Over 1 million individuals suffer a first acute myocardial infarction (AMI) or ischemic stroke annually in the United States despite low-cost, effective primary prevention [1]. This includes statin medications, which reduce the risk of major vascular events by 30% [2]. Sub-optimal risk identification and statin treatment may be drivers of this persistent morbidity.
Prior analyses evaluating primary prevention rates have focused on the proportion of patients on statin treatment based on their low-density lipoprotein cholesterol (LDL-C) or their estimated 10-year risk based on traditional risk scores, such as the Pooled Cohort Equations (PCE) [3], [4], [5]. However, most patients in registries and in local health systems either have missing data or are ineligible for existing risk equations and must thereby be excluded from the analysis [6]. Second, there are now multiple factors beyond traditional risk scores that are available to clinicians and substantially modify our understanding of a patient's risk [7]. Without these data, risk scores may inappropriately overestimate or underestimate patient risk.
An alternative approach to evaluating the adequacy of cardiovascular risk assessment is assessing the use of preventive therapies among individuals prior to suffering a first AMI or stroke. Using a commercially insured cohort, we identified patients without known atherosclerotic cardiovascular disease (coronary artery disease, ischemic cerebrovascular disease, or peripheral arterial disease) with a first AMI or stroke hospitalization between 2004 and 2019. We determined the proportion of these patients with prescription fills for statins or alternative lipid-lowering therapies (ezetimibe or PCSK9 inhibitors) prior to the index event.
Methods
We used the Optum de-identified Clinformatics® DataMart, a database comprising administrative health claims for members of commercial and Medicare Advantage plans across all 50 states. The DataMart included medical and pharmacy claims, enrollment information, inpatient data, and clinician characteristics. The database includes approximately 87 million unique individuals from between 2003 and 2020.
We selected patients aged 18 years or older hospitalized with a primary diagnosis of an AMI or stroke (based on International Classification of Diseases [ICD]-Version 9 or Version 10 codes listed in Supplement Table 1). We excluded patients with prior diagnoses of coronary artery disease, peripheral artery disease, or stroke and patients with prior coronary artery bypass graft surgery, percutaneous coronary intervention, or peripheral artery revascularization. To limit missing data, we also excluded patients without continuous insurance enrollment for 2 years before their hospitalization.
We captured demographic characteristics, including age, sex, and race/ethnicity. Race and ethnicity are defined in mutually exclusive categories in the database: Asian, Black, Hispanic (any race), and Non-Hispanic White. We also analyzed sociodemographic data, which included level of educational attainment (less than 12th grade, high school diploma, less than bachelor's degree, bachelor's degree plus, and unknown), and household income level (<$40,000, $40,000–49,000, $50,000–59,000, $60,000–74,000, $75,000–99,000 and >$100,000). We captured medical history based on diagnosis codes within 2 years prior to hospitalization (listed in Supplement Table 1).
We identified medication fills using prescription data. We captured two other non-statin lipid-lowering therapy classes (ezetimibe or PCSK9 inhibitors) that reduce cardiovascular risk given these may be statin substitutes for patients with statin intolerance. Our primary metric was a prescription fill of statin, ezetimibe, or PCSK9 inhibitor within 2 years before their incident AMI or stroke hospitalization. As a secondary outcome, we evaluated prescription rates within 90 or 180 days before incident AMI or stroke hospitalization.
We calculated summary statistics of our baseline patient cohort. We compared patient characteristics across those who received lipid-lowering therapies versus those who did not using effect size estimates - Cramer's V for categorical variables and Cohen's d for continuous variables [8]. We assumed a difference exceeding 0.5 was a medium to large difference and a difference of 0.1–0.5 was a small difference.
To better understand prescription rates, we evaluated treatment among several subgroups. First, to determine if sub-optimal treatment was predominantly related to life-threatening comorbidities, we excluded patients with the following diagnoses: cancer, cirrhosis, dementia, end-stage renal disease, and frailty. Second, we evaluated patients who filled lipid-lowering therapies following their hospitalization. Third, lab values were available among a subgroup of patients; in this subgroup, we evaluated treatment rates among patients with an LDL-C >130 mg/dL, which has historically been considered an elevated level [9]. Finally, we evaluated treatment rates among patients with an outpatient visit with a cardiologist.
A p-value of <0.05 was considered statistically significant. Data for this project were accessed using the Stanford Center for Population Health Sciences Data Core. This study was approved by the Stanford Institutional Review Board.
Results
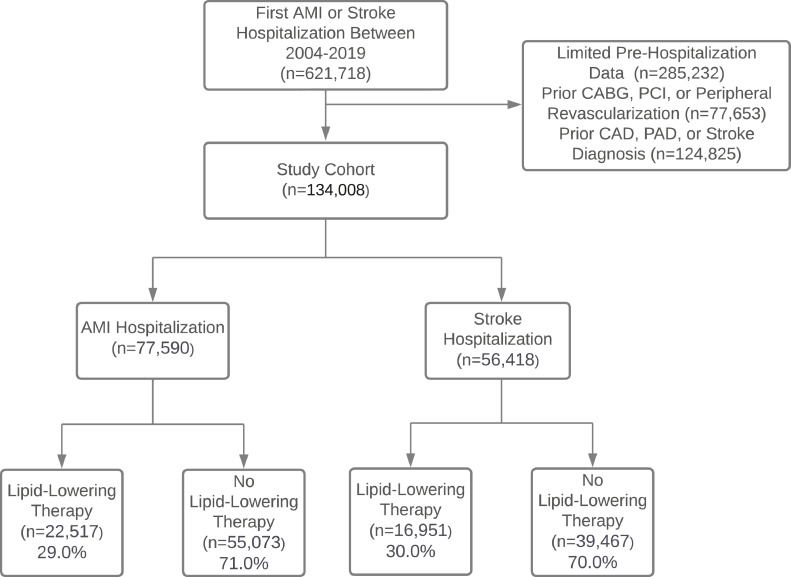
Between January 2004 and June 2019, we identified 134,008 patients without a history of ASCVD who were hospitalized for a first AMI (n = 77,590; 57.9%) or stroke (56,418; 42.1%). Fig. 1 displays the study flow diagram. The average patient age was 68.0 years (standard deviation [SD] 13.2) with 43.8% women (n = 58,731) (Table 1).
Fig. 1.
Study Flow Diagram. Abbreviations: AMI: acute myocardial infarction; CABG: coronary artery bypass graft surgery; CAD: coronary artery intervention; PAD: peripheral arterial disease; PCI: percutaneous coronary intervention. Lipid-lowering therapy counts refer to treatment with statins, ezetimibe, or PCSK9 inhibitors within the 2 years prior to the hospitalization.
Table 1.
Patient Characteristics.
| Total | Filled Statin, Ezetimibe, or PCSK9i | No Fills for Statin, Ezetimibe, or PCSK9i | Standardized Mean Differences | |
|---|---|---|---|---|
| N = 134,008 | N = 39,468 | N = 94,540 | ||
| Age, years | 68.0 (13.2) | 69.7 (11.6) | 67.3 (13.8) | 0.18 |
| Women | 58,731 (43.8%) | 18,547 (47.0%) | 40,184 (42.5%) | 0.09 |
| Race or Ethnicity | 0.05 | |||
| Asian | 3604 (2.7%)z | 1229 (3.1%) | 2375 (2.5%) | |
| Black | 14,471 (10.8%) | 4646 (11.8%) | 9825 (10.4%) | |
| Hispanic | 10,400 (7.8%) | 3629 (9.2%) | 6771 (7.2%) | |
| White | 95,649 (71.4%) | 27,071 (68.6%) | 68,578 (72.5%) | |
| Missing | 9884 (7.4%) | 2893 (7.3%) | 6991 (7.4%) | |
| Estimated Income | 0.04 | |||
| Unknown | 29,476 (22.0%) | 7982 (20.2%) | 21,494 (22.8%) | |
| <$40K | 31,769 (23.7%) | 10,079 (25.5%) | 21,690 (22.9%) | |
| $40K-$49K | 9522 (7.1%) | 2840 (7.2%) | 6682 (7.1%) | |
| $50K-$59K | 9548 (7.1%) | 2908 (7.4%) | 6640 (7.0%) | |
| $60K-$74K | 12,632 (9.4%) | 3787 (9.6%) | 8845 (9.4%) | |
| $75K-$99K | 16,344 (12.2%) | 4892 (12.4%) | 11,452 (12.1%) | |
| $100K+ | 24,717 (18.4%) | 6980 (17.7%) | 17,737 (18.8%) | |
| Educational Attainment | 0.02 | |||
| Less than high school | 755 (0.6%) | 264 (0.7%) | 491 (0.5%) | |
| Completed High School | 38,134 (28.5%) | 11,717 (29.7%) | 26,417 (27.9%) | |
| College | 70,288 (52.5%) | 20,299 (51.4%) | 49,989 (52.9%) | |
| Post-college Degree | 17,842 (13.3%) | 5064 (12.8%) | 12,778 (13.5%) | |
| Missing | 6869 (5.2%) | 2124 (5.4%) | 4865 (5.2%) | |
| Payer | 0.07 | |||
| Commercial | 61,525 (45.9%) | 16,049 (40.7%) | 45,476 (48.1%) | |
| Medicare Advantage | 72,483 (54.1%) | 23,419 (59.3%) | 49,064 (51.9%) | |
| Primary Care Visits, # | 4.6 (5.4) | 6.0 (5.6) | 4.0 (5.2) | 0.38 |
| Cardiology Visit | 12,912 (9.6%) | 5113 (13.0%) | 7799 (8.2%) | 0.16 |
| Comorbidities | ||||
| Alcohol Abuse | 5653 (4.2%) | 1320 (3.3%) | 4333 (4.6%) | |
| Atrial Fibrillation | 23,659 (17.7%) | 7449 (18.9%) | 16,210 (17.1%) | 0.05 |
| Asthma | 10,540 (7.9%) | 3580 (9.1%) | 6960 (7.4%) | 0.06 |
| Cancer | 14,359 (10.7%) | 4623 (11.7%) | 9736 (10.3%) | 0.05 |
| Chronic Kidney Disease | 18,261 (13.6%) | 7757 (19.7%) | 10,504 (11.1%) | 0.25 |
| Chronic Obstructive Pulmonary Disease | 19,618 (14.6%) | 6432 (16.3%) | 13,186 (13.9%) | 0.07 |
| Connective Tissue Disease | 7226 (5.4%) | 2322 (5.9%) | 4904 (5.2%) | 0.03 |
| Dementia | 3678 (2.7%) | 1065 (2.7%) | 2613 (2.8%) | 0.00 |
| Depression | 19,668 (14.7%) | 7276 (18.4%) | 12,392 (13.1%) | 0.15 |
| Diabetes Mellitus | 42,006 (31.3%) | 18,916 (47.9%) | 23,090 (24.4%) | 0.52 |
| Frailty | 15,739 (11.7%) | 4977 (12.6%) | 10,762 (11.4%) | 0.04 |
| Heart Failure | 25,768 (19.2%) | 8307 (21.0%) | 17,461 (18.5%) | 0.07 |
| HIV | 322 (0.2%) | 100 (0.3%) | 222 (0.2%) | 0.00 |
| Hypertension | 106,622 (79.6%) | 35,683 (90.4%) | 3785 (75.0%) | 0.39 |
| Liver Disease | 7320 (5.5%) | 2420 (6.1%) | 4900 (5.2%) | 0.04 |
| Lipid-Lowering Medications1 | — | |||
| Statin, High Intensity | 6268 (4.7%) | 6268 (16.2%) | 0 (0.0%) | |
| Statin, Intermediate Intensity | 27,615 (20.6%) | 27,615 (70.0%) | 0 (0.0%) | |
| Statin, Low Intensity | 4879 (3.6%) | 4879 (12.4%) | 0 (0.0%) | |
| Ezetimibe | 2840 (2.1%) | 2840 (7.2%) | 0 (0.0%) |
Abbreviations: HIV: Human Immunodeficiency Virus; PCSK9i: Proprotein convertase subtilisin/kexin type 9 inhibitor.
Intermediate intensity prescription includes only patients with an intermediate-intensity prescription without a high-intensity prescription. Low-intensity prescription includes only patients with a low-intensity prescription without an intermediate- or high-intensity prescription. Number of patients who filled a PCSK9 inhibitor not listed as ≤ 10 overall patients who filled a PCSK9 inhibitor before their hospitalization.
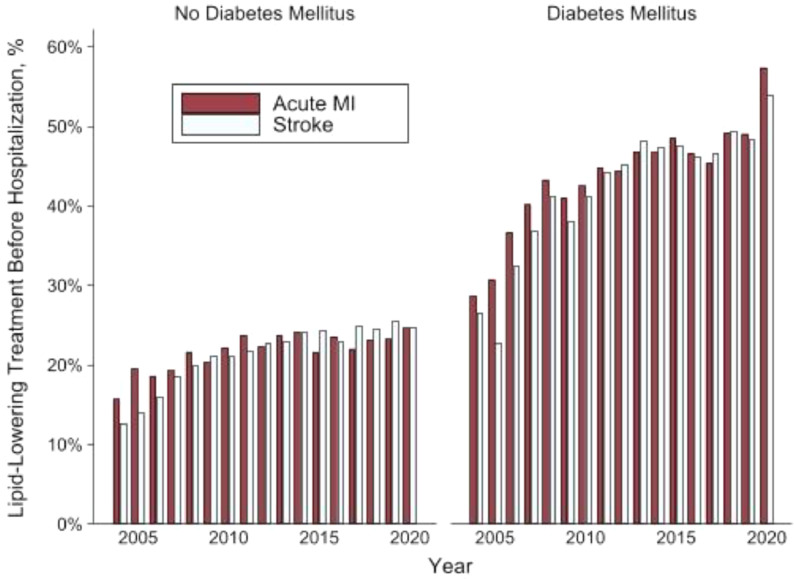
Only 29.5% (n = 39,468) of patients with a first AMI or stroke filled a lipid-lowering prescription in the 2 years preceding their hospitalization. The fill rate was 29.0% (n = 22,517) among patients with AMI and 30.0% (n = 16,951) among patients with stroke. This included 38,762 patients treated with a statin, 2840 with ezetimibe, and less than 10 treated with a PCSK9 inhibitor. Statin therapy included 6268 patients (4.7%) with a high-intensity statin prescription, 27,615 (20.6%) with a medium-intensity prescription without a high-intensity prescription, and 4879 (3.6%) with only a low-intensity prescription. An additional 706 (0.5%) of patients filled ezetimibe or a PCSK9 inhibitor without a statin prescription. The percentage of patients receiving treatment increased from 2004 through 2013 but has been steady since then (Fig. 2).
Fig. 2.
Lipid-Lowering Prescription Before AMI or Stroke Hospitalization Over Time.
Prescription rates were lower among lipid-lowering therapies in the period immediately before their hospitalization. In the 180 days pre-hospitalization, 23.0% (n = 30,763) filled one of these medications. In the 90 days pre-hospitalization, 19.6% (n = 26,263) filled a lipid-lowering medication, 19.3% before AMI (n = 14,965) and 20.0% before CVA (n = 11,298).
Patients with diabetes mellitus and hypertension were more likely to fill a prescription for lipid-lowering therapy than the overall cohort. However, even among patients with diabetes mellitus, only 45.0% (n = 18,916) had a prescription within 2 years before their event (Supplement Fig. 1).
We conducted multiple subgroup analyses. First, we evaluated treatment rates after excluding the 30,392 patients with diagnoses of cancer, cirrhosis, dementia, end-stage renal disease, or frailty. In the remaining 103,616 patients, 28.7% were treated with lipid-lowering therapy pre-hospitalization. Second, we evaluated the 94,849 patients who received lipid-lowering therapy post-hospitalization. Among this group, the fill rate pre-hospitalization was 35.5% (n = 33,638). Third, an LDL-C pre-hospitalization was available for 31,333 patients (23.4%). Among the 9442 patients with an LDL-C >130 mg/dL, the treatment rate was 37.5% (n = 3538). Finally, among the 12,912 patients seen by a cardiologist in the 2 years pre-hospitalization, the fill rate was 39.6% (n = 5113).
Discussion
Among a commercially insured cohort that suffered a first AMI or stroke hospitalization between 2004 and 2019, less than 30% filled a prescription for a statin, ezetimibe, or PCSK9 inhibitor in the 2 years pre-hospitalization. The treatment rate remained below 30% after excluding patients with cancer, cirrhosis, dementia, end-stage renal disease, or evidence of frailty, and below 40% among patients with an LDL-C >130 mg/dL pre-hospitalization. Even among patients with diabetes mellitus, treatment rates remained below 50%. For most patients who suffered a first AMI or stroke, there was a missed opportunity to lower their ASCVD risk before their AMI/stroke with statin therapy.
There are at least two potential explanations for our findings. The first is most high-risk patients are identified and appropriately treated, and, with highly effective therapy, do not suffer an AMI or stroke. The more plausible explanation is patients with elevated risk of AMI and stroke are sub-optimally identified and receive sub-optimal preventive therapy. The latter explanation is consistent with prior studies. In 2015–2016 National Health and Nutrition Examination Survey data, only 32.5% of patients with an estimated 10-year risk of ASCVD events exceeding 7.5% received statin therapy [10]. This extends beyond statin therapy to cardiovascular risk evaluation: among a cohort under the age of 55 with an AMI hospitalization, only 48.7% of females and 52.9% of males reported having been told that they were at risk for heart disease [11]. Our results further support prior work that cardiovascular risk is undertreated, which extends to patients with known ASCVD [3,12,13].
Evaluating the current quality of cardiovascular risk assessment is challenging. First, traditional risk scores cannot be calculated for many patients. Ward et al. found 48% of atherosclerotic cardiovascular events happened among patients ineligible for PCE calculation [6]. In an analysis of 941,546 patients with available lipid levels, Rana et al. found approximately 25% of patients were missing data required for PCE estimation [14]. Second, the imprecision of traditional risk assessment formulas, such as the PCE, can be improved by incorporating additional clinical data (e.g., family history) or additional testing (e.g., coronary artery calcium score or high-sensitivity C-reactive protein) [15]. Anchoring the evaluation of cardiovascular risk identification to traditional risk scores may fail to capture opportunities where clinicians could incorporate other risk factors or testing to identify high-risk individuals and intensify preventive therapies. An alternate, potential approach to evaluating the quality of cardiovascular risk assessment is to retrospectively evaluate risk identification among the high-risk cohort who end up having an AMI or stroke.
The frequency in a health system with which patients have an AMI or stroke without being on appropriate lipid-lowering therapy may be a surrogate for the quality of cardiovascular disease risk assessment. To address the identified gaps in primary prevention, there should be a focus on both promoting statin uptake among high-risk individuals and improving risk assessment. Risk assessment may be improved by incorporating additional existing data, such as longitudinal measurements of lipid levels or blood pressure. Risk assessment may also be improved by increasing the use of novel risk markers, such as coronary artery calcium scans, to help patients and clinicians in shared decision-making about statin initiation [16]. Given differences in patient populations in terms of demographics and comorbidities, expected AMI or stroke rates would likely differ across health systems and require adjustment to evaluate quality of care.
There are important limitations to our analysis. The use of claims data limits the granularity of our analysis and the accuracy of outcome ascertainment. We were unable to estimate the PCE for patients in our analysis. Diagnostic codes may also incorrectly identify AMI or stroke hospitalizations, although prior data has generally demonstrated a positive predictive value of over 80% for principal hospital diagnoses for both conditions [17], [18], [19], [20]. Second, we only evaluated diagnoses and prescription fills in the 2 years pre-hospitalization to minimize exclusions related to data completeness. Therefore, our cohort may include individuals with prevalent ASCVD without a diagnosis noted in the preceding 2 years. Third, medication fill rates do not perfectly equate to actual treatment rates and adherence, which may be even lower. Finally, a proportion of statin fills may be missed in administrative claims given low-cost prescriptions may be paid for with cash.
In a commercially insured cohort, the majority of patients hospitalized for incident AMI or stroke without a prior history of ASCVD were not previously treated with statins, ezetimibe, or PCSK9 inhibitors. This likely represents sub-optimal identification and preventive intervention among high-risk individuals. This may provide a useful metric for health systems to track appropriate identification of elevated cardiovascular disease risk.
CRediT authorship contribution statement
Alexander T. Sandhu: Conceptualization, Data curation, Formal analysis, Funding acquisition, Project administration, Writing – original draft. Fatima Rodriguez: Conceptualization, Writing – review & editing. David J. Maron: Conceptualization, Supervision, Writing – review & editing. Paul A. Heidenreich: Conceptualization, Supervision, Writing – review & editing.
Declaration of Competing Interest
Alexander Sandhu reports financial support was provided by National Heart Lung and Blood Institute. Fatima Rodriguez reports a relationship with Amgen Inc that includes: consulting or advisory. Fatima Rodriguez reports a relationship with Novartis that includes: consulting or advisory. Fatima Rodriguez reports a relationship with Novo Nordisk Inc that includes: consulting or advisory.
Funding
ATS receives research support from the National Heart, Lung, and Blood Institute (1K23HL151672-01). FR receives research support from the National Heart, Lung, and Blood Institute (5K01HL144607-02). The PHS Data Core is supported by a National Institutes of Health National Center for Advancing Translational Science Clinical and Translational Science Award (UL1TR003142) and from Internal Stanford funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2022.100426.
Appendix. Supplementary materials
References
- 1.Tsao C.W., Aday A.W., Almarzooq Z.I., Alonso A., Beaton A.Z., Bittencourt M.S., Boehme A.K., Buxton A.E., Carson A.P., Commodore-Mensah Y., Elkind M.S.V., Evenson K.R., Eze-Nliam C., Ferguson J.F., Generoso G., Ho J.E., Kalani R., Khan S.S., Kissela B.M., Knutson K.L., Levine D.A., Lewis T.T., Liu J., Loop M.S., Ma J., Mussolino M.E., Navaneethan S.D., Perak A.M., Poudel R., Rezk-Hanna M., Roth G.A., Schroeder E.B., Shah S.H., Thacker E.L., VanWagner L.B., Virani S.S., Voecks J.H., Wang N.Y., Yaffe K., Martin S.S. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 2.Chou R., Dana T., Blazina I., Daeges M., TL Jeanne. Statins for prevention of cardiovascular disease in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;316:2008–2024. doi: 10.1001/jama.2015.15629. [DOI] [PubMed] [Google Scholar]
- 3.Navar A.M., Wang T.Y., Li S., Robinson J.G., Goldberg A.C., Virani S., Roger V.L., Wilson P.W.F., Elassal J., Lee L.V., Peterson E.D. Lipid management in contemporary community practice: results from the Provider Assessment of Lipid Management (PALM) Registry. Am Heart J. 2017;193:84–92. doi: 10.1016/j.ahj.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pokharel Y., Gosch K., Nambi V., Chan P.S., Kosiborod M., Oetgen W.J., Spertus J.A., Ballantyne C.M., Petersen L.A., Virani S.S. Practice-level variation in statin use among patients with diabetes: insights from the PINNACLE registry. J Am Coll Cardiol. 2016;68:1368–1369. doi: 10.1016/j.jacc.2016.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanguturi V.K., Kennedy K.F., Virani S.S., Maddox T.M., Armstrong K., Wasfy J.H. Association between poverty and appropriate statin prescription for the treatment of hyperlipidemia in the United States: an analysis from the ACC NCDR PINNACLE registry. Cardiovasc Revasc Med. 2020;21:1016–1021. doi: 10.1016/j.carrev.2019.12.026. [DOI] [PubMed] [Google Scholar]
- 6.Ward A., Sarraju A., Chung S., Li J., Harrington R., Heidenreich P., Palaniappan L., Scheinker D., Rodriguez F. Machine learning and atherosclerotic cardiovascular disease risk prediction in a multi-ethnic population. NPJ Digit Med. 2020;3:125. doi: 10.1038/s41746-020-00331-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grundy S.M., Stone N.J., Bailey A.L., Beam C., Birtcher K.K., Blumenthal R.S., Braun L.T., de Ferranti S., Faiella-Tommasino J., Forman D.E., Goldberg R., Heidenreich P.A., Hlatky M.A., Jones D.W., Lloyd-Jones D., Lopez-Pajares N., Ndumele C.E., Orringer C.E., Peralta C.A., Saseen J.J., Smith S.C., Jr., Sperling L., Virani S.S., Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 2019;139:e1082–e1143. doi: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Serdar C.C., Cihan M., Yucel D., Serdar M.A. Sample size, power and effect size revisited: simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem Med (Zagreb) 2021;31 doi: 10.11613/BM.2021.010502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grundy S.M. National cholesterol education program -The National Cholesterol Guidelines in ATP, III. Approach to lipoprotein management in 2001 National Cholesterol Guidelines. Am J Cardiol. 2002;90:11i–21i. doi: 10.1016/s0002-9149(02)02631-0. [DOI] [PubMed] [Google Scholar]
- 10.Patel N., Bhargava A., Kalra R., Parcha V., Arora G., Muntner P., Arora P. Trends in lipid, lipoproteins, and statin use among U.S. adults: impact of 2013 cholesterol guidelines. J Am Coll Cardiol. 2019;74:2525–2528. doi: 10.1016/j.jacc.2019.09.026. [DOI] [PubMed] [Google Scholar]
- 11.Leifheit-Limson E.C., D'Onofrio G., Daneshvar M., Geda M., Bueno H., Spertus J.A., Krumholz H.M., Lichtman J.H. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO Study. J Am Coll Cardiol. 2015;66:1949–1957. doi: 10.1016/j.jacc.2015.08.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cannon C.P., de Lemos J.A., Rosenson R.S., Ballantyne C.M., Liu Y., Gao Q., Palagashvilli T., Alam S., Mues K.E., Bhatt D.L., Kosiborod M.N., Investigators G. Use of lipid-lowering therapies over 2 years in GOULD, a registry of patients with atherosclerotic cardiovascular disease in the US. JAMA Cardiol. 2021 doi: 10.1001/jamacardio.2021.1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nelson A.J., Haynes K., Shambhu S., Eapen Z., Cziraky M.J., Nanna M.G., Calvert S.B., Gallagher K., Pagidipati N.J., Granger C.B. High-intensity statin use among patients with atherosclerosis in the U.S. J Am Coll Cardiol. 2022;79:1802–1813. doi: 10.1016/j.jacc.2022.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rana J.S., Tabada G.H., Solomon M.D., Lo J.C., Jaffe M.G., Sung S.H., Ballantyne C.M., Go A.S. Accuracy of the atherosclerotic cardiovascular risk equation in a large contemporary, multiethnic population. J Am Coll Cardiol. 2016;67:2118–2130. doi: 10.1016/j.jacc.2016.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curry S.J., Krist A.H., Owens D.K., Barry M.J., Caughey A.B., Davidson K.W., Doubeni C.A., Epling J.W., Jr., Kemper A.R., Kubik M., Landefeld C.S., Mangione C.M., Silverstein M., Simon M.A., Tseng C.W., Wong J.B. Risk assessment for cardiovascular disease with nontraditional risk factors: US preventive services task force recommendation statement. JAMA. 2018;320:272–280. doi: 10.1001/jama.2018.8359. [DOI] [PubMed] [Google Scholar]
- 16.Rozanski A., Gransar H., Shaw L.J., Kim J., Miranda-Peats L., Wong N.D., Rana J.S., Orakzai R., Hayes S.W., Friedman J.D., Thomson L.E., Polk D., Min J., Budoff M.J., Berman D.S. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol. 2011;57:1622–1632. doi: 10.1016/j.jacc.2011.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kiyota Y., Schneeweiss S., Glynn R.J., Cannuscio C.C., Avorn J., Solomon D.H. Accuracy of medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148:99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 18.McCormick N., Bhole V., Lacaille D., Avina-Zubieta J.A. Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0135834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCormick N., Lacaille D., Bhole V., Avina-Zubieta J.A. Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PLoS ONE. 2014;9:e92286. doi: 10.1371/journal.pone.0092286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petersen L.A., Wright S., Normand S.L., Daley J. Positive predictive value of the diagnosis of acute myocardial infarction in an administrative database. J Gen Intern Med. 1999;14:555–558. doi: 10.1046/j.1525-1497.1999.10198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.