
| Other comorbidities | 15 (5.84) | 10 (5.08) | 5 (8.33) | 1.000d | |
| Gestational complications | 19 (7.39) | 13 (6.60) | 6 (10) | 0.401d | |
| Gestational diabetes | 12 (4.67) | 9 (4.57) | 3 (5.00) | 1.000d | |
| Gestational hypertension | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A | |
| Gestational hypothyroidism | 3 (1.17) | 2 (1.02) | 1 (1.67) | 0.551d | |
| Other complications | 4 (1.56) | 2 (1.02) | 2 (3.33) | 0.233d | |
| Admission routes | 0.676c | ||||
| Emergency department | 52 (20.23) | 41 (20.81) | 11 (18.33) | ||
| Outpatient department | 205 (79.77) | 156 (79.19) | 49 (81.67) | ||
Values are presented as median (interquartile range) or number (%).
BMI = body mass index, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2, N/A = not available.
aIndependent sample t-test was used for testing; bMann-Whitney U test was used for testing; cChi-squared test was used for testing; dFisher’s exact was used for testing; eThe available number of participants was presented as a denominator or in brackets owing to missing data.
The most common symptom was cough (53.7%), followed by fever (48.3%), sore throat (37.0%), and sputum (30.7%) (Table 2). The severity of COVID-19 in pregnant women according to oxygen demand is presented in Table 2. The distribution of patients by clinical severity, determined using the 8-point COVID-19 ordinal scale of the National Institute of Allergy and Infectious Diseases, was as follows: 76.7% had mild disease (1 point [0%], 2 points [0%], 3 points [0%], and 4 points [100%]), while 23.3% had severe disease (5 points [75%], 6 points [21.7%], 7 points [3.3%], and 8 points [0%]). Oxygen therapy was not required in 197 (76.7%) pregnant women with COVID-19 (Table 2). On the contrary, 9 (3.5%) patients and 2 (0.78%) patients were admitted in the ICU and required mechanical ventilation, respectively. However, none of the pregnant women with COVID-19 died. With regard to the use of therapeutic agents, pregnant women received remdesivir and regdanvimab (Table 2).
Table 2. Clinical characteristics according to the COVID-19 severity in pregnant women with COVID-19.
| Characteristics | Total pregnant women (N = 257) | Maternal disease severity | P value | ||
|---|---|---|---|---|---|
| Mild (n = 197) | Severe (n = 60) | ||||
| Symptoms | 228 (88.72) | 168 (85.28) | 60 (100) | 0.002b | |
| Fever | 124 (48.25) | 76 (38.58) | 48 (80) | < 0.001b | |
| Chills | 23 (8.95) | 17 (8.63) | 6 (10) | 0.745b | |
| Myalgia | 67 (26.07) | 48 (24.37) | 19 (31.67) | 0.259b | |
| Sore throat | 95 (36.96) | 68 (34.52) | 27 (45) | 0.141b | |
| Cough | 138 (53.70) | 92 (46.70) | 46 (76.67) | < 0.001b | |
| Diarrhea | 1 (0.39) | 0 (0.00) | 1 (1.67) | 0.233c | |
| Dyspnea | 31 (12.06) | 6 (3.05) | 25 (41.67) | < 0.001b | |
| Chest pain | 4 (1.56) | 1 (0.51) | 3 (5.00) | 0.041c | |
| Nasal congestion | 68 (26.46) | 53 (26.90) | 15 (25) | 0.770b | |
| Sputum | 79 (30.74) | 54 (27.41) | 25 (41.67) | 0.039c | |
| Headache | 47 (18.29) | 34 (17.26) | 13 (21.67) | 0.439b | |
| Hypogeusia | 21 (8.17) | 16 (8.12) | 5 (8.33) | 1.000c | |
| Hyposmia | 27 (10.51) | 24 (12.18) | 3 (5.00) | 0.112b | |
| Laboratory findingsd | |||||
| Highest WBC, × 103/μL | 7.79 (6.28–10.02) (n = 256) | 7.41 (5.98–9.03) (n = 196) | 9.77 (7.55–11.89) (n = 60) | < 0.001a | |
| Lowest platelet, × 103/μL | 188.5 (157.25–222) (n = 256) | 196.5 (169–231) (n = 196) | 157.5 (128.75–194.75) (n = 60) | < 0.001a | |
| Lowest Hb, g/dL | 11.2 (10.2–2) (n = 256) | 11.4 (10.7–12.2) (n = 196) | 10.15 (9.5–11.1) (n = 60) | < 0.001a | |
| Highest ALT, IU/L | 20 (12–35) (n = 256) | 18 (12–31.25) (n = 196) | 26.5 (14–44) (n = 60) | 0.069a | |
| Highest AST, IU/L | 25.5 (18–38) (n = 256) | 23 (17–31) (n = 196) | 38.5 (26–54) (n = 60) | 0.014a | |
| Highest bilirubin, mg/dL | 0.42 (0.3–0.57) (n = 250) | 0.40 (0.30–0.55) (n = 191) | 0.52 (0.36–0.69) (n = 59) | 0.042a | |
| Highest LDH, IU/L | 209 (179–281.3) (n = 237) | 200.5 (164.75–260.5) (n = 180) | 259 (206–326) (n = 57) | 0.002a | |
| Highest creatinine, mg/dL | 0.50 (0.44–0.58) (n = 256) | 0.51 (0.44–0.58) (n = 196) | 0.48 (0.43–0.56) (n = 60) | 0.382a | |
| Highest CRP, mg/L | 12.4 (4.35–39.55) (n = 255) | 8.1 (2.6–20.1) (n = 196) | 65.1 (35.95–90.8) (n = 59) | < 0.001a | |
| Highest procalcitonin, ng/mL | 0.04 (0.02–0.07) (n = 200) | 0.04 (0.02–0.06) (n = 150) | 0.07 (0.05–0.29) (n = 50) | 0.030a | |
| Treatment | 162 (63.04) | 103 (52.28) | 59 (98.33) | < 0.001b | |
| Regdanvimab | 2 (0.78) | 1 (0.51) | 1 (1.67) | 0.413c | |
| Remdesivir | 38 (14.79) | 2 (1.02) | 36 (60) | < 0.001b | |
| Antibiotics | 52 (20.23) | 24 (12.18) | 28 (46.67) | < 0.001b | |
| Corticosteroid | 61 (23.74) | 16 (8.12) | 45 (75) | < 0.001b | |
| Antipyretics | 136 (52.92) | 85 (43.15) | 51 (85) | < 0.001b | |
| Tocilizumab | 1 (0.39) | 0 (0.00) | 1 (1.67) | 0.233c | |
| Highest level of oxygen support | < 0.001c | ||||
| None | 197 (76.65) | 197 (100) | 0 (0.00) | ||
| Nasal cannula | 41 (15.95) | 0 (0.00) | 41 (68.33) | ||
| Mask | 4 (1.56) | 0 (0.00) | 4 (6.67) | ||
| NIV or high-flow nasal cannula | 13 (5.06) | 0 (0.00) | 13 (21.67) | ||
| Mechanical ventilation | 2 (0.78) | 0 (0.00) | 2 (3.33) | ||
| Co-infection | |||||
| Respiratory virus infection | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A | |
| Bacterial infection | 16 (6.23) | 7 (3.55) | 9 (15) | 0.003c | |
| ICU admission | 9 (3.50) | 0 (0.00) | 9 (15) | < 0.001c | |
| Renal replacement therapy | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A | |
| ECMO | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A | |
| Length of hospital stay, day | 11 (9–13) | 10 (9–11) | 14 (11–17) | < 0.001a | |
| Mortality | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A | |
Values are presented as median (interquartile range) or number (%).
COVID-19 = coronavirus disease 2019, WBC = white blood cell, Hb = hemoglobin, ALT = alanine transferase, AST = aspartate transaminase, LDH = lactate dehydrogenase, CRP = C-reactive protein, ECMO = extracorporeal membrane oxygenation, ICU = intensive care unit, N/A = not available, NIV = noninvasive ventilation.
aIndependent sample t-test was used for testing; bChi-squared test was used for testing; cFisher’s exact was used for testing; dThe available number of participants was presented as a denominator or in brackets owing to missing data.
Obstetric outcomes of pregnant women
Among 257 pregnant women with COVID-19, the obstetric outcomes of 65 patients were determined. Of these, 37 (56.9%) and 28 (43.1%) patients showed mild diseases (≤ 4 points) and severe diseases (≥ 5 points), respectively. The median gestational age at delivery was 38 (IQR, 36–39) weeks, and 25 (38.5%) patients had preterm birth (Table 3). Fifty-one (78.5%) pregnant women underwent cesarean delivery and especially, all pregnant women with severe COVID-19 underwent cesarean delivery (Table 3). Premature rupture of membranes (8.2%) and miscarriage (4.6%) occurred, but none of the patients experienced stillbirth (Table 3). The frequency of preterm birth (≤ 37 weeks) was higher in pregnant women with severe COVID-19 than in those with mild COVID-19 (Table 3).
Table 3. Obstetric outcomes according to COVID-19 severity in pregnant women with COVID-19.
| Characteristics | Total obstetric outcome (N = 65) | Maternal disease severity | P value | |
|---|---|---|---|---|
| Mild (n = 37) | Severe (n = 28) | |||
| Gestational age at delivery, wk | 38 (36–39) | 38 (38–39) | 36 (35–38) | < 0.001a |
| Preterm birth (≤ 37 wk) | 25 (38.46) | 7 (18.92) | 18 (64.29) | < 0.001b |
| Preeclampsia | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A |
| Miscarriage | 3 (4.62) | 3 (8.11) | 0 (0.00) | 0.253c |
| Stillbirth | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A |
| Premature rupture of membranes | 5 (7.69) | 1 (2.70) | 4 (14.29) | 0.156c |
| Cesarean delivery | 51 (78.46) | 23 (62.16) | 28 (100) | 0.001c |
Values are presented as median (interquartile range) or number (%).
COVID-19 = coronavirus disease 2019, N/A = not available.
aMann-Whitney U test was used for testing; bChi-squared test was used for testing; cFisher’s exact was used for testing.
Neonatal outcomes
As 3 pregnant women experienced miscarriage, only 62 neonates were included in this study. Among them, 28 (45.2%) neonates were born of pregnant women with severe illness (Table 4). Vertical transmission of COVID-19 did not occur in all neonates who were delivered from pregnant women with this illness (Table 4). Interestingly, the Apgar score of neonates born of patients with severe COVID-19 was significantly higher than that of neonates born of patients with mild COVID-19 (Table 4). All neonates survived.
Table 4. Neonatal outcomes according to maternal COVID-19 severity in pregnant women with COVID-19.
| Characteristics | Total neonates (N = 62) | Maternal disease severity | P value | ||
|---|---|---|---|---|---|
| Mild (n = 34) | Severe (n = 28) | ||||
| Gender | 1.000c | ||||
| Male | 35 (56.45) | 19 (55.88) | 16 (57.14) | ||
| Female | 27 (43.55) | 15 (44.12) | 12 (42.86) | ||
| Birth weight, g | 2.81 (2.59–3.20) | 2.90 (2.69–3.32) | 2.66 (2.40–3.15) | 0.066a | |
| Normal weight (> 2,500 g) | 52 (83.87) | 31 (91.18) | 21 (75) | ||
| Low weight (< 2,500 g) | 10 (16.13) | 3 (8.82) | 7 (25) | ||
| Birth height, cm | 47.75 (46–50) | 48 (47–50.50) | 46.5 (44.75–50) | 0.018a | |
| Positive COVID-19 RT-qPCRe | N/A | ||||
| Neonatal nasopharynx | 0/42 (0.00) | 0/19 (0.00) | 0/23 (0.00) | ||
| Neonatal gastric juice | 0/6 (0.00) | 0/2 (0.00) | 0/4 (0.00) | ||
| Amniotic fluid | 0/12 (0.00) | 0/7 (0.00) | 0/5 (0.00) | ||
| Cord blood | 0/10 (0.00) | 0/6 (0.00) | 0/4 (0.00) | ||
| Vaginal fluid | 0/8 (0.00) | 0/6 (0.00) | 0/2 (0.00) | ||
| Breast milk | 0/5 (0.00) | 0/4 (0.00) | 0/1 (0.00) | ||
| Apgar scoree | |||||
| 1-minute | 8 (8–9) (n = 57) | 8 (7–9) (n = 29) | 9 (8–9) (n = 28) | 0.050b | |
| 5-minute | 9 (9–10) (n = 57) | 9 (9–10) (n = 29) | 10 (9–10) (n = 28) | 0.048b | |
| Transient tachypnea of newborn | 1 (1.61) | 0 (0.00) | 1 (3.57) | 0.452d | |
| Respiratory distress syndrome | 1 (1.61) | 0 (0.00) | 1 (3.57) | 0.452d | |
| Neonatal pneumonia | 1 (1.61) | 0 (0.00) | 1 (3.57) | 0.452d | |
| Neonatal death | 0 (0.00) | 0 (0.00) | 0 (0.00) | N/A | |
| Breastfeedinge | 16/58 (27.59) | 15/32 (46.88) | 1/26 (3.85) | < 0.001c | |
Values are presented as median (interquartile range) or number (%).
COVID-19 = coronavirus disease 2019, N/A = not available, RT-qPCR = reverse transcription quantitative real-time polymerase chain reaction.
aIndependent sample t-test was used for testing; bMann-Whitney U test was used for testing; cChi-squared test was used for testing; dFisher’s exact was used for testing; eThe available number of participants was presented as a denominator or in brackets owing to missing data.
Risk factors associated with severe COVID-19
In the multivariate logistic regression analysis, the number of gestational age at COVID-19 diagnosis (odds ratio [OR], 1.096, 95% confidence interval [CI], 1.04–1.15) and parity (OR, 1.703, 95% CI, 1.13–2.57) were significant risk factors for severe COVID-19 (Table 5). Age, BMI, gestational age at the time of infection, parity, comorbidities, and gestational complications were included in the multivariate analysis adjusted for study center.
Table 5. Results of the logistic regression analysis of the factors of severe coronavirus disease 2019 in pregnant women.
| Characteristics | Univariable OR (95% CI) | P value | Multivariable OR (95% CI) | P value |
|---|---|---|---|---|
| Age, yr | 1.017 (0.959–1.08) | 0.572 | - | - |
| BMIa, kg/m2 | 1.071 (0.993–1.155) (n = 256) | 0.074 | 0.969 (0.877–1.07) (n = 256) | 0.530 |
| Gestational age at the time of infection, wk | 1.121 (1.078–1.165) | < 0.001 | 1.123 (1.076–1.172) | < 0.001 |
| Paritya | 1.517 (1.084–2.123) (n = 234) | 0.015 | 1.466 (1.006–2.135) (n = 234) | 0.046 |
| Comorbidities | 0.557 (0.158–1.971) | 0.364 | - | - |
| Gestational complications | 0.535 (0.203–1.409) | 0.205 | - | - |
BMI = body mass index, CI = confidence interval, OR = odds ratio.
aThe available number of participants was presented as a denominator or in brackets owing to missing data.
In addition, the ROC curve of gestational age was used to determine the optimal cutoff value for high-risk patients who are likely to progress to severe illness. The AUC of the ROC curve was 0.768 (95% CI, 0.711–0.826, P < 0.001). According to Youden’s index maximum principle, the cutoff value was 21.5 weeks. The sensitivity and specificity of this cut-off value were 0.950 and 0.553, respectively.
DISCUSSION
Our study aimed to describe the maternal, obstetrical, and neonatal outcomes of pregnant women with COVID-19; evaluate the possibility of vertical transmission; and investigate the predictors affecting the progression to severe diseases. Pregnant women diagnosed with COVID-19 rarely progressed to severe COVID-19 or had poor obstetric outcomes. The possibility of vertical transmission as well as maternal or fetal mortality was not observed in our analysis. Particularly, as the parity or gestational age increased, patients tended to progress to severe diseases.
Approximately 3.5% and 0.8% patients required ICU admission and mechanical ventilation, respectively. Compared with the ICU admission and mechanical ventilation rates (3–28.5% and 1.4–12%, respectively) reported in a previous systematic review, the rates reported in the present study were extremely low.16 These discrepancies may be owing to the different study populations, unique healthcare systems, and the appropriate use of therapeutic agents.
Recent data from the Korea Disease Control and Prevention Agency showed 1 (3.27%) died and 73 (3.27%) developed severe COVID-19 among the 2,232 pregnant women with COVID-19 from January 2020 to December 2021.30 The fatality rate of pregnant women with COVID-19 was 0.04%, which was not different from that of non-pregnant women of reproductive age (20–45 years), although the incidence rate of critical illness in pregnant women (3.3%) was nine times higher than that in non-pregnant women at reproductive age (0.4%). Even in three other studies conducted in the ROK, pregnant women with COVID-19 were not at higher risk of developing a severe disease,26,27,31 which was similar to the results of previous studies conducted outside of the ROK.13,14,18,19,20,21,22,23,24,25,28
With regard to the use of therapeutic agents in pregnant women, remdesivir and corticosteroids were administered in 14.8% and 23.7%, respectively, and even those with mild diseases were prescribed these medications. The United States Food and Drug Administration assigned remdesivir and corticosteroids to pregnancy risk category B and C, respectively. Patients with severe cases included in our study were more likely to receive remdesivir or corticosteroids than those with mild cases. According to the COVID-19 treatment guidelines developed by the National Institutes of Health, the therapeutic management of pregnant patients with COVID-19 should be the same as that of nonpregnant patients.32 However, the benefit-risk balances in each single case should be considered when selecting a specific drug for the treatment of COVID-19 in pregnant patients.33
The preterm birth and cesarean section rates in the present study were relatively high (38.5% and 78.5%, respectively) compared with that (20.6–25.0% and 52.3–95.8%, respectively) in a previous systematic review.16 Preterm birth (≤ 37 weeks) and cesarean section were more frequent in pregnant women with severe disease than in those with mild diseases. The mode of delivery did not lead to the vertical transmission of COVID-19 or did not affect the neonatal outcomes.34,35,36 The selection of mode of delivery may have been based on the hospital infection control status and medical condition of pregnant women in addition to the previous history of cesarean delivery, failure of labor to progress, breech presentation, and premature rupture of membranes.34,37,38,39
Our study showed no evidence of vertical transmission in pregnant women with COVID-19. In the recent study, 1.8% of newborns of pregnant women with COVID-19 tested positive for SARS-CoV-2 on RT-qPCR, and 1% experienced antenatal and intrapartum transmission.40 The study suggested that the severity of maternal COVID-19 seemed to be associated with SARS-CoV-2 positivity in neonates.40
In this study, the Apgar score was higher in newborns of mothers with severe illness compared with newborns of mothers with mild illness. However, the 1-minute and 5-minute Apgar scores of most newborns were 7 to 10; hence, no further intervention was provided. Only 6 neonates had a 1-minute Apgar score of 5 or 6, and were equally distributed in the mild and severe groups. Furthermore, the incidence of transient tachypnea of newborn, respiratory distress syndrome, and neonatal pneumonia was not different between the two groups, and none of the neonates died. Based on the results of this study, the disease severity of pregnant women with COVID-19 did not affect the neonatal outcomes.
Our findings demonstrated that pregnant women with COVID-19 with a gestational age of ≥ 21.5 weeks and a history of childbirth were more likely to progress to severe COVID-19. In previous studies, the severity of COVID-19 in pregnant women at ≥ 20 weeks of gestation or in the third trimester was higher than that of pregnant women who had not yet reached this gestational age.17,41,42 However, opinions regarding the differences in obstetric or neonatal outcomes according to gestational age remain controversial.43
This study has some limitations. First, although the data were collected from 15 hospitals, only some of the data from the study population were included in the analysis as a small sample size. Therefore, the interpretation of the results is limited, and our findings may have limited generalizability. Second, the severity of pregnant women with COVID-19 was possibly overestimated because the data were collected from a tertiary medical institution. Third, the vaccination status of pregnant women was not investigated in this study. However, COVID-19 vaccination was initiated in the ROK from October 18, 2020. Until December 2021, only 9.8% of pregnant women were vaccinated against COVID-19 in the ROK. Therefore, the maternal outcomes associated with COVID-19 vaccination did not significantly affect the results of this study. Finally, this study was conducted on patients with COVID-19 prior to the outbreak of omicron variant. The subjects included in our study are presumed to be mainly related to the wild type, the alpha variant, and delta variant of SARS-CoV-2. Hence, our results were difficult to apply in those infected with omicron variants.
To the best of our knowledge, this multicenter cohort study was the first to investigate the maternal, obstetric, and neonatal outcomes of pregnant women with COVID-19 according to disease severity in the ROK. In conclusion, the present study showed that outcomes of pregnant women with COVID-19 were similar to those of non-pregnant women, but they were at higher risk of progression to severe disease. In pregnant women with COVID-19, the probability of vertical transmission is extremely rare, but attention should be paid to the obstetrical complications according to severity of the patient’s clinical condition. Hence, the impact of COVID-19 on pregnant women should be clarified by conducting a nationwide prospective cohort study. These fundamental data will contribute to optimized allocation of scarce resources and formulation of rational healthcare policies to overcome the COVID-19 pandemic.
ACKNOWLEDGMENTS
We would like to express our special thanks of gratitude to Hyunju Lee (Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Republic of Korea), Jee Yoon Park (Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Republic of Korea) and Joong Sik Eom (Division of Infectious Disease, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Republic of Korea) who are fighting tirelessly at the forefront of this pandemic.
Footnotes
Funding: This study was partly supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute and funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI20C0384) and by the Korea University Medicine funds raised for coronavirus disease 19 research (grant number: O2001221). The funding sources had no role in the study design, data collection, data analysis, decision to publish, or preparation of the manuscript.
Disclosure: The authors have no potential conflicts of interest to disclosure.
- Conceptualization: Yoon YK.
- Data curation: Chung Y, Kim EJ, Kim HS, Park KH, Baek JH, Kim J,1 Lee JY, Lee CS, Lim S, Kim SW, Kim ES, Shi HJ, Hong SH, Jun JB, Hong KW, Choi JP, Kim J,2 Yang KS, Yoon YK.
- Formal analysis: Chung Y, Yoon YK.
- Funding acquisition: Yoon YK.
- Investigation: Chung Y, Yoon YK.
- Methodology: Chung Y, Yoon YK.
- Project administration: Yoon YK.
- Resources: Yoon YK.
- Software: Chung Y, Yoon YK.
- Supervision: Yoon YK.
- Validation: Yoon YK.
- Visualization: Chung Y, Yoon YK.
- Writing - original draft: Chung Y, Yoon YK.
- Writing - review & editing: Chung Y, Yoon YK.
Kim J,1 Jungok Kim; Kim J,2 Jinyeong Kim.
References
- 1.Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004;191(1):292–297. doi: 10.1016/j.ajog.2003.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lam CM, Wong SF, Leung TN, Chow KM, Yu WC, Wong TY, et al. A case-controlled study comparing clinical course and outcomes of pregnant and non-pregnant women with severe acute respiratory syndrome. BJOG. 2004;111(8):771–774. doi: 10.1111/j.1471-0528.2004.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Assiri A, Abedi GR, Al Masri M, Bin Saeed A, Gerber SI, Watson JT. Middle East respiratory syndrome coronavirus infection during pregnancy: a report of 5 cases from Saudi Arabia. Clin Infect Dis. 2016;63(7):951–953. doi: 10.1093/cid/ciw412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alfaraj SH, Al-Tawfiq JA, Memish ZA. Middle East respiratory syndrome coronavirus (MERS-CoV) infection during pregnancy: report of two cases & review of the literature. J Microbiol Immunol Infect. 2019;52(3):501–503. doi: 10.1016/j.jmii.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdullahi H, Elnahas A, Konje JC. Seasonal influenza during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2021;258:235–239. doi: 10.1016/j.ejogrb.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Goodnight WH, Soper DE. Pneumonia in pregnancy. Crit Care Med. 2005;33(10) Suppl:S390–S397. doi: 10.1097/01.ccm.0000182483.24836.66. [DOI] [PubMed] [Google Scholar]
- 7.O’Day MP. Cardio-respiratory physiological adaptation of pregnancy. Semin Perinatol. 1997;21(4):268–275. doi: 10.1016/s0146-0005(97)80069-9. [DOI] [PubMed] [Google Scholar]
- 8.Zambrano LD, Ellington S, Strid P, Galang RR, Oduyebo T, Tong VT, et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status — United States, January 22–October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(44):1641–1647. doi: 10.15585/mmwr.mm6944e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 Infection: the INTERCOVID multinational cohort study. JAMA Pediatr. 2021;175(8):817–826. doi: 10.1001/jamapediatrics.2021.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021;193(16):E540–E548. doi: 10.1503/cmaj.202604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Woodworth KR, Olsen EO, Neelam V, Lewis EL, Galang RR, Oduyebo T, et al. Birth and infant outcomes following laboratory-confirmed sars-cov-2 infection in pregnancy – SET-NET, 16 Jurisdictions, March 29–October 14, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(44):1635–1640. doi: 10.15585/mmwr.mm6944e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Delahoy MJ, Whitaker M, O’Halloran A, Chai SJ, Kirley PD, Alden N, et al. Characteristics and maternal and birth outcomes of hospitalized pregnant women with laboratory-confirmed COVID-19 – COVID-NET, 13 States, March 1–August 22, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(38):1347–1354. doi: 10.15585/mmwr.mm6938e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwartz DA, Graham AL. Potential maternal and infant outcomes from (Wuhan) coronavirus 2019-nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020;12(2):194. doi: 10.3390/v12020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trocado V, Silvestre-Machado J, Azevedo L, Miranda A, Nogueira-Silva C. Pregnancy and COVID-19: a systematic review of maternal, obstetric and neonatal outcomes. J Matern Fetal Neonatal Med. 2022;35(12):2362–2374. doi: 10.1080/14767058.2020.1781809. [DOI] [PubMed] [Google Scholar]
- 15.DeBolt CA, Bianco A, Limaye MA, Silverstein J, Penfield CA, Roman AS, et al. Pregnant women with severe or critical coronavirus disease 2019 have increased composite morbidity compared with nonpregnant matched controls. Am J Obstet Gynecol. 2021;224(5):510.e1–510.12. doi: 10.1016/j.ajog.2020.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papapanou M, Papaioannou M, Petta A, Routsi E, Farmaki M, Vlahos N, et al. Maternal and neonatal characteristics and outcomes of COVID-19 in pregnancy: an overview of systematic reviews. Int J Environ Res Public Health. 2021;18(2):596. doi: 10.3390/ijerph18020596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simsek Y, Ciplak B, Songur S, Kara M, Karahocagil MK. Maternal and fetal outcomes of COVID-19, SARS, and MERS: a narrative review on the current knowledge. Eur Rev Med Pharmacol Sci. 2020;24(18):9748–9752. doi: 10.26355/eurrev_202009_23068. [DOI] [PubMed] [Google Scholar]
- 18.Li N, Han L, Peng M, Lv Y, Ouyang Y, Liu K, et al. Maternal and neonatal outcomes of pregnant women with coronavirus disease 2019 (COVID-19) pneumonia: a case-control study. Clin Infect Dis. 2020;71(16):2035–2041. doi: 10.1093/cid/ciaa352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adhikari EH, Moreno W, Zofkie AC, MacDonald L, McIntire DD, Collins RR, et al. Pregnancy outcomes among women with and without severe acute respiratory syndrome coronavirus 2 infection. JAMA Netw Open. 2020;3(11):e2029256. doi: 10.1001/jamanetworkopen.2020.29256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Handley SC, Mullin AM, Elovitz MA, Gerson KD, Montoya-Williams D, Lorch SA, et al. Changes in preterm birth phenotypes and stillbirth at 2 Philadelphia hospitals during the SARS-CoV-2 pandemic, March–June 2020. JAMA. 2021;325(1):87–89. doi: 10.1001/jama.2020.20991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pineles BL, Alamo IC, Farooq N, Green J, Blackwell SC, Sibai BM, et al. Racial-ethnic disparities and pregnancy outcomes in SARS-CoV-2 infection in a universally-tested cohort in Houston, Texas. Eur J Obstet Gynecol Reprod Biol. 2020;254:329–330. doi: 10.1016/j.ejogrb.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahlberg M, Neovius M, Saltvedt S, Söderling J, Pettersson K, Brandkvist C, et al. Association of SARS-CoV-2 test status and pregnancy outcomes. JAMA. 2020;324(17):1782–1785. doi: 10.1001/jama.2020.19124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pettirosso E, Giles M, Cole S, Rees M. COVID-19 and pregnancy: a review of clinical characteristics, obstetric outcomes and vertical transmission. Aust N Z J Obstet Gynaecol. 2020;60(5):640–659. doi: 10.1111/ajo.13204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chi J, Gong W, Gao Q. Clinical characteristics and outcomes of pregnant women with COVID-19 and the risk of vertical transmission: a systematic review. Arch Gynecol Obstet. 2021;303(2):337–345. doi: 10.1007/s00404-020-05889-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta V, Yadav Y, Sharma R, Mishra M, Ambedkar D, Gupta V. Maternal and perinatal outcomes of hospitalized COVID-19 positive pregnant women. Cureus. 2022;14(2):e21817. doi: 10.7759/cureus.21817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chung Y, Choi DH, Ilagan JG, Lee J, Yoon YK. Maternal outcomes and clinical characteristics of COVID-19 in Korean pregnant women during the early period of the pandemic. J Korean Med Sci. 2021;36(41):e290. doi: 10.3346/jkms.2021.36.e290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim SH, Choi Y, Lee D, Lee H, Kim JH, Choi ES, et al. Impact of COVID-19 on pregnant women in South Korea: focusing on prevalence, severity, and clinical outcomes. J Infect Public Health. 2022;15(2):270–276. doi: 10.1016/j.jiph.2022.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peepal P, Rath TS, Nayak S, Pendyala S. Maternal and neonatal outcomes among women with and without severe acute respiratory syndrome corona virus-2 infection: a retrospective analytical study. J Mother Child. 2022;25(2):77–85. doi: 10.34763/jmotherandchild.20212502.d-21-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Desai A, Gyawali B. Endpoints used in phase III randomized controlled trials of treatment options for COVID-19. EClinicalMedicine. 2020;23:100403. doi: 10.1016/j.eclinm.2020.100403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Korea Disease Control and Prevention Agency. The disease burden among confirmed cases of pregnant women in South Korea. [Updated 2022]. [Accessed May 20, 2022]. https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&list_no=718363&cg_code=&act=view&nPage=28 .
- 31.Ahn KH, Kim HI, Lee KS, Heo JS, Kim HY, Cho GJ, et al. COVID-19 and vaccination during pregnancy: a systematic analysis using Korea National Health Insurance claims data. Obstet Gynecol Sci. 2022 doi: 10.5468/ogs.22060. Forthcoming. DOI: 10.5468/ogs.22060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Institutes of Health (US) Coronavirus disease 2019 (COVID-19) treatment guidelines. [Updated 2022]. [Accessed May 20, 2022]. https://www.covid19treatmentguidelines.nih.gov . [PubMed]
- 33.Arco-Torres A, Cortés-Martín J, Tovar-Gálvez MI, Montiel-Troya M, Riquelme-Gallego B, Rodríguez-Blanque R. Pharmacological treatments against COVID-19 in pregnant women. J Clin Med. 2021;10(21):4896. doi: 10.3390/jcm10214896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cai J, Tang M, Gao Y, Zhang H, Yang Y, Zhang D, et al. Cesarean section or vaginal delivery to prevent possible vertical transmission from a pregnant mother confirmed with COVID-19 to a neonate: a systematic review. Front Med (Lausanne) 2021;8:634949. doi: 10.3389/fmed.2021.634949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Debrabandere ML, Farabaugh DC, Giordano C. A review on mode of delivery during COVID-19 between December 2019 and April 2020. Am J Perinatol. 2021;38(4):332–341. doi: 10.1055/s-0040-1721658. [DOI] [PubMed] [Google Scholar]
- 36.Parazzini F, Bortolus R, Mauri PA, Favilli A, Gerli S, Ferrazzi E. Delivery in pregnant women infected with SARS-CoV-2: a fast review. Int J Gynaecol Obstet. 2020;150(1):41–46. doi: 10.1002/ijgo.13166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Katz D, Bateman BT, Kjaer K, Turner DP, Spence NZ, Habib AS, et al. The Society for Obstetric Anesthesia and Perinatology coronavirus disease 2019 registry: an analysis of outcomes among pregnant women delivering during the initial severe acute respiratory syndrome coronavirus-2 outbreak in the United States. Anesth Analg. 2021;133(2):462–473. doi: 10.1213/ANE.0000000000005592. [DOI] [PubMed] [Google Scholar]
- 38.Metz TD, Clifton RG, Hughes BL, Sandoval G, Saade GR, Grobman WA, et al. Disease severity and perinatal outcomes of pregnant patients with coronavirus disease 2019 (COVID-19) Obstet Gynecol. 2021;137(4):571–580. doi: 10.1097/AOG.0000000000004339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eman A, Balaban O, Kocayiğit H, Süner KO, Cirdi Y, Erdem AF. Maternal and neonatal outcomes of critically ill pgrenant and puerperal patients diagnosed with COVID-19 disease: retrospective comparative study. J Korean Med Sci. 2021;36(44):e309. doi: 10.3346/jkms.2021.36.e309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Allotey J, Chatterjee S, Kew T, Gaetano A, Stallings E, Fernández-García S, et al. SARS-CoV-2 positivity in offspring and timing of mother-to-child transmission: living systematic review and meta-analysis. BMJ. 2022;376:e067696. doi: 10.1136/bmj-2021-067696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vousden N, Bunch K, Morris E, Simpson N, Gale C, O’Brien P, et al. The incidence, characteristics and outcomes of pregnant women hospitalized with symptomatic and asymptomatic SARS-CoV-2 infection in the UK from March to September 2020: a national cohort study using the UK Obstetric Surveillance System (UKOSS) PLoS One. 2021;16(5):e0251123. doi: 10.1371/journal.pone.0251123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kumar R, Yeni CM, Utami NA, Masand R, Asrani RK, Patel SK, et al. SARS-CoV-2 infection during pregnancy and pregnancy-related conditions: Concerns, challenges, management and mitigation strategies-a narrative review. J Infect Public Health. 2021;14(7):863–875. doi: 10.1016/j.jiph.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aydın GA, Ünal S, Özsoy HG. The effect of gestational age at the time of diagnosis on adverse pregnancy outcomes in women with COVID-19. J Obstet Gynaecol Res. 2021;47(12):4232–4240. doi: 10.1111/jog.15051. [DOI] [PMC free article] [PubMed] [Google Scholar]


